Abstract
Studies have shown that unilateral cochlear implant users who have residual hearing in the contralateral ear can benefit from combining a hearing aid in the nonimplanted ear with their cochlear implant. The purpose of this study was to better understand the factors influencing decision making by adults. Adults who had discontinued hearing aid use shortly after cochlear implantation were selected from one Canadian cochlear implant program. An examination of hearing aid use revealed that of 96 patients, who used hearing aids preimplant, 49 had discontinued hearing aid use. Patient perspectives on the decision and experience of combining a hearing aid and a cochlear implant were collected through 12 individual semistructured interviews. The interviews were analyzed qualitatively to identify key themes. Questionnaires, based on the interview findings, were developed and sent to the 49 adults to further explore the factors affecting hearing aid decisions. Interview and questionnaire findings from 28 adults indicated that three factors primarily influenced patients' decision to discontinue hearing aid use: their perceptions of the experience with hearing aids prior to implantation, their views of superiority of a unilateral cochlear implant in comparison with hearing aids, and their perceptions of interference with sound quality when a cochlear implant and hearing aid were combined. This study provides information about patient perceptions, experiences, and understanding of the potential difficulties of a bimodal fitting that may assist clinicians in pre- and postimplant counseling.
Keywords: cochlear implant, hearing aid, bimodal hearing, deafness
Introduction
Cochlear implantation has progressed from an intervention in the 1990s for individuals with bilateral profound deafness who derived essentially no benefit from acoustic amplification (NIH Consensus Development Program, 1995) to a more widely used treatment procedure that also includes individuals with some usable residual hearing (Ching, van Wanrooy, & Dillon, 2007; Perreau, Tyler, Witt, & Dunn, 2007). Consequently, the current population of unilateral cochlear implant users includes adults with residual hearing in the contralateral ear, who may have access to sound through conventional acoustic amplification. Until recently, unilateral cochlear implantation has been standard practice; however, there is a trend toward bilateral implantation and a growing interest in the benefits of binaural hearing more generally. The combination of a unilateral cochlear implant and an acoustic hearing aid in the contralateral ear, also referred to as bimodal hearing (Ching et al., 2007; Ching, Incerti, & Hill, 2004; Luntz, Shpak, & Weiss, 2005), is one way of providing cochlear implant users, who have aidable hearing in the nonimplanted ear, with access to binaural hearing cues (Ching et al., 2004; Fitzpatrick, Séguin, Schramm, Chénier, & Armstrong, 2009; Mok, Grayden, Dowell, & Lawrence, 2006; Tyler et al., 2002).
The goals of bimodal hearing are to improve speech understanding by providing fine-frequency information that appears to be compromised through the presentation of electrical pulses from a cochlear implant as well as to provide binaural hearing cues (Ching et al., 2007; Ching, van Wanrooy, Hill, & Dillon, 2005; Dunn, Tyler, & Witt, 2005; Gifford, Dorman, McKarns, & Spahr, 2007; Holt, Kirk, Eisenberg, Martinez, & Campbell, 2005). Investigation of the complimentary effects of electric and acoustic stimulation has received increasing attention in recent years, first in laboratory-based studies and more recently in studies that also examine users' perspectives and satisfaction. The low-frequency information provided by acoustic amplification has been shown to blend with the high-frequency information provided by electrical stimulation despite the absence of open-set speech recognition through a hearing aid alone (Ching et al., 2004). Recent research has shown that even the addition of very low-frequency acoustic information (125-Hz low-passed signal) to electric information can result in improved word and sentence recognition (Zhang, Dorman, & Spahr, 2010). These investigators have proposed that much of the speech recognition benefit gained from combining these two different types of stimulation stems from the additional cues provided by the voice fundamental frequency (F0).
Despite the two different types of auditory input and the interaural differences in timing and level from the combination of acoustic and electrical stimulation, bimodal users are able to integrate auditory information to achieve binaural benefits (Potts, Skinner, Litovsky, Strube, & Kuk, 2009). Clinically, these enhancements translate into improved speech recognition in quiet and noise and improved localization abilities when performance with bimodal devices is compared with that with a unilateral cochlear implant (Ching et al., 2004, 2005; Luntz et al., 2005; Mok et al., 2006; Morera et al., 2005; Potts et al., 2009). In addition to benefits objectively measured in the laboratory, qualitative reports from patients using hearing aids in the nonimplanted ear suggest that bimodal hearing can improve listening for music, speech understanding in noise, and speech quality (Ching et al., 2004; Ching, Psarros, & Hill, 2000; Ching, Psarros, Hill, Dillon, & Incerti, 2001; Fitzpatrick et al., 2009; Keilmann, Bohnert, Gosepath, & Mann, 2009). Bimodal users have also reported greater ease of listening, improved auditory spatial organization, more balanced sound, and overall enhanced sound quality (Potts et al., 2009). These studies coupled with systematic literature reviews have led to strong support for bimodal hearing fittings for any patient with residual hearing as a first option to achieve binaural hearing benefits (Ching, 2005; Ching et al., 2007; Schafer, Amlani, Seibold, & Shattuck, 2007).
Despite evidence for the potential benefits of bimodal hearing for some patients, it is important to note that support for bimodal hearing is based primarily on laboratory studies with small clinical samples (see Ching et al., 2007; Schafer et al., 2007 for reviews). Relatively little is known about the extent to which individuals use bimodal hearing or about the factors that influence decisions to use a hearing aid in the contralateral ear. Our previous work with a clinical population of adults indicated that less than 40% of those with residual hearing of 100 dB HL or better (three frequency pure-tone average) used their hearing aid combined with their implant on a regular basis (Fitzpatrick et al., 2009). Other studies have documented low rates of hearing aid use of 10% to 19% (Syms & Wickenberg, 2002; Tyler et al., 2002), and anecdotal clinical evidences suggest that many patients discontinue hearing aid use in the contralateral ear following implantation. Some studies have indicated that there may be a relationship between amount of residual hearing in the nonimplanted ear and use of a hearing aid (Fitzpatrick et al., 2009; Mok et al., 2006; Morera et al., 2005).
In light of the documented benefits of binaural hearing through the use of acoustic amplification in the nonimplanted ear (Ching et al., 2007; Ching, Massie, Van Wanrooy, Rushbrooke, & Psarros, 2009; Schafer et al., 2007), it is important to investigate patient decisions related to hearing aid use. Studies examining bimodal hearing have generally focused on individuals who use a contralateral hearing aid, but it is also important to examine why other patients, despite having some residual hearing in the nonimplanted ear, have decided that combining a hearing aid and a cochlear implant is undesirable. Our previous research reported the benefits of bimodal stimulation from the perspective of patients who made the decision to continue using acoustic amplification postimplant (Fitzpatrick et al., 2009). To our knowledge, no studies have elicited the perceptions and experiences of patients relative to their decision to discontinue use of a hearing aid in the nonimplanted ear. The purpose of this study was therefore to further explore the decision-making process related to hearing aid use for adult cochlear implant recipients and to identify the factors affecting patients' decisions to discontinue hearing aid use.
Methods
Design
This study consisted of two inquiries: (a) semistructured interviews with patients who discontinued hearing aid use in the contralateral ear postimplantation, and (b) a survey of adult patients regarding their decision to discontinue hearing aid use with a cochlear implant. The qualitative interviews were conducted to elicit the perspectives of adult nonbimodal users and also to inform the subsequent survey. Ethical approval for the project was received from the Ottawa Hospital Research Ethics Board, and informed written consent was obtained prior to data collection.
Sample
The sample frame for the study was drawn from the adult patient population at the University of Ottawa Cochlear Implant Program, Ottawa Hospital. Patients who met the following inclusion criteria were identified through a review of patient records implanted from 1999 to 2009: (a) postlingual deafness, (b) age 18 years or older at implantation, (c) use of a hearing aid in the nonimplanted ear prior to cochlear implant surgery, and (d) nonbimodal user, defined as no hearing aid use or discontinued use by 6 months postimplant. A decision was made to select participants based on previous hearing aid use rather than to apply a definition of aidable hearing, as several previous studies have suggested that pure-tone audiometric levels may not be a useful predictor of bimodal fitting benefits (Ching et al., 2004; Gifford et al., 2007; Mok et al., 2006). We did not include any participant who did not wear a hearing aid in the nonimplanted ear preimplant as review of chart information indicated that no patient in this category had been fit with a hearing aid following surgery. We excluded patients who underwent surgery at other centers because information was not available on preimplant hearing aid use.
Only patients implanted since June 1999 were selected because our previous work (Fitzpatrick et al., 2009) showed that prior to that time, no patients combined a hearing aid with a cochlear implant. This practice was consistent with stricter audiometric criteria for cochlear implantation and clinical protocols at the time. Patients who could not complete the questionnaire in English or who were not followed for programming at the center were excluded. After applying all inclusion criteria except preimplant hearing aid use, 168 adults implanted and followed by the cochlear implant center were available. Of these, 72 individuals had not used a hearing aid in the nonimplanted ear prior to implantation, leaving 96 adults. Acoustic amplification continued to be used in the nonimplanted ear by 47 of these adults, leaving 49 participants with discontinued hearing aid use available for the study. Twelve patients were invited to participate in the qualitative interviews with the option to add additional interviews if theoretical saturation was not reached. Subsequently, all eligible patients identified through the chart review were invited to complete a survey questionnaire.
Qualitative Interviews
Consistent with qualitative techniques, purposeful sampling was used to select 12 patients who varied according to gender, amount of residual hearing, duration of deafness, age at implantation, and duration of implant use. Individual interviews were selected to probe specific issues with patients and to facilitate communication with this population. An interview guide provided base questions for the interviews, and questions were explored more in-depth with individual patients as is commonly practiced in qualitative research. The questions probed three general themes: (a) decision making, (b) experience with hearing aid and cochlear implant such as sound quality and speech understanding, and (c) factors influencing decisions to discontinue hearing aid use. Interviews of approximately 30 to 40 min in duration were conducted either at the cochlear implant clinic or in participants' home according to their preference. The interviewers included an audiologist experienced in cochlear implants and a graduate student. One researcher conducted the interview while another took notes during the meeting. Participants were asked to share their experiences in a conversation format and were encouraged to share any details they felt were important to contribute to understanding the reasons for nonbimodal use. Interviewing of new participants continued until theoretical saturation was used, that is, no new themes were apparent from the data.
Data analysis. Data collection and analysis proceeded concurrently with all interviews being transcribed verbatim shortly after the interviews. These 12 interviews and interview session notes provided the data set for analysis. The overall goal was to identify patterns and themes within the experiences recalled by the participants. Data were analyzed using qualitative software (NVivo Version 8) to sort and organize the textual data. Analysis involved a constant comparative analysis, a methodology drawn from grounded theory analysis described by Strauss and Corbin (1998). The first step involved reading and rereading of all transcripts, followed by open coding that consisted of a line by line coding of the data into concepts. These interview data were compared with all others to identify similarities and differences to develop conceptualizations of the relations between various pieces of data. These concepts were then grouped into categories or ideas and finally into major themes. All data were coded by one reviewer; verifications were conducted by a second reviewer; and category groupings were determined by both researchers together to identify the major themes.
Questionnaire
The four-page questionnaire used Likert-type scaled items and multiple-choice responses to elicit patients' views of (experiences with) hearing aid use with a unilateral cochlear implant and their reasons for discontinuing hearing aid use. The full questionnaire is included in Appendix. The 17 items were primarily based on the themes assembled from the qualitative interview analysis comments obtained from bimodal users in a previous study (Fitzpatrick et al., 2009) as well as literature that has documented benefits of bimodal use. The questions were divided into three main areas of inquiry pertaining to (a) experience with acoustic amplification before cochlear implantation, (b) decision process related to hearing aid use in the contralateral ear, and (c) experience with a cochlear implant combined with a hearing aid after surgery. For example, for the preimplant category, participants were asked to rate their experience with hearing aids from 1 = not at all helpful to 4 = very helpful. A question from the postsurgery category required participants to report how long a hearing aid was used in the contralateral ear with possible responses ranging from 1 = not at all to 4 = for 1 to 6 months. Some questions, for example, those probing quality of sound with a cochlear implant and hearing combined offered participants the possibility of providing multiple responses. Participants were also asked to add any additional comments regarding hearing aid and cochlear implant use. Participants were asked the number of years of implant use; all other demographic and clinical information was collected through chart reviews.
The survey was sent to a total of 49 participants including all 12 participants from the interview phase and the 37 other individuals who met the study criteria. The questionnaire was distributed through patients' audiologists via electronic or paper mail selected based on their usual method of correspondence with the patient. All participants were offered the option to respond electronically or via paper mail. Participants who did not respond were sent one reminder and a copy of the questionnaire and consent form 2 weeks after the initial distribution.
Data analysis. All results were entered into an Excel file, and questionnaire responses were analyzed descriptively. Components were assigned descriptive labels that corresponded to the information elicited, such as amount of hearing aid use preimplant, duration of hearing aid use postimplant, quality of speech. Questions that required a rating were assigned a number to facilitate coding: 1 = not helpful, 2 = rarely helpful, 3 = somewhat helpful, and 4 = very helpful. Qualitative questions that asked respondents to explain the principal factors for discontinued hearing aid use and to add other comments were summarized descriptively and organized according to themes. The responses were compiled for the 28 respondents, and all comments were coded by one investigator using qualitative coding techniques (Crabtree & Miller, 1992). The codes represented factors perceived to interfere with the decision to use a hearing aid and were reviewed by a second investigator for agreement.
Results
Qualitative Interviews
The clinical characteristics of the 12 interview participants, 9 women and 3 men, are shown in Table 1. Pure-tone average (500, 1,000, 2,000 Hz) in the nonimplanted ear ranged from 75.0 to 118.3 dB HL, and low-frequency pure-tone average at 250 and 500 Hz ranged from 30 to 125 dB HL. All but one patient used a unilateral Clarion cochlear implant. Patients underwent surgery between 2000 and 2008 and were implanted with the most current technology at the time. Duration of severe to profound hearing loss ranged from 1.2 to 20.4 years, and cochlear implant use ranged from 1.9 to 9.2 years.
Table 1.
Description of Interview Participants
| Participant | Sex | Duration of severe to profound HL (years) | Duration of CI use (years) | PTA contralateral ear (dB HL) | Low-frequency PTA (dB HL) | Low-mid-frequency PTA (dB HL) |
|---|---|---|---|---|---|---|
| P01 | F | 5.1 | 1.9 | 100.0 | 82.5 | 90.0 |
| P02 | F | 1.1 | 5.2 | 75.0 | 30.0 | 46.7 |
| P03 | F | 7.1 | 9.2 | 110.0 | 97.5 | 100.0 |
| P04 | M | 1.4 | 2.6 | 103.3 | 77.5 | 86.7 |
| P05 | F | 10.4 | 5.1 | 116.7 | 125.0 | 121.7 |
| P06 | F | 9.0 | 8.3 | 96.7 | 60.0 | 75.0 |
| P07 | F | 2.2 | 2.2 | 91.7 | 30.0 | 58.3 |
| P08 | F | 14.3 | 5.7 | 111.7 | 110.0 | 110.0 |
| P09 | F | 20.4 | 6.1 | 118.3 | 102.5 | 108.3 |
| P10 | F | 15.7 | 4.7 | 116.7 | 110.0 | 111.7 |
| P11 | M | 6.9 | 4.6 | 85.0 | 45.0 | 58.3 |
| P12 | M | 3.9 | 5.4 | 96.7 | 82.5 | 88.3 |
| Minimum | 1.1 | 1.9 | 75.0 | 30.0 | 46.7 | |
| Maximum | 20.4 | 9.2 | 118.3 | 125.0 | 121.7 | |
| Median | 7.0 | 5.2 | 101.6 | 82.5 | 89.2 |
HL = hearing loss; CI = cochlear implant; PTA = pure-tone average at 250, 500, 1,000 Hz; Low-frequency PTA = average of 250, 500 Hz; Low-mid-frequency PTA = average of 500, 1,000 Hz.
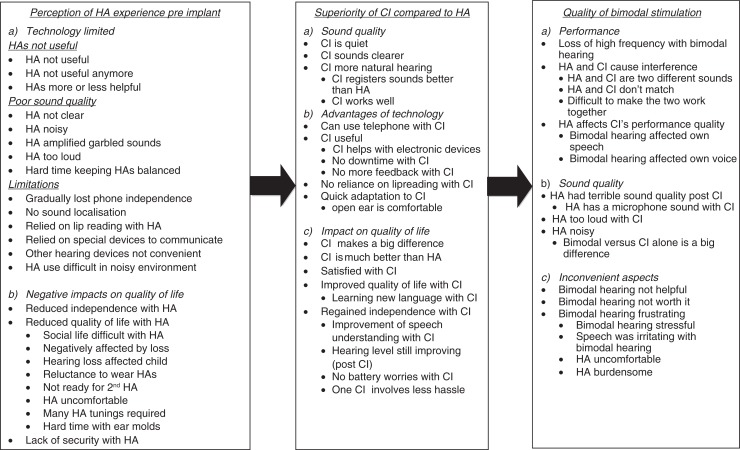
Through our data analysis, three key themes became apparent as influencing patients' decision to discontinue hearing aid use postimplant. Figure 1 provides an overview of the major themes and subthemes extracted from these qualitative interviews. The figure shows that there are three broad factors that influenced contralateral hearing aid use following unilateral cochlear implantation. These include perceptions of hearing aid experience preimplant, superiority of the cochlear implant, and quality of bimodal stimulation. The paragraphs below provide a brief summary of the topics as well as examples of these main themes from the participants themselves.
Figure 1.
Major themes and subthemes extracted from the qualitative interviews
Perception of hearing aid experience preimplant. Preimplant experience emerged as a dominant topic of discussion during the interviews. Patients described their experiences primarily as negative, characterizing their hearing aid as not helpful and cumbersome. Many participants noted that a hearing aid used to provide some assistance for hearing and communication but that gradually their hearing had deteriorated to the point where they perceived the hearing aid to be of little use. More interestingly, for some participants, hearing aids were viewed as outdated old technology compared with new cochlear implant technology. The hearing ability and new technology interrelationship for some individuals was substantive, and this perception of new versus old technology sometimes appeared to be a barrier to continuing to use a hearing aid with their implant. Overall, patients associated their previous functioning when using hearing aids with a poorer quality of life and suggested that their preimplant hearing aid experience was a principal reason for not having confidence that a hearing aid could be helpful when combined with a cochlear implant.
I just think× it's [cochlear implant] so new, and if somebody's been wearing hearing aids for a long time and then they get an implant and it works well for them. (P01)
They [hearing aids] more or less provided what I needed, but I always seemed to need stronger and stronger and stronger. At the end I had two very powerful hearing aids× I was really getting up in technology, but the s-sound was never clear. (P06)
And [with] just the hearing aid, I hadn't used the phone in ten years. (P06)
Superiority of cochlear implant compared with hearing aid. The implant represents for most individuals a major decision and personal investment for themselves and their families. Accordingly, their early postimplant experience greatly affects individuals' overall views of what constitutes good or at least adequate hearing. For these participants, there was generally a sense of security, success, and attachment associated with their cochlear implant that far surpassed their perception of hearing and overall well-being prior to cochlear implantation. All but one patient reported having tried a hearing aid at least for a very brief period of time following surgery. However, frequently, the superiority of the cochlear implant, compared with previous experience with hearing aids, was put forth as a reason for not “bothering” with the use of a hearing aid in the contralateral ear. For these patients, the perception of restoration of better hearing from a very positive cochlear implant experience was an important factor influencing their decision to discontinue hearing aid use after implantation.
I find like, the implant is so much better—that the hearing aid and the implant are two different things. (P01)
I was so pleased with it [cochlear implant] and it was successful that I just forgot the hearing aid. (P05)
Quality of bimodal stimulation. The initial experiences of individuals when they use a hearing aid, combined with a cochlear implant, influence their willingness to continue to access acoustic information through both devices. For these individuals, bimodal hearing was described as falling into two broad dimensions: not helpful and poorer sound quality. For the “not helpful” group, hearing aid use did not improve the adult's perception of improved hearing. This group of individuals simply felt that it did not contribute any additional information to assist with speech understanding and therefore was not worth the trouble, as explained in one participant's words:
I've gone through the surgery, it's [cochlear implant] working beautifully for me; why would I put myself through the [agony] of more garbled sounds?. (P02)
Other individuals clearly rated the combined devices as not only unhelpful but also having a negative effect on the quality of sound. They reported that using a hearing aid with their implant interfered with “good” hearing. These individuals described bimodal hearing as bothersome and a threat to the improved hearing they had achieved through cochlear implantation. As illustrated below, various descriptive terms were used when discussing this phenomenon.
Because it was taking away all the good sound× of my implant, and it sounded so “ugh,” it sounded awful× even my implant didn't sound the same. (P06)
Questionnaire
Characteristics of participants. Of the 49 questionnaires distributed, 28 (57.1%) were returned. Eight of these were from the 12 adults who also participated in the interviews. Table 2 presents information on the questionnaire respondents as well as the 21 nonrespondents. The majority (45 of 49) of the total patients available for study used a Clarion implant. Of the 28 respondents, 4 used a Nucleus device and 24 used a Clarion device. The Clarion group included 7 individuals implanted between 2000 and 2001 who used a Clarion CII device, and the remaining 17 individuals were implanted from 2002 to 2009 with the most recent version of the Clarion HiRes90K implant that was available at the time. The groups did not differ significantly on any key clinical characteristics; however, there were more women than men among the respondents. The respondents included 20 women and 8 men who were implanted at a mean age of 59.0 (SD = 12.7) years and had a mean duration of cochlear implant use of 6.3 (SD = 2.3) years.
Table 2.
Characteristics of Questionnaire Respondents and Nonparticipants
| Questionnaire respondents (n = 28) | Nonparticipants (n = 21) | |
|---|---|---|
| Gender (%) | ||
| Female | 20 (71.4%) | 10 (47.6%) |
| Male | 8 (28.6%) | 11 (52.4%) |
| Duration of deafness—years, median (IQR) | 6.5 (1.48–14.9) | 7.0 (3.8–16.3) |
| PTA contralateral ear—dB HL, M (SD) | 98.8 (14.7) | 98.2 (14.6) |
| Low-frequency PTA contralateral ear—dB HL, M (SD) | 84.5 (22.3) | 80.4 (26.3) |
| Low-mid-frequency contralateral ear—dB HL, M (SD) | 89.8 (18.7) | 87.0 (20.7) |
| Age implanted—years, M (SD) | 59.0 (12.7) | 56.2 (15.4) |
| Duration of CI use—years, M (SD) | 6.3 (2.3) | 5.6 (2.9) |
CI = cochlear implant; PTA = pure-tone average at 250, 500, 1,000 Hz; Low-frequency PTA = average of 250, 500 Hz; Low-mid-frequency PTA = average of 500, 1,000 Hz; IQR = interquartile range.
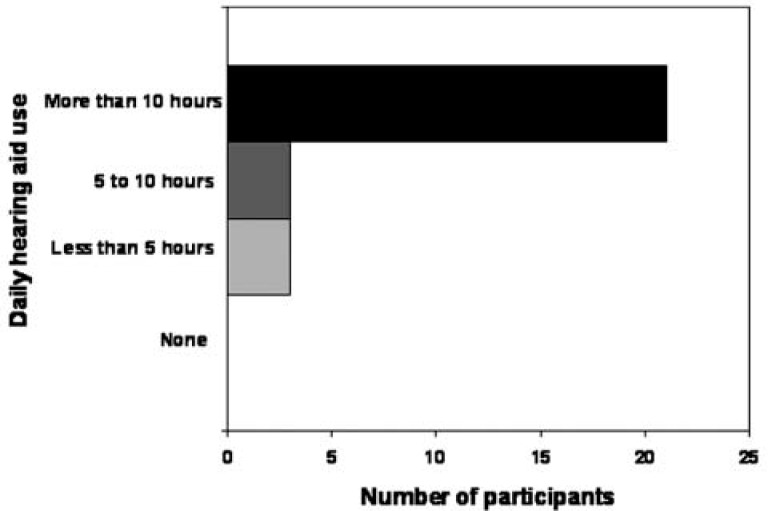
Preimplant hearing aid experience. Although the participants in this study had all discontinued hearing aid use immediately or within 3 months after cochlear implantation, as shown in Figure 2, the majority of the participants were regular hearing aid users prior to surgery (21/28). Most (19/28) individuals achieved speech understanding with their hearing aids combined with lipreading. Furthermore, the majority of these individuals (19/28) judged their amplification to be somewhat or very helpful. Therefore, there was no clear indication from these responses that decision making was related to a lack of hearing aid use prior to implantation. Individuals were asked to rate their perception of how they coped with hearing aids. Approximately half (15/28) judged that they coped well at least some of the time, whereas another half indicated that they did not cope well with hearing aids.
Figure 2.
Participants' report of daily hearing aid use preimplant
Decision process regarding hearing aid use with a cochlear implant. The majority of individuals indicated, prior to their surgery they had not made a decision regarding hearing aid use after implantation. Most of the patients (17 of 28) recalled having discussed hearing aid use with their audiologist either before or both before and after surgery. A few patients could not remember whether the topic had been discussed. Fourteen individuals also indicated that their audiologist had specifically encouraged them to wear their hearing aid along with their cochlear implant.
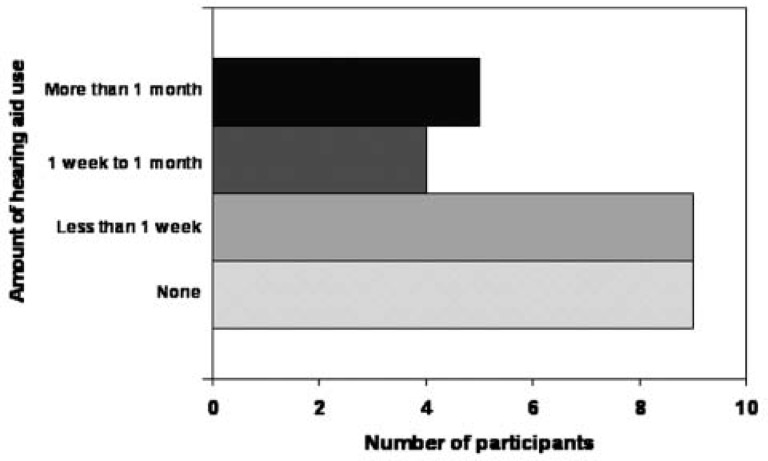
Experience with hearing aids after cochlear implantation. As shown in Figure 3, of the 27 participants who completed questions about postimplant hearing aid use, the majority (18 of 27) reported less than 1 week of hearing aid use, and half of these (9 of 18) reported no postimplant hearing aid use. Only 9 individuals attempted hearing aid use for more than 1 week, 5 of them having tried the hearing aid for more than 1 month. Of those who used their aid, the majority (11 of 14) reported wearing it all the time during the early trial period. The majority of individuals indicated that their device was less than 5 years old (12 of 18). Six individuals indicated that they required hearing aid optimization or adjustments by their audiologist during the trial period. The following comment from one respondent captures the experience of several of these patients:
Figure 3.
Participants' report of hearing aid use postimplant
I only wore my hearing aid, in the left ear, until my implant was working well enough to wear alone. During this time, in the first month/month and a half I wore my hearing aid in the left ear and the implant at the same time to work and at home but many times throughout the day, I would turn off the hearing aid in order to get the implant working. The hearing aid was only turned on when I needed to listen and communicate with family and co-workers. The more I used the implant by itself the better everything got. Eventually, once the implant was working very well and I felt comfortable with it, I stopped wearing the hearing aid, altogether.
Factors affecting hearing aid use. In an open-ended question, participants were asked to identify the three principal factors that influenced their decision to discontinue using their hearing aid with their cochlear implant. The three primary reasons reported for discontinuing hearing aid use included: superior sound quality with the cochlear implant compared with the hearing aid (8 participants), no perceived additional benefit from the hearing aid (7 participants), and degraded acoustic signal with the hearing aid and cochlear implant combined (6 participants). One participant indicated that the additional hearing aid costs were not justified given the limited benefits. The following responses extracted from six different questionnaires summarize these participants' perceptions.
(a) The quality of the cochlear implant sound was lost using the hearing aids. (b) Sound seemed “unbalanced” and confusing. (c) I wore these half my life, and I preferred to work more on perfecting my cochlear implant programs than hassling with hearing aids.
I was so happy with the success of my cochlear implant. Just one less thing to be concerned with, hearing aid, batteries, and so on.
I was able to hear so well with the implant that I felt I didn't need the hearing aid.
Did not like the difference in sound between cochlear implant and hearing aid.
I can only think of one [reason] and that is that it did not make any difference in my hearing, if I used it or did not use it.
The two different sounds were confusing. I only had low noises on the hearing aid side. My hearing was too far gone.
It just did not make a difference. It is as if I could no longer benefit from hearing aid and was only able to hear from the implant.
Discussion
This is the first questionnaire to examine the factors influencing patients' decision to use a hearing aid in conjunction with a bilateral cochlear implant. In a previous study, we documented that, despite evidence of the binaural advantages, less than 25% of adult patients implanted between 1999 and 2005 regularly used bimodal hearing (Fitzpatrick et al., 2009). In the present study, detailed descriptive data from both qualitative interviews and questionnaires revealed several key factors associated with patients' decision making on bimodal hearing use. The principal factors were related to their perceptions that hearing aids were not helpful preimplant; hearing aids were old technology; hearing with a cochlear implant far surpassed that with hearing aids; and bimodal hearing interfered with speech understanding. It is striking that although a majority of questionnaire respondents (21 of 28) reported always wearing their hearing aid before implantation and 19 of 28 rated acoustic aids as very or somewhat helpful, none of these patients used a hearing aid after cochlear implant surgery. In fact, only five participants used a hearing aid for more than a 1-month period.
Patients in this study frequently described their preimplant hearing aid experience as negative both in terms of speech understanding and social inclusion. A number of patients referred to hearing aids as old technology. In this regard, some patients appeared to have made the decision to discard their hearing aid based on their previous experience with acoustic amplification even without a trial period with bimodal devices. A dominant theme from our interviews and questionnaire responses was that the cochlear implant was superior in terms of the amount and quality of hearing to anything that the hearing aid could offer. Participants tended to compare and contrast the very substantive benefits from their cochlear implant with the limited benefit from hearing aids and frequently indicated that the hearing provided by their cochlear implant was sufficient and had improved their daily functioning and overall quality of life. Essentially, when the cochlear implant was viewed as successful, patients felt it was unnecessary to add another device. In this sense, these participants tended to view acoustic and electric stimulation as two separate treatments for hearing loss, rather than as an ensemble of hearing technology that could be combined to optimize hearing.
The perceptions of patients in this study are in contrast to other reports that suggest (Ching et al., 2007; Schafer et al., 2007) that many patients with residual hearing can benefit from bimodal hearing. In the present study, more than half of the patients who used a hearing aid in the nonimplanted ear prior to implantation discontinued hearing aid use in the contralateral ear after unilateral implantation. Although hearing aids were consistently used preimplant, many patients did not feel that the hearing aid contributed additional information postimplant. Similar to our previous study, in which we investigated patients' experiences with bimodal fittings, our findings suggest that bimodal use may not be desirable for many patients and that hearing aid use may not be related to amount of residual hearing (Fitzpatrick et al., 2009).
Despite the evidence in the literature for binaural advantages, this analysis revealed that numerous patients do not perceive improvement with a hearing aid and cochlear implant and in fact, judge the hearing aid as interfering with the good sound quality of the implant, therefore causing deterioration in hearing quality. Given the range of preimplant residual hearing for participants in this study and limited amount of postimplant hearing aid use, there is no indication that these perceptions were related to hearing loss characteristics. An interesting finding of this analysis was that decision to use hearing aid was strongly influenced by the perception that hearing was very good with a cochlear implant and that a hearing aid was simply not worth the extra trouble and discomfort. In fact, hearing aid discomfort and annoyances were a major theme in the interview data collected.
Although a body of evidence has accumulated in support of bilateral implants, as pointed out by Ching et al. (2009), there is a lack of high-quality studies comparing bimodal fitting and binaural implant results. Consequently, guidelines for deciding on bimodal fitting or bilateral implantation to achieve binaural hearing have not been well established. Furthermore, studies indicate that it is difficult to determine who will benefit from bimodal fittings and that there is no clear relationship between bimodal use and preimplant audiometric characteristics such as pure-tone average or speech perception scores (Schafer et al., 2007). Continued research and evaluation in this area will help identify whether certain interventions, for example, counseling techniques, hearing aid trial periods, would likely positively influence the bimodal experience, allowing some adults to benefit from some aspects of binaural hearing. The potential policy implication of this type of research is whether investment in bimodal hearing will be more cost-effective than the more expensive bilateral implant interventions. The relative benefits of different interventions would be a consideration. In some health regions, where implants are publicly funded, bilateral implants are not yet widely available for adults. Therefore, any opportunity to offer binaural hearing should be considered. The increased attention to binaural hearing, largely motivated by the trend toward bilateral cochlear implants, makes the potential benefits or negative aspects of bimodal hearing a good choice for further examination. In this study, we have outlined factors beyond specific quantitative outcomes such as speech recognition ability that appear to influence the decision to pursue bimodal hearing. Achieving the best available hearing for a given individual, as pointed out by Perreau et al. (2007), is a complex issue.
It is increasingly understood that health-related behaviors are influenced by more than health services. In this article, a number of factors are presented that help focus our understanding of why some adults choose not to use a hearing aid postimplant. Although this study highlights the role of prior experience and beliefs, current cochlear implant experience, and bimodal listening experiences in shaping decisions around bimodal use, there are unanswered questions. One question is whether pre- and postimplant counseling might influence adults' choices and possibly enhance bimodal listening experiences for some patients. Another area of exploration is whether a trial period for all patients would affect hearing aid use. An improved understanding of these determinants of behavior may help audiologists focus their counseling when discussing the benefits of contralateral hearing aid use. For any given intervention, it is important to understand the factors that are most likely to lead to a positive outcome. Pre- and postimplant hearing experiences with hearing aids and a cochlear implant clearly influence the likelihood of subsequent hearing aid use, but it is unclear to what degree clinical support and services can mediate the relationship between positive cochlear implant experience and use of bimodal hearing. Continued research in this area including patients' experiences and views can help inform the evidence base for clinical decision making relative to appropriate recommendations for hearing aid use. A better understanding of the interrelationship between cochlear implant satisfaction, quality of hearing, and other factors would be useful.
The bulk of the existing evidence for bimodal hearing is related to quantifiable outcomes measures from speech perception tests obtained in laboratory and clinical settings. This study extends previous work by examining, from the perspective of patients, the factors that influence their decision to discontinue hearing aid use despite the presence of residual hearing that was amplified prior to implantation. The factors identified here may not be the most important bimodal hearing-related factors, but rather they were the easiest for participants to explain their behaviors related to hearing aid use. Other mechanisms such as amount of residual hearing and quality of residual hearing could be more important; however, the relationship between degree and range of hearing and bimodal outcomes is not well established. Costs of maintaining a hearing aid may be a factor when benefit is perceived as limited; however, patients in this study were responsible for the upkeep of their cochlear implant devices and did not refer to costs as a barrier to hearing aid use. All patients received audiologic services through a publicly funded health care system. In our previous research (Fitzpatrick et al., 2009), we questioned whether lack of hearing aid adjustment or information from clinicians about bimodal hearing might be a factor. This factor was not strongly supported by the current study findings as most patients appeared to be aware that hearing aid use was an option and in many cases reported that their audiologist had recommended bimodal use. All patients who undergo cochlear implantation are followed through the same publicly funded cochlear implant center where they are provided with audiologic services for cochlear implant and hearing aid management. Therefore, the patients described in our previous work who used a hearing aid postimplant (Fitzpatrick et al., 2009), and the participants in the current study had access to the same hearing aid fitting and optimization practices. A potentially motivating factor influencing the adaptation to and adoption of any hearing technology may be individual lifestyle factors such as type of employment and socialization. Our previous examination of cochlear implants recipients' decision to use an FM system suggested that factors related to individual expectations and lifestyle influenced frequency and amount of FM use (Fitzpatrick et al., 2010). This factor did not surface during the qualitative interviews as a determinant of hearing aid use but was not specifically explored with participants.
The study is limited by the fact that participants were drawn from only one clinical setting, and it is not possible to disentangle the effects of specific clinical practices on patients' perceptions related to hearing aid experiences. The majority of participants in this study used various generations of the Clarion device; however, we are unaware of any evidence that supports a higher probability of hearing aid use in combination with specific cochlear implant devices. As only nonbimodal users were included in this research, we are unable to compare any participant-related factors with the decision to use or not use hearing aids. It is also possible that the results were affected by social response bias in that patients may have provided socially desirable answers, particularly when asked questions about the information received through their clinical programs. Therefore, the findings of this research need to be interpreted within the context of these potential weaknesses. A strength of this study is that two data sources were used to collect the data. Through the 28 questionnaire responses, we were able to elicit and quantify the perspectives of a larger number of non–hearing aid users than was possible through only patient interviews. This triangulation of data allowed us to confirm the findings from the smaller number of qualitative interviews. At the same time, the questionnaire was strengthened by grounding the questions in patient-specific concerns and experiences documented during the interviews.
Achieving optimal hearing for individuals with cochlear implants requires consideration of many different options and different benefits experienced from different technologies. Despite the fact that research has documented, at least in a laboratory setting, benefits related to bimodal hearing, many patients do not find the addition of a hearing aid to provide binaural advantages or to be a positive experience. This study indicates that patients' willingness to use bimodal hearing is related to their perceptions of their preimplant experience, quality hearing through a cochlear implant, and their perception of improved sound quality in real-life situations that would make the perceived extra efforts related to operating and wearing a hearing aid worthwhile. Further research is required to study whether these factors are effective barriers that can be overcome through appropriate counseling and bimodal hearing trial periods with optimal management of combined hearing technologies. An enhanced understanding of the factors influencing patients' decisions may help clinicians to modify their recommendations and counseling and thereby increase patient exposure to the potential benefits of combining acoustic and electrical stimulation.
Acknowledgments
We are grateful to the patients from the University of Ottawa (Ottawa Hospital) Cochlear Implant Program for so willingly participating in our research. We also thank C. Séguin, S. Armstrong, and J. Chénier at the Ottawa Hospital for informing participants about the study and for their ongoing interest in this area of research. We thank J. Whittingham and V. Doiron for assistance with data management.
Appendix: Questionnaire: The Benefits of a Hearing Aid for Cochlear Implant Patients
Some people who have received a cochlear implant continue to wear their hearing aid in the opposite ear, whereas others do not. Through the following questions, we are seeking a better understanding of the factors that influenced your decision not to use your hearing aid with your cochlear implant. Please respond to each question by marking the box □ beside the answer that best describes your experience. Please feel free to add any information or comments in the space provided or on a separate page (Please write the question number beside your comments).
Your Experience With Hearing Aids Before You Received Your Cochlear Implant
-
Could you hear environmental sounds with your hearing aid(s) before your surgery?
-
□
Yes
-
□
No
-
□
-
Could you understand people talking to you with your hearing aid(s) before your surgery?
Without lipreading □ Yes □ No
With lipreading □ Yes □ No
-
How much did you wear your hearing aid(s)?
-
□
More than 10 hr a day (always or almost always)
-
□
5 to 10 hr a day (sometimes)
-
□
Less than 5 hr a day (rarely)
-
□
Never
-
□
-
All in all, how helpful was your hearing aid(s)?
-
□
Very helpful
-
□
Somewhat helpful
-
□
Rarely helpful
-
□
Not at all helpful
-
□
-
How do you feel that you coped with your hearing loss before you received your implant?
-
□
Well all of the time
-
□
Well much of the time
-
□
Well some of the time
-
□
Not well at all (It really affected me negatively)
-
□
Comments on coping with hearing loss before receiving a cochlear implant:

Your Decision Process About Using a Hearing Aid With Your Cochlear Implant
-
6.
Had you made a decision before your surgery about whether you would use your hearing aid with your cochlear implant?
-
□
Yes
-
□
No
-
□
-
Did your audiologist talk to you about the possibility of wearing your hearing aid with your cochlear implant?
-
□
Yes, before my surgery
-
□
Yes, after my surgery
-
□
Yes, both before and after my surgery
-
□
No, use of a hearing aid was not discussed
-
□
I can't remember
-
□
-
Did your audiologist encourage you to try wearing your hearing aid with your cochlear implant?
-
□
Yes, before my surgery
-
□
Yes, after my surgery
-
□
Yes, both before and after my surgery
-
□
No
-
□
I can't remember
-
□
Comments:

Your Experience With Hearing Aids After Your Cochlear Implant Surgery
-
9.
After receiving your implant, how long did you use your hearing aid in the other ear?
-
□
I used my hearing aid for 1 to 6 months
-
□
I used my hearing aid for 1 to 4 weeks
-
□
I used my hearing aid for 1 to 7 days
-
□
I used my hearing aid for less than 1 day
-
□
I did not use my hearing aid at all
-
□
-
In which of the following settings did you wear your hearing aid with your cochlear implant? Please check ALL that apply.
-
□
I wore my hearing aid at work only
-
□
I wore my hearing aid at home only
-
□
I wore my hearing aid at home and work
-
□
I wore my hearing aid everywhere I went
-
□
I did not wear my hearing aid at all
-
□
-
In which of the following listening conditions did you wear your hearing aid with your cochlear implant? Please check ALL that apply.
-
□
I wore my hearing aid in noisy situations only
-
□
I wore my hearing aid in quiet situations only
-
□
I wore my hearing aid in both noisy and quiet situations
-
□
I wore my hearing aid when listening to music
-
□
Other, specify:_____
-
□
I did not wear my hearing aid at all
-
□
-
How did speech sound when you used your hearing aid with your cochlear implant? Please check ALL that apply.
-
□
Speech was not clear
-
□
Speech was too loud
-
□
There was interference between the cochlear implant and the hearing aid
-
□
Cochlear implant and hearing aid were two very different sounds
-
□
Comments:

-
13.
When you used your hearing aid with your cochlear implant, did you use the same hearing aid you wore before your surgery?
-
□
Yes
-
□
No
-
□
-
How old was the hearing aid you used with your cochlear implant?
-
□
More than 10 years old
-
□
5 to 10 years old
-
□
3 to 5 years old
-
□
Less than 3 years old
-
□
-
Did your audiologist make any adjustments to your hearing aid with your cochlear implant?
-
□
Yes
-
□
No (the same settings that were in place before my surgery were used)
-
□
-
List the three factors that most influenced your decision not to use your hearing aid with your cochlear implant?
_________________________________________
_________________________________________
_________________________________________
-
Please feel free to share any additional information concerning the reasons why you decided not to wear your hearing aid in conjunction with your cochlear implant.
_________________________________________
_________________________________________
_________________________________________
Thank you for completing this questionnaire.
Declaration of Conflicting Interests
The author(s) declared that they had no conflicts of interest with respect to their authorship or the publication of this article.
Funding
The author(s) disclosed that they received the following support for their research and/or authorship of this article: This study was funded by grants from the Faculty of Health Sciences and the Faculty of Graduate Studies, University of Ottawa.
References
- Ching T. Y. C. (2005). The evidence calls for making binaural–bimodal fittings routine. Hearing Journal, 58(11), 32, 34,, 36,, 38,, 40–41 [Google Scholar]
- Ching T. Y. C., Incerti P., Hill M. (2004). Binaural benefits for adults who use hearing aids and cochlear implants in opposite ears. Ear and Hearing, 25, 9–21 [DOI] [PubMed] [Google Scholar]
- Ching T. Y. C., Massie R., Van Wanrooy E., Rushbrooke E., Psarros C. (2009). Bimodal fitting or bilateral implantation? Cochlear Implants International, 10(Suppl. 1), 23–27. 10.1002/cii.381 [DOI] [PubMed] [Google Scholar]
- Ching T. Y. C., Psarros C., Hill M. (2000). Hearing aid benefit for children who switched from the SPEAK to the ACE strategy in their contralateral nucleus 24 cochlear implant system. Australian and New Zealand Journal of Audiology, 22, 123–132 [Google Scholar]
- Ching T. Y. C., Psarros C., Hill M., Dillon H., Incerti P. (2001). Should children who use cochlear implants wear hearing aids in the opposite ear? Ear & Hearing, 22, 365–380 [DOI] [PubMed] [Google Scholar]
- Ching T. Y. C., van Wanrooy E., Dillon H. (2007). Binaural–bimodal fitting or bilateral implantation for managing severe to profound deafness: A review. Trends in Amplification, 11, 161–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching T. Y. C., van Wanrooy E., Hill M., Dillon H. (2005). Binaural redundancy and inter-aural time difference cues for patients wearing a cochlear implant and a hearing aid in opposite ears. International Journal of Audiology, 44, 513–521 [DOI] [PubMed] [Google Scholar]
- Crabtree B., Miller W. (1992). Doing qualitative research. Newbury Park, CA: Sage [Google Scholar]
- Dunn C. C., Tyler R. S., Witt S. A. (2005). Benefit of wearing a hearing aid on the unimplanted ear in adult users of a cochlear implant. Journal of Speech, Language, and Hearing Research, 48, 668–680 [DOI] [PubMed] [Google Scholar]
- Fitzpatrick E. M., Fournier P., Séguin C., Armstrong A., Chénier J., Schramm D. (2010). Users' perspectives on the benefits of FM sytems. International Journal of Audiology, 49, 44–53 [DOI] [PubMed] [Google Scholar]
- Fitzpatrick E. M., Séguin C., Schramm D., Chénier J., Armstrong S. C. (2009). Users' experience of a cochlear implant combined with a hearing aid. International Journal of Audiology, 48, 172–182 [DOI] [PubMed] [Google Scholar]
- Gifford R. H., Dorman M. F., McKarns S. A., Spahr A. J. (2007). Combined electric and contralateral acoustic hearing: Word and sentence recognition with bimodal hearing. Journal of Speech, Language, and Hearing Research, 50, 835–843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt R. F., Kirk K. I., Eisenberg L. S., Martinez A. S., Campbell W. (2005). Spoken word recognition development in children with residual hearing using cochlear implants and hearing aids in opposite ears. Ear and Hearing, 26, 82S–91S [DOI] [PubMed] [Google Scholar]
- Keilmann A. M., Bohnert A. M., Gosepath J., Mann W. J. (2009). Cochlear implant and hearing aid: A new approach to optimizing the fitting in this bimodal situation. European Archives of Otorhinolaryngology, 266, 1879–1884. 10.1007/s00405-009-0993-9 [DOI] [PubMed] [Google Scholar]
- Luntz M., Shpak T., Weiss H. (2005). Binaural-bimodal hearing: Concomitant use of a unilateral cochlear implant and a contralateral hearing aid. Acta Oto-Laryngologica, 125, 863–869 [DOI] [PubMed] [Google Scholar]
- Mok M., Grayden D., Dowell R. C., Lawrence D. (2006). Speech perception for adults who use hearing aids in conjunction with cochlear implants in opposite ears. Journal of Speech, Language, and Hearing Research, 49, 338–351 [DOI] [PubMed] [Google Scholar]
- Morera C., Manrique M., Ramos A., Garcia-Ibanez L., Cavalle L., Huarte A., Estrada E. (2005). Advantages of binaural hearing provided through bimodal stimulation via a cochlear implant and a conventoinal hearing aid: A 6-month comparative study. Acta Oto-Laryngologica, 125, 596–606 [DOI] [PubMed] [Google Scholar]
- NIH Consensus Development Program. (1995). Cochlear implants in adults and children. NIH Consens Statement Online, 13(2), 1–30 Retrieved from http://consensus.nih.gov/1995/1995CochlearImplants100html.htm [PubMed] [Google Scholar]
- Perreau A. E., Tyler R. S., Witt S., Dunn C. (2007). Selection strategies for binaural and monaural cochlear implantation. American Journal of Audiology, 16, 85–93 [DOI] [PubMed] [Google Scholar]
- Potts L. G., Skinner M. W., Litovsky R. A., Strube M. J., Kuk F. (2009). Recognition and localization of speech by adult cochlear implant recipients wearing a digital hearing aid in the nonimplanted ear (Bimodal hearing). Journal of the American Academy of Audiology, 20, 353–373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer E. C., Amlani A. M., Seibold A., Shattuck P. L. (2007). Meta-analytic comparison of binaural benefits between bilateral cochlear implants and bimodal stimulation. Journal of the American Academy of Audiology, 18, 760–776 [DOI] [PubMed] [Google Scholar]
- Strauss A., Corbin J. (1998). Basics of qualitative research: Techniques and procedures for developing grounded theory. Thousand Oakes, CA: Sage [Google Scholar]
- Syms C. A., Wickenberg J. (2002). Concurrent use of cochlear implants and hearing aids. In Kubo T., Takahashi Y., Iwaki T. (Eds.), Cochlear implants: An update (pp. 535–539). The Hague, Netherlands: Kubler [Google Scholar]
- Tyler R. S., Parkinson A. J., Wilson B. S., Witt S., Preece J. P., Noble W. (2002). Patients using a hearing aid and a cochlear implant: Speech perception and localization. Ear and Hearing, 23, 98–105 [DOI] [PubMed] [Google Scholar]
- Zhang T., Dorman M. F., Spahr A. (2010). Information from the voice fundamental frequency (F0) region accounts for the majority of the benefit when acoustic stimulation is added to electric stimulation. Ear and Hearing, 31, 63–69 [DOI] [PMC free article] [PubMed] [Google Scholar]