Abstract
Introduction
White spot lesions are a common sequela of orthodontic therapy. In this parallel-group randomized trial, we assessed the effectiveness of 2 agents commonly used to ameliorate white spot lesions compared with a normal home-care regimen.
Methods
Patients aged 12 to 20 years were recruited from the offices of orthodontists and dentists who belonged to the Practice-based Research Collaborative in Evidence-based Dentistry network. The patients had their orthodontic appliances removed within the past 2 months and had at least 1 white spot lesion affecting their maxillary incisors. The subjects were randomized to 1 of 3 arms: (1) an 8-week regimen of MI Paste Plus (GC America, Alsip, Ill), (2) a single application of PreviDent fluoride varnish (Colgate Oral Pharmaceuticals, New York, NY), and (3) usual home care (control). Photographs were taken at enrollment and 8 weeks later. Two panels consisting of 5 dental professionals and 5 laypersons assessed the before-and-after pairs of photographs in a blinded fashion. Objective assessments and self-assessments were also performed.
Results
One hundred fifteen subjects completed the study; 34 were assigned to the MI Paste Plus group, 40 to the fluoride varnish group, and 41 to the control group. The mean improvements assessed by the professional panel were 21%, 29%, and 27% in the MI Paste Plus, fluoride varnish, and control groups, respectively. The results from the lay panel were 29%, 31%, and 25%, respectively. Objective improvements in the surface affected were 16%, 25%, and 17%, respectively; self-assessments of improvement were 37% in all 3 groups. No assessments indicated significant differences between subjects in the active arms compared with the control arm.
Conclusions
MI Paste Plus and PreviDent fluoride varnish do not appear to be more effective than normal home care for improving the appearance of white spot lesions over an 8-week period.
White spot lesions (WSLs), clinically defined as opaque, white areas caused by the loss of minerals below the outermost enamel layer, can be an unfortunate sequela of orthodontic treatment.1 Although prevention of these lesions is the goal of every orthodontist, the prevalence of WSLs after orthodontic treatment has been reported to be 5% to 97%.2,3 Once formed, WSLs compromise esthetics and can be extremely difficult or even impossible to reverse.
Saliva can remineralize WSLs to some degree, but this process is slow and rarely results in complete resolution of the lesions.4,5 The pattern of remineralization follows a time trend, with greater remineralization during the first few months and then continuing at a slower rate.6–8 Fluoride has been shown to increase the initial rate of remineralization.9 High doses of fluoride have been recommended during and after orthodontic treatment for arresting areas of decalcification and preventingWSLs from progressing to carious lesions. This should cause an increase in remineralization of the outer enamel and a decrease in demineralization of the inner enamel, resulting in a significant mineral gain.10–14 However, some authors warn against the use of high concentrations of fluoride because they believe this will cause remineralization mainly in the superficial part of the WSLs.15–18 This superficial layer might prevent calcium and phosphate from penetrating to the deeper layers of the enamel, thus inhibiting deeper remineralization and limiting the cosmetic improvement of the WSLs.19,20 Thus, the most ideal concentrations and delivery vehicles for fluoride remain controversial.21
In recent years, MI Paste (GC America, Alsip, Ill) has often been prescribed for remineralization of WSLs. The active agent, casein phosphopeptide-amorphous calcium phosphate, is thought to stabilize and localize calcium, fluoride, and phosphate at the tooth surface in a slow-release amorphous form, thus enhancing deeper remineralization of WSLs.22 A number of in-vitro and in-situ studies have demonstrated the remineralizing potential of casein phosphopeptide-amorphous calcium phosphate.23–32 Recent studies have investigated the remineralization potential of casein phosphopeptide-amorphous calcium phosphate combined with fluoride and have found a synergistic effect when these are administered together.25,33–37 A newer product, MI Paste Plus (GC America), containing 900 ppm fluoride and casein phosphopeptide-amorphous calcium phosphate, is now commercially available.
Few in-vivo studies have investigated the effectiveness of remineralization products to address the appearance of WSLs after orthodontic treatment. With that in mind, we conducted this randomized trial of 2 commercially available products, MI Paste Plus and PreviDent fluoride varnish (Colgate Oral Pharmaceuticals, New York, NY), to assess their clinical effectiveness over an 8-week period.
Our objective was to compare the effectiveness of MI Paste Plus and PreviDent fluoride varnish (22,600 ppm of fluoride) with a standard oral hygiene regimen with toothpaste (1100 ppm of fluoride; Colgate Oral Pharmaceuticals) (control group) in improving the appearance of WSLs after orthodontic treatment. The results were (1) assessed by 2 blinded panels (expert panel and lay panel), using subjective measures; (2) assessed by 2 blinded examiners using objective measures; and (3) measured by the subjects’ self-assessments.
MATERIAL AND METHODS
This was a randomized (1:1:1), single-blind, 3- armed, active-controlled, parallel-group trial. The trial was registered at ClinicalTrials.gov.
The study began in April 2010 in private orthodontic and general dentistry offices as part of the Practice-based Research Collaborative in Evidence-based Dentistry network (PRECEDENT). The network was operated jointly by the University of Washington and the Oregon Health and Science University, and it comprised a region of northwest states—Washington, Oregon, Montana, Idaho, and Utah—(NW PRECEDENT). The study was approved by the NW PRECEDENT Protocol Review Committee and the Human Subjects Review Committee at the University of Washington.
Eligible patients were recruited consecutively from the offices of NW PRECEDENT orthodontists and general dentists if they met the following eligibility criteria: completed fixed appliance orthodontic therapy within the past 2 months in the participating orthodontist’s or dentist’s office, had at least 1 WSL on the facial surface of a maxillary central or lateral incisor that was not present before orthodontic treatment (assessed with pretreatment photographs that were available as part of the routine initial records before orthodontic treatment), and were between the ages of 12 and 20 years. Exclusion criteria included unwillingness to be randomly assigned to 1 of the 3 treatment groups; any abnormal oral, medical, or mental condition (including any milk-related allergies and medical condition involving the kidneys); any therapy for WSLs after orthodontic treatment; any WSLs present on qualifying teeth with frank cavitation; and non-English speaking or non- English reading patients. Patients (and parents, if the patient was under 18 years old) consented before the start of the study.
The patients were randomly assigned in blocks of 3 or 6 to 1 of the 3 arms of the study.
MI Paste Plus group (intervention). These patients received an 8-week supply of MI Paste Plus at the start of the study and instructions to apply a pea-sized amount to each arch twice daily. They also received the usual home-care oral hygiene instructions and a packet with nonprescription fluoride toothpaste (1100 ppm of fluoride), a manual toothbrush, and dental floss. Compliance was checked by questions at the follow-up visit about the frequency of application of the MI Paste Plus.
Fluoride varnish group (intervention). These patients received 0.4 mL of 5% sodium fluoride varnish (22,600 ppm of fluoride, PreviDent) as a single application at the start of the study. They also received the usual home-care oral hygiene instructions and a packet with nonprescription fluoride toothpaste (1100 ppm of fluoride), a manual toothbrush, and dental floss.
Home-care group (control). These patients received the usual home-care oral hygiene instructions and a packet with nonprescription fluoride toothpaste (1100 ppm of fluoride), a manual toothbrush, and dental floss.
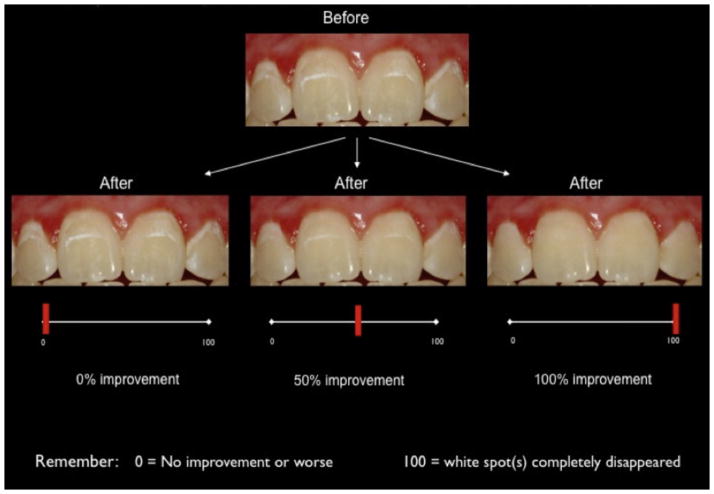
Each NW PRECEDENT provider and staff member completed study training before the enrollment of the patients. Calibration of the photographic protocols to standardize magnification, color, and shade was performed. Photographs were taken digitally as intraoral frontal views with the patient’s head tilted up approximately 5° to 10° to limit reflection from the flash to the incisal third of the maxillary incisors. Several digital photographs were taken at each time point to allow selection of the optimal image. The photographs (Fig 1) were cropped to include only the 4 maxillary incisors, adjusted for brightness, color matched between sets, and saved in a 3000 × 1200 pixel 24-bit bitmap format with Photoshop (CS3 extended version 10.0.1; Adobe, San Jose, Calif). The NW PRECEDENT provider supervised all study-related activities, certified the accuracy of data collection, and authorized the data transmission. A baseline data form was completed during enrollment with the following information from the patient’s chart: length of the patient’s orthodontic treatment, date of removal of the orthodontic appliances, type of retainers used, oral hygiene status during treatment, and prior history of therapy to treat WSLs. The patient’s general or pediatric dentist was informed about his or her participation in the study and asked not to introduce any additional treatments for WSLs during the trial. Photographs were obtained when the intervention was begun and at follow-up 8 weeks later. If a patient was recruited on the day of removal of the fixed orthodontic appliances, the intervention photographs were delayed several days to coincide with the day of retainer delivery (typically 2–7 days after removal of the appliances). The rationale for delaying the intervention a few days was to allow resolution of gingival inflammation that might have masked portions of the WSLs and to allow the enamel to hydrate to physiologic levels after removal of the orthodontic adhesives. At the 8-week follow-up visit, the patient had posttreatment photographs and completed a questionnaire about satisfaction with the treatment, compliance, oral hygiene practices, and self-assessment of the percentage of improvement of the WSLs on a 100-mm visual analog scale. All data collection forms and photographs were uploaded through a secure online data transfer system maintained by the Axio Research Corporation (Seattle, Wash).
Fig 1.

Examples of before-and-after photos.
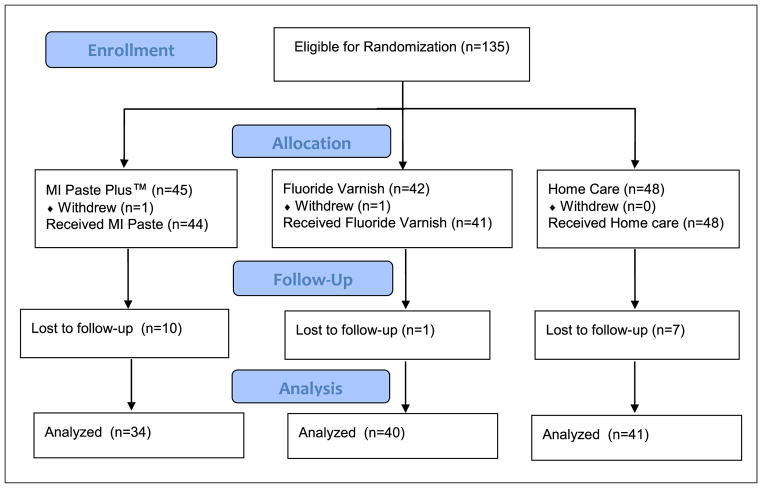
The primary outcomes with respect to the effectiveness of the MI Paste Plus and the PreviDent fluoride varnish were the mean percentages of improvement of the WSLs from entry to the 8-week follow-up with both subjective and objective assessments. For the subjective assessment, 2 blinded panels rated the improvement in WSL over the 8-week period using a visual analog scale. The first panel consisted of 5 dental experts (2 women, 3 men: 3 general dentists, 2 orthodontists). The second panel consisted of 5 laypersons (3 women, 2 men). The cropped and color-matched before-and-after images for each patient were imported into a Power-Point (Microsoft, Redmond, Wash) slide with a black background. The raters then viewed these paired images on a laptop computer. To assist with calibration of the assessors, each examiner’s session began with instructions on the rating system, as well as several example sets of before-and-after images, altered in Photoshop to demonstrate improvements of 0%, 50%, and 100% (Fig 2). The examiners evaluated the esthetic improvements of the paired images using the visual analog scale from 0 to 100 mm (0 mm, no improvement or worsened, to 100 mm, WSL completely disappeared). Each examiner performed the evaluation independently, and the order of the patients was shuffled to prevent bias from examiner fatigue. For each patient, the median value of the visual analog scores in each panel was selected to represent the percentage of improvement for that patient. For example, if the 5 examiners in the lay panel judged improvement to be 15%, 19%, 23%, 24%, and 35% for a particular patient, the median value for that patient would be 23%. To assess intraexaminer reliability, a random sample of 20 image pairs was selected for double evaluation by each rater with at least a week between evaluations.
Fig 2.
Calibration photo.
Two examiners (a dental student and a general dentist) performed the objective assessments of the WSLs. Both were blinded to the treatment arms. They assessed the same initial and follow-up images used for the subjective assessments. These images were measured side by side to allow for exclusion of preexisting enamel variations and increase the examiner’s consistency and reliability. The WSLs and the total tooth surface area of the 4 maxillary incisors were outlined by using the “freehand selection” tool with a Genius MousePen 8 × 6 tablet (KYE Systems America, Miami, Fla) in the software program Image J (version 1.39; National Institutes of Health, Bethesda, Md). The total surface area of the WSLs of the 4 maxillary incisors was divided by the total surface area of the 4 maxillary incisors, and an average of the 4 teeth was calculated, resulting in the pretreatment and posttreatment proportions of WSLs relative to the total surface area of the 4 incisors. The change in percentage of the area affected was obtained by subtracting the posttreatment proportion from the pretreatment proportion. When this resulted in a negative value (ie, the percentage of the area of the affected teeth appeared to increase for a subject), a value of zero was assigned to the change score to standardize the scale used in the objective and subjective assessments. The same 20 sets of duplicates used in the subjective assessment were measured side by side a week apart to determine intraexaminer reliability.
An a-priori power analysis was conducted to determine the required number of patients to assess the influence of the 2 treatments on the reduction of WSLs. Data from 2 studies provided estimates of standard deviations of percentage changes in lesion size directly after fixed orthodontic appliance removal.6,8 The average percentage of reduction in WSL area was 50% (SD, 27%). Time course curves in both articles appeared to indicate that the reductions at 26 and 52 weeks, respectively, would be 20% greater than the reduction at 8 weeks, the length of the follow-up for this study. At a sample size of 120 subjects, the study was calculated to have good power (80%) to detect a 20% difference in WSL improvement on the visual analog scale, if the standard deviation was 25%. These estimates assumed a 10% loss to follow-up and nominal significance levels of 0.025 for each between-group comparison.
The randomization sequence was created by using statistical software (Axio Research) and was stratified by each office by using random block sizes of 3 and 6. The random block sizes were used to prevent practitioners from guessing patient assignments. The allocation sequence was concealed from the office during enrollment, and patients were consecutively enrolled as inclusion criteria were met. After informed consent was obtained and baseline enrollment forms were completed, the NW PRECEDENT office phoned Axio Research to receive the patient’s treatment assignment.
NW PRECEDENT providers, staff, and patients were aware of their allocated arm, but the outcome assessors and the study investigators were kept blinded to the study arms until completion of the statistical analyses.
All patients in the study received their assigned treatment and a small gift for participating in the study. A data safety monitoring board, composed of persons not directly involved in patient care or data collection, periodically reviewed accumulated data for evidence of adverse or beneficial treatment effects, a need for modification of study protocols, and assessment of data quality and clinic performance.
Statistical analysis
Analyses were conducted by using SAS software (version 9.2; SAS Institute, Cary, NC) on a Windows operating system (Microsoft).
Demographic data were summarized by using frequency tables with 95% confidence intervals for proportions.
The first aim was to compare the active treatments (MI Paste Plus, PreviDent fluoride varnish) with the control (standard oral hygiene with fluoride toothpaste) in their overall WSL percentages of improvement (ie, the mean of the medians of the visual analog scores). Expert and layperson scores were considered to be separate outcomes. Therefore, this aim comprised 2 hypothesis tests for each type of assessment with a significance threshold of an alpha of 0.025 for each comparison: no difference between active treatment and control in median expert visual analog scale ratings, and no difference between active treatment and control in median layperson visual analog scale ratings.
The second aim compared the objective assessment of WSL improvement: no difference between active treatment and control in the objective ratings.
The third aim compared the patient’s self-assessment of improvement: no difference between active treatment and control in self-assessed improvement.
The analyses for the aims were performed by using a linear regression model, accounting for possible effects associated with age, sex, and initial WSL severity. The methods of generalized estimating equations were incorporated into these models to account for possible correlations between patients from the same orthodontic practice. The effect of interest was the mean percentage of improvement over 8 weeks.
RESULTS
A total of 135 patients were eligible for randomization into the study (Fig 3). Twenty participants withdrew or were lost to follow-up between the start and the end of the study, including 11 from the MI Paste Plus group, 2 from the PreviDent group, and 7 from the home-care control group. They did not vary with respect to demographic data and initial WSL severity compared with the subjects who completed the study.
Fig 3.
Flow diagram of study.
Using the 20 sets of duplicate measurements, the intracluster correlation coefficients for the lay panel, the expert panel, and the objective raters were 0.71, 0.72 and 0.85, respectively, indicating good reliability.
A total of 115 participants (56 boys, 59 girls; mean age, 14.4 ± 1.5 years) finished the study and had complete records for analyses. The primary analysis was intention to treat and involved all patients who were randomly assigned. The 3 groups were well matched in all characteristics at enrollment (Table I). Of the 115 subjects, 34 received MI Paste Plus, 41 received PreviDent, and 40 received no active treatment.
Table I.
Comparison of baseline characteristics across the 3 treatment arms*
| Treatment group | ||||
|---|---|---|---|---|
| MI Paste Plus (n = 34) | PreviDent fluoride varnish (n = 40) | Home care (n = 41) | All (n = 115) | |
| Age (y) | 14.6 (1.4) | 14.4 (1.5) | 14.3 (1.5) | 14.4 (1.5) |
| Female | 15 (44%) | 23 (58%) | 21 (51%) | 59 (51%) |
| Race/ethnicity | ||||
| Non-Hispanic white | 19 (56%) | 23 (58%) | 25 (61%) | 67 (58%) |
| Other or multiple race | 6 (18%) | 3 (8%) | 4 (10%) | 13 (11%) |
| Unreported | 9 (26%) | 14 (35%) | 12 (29%) | 35 (30%) |
| Number of teeth affected by WSL (1–4) | 3.3 (1.0) | 3.2 (0.9) | 3.2 (1.1) | 3.2 (1.0) |
| Initial surface area affected by WSL (%) | 11.8 (8.6) | 11.2 (6.2) | 11.5 (9.6) | 11.5 (8.2) |
| Oral hygiene level (based on latest toothbrushing and flossing habits) (%) | ||||
| Good | 3 (9%) | 2 (5%) | 5 (12%) | 10 (9%) |
| Fair | 15 (44%) | 18 (45%) | 14 (34%) | 47 (41%) |
| Poor | 16 (47%) | 20 (50%) | 22 (54%) | 58 (50%) |
| Weeks from orthodontic appliance removal to enrollment | ||||
| Mean (SD) | 1.03 (1.8) | 0.93 (1.7) | 1.5 (2.3) | 1.2 (2.0) |
| ≤1 week (%) | 24 (71%) | 31 (78%) | 27 (66%) | 82 (71%) |
| Weeks from baseline to follow-up photograph | 9.5 (4.6) | 9.6 (3.0) | 11.0 (6.8) | 10.1 (5.1) |
For the continuous variables, the values reported are means (and standard deviations). For categorical variables, count (%).
The mean improvements assessed by the expert panel were 21%, 29%, and 27% in the MI Paste Plus, Previ- Dent, and home-care control groups, respectively (Table II). The results from the lay panel were 29%, 31%, and 25%, respectively. The objective improvement scores were 16%, 25%, and 17%, and the self-assessed improvement scores were 37% in all 3 arms. Differences with 95% confidence intervals between the active treatment groups and the control group, after adjustment for Dental Practice-based Research Network office, age, sex, and WSL severity, are presented in Table III. No statistically significant differences were observed when comparing either active group with the control group. The differences in adjusted improvement between the active treatment groups and the control group did not differ by more than ± 6% for any comparison. The estimates of intracluster correlation coefficients for the various types of assessment within practices were the following: expert judges, 0; lay judges, 0.01; objective assessment, 0; and self-assessment, 0.23.
Table II.
Improvement scores by treatment group
| Assessment | MI Paste Plus (n = 34)
|
PreviDent fluoride varnish (n = 40)
|
Normal home care (n = 41)
|
All (n = 115)
|
||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Expert panel | 21.1 | 21.6 | 28.5 | 25.9 | 27.3 | 22.7 | 25.9 | 23.6 |
|
| ||||||||
| Lay panel | 29.4 | 23.2 | 31.0 | 25.9 | 25.4 | 23.5 | 28.5 | 24.2 |
|
| ||||||||
| Objective | 15.7 | 19.3 | 24.6 | 24.3 | 17.2 | 18.6 | 19.3 | 21.1 |
|
| ||||||||
| Self | 37.0 | 26.9 | 37.3 | 27.9 | 36.9 | 27.8 | 37.0 | 27.3 |
Table III.
Difference in mean improvement scores between the active treatment groups and the control group*
| Assessment | MI Paste Plus
|
PreviDent fluoride varnish
|
||||||
|---|---|---|---|---|---|---|---|---|
| MI Paste Plus-control* | 95% CI | P value | PreviDent-control* | 95% CI | P value | |||
| Expert panel | −6.2 | −19.1 | 6.7 | 0.35 | 1.2 | −11.8 | 14.2 | 0.85 |
|
| ||||||||
| Lay panel | 3.1 | −7.0 | 13.2 | 0.55 | 5.1 | −7.8 | 18.0 | 0.44 |
|
| ||||||||
| Objective | −3.8 | −11.6 | 3.9 | 0.33 | 6.2 | −5.3 | 17.7 | 0.29 |
|
| ||||||||
| Self† | 1.2 | −9.1 | 11.4 | 0.83 | −0.66 | −12.0 | 10.7 | 0.91 |
CI, Confidence interval.
Adjusted for office, age, sex, and initial severity;
Only 39 subjects in the varnish group.
Overall, the lay panel’s assessments were slightly higher than those of the expert panel (Table II). The objective measurements tended to be slightly lower than the subjective measurements (6.6% lower than the expert assessments and 9.2% lower than the lay assessments). The self-assessment scores showed the greatest improvements: 11.1% higher than the expert panel and 8.5% higher than the lay panel.
Scattergrams of the improvement in WSLs over 8 weeks, stratified by assessment group and treatment arm, indicated wide variations of improvement among the subjects (Fig 4). There tended to be more scores in the lower half of the improvement scale than in the upper half.
Fig 4.
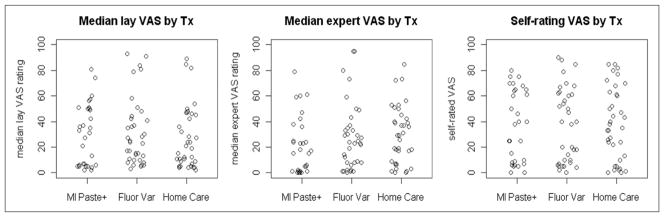
Scattergrams for improvement in WSL (displayed by assessment method and then treatment arm). VAS, Visual analog scale; Tx, treatment.
DISCUSSION
Despite the many treatments that have been proposed for WSLs, in this randomized controlled clinical trial, we did not find that either of 2 common therapies was better than regular home care (nonprescription fluoride toothpaste) for improving the appearance of WSLs over an 8-week period. Each assessment method resulted in similar levels of improvement across the 3 treatment groups. Although in-vitro studies are certainly valuable in assessing the ability of agents to remineralize enamel, this randomized trial illustrates the importance of conducting in-vivo studies and using patient-centered outcomes.
The results of this study agree with several other clinical trials. One recent randomized clinical compared casein phosphopeptide-amorphous calcium phosphate with fluoride paste with a control paste, by using quantitative laser fluorescence images to measure WSL regression. The authors reported that, at 6 and 12 weeks, the size of the lesions did not change significantly over time or between the groups.38 They concluded that there was no clinical advantage for the use of the casein phosphopeptide-amorphous calcium phosphate with fluoride paste supplementary to normal oral hygiene over 12 weeks. In a randomized trial conducted in Europe, 60 healthy adolescents with at least 1 WSL received either a daily application of casein phosphopeptide-amorphous calcium phosphate (Tooth Mousse) or standard fluoride toothpaste.39 The intervention period was 4 weeks, and the endpoints were quantitative laser fluorescence and visual scoring (Gorelick scale) from digital photographs. The mean areas of the lesions decreased by 26% to 58% in the study, but no significant differences were found between the casein phosphopeptide-amorphous calcium phosphate and the control groups. Another randomized trial compared WSLs treated with a low-fluoride mouthrinse (50 ppm) to those treated with a nonfluoride mouthrinse.8 At 12 weeks, the lesions had decreased by 40% (SD, 14.5) in the treatment group and by 51.5% (SD, 12.3) in the control group, indicating no significant benefit from the low-level fluoride.
In contrast to our results, several randomized clinical trials reported a beneficial effect from either supplemental fluoride or casein phosphopeptide-amorphous calcium phosphate. For example, a high-concentration fluoride varnish was shown to be effective in reversing WSLs at 3-month and 6-month follow-ups after debonding. 40 In this study, varnish was applied every month during the first 6 months after debonding. Another randomized clinical trial compared patients who used fluoridated chewing sticks impregnated with 0.5% sodium fluoride with nonfluoridated chewing sticks.41 The authors reported that fluoridated chewing sticks had a stronger remineralization effect on WSLs compared with the controls over a 6-week period. In a randomized trial comparing casein phosphopeptide-amorphous calcium phosphate cream (Topacal) with a 0.05% sodium fluoride mouthwash and fluoridated dentifrice combination, the subjects in both groups demonstrated improvements.42 However, the casein phosphopeptide-amorphous calcium phosphate group was associated with a greater number of WSLs that totally disappeared after 12 months (63% of the sites, compared with 25% in the control group). Another trial randomized 45 adolescents to 10% casein phosphopeptide-amorphous calcium phosphate paste (Tooth Mousse) or a control (placebo) cream.43 Over a 12-week period, the authors reported that 31% more WSLs had regressed with the remineralizing paste than with the placebo. A final randomized trial assessed regression of WSLs during the initial period of orthodontic treatment.44 MI Paste was reported to significantly reduce WSLs, compared with a placebo paste.
Because of the conflicting nature of the current WSL remineralization literature, it is difficult to determine whether various agents are effective. Additional studies are warranted, and this topic is being actively investigated. At least 5 randomized trials registered at ClinicalTrials.gov indicated that they are recruiting subjects for WSL studies.45 Currently, no systematic review specifically addressing remineralization of WSLs after orthodontic treatment has been published. A review on this topic could assess the strengths and limitations of the published studies and would certainly help clinicians weigh the effectiveness of various remineralization agents.
The patients in our study exhibited a wide range of improvement. Since our results indicated that the interventions were not a major factor in the amount of improvement, perhaps other factors might be related to the degree of improvement. Although the subjects in each arm appeared to be well matched, we plan to conduct additional analyses to determine whether there are any predictors for the degree of improvement that was observed, such as time since removal of appliances or severity of lesions. In the MI Paste Plus group, we did not find a relationship between compliance with the product and the amount of improvement.
There were several challenges to conducting this study in a network setting. Photographic assessment is commonly used for clinical assessment of WSLs.46–48 However, in a multisite trial, special attention must be given to the varying photographic systems and protocols used by network offices. The offices were carefully trained and calibrated before the study to standardize image quality. Others have used digital photographs for evaluation of dental outcomes, and they reported this to be a reproducible and reliable method for evaluating WSLs.49–52 During photo calibration with each NW PRECEDENT provider, it was recommended to angle the patient’s head about 5° to 10° to minimize flash reflections; this follows the advice of Benson et al,53 who found that the camera should be angled no more than 20° to the perpendicular of the buccal surface.
Another challenge was tracking the patients in multiple offices as the trial progressed. Follow-up visits were sometimes difficult to schedule in busy practices. To help with this issue, a study coordinator was assigned to assist offices with tracking and recalling patients for their follow-up visits.
A limitation to our study design was a lack of blinding for patients and providers. Theoretically, placebo varnishes and pastes could have been formulated. However, we thought that blinding of the evaluators was the most important factor in preventing biased assessments. Another limitation was the dropout rate, which was slightly greater than planned. Our actual dropout rate was 15%, compared with the 10% we had expected, even though a study coordinator was assigned to assist with patient recall. We also were unsure why the MI Paste Plus group experienced the highest rate of patients lost to follow-up. Although we had a higher dropout rate than planned, the final study numbers were actually greater than planned, since we enrolled more than the goal of 120. A priori, we powered the study to detect a 20% difference in WSL improvement, with an estimated standard deviation of 25%. The confidence intervals based on our data ruled out differences of more than 19%, and the standard deviations associated with our data were close to our estimate.
There were many strengths to this study. The study design was a randomized controlled trial, the subjects were recruited from 20 offices in a 5-state region, and the primary outcome was a parameter that was important to patients. Because the study was conducted in a network of providers, these results should have good generalizability to other populations of orthodontic patients. Additionally, all groups were comparable at enrollment, and the results were consistent when adjusted for office, age, sex, and initial severity. All examiners were blinded to the study arms during assessment. The intracluster correlation coefficients for practices indicated that the site of treatment was minimally related to the amount of WSL improvement, as judged by the various assessments, other than for the patient self-reports.
Regarding assessment methods, we used multiple judges and multiple methods to thoroughly investigate improvement over the 8-week period. The 8-week period was chosen to capture the time when the greatest change was expected, while minimizing loss to follow-up. Our objective method assessed a proportional change in the affected surface area, compared with the entire surface area of the incisors. Most relevant articles from a literature review used proportional8,37,48,50,51 rather than absolute measurements of luminance or size.52,54 Other studies have used a combined scoring system based on the surface area and severity of the opacity.2,55–57 These scales can be deceiving because they might be insensitive to moderate and small changes in areas of WSLs.7 Using a proportional change for the objective method may be better because of slight differences in magnification and angulations of the teeth.
With respect to visual assessment of improvement, we thought that this outcome, assessed by dental experts, laypersons, and the patients themselves, was most important, since it demonstrated the changes that will be perceived by the patients, their peers, and their health care providers. These multiple methods all indicated that there was no evidence for a difference in the improvement of WSLs between the 3 study arms. Laser fluorescence and quantitative light-induced fluorescence have also been used to assess WSLs and could have provided another method of assessment. However, the use of this technology in our multisite trial was not feasible because of budget limitations.
CONCLUSIONS
In this randomized controlled trial, we did not find a difference in the effectiveness of MI Paste Plus or PreviDent fluoride varnish compared to a standard oral hygiene and toothpaste regimen for ameliorating WSLs during an 8-week period.
Acknowledgments
Supported by the National Institute of Dental and Craniofacial Research.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Murphy TC, Willmot DR, Rodd HD. Management of postorthodontic demineralized white lesions with microabrasion: a quantitative assessment. Am J Orthod Dentofacial Orthop. 2007;131:27–33. doi: 10.1016/j.ajodo.2005.04.041. [DOI] [PubMed] [Google Scholar]
- 2.Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81:93–8. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 3.Boersma JG, van der Veen MH, Lagerweij MD, Bokhout B, Prahl-Andersen B. Caries prevalence measured with QLF after treatment with fixed orthodontic appliances: influencing factors. Caries Res. 2005;39:41–7. doi: 10.1159/000081655. [DOI] [PubMed] [Google Scholar]
- 4.Dirks OB. Posteruptive changes in dental enamel. J Dent Res. 1966;45:503–11. [Google Scholar]
- 5.Karlinsey RL, Mackey AC, Stookey GK, Pfarrer AM. In vitro assessments of experimental NaF dentifrices containing a prospective calcium phosphate technology. Am J Dent. 2009;22:180–4. [PubMed] [Google Scholar]
- 6.Al-Khateeb S, Forsberg CM, de Josselin de Jong E, Angmar-Mansson B. A longitudinal laser fluorescence study of white spot lesions in orthodontic patients. Am J Orthod Dentofacial Orthop. 1998;113:595–602. doi: 10.1016/s0889-5406(98)70218-5. [DOI] [PubMed] [Google Scholar]
- 7.Shungin D, Olsson AI, Persson M. Orthodontic treatment-related white spot lesions: a 14-year prospective quantitative follow-up, including bonding material assessment. Am J Orthod Dentofacial Orthop. 2010;138:136, e1–8. doi: 10.1016/j.ajodo.2009.05.020. discussion 136–7. [DOI] [PubMed] [Google Scholar]
- 8.Willmot DR. White lesions after orthodontic treatment: does low fluoride make a difference? J Orthod. 2004;31:235–42. doi: 10.1179/146531204225022443. [DOI] [PubMed] [Google Scholar]
- 9.Ogaard B. White spot lesions during orthodontic treatment: mechanisms and fluoride preventative aspects. Semin Orthod. 2008;14:183–93. [Google Scholar]
- 10.Bishara S, Ostby A. White spot lesions: formation, prevention, and treatment. Semin Orthod. 2008;14:174–82. [Google Scholar]
- 11.Castellano JB, Donly KJ. Potential remineralization of demineralized enamel after application of fluoride varnish. Am J Dent. 2004;17:462–4. [PubMed] [Google Scholar]
- 12.Mellberg JR, Chomicki WG, Mallon DE, Castrovince LA. Remineralization in vivo of artificial caries lesions by a monofluorophosphate dentifrice. Caries Res. 1985;19:126–35. doi: 10.1159/000260839. [DOI] [PubMed] [Google Scholar]
- 13.ten Cate JM, Buijs MJ, Miller CC, Exterkate RA. Elevated fluoride products enhance remineralization of advanced enamel lesions. J Dent Res. 2008;87:943–7. doi: 10.1177/154405910808701019. [DOI] [PubMed] [Google Scholar]
- 14.Trairatvorakul C, Kladkaew S, Songsiripradabboon S. Active management of incipient caries and choice of materials. J Dent Res. 2008;87:228–32. doi: 10.1177/154405910808700301. [DOI] [PubMed] [Google Scholar]
- 15.Garcia-Godoy F, Hicks MJ. Maintaining the integrity of the enamel surface: the role of dental biofilm, saliva and preventive agents in enamel demineralization and remineralization. J Am Dent Assoc. 2008;139(Supp):25S–34S. doi: 10.14219/jada.archive.2008.0352. [DOI] [PubMed] [Google Scholar]
- 16.Linton JL. Quantitative measurements of remineralization of incipient caries. Am J Orthod Dentofacial Orthop. 1996;110:590–7. doi: 10.1016/s0889-5406(96)80034-5. [DOI] [PubMed] [Google Scholar]
- 17.Ogaard B, Rølla G, Arends J, ten Cate JM. Orthodontic appliances and enamel demineralization. Part 2. Prevention and treatment of lesions. Am J Orthod Dentofacial Orthop. 1988;94:123–8. doi: 10.1016/0889-5406(88)90360-5. [DOI] [PubMed] [Google Scholar]
- 18.Willmot DR. White spot lesions after orthodontic treatment. Semin Orthod. 2008;14:209–19. [Google Scholar]
- 19.Ogaard B. The cariostatic mechanism of fluoride. Compend Contin Educ Dent. 1999;20(1 Supp):10–7. [PubMed] [Google Scholar]
- 20.Phantumvanit P, Feagin FF, Koulourides T. Strong and weak acid sampling for fluoride of enamel remineralized in sodium fluoride solutions. Caries Res. 1977;11:52–61. doi: 10.1159/000260249. [DOI] [PubMed] [Google Scholar]
- 21.Benson PE, Shah AA, Millett DT, Dyer F, Parkin N, Vine RS. Fluorides, orthodontics and demineralization: a systematic review. J Orthod. 2005;32:102–14. doi: 10.1179/146531205225021033. [DOI] [PubMed] [Google Scholar]
- 22.Reynolds EC. Calcium phosphate-based remineralization systems: scientific evidence? Aust Dent J. 2008;53:268–73. doi: 10.1111/j.1834-7819.2008.00061.x. [DOI] [PubMed] [Google Scholar]
- 23.Cai F, Shen P, Morgan MV, Reynolds EC. Remineralization of enamel subsurface lesions in situ by sugar-free lozenges containing casein phosphopeptide-amorphous calcium phosphate. Aust Dent J. 2003;48:240–3. doi: 10.1111/j.1834-7819.2003.tb00037.x. [DOI] [PubMed] [Google Scholar]
- 24.Iijima Y, Cai F, Shen P, Walker G, Reynolds C, Reynolds EC. Acid resistance of enamel subsurface lesions remineralized by a sugar-free chewing gum containing casein phosphopeptide-amorphous calcium phosphate. Caries Res. 2004;38:551–6. doi: 10.1159/000080585. [DOI] [PubMed] [Google Scholar]
- 25.Kumar VL, Itthagarun A, King NM. The effect of casein phosphopeptide-amorphous calcium phosphate on remineralization of artificial caries-like lesions: an in vitro study. Aust Dent J. 2008;53:34–40. doi: 10.1111/j.1834-7819.2007.00006.x. [DOI] [PubMed] [Google Scholar]
- 26.Manton DJ, Walker GD, Cai F, Cochrane NJ, Shen P, Reynolds EC. Remineralization of enamel subsurface lesions in situ by the use of three commercially available sugar-free gums. Int J Paediatr Dent. 2008;18:284–90. doi: 10.1111/j.1365-263X.2008.00920.x. [DOI] [PubMed] [Google Scholar]
- 27.Reynolds EC, Cai F, Shen P, Walker GD. Retention in plaque and remineralization of enamel lesions by various forms of calcium in a mouthrinse or sugar-free chewing gum. J Dent Res. 2003;82:206–11. doi: 10.1177/154405910308200311. [DOI] [PubMed] [Google Scholar]
- 28.Schulz KF, Altman DG, Moher D for the CONSORT group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63:834–40. doi: 10.1016/j.jclinepi.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 29.Shen P, Cai F, Nowicki A, Vincent J, Reynolds EC. Remineralization of enamel subsurface lesions by sugar-free chewing gum containing casein phosphopeptide-amorphous calcium phosphate. J Dent Res. 2001;80:2066–70. doi: 10.1177/00220345010800120801. [DOI] [PubMed] [Google Scholar]
- 30.Walker G, Cai F, Shen P, Reynolds C, Ward B, Fone C, et al. Increased remineralization of tooth enamel by milk containing added casein phosphopeptide-amorphous calcium phosphate. J Dairy Res. 2006;73:74–8. doi: 10.1017/S0022029905001482. [DOI] [PubMed] [Google Scholar]
- 31.Walker GD, Cai F, Shen P, Adams GG, Reynolds C, Reynolds EC. Casein phosphopeptide-amorphous calcium phosphate incorporated into sugar confections inhibits the progression of enamel subsurface lesions in situ. Caries Res. 2010;44:33–40. doi: 10.1159/000275572. [DOI] [PubMed] [Google Scholar]
- 32.Willershausen B, Schulz-Dobrick B, Gleissner C. In vitro evaluation of enamel remineralisation by a casein phosphopeptide-amorphous calcium phosphate paste. Oral Health Prev Dent. 2009;7:13–21. [PubMed] [Google Scholar]
- 33.Cochrane NJ, Saranathan S, Cai F, Cross KJ, Reynolds EC. Enamel subsurface lesion remineralisation with casein phosphopeptide stabilised solutions of calcium, phosphate and fluoride. Caries Res. 2008;42:88–97. doi: 10.1159/000113161. [DOI] [PubMed] [Google Scholar]
- 34.Elsayad I, Sakr A, Badr Y. Combining casein phosphopeptide-amorphous calcium phosphate with fluoride: synergistic remineralization potential of artificially demineralized enamel or not? J Biomed Opt. 2009;14:044039. doi: 10.1117/1.3210780. [DOI] [PubMed] [Google Scholar]
- 35.Reynolds EC, Cai F, Cochrane NJ, Shen P, Walker GD, Morgan MV, et al. Fluoride and casein phosphopeptide-amorphous calcium phosphate. J Dent Res. 2008;87:344–8. doi: 10.1177/154405910808700420. [DOI] [PubMed] [Google Scholar]
- 36.Srinivasan N, Kavitha M, Loganathan SC. Comparison of the remineralization potential of CPP-ACP and CPP-ACP with 900 ppm fluoride on eroded human enamel: an in situ study. Arch Oral Biol. 2010;55:541–4. doi: 10.1016/j.archoralbio.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 37.Wu G, Liu X, Hou Y. Analysis of the effect of CPP-ACP tooth mousse on enamel remineralization by circularly polarized images. Angle Orthod. 2010;80:933–8. doi: 10.2319/110509-624.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Beerens MW, van der Veen MH, van Beek H, ten Cate JM. Effects of casein phosphopeptide amorphous calcium fluoride phosphate paste on white spot lesions and dental plaque after orthodontic treatment: a 3-month follow-up. Eur J Oral Sci. 2010;118:610–7. doi: 10.1111/j.1600-0722.2010.00780.x. [DOI] [PubMed] [Google Scholar]
- 39.Bröchner A, Christensen C, Kristensen B, Tranæus S, Karlsson L, Sonnesen L, et al. Treatment of post-orthodontic white spot lesions with casein phosphopeptide-stabilised amorphous calcium phosphate. Clin Oral Investig. 2011;15:369–73. doi: 10.1007/s00784-010-0401-2. [DOI] [PubMed] [Google Scholar]
- 40.Du M, Cheng N, Tai B, Jiang H, Li J, Bian Z. Randomized controlled trial on fluoride varnish application for treatment of white spot lesion after fixed orthodontic treatment. Clin Oral Investig. 2011 Feb 18; doi: 10.1007/s00784-011-0520-4. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Baeshen HA, Lingström P, Birkhed D. Effect of fluoridated chewing sticks (Miswaks) on white spot lesions in postorthodontic patients. Am J Orthod Dentofacial Orthop. 2011;140:291–7. doi: 10.1016/j.ajodo.2010.04.034. [DOI] [PubMed] [Google Scholar]
- 42.Andersson A, Sköld-Larsson K, Hallgren A, Petersson LG, Twetman S. Effect of a dental cream containing amorphous cream phosphate complexes on white spot lesion regression assessed by laser fluorescence. Oral Health Prev Dent. 2007;5:229–33. [PubMed] [Google Scholar]
- 43.Bailey DL, Adams GG, Tsao CE, Hyslop A, Escobar K, Manton DJ, et al. Regression of post-orthodontic lesions by a remineralizing cream. J Dent Res. 2009;88:1148–53. doi: 10.1177/0022034509347168. [DOI] [PubMed] [Google Scholar]
- 44.Robertson MA, Kau CH, English JD, Lee RP, Powers J, Nguyen JT. MI Paste Plus to prevent demineralization in orthodontic patients: a prospective randomized controlled trial. Am J Orthod Dentofacial Orthop. 2011;140:660–8. doi: 10.1016/j.ajodo.2010.10.025. [DOI] [PubMed] [Google Scholar]
- 45.ClinicalTrials.gov. Bethesda, Md: National Library of Medicine; 2000. [Accessed on May 29, 2012]. Available at: http://clinicaltrials.gov/ct2/results?term=white+spot+lesion. [Google Scholar]
- 46.Benson PE, Pender N, Higham SM. Quantifying enamel demineralization from teeth with orthodontic brackets—a comparison of two methods. Part 1: repeatability and agreement. Eur J Orthod. 2003;25:149–58. doi: 10.1093/ejo/25.2.149. [DOI] [PubMed] [Google Scholar]
- 47.Benson PE, Pender N, Higham SM. Quantifying enamel demineralization from teeth with orthodontic brackets–a comparison of two methods. Part 2: validity. Eur J Orthod. 2003;25:159–65. doi: 10.1093/ejo/25.2.159. [DOI] [PubMed] [Google Scholar]
- 48.Chapman JA, Roberts WE, Eckert GJ, Kula KS, González-Cabezas C. Risk factors for incidence and severity of white spot lesions during treatment with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2010;138:188–94. doi: 10.1016/j.ajodo.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 49.Benson P. Evaluation of white spot lesions on teeth with orthodontic brackets. Semin Orthod. 2008;14:200–8. [Google Scholar]
- 50.Benson PE, Shah AA, Willmot DR. Measurement of white lesions surrounding orthodontic brackets: captured slides vs digital camera images. Angle Orthod. 2005;75:226–30. doi: 10.1043/0003-3219(2005)075<0222:MOWLSO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 51.Kanthathas K, Willmot DR, Benson PE. Differentiation of developmental and post-orthodontic white lesions using image analysis. Eur J Orthod. 2005;27:167–72. doi: 10.1093/ejo/cjh084. [DOI] [PubMed] [Google Scholar]
- 52.Livas C, Kuijpers-Jagtman AM, Bronkhorst E, Derks A, Katsaros C. Quantification of white spot lesions around orthodontic brackets with image analysis. Angle Orthod. 2008;78:585–90. doi: 10.2319/0003-3219(2008)078[0585:QOWSLA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 53.Benson PE, Pender N, Higham SM. Enamel demineralisation assessed by computerised image analysis of clinical photographs. J Dent. 2000;28:319–26. doi: 10.1016/s0300-5712(00)00002-6. [DOI] [PubMed] [Google Scholar]
- 54.Benson PE, Shah A, Willmot DR. Polarized versus nonpolarized digital images for the measurement of demineralization surrounding orthodontic brackets. Angle Orthod. 2008;78:288–93. doi: 10.2319/121306-511.1. [DOI] [PubMed] [Google Scholar]
- 55.Geiger AM, Gorelick L, Gwinnett AJ, Benson BJ. Reducing white spot lesions in orthodontic populations with fluoride rinsing. Am J Orthod Dentofacial Orthop. 1992;101:403–7. doi: 10.1016/0889-5406(92)70112-N. [DOI] [PubMed] [Google Scholar]
- 56.Kitasako Y, Cochrane NJ, Khairul M, Shida K, Adams GG, Burrow MF, et al. The clinical application of surface pH measurements to longitudinally assess white spot enamel lesions. J Dent. 2010;38:584–90. doi: 10.1016/j.jdent.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 57.Mizrahi E. Surface distribution of enamel opacities following orthodontic treatment. Am J Orthod. 1983;84:323–31. doi: 10.1016/s0002-9416(83)90348-2. [DOI] [PubMed] [Google Scholar]