Abstract
The use of ex vivo perfused models can mimic the physiological conditions of the liver for short periods, but to maintain normal homeostasis for an extended perfusion period is challenging. We have added the kidney to our previous ex vivo perfused liver experiment model to reproduce a more accurate physiological state for prolonged experiments without using live animals. Five intact livers and kidneys were retrieved post-mortem from sacrificed pigs on different days and perfused for a minimum of 6 hr. Hourly arterial blood gases were obtained to analyze pH, lactate, glucose and renal parameters. The primary endpoint was to investigate the effect of adding one kidney to the model on the acid base balance, glucose, and electrolyte levels. The result of this liver-kidney experiment was compared to the results of five previous liver only perfusion models. In summary, with the addition of one kidney to the ex vivo liver circuit, hyperglycemia and metabolic acidosis were improved. In addition this model reproduces the physiological and metabolic responses of the liver sufficiently accurately to obviate the need for the use of live animals. The ex vivo liver-kidney perfusion model can be used as an alternative method in organ specific studies. It provides a disconnection from numerous systemic influences and allows specific and accurate adjustments of arterial and venous pressures and flow.
Keywords: Medicine, Issue 82, Ex vivo, porcine, perfusion model, acid base balance, glucose, liver function, kidney function, cytokine response
Introduction
Studying a large animal organ physiology in an artificial environment is challenging. Furthermore, maintaining normal physiological and biochemical parameters for a prolonged period requires a closely monitored perfusion method and model. We have previously described our ex vivo autologous perfused porcine liver model for the study of hepatic physiology and significant progress has been achieved, since we began our liver reperfusion ex vivo model in 2005, in areas such as harvesting technique, understanding hepatic artery anatomical variations1, inflammatory response2,3, histological changes following liver electrolytic ablation (EA)4, and changes in acid base balance during EA5. Unfortunately hyperglycemia and metabolic acidosis require external supplements of insulin and bicarbonate to maintain an accurate physiological environment. Stable blood sugar levels and acid base balance are crucial when studying islet auto-transplantation, especially in the early implantation phase. We have developed a new model incorporating the kidney to clear excess metabolites and improve the environment for the islet transplantation6,7.
Extracorporeal perfusion experiments lasting longer than 24 hr can also be performed, but these require a larger team to perform the experiments8.
Animals used in this study received human care and study protocols were in accordance with the United Kingdom laws. They were euthanized with final exsanguinations during the blood-harvesting procedure according to United Kingdom regulations. Porcine liver and a left kidney were retrieved from animals in the food chain and that would otherwise be discarded. In this way important ethical implications can be overcome and the economic burden is lower than more common in vivo studies. The short duration of liver and kidney perfusion time in this model, lasting from 6-24 hr, has been a major limitation of our studies; this can be improved by minimizing the exposure of the organs to the ischemic injury (cold and warm ischemia).
Protocol
1. Preparation of the Procedure Equipment, Solutions, and Experiment Setup
- Equipment: The following equipment is required:
- Dissecting instruments: scissors, scalpels, artery forceps, 6x artery clips.
- 4x 12-14F catheters (for portal vein, hepatic artery, bile duct and renal artery), 1x 12F catheter (ureter), suture material (20x Vicryl stitches and Vicryl ties), stitch scissors, 3x infusion sets, ice in large insulated transport container, gloves, a large sterile container for the blood collection. At least three researchers are required to perform the organ retrieval.
Solutions and/ or drugsTable 1 and the table of specific reagents and materials summarize all the required solutions and drugs required for the experiment.
- Extracorporeal circuit preparation Setup the circuit before the organ is harvested. The circuit is similar to those used for cardiopulmonary extracorporeal bypass surgery. It consists of nontraumatic centrifugal pump that provides the hepatic/renal arterial blood flow and pressure readings, an oxygenator, a heat exchanger unit and a venous reservoir to stimulate the venous flow and pressures. After passage through the liver and kidney, the venous blood is collected from both the Inferior Vena Cava (IVC) and renal vein into a container simulating the systemic venous reservoir and returned to the centrifugal pump (Figure 1).
- Remove the circuit from the packaging ensuring its sterility. The circuit consists of two reservoirs; one supplying the pseudo portal circulation and one supplying the pseudo systemic circulation as per Figure 1.
- Connect the drainage lines from the IVC and renal vein to the systemic reservoir.
- Connect the systemic reservoir to the pump and then the oxygenator.
- There are 3 lines exiting the oxygenator. Connect one to each of the following: the hepatic artery, renal artery, and the reservoir supplying the hepatic portal vein. Connect this reservoir to the hepatic portal vein.
2. Harvesting the Porcine Kidney and Liver and Washing the Organs with Preservation Solution
Animals used in this study received human care and study protocols were in accordance with the United Kingdom laws. They were euthanized with final exsanguinations during the blood-harvesting procedure according to United Kingdom regulations.
Collect the autologous blood into a preheparinized nonpyogenic container with 25,000 units of Heparin.
Immediately following the laparotomy and sternotomy incision, shift all bowel loops to the right side, open the left retroperitoneal space and free up the left kidney from its attachments
Identify the renal artery and vein then resect them at their origin from the aorta and IVC.
Identify the ureter and cut approximately 10-15 cm distal to origin. One team member should take the kidney to a backbench table and place it in a kidney dish prefilled with ice and preservation solution (50:50).
Cannulate the renal artery as soon as possible and start an infusion of 500 ml (4 °C) preservation solution. Take all precautions to avoid any kink in the ureter as this will lead to hydronephrosis. On completion of the preservation infusion solution, place the kidney in a bag filled with preservation solution and store on ice, in an insulated container for transport to the laboratory.
Identify both the gastrocolic and treitz ligament and divide them; the Superior Mesenteric Vein (SMV) is found close to treitz ligament.
Cannulate the SMV to reach the portal vein and fix with a 0 Vicryl tie. Ligate the splenic vein (SV), and infuse cold 0.9% Sodium Chloride solution through the portal vein to remove any residual blood clots.
Identify the third part of the duodenum, ligate and then divided it. Mobilize the stomach, identify and resect the infra-hepatic IVC at any level. Identify the suprahepatic IVC and divide it along with the aorta and esophagus. Detach the aorta from the vertebral column attachments up to the level of the renal vessels and divide it at this level. Dissect any nonvascular attachments allowing the liver, stomach, second part of duodenum, pancreas, and spleen to be removed en-bloc, and then move the specimen on to a tray filled with ice on a separate bench table.
Start an infusion of approximately 1.5 L of the cold preservation solution (4 °C) through the portal vein.
Identify and cannulate the hepatic artery. Secure the cannula with a Vicryl tie and commence an infusion of 1 L of cold (4 °C) preservation solution. All of the above steps should be completed as fast as possible to minimize the warm ischemic injury time to the organs.
Mobilize the spleen and divide the gastrosplenic ligament, ligate the right gastric artery and then discard the spleen and stomach.
Finally, carefully dissect the pancreas from the splenic artery and free the pancreatic branches of the hepatic artery and ligate them, then identify the common bile duct and cut it long.
Thoroughly flush the retrieved liver to remove all blood clots, transfer the liver into a bag containing cold preservation solution and then place it inside an ice box for transport to the laboratory.
3. Priming the Circuit
Add approximately 1.5-2.5 L of the heparinized autologous porcine blood to the systemic venous reservoir of the circuit during the backbench preparation. This blood is the perfusate for the ex vivo liver and kidney experiment. Start the centrifugal pump and allow the perfusate to run through the intra-luminal and extra-luminal compartments and fill in all circuit lines as well as the hollow fiber filter
Add the following to the above perfusate: 40 ml of 8.4% sodium bicarbonate, 20 ml of epoprostenol sodium (500 μg in 50 ml of diluent, diluted with 200 ml of 0.9% sodium chloride), 750 mg of cefuroxime sodium in 10 ml water, 10 mmol in 10 ml calcium chloride 14.7%, and 50 units of insulin actrapid.
Prime the centrifugal pump with perfusate under the effect of gravity. Manually tap the circuit to remove any air bubbles toward the venous reservoir.
Start the centrifugal pump at a pump speed of 1,200 rpm to prime the remaining part of the circuit with perfusate.
Supply the oxygen (mixture of 95% oxygen and 5% carbon dioxide) to the oxygenator at a rate of 2 L/min and connect the oxygenator to the water bath/ heat exchanger preset at temperature of 38 °C (the physiologic temperature of pig).
Zero the pressure measuring device on the centrifugal pump to air (to zero the flow, both the inlet and outlet into the flow transducer should be fully clamped).
Once the perfusion has started maintain a continuous infusion of epoprostenol sodium 20 ml/hr and sodium taurocholate at 10 ml/hr (10 units/ml).
Administer boluses of 40 ml 8.4% sodium bicarbonate and 50 units of insulin actrapid to maintain physiological parameters of glucose and acid base balance.
If the metabolic acidosis and hyperglycemia are not corrected with boluses after the first hour, administer sodium bicarbonate 8.4% as an infusion at a rate of 40 ml/hr and titrate it according to the ABG and 100 units/hr Insulin. These continuous infusions need to be started to mimic the normal physiologic conditions and to maintain the pH within the physiologic range after reperfusion, ameliorating the acidotic changes derived from the ischemic reperfusion injury.
4. Backbench Preparation of Liver and Kidney for the Perfusion
Identify both the ureter and the common bile duct, cannulate and secure them.
Infuse 1 L of 0.9% sodium chloride solution through the portal vein, 500 ml through the hepatic artery and 500 ml through the renal artery to remove any blood clots from the organs and the cannulas and to flush out the preservation solution.
Identify any leaks from the vascular branches (as these will bleed during the perfusion) and ligate them with 2/0 Vicryl tie or stitches.
5. Ex vivo Liver-kidney Perfusion
Once all the lines are primed and the perfusate is optimized, collect a baseline blood sample for full blood count, biochemical and blood gas analysis before connecting the first organ. Take a tissue biopsy if performing histological examination.
Transfer the retrieved kidney into the allocated nonpyogenic perfusion chamber; connect the renal artery catheter to the respective line of the extracorporeal circuit and the catheterized ureter into an hourly urometer for urine output monitoring.
Adjust the perfusion pressure of the kidney and maintain the renal arterial pressure between 80-90 mmHg.
Transfer the liver into the allocated perfusion chamber, and immediately connect the hepatic artery and portal vein to their respective lines of the extracorporeal circuit. Allow the cannulated bile duct to drain freely into an allocated bile bag for monitoring.
Adjust the perfusion pressure and maintain the hepatic artery pressure between 80-100 mmHg and the portal vein pressure at <10 mmHg. The resistance in the portal venous system is low compared to the arterial channels, therefore, apply a clamp on the inlet tubing of the portal reservoir to control the inflow into the portal reservoir and maintain physiological pressures in the hepatic artery and portal vein. Tightening the clamp will decrease the inflow into the portal reservoir and increase the flow and pressure into the arterial lines, and vice versa.
To maintain the perfusion within physiological values of the arterial and venous flows and pressure, alter both the pump speed and change the inflow resistance of the reservoir aiming for a hepatic and renal artery flow of between 0.2-0.3 L/min and the portal vein flow above 1 L/min.
Collect blood samples hourly for hematological, biochemical and blood gas analysis and correct any electrolyte, glycemic and metabolic changes using the relevant solution (Table 1). Collect the last blood sample after 6 hr of perfusion and discard the organs according to your local policies.
Representative Results
Liver Function
The liver function tests remained stable for the first 6 hr. However, there were significant changes present only from the 19th hour of the 24 hr experiment (P<0.001). Factor V and X were progressively diminished during the whole experiment and significant changes were evident from the 5th hour of perfusion for factor V and from the 3rd hour for the factor X onward, (P<0.05; Figure 2)20.
Renal Function
The overall levels of urea and creatinine concentrations were significantly lower in the liver kidney model and no significant differences were observed over the hours of perfusion (P<0.001). However, in the liver only model these levels were significantly increased from the first hour onward (Figure 3)9.
Glucose
The glucose concentration normalized when the ex vivo porcine liver model was connected with one kidney when compared to liver circuit alone (P<0.001). There was no major difference between pre and immediately post perfusion changes in blood sugar levels9. In this ex vivo porcine liver-kidney model, the amount of insulin required was much lower compared to the liver ex vivo model alone, where insulin infusion was required continuously to control high glucose concentration (Figure 4).
Acid base Balance
Metabolic acidosis was well controlled with the ex vivo porcine liver-kidney model and sodium bicarbonate was given as required to titrate the acidosis (in boluses). Sodium bicarbonate was not required as a continuous infusion, where it was in the liver ex vivo model. Blood gas analysis showed a significant lower levels of pH in the liver kidney circuits than in the liver circuit alone (P< 0.001). The bicarbonate values of the liver alone model was significantly higher compared to the liver kidney model (P<0.01). A significant increase of the bicarbonate levels was noted in liver alone 3 hr post perfusion onward when compared to the bicarbonate levels at the beginning of the perfusion (p<0.05). We demonstrated a similar result for the base excess result (P<0.05) (Figure 4)9. These results demonstrate that the difference in the acid base balance was obviously corrected by the addition of a homeostatic organ (kidney) in the liver kidney circuit.
Cytokine Response
We used this model to study the differences between IL6 and IL8. Five liver-kidney perfusion experiments compared to seven livers alone model were performed. IL6 and IL8 values were increased considerably after the first and second hour respectively compared with the baseline levels and remained high afterwards (P<0.001). There were no significant differences between liver alone and liver kidney models (Figure 5 and Table 2)10.
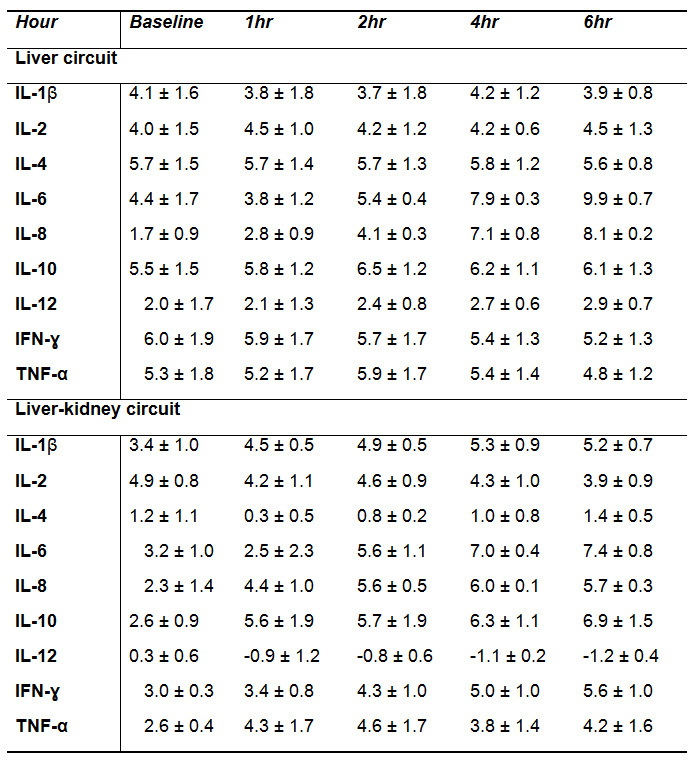 Table 1.
Experiment bolus and infusion medications.
Table 1.
Experiment bolus and infusion medications.
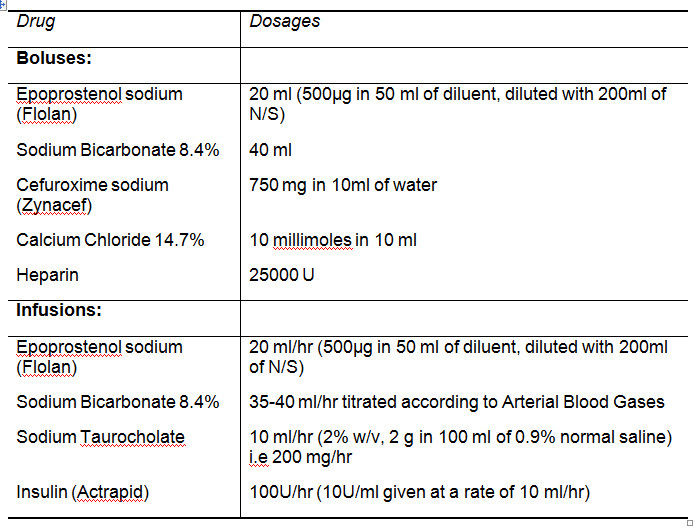 Table 2. Descriptive data of Interleukins 'IL', Interferon 'INF' and Tumor Necrosis Factor alpha 'TNF' according to the groups. This figure is reprinted with permission from the Journal of Artificial Organs6.
Table 2. Descriptive data of Interleukins 'IL', Interferon 'INF' and Tumor Necrosis Factor alpha 'TNF' according to the groups. This figure is reprinted with permission from the Journal of Artificial Organs6.
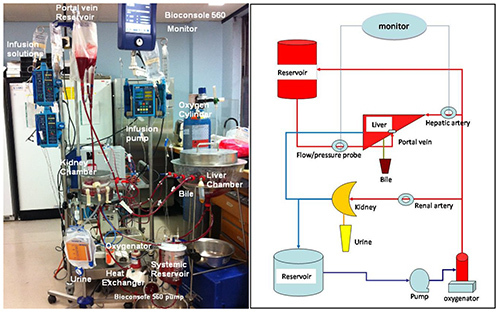 Figure 1. Photograph of the circuit for the ex vivo porcine liver-kidney perfusion model (Left) and schematic liver kidney circuit (Right). This figure is reprinted with permission from the Journal of Artificial Organs10.Click here to view larger image.
Figure 1. Photograph of the circuit for the ex vivo porcine liver-kidney perfusion model (Left) and schematic liver kidney circuit (Right). This figure is reprinted with permission from the Journal of Artificial Organs10.Click here to view larger image.
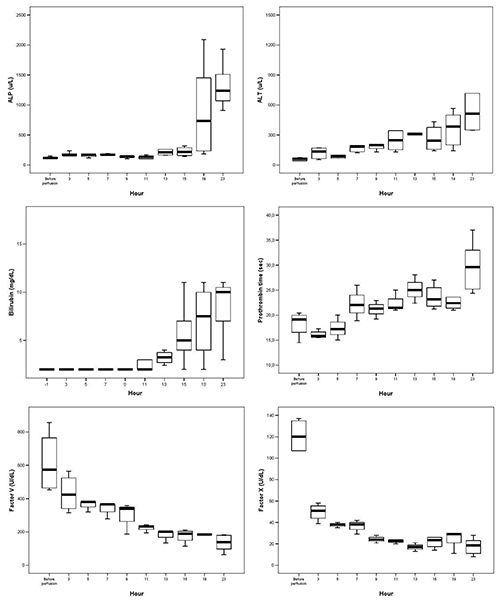 Figure 2. Box plot graphs showing the biochemical Liver function outcome after 24 hr liver-kidney experiment, data representing the median values and 95% confidence intervals. This figure is reprinted with permission from the Artificial Organs Journal20.Click here to view larger image.
Figure 2. Box plot graphs showing the biochemical Liver function outcome after 24 hr liver-kidney experiment, data representing the median values and 95% confidence intervals. This figure is reprinted with permission from the Artificial Organs Journal20.Click here to view larger image.
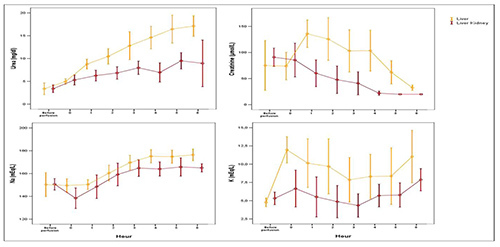 Figure 3. Error Bars graph demonstrating a comparison of the renal function outcome between liver alone and liver-kidney perfusion experiment for 6 hr. Circles represent the mean and Bars represent two standard deviations. This figure is reprinted with permission from the American Journal of Surgery9.Click here to view larger image.
Figure 3. Error Bars graph demonstrating a comparison of the renal function outcome between liver alone and liver-kidney perfusion experiment for 6 hr. Circles represent the mean and Bars represent two standard deviations. This figure is reprinted with permission from the American Journal of Surgery9.Click here to view larger image.
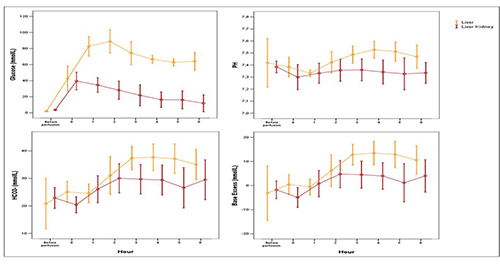 Figure 4. Error Bars Graph demonstrating Glucose level and metabolic parameters in liver alone and liver-kidney perfusion model for 6 hr. Circles represent the mean and Bars represent two standard deviations. This figure is reprinted with permission from the American Journal of Surgery9.Click here to view larger image.
Figure 4. Error Bars Graph demonstrating Glucose level and metabolic parameters in liver alone and liver-kidney perfusion model for 6 hr. Circles represent the mean and Bars represent two standard deviations. This figure is reprinted with permission from the American Journal of Surgery9.Click here to view larger image.
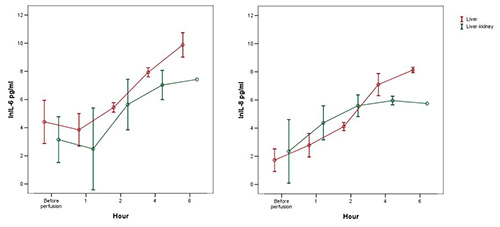 Figure 5. Error Bars illustrating the IL6 and IL8 outcome in liver alone and liver-kidney perfusion model for 6 hr. Circles represent the mean. This figure is reprinted with permission from the Journal of Artificial Organs10.Click here to view larger image.
Figure 5. Error Bars illustrating the IL6 and IL8 outcome in liver alone and liver-kidney perfusion model for 6 hr. Circles represent the mean. This figure is reprinted with permission from the Journal of Artificial Organs10.Click here to view larger image.
Discussion
In our group the experience and the results achieved with the ex vivo perfusion of the liver have been paralleled over the years by concomitant modifications in the retrieval technique adopted. In the last few years our group has achieved considerable experience using an ex vivo porcine model to study the hepatic physiology5,11, new liver ablation techniques2,5, and liver immunology3. Despite the technical challenges derived from an additional organ, corrections of hyperglycemia, electrolytes imbalances and acid base changes were significant7 and have lead the way to more complex experiments that require strict homeostatic conditions.
The addition of parenteral nutrition to an extracorporeal experiment has been used in a perfusion running for 72 hr12. We didn't provide any parenteral nutrition to the ex vivo perfused organs in our experiment due to the shorter perfusion period.
Comparable to our previous liver ex vivo perfusion models13,14, the outcome of our liver ex vivo perfusion model showed similar changes in the liver physiology, biochemical, immunologic, and pathological findings2,3,5,11, to those more expensive in vivo studies and this confirm our model is reliable and economical acceptable model for the study of porcine liver and related pathology.
The warm ischemia time is an important parameter for the organ survival following transplantation. When longer than 30 min it has been associated with delayed graft function15 and primary nonfunction16. Differently from in vivo retrievals, the ex vivo harvesting process necessarily implies longer warm ischemia times as the animal corresponds, at the time of the harvesting, to a "nonheart-beating" donor and not to a "brain-dead" donor with still a good circulation17. In our initial experiments the wash-out of the warm blood with cold perfusion solutions was achieved once the organs were out of the animal and the average warm ischemia time was approximately 19-20 min. However, to correct the biochemical imbalances produced by the lack of homeostatic organs (lungs, kidney) on the arterial blood gases, electrolytes and glucose levels we decided to add to our model a kidney. The start of a program of multiorgan ex vivo perfusion would necessary require shorter warm ischemia times because the harvesting time would be extended by the retrieval of the second organ. If this bias could not be correct, experiments with transplants particularly sensitive to warm ischemia times, in example pancreatic islet18, could not be possible or would produce biased results.
This technique mimics more closely the retrieval process of human transplantations19. The major organ vessels are approached immediately after the laparotomy when the organs are still in situ. The major difference with the our previous technique is that the organ perfusion with cold solutions, aimed to cool the organ and remove the blood to decrease the metabolic cellular processes, starts earlier when the organs are in the animal and not on the bench table. This difference corresponds to a net gain of approximately 10 min, improving the warm ischemia time of the liver and allowing a good time frame for a second organ to be collected effectively.
Future improvements to reduce the warm ischemia time are still possible. While in the current technique the renal vessels are isolated and the organ harvested after the liver-spleen-stomach-pancreas are removed en-bloc, these vessels could be isolated and cannulated immediately after the perfusion of the liver with the cold preservation solution has started. This would decrease the warm ischemia time of the kidney. Furthermore, similarly to what happen with the current techniques of human transplantation, the organs could be bathed immediately after the laparotomy by large amounts of ice that would decrease the organs' temperature while the vessels are isolated.
In summary, the addition of a single kidney to the previously implemented ex vivo liver perfusion model provides an improved physiological and metabolic environment of the reperfused liver and kidney. In particular, the improved hyperglycemia and acid base status, which make this model more reliable and financially acceptable.
Disclosures
Authors have nothing to disclose.
Acknowledgments
We would like to thank Sarah Hosgood from the Department of Transplantation, University Hospitals of Leicester, for technical support with the porcine kidney in this model.
References
- Gravante G, Ong SL, Metcalfe MS, Lloyd DM, Dennison AR. The porcine hepatic arterial supply, its variations and their influence on the extracorporeal perfusion of the liver. J. Surg. Res. 2011;1:56–61. doi: 10.1016/j.jss.2009.09.050. [DOI] [PubMed] [Google Scholar]
- Gravante G, et al. Cytokine response of electrolytic ablation in an ex vivo perfused liver model. ANZ J. Surg. 2010. pp. 7–8. [DOI] [PubMed]
- Gravante G, et al. Cytokine response to ischemia/reperfusion injury in an ex vivo perfused porcine liver model. Transplant Proc. 2009;4:1107–1112. doi: 10.1016/j.transproceed.2009.02.054. [DOI] [PubMed] [Google Scholar]
- Gravante G, et al. Patterns of histological changes following hepatic electrolytic ablation in an ex-vivo perfused model. Pathol. Oncol. Res. 2012;4:1085–1089. doi: 10.1007/s12253-012-9549-1. [DOI] [PubMed] [Google Scholar]
- Gravante G. Changes in acid-base balance during electrolytic ablation in an ex vivo perfused liver model. Am. J. Surg. 2012;5:666–670. doi: 10.1016/j.amjsurg.2009.12.019. [DOI] [PubMed] [Google Scholar]
- Chung WY, et al. Addition of a kidney to the normothermic ex vivo perfused porcine liver model does not increase cytokine response. J. Artif. Organs. 2012;3:290–294. doi: 10.1007/s10047-012-0641-9. [DOI] [PubMed] [Google Scholar]
- Chung WY, et al. The autologous normothermic ex vivo perfused porcine liver-kidney model: improving the circuit's biochemical and acid-base environment. Am. J. Surg. 2012;4:518–526. doi: 10.1016/j.amjsurg.2011.11.016. [DOI] [PubMed] [Google Scholar]
- Yanaga K, Makowka L, Lebeau G, Hwang RR, Shimada M, Kakizoe S, et al. A new liver perfusion and preservation system for transplantation research in large animals. J. Invest. Surg. 1990;3(1):65–75. doi: 10.3109/08941939009140337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung WY, et al. The autologous normothermic ex vivo perfused porcine liver-kidney model: improving the circuit's biochemical and acid-base environment. Am. J. Surg. 2012;4:518–526. doi: 10.1016/j.amjsurg.2011.11.016. [DOI] [PubMed] [Google Scholar]
- Chung WY, et al. Addition of a kidney to the normothermic ex vivo perfused porcine liver model does not increase cytokine response. J. Artif. Organs. 2012;3:290–294. doi: 10.1007/s10047-012-0641-9. [DOI] [PubMed] [Google Scholar]
- Gravante G, et al. Effects of hypoxia due to isovolemic hemodilution on an ex vivo normothermic perfused liver model. J. Surg. Res. 2010;1:73–80. doi: 10.1016/j.jss.2008.09.024. [DOI] [PubMed] [Google Scholar]
- Butler AJ, et al. Successful extracorporeal porcine liver perfusion for 72 hr. Transplantation. 2002;8:1212–1218. doi: 10.1097/00007890-200204270-00005. [DOI] [PubMed] [Google Scholar]
- St Peter SD, Imber CJ, Lopez I, Hughes D, Friend PJ. Extended preservation of non-heart-beating donor livers with normothermic machine perfusion. Br. J. Surg. 2002;5:609–616. doi: 10.1046/j.1365-2168.2002.02052.x. [DOI] [PubMed] [Google Scholar]
- Schon MR, et al. Liver transplantation after organ preservation with normothermic extracorporeal perfusion. Ann. Surg. 2001;1:114–123. doi: 10.1097/00000658-200101000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siedlecki A, Irish W, Brennan DC. Delayed graft function in the kidney transplant. Am. J. Transplant. 2011;11:2279–2296. doi: 10.1111/j.1600-6143.2011.03754.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monbaliu D, et al. Primary graft nonfunction and Kupffer cell activation after liver transplantation from non-heart-beating donors in pigs. Liver Transpl. 2007;2:239–247. doi: 10.1002/lt.21046. [DOI] [PubMed] [Google Scholar]
- Skaro AI, Jay CL, Ladner D, Abecassis MM. Trends in donation after cardiac death and donation after brain death--reading between the lines. Am. J. Transplant. 2010;11:2390–2391. doi: 10.1111/j.1600-6143.2010.03299.x. [DOI] [PubMed] [Google Scholar]
- Brandhorst D, Iken M, Bretzel RG, Brandhorst H. Pancreas storage in oxygenated perfluorodecalin does not restore post-transplant function of isolated pig islets pre-damaged by warm ischemia. Xenotransplantation. 2006;5:465–470. doi: 10.1111/j.1399-3089.2006.00340.x. [DOI] [PubMed] [Google Scholar]
- Lin QY, Chui KK, Rao AN. Rapid donor liver procurement with only aortic perfusion. World. J. Gastroenterol. 2001;6:884–886. doi: 10.3748/wjg.v7.i6.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung WY, et al. The development of a multiorgan ex vivo perfused model: results with the porcine liver-kidney circuit over 24 hours. Artif. Organs. 2013;5:457–466. doi: 10.1111/aor.12003. [DOI] [PubMed] [Google Scholar]


