Abstract
Objectives:
This descriptive summary of the literature provides an overview of the available studies (published between January 1980 and January 2009) on correlates of help-seeking behavior for hearing loss, hearing-aid uptake, hearing-aid use, and satisfaction with the device.
Methods:
Publications were identified by structured searches in Pubmed and Cinahl and by inspecting the reference lists of relevant articles. The articles covered different stages that a person with hearing impairment may go through: prior to hearing aid fitting, the period covering the fitting and the period post hearing aid fitting. Inclusion of articles occurred according to strict inclusion and exclusion criteria. Data were extracted by two independent researchers. Thirty-nine papers were included that identified 31 factors examined in relation to the four outcome measures. These covered personal factors (e.g., source of motivation, expectation, attitude), demographic factors (e.g., age, gender) and external factors (e.g., cost, counseling). Only two studies covered the actual fitting process. There was only one factor positively affecting all four outcome variables. This was self-reported hearing disability. The vast majority of studies showed no relationship of age and gender with any of the outcome domains.
Discussion and conclusion:
Whereas research of the last 28 years yielded valuable information regarding relevant and irrelevant factors in hearing aid health care, there are still many relevant issues that have never been investigated in controlled studies. These are discussed.
Keywords: hearing aid, help seeking, uptake, use, satisfaction, review
Introduction
Despite the large prevalence of hearing impairment in human populations, the uptake of hearing aids is still poor. A relatively small proportion of adults with hearing impairment seek help for their hearing problems and use hearing aids. Several studies have shown that a large proportion of people who could benefit from hearing aids do not have them (Popelka et al., 1998; Smeeth et al., 2002; Smits et al., 2006). In addition, not all adults provided with hearing aids use them, wear them regularly, or are satisfied with them. Surveys conducted in the United Kingdom, Australia, Finland, Denmark, and the United States revealed that between 1% and 40% of hearing aids dispensed are never or rarely used (Dillon et al., 1999; Hickson and Worrall, 2003; Lupsakko, Kautiainen, & Sulkava, 2005; Smeeth et al., 2002).
It is widely assumed that the sequence of (psychological) events (the “journey”) experienced by the hearing impaired person in his or her process of seeking and obtaining help has a large impact on the individual's decision to acquire a hearing aid, use it, and become satisfied with it. The way people are guided along their journey may vary widely. Some may have received support from hearing care professionals by means of individual or group counseling, whereas others may have independently searched for information about hearing health care, for example consulting others with hearing aids. It is also known that people may abandon the rehabilitation process (Gianopoulos & Stephens, 2005; Schumacher & Carruth, 1997), but not much knowledge is yet available about where in their journey the potential hearing-aid users are lost and why.
The initial aim of the present study was to perform a systematic review of the evidence regarding the impact that different patient journeys have on people becoming satisfied hearing aid users. However, a search of the literature revealed that no data-based studies strictly focusing on the patient journey exist. It is not known how different pathways may affect a person's decisions to seek help and obtain a hearing aid. Whereas ideal journeys and rehabilitation pathways are defined in the literature and prescribed in guidelines or discussed in research papers (Goldstein & Stephens, 1981; Gianopoulos & Stephens, 2005, Gussekloo et al., 2003; Kapteyn et al., 1997; Kiessling et al., 2003; Stephens, 1989; Stephens et al., 1990), there are no studies providing evidence regarding their impact.
To our knowledge, only three peer-reviewed scientific articles in the field of Audiology have explicitly addressed and investigated the patient's pathway toward seeking help and obtaining hearing aids (Grutters et al., 2007, 2008; Smith et al., 2008). Grutters et al. (2007, 2008) did not provide experimental data on how the journey affects patients' decisions to pursue amplification. For example, Grutters et al. (2007) evaluated the attitudes of professionals (General Practitioner [GP], hearing aid dispenser, ENT specialist, and clinical audiologist) and patients toward a direct referral pathway for hearing aid fitting (dispenser) as opposed to an alternative route (via the GP and ENT specialist and clinical audiologist). The hearing-impaired persons, the GP's, and the hearing aid dispensers generally had positive attitudes toward the direct pathway, whereas the ENT doctors and the clinical audiologists had negative concerns about the direct referral. In an additional study, Grutters et al. (2008) evaluated patients' preferences. However, it was not examined how the different pathways affected hearing aid uptake or success with the fitted hearing aid. Smith et al. (2008) examined the efficiency of an assess-and-fit pathway and compared it to traditional patient pathways in the United Kingdom. The assess-and-fit model included an open-fit hearing aid fitting following an ENT visit on the same day. The authors found that such a pathway reduced patients' time in visits to the clinic as well as staff time and concluded that the assess-and-fit pathway was efficient seen from a service perspective. It was recommended to apply the assess-and-fit model to patients having mild to moderate hearing losses (who might be concerned about the appearance of the aids) and good manual dexterity. Again, it was not examined how the alternative pathway affected hearing aid rehabilitation outcome variables.
Thinking in terms of a journey related to amplification, one can discern a few crucial junctures. The first is the decision to seek help (help seeking). The next step is the decision to acquire a hearing aid (uptake). The third is a patient's decision to continue to use an acquired hearing aid, and finally, there is the issue of satisfaction with the hearing aid. These four variables (i.e., help seeking, hearing aid uptake, hearing aid use, and satisfaction) may be considered as key elements in a journey.
Because of the lack of empirical data on the impact of a patient's entire journeys on success with hearing aid fitting, we decided to review the literature by focusing on each of those crucial steps in the journey separately (i.e., help seeking, uptake, use, satisfaction), so as to learn more about which factors are known to be evidently important at what stage in the process of getting a hearing aid. The vast majority of existing data-based studies identifying factors that may influence an individual's decision to seek help, acquire a hearing aid, and become satisfied with it, focus on a restricted part of the journey, or just present a pre- and postmeasure (e.g., pre- and postfitting), rather than specifying the whole sequence of events within a certain time frame. The main body of literature divides the patient journey into three stages:
The stage prior to help seeking and uptake of hearing aids;
The period covering the process of the fitting; and
The short- or long-term period after the hearing aid fitting.
Studies focusing on parts of the journey do provide useful information about factors contributing to an individual's decision to seek help, pursue, and use amplification. Thus, summarizing the research addressing these four variables (i.e., help seeking, uptake, use, and satisfaction) in different stages may help us to learn more about the journey of a person with hearing impairment. It may also identify what is known about factors influencing the stages and help us to evaluate the strength of any evidence.
Hence, the aim of this study was to provide a review of the existing literature to identify factors that have been shown to significantly affect help seeking, uptake, use, and satisfaction with hearing aids in different stages of the client's journey. The review will cover the literature published between January 1980 and January 2009 inclusive.
Method
The search of literature was divided into several steps. First we decided to restrict the scope of this review by applying certain criteria. We then developed a search strategy. The steps are described in more detail in the following paragraphs.
Inclusion and Exclusion Criteria
Studies were selected for analysis in the review process if they met the following criteria:
The study included adults.
The outcome measure was clearly focused on (some aspects of) help seeking, hearing aid uptake, hearing aid use, or satisfaction with hearing aid(s) and the items and response categories were clearly described.
The study was published in the period from January 1980 to January 2009.
The study was published in a peer-reviewed scientific journal.
The evidence described in the article was based on empirical data. Qualitative studies were not included.
The statistical method to analyze the data was clearly described in the article.
To provide the reader with information about the study design, we decided to use the classification as proposed by Cox (2005):
A randomized controlled trial (RCT).
A nonrandomized intervention study (NRIS; a controlled study, but groups not randomized, but matched).
Nonintervention descriptive designs (NIDD; examples are a cohort study, a cross-sectional survey).
It must be mentioned that many studies focusing on a part of the patient journey used outcome measures reflecting quality of life or well-being to evaluate an intervention (e.g., a communication course to be followed after the hearing aid fitting). As these outcomes are not the variables of interest in the present review, we excluded those papers. Studies dealing with technological features of hearing aids or technical devices other than conventional hearing aids (e.g., bone-anchored hearing aids, cochlear implants, assistive listening devices) were also excluded. In addition, whenever hearing aid satisfaction was expressed as benefit assessed with objective measures (e.g., speech performance tests) or with self-report tools, such as the Profile of Hearing Aid Benefit (PHAB; Cox et al., 1991) or the Hearing Handicap Inventory for the Elderly (HHIE; Ventry & Weinstein, 1982), we excluded these papers from the review. Hearing aid benefit refers to a relative change in performance on a particular measure between aided and unaided listening conditions. Studies aiming to demonstrate the benefit of hearing aids generally show at best a weak relationship between benefit and satisfaction (Souza et al., 2000; Wong et al., 2003, 2004).
Search Strategy
We searched for relevant articles in two major electronic databases: Pubmed and CINAHL. These databases are the most relevant and cover most of the audiological journals (Cox, 2005). The search string was developed with the following search terms and Booleans:
(hearing aid∗ OR amplification∗ OR audiological rehabilitation∗ OR aural rehab∗ OR auditory rehab∗) AND (nonuse∗ OR prefitting∗ OR fitting∗ OR postfitting∗ OR ongoing care∗ OR refusal∗ OR long term care∗ OR adherent∗ OR nonadherent∗ OR referral∗) AND (help seeking∗ OR uptake∗ OR use∗ OR utilization∗ OR utilization∗ OR satisfaction∗ OR rejection∗ OR benefit∗) NOT (signal process∗ OR feedback∗ OR cochlear implant∗ OR CI OR fine tuning∗ OR child∗).
The ∗ denotes truncation and allows for different endings of a word.
In a second step, an additional search was carried out by scrutinizing the reference lists (reference checking) of the articles extracted in the first step. Also reference lists in textbooks were examined.
Selection Procedure
The abstracts of all articles retrieved in the two previous steps were reviewed by two investigators independently with regard to the inclusion criteria. When there was no consensus on the basis of the abstract, the full text article was retrieved and reviewed. A third reviewer was consulted when the two investigators could not reach consensus on whether to include a paper or not. Included articles were then inspected closely to extract data on relevant outcomes. A standardized form was used to summarize the information in each article. Variables extracted were aim of the study (main outcome), determinants, outcome measures used, study design, information about hearing aids, number of participants, and age.
Outcome Measures and Factors
As mentioned, this review focuses on four outcome variables: help-seeking, hearing-aid uptake (or rejection), use, and satisfaction. Hearing-aid uptake is different from help seeking in that the latter does not automatically imply that people also pursue amplification. We therefore included both variables. Most of the studies examining help-seeking and hearing-aid uptake just counted the number (or calculated the proportion) of people opting for these actions. All studies included used self-report outcome measures to assess use and satisfaction. Well-known and frequently used instruments are the Satisfaction with Amplification in Daily Life (SADL; Cox & Alexander, 1999), the Glasgow Hearing Aid Benefit Profile (GHABP; Gatehouse, 1997) and the International Outcome Inventory for Hearing Aids (IOI-HA; Cox et al., 2000). Thus most results collected and summarized in this article are based on self-report. Note that we only included measures of self-report when both the literal item(s) and the response categories, including the coding, were provided. We use the term “factors” for variables that were examined in the studies. Here, we adopt the terminology of the original articles verbatim.
Nature of the Review
Whereas we initially aimed to systematically review the literature using a quantitative approach, the large heterogeneity of the methods used in the studies in this review (i.e., heterogeneity regarding type and quality of outcome measures and study design) do not allow such an analysis. Randomized controlled trials using similar outcome measures among comparable samples of participants are required for such purposes. Hence, we proceeded to review the literature in a qualitative way, which means that we summarized the results of the studies, rather than statistically combining them (see also Cook et al., 1997).
Presentation of Data
Rather than repeating a description of which outcome measures or study design was used each time we present a given study, we created a table providing this information in the appendix and refer to this throughout the article. In addition, when four or more articles were available reporting on the same factor, we provide small tables after each paragraph to provide the reader with a quick overview of the results. Here we use signs to denote the results. Note that the majority of studies used regression models to determine associations between variables, calculated correlation coefficients, or performed analyses of variance to determine differences between group means. So, a “+” sign indicates a positive correlation between the factor and the outcome variable, or it indicates that a group mean (outcome variable) was significantly greater than the compared (control) group mean. A “-” sign indicates a negative correlation between the factor and the outcome variable, or it indicates that a group mean (of the outcome variable) was significantly smaller than the compared (control) group mean. A “0” sign means that there was no correlation or that group means were not significantly different between test and control groups.
Results
The search in Pubmed yielded 324 hits. Only 18 of those studies fulfilled the inclusion criteria as described above and could be included. Hence, 306 articles were excluded. The search in Cinahl gave 52 hits. Only three of those studies fulfilled the inclusion criteria although they had all been yielded by the Pubmed search. Inspection of the reference lists of relevant articles yielded a total of 21 additional articles fulfilling the inclusion criteria.
In total, 39 articles met the inclusion criteria and were included.
Studies Across Three Stages
As mentioned in the introduction, the main body of literature divides the patient journey into three stages: prefitting, fitting, and postfitting. The review yielded 22 studies focusing on the prefitting period. The following factors were addressed in these studies: source of motivation, attitudes towards hearing aids, attitudes to hearing loss (also dealing with acceptance of hearing loss), expectations, personality, self-reported hearing (activity limitation, participation restriction), dexterity, health, hearing sensitivity, age, age at onset of hearing loss, duration of hearing loss, gender, educational level, socioeconomic status, living relations, matrimonial status, amount of social interaction, cost, type of clinic (private vs. public), general health attitude, speech reading, and prefitting counseling.
Only two studies were found dealing with factors potentially playing a role within the actual hearing aid fitting stage. Factors addressed were fitting counseling, first impression of hearing aids (assessed by audiologist), dexterity/handling of the hearing aids during the fitting, and satisfaction with hearing aid professional/audiologist.
In all, 17 studies were concerned with the period following hearing aid fitting up to approximately 1 year. Factors that were subject of study in these articles were, time or longitudinal change, lifetime hearing aid experience, personality, self-reported hearing (activity limitation, participation restriction), attitude toward own hearing loss, activity of daily living (ADL), hearing sensitivity, age, gender, socioeconomic status, living relations, medication, major life events, cosmetic appearance of the hearing aids, postfitting counseling, and the hearing aid professional.
There were two studies covering more than one of the abovementioned three stages; hence the sum of the numbers of studies dealing with each stage is 41, rather than the total number (39) of studies included in the review.
Details about outcome measures and other features are presented in the appendix.
Each of the factors will be described separately in each of the following paragraphs. The results are arranged in tabular form, only if at least four studies were available. A list of factors that were covered in only one study is provided in the end.
Source of Motivation
The search yielded a total of four studies dealing with source of motivation of the hearing impaired client entering the hearing clinic. All of these focused on whether the hearing aid candidates were self-motivated or motivated by others (e.g., spouse, family) to seek help or whether the source of motivation had an effect on hearing aid use and satisfaction.
Duijvestijn et al. (2003) investigated a group of people (>55 years old) who had taken part in a hearing screening program and looked at differences between those who had sought help for their hearing problems from their GP and those with the same level of hearing loss who had not. It was found that those seeking help had experienced more social pressure by significant others than those not seeking help.
A study by Hickson et al. (1986) among 135 persons fitted with hearing aids revealed that there was no difference in hearing aid use between self-motivated hearing aid candidates and candidates motivated by others to seek help. A similar finding was reported in Hickson et al. (1999). Also Wilson and Stephens (2003) found that hearing aid use was not affected by prefitting motivation (self-motivated or other).
Wilson and Stephens (2003) did not find an association between source of motivation and hearing aid satisfaction. However, Hickson et al. (1999) observed a significant relation between the source of motivation (self vs. other) for attending a hearing clinic and the satisfaction with hearing aids (measured several months postfitting). This study demonstrated that self-motivated persons were more satisfied than those motivated by others.
To sum up, the studies on source of motivation demonstrate a positive association between help seeking and motivation by others (as opposed to self-motivated; see Table 1). It seems that motivation (self or other) does not affect use. There are mixed findings regarding the association between prefitting motivation (self vs. other) and satisfaction with hearing aids. However, the number of studies on each outcome measure is small. Data on the influence of prefitting source of motivation on the uptake/rejection of hearing aids are lacking. Note that studies addressing an individual's degree or amount of self-motivation and its association with any of the four outcome variables were not encountered.
Table 1.
Summary of the Results of Studies of the Relationship Between Source of Motivation and the Outcome Variables
| Outcome variable | Number of studies | Result |
|---|---|---|
| Help seeking | 1 | by others + |
| Uptake | 0 (No data) | |
| Use | 3a | 0 0 0 |
| Satisfaction | 2a | 0 by self + |
Note: “+” indicates a positive association between the factor and the outcome, “0” no association.
Some studies had both use and satisfaction as outcome measures, therefore the number of studies sums up to more than four.
Attitude Toward Hearing Aids
In all, eight studies investigated the influence of attitude toward hearing aids on one or more of the variables of interest in this study. All eight focused on the attitude toward hearing aids in the period prior to hearing aid fitting. Note that the attitude toward one's own hearing loss is described in the next paragraph.
Duijvestijn et al. (2003) did not find a difference between those seeking help and those not seeking help for their hearing loss in the scores on questions concerning hearing aid image (e.g., do you think there are disadvantages in wearing a hearing aid?).
When looking at uptake, van den Brink, Wit, Kempen, and van Heuvelen (1996) reported that those people who consulted for help but ended up not acquiring hearing aids (rejection/uptake) had less favorable attitudes toward hearing aids than those acquiring hearing aids.
Hickson et al. (1986, 1999) classified clients' attitude into one of four different attitude types as described by Goldstein and Stephens (1981),1 based on the initial interview in the clinic. Hearing aid use of these clients was measured 3 to 9 months postfitting. The results in both studies showed that type III attitude (fundamentally negative against [instrumental] help) was associated with occasional or nonuse of hearing aids, whereas the remaining groups (type I “strongly positive toward help” and type II “essentially positive”) showed consistent use. (Clients with the type IV attitude “rejection of hearing aids and the entire rehabilitation process” were not fitted with hearing aids and were not included in this analysis). The later study (Hickson et al., 1999) did not reveal differences in satisfaction between type I, II, and III attitude.
Wilson and Stephens (2003) reported significantly more frequent use of hearing aids as well as higher satisfaction levels among those with a positive (prefitting) attitude toward hearing aid rehabilitation compared to those with negative attitudes.
Comparable findings were reported by Gatehouse (1994), who observed significant positive correlations between attitude toward HA (as measured with the Initial Disability Interview (IDI; Gatehouse, 1993) and hearing aid use and satisfaction. Another study looking at the relationship between a person's attitude toward hearing aids and later use and satisfaction was made by Brooks and Hallam (1998). They administered the Hearing Attitudes in Rehabilitation Questionnaire (HARQ; Hallam & Brooks, 1996) prior to the patient's visit and observed that stigma toward hearing aids was not predictive of later hearing aid use or satisfaction. The authors suggested that their prefitting counseling to these patients could probably have influenced these findings.
Jerram and Purdy (2001) failed to find significant correlations between the attitude toward hearing aids prior to hearing aid fitting and hearing aid use and satisfaction when measured 10 weeks after hearing aid fitting.
In summary, there seems to exist no clear evidence of the impact of attitude toward hearing aids (see Table 2). The majority of studies addressing the effect on hearing aid use demonstrated a significant positive relationship or a significant difference between groups (i.e., higher use among those with positive attitude). Whereas evidence for help seeking, uptake, and satisfaction is less clear, the available studies demonstrate either no effect/relationship or a positive association. There is no study demonstrating a negative relationship. It is clear that no conclusions can be drawn for help seeking and hearing aid uptake due to the fact that there is only one study for each of these outcomes. It may be relevant to mention here that people with negative attitudes toward hearing aids may be less likely to make the step to the initial consultation and thus may not be reached by a survey like the ones carried out by Brooks and Hallam (1998). The attitudes of hearing impaired people who have not yet been in touch with the hearing health care system are difficult to study although the study by Duijvestijn et al. (2003) achieved this by recruiting people who participated in a driving test and found that the willingness to use hearing aids was much more prevalent among the respondents who ended up seeking help for hearing loss compared to the nonconsulters.
Table 2.
Summary of the Results of Studies of the Relationship Between Prefitting Attitudes Toward Hearing Aids and the Outcome Variables
| Outcome variable | Number of studies | Result |
|---|---|---|
| Help seeking | 1 | 0 |
| Uptake | 1 | + |
| Use | 6a | 0 0 + + + + |
| Satisfaction | 5a | 0 0 0 + + |
Note: “+” indicates a positive association between the factor and the outcome, “-” a negative association, “0” no association.
Some studies had both use and satisfaction as outcome measures, therefore the number of studies sums up to more than eight.
Own Attitudes Toward Hearing Loss, Including Acceptance of and Coping With Hearing Loss
An individual's attitude toward his or her own hearing loss (including coping behavior) and its effect on any of the four outcome variables has been examined in seven studies.
Cox et al. (2005) investigated the influence of an individual's overall coping style (not related to hearing) on help seeking. Hearing aid seekers reported using less coping strategies than their non-hearing peers.
Garstecki and Erler (1998) found significantly higher uptake among males who accepted their hearing loss and found hearing loss less stigmatizing than among males who did not accept their hearing loss and found it stigmatizing. Helvik et al. 2008 found that the use of maladaptive behaviors was related to the decrease of hearing aid uptake.
Humes et al. (2003) examined the differences between groups of successful and unsuccessful hearing aid candidates matched for age, gender, and hearing loss. Three groups were compared: (a) nonadherents, (b) adherents who subsequently rejected their hearing aid, and (c) adherents accepting and using their hearing aid. The results obtained with the Communication Profile for the Hearing Impaired (CPHI; Demorest & Erdman, 1987) demonstrated that the nonadherent group (uptake) in that study had poorer problem awareness and greater denial of communication problems. The nonadherents had also better self-acceptance and less stress associated with their hearing problems.
Brooks (1989) investigated the use of hearing aids 4 months postfitting in relation to four questions regarding the participants' attitude to their hearing loss. For each of the four questions, it was found that a higher degree of acceptance of own hearing problems prior to hearing aid fitting was related to a higher amount of hours of hearing aid use per day when measured 4 months postfitting.
Jerram and Purdy (2001) observed that those with better acceptance of their hearing loss prior to hearing aid fitting used their hearing aids more frequently than those with less acceptance of their hearing loss. They found no relation between acceptance of hearing loss prior to fitting and hearing aid satisfaction. Brooks and Hallam (1998) found that people who were least distressed by their hearing loss and also reported that they neither wanted nor needed a hearing aid were also those with the lowest hearing aid use when measured after fitting.
Acceptance of hearing loss prior to hearing aid fitting has thus been shown to positively influence both hearing aid uptake and hearing aid use. A summary is presented in Table 3. Some other aspects related to acceptance of hearing loss have been mentioned separately in the table. The number of studies is still small.
Table 3.
Summary of the Results of Studies of the Relationship Between Prefitting Attitude Toward Own Hearing Loss and the Outcome Variables
| Outcome variable | Number of studies | Result |
|---|---|---|
| Help seeking | 1 | Coping style − |
| Uptake | 3 | Acceptance of hearing loss + Distress + Problem awareness + Denial of problems − Self-acceptance − Maladaptive behavior − |
| Use | 3 | Attitude measures (Brooks 1989) + Distress + Acceptance of hearing loss + |
| Satisfaction | 1 | Acceptance of hearing loss 0 |
Note: “+” indicates a positive association between the factor and the outcome, “-” a negative association.
Expectations
The search yielded six studies investigating the relationship between prefitting expectations of hearing aids and hearing aid uptake, use, and satisfaction. Studies looking at prefitting expectations in relation to help seeking were not found.
Prefitting expectations did not distinguish adherents from nonadherents (uptake) in Humes et al. (2003).
Although Gatehouse (1994) did not find any relation between prefitting expectations and hearing aid use, he did observe a positive association between prefitting expectations and hearing aid satisfaction. Contradicting these findings, Jerram and Purdy (2001) failed to observe a significant association between expectations and satisfaction at 10 weeks postfitting but found a positive relationship between expectations and hearing aid use.
The Expected Consequences of Hearing Aid Ownership (ECHO) questionnaire was used by Cox and Alexander (2000) to measure expectations toward hearing aids. One of the four subscales (Positive Effect) appeared to correlate positively with satisfaction (as measured with the SADL). This finding was confirmed in a later study (Cox et al., 2007) in which expectations explained a significant proportion of variance in overall satisfaction (as measured 6 months postfitting). Prefitting expectations did not predict hearing aid use.
Wong et al. (2004) (measuring pre-fitting expectations and general satisfaction with hearing aids 3 months post fitting) were not able to demonstrate any significant correlations.
The findings concerning prefitting expectations are summarized in Table 4. Whenever significant, the associations between expectations and use or satisfaction were positive, indicating that the higher the expectations, the higher the use and satisfaction. No study reported negative correlations. Note that the studies in this section all used different tools to measure expectations and to evaluate use and satisfaction (see appendix).
Table 4.
Summary of the Results of Studies of the Relationship Between Prefitting Expectations and the Outcome Variables
| Outcome variable | Number of studies | Result |
|---|---|---|
| Help seeking | No data | |
| Uptake | 1 | 0 |
| Use | 3a | + 0 0 |
| Satisfaction | 5a | + + + 0 0 |
Note: “+” indicates a positive association between the factor and the outcome, “0” no association.
Some studies had both use and satisfaction as outcome measures, therefore the number of studies sums up to more than five.
Also, as pointed out by Wong et al. (2003), there is some variation in the studies reporting on prefitting expectations regarding the length of time between the hearing aid fitting and the outcome measurement.
Various other studies have suggested that prefitting expectations may be greatly dependent on an individual's personality (Cox et. al., 2005; Gatehouse, 1990; Saunders & Cienkowski, 1996). The following section is concerned with the relations between personality and the variables of interest in this study.
Personality
The literature search yielded six articles reporting on personality as a possible predictor of help seeking, hearing aid uptake, use, and/or satisfaction.
The research question in Cox et al. (2005) was whether older adults who chose to pursue amplification were different from general population norms in terms of their personality trait levels or sense of personal control. The results revealed that even though hearing aid seekers (help seeking) were not strikingly different from the general adult population, they displayed significantly lower Neuroticism scores and significantly lower scores on Openness (as measured with the NEO-Five-Factor Inventory (NEO-FFI; Costa & McCrae, 1997). Also, hearing aid seekers tended to be more pragmatic and routine oriented than the typical adult in the general population and they had a significantly higher internal locus of control.
In a follow-up study investigating use and satisfaction with hearing aids 6 months postfitting (among a variety of other variables), use was not related to any personality trait (Cox et al., 2007). Of the measures of satisfaction in that study, the Personal Image subscale of the SADL was found to be related to four of the five personality traits (Neuroticism, Extraversion, Agreeableness, Consciousness). However, personality traits did not figure independently in the regression equations predicting success of amplification (use and satisfaction).
Garstecki and Erler (1998) measured the personality factors of potential hearing aid users with adult-onset hearing loss and compared those acquiring hearing aids (uptake) with those not acquiring hearing aids (nonadherents). The sample was stratified by gender, resulting in four groups (female adherents, female nonadherents, male adherents, male nonadherents). Individuals who felt greatest responsibility for communication problems were more likely to become adherents, regardless of gender. Among the females, locus of control and ego strength appeared to be critical variables as female adherents demonstrated higher internal locus of control and higher ego strength than female nonadherents.
Gatehouse (1994) found that some aspects of personality (when measured at the initial appointment) had a significant relation to hearing aid use and satisfaction, as those with lower depression scores (according to the Crown-Crisp Experiential Index; Crown & Crisp, 1979) also scored higher on postfit hearing aid use and satisfaction levels. Those with higher hysteria scores scored higher on post-fit hearing aid use and satisfaction levels. Whereas those with higher scores on obsession had higher scores on satisfaction. In the study by Kricos et al. (2007) optimism, as assessed by the Life Orientation Test (LOT), did not influence hearing aid use.
The results described in this paragraph do not lend themselves for a summarizing table, as each of the studies focused on different aspects of personality. Personality is an umbrella term covering many different terms, and each of the studies focused on a different aspect or aspects of personality. Apparently, audiological research in this area is still at a stage of discovering which personality traits may play a role in help seeking, uptake, use, and satisfaction.
Counseling
Our literature search revealed eight studies reporting on the effects of counseling programs on hearing aid use and satisfaction. The studies varied both with regard to the type of counseling programs offered as well as with regard to the tools used to assess outcomes. Some studies described the effects of programs offered prior to hearing aid fitting. Others looked at the effect of counseling offered along with or post hearing aid fitting.
The prefitting counseling by Norman and colleagues (1994), covering a discussion about one's personal hearing problems and the provision of general information about hearing loss and hearing aids, appeared to have no effect on hearing aid use and satisfaction in a controlled study.
Kemker and Holmes (2004) conducted a randomized controlled trial (RCT) in the United States with two experimental groups receiving counseling and a control group (receiving no counseling). The experimental groups received the same two 1-hr sessions; however, the timing of the intervention differed. One group completed the two sessions at least a week prior to hearing aid fitting, whereas the other group attended one session prior to fitting and one session postfitting. The intervention included communication skills training, hearing aid orientation, and a package with written material. Prefitting counseling resulted in significantly higher levels of satisfaction 5 weeks after fitting among those with greater initial disability (Glasgow Hearing Aid Benefit Profile; GHABP Item 1) when compared to the controls.
Another experimental study was carried out in the Netherlands by Kapteyn et al. (1997), who designed a referral pathway and a fitting program that included structured exchange of information between the GP and the ENT specialist to improve the streamlining between these professionals. The fitting program also included a controlled 4-week trial period as well as a home visit by a trained volunteer. The proportion (in)effective use of the hearing aid in six different listening situations was adopted as the outcome. It was found that especially the home visits had a beneficial influence on hearing aid use. Those receiving home visits showed significantly less ineffective use (27%) compared to those not receiving home visits (37%).
An RCT was carried out in Sweden by Öberg et al. (2008) on prefitting programs with sound-awareness training. The prefitting program did not lead to significant differences between the test group and the control group with regard to hours of hearing aid use or satisfaction, when measured 1 year after fitting. The sound-awareness training consisted of three visits including different listening exercises.
Eriksson-Mangold et al. (1990) reported on a fitting program that included clinic visits before and after issue of hearing aids. This so-called active fitting (AF) program covered five visits at a Hearing Centre, a more structured guidance of the patient compared to the usual practice, tasks to be carried out by the client between appointments, and gradually increasing hearing aid use during the 1st month of training (starting up with 2 hr per day). This study used a randomized controlled design. Those participating in the AF program were compared 10 months postfitting to a control group receiving “care as usual.” Among the various findings, the results demonstrated a significantly higher use of the hearing aids in the experimental group compared to the control group. Also, the experimental group had more positive opinions (satisfaction) about wearing hearing aids and experienced greater satisfaction with sound quality.
Cherry and Rubinstein (1994) investigated the effectiveness of a postfitting telephone counseling program in an RCT. The participants in the experimental group (N = 30, >50 years) were contacted at 6, 9, and 12 weeks after the fitting to address questions and to encourage them to return to the clinic to resolve any hearing-aid-related problems. The control group did not receive the telephone intervention. Whereas a significant reduction in perceived participation restriction was observed 16 weeks postfitting, there was no effect of the intervention on hearing aid use and satisfaction.
The intervention program in a study by Norman et al. (1995) comprised a communication course (three 2-hr sessions at weekly intervals) including hearing tactics, role play exercise, and leaflets with information. Hearing aid use and satisfaction were evaluated 4 months after fitting in the study group and were compared to the scores in a control group. No significant difference in use time between the study group and the control group was observed. However, it was found that the study group was significantly more satisfied with their hearing aids than the control group.
Brickley et al. (1996) studied the differences between individual follow-up and group follow-up sessions for first time hearing aid users with regard to hearing aid use and satisfaction. The groups were matched for age, gender, and hearing loss. There was no significant difference between the groups regarding hours of use or satisfaction, despite a significant difference in perceived performance of the hearing aid (the follow-up group showing higher perceived performance).
Altogether, we may conclude that effect of counseling on hearing aid use and satisfaction is still uncertain (see Table 5). Whereas short-term effects may appear significant (e.g., Kemker & Holmes, 2004), it seems to be important to also evaluate whether these effects remain stable in the long term (e.g., Öberg et al., 2008). Comparable conclusions were drawn by others (e.g., Hickson (1999) and Öberg et al. (2008). It must be noted that many more studies on the effects of counseling either along with or following amplification have been performed. However, most of these used measures of quality of life or communication as outcomes and, hence, are not included in this review.
Table 5.
Summary of the Results of Studies of the Relationship Between Counseling and the Outcome Variables
| Outcome variable | Number of studies | Result |
|---|---|---|
| Help seeking | No data | |
| Uptake | No data | |
| Use | 7a | 0 0 0 0 0 ++ |
| Satisfaction | 7a | 0 0 0 0 + + + |
Note: “+” indicates a positive association between the factor and the outcome, “0” no association.
Some studies had both use and satisfaction as outcome measures, so the number of studies in the table does not sum up to eight.
Self-Reported Hearing Problems (Activity Limitation, Participation Restriction)
Self-perceived hearing-related activity limitation and/or participation restriction in the period prior to hearing aid fitting have been the subject of 11 studies included in our review.
Swan and Gatehouse (1990) examined the differences between consulters for hearing aids (help seekers) and nonconsulters by using a Hearing Questionnaire. A highly significant difference between the reported participation restriction of consulters and nonconsulters was found in all analyses, controlling for hearing sensitivity. In addition, consulters had greater self-assessed disability than nonconsulters when controlled for their hearing impairment. van den Brink et al. (1996) compared three groups—nonconsulters (Group A), consulters who ended up not acquiring hearing aids (Group B), hearing aid users (Group C)—and found that all consulters (Groups B and C) had higher degrees of self-reported hearing loss compared with nonconsulters, thereby indicating that those reporting more hearing problems (subjective hearing loss) were more likely to seek help (help seeking) for hearing impairment. Similarly, a study by Duijvestijn et al. (2003) showed that a significant predictor of help seeking for hearing impairment was the reporting of poor or bad hearing combined with being bothered by hearing problems on an ordinary daily basis.
The study of Humes et al. (2003) also compared three groups (A. nonadherents B. adherents who subsequently rejected their hearing aid C. adherents accepting their hearing aid). The nonadherent group (Group A) differed from one or both of the other groups in that the nonadherents had significantly lower scores on the HHIE (lower self-perceived participation restriction) than the groups who purchased hearing aids (B) and (C). This study thus showed that a low degree of subjective hearing loss is likely to lead to low hearing aid uptake. Note that the adherents in Humes et al. (2003) also comprised people who rejected their hearing aids later in the trial period. Gussekloo et al. (2003) used the HHDI (The Hearing Handicap and Disability Inventory (van den Brink, 1995) to assess self-reported hearing disability among those elderly (85+ years) in a population-based study who chose to participate in a hearing aid rehabilitation program (hearing aid uptake) and those who rejected. It was found that the median hearing disability rate was higher among those who chose to accept hearing aid rehabilitation compared to those who did not.
Recently, Helvik and colleagues (2008) compared hearing aid candidates who accepted and who rejected hearing aids 1.5 years after issue. Higher levels of activity limitation and participation restrictions were associated with lower odds of rejecting a hearing aid (i.e., increased the odds for uptake). In Cox et al. (2007), a significant proportion of variance in the equations to predict use and overall satisfaction was explained by unaided hearing activity limitation measured prefitting, such that higher levels of self-perceived difficulties were associated with higher use and higher satisfaction.
The search revealed four studies investigating the influence of self-reported hearing loss during the postfitting period. Takahashi et al. (2007) investigated hearing aid use and satisfaction at 6 years postfitting and compared subjective unaided hearing difficulties with satisfaction as measured with the IOI-HA questionnaire. Here, significant positive correlations between subjective hearing difficulties and hearing aid use and satisfaction were found; the greater the self-perceived hearing difficulties, the more use and satisfaction was reported. A positive relationship between perceived hearing difficulties without a hearing aid and satisfaction with hearing aids was also reported by Uriarte et al. (2005) as well as by Mulrow et al. 1992. Finally, Hosford-Dunn and Halpern (2001) reported a positive correlation between self-perceived hearing difficulties and hearing aid use and satisfaction. In addition, they examined the impact of one's hearing loss on others and concluded that those who evaluated their hearing loss having more impact on others were more satisfied with their hearing aids than those reporting their hearing loss having less impact on others.
Thus it can be concluded that the user's perception of their own hearing difficulties does affect help seeking, hearing aid uptake, hearing aid use, and satisfaction. This is clearly demonstrated in Table 6.
Table 6.
Summary of the Results of Studies of the Relationship Between Self-Reported Hearing Problems (and/or Activity Limitation, Participation Restriction) and the Outcome Variables
| Outcome variable | Number of studies | Result |
|---|---|---|
| Help seeking | 3a | + + + |
| Uptake | 3a | + + + |
| Use | 3a | + + + |
| Satisfaction | 5a | + + + + + |
Note: “+” indicates a positive association between the factor and the outcome.
Two of these studies had several relevant outcome measures, therefore the number of studies sums up to more than 11.
Hearing Sensitivity
Hearing sensitivity (i.e., hearing threshold level) has been investigated in relation to its influence on help seeking, hearing aid uptake, use, and overall satisfaction with the device in 15 studies.
Humphrey et al. (1981) compared four groups of participants: A. Hearing impaired persons not accepting having a hearing loss, B. Hearing impaired persons who admitted having a hearing loss but did not consult their GP, C. Persons who consulted their GP about their hearing but did not acquire hearing aids, and D. Persons who acquired hearing aids. They found that the help seekers (Groups C and D) were those with the highest degrees of pure tone hearing loss (1, 2, and 4 kHz average of 56 dB and 69 dB respectively) compared to the remaining groups (44 dB in A and 52 dB in Group B). Similar findings were reported by van den Brink et al. (1996). Swan and Gatehouse (1990) found that the worse-ear hearing of consulters was worse by 6 dB compared to nonconsulters. They also observed that people with an asymmetrical hearing loss were more likely to consult (seek help) for hearing problems than those with a symmetrical loss. In constrast, in Duijvestijn et al. (2003) pure tone hearing loss was not a significant predictor of help seeking (the four-frequency average threshold for help seekers and nonhelp seekers was 39.1 dB and 37.1 dB respectively).
Gussekloo et al. (2003) reported an effect of hearing sensitivity on uptake. Older adults who accepted the offer to receive aural rehabilitation (i.e., hearing aid fitting, uptake) had a significantly higher degree of hearing loss (60 dB median at 1, 2, 4 kHz) than those who declined it (48 dB). The results of Garstecki and Erler (1998) demonstrated that female adherents (uptake) had significantly poorer pure-tone air conduction thresholds (four-frequency hearing thresholds around 42.5 dB) than female nonadherents (33.2 dB). The better-ear four-frequency average threshold contributed most to the variability in adherence (females). Helvik et al. (2008) reported similar results. In the analyses adjusting for confounders, the 4-frequency average hearing loss in the better ear was positively associated with the likelihood to pursue amplification (uptake).
Gatehouse (1994) observed a significant positive relationship between hearing loss and hearing aid use but not on hearing aid satisfaction in a stepwise regression analysis. The mean hearing loss in the sample was 48 dB HL (SD 13).
In Brooks and Hallam (1998) and Jerram and Purdy (2001; each with an average four-frequency hearing loss around 52 dB HL) hearing sensitivity did not contribute significantly in regression models predicting hearing aid use and satisfaction. Hickson et al. (1986) found no relation between hearing sensitivity (average 0.5, 1, 2 kHz <55 dB HL) and hearing aid use. Hickson et al. (1999) concluded that neither the type nor the severity of hearing loss were variables differentiating between groups in terms of hearing aid use or hearing aid satisfaction (the average four-frequency hearing loss ranged from 22.5 to 62.5 dB HL). In regression models derived by Cox et al. (2007), predicting hearing aid use and overall satisfaction, the pure-tone audiogram did not contribute significantly.
Hosford-Dunn and Halpern (2001) measured the relation between hearing loss (PTA) and the amount of hearing aid use per day as well as satisfaction. The average hearing level at 0.5, 1, 2, and 4 kHz was 35, 42, 53, and 66 dB respectively. They found that those with greater hearing thresholds also reported a greater amount of hearing aid use per day and greater satisfaction levels. Uriarte et al. (2005) found that hearing aid users with higher degrees of hearing loss were more likely to be satisfied with their hearing aids than those with better hearing. Hearing thresholds ranged from 0 to 110 dB HL with a mean of 40.2 dB (SD 14.5; mean better ear three-frequency average).
Overall, it may be concluded that hearing sensitivity (i.e., average pure-tone hearing threshold) tends to be significantly associated with help seeking and uptake, such that a poorer threshold increases the likelihood of seeking help and the acquisition of hearing aids (see Table 7), but it seems not to affect use or satisfaction.
Table 7.
Summary of the Results of Studies of the Relationship Between (Prefitting) Hearing Sensitivity (Pure Tone Hearing Loss) and the Outcome Variables
| Outcome variable | Number of studies | Result |
|---|---|---|
| Help seeking | 4 | 0 + + + |
| Uptake | 3 | + + + |
| Use | 6a | 0 0 0 0 0 + |
| Satisfaction | 7a | 0 0 0 0 + + + |
Note: “+” indicates a positive association between the factor and the outcome, “0” no association.
Some studies had both use and satisfaction as outcome measures, therefore the number of studies sums up to more than 15.
Age
When reporting the results on the influence of age on the variables of interest in this review, it must be mentioned that whereas almost all studies included age (and gender) as variables, only a few regarded these as the primary research variable or investigated them as independent predictors in a regression model. A number of studies regarded age and gender as potential confounders or controlled for them by matching groups (e.g., Humes et al., 2003; see also appendix).
Humphrey et al. (1981) failed to find an association between age and the likelihood of help seeking. Duijvestijn et al. (2003) drew a more or less random sample of adults (>55 years) from the general population and found (after controlling for hearing sensitivity) that there were no age differences between those who had consulted their GP for hearing problems (help seeking) and those who had not. A similar finding was reported by van den Brink et al. (1996). When controlling for confounders (e.g., hearing sensitivity) Helvik et al. (2008) did not find an association between age and uptake. Similarly, Gussekloo et al. (2003) found no relation between age and uptake of hearing aids.
Hickson et al. 1986 reported no significant relation between age and hearing aid use. A range of studies reported to find no relation between age and both hearing aid use and satisfaction (Bentler et al., 1993; Gatehouse, 1994; Hickson et al., 1999; Norman et al., 1994). A similar conclusion was drawn by Henrichsen et al. (1988) who investigated the effect of age on the use and satisfaction with in-the-ear hearing aids (ITE-HA). In the study by Jerram and Purdy (2001), regression analyses predicting hearing aid use and satisfaction (i.e., dependent variables) with prefitting measures as independent variables showed age making no significant contribution to the models. Similar findings using similar regression techniques were reported by Brooks and Hallam (1998). Chang et al. (2008) investigated the relation between age and both the amount of hearing aid use and satisfaction among persons in on-going hearing aid care by dividing the study group into two age-specific subgroups. There were no significant differences in hearing aid use or satisfaction between the two age groups (a) 65 to 80 years (n = 32) and (b) >80 years (n = 27). Uriarte (2005) concluded likewise that age is a non-influential factor with regard to hearing aid satisfaction.
On the other hand, Mulrow et al. (1992) found that lower age was related to higher satisfaction. Hosford-Dunn and Halpern (2001) observed that younger hearing aid wearers reported higher levels of satisfaction than older users but no relation between age and hearing aid use was found in their study.
The vast majority of studies in the literature seem to agree that there is no influence of age on either hearing aid use or satisfaction. This is shown in Table 8. Exceptions are studies by Mulrow et al. (1992) and Hosford-Dunn and Halpern (2001), which agree that young elderly are more satisfied with their hearing aids than the older old people. Note that the vast majority of studies reporting on age included participants older than 60 years.
Table 8.
Summary of the Results of Studies of the Relationship Between Age and the Outcome Variables
| Outcome variable | Number of studies | Result |
|---|---|---|
| Help seeking | 3 | 0 0 0 |
| Uptake | 2 | 0 + |
| Use | 10a | 0 0 0 0 0 0 0 0 0 0 |
| Satisfaction | 11a | 0 0 0 0 0 0 0 0 0 − − |
Note: “+” indicates a positive association between the factor and the outcome, “-” a negative association, “0” no association.
Some studies had both use and satisfaction as outcome measures, so the number of studies in the table sum up to more than 17.
Gender
Humphrey et al. (1981), Duijvestijn et al. (2003), and van den Brink et al. (1996) failed to find an association between gender and the likelihood of help seeking. Gussekloo et al. (2003) reported that gender did not affect the likelihood of the elderly participants taking part in hearing aid rehabilitation (uptake) and Helvik et al. (2008) found that gender did not differentiate between those rejecting hearing aids and those accepting them (uptake).
Several articles examined the influence of gender on postfitting success and these seem to agree in that they failed to find an association between gender and hearing aid use (Gatehouse, 1994; Hickson et al., 1986, 1999; Lupsakko et al., 2005; Norman et al., 1994). Using regression techniques, both Brooks and Hallam (1998) and Jerram and Purdy (2001) found no relation between gender and hearing aid use or satisfaction. Likewise, Gatehouse (1994), Hickson et al. (1999), Norman et al. (1994), and Uriarte et al. (2005) did not find an association between gender and hearing aid satisfaction.
None of the studies conducted so far found an influence of gender on any of the outcomes (Table 9). This was also concluded in the review by Wong et al. (2003).
Table 9.
Summary of the Results of Studies of the Relationship Between Gender and the Outcome Variables
| Outcome variable | Number of studies | Result |
|---|---|---|
| Help seeking | 3 | 0 0 0 |
| Uptake | 2 | 0 0 |
| Use | 7a | 0 0 0 0 0 0 0 |
| Satisfaction | 6a | 0 0 0 0 0 0 |
Note: “0” indicates no association between the factor and the outcome.
Some studies had both use and satisfaction as outcome measures, so the number of studies in the table does not sum up to 13.
Socioeconomic Status/Working Conditions/Social Relations
Six studies looked at the relationship between socioeconomic status (or related variables) and the relevant outcome measures.
Humphrey et al. (1981) did not find a relation between socioeconomic status and uptake. Note that this study was conducted in the United Kingdom where hearing aids provided by the National Health Service (NHS) are free of charge. Humes et al. (2003) found that socioeconomic status did not significantly differentiate the accept-HA group from the reject-HA group (so demonstrating no effect of this variables on uptake). Also Gussekloo et al. (2003) found no differences in income levels between those elderly participants who accepted a hearing aid rehabilitation program (hearing aid uptake) and those who did not.
In regression analyses predicting hearing aid use and satisfaction (i.e., dependent variables) with prefitting measures as independent variables, employment status (not employed, part time, full time) did not contribute significantly in the study by Jerram and Purdy (2001).
Garstecki and Erler (1998) did find that the level of “income satisfaction” was higher among adherents of hearing aids compared to nonadherents. Lupsakko et al. (2005) investigated the factors that distinguished nonusers (who already had acquired hearing aids) from part-time or full-time users and found that the group of nonusers had approximately half the median income compared to the other two groups. This indicated that the annual income of a hearing aid user may have an influence on whether a person continues using hearing aids already acquired. In this context, it should be mentioned that hearing aids were free but hearing aids wearers were to purchase their batteries themselves.
The results concerning socioeconomic status are mixed. An overview is provided in Table 10. Note that these results do not concern perceived or actual cost of hearing aids (see section on “Factors Examined in Only One Study”).
Table 10.
Summary of the Results of Studies of the Relationship Between Socioeconomic Status and the Outcome Variables
| Outcome variable | Number of studies | Result |
|---|---|---|
| Help seeking | No data | |
| Uptake | 4 | 0 0 0 + |
| Use | 2a | 0 + |
| Satisfaction | 1a | 0 |
Note: “+” indicates a positive association between the factor and the outcome, “0” no association.
One study had both use and satisfaction as outcome measures, so the number of studies in the table does not sum up to six.
Living Arrangement
Five studies addressed the issue of living arrangement and its association with hearing aid uptake, use, or satisfaction.
Gussekloo et al. (2003) found no relation between living relations (alone vs. with others) between those elderly participants who accepted a hearing aid rehabilitation program (hearing aid uptake) and those who did not. Similarly Humes et al. (2003) and Helvik et al. (2008) found that living arrangement did not relate to the rejection of hearing aids (uptake).
In the two studies by Hickson et al. (1986, 1999), the issue of an individual's residential situation was addressed. It was found that whether a hearing aid user lived alone or in a nursing home did not affect the amount of hearing aid use per day (Hickson et al., 1986). Also in the later study Hickson (Hickson et al., 1999) demonstrated that residential situation was not related to the use of or satisfaction with hearing aids.
Thus none of the studies found an association between living arrangement and three of the outcomes (uptake, use, satisfaction). See Table 11.
Table 11.
Summary of the Results of Studies Reporting of the Relationship Between Living Arrangement and the Outcome Variables
| Outcome variable | Number of studies | Result |
|---|---|---|
| Help seeking | No data | |
| Uptake | 3 | 0 0 0 |
| Use | 2a | 0 0 |
| Satisfaction | 1a | 0 |
Note: “0” indicates no association between the factor and the outcome.
One study had both use and satisfaction as outcome measures, so the number of studies in the table does not sum up to five.
Educational Level
Three studies reported on the influence of educational level on the uptake of hearing aids.
A study by Humes et al. (2003) attempted to identify prefit variables differentiating an accept-HA group (uptake) from a reject-HA group (the two groups were matched for age, gender, and hearing loss). The two groups did not differ in educational level. Also the population study by Gussekloo et al. (2003) found no relation between educational level and uptake of hearing aids. In a study by Helvik et al. (2008), educational level (dichotomized into two groups: <13 years and >13 years of schooling), appeared to influence uptake, such that a high educational level increased the odds of rejecting a hearing aid.
Time or Longitudinal Change
Three studies were found dealing with time (also defined as adaptation or acclimatization) postfitting and explicitly focusing on hearing aid use or satisfaction as outcome measures.
The first is the longitudinal study by Munro and Lutman (2004) who followed 32 first-time hearing aid users. They measured hearing aid use and satisfaction using the Glasgow Hearing Aid Benefit Profile (GHABP), up to 6 months postfitting. They found a statistically significant gradual increase in satisfaction scores during the first 3 months post fitting but only among those participants who referenced their satisfaction scores to their performance 3 weeks earlier. There was no significant change in use in this period.
Another longitudinal study was conducted by Bentler et al. (1993). No significant changes in hearing aid use and satisfaction were found in the period between 6 and 12 months postfitting. Humes et al. (2002) reported contradictory findings. Their study among 134 participants demonstrated a significant decline in satisfaction and use at 6 and 12 months postfitting, compared to the perceived satisfaction 1 month after fitting.
In sum, the two studies (Humes et al., 2002 and Bentler et al., 1993) that are comparable in terms of the timing at which hearing aid use and satisfaction were measured (i.e., 6–12 months postfitting) show dissimilar results. Humes et al. (2002) observed significantly lower use at 1-year postfitting (compared to 6 months postfitting), whereas Bentler et al. (1993) did not observe any change in that period.
Lifetime Hearing Aid Experience
Three studies provided knowledge describing how having experience with hearing aids is associated with the amount of daily hearing aid use and the satisfaction level. Hosford-Dunn and Halpern (2001) found a positive correlation between years of hearing aid use (experience with hearing aids) and hearing aid use and satisfaction. Data reported by Saunders and Jutai (2004) demonstrated a significant relationship between daily hearing aid use and total lifetime use (>10 years), such that over time individuals wear their hearing aids for longer each day. With regard to hearing aid satisfaction, Uriarte et al. (2005) observed a significant effect of previous hearing aid experience on global satisfaction, such that greater experience with hearing aids was associated with higher satisfaction.
Age at Onset of Hearing Loss
Two studies investigated how age at onset of hearing loss was associated with hearing help seeking and hearing aid uptake. Humphrey et al. (1981) found that people who experienced hearing difficulties before retirement age (i.e., 65 years) were more likely to seek help than those who started experiencing hearing problems at a later stage in life. Humes et al. (2003) found that age at onset of hearing loss was not related to hearing aid uptake.
Hearing Aid Professional
Two studies addressing the role of the hearing aid professional were conducted by Uriarte and colleagues (2005). A positive correlation between satisfaction with hearing aids (as measured with the SADL) and satisfaction with the practitioner was observed. Note that correlations do not disclose whether satisfaction with the professionals led to satisfaction with hearing aids or vice versa. In a clinical study involving three different audiologists, Hickson et al. (1986) found that there was no variety in hearing aid use related to the different audiologists.
Dexterity
In the study of Humes et al. (2003), there were two groups of participants who tried hearing aids (those who retained the hearing aid and those who rejected it). Those who retained their hearing aid use had better finger dexterity (nine-hole peg test). Hickson et al. (1986) observed that difficulty handling the hearing aids was associated with less use. The same was observed by Wilson and Stephens (2003) who also reported a positive association with satisfaction. However, in these two latter studies manual skills were measured as perceived by the audiologist, and this may not be a reliable measure.
Factors Examined in Only One Study
Amongst the 39 studies included in our review, we encountered 13 factors that appeared in only one study. These factors are listed below.
Amount of social interaction: not related to uptake of hearing aids. (Humes et al., 2003).
Concern about costs was more likely in the nonadherent group (uptake; Garstecki & Erler, 1998).
Duration of hearing loss: not related to rejection of hearing aid rehabilitation (uptake; Helvik et al. (2008).
Marital status (married, not married): not related to uptake (Gussekloo et al., 2003).
Type of clinic (public vs. private), no influence on use or satisfaction. (Jerram & Purdy, 2001).
First impression of the aid: no effect on hearing aid use (Hickson et al., 1986).
Activity of daily living (ADL; Wade & Collin, 1988) refers to physical (dis)abilities. Lupsakko et al. (2005) studied the relationship between ADL and hearing aid use as part of the Kuopio (Finland) 75+ study. The authors found that the more help was needed in all activities of daily living, the less was the hearing aid use.
Major life events (loss of employment, death of spouse, illness): negative impact on hearing aid use (Kricos et al., 2007).
Cosmetic appearance of hearing aids correlated positively with overall satisfaction, not with use. (Hickson et al., 1999)
Health: Gussekloo et al. (2003) found that none of the four factors, cognitive function, subjective health, depression, or feelings of loneliness were related to uptake of hearing aids. Note that depression has elsewhere (see section on Personality) been described as an element of personality. This was done because the studies mentioned in that paragraph considered it as such.
Use of medication: negatively related to hearing aid use (Mulrow et al., 1992).
General health attitude: not related to uptake (Humes et al., 2003)
Speech reading: not related to uptake (Humes et al., 2003)
Number of Studies and Factors Divided Over Stages
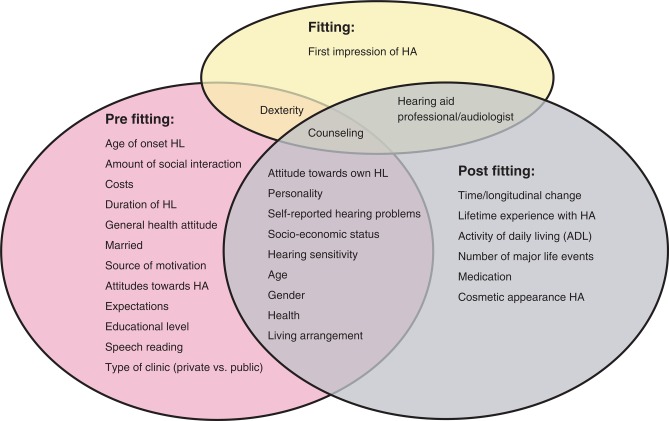
Figure 1 provides an overview of all factors that were included in the studies. It also shows how the factors are divided over the different stages (i.e., prior to hearing aid fitting, the period covering the fitting, and the postfitting period). Some were examined both prior and posthearing aid (i.e., attitude toward own HL, personality, self-reported hearing problems, socioeconomic status, hearing sensitivity, age, gender, health, living arrangement). Counseling was studied in all three periods, dexterity was studied in both prefitting and fitting period, and the importance of the hearing aid professional/audiologist was studied in both fitting and postfitting period.
Figure 1.
Overview of all factors that were included in the studies, divided over the different stages (i.e. prior to hearing aid fitting, the period covering the fitting and the period post fitting).
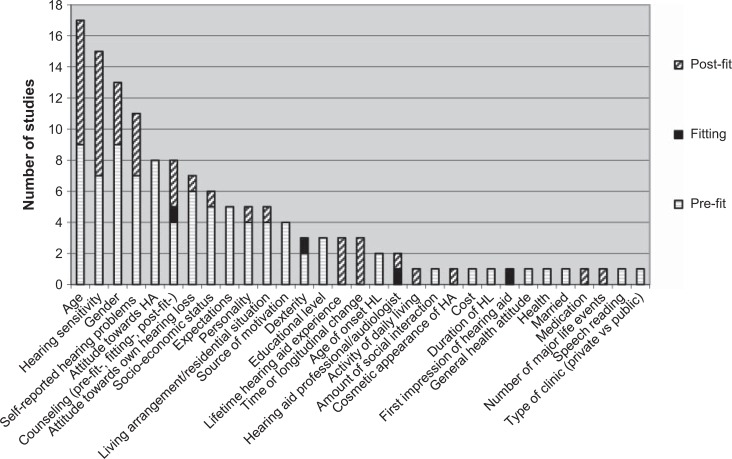
An overview of how many times each particular factor was studied is shown in Figure 2. Age is the factor most frequently studied, followed by hearing sensitivity, gender, self-reported hearing loss, attitude toward hearing aids (only in prefitting stage) and counseling (both prefit, fitting, and postfit). Some factors obviously belong to one stage (e.g., experience with hearing aids, postfitting counseling in the postfitting section). Figure 2 also demonstrates the disproportionate number of studies in the different stages. In particular the stage covering the hearing aid fitting itself has scarcely been investigated, meaning that very little empirical evidence is available regarding how the sequence of events during the fitting process affects hearing aid use and satisfaction.
Figure 2.
Number of studies per factor divided over stage (i.e., prefitting, fitting, postfitting)
Discussion
Effects Found
The primary aim of this review was to learn more about the factors at three different stages in a client's journey (i.e., prior to the actual hearing aid fitting, during the actual fitting period, and postfitting) influencing help seeking, hearing aid uptake, use, and satisfaction. Whereas other reviews have focused on one of those outcomes (e.g., Wong et al., 2003), this study listed the results for four outcomes and thus is able to reveal patterns of effects across outcome domains.
The first notable finding of this study is that the same factor may have quite different effects on each of the four outcome variables (help seeking, uptake, use, satisfaction). The small tables at the end of each paragraph illustrate this. A factor may significantly influence one of the variables and have no relationship with the others. For example, motivation (by others; Table 1) seems to have a positive effect on help seeking, but there is no evident association between prefitting source of motivation and later hearing aid use or satisfaction. Also, whereas motivation by others may have a significant positive influence on help seeking, satisfaction with hearing aids may be positively affected by self-motivation, rather than by motivation by others (Hickson et al., 1999). It is thus very important for both clinicians and researchers to carefully consider what the main aim of a certain intervention is. For example, if the long-term goal is to ensure satisfaction with hearing aids, forcing somebody into the health care system (help seeking) may not be the most adequate strategy; Developing interventions aiming to create self-motivated persons (as opposed to motivated by others) may be a better alternative. Similarly, the majority of studies examining hearing sensitivity as a factor showed a significant positive association with hearing aid uptake. However, hearing sensitivity seems to be a poor predictor for hearing aid use or satisfaction.
Of the four outcome variables in this study (help seeking, uptake, use, and satisfaction), use and satisfaction are probably most closely related. A range of studies have demonstrated a positive association between these two (Hickson et al., 1999; Jerram & Purdy, 2001; Öberg et al., 2007; Uriarte et al., 2005). However, others found that people who use their hearing aids a relatively short time per day, may be very satisfied with them (Dillon et al., 1999; Kochkin, 1997; Wong et al., 2003).
Some factors appeared to have a “universal” effect in that they significantly influenced all four variables in the same direction or demonstrated no relationship with any of the outcomes in any stage of the process. This was observed for three factors: self-perceived hearing, age, and gender. The former had significant positive effect toward help seeking, uptake, use, and satisfaction, whereas the vast majority of studies on age and gender showed no relationship with help seeking, uptake, use, or satisfaction.
The fact that self-perceived hearing difficulties appeared to correlate positively with all four outcome variables is quite a noteworthy finding. It means that self-perceived activity limitation (and participation restriction) may be regarded as a very important determinant in aural rehabilitation as it is able to predict four key elements. Meanwhile hearing sensitivity did not show such a pattern. Note that Cox et al. (2003), when developing norms for the IOI-HA, also found that self-reported hearing difficulties related more closely to the IOI-HA (including questions on hearing aid use and satisfaction) than measures of hearing sensitivity. This finding resulted in the development of two sets of norms based on people's perceptions of their own hearing problems.
The finding of self-reported hearing problems affecting all outcomes in the same direction may have consequences for other activities within audiology such as, for example, screening for hearing aid candidacy. Programs covering screening for hearing loss usually aim to increase the uptake and satisfaction with hearing aids (e.g., Davis et al., 2007). In line with the suggestion of Stephens et al. (1990), the present data indicate that self-report may be a better choice than measuring hearing sensitivity when screening for hearing aid candidacy.
One may also argue that providing measures of self-reported hearing difficulty may be more meaningful than providing measures of hearing sensitivity when describing groups of participants in future hearing aid–related studies, including those aiming to quantify the true size of the population that could benefit from hearing aid fittings. Self-report instruments appropriate for this task, as well as convenient to administer and properly validated, are available nowadays (Bentler & Kramer, 2000).
Gender appears to be an irrelevant factor with regard to help seeking, uptake, use, and satisfaction. More or less the same conclusion can be drawn for age. Two (out of 11) reported a significant negative effect of age on satisfaction (Hosford-Dunn & Halpern, 2001; Mulrow et al., 1992). Younger adults were more satisfied and used their hearing aids more than older participants. It must be noted that almost all studies included samples predominantly consisting of elderly people. Possible covariates, such as occupational status (working versus retired; Humphrey et al., 1981) may have played a role here. The findings indicate that there is no basis for doing things differently if the client is male vs. female.
The studies examining living arrangement also showed unanimous results, that is, no associations. However the total number of studies was small and they addressed only uptake, use, and satisfaction. Furthermore, the causality in the associations is difficult to determine without making longitudinal studies.
Data Treatment and Quality
One could argue that we should have assigned a weight to each study referring to the level of statistical evidence, those with a higher level of evidence receiving a higher weight.
According to Cox (2005), a randomized controlled design should receive the highest weight as it has the highest level of evidence. As shown in the appendix, there were only four randomized controlled trials out of 39 studies (Brickley et al., 1996; Eriksson-Mangold et al., 1990; Kemker & Holmes, 2004; Öberg et al., 2008) and these all addressed the effect of a counseling program on hearing aid use and satisfaction. The RCTs did not show unanimous findings and hence it can be concluded that the effects of counseling on use and satisfaction are not certain. Seven studies were nonrandomized intervention studies (NRIS), comparing groups that were sometimes matched (Brooks, 1989; Gussekloo et al., 2003; Humes et al., 2003; Kapteyn et al., 1997; Munro & Lutman, 2004; Norman et al., 1994, 1995; see appendix). Three of these addressed the effect of counseling on the variables of interest. Hence the vast majority of the factors described in this review were examined in studies using a noninterventional descriptive design (NIDD). A NIDD has a lower level of evidence than an NRIS or an RCT. Hence we argue that the studies included in this review have at least a minimum amount of evidence of reasonable quality and that assigning different weights would make little difference to the conclusions.
Another important issue is the quality of the outcome measures used. Even though the vast majority of studies fell in the same category (NIDD) and had comparable age groups, there was still a large variation in outcome measures used to assess the factors (e.g., expectation, attitude, personality) or to assess the outcome variables (help seeking, uptake, use, satisfaction). This is illustrated in the appendix. Most studies used one of the following questionnaires (or scales of these questionnaires) to measure use and/or satisfaction: SADL, HAR (Brooks, 1989), IOI-HA, IDI, GHABP, HAUQ (Forster & Tomlin, 1988), HAOQ (Wong, 2004), Visual Analogue Scale (Wilson & Stephens, 2003). Some studies used a set of questions designed for that particular study (referred to as own questionnaire (OQ) in the Appendix). Whereas the majority of studies applied questionnaires with known reliability and validity, in a number of articles this was not explicitly mentioned. To enhance the quality of reporting, it is recommended that authors give a rationale for the choice of a certain tool and declare its reliability and validity for their particular sample. Within this context, it is worth mentioning that all studies in this review just administered one single question to assess hearing aid use. This occurred either by asking about the hours of use per day or it addressed the frequency of use (almost never—almost always). It is known that single questions lack reliability (for a comprehensive outline of issues related to reliability and validity, we refer to Wong et al., 2003) and this issue deserves attention in future studies.
State-of-the-Art
The results of the current study bring us to the discussion as to what we know from the literature so far and where there still are gaps in our knowledge. The current review revealed that a total of 31 factors have been examined in relation to help seeking, uptake, use, and satisfaction in the last 28 years (see Figure 1). Many factors have been the subject of only one study (e.g., amount of social interaction, health, type of clinic).
Tables 2 to 11 summarize the data for all cases where there may be sufficient data to begin to discern patterns in the relations between factors and outcomes. Although it is encouraging to observe that contradictory results were not found (i.e., a “+” and a “-” in the same row of a table), there are few cases where all studies showed the same relation between factor and outcomes (i.e., rows containing only one type of symbol).
In addition, even when a significant correlation is observed, the proportion of variance explained may still be small (Cox et al., 2007) leaving room for other factors that were not examined.
So, the overall impression is that research in audiology is still struggling to identify factors that really matter, remain consistent over studies, and explain a substantial amount of variation. The study of Humes et al. (2003) who failed to identify any factor (from a long list of factors) that significantly differentiated two groups of participants who tried hearing aids (i.e., differentiate the reject-HA group from the accept-HA group), is a good example in this respect. The choice of outcome measures also varies widely between the studies reviewed here, indicating that progress in identifying critical outcome domains is also required.
An interesting outcome of this study is the distribution of studies over the three periods (i.e., prefitting, fitting, postfitting). There are only 2 studies addressing the actual fitting process (appendix, Figure 1). It is quite surprising that there is so little empirical evidence about how variations in the actual fitting process affect on uptake, use, and satisfaction. The two studies revealed that the first impression of the hearing aid or the client's impression of the professional did not affect any of the outcome variables. Counseling during the fitting did. It is clear that much more research is required in this area. There are several papers in the non-peer-reviewed domain (and papers not measuring the four outcome variables in this study) discussing the fitting process itself. These papers provide valuable pointers information as to which aspects of the fitting process could fruitfully be examined in future controlled studies and are the subject of the next paragraph.
All of the studies reviewed in this article reported on statistical relationships between factors and outcomes. However it is the causal relationships that have to be clarified before one can understand how to improve outcomes. Longitudinal designs are required for that purpose. Thus longitudinal studies following people for several years are also essential.
Potentially Influential Factors Not Included in the Formal Review
Throughout this review process and also when reviewing the articles in the non-peer-reviewed domain, we have come across a number of potentially influential factors and issues that were discussed in these papers and that we find worth mentioning here. These factors could be considered for future research.
As an example, Kirkwood (2005) conducted a survey among dispensers and asked their views on what factors determine a client's satisfaction with hearing aids. Of the 674 dispensing professionals interviewed, only 6% of them perceived the hearing aids as the most important factor leading to a successful fitting; 39% regarded the counseling skills of the dispenser as the most relevant. Twenty-six percent of the dispensers selected the dispenser's fitting/programming skills as the most important. Another example is a study by Kargas and Doyle (1996) who addressed the issue of time spent in the clinic (in relation to patient satisfaction). The type of clinic may also play a relevant role. This was illustrated by Cox et al. (2005) who observed personality differences between VA and private practice patients and concluded that it might be inappropriate to generalize research findings from one group to the other.
Additional to this are the style of counseling employed during the clinical setting including the overall type and quality of the interaction between the professional and the client. Different styles are described in the literature and these are also known as the medical model, the patient-centered model, and the relationship model. English (2005) gives an outline with descriptions of each of these. Other relevant articles are Clark (2007) and Boothroyd (2007).
The role of the GP or the medical doctor as gatekeepers or as instruments leading a person to seek help and obtain a hearing aid (or not do so) is also important to consider within this context (Grutters et al., 2007; Humphrey et al., 1981; Kochkin, 1998, 2004; Stephens, 1989).
Cox et al. (2005) discussed the role of the significant other (e.g., spouse, family member, sibling). Significant others around the person with the hearing impairment may make efforts to minimize the restrictions of the hearing impairment. This mechanism is described as the social support coping used by significant others. The more the person with hearing impairment is surrounded by such coping, the less likely it may be that he or she regards himself or herself as having a hearing loss and seeks help to acquire hearing aids.
The concept of “self-efficacy” is another factor that deserves attention in future studies. Self-efficacy reflects the idea that what people think, feel, and believe they are capable of affects what they are actually capable of. Numerous studies within the areas of adult and child psychology have shown that measured self-efficacy can predict the success of coping with difficult situations (Bandura 1986, 1989). Several authors (Carson & Pichora-Fuller, 1997; Kricos, 2000, 2006; Tsuroka et al., 2001; Weinstein, 2000) suggested that self-efficacy may have a significant impact on audiological rehabilitation such that “the low uptake and lack of continued use of hearing aids by older adults may be partly due to their low self-efficacy for learning how to use and take care of hearing aids” (from Kricos, 2006, p. 19).
A further issue is the lack of general visibility of the field of audiology and its practices, such as hearing aid rehabilitation. The low percentage of people seeking help and taking up hearing aid rehabilitation (when compared to the estimated amount of people with a hearing loss) may be the result of the invisibility of the health care services and audiology as a discipline (English, 2005) as well as a general lack of factual knowledge about what can and cannot be accomplished by engaging in hearing aid rehabilitation (Meis & Gabriel, 2006). However, Kochkin (1998) found that marketing and mass media exposure of the positive possibilities of hearing aids only caused marginal expansions in the uptake of hearing aids. He argued that there is no potential progress in uptake to be made by increasing the visibility.
Finally, the journey that a person with hearing impairment is guided along may be relevant in terms of help seeking, hearing aid uptake, use, and satisfaction. A person with auditory difficulties goes through various emotional stages and coping with hearing loss is a dynamic process. As mentioned in the introduction, there is no scientific evidence yet as to how different journeys may affect any of the outcomes in this review. But the literature does contain models and articles that describe the process of becoming hearing impaired and factors influencing the adjustment to it. Already in the 1980s, Jones et al. (1987) presented a holistic model (figure 13.1, p. 216, figure 13.2, p. 218,) with factors influencing the adjustment to hearing impairment in the period prior to hearing aid fitting. Furthermore, Kochkin (1998, 2007) studied a large amount of both internal and external factors that may affect the journey toward a “hearing solution” (in this study this was defined as purchasing a hearing aid). Dominant reasons for not purchasing hearing aids were that people found their hearing loss to be too mild (to need hearing aids) and that they presumed they would not be able to afford hearing aids. On the basis of this survey, Kochkin (1998, figure 1, p. 31; 2007, figure 3, p. 33.) developed models of the ideal hearing solution or hearing aid adaptation process. More recently, Engelund (2006) identified four stages of “consciousness of hearing problems” in the process of adjusting to hearing impairment, prior to help seeking, and interpreted those as (a) attracting attention, (b) becoming suspicious, (c) sensing tribulation, and (d) jeopardizing the fundamental self. The sequence of stages is characterized by the extent to which a person with hearing impairment is aware of their problems and their actions. It is argued that a person is only ready to seek help and take up a hearing aid when Stage 4 has been reached. It would be interesting to seek further evidence for such stages in future research.
Engelund's study is an example of how qualitative research may reveal in-depth information about interpersonal processes relevant in a person's journey toward the decision to seek help and pursue amplification. We foresee that more qualitative studies are required in the future to obtain insight into factors that have been missed so far.
Conclusion
An extensive search of the literature covering studies addressing help seeking, hearing aid uptake, use, and satisfaction with hearing aids yielded 39 empirical studies published in the period between January 1980 and January 2009. A total of 31 factors have been examined in these studies. These were personal factors (e.g., source of motivation, expectation, attitude, hearing sensitivity), demographic factors (e.g., age, gender), or external factors (e.g., cost, counseling). Whereas we found mixed results for the majority of factors, three appeared to show consistent effects across the four outcome domains: gender, age, and self-reported activity limitation. Gender was not related to any of the four outcome variables. So, we conclude that gender is a rather irrelevant factor. The same applies for age, but it must be noted that broader age ranges are needed in future studies to draw firm conclusions about the effects of age on the outcome domains. Self-reported activity limitation as measured prior to treatment correlated positively with all four outcomes throughout all stages (prefitting, fitting, postfitting). This is a noteworthy finding that clearly demonstrates that self-reported auditory difficulty is highly important in aural rehabilitation, possibly more important than objective hearing sensitivity, which showed less consistent effects on outcomes.
Some factors (e.g., source of motivation) had opposite effects on different outcomes. This result underlines the need to carefully consider what outcome (help seeking, uptake, use, or satisfaction) is the prime interest when designing rehabilitation programs.
Only two studies addressed the actual fitting process, indicating a great need for more empirical research on this stage.
We conclude that whereas there is a large body of literature available on factors possibly influencing the different stages in the process toward help seeking, obtaining a hearing aid, using it, and becoming satisfied with it, there are many issues that have not yet been investigated in controlled studies. We tentatively identify the most important or fruitful issues for further research to be the interaction between the professional and the client throughout an individual's hearing journey, self-efficacy, counseling style, and the role of professionals as gatekeepers. Causality is another issue that should be addressed in future research. Longitudinal studies are required for that purpose.
Acknowledgments
The authors acknowledge the helpful comments of Thomas Lunner and Elisabet Sundewall-Thorén on an earlier version of the manuscript.
Appendix: Overview of the Reviewed Studies Including Factors, Outcomes, Study Design and Other Descriptive Variables
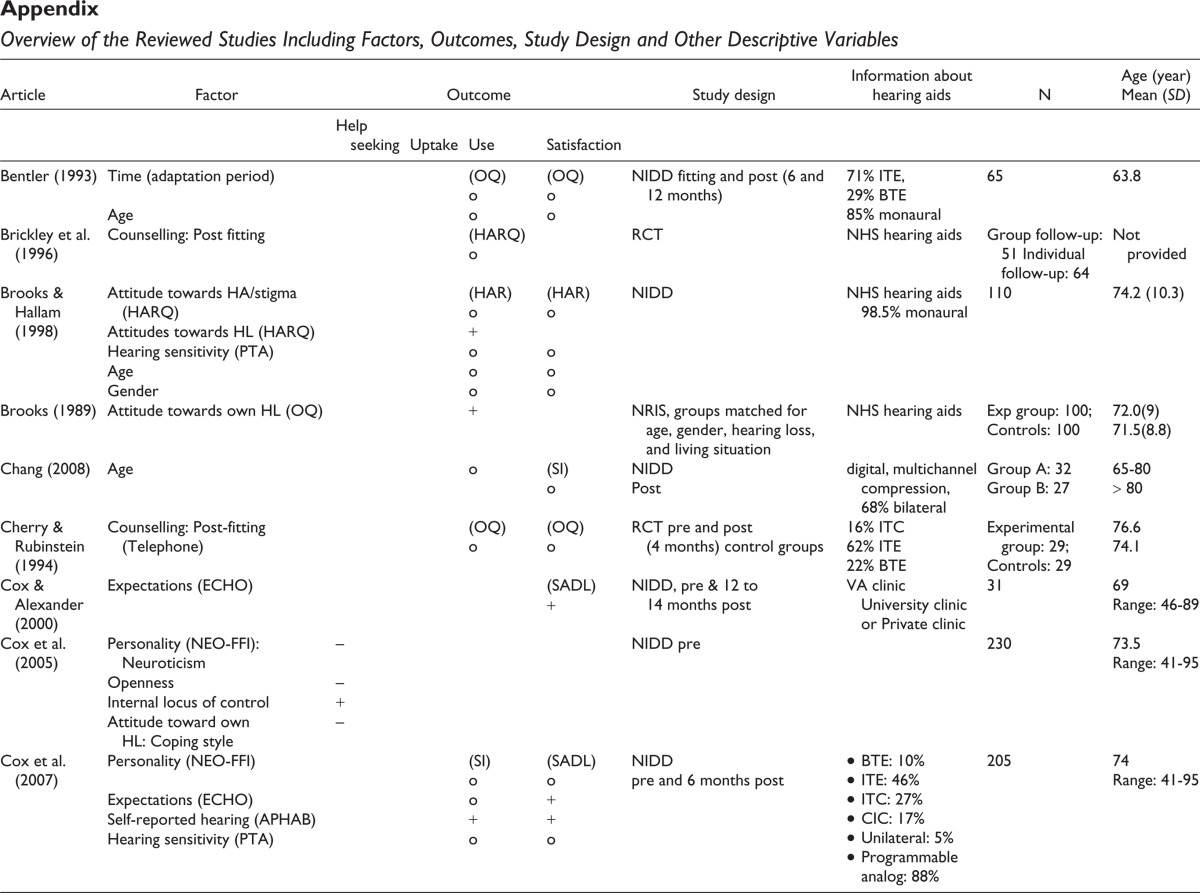
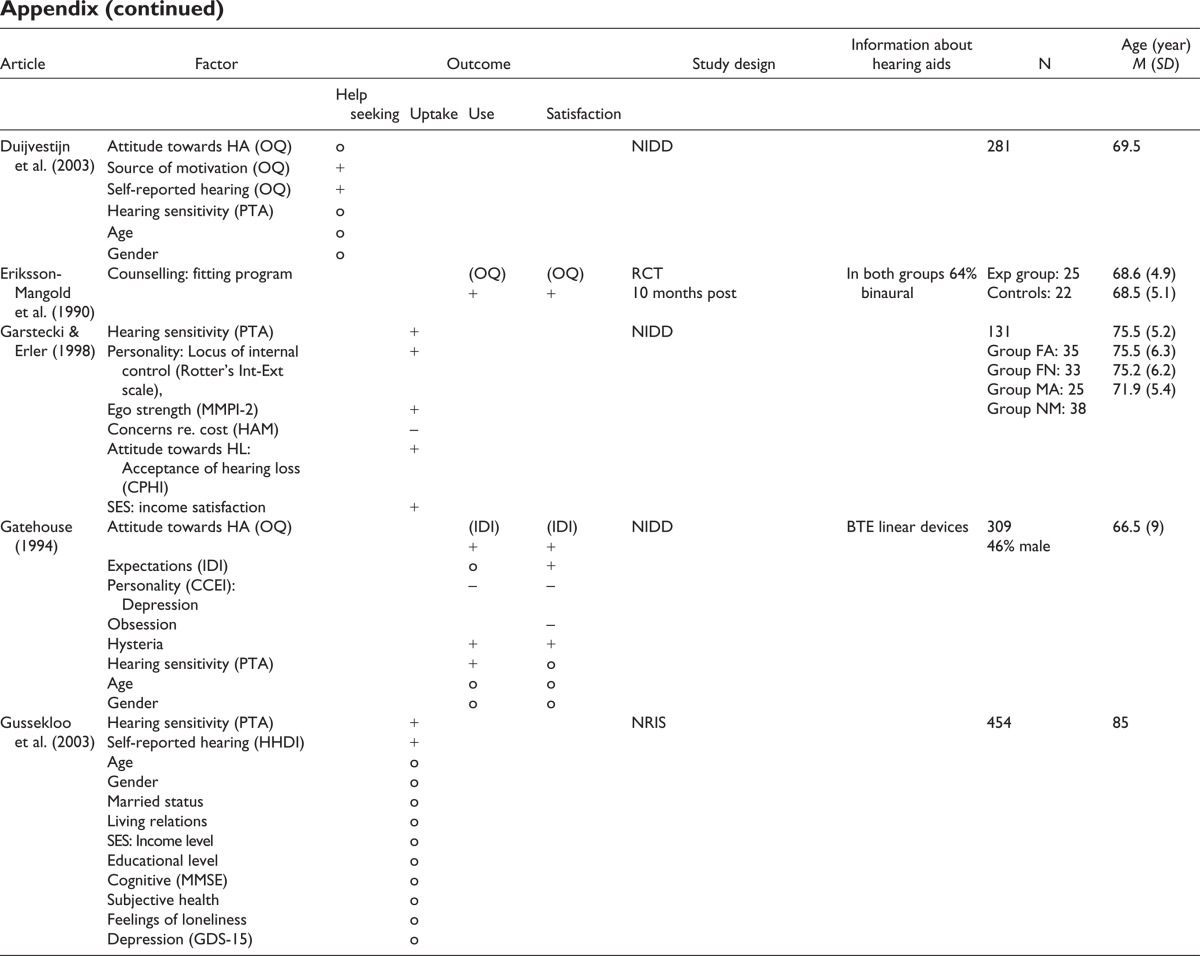
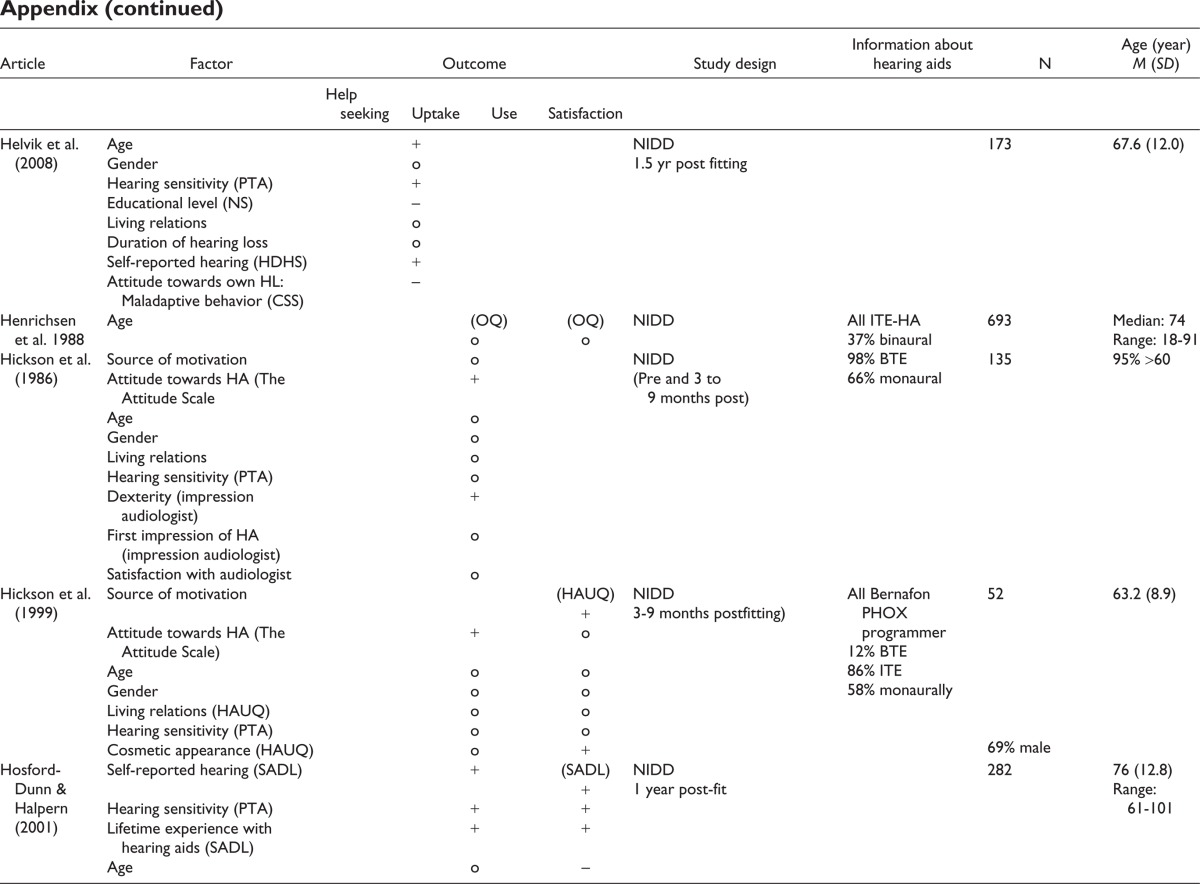
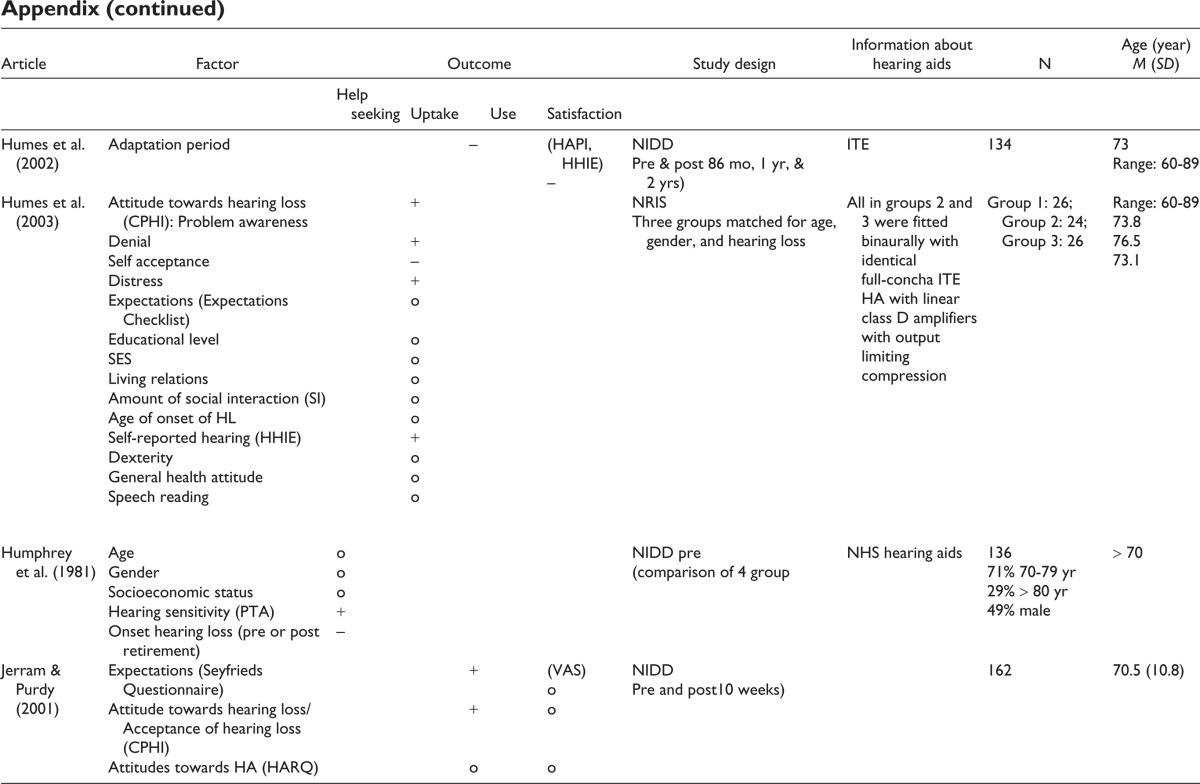
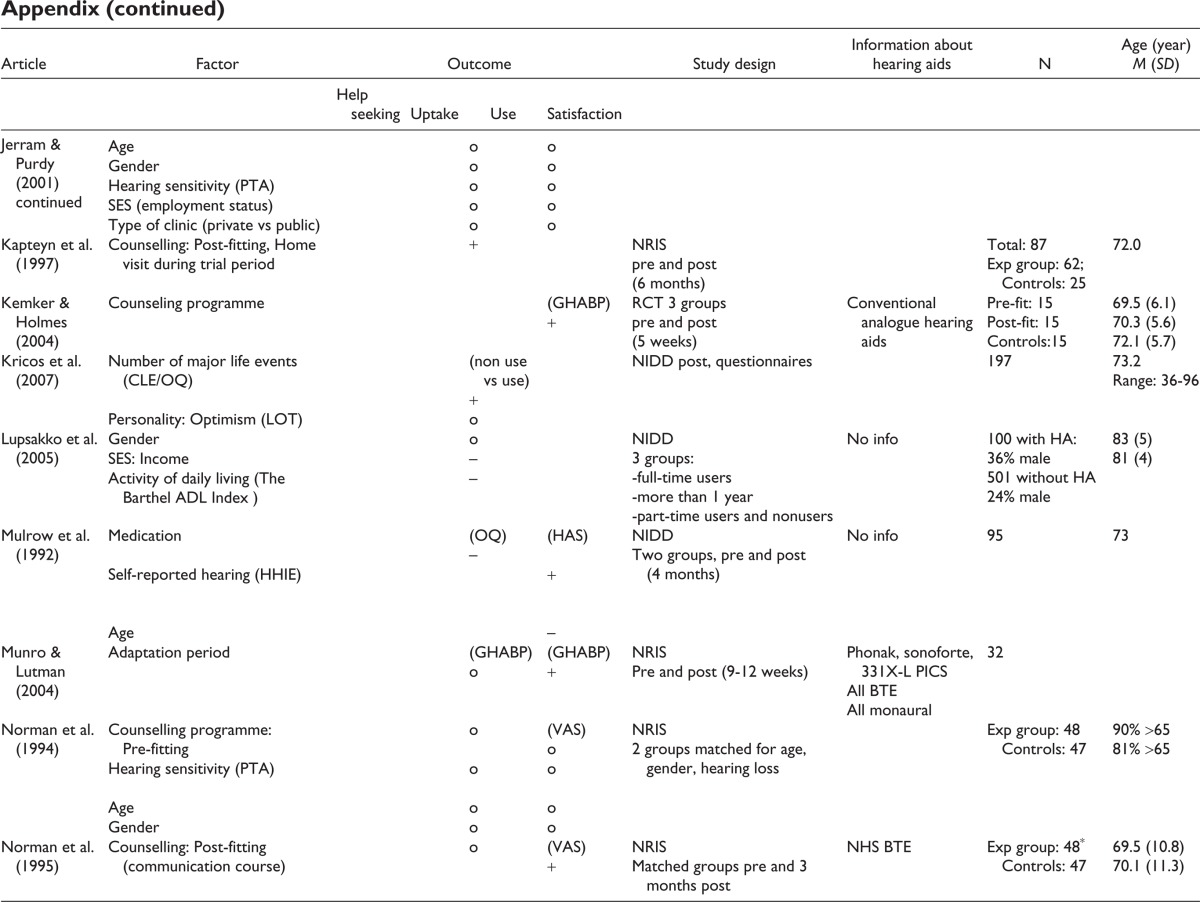
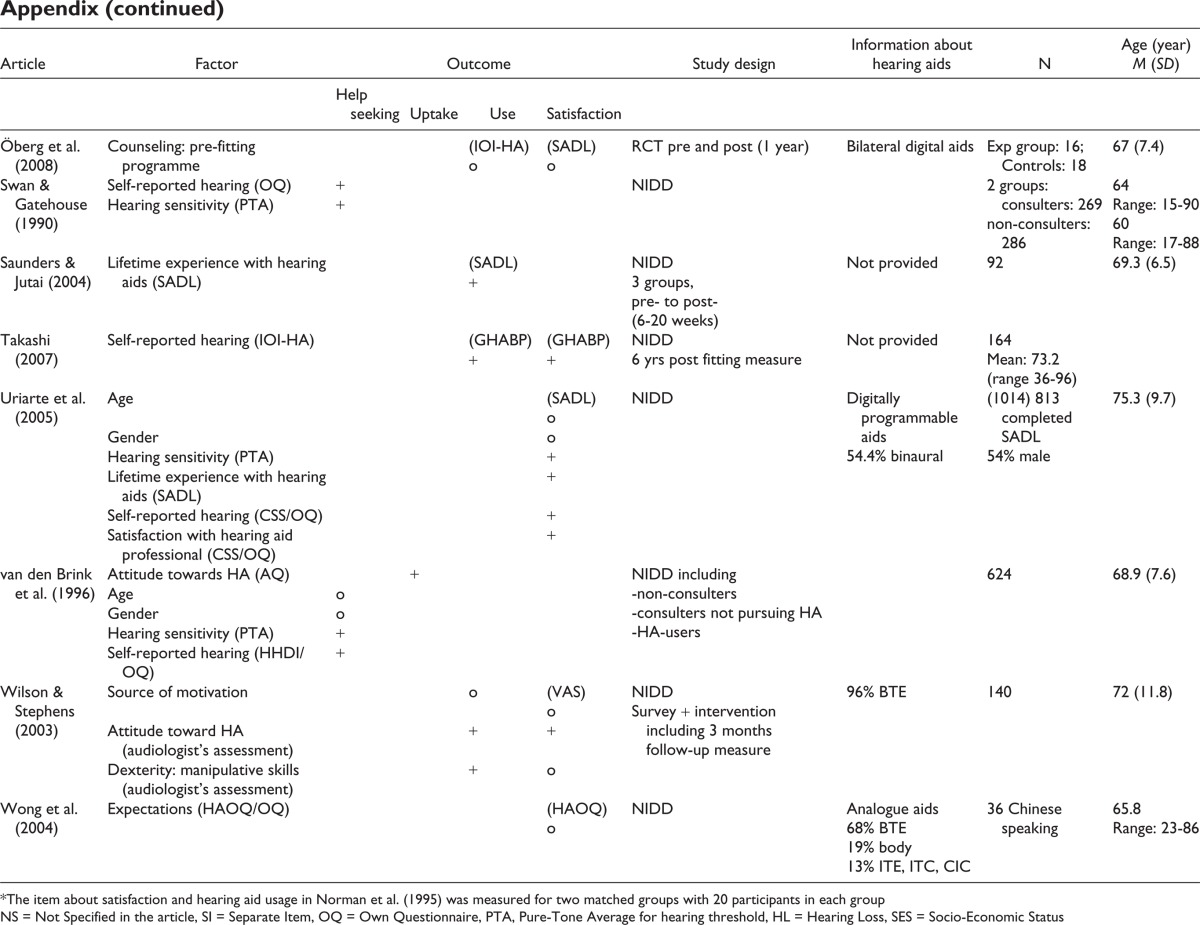
| Article | Factor | Outcome | Study design | Information about hearing aids | N | Age (year) Mean (SD) | |||
|---|---|---|---|---|---|---|---|---|---|
| Help seeking | Uptake | Use | Satisfaction | ||||||
| Bentler (1993) | Time (adaptation period) Age |
(OQ) o o |
(OQ) o o |
NIDD fitting and post (6 and 12 months) | 71% ITE, 29% BTE 85% monaural |
65 | 63.8 | ||
| Brickley et al. (1996) | Counselling: Post fitting | (HARQ) o |
RCT | NHS hearing aids | Group follow-up: 51 Individual follow-up: 64 | Not provided | |||
| Brooks & Hallam (1998) | Attitude towards HA/stigma (HARQ) Attitudes towards HL (HARQ) Hearing sensitivity (PTA) Age Gender |
(HAR) o + o o o |
(HAR) o o o o |
NIDD | NHS hearing aids 98.5% monaural | 110 | 74.2 (10.3) | ||
| Brooks (1989) | Attitude towards own HL (OQ) | + | NRIS, groups matched for age, gender, hearing loss, and living situation | NHS hearing aids | Exp group: 100; Controls: 100 |
72.0(9) 71.5(8.8) |
|||
| Chang (2008) | Age | o | (SI) o |
NIDD Post |
digital, multichannel compression, 68% bilateral | Group A: 32 Group B: 27 |
65–80 > 80 | ||
| Cherry & Rubinstein (1994) | Counselling: Post-fitting (Telephone) | (OQ) o |
(OQ) o |
RCT pre and post (4 months) control groups | 16% ITC 62% ITE 22% BTE |
Experimental group: 29; Controls: 29 |
76.6 74.1 |
||
| Cox & Alexander (2000) | Expectations (ECHO) | (SADL) + |
NIDD, pre & 12 to 14 months post | VA clinic University clinic or Private Clinic |
31 | 69 Range: 46–89 |
|||
| Cox et al. (2005) | Personality (NEO-FFI): Neuroticism Openness Internal locus of control Attitude toward own HL: Coping style |
− − + − |
NIDD pre | 230 | 73.5 Range: 41–95 |
||||
| Cox et al. (2007) | Personality (NEO-FFI) Expectations (ECHO) Self-reported hearing (APHAB) Hearing sensitivity (PTA) |
(SI) o o + o |
(SADL) o + + o |
NIDD pre and 6 months post |
• BTE: 10% • ITE: 46% • ITC: 27% • CIC: 17% • Unilateral: 5% • Programmable analog: 88% |
205 | 74 Range: 41–95 |
||
| Duijvestijn et al. (2003) | Attitude towards HA (OQ) Source of motivation (OQ) Self-reported hearing (OQ) Hearing sensitivity (PTA) Age Gender |
o + + o o o |
NIDD | 281 | 69.5 | ||||
| Eriksson-Mangold et al. (1990) | Counselling: fitting program | (OQ) + |
(OQ) + |
RCT 10 months post |
In both groups 64% binaural | Exp group: 25 Controls: 22 |
68.6 (4.9) 68.5 (5.1) |
||
| Garstecki & Erler (1998) | Hearing sensitivity (PTA) Personality: Locus of internal control (Rotter's Int-Ext scale), Ego strength (MMPI-2) Concerns re. cost (HAM) Attitude towards HL: Acceptance of hearing loss (CPHI) SES: income satisfaction |
+ + + − + + |
NIDD | 131 Group FA: 35 Group FN: 33 Group MA: 25 Group NM: 38 |
75.5 (5.2) 75.5 (6.3) 75.2 (6.2) 71.9 (5.4) |
||||
| Gatehouse (1994) | Attitude towards HA (OQ) Expectations (IDI) Personality (CCEI): Depression Obsession Hysteria Hearing sensitivity (PTA) Age Gender |
(IDI) + o − + + o o |
(IDI) + + − − + o o o |
NIDD | BTE linear devices | 309 46% male |
66.5 (9) | ||
| Gussekloo et al. (2003) | Hearing sensitivity (PTA) Self-reported hearing (HHDI) Age Gender Married status Living relations SES: Income level Educational level Cognitive (MMSE) Subjective health Feelings of loneliness Depression (GDS-IS) |
+ + o o o o o o o o o o |
NRIS | 454 | 85 | ||||
| Helvik et al. (2008) | Age Gender Hearing sensitivity (PTA) Educational level (NS) Living relations Duration of hearing loss Self-reported hearing (HHDI) Attitude towards own HL: Maladaptive behavior (CSS) |
+ o + − o o + − |
NIDD 1.5 yr post fitting |
173 | 67.6 (12.0) | ||||
| Henrichsen et al. 1988 | Age | (OQ) o |
(OQ) o |
NIDD | All ITE-HA 37% binaural |
693 | Median: 74 Range: 18–91 |
||
| Hickson et al. (1986) | Source of motivation Attitude towards HA (The Attitude Scale Age Gender Living relations Hearing sensitivity (PTA) Dexterity (impression audiologist) First impression of HA (impression audiologist) Satisfaction with audiologist |
o + o o o o + o o |
NIDD (Pre and 3 to 9 months post) |
98% BTE 66% monaural |
135 | 95% >60 | |||
| Hickson et al. (1999) | Source of motivation Attitude towards HA (The Attitude Scale) Age Gender Living relations (HAUQ) Hearing sensitivity (PTA) Cosmetic appearance (HAUQ) |
+ o o o o o |
(HAUQ) + o o o o o + |
NIDD 3–9 months postfitting) |
All Bernafon PHOX programmer 12% BTE 86% ITE 58% monaurally |
52 69% male |
63.2 (8.9) | ||
| Hosford-Dunn & Halpern (2001) | Self-reported hearing (SADL) Hearing sensitivity (PTA) Lifetime experience with hearing aids (SADL) Age |
+ + + o |
(SADL) + + + − |
NIDD 1 year post-fit |
282 | 76 (12.8) Range: 61–101 |
|||
| Humes et al. (2002) | Adaptation period | − | (HAPI, HHIE) − |
NIDD Pre & post 86 mo, 1 yr, & 2 yrs) |
ITE | 134 | 73 Range: 60–89 |
||
| Humes et al. (2003) | Attitude towards hearing loss (CPHI): Problem awareness Denial Self acceptance Distress Expectations (Expectations Checklist) Educational level SES Living relations Amount of social interaction (SI) Age of onset of HL Self-reported hearing (HHIE) Dexterity General health attitude Speech reading |
+ + − + o o o o o + o o o |
NRIS Three groups matched for age, gender, and hearing loss |
All in groups 2 and 3 were fitted binaurally with identical full-concha ITE HA with linear class D amplifiers with output limiting compression | Group 1: 26; Group 2: 24; Group 3: 26 | Range: 60–89 73.8 76.5 73.1 |
|||
| Humphrey et al. (1981) | Age Gender Socioeconomic status Hearing sensitivity (PTA) Onset hearing loss (pre or post retirement) |
o o o + − |
NIDD pre (comparison of 4 group |
NHS hearing aids | 136 71% 70–79 yr 29% > 80 yr 49% male |
>70 | |||
| Jerram & Purdy (2001) | Expectations (Seyfrieds Questionnaire) Attitude towards hearing loss/Acceptance of hearing loss (CPHI) Attitudes towards HA (HARQ) Age Gender Hearing sensitivity (PTA) SES (employment status) Type of clinic (private vs public) |
+ + o o o o o o |
(VAS) o o o o o o o |
NIDD Pre and post 10 weeks) |
162 | 70.5 (10.8) | |||
| Kapteyn et al. (1997) | Counselling: Post-fitting, Home visit during trial period | + | NRIS pre and post (6 months) |
Total: 87 Exp group: 62; Controls: 25 |
72.0 | ||||
| Kemker & Holmes (2004) | Counseling programme | (GHABP) + |
RCT 3 groups pre and post (5 weeks) |
Conventional analogue hearing aids | Pre-fit: 15 Post-fit: 15 Controls: 15 |
69.5 (6.1) 70.3 (5.6) 72.1 (5.7) |
|||
| Kricos et al. (2007) | Number of major life events (CLE/OQ) Personality: Optimism (LOT) |
(non use vs use) + o |
NIDD post, questionnaires | 197 | 73.2 Range: 36–96 |
||||
| Lupsakko et al. (2005) | Gender SES: Income Activity of daily living (The Barthel ADL Index) |
o o − − |
NIDD 3 groups: -full-time users -more than 1 year -part-time users and nonusers |
No info | 100 with HA: 36% male 501 without HA 24% male |
83 (5) 81 (4) |
|||
| Mulrow et al. (1992) | Medication Self-reported hearing (HHIE) Age |
(OQ) − |
(HAS) + − |
NIDD Two groups, pre and post (4 months) |
No info | 95 | 73 | ||
| Munro & Lutman (2004) | Adaptation period | (GHABP) o |
(GHABP) + |
NRIS Pre and post (9–12 weeks) |
Phonak, sonoforte, 33IX-L PICS All BTE All monaural |
32 | |||
| Norman et al. (1994) | Counselling programme: Pre-fitting Hearing sensitivity (PTA) Age Gender |
o o o o |
(VAS) o o o o |
NRIS 2 groups matched for age, gender, hearing loss |
Exp group: 48 Controls: 47 |
90% >65 81 % >65 |
|||
| Norman et al. (1995) | Counselling: Post-fitting (communication course) | o | (VAS) + |
NRIS Matched groups pre and 3 months post |
NHS BTE | Exp group: 48* Controls: 47 |
69.5 (10.8) 70.1 (1 1.3) |
||
| Öberg et al. (2008) | Counseling: pre-fitting programme | (IOI-HA) o |
(SADL) o |
RCT pre and post (1 year) | Bilateral digital aids | Exp group: 16; Controls: 18 | 67 (7.4) | ||
| Swan & Gatehouse (1990) | Self-reported hearing (OQ) Hearing sensitivity (PTA) |
+ + |
NIDD | 2 groups: consulters: 269 non-consu Iters: 286 |
64 Range: 15–90 60 Range: 17–88 |
||||
| Saunders & Jutai (2004) | Lifetime experience with hearing aids (SADL) | (SADL) + |
NIDD 3 groups, pre- to post- (6–20 weeks) |
Not provided | 92 | 69.3 (6.5) | |||
| Takashi (2007) | Self-reported hearing (IOI-HA) | (GHABP) + |
(GHABP) + |
NIDD 6 yrs post fitting measure |
Not provided | 164 Mean: 73.2 (range 36–96) |
|||
| Uriarte et al. (2005) | Age Gender Hearing sensitivity (PTA) Lifetime experience with hearing aids (SADL) Self-reported hearing (CSS/OQ) Satisfaction with hearing aid professional (CSS/OQ) |
(SADL) o o + + + + |
NIDD | Digitally programmable aids 54.4% binaural |
(1014) 813 completed SADL 54% male |
75.3 (9.7) | |||
| van den Brink et al. (1996) | Attitude towards HA (AQ) Age Gender Hearing sensitivity (PTA) Self-reported hearing (HHDI/OQ) |
o o + + |
+ | NIDD including -non-consu Iters -consulters not pursuing HA -HA-users |
624 | 68.9 (7.6) | |||
| Wilson & Stephens (2003) | Source of motivation Attitude toward HA (audiologist's assessment) Dexterity: manipulative skills (audiologist's assessment) |
o + + |
(VAS) o + o |
NIDD Survey + intervention including 3 months follow-up measure |
96% BTE | 140 | 72 (1 1.8) | ||
| Wong et al. (2004) | Expectations (HAOQ/OQ) | (HAOQ) o |
NIDD | Analogue aids 68% BTE 19% body 13% ITE, ITC, CIC |
36 Chinese speaking | 65.8 Range: 23–86 |
|||
The item about satisfaction and hearing aid usage in Norman et al. (1995) was measured for two matched groups with 20 participants in each group
NS = Not Specified in the article, SI = Separate Item, OQ = Own Questionnaire, PTA, Pure-Tone Average for hearing threshold, HL = Hearing Loss, SES = Socio-Economic Status
Declaration of Conflicting Interests
The author(s) declared that they had no conflicts of interest with respect to their authorship or the publication of this article.
Funding
The author(s) disclosed that they received the following support for their research and/or authorship of this article: The contributions of authors M. Öberg and S. E. Kramer to this study were made possible by a grant from the Oticon Foundation.
Note
Goldstein and Stephens (1981; not in the table) classified four different “Attitude Types” commonly found among people in the prefitting stage: (a) strongly positive, (b) essentially positive/though complications are present, (c) fundamentally negative/though cooperative intent, and (d) rejective. Based on their clinical experience (rather than empirical data), Goldstein and Stephens argued that each type has its own predictive value toward the prospect of getting engaged in clinical hearing rehabilitation.
Questionnaires
The Attitude Scale (Goldstein & Stephens, 1981)
AQ, The Attitude Questionnaire (van den Brink, 1995)
The Barthel ADL Index (Wade & Collin, 1988)
CCEI, Crown-Crisp Experiential Index (Crown & Crisp, 1979)
CLE Checklist of Life Events (Kricos et al., 2007).
CPHI, Communication Profile for the Hearing Impaired (Demorest & Erdman, 1987)
CSS Communication Strategies Scale, subscale in the CPHI see above
CSS, Client Satisfaction Survey (Uriarte et al., 2005) ∗The questionnaire is adapted from the HAUQ.
ECHO, Expected Consequences of Hearing Aid Ownership (Cox & Alexander, 2000)
EC, Expectations Checklist (Bentler, Niebuhr, Getta, & Anderson, 1993)
GDS-15 Geriatric Depression Scale (Yesavage et al., 1982)
GHABP, Glasgow Hearing Aid Benefit Profile (Gatehouse, 1997)
HAM, Hearing Aid Management questionnaire (Garstecki, 1994)
HAOQ, Hearing Aid Outcomes Questionnaire (Wong et al., 2004)
HAR, Hearing Aid Review (Brooks, 1989)
HARQ Hearing Attitude in Rehabiliation Questionaire (Hallam & Brooks, 1996)
HAS Hearing Aid Satisfaction (Lazenby, Logan, Ahlstrom, & Bess, 1986)
HAUQ, Hearing Aid User's Questionnaire (Forster & Tomlin, 1988)
HHIE, Hearing Handicap Inventory for the Elderly (Ventry, & Weinstein, 1982)
HDHS, Hearing Disability and Handicap Scale (Hetu et al., 1994)
HHDI, The Hearing Handicap and Disability Inventory (Brink, van den, 1995)
IDI, Initial Disability Interview (Gatehouse, 1993)
IOI-HA, International Outcome Inventory for Hearing Aids (Cox et al., 2000)
LOT, Life Orientation Test (dispositional optimism; Kricos et al., 2007)
MMPI, Minnesota Multiphasic Personality Inventory Depression scale (Hathaway & McKinley, 1940)
MMSE Mini-Mental State Examination (Tombaugh & McIntyre, 1992)
NEO-FFI, Neuroticism, Extraversion, Openness-Five Factor Inventory (Costa & McCrae, 1997)
NHHI, The Nursing Home Handicap Index (Schow & Nerbonne, 1977)
PHAB, Profile of Hearing Aid Benefit (Cox et al., 1991)
Rotter's Internal-External scale (Rotter, 1966)
SADL, Satisfaction with Amplification in Daily Life (Cox & Alexander, 1999)
Seyfrieds Questionnaire (Seyfried, 1990)
SOC, Sense of Coherence Scale (Antonovsky, 1987)
References
- Antonovsky A. (1987). Unravelling the mystery of health. San Francisco: Jossey-Bass [Google Scholar]
- Bandura A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs NJ: Prentice-Hall [Google Scholar]
- Bandura A. (1989). Human agency in social-cognitive theory. American Psychologist, 44, 1175–1184 [DOI] [PubMed] [Google Scholar]
- Bentler R., Kramer S. E. (2000). Guidelines for choosing a self-report outcome measure. Ear and Hearing, 21, 37S–49S [DOI] [PubMed] [Google Scholar]
- Bentler R., Niebuhr D., Getta J., Anderson C. (1993). Longitudinal study of hearing aid effectiveness. II: Subjective measures. Journal of Speech and Hearing Research, 36, 820–831 [DOI] [PubMed] [Google Scholar]
- Boothroyd A. (2007). Adult Aural Rehabilitation: What is it and does it work? Trends in Amplification, 11, 63–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brickley G., Cleaver V., Bailey S. (1996). An evaluation of a group follow-up scheme for new NHS hearing aid users. British Journal of Audiology, 30, 307–312 [DOI] [PubMed] [Google Scholar]
- Brooks D. N. (1989). The effect of attitude on benefit obtained from hearing aids. British Journal of Audiology, 23, 3–11 [DOI] [PubMed] [Google Scholar]
- Brooks D. N., Hallam R. S. (1998). Attitudes to hearing difficulty and hearing aids and the outcome of audiological rehabilitation. British Journal of Audiology, 32, 217–226 [DOI] [PubMed] [Google Scholar]
- Carson A. J., Pichora-Fuller M. K. (1997). Health promotion and audiology: The community-clinic link. Journal of the Academy of Rehabilitation Audiology, 30, 29–51 [Google Scholar]
- Chang W. H., Tseng H. C., Chao T. K., Hsu C. J., Liu T. C. (2008). Measurement of hearing aid outcome in the elderly: Comparison between young and old elderly. Otolaryngology-Head and Neck Surgery, 138, 730–734 [DOI] [PubMed] [Google Scholar]
- Cherry R., Rubinstein A. (1994). The effect of telephone intervention on success with amplification. Ear and Hearing, 15, 256–261 [DOI] [PubMed] [Google Scholar]
- Clark J. (2007). Patient-centered practice: Aligning professional ethics with patient goals. Seminars in hearing, 28, 163–170 [Google Scholar]
- Cook D. J., Mulrow M. D., Haynes R. B. (1997). Systematic reviews: Synthesis of best evidence for clinical decisions. Annals of Internal Medicine, 126, 376–380 [DOI] [PubMed] [Google Scholar]
- Costa P. T., Jr., McCrae R. R. (1997). Longitudinal stability in adult personality. In Hogan R., Johnson J., Briggs S. (Eds.), Handbook of personality psychology (pp. 269–293). San Diego, CA: Academic Press [Google Scholar]
- Cox R. (2005). Evidence-based practice in provision of amplification. Journal of the American Academy of Audiology, 16, 419–438 [DOI] [PubMed] [Google Scholar]
- Cox R. M., Alexander C. G. (1999). Measuring satisfaction with amplification in daily life: The SADL scale. Ear and Hearing, 20, 306–320 [DOI] [PubMed] [Google Scholar]
- Cox R. M., Alexander G. C. (2000). Expectations about hearing aids and their relationship to fitting outcome. Journal of the American Academy of Audiology, 11, 368–382 [PubMed] [Google Scholar]
- Cox R. M., Alexander G. C., Beyer C. M. (2003). Norms for the international outcome inventory for hearing aids. Journal of the American Academy of Audiology, 14, 403–413 [PubMed] [Google Scholar]
- Cox R. M., Alexander G. C., Gray G. A. (2005). Who wants a hearing aid? Personality profiles of hearing aid seekers. Ear and Hearing, 26, 12–26 [DOI] [PubMed] [Google Scholar]
- Cox R. M., Alexander G. C., Gray G. A. (2007). Personality, hearing problems, and amplification characteristics: Contributions to self-report hearing aid outcomes. Ear and Hearing, 28, 141–162 [DOI] [PubMed] [Google Scholar]
- Cox R. M., Gilmore C., Alexander G. C. (1991). Comparison of two questionnaires for patient-assessed hearing aid benefit. Journal of the American Academy of Audiology, 2, 134–145) [PubMed] [Google Scholar]
- Cox R., Hyde M., Gatehouse S., Noble W., Dillon H., Bentler R., et al. (2000). Optimal outcome measures, research priorities, and international cooperation. Ear and Hearing, 21, 106S–115S [DOI] [PubMed] [Google Scholar]
- Crown S., Crisp A. H. (1979). Manual of the Crown-Crisp Experiential Index. London: Hodder & Stoughton [Google Scholar]
- Davis A., Smith P., Ferguson M., Stephens D., Gianopoulos I. (2007). Acceptability, benefit and costs of early screening for hearing disability: A study of potential screening tests and models. Health Technology Assessment, 11, 1–294 [DOI] [PubMed] [Google Scholar]
- Demorest M. E., Erdman S. A. (1987). Development of the Communication Profile for the Hearing Impaired. Journal of Speech and Hearing Disorder, 52, 129–143 [DOI] [PubMed] [Google Scholar]
- Dillon H., Birtles G., Lovegrove R. (1999). Measuring the outcomes of a national rehabilitation program. Normative data for the Client Oriented Scale of Improvement (COSI) and the Hearing Aid Users's Questionnaire. Journal of the American Academy of Audiology 10, 67–79 [Google Scholar]
- Duijvestijn J. A., Anteunis L. J., Hoek C. J., van Den Brink R. H. S., Chenault M. N., Manni J. J. (2003). Help-seeking behaviour of hearing-impaired persons aged ≥ 55 years; effect of complaints, significant others and hearing aid image. Acta Otolaryngology, 123, 846–850 [DOI] [PubMed] [Google Scholar]
- Engelund G. (2006). “Time for hearing”—Recognising process for the individual: A grounded theory. Unpublished doctoral dissertation, University of Copenhagen, Denmark [Google Scholar]
- English K. (2005). Get ready for the next big thing in audiologic counseling. Hearing Journal, 58, 10–15 [Google Scholar]
- Eriksson-Mangold M., Ringdahl A., Björklund A. K., Wåhlin B. (1990). The active fitting (AF) programme of hearing aids: A psychological perspective. British Journal of Audiology, 24, 277–285 [DOI] [PubMed] [Google Scholar]
- Forster S. E., Tomlin A. J. (1988, May). Hearing aid usage in Queensland. Paper presented at the Audiological Society of Australia Conference, Perth, Australia.
- Garstecki D. C. (1994). Perception of (psychological) control and competence: A basis for behavioral differences in management of hearing loss by aging adults. Chicago: Retirement Research Foundation [Google Scholar]
- Garstecki D. C., Erler S. F. (1998). Hearing loss, control, and demographic factors influencing hearing aid use among older adults. Journal of Speech, Language, and Hearing Research, 41, 527–537 [DOI] [PubMed] [Google Scholar]
- Gatehouse S. (1990). The role of non-auditory factors in measured and self-reported disability. Acta Otolaryngology, 476, 249–256 [PubMed] [Google Scholar]
- Gatehouse S. (1993). Hearing aid evaluation: Limitation of present procedures and future requirements [Monograph supplement]. Journal of Speech-Language Pathology and Audiology, 1, 50–57 [Google Scholar]
- Gatehouse S. (1994). Components and determinants of hearing aid benefit. Ear and Hearing, 15, 30–49 [DOI] [PubMed] [Google Scholar]
- Gatehouse S. (1997). Approaches to the evaluation of the benefits provided by hearing aids and other rehabilitation services. Paper presented at the Annual Summer Institute of the Academy of Rehabilitative Audiology, Magog, Quebec.
- Gianopoulos I., Stephens D. (2005). General considerations about screening and their relevance to adult hearing screening. Audiological Medicine, 3, 165–174 [Google Scholar]
- Goldstein D. P., Stephens S. D. G. (1981). Audiological Rehabilitation: Management model I. Audiology, 20, 432–452 [DOI] [PubMed] [Google Scholar]
- Grutters J. P., Van der Horst F., Joore M. A., Verschuure H., Dreschler WA., Anteunis L. J. (2007). Potential barriers and facilitators for implementation of an integrated care pathway for hearing-impaired persons: An exploratory survey among patients and professionals. BMC Health Services Research, 7, 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grutters J. P., Joore M. A., Kessels A. G., Davis A. C., Anteunis L. J. (2008). Patient preferences for direct hearing aid provision by a private dispenser. A discrete choice experiment. Ear and Hearing, 29, 557–564 [DOI] [PubMed] [Google Scholar]
- Gussekloo J., de Bont L. E. A., von Faber M., Eekhof J. A. H., de Laat J. A. P.M., Hulshof J. H., et al. (2003). Auditory rehabilitation of older people from the general population—The Leiden 85-plus Study. British Journal of General Practice, 53, 536–540 [PMC free article] [PubMed] [Google Scholar]
- Hallam R. S., Brooks D. N. (1996). Development of the hearing attitudes in rehabilitation questionnaire. (HARQ). British Journal of Audiology, 30, 199–213 [DOI] [PubMed] [Google Scholar]
- Hathaway S. R., Mc Kinley J. C. (1940). A Multiphasic personality schedule (Minnesota) I. Construction of the schedule. Journal of Psychology, 10, 249–254 [Google Scholar]
- Henrichsen J., Noring E., Christensen B., Pedersen F., Parving A. (1988). In-the-ear hearing aids. The Use and Benefit in the Elderly Hearing-Impaired. Scandinavian Audiology, 17, 209–212 [DOI] [PubMed] [Google Scholar]
- Hickson L., Hamilton L., Orange S. P. (1986). Factors associated with hearing aid use. Australian Journal of Audiology, 8, 37–41 [Google Scholar]
- Hickson L., Timm M., Worrall L. (1999). Hearing aid fitting: Outcomes for older adults. Australian Journal of Audiology, 21, 9–21 [Google Scholar]
- Hickson L., Worrall L. (2003). Beyond hearing aid fitting: Improving communication for older adults. International Journal of Audiology. 2003. Jul; 42 Suppl 2: 2S84–91 [PubMed] [Google Scholar]
- Helvik A. S., Wennberg S., Jacobsen G., Hallberg L. R. M. (2008). Why do some individuals with objectively verified hearing loss reject hearing aids? Audiological Medicine, 6, 141–148 [Google Scholar]
- Hetu R., Getty L., Philibert L., Desilets F., Noble W., Stephens D. (1994). Development of a clinical tool for the measurement of the severity of hearing disabilities and handicaps. Journal of Speech-Lang Pathology and Audiology, 18, 82–95 [Google Scholar]
- Hosford-Dunn H., Halpern J. (2001). Clinical application of the SADL scale in private practice II: Predictive validity of fitting variables. Journal of the American Academy of Audiology, 12, 15–36 [PubMed] [Google Scholar]
- Humes L. E., Wilson D. L., Barlow N. N., Garner C. (2002). Longitudinal changes in hearing aid satisfaction and usage in the elderly over a period of one or two years after hearing aid delivery. Ear and Hearing, 23, 428–438 [DOI] [PubMed] [Google Scholar]
- Humes L. E., Wilson D. L., Humes A. C. (2003). Examinations of differences between successful and unsuccessful elderly hearing aid candidates matched for age, hearing loss and gender. International Journal of Audiology, 42, 432–441 [DOI] [PubMed] [Google Scholar]
- Humphrey C., Gilhome Herbst K., Faurqi S. (1981). Some characteristics of the hearing-impaired elderly who do not present themselves for rehabilitation. British Journal of Audiology, 15, 25–30 [DOI] [PubMed] [Google Scholar]
- Jerram J. C. K., Purdy S. C. (2001). Technology, expectations, and adjustment to hearing loss: Predictors of hearing aid outcome. Journal of American Academy of Audiology, 12, 64–79 [PubMed] [Google Scholar]
- Jones L., Kyle J. G., Wood P. L. (1987). Words apart: Adjustment to hearing loss in adult life. London: Tavistock Press [Google Scholar]
- Kargas S., Doyle J. (1996). Patient satisfaction with time use in audiological consultations. British Journal of Audiology, 30, 355–361 [DOI] [PubMed] [Google Scholar]
- Kapteyn T. S., Wijkel D., Hackenitz E. (1997). The effects of involvement of the general practitioner and guidance of the hearing impaired on hearing-aid use. British Journal of Audiology, 31, 399–407 [DOI] [PubMed] [Google Scholar]
- Kemker B. E., Holmes A. E. (2004). Analysis of prefitting versus hearing aid orientation using the Glasgow Hearing Aid Benefit Profile (GHABP). Journal of American Academy of Audiology, 15, 311–323 [DOI] [PubMed] [Google Scholar]
- Kiessling J., Pichora-Fuller M. K., Gatehouse S., Stephens D., Arlinger S., Chisolm T., Davis A. C., Erber N. P., Hickson L., Holmes A., Rosenhall U., von Wedel Candidature H. For and delivery of audiological services: Special needs of older people. International Journal of Audiology. 2003 Jul;42 Suppl 2:2S92–101 [PubMed] [Google Scholar]
- Kirkwood D. H. (2005). Dispenser surveyed on what leads to patient satisfaction. Hearing Journal, 58(4), 19–26 [Google Scholar]
- Kochkin S. (1997). Subjective measures of satisfaction and benefit. Establishing norms. Seminars in Hearing, 18, 37–48 [Google Scholar]
- Kochkin S. (1998). MarkeTrak IV: Correlates of hearing aid purchase intent. Hearing Journal, 51(1), 30–38 [Google Scholar]
- Kochkin S. (2004). BHI physician program found to increase use of hearing health care. Hearing Journal, 57(8), 27–29 [Google Scholar]
- Kochkin S. (2007). Marketrak VII: obstacles to adult non-user adoption to hearing aids. Hearing Journal, 60(4) [Google Scholar]
- Kricos P. (2000). The influence of nonaudiological variables on audiological rehabilitation outcomes. Ear Hear, 21, 7S–14S [DOI] [PubMed] [Google Scholar]
- Kricos P. B. (2006). Processing Capabilities Audiologic Management of Older Adults With Hearing Loss and Compromised Cognitive/Psychoacoustic Auditory. Trends in Amplification, 10(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kricos P. B., Erdman S., Bratt G. W., Williams D. W. (2007). Psychosocial correlates of hearing aid adjustment. Journal of American Academy of Audiology, 18, 304–322 [DOI] [PubMed] [Google Scholar]
- Lazenby B. B., Logan S. A., Ahlstrom J. B., Bess F. H. (1986). Self-assessment questionnaire for the elderly: Hearing aid dispensary use. Hearing Journal, 39, 18–21 [Google Scholar]
- Lupsakko T. A., Kautiainen H. J., Sulkava R. (2005). The nonuse of hearing aids in people aged 75 years and over in the city of Kuopio in Finland. European Archive of Otorhinolaryngology, 262, 165–169 [DOI] [PubMed] [Google Scholar]
- Meis M., Gabriel B. (2006). Barriers in hearing instrument provision—From a customer perspective. In Proceedings of the 51th International Congress of Hearing Aid Acousticians, Frankfurt am Main, Germany.
- Mulrow C. D., Tuley M. R., Aguilar C. (1992). Correlates of Succesful Hearing Aid Use in Older Adults. Ear and Hearing, 13(2), 108–113 [DOI] [PubMed] [Google Scholar]
- Munro K. J., Lutman M. E. (2004). Self-reported outcome in new hearing aid users over a 24-week post-fitting period. International Journal of Audiology, 43, 555–562 [DOI] [PubMed] [Google Scholar]
- Norman M. G., George C. R., McCarthy D. (1994). The effect of pre-fitting counselling on the outcome of hearing aid fittings. Scandinavian Audiology, 23, 257–263 [DOI] [PubMed] [Google Scholar]
- Norman M., George CR., Downie A., Milligan J. (1995). Evaluation of a communication course for new hearing aid users. Scandinavian Audiology, 24, 63–69 [DOI] [PubMed] [Google Scholar]
- Öberg M. (2008). Approaches to audiological rehabilitation with hearing aids-studies on pre-fitting strategies and assessment of outcomes. Unpublished doctoral dissertation, University of Linköping, Sweden.
- Öberg M., Andersson G., Wänström G., Lunner T. (2008). The effects of a sound awareness pre-fitting intervention: A randomized controlled trial. Audiological Medicine, 6, 129–140 [Google Scholar]
- Popelka M. M., Cruickshanks K. J., Wiley T. L., Tweed T. S., Klein B. E., Klein R. (1998). Low prevalence of hearing aid use among older adults with hearing loss: The epidemiology of hearing loss study. Journal American Geriatrics Society, 46, 1075–1078 [DOI] [PubMed] [Google Scholar]
- Rotter J. B. (1966). Generalized expectancies for internal versus external control of reinforcement. Psychological Monograph, 80, 1–28 [PubMed] [Google Scholar]
- Saunders G. H., Cienkowski K. M. (1996). Refinement and psychometric evaluation of the Attitudes Toward Loss of Hearing questionnaire. Ear and Hearing, 17, 505–519 [DOI] [PubMed] [Google Scholar]
- Saunders G. H., Jutai J. W. (2004). Hearing specific and generic measures of the psychosocial impact of hearing aids. Journal of American Academy Audiology, 15, 238–248 [DOI] [PubMed] [Google Scholar]
- Schow R. L., Nerbonne M. A. (1977). Assessment of hearing handicap by nursing home residents and staff. Journal of the Academy of Rehabilitative Audiology, 10, 2–12 [Google Scholar]
- Schumacher D. U., Carruth J. A. (1997). Long-term use of hearing aids in patients with presbyacusis. Clinical Otolaryngology & Allied Science, 22, 430–433 [PubMed] [Google Scholar]
- Seyfried D. A. (1990). Use of a communication self-report inventory to measure hearing aid counseling effects. Unpublished doctoral dissertation, University of Iowa, Iowa City, IA [Google Scholar]
- Smeeth L., Fletcher A. E., Ng E. S., Stirling S., Nunes M., Breeze E., et al. (2002). Reduced hearing, ownership, and use of hearing aids in elderly people in the UK—The MRC Trial of the Assessment and Management of Older People in the Community: A cross-sectional survey. Lancet, 359, 1466–1470 [DOI] [PubMed] [Google Scholar]
- Smith P., Mack A., Davis A. (2008). A multicenter trial of an assess-and-fit hearing aid service using open canal fittings and comply ear tips. Trends in Amplification, 12(2), 121–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits C., Kramer S. E., Houtgast T. (2006). Speech-reception-thresholds in noise and self-reported hearing disability in a general adult population. Ear and Hearing, 27, 538–549 [DOI] [PubMed] [Google Scholar]
- Souza P. E., Yueh B., Sarubbi M., Loovis C. F. (2000). Fitting hearing aids with the Articulation Index: Impact on hearing aid effectiveness, Journal Rehabilitation Research Development, 37, 473–481 [PubMed] [Google Scholar]
- Stephens D. (1989). GPs and the fitting of hearing aids. Clinical Otolaryngology & Allied Science, 14, 481–484 [DOI] [PubMed] [Google Scholar]
- Stephens S. D., Callaghan D. E., Hogan S., Meredith R., Rayment A., Davis A. C. (1990). Hearing disability in people aged 50–65: Effectiveness and acceptability of rehabilitative intervention. British Medical Journal, 300, 508–511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan I. R. C., Gatehouse S. (1990). Factors influencing consultation for management of hearing disability. British Journal of Audiology, 24, 155–160 [DOI] [PubMed] [Google Scholar]
- Takahashi G., Martinez C. D., Beamer S., Bridges J., Noffsinger D., Sugiura K., et al. (2007). Subjective measures of hearing aid benefit and satisfaction in the NIDCD/VA follow-up study. Journal of American Academy Audiology, 18, 323–349 [DOI] [PubMed] [Google Scholar]
- Tombaugh T. N., McIntyre N. J. (1992). The mini-mental state examination: A comprehensive review. Journal of American Geriatric Society, 40, 922–935 [DOI] [PubMed] [Google Scholar]
- Tsuruoka H., Masuda S., Ukai K., Sakakura Y., Harada T., Majima Y. (2001). Hearing impairment and quality of life for the elderly in nursing homes. Auris Nasus Larynx, 28, 45–54 [DOI] [PubMed] [Google Scholar]
- Uriarte M., Denzin L., Dunstan A., Sellars J., Hickson L. (2005). Measuring hearing aid outcomes using the Satisfaction with Amplification in Daily Life (SADL) Questionnaire: Australian data. Journal of American Academy Audiology, 16, 383–402 [DOI] [PubMed] [Google Scholar]
- van den Brink R. H. S., Wit H. P., Kempen G. I. J.M., van Heuvelen M. J. G. (1996). Attitude and help-seeking for hearing impairment. British Journal of Audiology, 30, 313–324 [DOI] [PubMed] [Google Scholar]
- van den Brink R. H. S. (1995). Attitude and illness behaviour in hearing impaired elderly. Unpublished doctoral dissertation, University of Groningen, Groningen, the Netherlands.
- Ventry I. M., Weinstein B. E. (1982). The hearing handicap inventory for the elderly: A new tool. Ear and Hearing, 3, 128–134 [DOI] [PubMed] [Google Scholar]
- Wade D. T., Collin C. (1988). The Barthel ADL Index: A standard measure of physical disability? International Disability Studies, 10, 64–67 [DOI] [PubMed] [Google Scholar]
- Weinstein B. (2000). Geriatric audiology. New York: Thieme [Google Scholar]
- Wilson C., Stephens D. (2003). Reasons for referral and attitudes toward hearing aids: Do they affect outcome? Clinical Otolaryngology, 28, 81–84 [DOI] [PubMed] [Google Scholar]
- Wong L. N., Hickson L., McPherson B. (2003). Hearing aid satisfaction: What does research from the past 20 years say? Trends in Amplification, 7, 116–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong L. N., Hickson L., McPherson B. (2004). Hearing aid expectations among Chinese first-time users: Relationships to post-fitting satisfaction. Australian and New Zealand Journal of Audiology, 26, 53–69 [Google Scholar]
- Yesavage J. A., Brink T. L., Rose T. L., Lum O., Huang V., Adey M., et al. (1982). Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research, 17(1), 37–49 [DOI] [PubMed] [Google Scholar]