Abstract
Introduction
Celiac disease (CD) may initially present as a neurological disorder or may be complicated by neurological changes. To date, neurophysiological studies aiming to an objective evaluation of the potential central nervous system involvement in CD are lacking.
Objective
To assess the profile of cortical excitability to Transcranial Magnetic Stimulation (TMS) in a group of de novo CD patients.
Materials and methods
Twenty CD patients underwent a screening for cognitive and neuropsychiatric symptoms by means of the Mini Mental State Examination and the Structured Clinical Interview for DSM-IV Axis I Disorders, respectively. Instrumental exams, including electroencephalography and brain computed tomography, were also performed. Cortico-spinal excitability was assessed by means of single and paired-pulse TMS using the first dorsal interosseus muscle of the dominant hand. TMS measures consisted of resting motor threshold, motor evoked potentials, cortical silent period (CSP), intracortical inhibition (ICI) and facilitation (ICF). None of the CD was on gluten-free diet. A group of 20 age-matched healthy controls was used for comparisons.
Results
CD showed a significantly shorter CSP (78.0 vs 125.0 ms, p<0.025), a reduced ICI (0.3 vs 0.2, p<0.045) and an enhanced ICF (1.1 vs 0.7, p<0.042) compared to controls. A dysthymic disorder was identified in five patients. The effect size between dysthymic and non-dysthymic CD patients indicated a low probability of interference with the CSP (Cohen's d -0.414), ICI (-0.278) and ICF (-0.292) measurements.
Conclusion
A pattern of cortical excitability characterized by “disinhibition” and “hyperfacilitation” was found in CD patients. Immune system dysregulation might play a central role in triggering changes of the motor cortex excitability.
Introduction
Celiac disease (CD) is a systemic autoimmune disorder triggered by gliadin ingestion in genetically susceptible individuals [1]–[3]. Genetic factors strongly contribute to CD, especially regarding HLA-DQ2 and DQ8, but also involving other non-HLA regions [1], [4], [5].
Although the main target in CD is the proximal small bowel, the clinical presentation is highly heterogeneous, ranging from asymptomatic to dramatically symptomatic forms and affecting several organs, such as skin, joints, bones, blood cells, endocrine glands, the reproductive system and the nervous system. In this context, approximately 50% of CD patients manifest extraintestinal dysfunctions and up to 22.5% have otherwise unexplained neurological symptoms [6]. Furthermore, neurological disorders may complicate the course or represent the onset of CD. Ataxia, peripheral neuropathy and seizures (with or without cerebral calcifications) are the most common neurological complications, with cerebellar ataxia being the most frequent, often associated with cerebellar atrophy at neuroimaging [7]. A possible association between CD and progressive cognitive impairment can be particularly observed, at neuropsychological tests evaluating verbal memory and executive functions [8], [9]. Different neuropsychiatric disorders, such as schizophrenia, depression, and anxiety, have also been reported to be associated with CD [10]. Therefore, CD should be considered in patients with unexplained neurological disorders and a neurological screening might disclose valuable information in these patients.
Nevertheless, although there is a relevant impact of CD and its complications on health and social life, to date techniques allowing an objective evaluation of the potential central nervous system involvement in CD are lacking.
In the last years, several investigators have used transcranial magnetic stimulation (TMS) to define the electrophysiological profile of several neuropsychiatric disorders [11], [12], physiological brain aging [13], different models of cognitive decline [14], [15] and some systemic diseases with a neurological involvement [16], [17]. TMS is a safe and non-invasive neurophysiological technique specifically able to evaluate the excitability and functioning of the primary motor cortex and the cortico-spinal tract [18]. TMS studies have provided findings that, although not disease specific, shed light on the cortical pathophysiology and the neurochemical basis underlying disease processes and represent a rationale for the plasticity-based interventions [18], [19]. More recently, TMS-derived parameters have allowed to explore the regulatory mechanisms of cortical excitability, supporting the concept of a cortical motor network whose output is also influenced by non-primary motor areas, including ventral and dorsal premotor cortex, supplementary motor area and cingulate cortex [20]. In particular, it is known that the cingulate cortex, together with the dorsolateral prefrontal cortex, is crucial for cognition and mood regulation [21].
Converging evidences suggest that gluten-mediated immune response in CD is associated with neuropsychiatric manifestations. Given that glutamic acid decarboxylase (GAD) antibodies may interfere with the GABAergic synaptic transmission, thus affecting inhibitory interneurons activity, in the present paper we first aimed to explore the potential involvement of inhibitory and facilitatory intracortical circuits to single- and paired-pulse TMS in de novo CD patients. We hypothesized that gluten intolerance might be associated with changes of specific TMS measures of excitation and inhibition.
Materials and methods
Ethics Statement
The study was approved by the ethics committee of the Azienda Ospedaliero-Universitaria “Policlinico-Vittorio Emanuele”, Catania (Italy). Written informed consent was obtained from all participants prior to participation in accordance with the Declaration of Helsinki. All assessments were performed in a controlled laboratory environment.
Subjects
Twenty de novo CD patients (4 males and 16 females; median age 33.0 years, interquartile range 24.0–45.0), according to the European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) guidelines for the diagnosis of CD [22], were consecutively recruited from the Regional Center for Celiac Disease of the University of Catania, Italy. The clinical-serological features and the main findings from the diagnostic work-up of CD patients are summarized in Table 1. Twenty age-matched healthy volunteers (8 males and 14 females; median age 29.5 years, interquartile range 26.0–45.5) were used as a control group. At the time of the examination, none of the patients was on gluten-free diet. Exclusion criteria were: major neurological disorder (i.e. Parkinson's disease, stroke, Alzheimer's disease, etc.); head trauma or epilepsy; acute, chronic or not compensated medical illness (i.e. myocardial infarction, kidney or liver failure, heart failure, etc.); Mini Mental State Examination score <24 [23], alcohol or drug abuse; age <18 years; use of drugs affecting cortical excitability (i.e. mood stabilizers, benzodiazepines, antipsychotics); any condition precluding TMS execution. On a total sample of 23 consecutive CD patients, 2 were excluded because of current intake of benzodiazepines and one refused the TMS protocol.
Table 1. Clinical-serological features and diagnostic work-up of CD patients.
| Patient | Symptoms at onset | Co-morbidities | Antibodies | Endoscopy | Histopathology |
| 1 | Dyspepsia, tiredness | - | tTG, EMA | Scalloped duodenal folds | 3b |
| 2 | Tiredness | - | tTG, EMA | Reduced duodenal folds | 3b |
| 3 | Abdominal pain | Thyroiditis | tTG, EMA | Scalloped duodenal folds | 3b |
| 4 | Diarrhea, abdominal pain | - | tTG, EMA | Reduced duodenal folds | 3c |
| 5 | Constipation | - | tTG | Mucosal fissures | 3b |
| 6 | Diarrhea | Asthma | tTG, EMA | Mosaic pattern | 3c |
| 7 | Poliabortivity, tiredness | - | tTG, EMA | Mucosal fissures | 3c |
| 8 | Abdominal pain | Thyroiditis | tTG, EMA | Reduced duodenal folds | 3c |
| 9 | Dyspepsia, tiredness | Thyroiditis | tTG, EMA | Mosaic pattern | 3c |
| 10 | None (screening, family history for CD) | - | tTG | Mosaic pattern | 3c |
| 11 | Diarrhea, abdominal pain | Asthma | tTG, EMA | Absent duodenal folds | 3c |
| 12 | Weight loss | Thyroiditis | tTG, EMA | Mosaic pattern | 3c |
| 13 | Abdominal pain | - | tTG | Mucosal fissures | 3b |
| 14 | Weight loss, diarrhea | Vitiligo | tTG, EMA | Scalloped duodenal folds | 3a |
| 15 | Infertility, tiredness | Thyroiditis | tTG, EMA | Reduced duodenal folds | 3c |
| 16 | Diarrhea | - | negative | Scalloped duodenal folds | 3a |
| 17 | Weight loss | - | tTG, EMA | Mosaic pattern | 3c |
| 18 | Weight loss, abdominal pain, | - | tTG, EMA | Mosaic pattern | 3c |
| 19 | Dyspepsia, abdominal pain, diarrhea | - | tTG, EMA | Mosaic pattern | 3c |
| 20 | Tiredness | Thyroiditis | tTG, EMA | Mosaic pattern | 3c |
CD = celiac disease; tTG = tissue transglutaminase antibodies; EMA = endomysial antibodies.
Histopathological classification is based on the Marsh–Oberhuber grading system [51]. 3a: mild villous flattening; 3b: marked villous flattening; 3c: total villous flattening.
Assessment
The clinical-demographic evaluation included: age, gender, education, handedness, social and living conditions, general and neurological examinations, and co-morbidities. Neuropsychological tests included a screening of overall cognitive functions (Mini Mental State Examination), evaluation of neuropsychiatric symptoms diagnosed by the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the 17-items Hamilton Depression Rating Scale [24], for the quantification of any depressive symptom. Cognitive assessment was performed by a physician blind to the aim of the study. Instrumental exams included standard electroencephalogram (EEG), brain computed tomography (CT) scan and both single- and paired-pulse TMS.
EEG was recorded by means of a Micromed Brain Quick (System Plus), with a standard montage according to the 10-20 International System and with a pre-cabled EEG head cap. Brain CT was acquired with a helical 64-slices General Electric Scanning, with 2.5 mm slice thickness. Only the clinical, neuropsychological and TMS studies were carried out in controls.
Transcranial magnetic stimulation
TMS was performed using a High-power Magstim 200 magnetic stimulator (Magstim Co., Whitland, Dyfed, UK). A 70 mm figure-of-eight coil was held over the motor cortex at the optimum scalp position to elicit Motor Evoked Potentials (MEPs) in the contralateral First Dorsal Interosseous (FDI) muscle of the dominant hand, according to the Edinburgh Handedness Inventory [25]. Resting motor threshold (rMT) was defined as the lowest stimulus intensity able to elicit MEPs at rest of an amplitude >50 µV in at least 5 of 10 trials, according to the IFCN recommendation [26]. Central motor conduction time was calculated by subtracting the conduction time in peripheral nerves, estimated by F wave techniques, from MEP latency obtained during moderate active muscle contraction, with a stimulus intensity set at 130% of the rMT. M and F waves are elicited by giving supramaximal electrical stimulation to the ulnar nerve at wrist. The size of the MEPs was expressed as a percentage of supramaximal M wave amplitude (A ratio). The cortical silent period (CSP) was determined with an approximately 50% of maximum tonic voluntary contraction of the FDI muscles, induced by single TMS pulses delivered at 130% of rMT. The mean CSP duration of 10 rectified trials was calculated. Intracortical inhibition (ICI) and Intracortical facilitation (ICF) were studied using the conditioning-test paradigm applying two magnetic stimuli in rapid succession [27]. The conditioning stimulus was set at 80% of the subjects rMT whereas the test stimulus at 130% of the rMT. The interstimulus intervals (ISIs) tested were 2, 3, 10 and 15 ms. Ten trials for each ISI were recorded in a random way with an 8-s interval between each trial. The responses were expressed as the ratio between the MEP amplitude produced by paired stimulation and that produced by TS alone. Paired-pulse TMS curves of intracortical excitability were obtained with a 70-mm figure-of-eight coil deriving pulses from a couple of Magstim 200 Stimulators, connected each other through a BiStim module (The Magstim Company, Whitland, Dyfed). The BiStim was connected to a CED Micro 1401 interface (Cambridge Electronic Design, Cambridge, UK) allowing stimulus generation and data capture. Electromyographic (EMG) activity was recorded with silver/silver-chloride disposable self-adhesive and self-conductive surface electrodes. The active electrode was placed over the muscular belly of the target muscle (FDI), the reference distally at the metacarpo-phalangeal joint of the index finger and the ground on the dorsal face of the wrist. For the motor nerve conduction study (M and F waves from the FDI muscle), a bipolar nerve stimulation electrode with 6-mm diameter felt pads and an interelectrode separation of 25 mm was used and applied to the ulnar nerve at wrist, bilaterally. All measurements were conducted while subjects were seated in a comfortable chair with continuous EMG monitoring to ensure either a constant level of EMG activity during tonic contraction or complete relaxation at rest. Data were collected and stored on a computer with an ad-hoc software, allowing data acquisition, processing and analysis [28]. To minimize the inter-subjects variability, all TMS procedures were performed in the same laboratory and situation, by the same operators and at the same time during the day.
Statistical analysis
The comparison of the frequency of observation of some features in the CD group and in the control group was carried out by means of the Chi-square test. Because of the relatively low number of subjects in both groups and the non normal distribution of data (as determined by the Shapiro-Wilk's test of normality), all the other comparisons were performed by means of the non-parametric Mann-Whitney test for unpaired datasets. Differences were considered significant when they were below the p<0.05 level. However, because of the relatively limited number of subjects available and to rule out possible type II errors, we also calculated effect sizes using the Cohen's d value [29]. Cohen's d is defined as the difference between two means divided by their pooled standard deviation. According to Cohen, 0.2 is indicative of a small effect, 0.5 of a medium and 0.8 of a large effect size.
Results
Demographic, clinical and neuropsychological characteristics of the participants are summarized in Table 2. The general examination of the CD group was unremarkable except for one overweight patient. The neurological examination of all patients was essentially normal. Nine patients had autoimmune co-morbidities, the most common being positive antithyroid peroxidase autoantibodies (six, altough euthyroid), followed by asthma (two) and vitiligo (one). Patients and controls were similar in terms of age, gender, handedness and educational level. The 17 item-HDRS scores were significantly worse in patients (7.0 vs 2.0, p<0.0058), whereas the SCID-I disclosed a dysthymic disorder in five CD patients; anxiety was also found in two of them. EEG and CT scan ruled out epileptic changes as well as intracranial calcifications or other clear neuroradiological abnormalities.
Table 2. Clinical features of the subjects included in this study.
| Celiac disease (n = 20) | Controls (n = 20) | Mann-Whitney | Effect size | ||||
| median | (25th-75th quartile) | median | (25th-75th quartile) | U | p< | Cohen's d | |
| Age, years | 33.0 | (24.0–45.0) | 29.5 | (26.0–45.5) | 180 | NS | −0.123 |
| Education, years | 13.0 | (9.0–13.0) | 14.0 | (13.5–14.0) | 133 | NS | −0.402 |
| MMSE | 30.0 | (29.0–30.0) | 30.0 | (28.8–30.0) | 182 | NS | 0.183 |
| 17 item-HDRS | 7.0 | (2.0–9.0) | 2.0 | (0.0–4.0) | 98 | 0.0058 | 1.451 |
| Chi2 | p< | ||||||
| Sex, males/females | 4/16 | 8/12 | 1.90 | NS | |||
| Handedness, right/left | 18/2 | 18/2 | 0.00 | NS | |||
| Neurological signs, yes/no | 3/17 | 0/20 | 3.24 | NS | |||
| Comorbidity, yes/no | 9/11 | 0/20 | 11.60 | 0.001 | |||
| SCID-I, yes/no | 5/15 | 0/20 | 5.71 | 0.017 | |||
MMSE = Mini Mental State Examination; HDRS = Hamilton Depression Rating Scale; SCID-I = Structured Clinical Interview for DSM-IV Axis I.
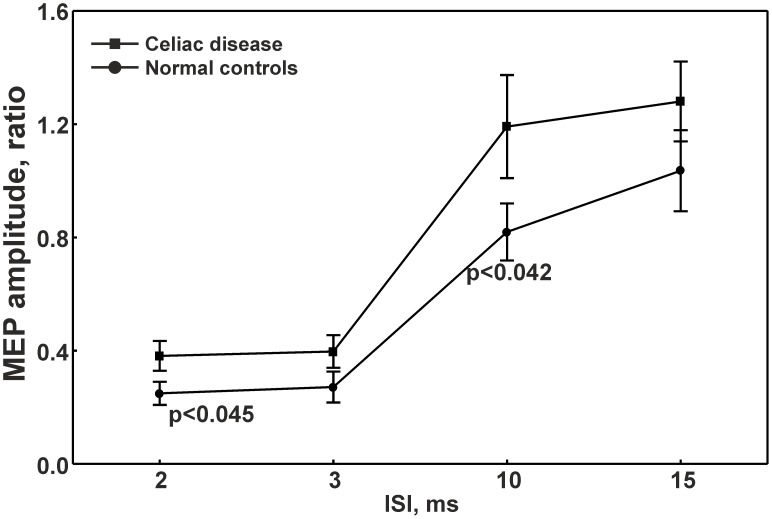
As shown in Table 3, CSP duration was significantly shorter in CD subjects with respect to controls (78.0 vs 125.0 ms, p<0.025), whereas no statistically significant differences were found for rMT. Fig. 1 shows curves of intracortical excitability at the different ISIs obtained in the two groups of participants. Conditioned MEPs amplitudes at ISI of 2 (0.3 vs 0.2, p<0.045) and 10 ms (1.1 vs 0.7, p<0.042) were significantly higher in CD patients than controls, indicating a reduced ICI and enhanced ICF in celiac individuals, respectively.
Table 3. Comparison of electrophysiological data in patients with celiac disease and controls.
| Celiac disease (n = 20) | Controls (n = 20) | Mann-Whitney | Effect size | ||||
| median | (25th-75th quartile) | median | (25th-75th quartile) | U | p< | Cohen's d | |
| rMT | 35.0 | (34.0–41.5) | 37.0 | (32.0–40.0) | 194.5 | NS | 0.070 |
| CSP, ms | 78.0 | (61.5–100.0) | 125.0 | (69.5–160.0) | 117 | 0.025 | −0.872 |
| MEP latency, ms | 18.6 | (18.2–19.7) | 19.3 | (18.5–20.2) | 151 | NS | −0.428 |
| CMCT | 5.9 | (4.5–6.3) | 5.8 | (5.6–6.6) | 168 | NS | −0.368 |
| CMCTF | 4.8 | (4.5–5.6) | 5.3 | (4.2–5.7) | 175 | NS | −0.148 |
| A ratio | 0.2 | (0.2–0.5) | 0.5 | (0.3–0.7) | 88.5 | 0.0026 | −0.653 |
| F amplitude, µV | 0.1 | (0.1–0.2) | 0.1 | (0.1–0.2) | 179.5 | NS | 0.627 |
rMT = resting motor threshold; CSP = cortical silent period; MEP = Motor Evoked Potentials; CMCT = central motor conduction time; CMCTF = central motor conduction time estimated by F wave; A ratio = amplitude ratio.
Figure 1. Intracortical excitability at different interstimuls intervals obtained from patients and controls.
ISI = interstimuls interval; MEP = Motor Evoked Potential.
Additionally, in order to evaluate the eventual influence of the five dysthymic CD patients on the TMS data, we have estimated the effect size between dysthymic and non-dysthymic CD patients, which was very low in all instances indicating a low probability of interference with the CSP (Cohen's d -0.414), ICI (-0.278) and ICF (-0.292) measurements.
Discussion
This is the first multi-disciplinary investigation examining the impact of CD on motor cortex excitability. The main finding is the observation of electrophysiological changes within the motor cortex of these patients. In particular, we observed a significant reduction of the intracortical inhibitory amount indicated by shortened CSP and reduced ICI, together with a significant enhancement of ICF, in patients with CD compared to controls. This pattern, basically characterized by a “disinhibition” and “hyperfacilitation”, was observed in the absence of substantial changes of rMT. On the other hand, changes of different TMS measures without modification of rMT has already been reported and is likely due to the different electrophysiological and neurochemical basis that these measures have and explore [30], [31]. Resting MT represents a global parameter of cortical excitability and reflects the neuronal membrane excitability, as well as the local density of the excitatory interneurons and the cortico-spinal neurons within the motor cortex [18]. CSP, defined as the interval of suppressed voluntary EMG activity following a single-pulse TMS stimulus, is an index of motor cortical inhibition, basically due to the activation of GABA-B cortical inhibitory interneurons [32], [33]. ICI is probably mediated by GABA-A receptors [34], whereas ICF may represent an activating phenomenon arising from intracortical glutamatergic neurons [18], [35], but also tempered by GABAergic inhibition and modulated by serotoninergic, adrenergic, cholinergic and dopaminergic neurotransmission [36].
The mechanisms underlying this cortical disinhibition in CD patients are rather complex to explain, also because of the lack of similar studies. The pathophysiology of CD and the most accepted hypothesis explaining its neurological involvement may help understanding our results. Vitamins and trace elements deficiency is unlikely to explain the subtle neurophysiological changes to TMS, because it usually occurs in the most affected CD patients, in whom a wide intestinal damage is already evident, resulting in severe malabsorption and related consequences [7], [37].
An autoimmune-mediated pathogenesis for CD is supported by increasingly convincing evidence. Molecular mimicry between gliadin and nervous system proteins could lead to a cross-reaction of anti-gliadin antibodies (Abs) with nervous system antigens. Abs can react with Purkinje cells and peripheral nerve epitopes [10], [38]. Furthermore, anti-gliadin Abs have a immunoreactivity to synapsin I, which is very similar to gliadin because of the high frequency of proline and glutamine regions. Synapsin I is a neuronal phosphoprotein of the central and peripheral nervous system involved in forming and maintaining the reserve pool of synaptic vesicles and in managing neurotransmitter release [39], [40]. In CD patients, anti-gliadin Abs might possibly interfere with the normal balance between excitatory and inhibitory neural circuits as a consequence of the interaction with synapsin I.
Another interesting hypothesis regards a possible involvement of GABA, which is the main inhibitory neurotransmitter synthesized in the central nervous system from glutamate by GAD. Since GABA and GAD are also synthesized by neurons of the enteric plexus [41], anti-GAD Abs may arise in CD patients and concentrate in the Purkinje cells and peripheral nerves [42], [43] and may interfere with GABAergic synaptic transmission, thus affecting inhibitory interneurons activity [10].
Within humoral autoimmunity to neuronal antigens, anti-transglutaminase 2- or transglutaminase 6-related immunoglobulin depositions have been identified not only in the gut but also in the cerebellum, pons, medulla and around brain blood vessels [38], [44]. Additional findings show diffuse T-lymphocytic infiltration within the perivascular cuffing with inflammatory cells that could possibly damage the blood-brain barrier and expose the cerebral tissues to Abs [7], driving altered ion levels. Taken together, this may lead to a vicious circle resulting in a imbalance between inhibitory and facilitatory neuronal excitability.
Finally, growing evidence indicates that immune system dysregulation might play a central role in triggering neurological impairment in CD, leading not only to the neurophysiological alterations but also to neurobehavioral changes. In this context, another finding of our study is the evidence of a degree of depressive and anxiety symptoms in CD patients, adding further support to the relationship between psychiatric disorders and CD [45], [46]. Major depression has been widely studied by TMS, which has confirmed the key role of the GABAergic dysfunction in the neurochemical pattern of depressed mood, as indexed by a reduction of both CSP and ICI [11], [47]-[50]. In this view, it can be argued that our TMS findings might be explained as a result of depressive mood in five of the CD patients. However, to our knowledge no study assessing cortical excitability to TMS in dysthimia is available. Besides, in this series of patients, TMS modifications do not seem to be significantly influenced by the depressive disorder. Therefore, it can be hypothesized that the observed TMS changes of inhibitory circuits might be related to the synaptic disruption due to the gluten-mediated immune response and that an imbalance between inhibitory and facilitatory intracortical circuits occurs even at a subclinical neurological stage of CD.
This study has some limitations. First, TMS-related measures of cortical excitability do not provide specific pathophysiological information although they are sensitive to the “global weight” of several neurotransmitters, as well as to subcortical and cortical motor inputs. Second, the observed findings obtained from a relatively small number of patients do not allow to draw conclusions on the eventual causal relationship between CD and a specific pattern of cortical excitability to TMS. Therefore, these results need to be confirmed by further independent investigations with larger group sizes and to be correlated to the clinical presentation and course of CD, even after an adequate course of gluten-free dietary regimen. In this context, a “normalization” of the TMS parameters after the gluten-free diet might add support to the hypothesis of a direct correlation between TMS profile and CD.
In conclusion, this study reveals that CD patients seem to exhibit a relatively distinct pattern of cortical excitability to TMS, suggesting that even asymptomatic patients might disclose a subclinical neurological involvement. The identification of potential neuromarkers might be useful in the diagnosis, follow-up and prognosis of these patients, such as in the monitoring of any change of clinical, neuropsychological and neurophysiological data over time or after a gluten-free dietary regimen. TMS, together with clinical-cognitive, immunological and imaging data, can be considered to be an additional tool able to capture subtle changes in the pathophysiological and neurochemical mechanisms underlying the exciting connections between gut and brain.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1. Di Sabatino A, Corazza GR (2009) Coeliac disease. Lancet 25 373(9673): 1480–93. [DOI] [PubMed] [Google Scholar]
- 2. Volta U, De Giorgio R (2010) Gluten sensitivity: an emerging issue behind neurological impairment? Lancet Neurol 9(3): 233–5. [DOI] [PubMed] [Google Scholar]
- 3. Volta U, De Giorgio R (2012) New understanding of gluten sensitivity. Nat Rev Gastroenterol Hepatol 28 9(5): 295–9. [DOI] [PubMed] [Google Scholar]
- 4. Sollid LM, Jabri B (2005) Is celiac disease an autoimmune disorder? Curr Opin Immunol 17(6): 595–600. [DOI] [PubMed] [Google Scholar]
- 5. Greco L, Romino R, Coto I, Di Cosmo N, Percopo S, et al. (2002) The first large population based twin study of coeliac disease. Gut 50(5): 624–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Briani C, Zara G, Alaedini A, Grassivaro F, Ruggero S, et al. (2008) Neurological complications of celiac disease and autoimmune mechanisms: a prospective study. J Neuroimmunol 195(1-2): 171–5. [DOI] [PubMed] [Google Scholar]
- 7. Hadjivassiliou M, Sanders DS, Grünewald RA, Woodroofe N, Boscolo S, et al. (2010) Gluten sensitivity: from gut to brain. Lancet Neurol 9(3): 318–30. [DOI] [PubMed] [Google Scholar]
- 8. Bürk K, Bösch S, Müller CA, Melms A, Zühlke C, et al. (2001) Sporadic cerebellar ataxia associated with gluten sensitivity. Brain 124(Pt 5): 1013–9. [DOI] [PubMed] [Google Scholar]
- 9. Hu WT, Murray JA, Greenaway MC, Parisi JE, Josephs KA (2006) Cognitive impairment and celiac disease. Arch Neurol 63(10): 1440–6. [DOI] [PubMed] [Google Scholar]
- 10. Jackson JR, Eaton WW, Cascella NG, Fasano A, Kelly DL (2012) Neurologic and psychiatric manifestations of celiac disease and gluten sensitivity. Psychiatr Q 83(1): 91–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Radhu N, De Jesus DR, Ravindran LN, Zanjani A, Fitzgerald PB, et al. (2013) A meta-analysis of cortical inhibition and excitability using transcranial magnetic stimulation in psychiatric disorders. Clin Neurophysiol 124(7): 1309–20. [DOI] [PubMed] [Google Scholar]
- 12. Bella R, Ferri R, Cantone M, Pennisi M, Lanza G, et al. (2011) Motor cortex excitability in vascular depression. Int J Psychophysiol 82(3): 248–53. [DOI] [PubMed] [Google Scholar]
- 13. Rossini PM, Rossi S, Babiloni C, Polich J (2007) Clinical neurophysiology of aging brain: from normal aging to neurodegeneration. Prog Neurobiol 83(6): 375–400. [DOI] [PubMed] [Google Scholar]
- 14. Pennisi G, Ferri R, Cantone M, Lanza G, Pennisi M, et al. (2011) A review of transcranial magnetic stimulation in vascular dementia. Dement Geriatr Cogn Disord 31(1): 71–80. [DOI] [PubMed] [Google Scholar]
- 15. Pennisi G, Ferri R, Lanza G, Cantone M, Pennisi M, et al. (2011) Transcranial magnetic stimulation in Alzheimer's disease: a neurophysiological marker of cortical hyperexcitability. J Neural Transm 118(4): 587–98. [DOI] [PubMed] [Google Scholar]
- 16. Andersen H, Nielsen S, Nielsen JF (2006) Motor cortical excitability remains unaffected of short-term hyperglycemia in Type 1 diabetic patients. J Diabetes Complications 20(1): 51–5. [DOI] [PubMed] [Google Scholar]
- 17. Oliviero A, Gaspari R, Tonali PA, Pennisi MA, Mercurio G, et al. (2002) Changes in excitability of motor cortex in severe hepatic failure. J Neurol Neurosurg Psychiatry 72(3): 414–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kobayashi M, Pascual-Leone A (2003) Transcranial magnetic stimulation in neurology. Lancet Neurol 2(3): 145–56. [DOI] [PubMed] [Google Scholar]
- 19. Rossini PM, Rossi S (2007) Transcranial magnetic stimulation: diagnostic, therapeutic, and research potential. Neurology 68(7): 484–8. [DOI] [PubMed] [Google Scholar]
- 20. Reis J, Swayne OB, Vandermeeren Y, Camus M, Dimyan MA, et al. (2008) Contribution of transcranial magnetic stimulation to the understanding of cortical mechanisms involved in motor control. J Physiol 586(2): 325–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Leech R, Sharp DJ (2014) The role of the posterior cingulate cortex in cognition and disease. Brain 137(Pt 1): 12–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Husby S (2012) European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr 54: 136–160. [DOI] [PubMed] [Google Scholar]
- 23. Folstein MF, Folstein SE, McHugh PR (1975) Mini-Mental State. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3): 189–98. [DOI] [PubMed] [Google Scholar]
- 24. Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry. 23: 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Oldfield RC (1971) The assessment and analysis of handedness: the Edinburgh Inventory. Neuropsychologia 9(1): 97–113. [DOI] [PubMed] [Google Scholar]
- 26. Rossini PM, Barker AT, Berardelli A, Caramia MD, Caruso G, et al. (1994) Non-invasive electrical and magnetic stimulation of the brain, spinal cord and roots: basic principles and procedures for routine clinical application. Report of an IFCN committee. Electroencephalogr Clin Neurophysiol 91(2): 79–92. [DOI] [PubMed] [Google Scholar]
- 27. Kujirai T, Caramia MD, Rothwell JC, Day BL, Thompson PD, et al. (1993) Corticocortical inhibition in human motor cortex. J Physiol 471: 501–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Giordano D, Kavasidis I, Spampinato C, Bella R, Pennisi G, et al. (2012) An integrated computer-controlled system for assisting researchers in cortical excitability studies by using transcranial magnetic stimulation. Comput Methods Progr Biomed 107(1): 4–15. [DOI] [PubMed] [Google Scholar]
- 29.Cohen J (1988) Statistical power analysis for the behavioural sciences (2nd ed.). Erlbaum. Hillsdale, NJ.
- 30. Bella R, Ferri R, Pennisi M, Cantone M, Lanza G, et al. (2011) Enhanced motor cortex facilitation in patients with vascular cognitive impairment no-dementia. Neurosci Lett 10 503(3): 171–5. [DOI] [PubMed] [Google Scholar]
- 31. Paulus W, Classen J, Cohen LG, Large CH, Di Lazzaro V, et al. (2008) State of the art: pharmacologic effects on cortical excitability measures tested by transcranial magnetic stimulation, Brain Stimul. 1(3): 151–63. [DOI] [PubMed] [Google Scholar]
- 32. Werhahn KJ, Kunesch E, Noachtar S, Benecke R, Classen J (1999) J Physiol. Differential effects on motorcortical inhibition induced by blockade of GABA uptake in humans. J Physiol 1;517(Pt 2): 591–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chen R, Lozano AM, Ashby P (1999) Mechanism of the silent period following transcranial magnetic stimulation: evidence from epidural recordings. Exp Brain Res 128: 539–42. [DOI] [PubMed] [Google Scholar]
- 34. Di Lazzaro V, Oliviero A, Meglio M, Cioni B, Tamburrini G, et al. (2000) Direct demonstration of the effect of lorazepam on the excitability of the human motor cortex. Clin Neurophysiol 111(5): 794–9. [DOI] [PubMed] [Google Scholar]
- 35. Ziemann U, Rothwell JC, Ridding MC (1996) Interaction between intracortical inhibition and facilitation in human motor cortex. J Physiol 1;496(Pt 3): 873–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ziemann U (2004) TMS and drugs. Clin Neurophysiol 115(8): 1717–29. [DOI] [PubMed] [Google Scholar]
- 37. Freeman HJ (2008) Pearls and pitfalls in the diagnosis of adult celiac disease. Can J Gastroenterol 22(3): 273–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hadjivassiliou M, Aeschlimann P, Strigun A, Sanders DS, Woodroofe N, et al. (2008) Autoantibodies in gluten ataxia recognize a novel neuronal transglutaminase. Ann Neurol 64(3): 332–43. [DOI] [PubMed] [Google Scholar]
- 39. Alaedini A, Okamoto H, Briani C, Wollenberg K, Shill HA, et al. (2007) Immune cross-reactivity in celiac disease: anti-gliadin antibodies bind to neuronal synapsin I. J Immunol 15. 178(10): 6590–5. [DOI] [PubMed] [Google Scholar]
- 40. Humeau Y, Doussau F, Vitiello F, Greengard P, Benfenati F, et al. (2001) Synapsin Controls Both Reserve and Releasable Synaptic Vesicle Pools during Neuronal Activity and Short-Term Plasticity in Aplysia. J Neurosci 21(12): 4195–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Williamson S, Faulkner-Jones BE, Cram DS, Furness JB, Harrison LC (1995) Transcription and translation of two glutamate decarboxylase genes in the ileum of rat, mouse and guinea pig. J Auton Nerv Syst 5 55(1-2): 18–28. [DOI] [PubMed] [Google Scholar]
- 42. Takenoshita H, Shizuka-Ikeda M, Mitoma H, Song S, Harigaya Y, et al. (2001) Presynaptic inhibition of cerebellar GABAergic transmission by glutamate decarboxylase autoantibodies in progressive cerebellar ataxia. J Neurol Neurosurg Psychiatry 70(3): 386–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hadjivassiliou M (2004) Glutamic acid decarboxylase as a target antigen in gluten sensitivity: the link to neurological manifestation? Proceedings of the 11th International Symposium on Celiac Disease. Belfast.
- 44. Hadjivassiliou M, Mäki M, Sanders DS, Williamson CA, Grünewald RA, et al. (2006) Autoantibody targeting of brain and intestinal transglutaminase in gluten ataxia. Neurology 14 66(3): 373–7. [DOI] [PubMed] [Google Scholar]
- 45. Hallert C, Derefeldt T (1982) Psychic disturbances in adult coeliac disease. Scand J Gastroenterol 17(1): 17–9. [DOI] [PubMed] [Google Scholar]
- 46. Ciacci C, Iavarone A, Mazzacca G, De Rosa A (1998) Depressive symptoms in adult coeliac disease. Scand J Gastroenterol 33(3): 247–50. [DOI] [PubMed] [Google Scholar]
- 47. Spampinato C, Aguglia E, Concerto C, Pennisi M, Lanza G, et al. (2013) Transcranial magnetic stimulation in the assessment of motor cortex excitability and treatment of drug-resistant major depression. IEEE Trans Neural Syst Rehabil Eng 21(3): 391–403. [DOI] [PubMed] [Google Scholar]
- 48. Bajbouj M, Lisanby SH, Lang UE, Danker-Hopfe H, Heuser I, et al. (2006) Evidence for impaired cortical inhibition in patients with unipolar major depression. Biol Psychiatry 1 59(5): 395–400. [DOI] [PubMed] [Google Scholar]
- 49. Fitzgerald PB, Brown TL, Marston NA, Daskalakis ZJ, de Castella A, et al. (2004) Motor cortical excitability and clinical response to rTMS in depression. J Affect Disord 82(1): 71–6. [DOI] [PubMed] [Google Scholar]
- 50.Brambilla P, Perez J, Barale F, Schettini G, Soares JC (2003) GABAergic dysfunction in mood disorders. Mol Psychiatry 8(8):721–37,715. [DOI] [PubMed]
- 51. Oberhuber G (2000) Histopathology of celiac disease. Biomed Pharmacother 54(7): 368–72. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.