Abstract
Background:
Abdominal pain is a relatively frequent occurrence in sickle cell disease. The aetiology of abdominal pain in sickle cell disease is often difficult to diagnose clinically. Despite the frequent occurrence, diagnostic dilemma, and the need for an accurate, early diagnosis, abdominal pain in sickle cell disease has not been rigorously studied.
Objective:
We therefore sought to describe the different presentations and patterns of abdominal pain in persons with sickle cell disease.
Methods:
A prospective case series of 20 patients was done in which data was collected on demographic characteristics, hemoglobin electrophoresis patterns, a description of the abdominal pain including sites, severity, and type of pain, packed cell volume and the provisional and final diagnosis.
Results:
Haemoglobin S patients were 17 in number constituting eightyfive percent (85%) of our study population whilst the rest 3 were Hb S+C. Most patients (70%) had one site of abdominal pain. The pain was mainly colicky or tightening, moderate to severe in nature and, in some cases, associated with vomiting. We did not find any significant difference between the steady state PCV and the PCV during the acute abdominal pain episodes. The final diagnosis showed that only 38.8% of the patients had vasoocclusive crises and the reliability index between the provisional diagnosis and the final diagnosis was 67%.
Conclusion:
Abdominal pain in sickle cell disease may present in different ways and it is important to recognize that the possible diagnoses are numerous. Not all cases are due to vasoocclusive crises. Early diagnosis and prompt treatment can be life saving.
Keywords: Abdominal Pain, Sickle Cell Disease, Anaemia.
INTRODUCTION
Sickle Cell Disease (SCD) is defined as the inheritance of a sickle cell gene (Haemoglobin S) and another abnormal haemoglobin gene1 , 2. It is the commonest genetic condition in Africa with up to 2% of children being born with the condition in some sub-Saharan countries3. Sickle cell anaemia, the homozygous form of sickle cell disease, is the commonest SCD variant in Africa with most of the rest being haemoglobin S+C disease1. In Nigeria, where our study population is drawn from, about 150,000 children are born with sickle cell anaemia yearly3 and it appears that an increasing number of children with SCD are surviving into adulthood.
SCD has clinical manifestations in many organs which are thought to be as a result of structural changes in the haemoglobin molecule1. Pain, the hallmark of sickle cell disease, is usually the major concern of patients and their care givers. Abdominal pain is a commonly encountered form of sickle cell pain2.
Abdominal vasoocclusive crisis is thought to be secondary to vasoocclusion of mesenteric vessels, and may be a sole complaint or may be associated with pain in other parts of the body usually musculoskeleta2,4. Abdominal vasoocclusive crises may be clinically indistinguishable from acute abdominal pain from other causes and can pose a diagnostic dilemma2 , 4. Despite abdominal pain being a relatively frequent complaint in persons with sickle cell disease, and difficulty with the diagnosis, acute abdominal pain crisis has not been extensively evaluated in adult Africans with sickle cell disease.
Since the initial diagnosis is largely clinical, and decides the early line of management in most sub-Saharan settings including ours, we sought to describe the pattern of presentation and associated clinical features, the initial and the final diagnosis of abdominal pain in patients attending the haematology day care unit (HDCU) of the University College Hospital in Ibadan, South Western Nigeria.
Location
The study was conducted in the Haematology day care unit (HDCU) of the University College Hospital, Ibadan.
Methods
This study is a pioneer prospective case series of 20 consecutive SCD patients presenting with abdominal pain at the HDCU, University College Hospital, Ibadan, Nigeria over an 18-month period spanning May 2005 - Nov 2006. All participants were previously diagnosed cases of sickle cell haemoglobinopathy with prior haemoglobin electrophoresis by cellulose acetate at an alkaline medium (pH 8.4). Structured questionnaires were administered to the SCD patients presenting with abdominal pain after due consent by calibrated inter viewers (Resident doctors). Questionnaire items included sociodemographic data, clinical features, laboratory findings, treatment modalities and pain assessment (location, frequency and intensity). Pain quality assessment was based on both the numerical and descriptive scales. The numerical or nominal scale spanning 1 to 10 was employed5. Data was analyzed using version 11 of window based statistical soft ware package (SPSS). Qualitative variables were expressed as percentages and compared using Chi square statistics while quantitative variables were summarized as means, SD, and confidence intervals and further compared using either student’s t-test for two variables or analysis of variance (ANOVA) test for more than two variables.
Results
Twenty registered SCD patients aged 16 –50 years (mean 26 ± 2.07) were evaluated. Seventeen of these twenty patients (85%) were homozygous S while the rest were Hb S+C. Male to Female ratio was 1:1. Pain quality was mostly colicky or tightening. The mean pain score according to numerical scale was 5.8+ 2.2., an 11 point pain scale in which 0 is no pain, and 10 is the worst possible pain. Using the descriptive pain scale of mild, moderate or severe; majority (70%) of patients presented with moderate to severe pain. Most commonly associated symptoms were vomiting (60%) and bone pains (45%). Recurrent abdominal pain was documented in 53.8% of cases.
Majority (70%) of cases presented with one abdominal pain site while the remaining cases had multiple pain sites (double sites 15%, triple sites 5% and diffuse pain sites 10%).
The commonest single site was the epigastric region accounting for 21.41% while the lumbar, suprapubic, right upper abdomen, left upper abdomen and right iliac abdominal regions each constituted 14.3%.
Pain locations
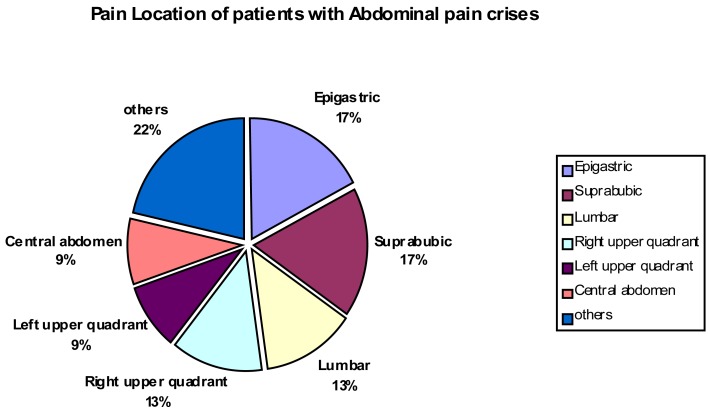
were as follows: 17.4% each for epigastric and suprapubic; 13% each for the lumbar and right upper quadrants, 8.7% each for central abdomen and left upper quadrant; other sites 21.8% (60% of which were diffuse). See figure 1
Figure 1:
Pain location and their percentages.
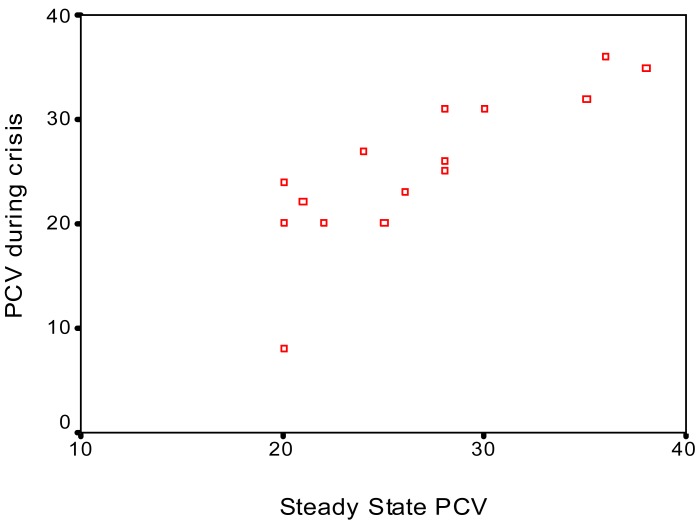
Pallor was mild in the majority (90.9%). 45% were jaundiced. Frequency of splenomegaly and hepatomegaly were 25% and 45% respectively. Steady and abdominal crisis state haematocrit showed good correlation (r = 0.838) and there was no significant difference in the mean counts (p = 0.216, see figure 2).
Figure 2:
Scatter graph showing correlation between steady and crisis states haematocrit in SCD patients presenting with abdominal pains (r = 0.838)
Management
Sixty percent (60%) of the patients seen were managed on out-patient basis while the remaining forty percent (40%) were admitted. Most commonly associated symptoms were vomiting sixty per cent (60%) and bone pains forty-five (45%). Thirty per cent (30%) of the patients had pyrexia while 40% were icteric. Patients were investigated based on the provisional diagnosis. 27.8% were co-managed with the surgical team; 11.7% had minor surgical intervention (nasogastric tube insertion and pleural tap). Patients had varying analgesia including opioids. Overall management of each case was based on the final diagnosis.
DISCUSSION
Sickle cell disease runs an extremely variable clinical course partly explained by the remarkable differences in phenotypic expression of the same genetic defect6. Climate and socioeconomic factors such as availability of early treatment of infections are thought to be major environmental determinants of the disease’s outcome 7 , 8.
Abdominal pain is a common symptom of sickle cell disease however, not all abdominal pain in sickle cell disease is due to vasoocclusive crisis. Some of the non-vasoocclusive disorders associated with abdominal pain in sickle cell disease recorded in literature include enlarged mesenteric and retroperitoneal lymph nodes, bone marrow hyperplasia, or infarction of vertebral bodies resulting in pressure on the nerve roots, hepatobiliary disease such as micro-infarction and cholelithiasis, splenic disorders like splenitis, splenic hemorrhage, splenic thrombosis, and mesenteric arterial thrombosis 9,10. Unusual causes of abdominal pain in sickle cell disease have also been reported. Of interest is that of a 21 year old patient with sickle cell anaemia who was found to have candida perihepatic abscess 11. However, many of the cases of abdominal pain have been attributed to the poorly understood abdominal vasoocclusive crises.
In our study, the sites of abdominal pain were varied and may give an indication to their aetiology. Most patients had a single site of abdominal pain (70%), commonest of which was the in the epigastric region (21%) and most of our patients described the pain as colicky or tightening. This is in contrast to Baumgartner and Klein’s 1989 report of 50% of the pain locations being diffuse12. Baumgartner and Klein also found back pain as a common associated feature which was rare in our study. 12
The commonest associated clinical feature in our study was pallor; this was probably due to the underlying chronic anaemic state, and not necessarily the abdominal pain or its cause. Hepatic and splenic enlargements were also common. The hepatic enlargement may have been secondary to cholelithiasis which occurs in about 40% to 70% of adolescent and adult sickle cell disease patients13 , 14. Both acute and chronic intrahepatic cholestasis have been associated with sickle cell disease and there are reports of increased incidences of Hepatitis B and C viral infections in these patients15,16. These increased incidences have been directly related to blood transfusion17. Our study, however, did not include serological testing for hepatitis viruses.
Splenic enlargement, a common finding in our study, appears to be universally common in young patients with sickle cell disease. Abdominal pain of splenic origin has been attributed to sequestration, hypersplenism, sepsis and splenic abscess 18. Autosplenectomy is commoner in patients with homozygous sickle cell disease who are in their adolescence or older. The presence of fever, seen in 30% of our patients, may indicate the association between an infective process and the abdominal pain. Vomiting, though common in our study, may not be very informative due to its many possible causes in the presence of abdominal pain.
Less commonly is the acute hepatic crisis which presents with right upper quadrant abdominal pain, hepatomegaly, jaundice and fever, serum aminotransferases are elevated and the hyperbilirubinemia is mainly conjugated19.
A final diagnosis of vasoocclusive abdominal pain crisis was made in about a third of our patients which again is in contrast to the 57% found by Baumgartner et al but closer to the 26% found by Akinola and colleagues12 , 20. Interestingly, the retrospective study by Akinola et al., looking at patients with sickle cell disease and abdominal pain over ten years, all the cases of abdominal pain attributable to a vasoocclusive event was in patients with homozygous sickle cell disease20. This finding is worth investigating further. Baumgartner et al. found that 23% of their study participants had a surgical entity, mostly cholecystits, as the source of the abdominal pain which was similar to the 11.1% in the study (cholecystits/cholelithiasis, partial intestinal obstruction and sub acute appendicitis)12. We emphasize the importance of early diagnosis of surgical pathologies in patients with sickle cell disease because the special pre-operative preparation required and the complications of surgery that are higher in these patients. Gastritis/gastroenteritits was the second most common diagnosis and this was not surprising because of the continual administration of non-steroidal analgesia, though it has been suggested that duodenal ulcers in homozygous sickle cell disease may be due to ischemia21.
Hepatic sequestration, which presents as right upper quadrant abdominal pain, hepatomegaly, jaundice and fever, elevated serum aminotransferases and conjugated hyperbilirubinemia was seen in one patient19. This is important because it is a commonly forgotten cause of abdominal pain in adult patients with sickle cell disease, and can rapidly lead to death from fulminant hepatitis if not managed early19.
General measures such as hydration and analgesia seem to be helpful irrespective of the diagnosis though specific management should be tailored towards the diagnosis as was done in this study.
CONCLUSION
The pattern of presentation of abdominal pain in sickle cell disease in our patients is similar to what is found in the literature though we have demonstrated that not all cases of abdominal pain in patients with sickle cell disease is due to a vasoocclusive event. A much smaller percentage of cases occur in the HbS+C. Surgical abdomen is not an infrequent cause of abdominal in patients with sickle cell disease and, as such a surgical entity should be kept in mind when evaluating sickle cell disease patients with abdominal pain. Sequestration crises of the spleen or less commonly, the liver, should be ruled out in all cases of abdominal pain in sickle cell disease (SCD) even in adult patients. This is because late diagnosis of either of these disorders may be fatal.
Even in a teaching hospital setting, only 67% of the time was the final diagnosis the same as the provisional diagnosis, underscoring the tricky nature of abdominal pain in sickle cell disease
Table 1:
Agreement scores on disorders associated with abdominal pain in SCD
| Serial no | Provisional diagnosis | Final diagnosis | Agreement score |
|---|---|---|---|
| 1. | Haemolytic crisis | Hepatic sequestration | 0 |
| 2. | Gastritis with hepatomegaly | Gastritis | 1 |
| 3. | partial intestinal obstruction | partial intestinal obstruction | 1 |
| 4. | Cystitis | Cystitis | 1 |
| 5 | Acute abdomen/intestinal obstruction | Vaso occlusive abdominal crisis | 0 |
| 6. | Food poisoning | Cholecystitis | 0 |
| 7 | Enteritis | Enteritis | 1 |
| 8. | Urinary retention | Urinary Retention | 1 |
| 9. | Abdominal vasoocclusive crisis | Abdominal vasoocclusive crisis | 1 |
| 10. | Splenic rupture | Blunt Chest Injury | 0 |
| 11. | Cholelithiasis | Cholelithiasis | 1 |
| 12. | Bone pain crisis & mild abdominal pain crisis | Bone pain crisis and mild abdominal pain crisis | 1 |
| 13. | Abdominal and bone pain crisis | Abdominal and bone pain crisis | 1 |
| 14. | Abdominal pain crisis | Abdominal pain crisis | 1 |
| 15. | Abdominal pain crisis Appendicitis | Hb S with abdominal crisis | 0 |
| 16. | Abdominal and bone pain crisis | Abdominal and bone pain crisis | 1 |
| 17. | Abdominal crisis | Gastroenteritis | 0 |
| 18. | Hb S with abdominal crisis Appendicitis | Sub-acute Appendicitis | 1 |
Reliability index between provisional and final diagnosis = 67%.
REFERENCES
- 1.Rees DC, Williams TN, Gladwin MT. Sickle-cell disease. The Lancet. 2010;376(9757 ):2018–2031. doi: 10.1016/S0140-6736(10)61029-X. [DOI] [PubMed] [Google Scholar]
- 2. Konotey-Ahulu FID. The Sickle Cell Diseases: Clinical Manifestations Including the “Sickle Crisis”. Arch Intern Med. 1974;133(4 ):611–619. [PubMed] [Google Scholar]
- 3.World health Assembly. Sickle-Cell Anaemia: Report by the Secretariat. Available at: http://apps.who.int/gb/ebwha/pdf_files/WHA59/ A59_9-en.pdf . 2006.
- 4. Ahmed S, Shahid RK, Russo LA. Unusual causes of abdominal pain: sickle cell anemia. Best Practice & Research Clinical Gastroenterology. 2005;19(2 ):297–310. doi: 10.1016/j.bpg.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 5. Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1 ):117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- 6. Chui DH, Dover GJ. Sickle cell disease: no longer a single gene disorder. Curr. Opin. Pediatr. 2001;13(1 ):22–27. doi: 10.1097/00008480-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 7. Tudawe MN, Senadheera NB, Gooneratne LV. Variations in the presentation of sickle cell beta thalassaemia - a report of two cases. Ceylon Med J. 2005;50(3 ):134–135. doi: 10.4038/cmj.v50i3.1438. [DOI] [PubMed] [Google Scholar]
- 8. Tomlinson WJ. Abdominal Crises in Uncomplicated Sickle Cell Anemia: A Clinico-Pathologic Study of 11 Cases with a Suggested Explanation of Their Cause. The American Journal of the Medical Sciences. 1945;209(6) Available at: http://journals.lww.com/amjmedsci/Fulltext/1945/06000/ABDOMINAL_CRISES_IN_UNCOMPLICATED_SICKLE_CELL.4.aspx . [Google Scholar]
- 9. Crastnopol P, Stewart CF. Acute abdominal manifestations in sickle cell disease; a report of three cases, with laparotomy in two. Arch Surg. 1949;59(5 ):993–1000. doi: 10.1001/archsurg.1949.01240041003001. [DOI] [PubMed] [Google Scholar]
- 10. Arya R, Wade J, Stephens A. An Unusual Cause of Abdominal Pain in Sickle Cell Disease. Blood. 1998;92(9 ):3477 –3478. [PubMed] [Google Scholar]
- 11. Baumgartner F, Klein S. The presentation and management of the acute abdomen in the patient with sickle-cell anemia. Am Surg. 1989;55(11 ):660– 664. [PubMed] [Google Scholar]
- 12. Malone BS, Werlin SL. Cholecystectomy and cholelithiasis in sickle cell anemia. Am. J. Dis. Child. 1988;142(7 ):799–800. doi: 10.1001/archpedi.1988.02150070113040. [DOI] [PubMed] [Google Scholar]
- 13. Bond LR, Hatty SR, Horn ME, et al. Gall stones in sickle cell disease in the United Kingdom. Br Med J (Clin Res Ed) 1987;295(6592 ):234–236. doi: 10.1136/bmj.295.6592.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Abiodun PO, Fatunde OJ, Flach KH, Buck T. Increased incidence of hepatitis B markers in children with sickle-cell anemia. Blut. 1989;58(3 ):147–150. doi: 10.1007/BF00320435. [DOI] [PubMed] [Google Scholar]
- 15. Hassan M, Hasan S, Giday S, et al. Hepatitis C virus in sickle cell disease. J Natl Med Assoc. 2003;95(10 ):939–942. [PMC free article] [PubMed] [Google Scholar]
- 16. Fasola FA, Odaibo GN, Aken'Ova YA, Olaleye OD. Hepatitis B and C viral markers in patients with sickle cell disease in Ibadan, Nigeria. Afr J Med Med Sci. 2003; 32(3 ):293–295. [PubMed] [Google Scholar]
- 17. Holt RW, Wagner R. Ultrasonic Evaluation of the Gallbladder in Sickle Cell Disease. J Natl Med Assoc. 1979;71(10 ):1027–1028. [PMC free article] [PubMed] [Google Scholar]
- 18. Woodward TA. Gastrointestinal manifiestations of sickle cell disease. Available at: http://www.dcmsonline.org/jax-medicine/2000journals/june2000/gastro.htm . 2000.
- 19. Akinola NO, Bolarinwa RA, Faponle AF. The import of abdominal pain in adults with sickle cell disorder. West Afr J Med. 2009;28(2 ):83–86. doi: 10.4314/wajm.v28i2.48429. [DOI] [PubMed] [Google Scholar]
- 20. Lee MG, Thirumalai CH, Terry SI, Serjeant GR. Endoscopic and gastric acid studies in homozygous sickle cell disease and upper abdominal pain. Gut. 1989;30(5 ):569–572. doi: 10.1136/gut.30.5.569. [DOI] [PMC free article] [PubMed] [Google Scholar]