Abstract
A discussion of the protocols used particularly in the clinical application of the Desired Sensation Level (DSL) Method is presented in this chapter. In the first section, the measurement and application of acoustic transforms is described in terms of their importance in the assessment phase of the amplification fitting process. Specifically, the implications of individual ear canal acoustics and their impact on accurately defining hearing thresholds are discussed. Detailed information about the statistical strength of the real-ear-to-coupler difference (RECD) measurement and how to obtain the measure in young infants is also provided. In addition, the findings of a study that examined the relationship between behavioral and electrophysiologic thresholds in real-ear SPL is described. The second section presents information related to the electroacoustic verification of hearing instruments. The RECD is discussed in relation to its application in simulated measurements of real-ear hearing instrument performance. In particular, the effects of the transducer and coupling method during the RECD measurement are described in terms of their impact on verification measures. The topics of insertion gain, test signals, and venting are also considered. The third section presents three summary tables that outline the hearing instrument fitting process for infants, children, and adults. Overall, this chapter provides both clinical and scientific information about procedures used in the assessment and verification stages of the DSL Method.
Assessment Measures
Measuring and Applying Acoustic Transforms
The first stage of the hearing instrument fitting process defines the audiometric thresholds and converts them to ear canal sound pressure levels so that they may be compared with hearing instrument measurements in later stages of the fitting process. At this stage, the Desired Sensation Level (DSL) Method considers both the acoustic and audiometric characteristics of the patient to be fitted with amplification. Whether the patient is an infant or an adult, ear-specific and frequency-specific hearing thresholds must be collected before the prescription is calculated (Cox, 1985; Pediatric Working Group, 1996). In addition, it is recommended that ear canal acoustics be measured at this stage so that audiometric thresholds can be converted accurately to ear canal sound pressure level (SPL). This chapter will describe the relevant information supporting the measurement and application of individual ear canal acoustics in the assessment stage of the amplification process. Special considerations related to audiometric characteristics at this stage will also be provided.
A key aspect of the DSL Method is the application of ear canal acoustics in the process of hearing instrument fitting. With the introduction of real-ear measurement systems in the mid-to-late 1980s, researchers and clinicians were encouraged by the possibilities they offered. In fact, clinical procedures were developed and implemented in the DSL Method with the goal of individualizing hearing instrument prescription and fitting to children. The main focus of this work was the development and validation of protocols that applied the real-ear-to-coupler difference (RECD) as a fundamental component of the pediatric hearing instrument fitting process. The relevant literature describing these protocols and the current status of normative RECD data will be summarized within the sections below.
Hearing Level (HL) to Sound Pressure Level (SPL) Transforms
The DSL Method takes a specific approach in accounting for age-related variance in audiometric data. Specifically, the prescription algorithm does not use data in the HL scale in its calculations. Instead, it converts HL data to the ear canal SPL before the prescription is computed. This approach is specifically included in DSL to circumvent the issue of ear canal growth in childhood: as the child's ear grows, the HL required to generate a given SPL in the ear canal will increase. Therefore, lack of precision at the assessment stage can result in amplified speech signals that are inappropriate in shape or level, or a hearing instrument maximum SPL that exceeds the threshold for loudness discomfort.
The next section will describe the measurement concepts required to adequately address this issue of age-related ear canal acoustics in audiometric assessment, summarize the relevant research, and provide a clinical approach that can be applied with both pediatric and adult populations.
Audiometric Calibration and Prescriptive Targets
When an audiometer is calibrated, the levels from each audiometric transducer are adjusted until all test frequencies are presented at levels approximating the normal threshold of hearing when presented at 0 dB HL. These levels, termed the reference equivalent threshold sound pressure level (RETSPL), are defined specifically for each audiometric transducer and cannot be interchanged (ANSI S3.6, 1996). The standardization of the dB HL scale allows for consistent definitions of hearing levels across clinics, stimuli, and clinicians. The 1996 version of this standard is harmonized with that of the International Standards Organization, creating a consistent definition of the HL scale across nations (International Standards Organization, 1996).
Despite the advantages of having a standardized scale for hearing levels, some challenges exist in pediatric practice. Specifically, one of the primary disadvantages of defining hearing loss by using a dB HL reference is that the RETSPL is defined relative to the average of the normal hearing adult population. Therefore, the HL scale does not accurately reflect the audiometric threshold values in ear canal SPL for an individual, particularly if the individual has unusual external ear canal resonances. For children, the average adult's difference between the HL and ear canal SPL will underestimate that of the child's ear canal. For example, for a given HL value, the SPL in a child's ear can be up to 20 dB greater compared with an adult. Furthermore, a given child's ear canal acoustics will change with growth, complicating the issue of accuracy in assessment for hearing instrument prescription.
Age-related trends in ear canal acoustics have been demonstrated for the real-ear unaided gain (REUG) (Kruger, 1987), and the RECD (Feigin et al., 1989; Bagatto et al., 2002). Published estimates of individual differences between HL and SPL in adults show a great intersubject variability in the clinical population (Valente et al., 1994; Saunders and Morgan, 2003). Case examples illustrating this problem have been described in the literature (Moodie et al., 1998). Therefore, defining hearing loss in dB HL makes it difficult to know the precise relationship between the child's hearing sensitivity across frequencies and the amplified speech output in the ear canal (Seewald, 1992).
One solution to the problem of HL-to-SPL differences in an individual is to measure the individual's hearing threshold values in dB SPL in the ear canal. Early in the development of the DSL Method there was an attempt to develop a signal delivery/real-ear measurement system for quantifying an individual's auditory characteristics in dB SPL in the ear canal (Gagné et al., 1991; Zelisko et al., 1992). Study results indicated that the signal delivery system and procedure used for measuring dB SPL thresholds was sufficiently accurate to recommend clinical implementation.
This direct measurement procedure had two major drawbacks. First, hearing levels that are lower than the noise floor of the probe microphone measurement system (usually 40 to 50 dB SPL) or lower than the ambient noise in the room cannot be measured with this approach. Second, the direct measurement approach required that the individual being tested wear both the probe microphone assembly and audiometric measurement transducer during the entire test session. This was seen as a potential problem when evaluating young children.
As a clinically feasible alternative to direct measurement of ear canal SPL thresholds, procedures for predicting the ear canal SPL for audiometric measures were developed. These procedures required the measurement of an individual's RECD, and the use of the RECD as part of a transform that converted HL values to ear canal SPL. A study performed in our laboratory examined the validity and reliability of level-independent HL-to-SPL transforms for insert and TDH-series earphones (Scollie et al., 1998). This work indicated that measuring individualized HL-to-SPL transforms for specific audiometric transducers had equal and high reliability and validity in predicting real-ear SPL. This finding has since been replicated in other laboratories (e.g., Munro and Lazenby, 2001). Based on the results of these and other studies (Kiessling, 1987; Feigin et al., 1989; Fikret-Pasa and Revit, 1992), an integral component of the DSL Method includes transforming dB HL thresholds to an ear canal SPL reference using level-independent HL-to-SPL values.
Clinical Procedures
In clinical audiology, various transducers are used, including insert earphones, TDH-series earphones, or sound field loudspeakers. Some transducers occlude the ear (i.e., insert earphones), whereas others leave it partially occluded (i.e., TDH-series earphones) or nonoccluded (i.e., sound field). If the ear is occluded, as is the case if insert earphones have been used, the HL-to-SPL transform appropriate to the occluded ear acoustics (the RECD values as a function of frequency) is coupled with the RETSPL values for insert earphones and the dB HL threshold values to calculate the threshold value in dB SPL (ear canal level). Details of each transducer's advantages and disadvantages will be discussed below, along with the specifics of HL-to-SPL transformation and relevant normative data.
Insert earphones are the preferred transducer for measuring audiometric thresholds within the DSL Method for reasons of improved interaural attenuation, light weight, and calibration in the 2-cc coupler. The 2-cc calibration of insert earphones allows the individualized RECD to be used both within the HL-to-SPL transform and within the hearing instrument selection and verification transform (discussed later in this chapter). For the HL-to-SPL transform, age-appropriate average or individualized RECD values are combined with the appropriate RETSPL values for insert earphones. Individual RECD values are preferred, whenever possible, because they offer increased accuracy of the transform. Arithmetically, this equation is written for each frequency as:
TDH-series earphones are the second preferred transducer in clinical audiometry. They are successful in achieving ear-specific test results, although they have a much lower interaural attenuation, resulting in the need for masking in more cases (Chaiklin, 1967). They are also heavier than insert earphones, making them somewhat more intimidating and bulky for use with infants and young children. The ear is occluded by TDH-series earphones, but the residual volume is larger than with insert earphones. Therefore, TDH-series earphones are calibrated on a 6-cc coupler rather than a 2-cc coupler. Clinical probe microphone systems do not allow measurement in a 6-cc coupler, preventing the clinical measurement of a 6-cc-based RECD. Therefore, clinical measurement of the HL-to-SPL transform for TDH-series earphones is usually the difference between the measured real-ear SPL from the TDH-series earphone and the audiometer dial reading, the real-ear-to-dial difference (REDD) (Revitt, 1997).
The REDD measurement has the advantage of being able to account for slight errors in audiometer calibration, because both the output of the audiometer and the effects of the external ear are included in the measurement. The DSL Method will accept clinician-entered REDD values and use them as the HL-to-SPL transform. Arithmetically, this equation is written for each frequency as:
If an individually measured REDD is unavailable, the HL-to-SPL transform will be built from the average adult 6-cc-to-eardrum transform (Bentler and Pavlovic, 1989), and the RETSPL for TDH-series earphones. This predicted HL-to-SPL transform is not age-dependent, because no age-related values exist in the literature. In fact, one study demonstrated that the large intersubject variability across age groups supported the need for measures of the REDD on an individual basis (Lewis and Stelmachowicz, 1993). Arithmetically, this equation is written for each frequency as:
Testing hearing in the sound field is the third preferred option in clinical audiometry. Sound field measurements are not ear-specific, so thresholds cannot be interpreted as arising from either the left or right ear unless one ear is plugged during testing (in which case, insert earphones may be a better choice). Because the ear is nonoccluded in the case of the measurement of hearing in sound field, the HL-to-SPL transform is defined as the REUG. The REUG is added to the RETSPL values for the sound field loudspeaker azimuth of choice (0, 45, or 90 degrees) and the dB HL threshold values to calculate the corresponding value in dB SPL (ear canal level). Arithmetically, this equation is written for each frequency as:
Regardless of the transducer used for audiometry, the measurement of individual HL-to-SPL transform values is recommended for the purposes of accurately defining hearing loss for hearing instrument prescription (Bentler, 1989; Bagatto et al., 2002). If measurement of individualized transform values is not possible, such as the case for young, active children, age-appropriate average predicted values should be used rather than average adult values. The normative data for the RECD is described by age in more detail than are the normative data for the REUG, and normative data by age for the REDD are unavailable (Gengel et al., 1971; Kruger, 1987; Feigin et al., 1989; Bagatto et al., 2002). For these and other reasons (see Verification, below), the RECD is the ear canal measurement that offers the greatest clinical utility. The current status of the RECD will be summarized in the next sections in terms of normative data and research regarding reliability and validity.
Definition of the RECD
The first demonstration of age-related differences in the RECD was reported by researchers at Boys Town National Research Hospital (Feigin et al., 1989). They demonstrated that the SPL measured in the occluded ear of an infant compared with that measured in a 2-cc coupler was significantly higher than the values measured from an average adult ear. The small volume of the infant ear canal results in higher SPL values compared with an average adult. Unfortunately, a measure of ear canal volume is not a good predictor of the difference in SPL between the real ear and the coupler (Nelson Barlow et al., 1988; Feigin et al., 1989).
It was suggested that factors such as impedance of the middle ear and ear canal length may interact with volume to affect ear canal SPL (Nelson Barlow et al., 1988). As such, clinical procedures have since been developed to exploit the RECD measurement so that the individual ear canal acoustics of young patients could be captured and applied in the assessment stage of the hearing instrument fitting process. The RECD has been the focus of this work, rather than other ear canal measures such as the REUG, for a variety of reasons. Perhaps most importantly, the RECD can be measured without the use of a sound field loudspeaker. This allows the measurement to be made without requiring a specific seating position and stillness from an infant or young child, thereby avoiding any errors that could be introduced into the calibration of the sound field. This is likely the greatest factor in determining the efficiency of the RECD in clinical practice, both in terms of accuracy and feasibility.
Although the RECD is not a standardized measure, it has been used in a consistent manner within the DSL Method since the early 1990s. Specifically, the RECD is the difference between the SPL measured in an occluded ear canal and that in a 2-cc coupler, measured across frequency. The RECD measurement is made with an insert earphone transducer (Moodie et al., 1994), rather than with a hearing instrument, as was proposed in early RECD measurement protocols (Fikret-Pasa and Revit, 1992). The values are obtained by delivering a stimulus from an insert earphone into the HA2 2-cc coupler, then delivering the same stimulus into the patient's ear with the insert earphone coupled to a foam tip or a personal earmold. The SPL values from the coupler are subtracted from the values measured from the real ear to obtain the RECD. These values are typically positive and rise with increasing frequency.
RECD Reliability, Variability and Normative Data
The test-retest variability of this procedure has been investigated in both children and adults (Sinclair et al., 1996; Munro and Davis, 2003). In adults, test-retest differences are reported to be close to 0 dB with a standard deviation of 1 dB (Munro and Davis, 2003). Sinclair et al. (1996) found that the mean test-retest variability of the RECD procedure in children and adults was less than 2 dB regardless of age or frequency. Another study of RECD test-retest differences within the first year of life suggested a 1-dB difference between the first and second measurement and a standard deviation of 2 dB for infants aged birth to 6 months and 4 dB for those aged 7 to 12 months (Tharpe et al., 2001). Although these results represent the average test-retest difference, it is important to note that individual test-retest values may be large even though they are highly correlated. Nevertheless, these studies indicate that when performed by a trained clinician, the RECD is a highly repeatable measurement of ear canal acoustics in infants, toddlers, children, and adults and should therefore be measured whenever possible.
The RECD is a clinically useful measurement, and may be feasibly and reliably obtained in the pediatric and adult populations in most cases. However, circumstances may exist when the measurement is unobtainable from a particular patient. For example, if an infant's ear has outgrown the earmold, or if a 2-year-old child will not remain still for probe tube placement, measurement may not be possible during a specific clinical appointment. In these cases, age-appropriate normative values for the RECD are a useful alternative.
Feigin et al. (1989) collected RECDs from children aged 1 month to 5 years with normal middle ear function. The values were segmented into 12 to 24 month age ranges up to an age of 5 years. This data set is the basis for most implementations of age-related RECD predictions in current clinical use, including DSL v4.1, NAL-NL1, and most hearing instrument programming modules and probe microphone systems (Seewald et al., 1997; Byrne et al., 2001).
With the emergence of Early Hearing Detection and Intervention (EHDI) programs, infants will have a complete hearing assessment by 3 months of age and be fitted with amplification by 6 months of age (American Academy of Audiology, 2003). Because they were collected well before the onset of EHDI programs, the Feigin et al. (1989) normative data set did not include many infant subjects and may not describe infant ear canal acoustics in sufficient detail to differentiate between infants of ages 3, 6, and 12 months. Also, the norms were collected with standard eartips rather than custom earmolds. For these reasons, a collaborative study was completed by researchers at the University of Western Ontario and Boys Town National Research Hospital to gather normative data that included infant subjects and custom earmolds (Bagatto et al., 2002).
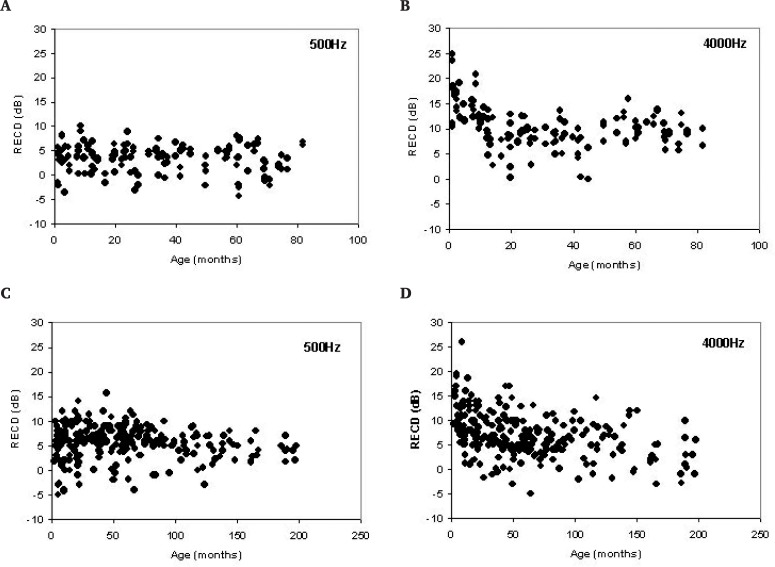
RECD measurements were obtained from 392 infants and children, aged 1 month to 16 years. Acoustic immittance tips were used to measure RECDs on 141 ears, and personal earmolds were used on 251 ears. The data for both coupling procedures indicated substantial between-subject variability across frequency (Figure 1). For example, the range of variability of RECDs measured with personal earmolds on infants younger than 6 months old was 15 dB at 500 Hz. More variability was noted in the very high and very low frequencies.
Figure 1.
Real-ear-to-coupler differences (RECD) (in dB) measured with (A and B) foam/immittance tips and (C and D) earmolds as a function of age at 500 and 4000 Hz (adapted from Bagatto et al., 2002).
Logarithmic regression analyses were performed on the RECD data for each coupling method at each frequency to develop two sets of age-related RECD predictions: (1) frequency-specific predictions by age for eartip coupling, and (2) frequency-specific predictions by age for earmold coupling. The published regressions resulted in a poor association between measured RECD values and subject age (r2 = 0.00 to 0.32). It is also important to note that using these equations to predict RECDs for immittance tips and earmolds may result in values that fall within 14 dB of the actual RECD in 95% of cases (Bagatto et al., 2002). To achieve an improvement in the predictive power of the regression equations, a reanalysis of the data was completed and the results are reported below.
Error in probe microphone measurements typically takes two forms: slit leak venting and shallow probe tube placement (Bagatto, 2001). Certainly, these are likely to occur in the pediatric population, as babies and young children may not cooperate fully during the measurement and may have earmolds that are slightly outgrown. Given that these data were gathered in a clinical context, both factors may have contributed to increased variability in these data. Therefore, the first step in the reanalysis was to screen the raw data to account for measurement error1 and normalize the distribution of values by generating histograms (Tabachnick and Fidell, 1996).
Acoustic leakage in the measurement was suspected if RECD values were below zero in the low-frequency region (i.e., 250–750 Hz) (Dirks and Kincaid, 1987). When this was noted, RECD values were coded as missing data for the analysis if they were −5 dB or less. For data collected with earmolds, this resulted in missing values for 13% and 4% of the data at 250 and 500 Hz. For tip data, 15% and 1% of the data were coded as missing at 250 and 500 Hz. Inspection of the high-frequency values for roll-off was done to determine appropriate probe tube insertion depth (Dirks and Kincaid, 1987). Results of the inspection revealed that the high frequency RECD values for both tip and earmold data were appropriate and no values were coded as missing.
Inspection of the censored data revealed that RECD values in the low frequencies for both immittance tips and earmolds did not demonstrate a clear age-related trend. Therefore, a regression analysis was not performed on the RECD data in the low frequencies. Instead, the means and standard deviations of the values, ranging from 250 to 1000 Hz and 250 to 750 Hz for immittance tips and earmolds, respectively, were calculated. These values are shown in Table 1. Mean low-frequency immittance tip RECD values ranged from a low of 0.1 dB at 250 Hz to a high of 7.9 dB at 1000 Hz across age. For earmolds, RECD values ranged from 2.0 at 250 Hz to 8.0 dB at 750 Hz across age.
Table 1.
Mean and Standard Deviations for Real-Ear-to-Coupler Differences Measured With Immittance Tips and Earmolds as a Function of Frequency*
| Coupling | Frequency (Hz) | Mean (dB) | Standard Deviation (dB) |
|---|---|---|---|
| Immittance tip | 250 | 0.13 | 2.90 |
| 500 | 3.81 | 2.81 | |
| 750 | 6.03 | 2.90 | |
| 1000 | 7.91 | 3.38 | |
| Earmold | 250 | 1.99 | 3.83 |
| 500 | 5.66 | 4.07 | |
| 750 | 7.96 | 3.75 |
Data were reanalyzed from Bagatto et al., 2002.
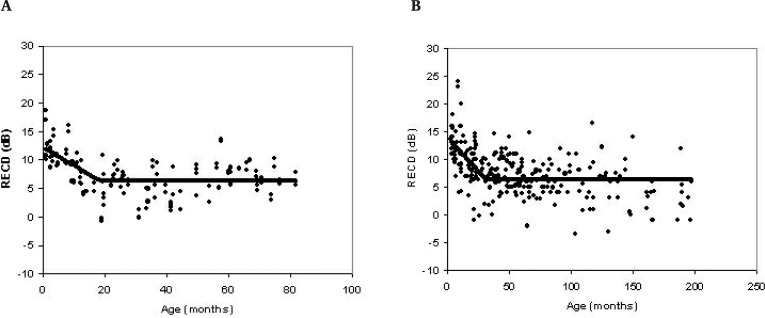
Analysis of the high frequencies indicated a limited age-related trend for both immittance tip and earmold RECD data. Since the trend asymptotes with increasing age, a bilinear regression approach was completed on immittance tip and earmold RECD data separately. Each data set showed a different point at which the age trend occurred. Therefore, the age limit for the regression analysis differed for immittance tip and earmold data across frequencies. Specifically, a linear regression analysis was performed on RECD data collected using immittance tips up to and including age 24 months for 1500 to 6000 Hz. Next, the mean and standard deviation were calculated at the same frequencies for data above the 24 month age limit (see Figure 2).
Figure 2.
Real-ear-to-coupler differences (RECD) (in dB) measured with (A) foam/immittance tips and (B) earmolds as a function of age at 3000 Hz. The sloping line indicates the linear regression represented by the prediction equation. The horizontal line represents the mean RECD values for a particular age range.
The same analysis was completed on earmold data up to an age limit of 36 months for the frequencies 1000 to 6000 Hz. This resulted in a linear regression equation for immittance tip and earmold data up to the age limit (i.e., 24 months for tips, 36 months for earmolds) and mean (and standard deviation) data for values above the age limit. The regression coefficients and r2 values as well as mean and standard deviations for RECD data collected with immittance tips and earmolds are found in Tables 2 and 3, respectively.
Table 2.
Regression Coefficients, r2 Values, Means and Standard Deviations for Real-Ear-to-Coupler Differences Measured With Immittance Tips Across Frequency*
| 1500 | 2000 | Frequency (Hz) 3000 | 4000 | 6000 | |
|---|---|---|---|---|---|
| Slope | −0.19 | −0.24 | −0.32 | −0.43 | −0.50 |
| y-intercept | 9.23 | 10.43 | 12.31 | 16.73 | 17.01 |
| r2 | 0.11 | 0.19 | 0.41 | 0.44 | 0.32 |
| SE | 4.02 | 3.68 | 2.88 | 3.60 | 5.47 |
| Mean (dB) | 6.89 | 7.61 | 6.36 | 9.15 | 9.09 |
Regression results are reported on data from subjects up to and including 24 months of age. Mean and standard deviation results are reported on data from subjects 25 months and older. Data were re-analyzed from Bagatto et al., 2002.
Table 3.
Regression Coefficients, r2 Values, Means and Standard Deviations for Real-Ear-to-Coupler Differences Measured With Earmolds Across Frequency*
| Frequency (Hz) | ||||||
|---|---|---|---|---|---|---|
| 1000 | 1500 | 2000 | 3000 | 4000 | 6000 | |
| Slope | −0.08 | −0.12 | −0.10 | −0.24 | −0.21 | −0.27 |
| y-intercept | 11.12 | 13.24 | 12.49 | 13.90 | 12.58 | 14.12 |
| r2 | 0.04 | 0.10 | 0.07 | 0.28 | 0.15 | 0.14 |
| SE | 3.75 | 3.40 | 3.38 | 3.71 | 4.69 | 6.19 |
| Mean (dB) | 8.58 | 9.90 | 9.44 | 6.27 | 5.78 | 4.53 |
Regression results are reported on data from subjects up to and including 36 months of age. Mean and standard deviation results are reported on data from subjects 37 months and older. Data were re-analyzed from Bagatto et al., 2002.
When predicted RECD values are generated across ages in DSL v5.0, the coefficients presented in Tables 1, 2 and 3 are used as predictive equations, with two modifications. Initially, one standard deviation (Table 1) or standard error (Tables 2 and 3) was added to the predicted values for infants and young children aged 36 months or younger to generate conservative (i.e., large) predicted values. This was reduced to a 0.5 standard deviation/error for children aged 37 to 60 months. Upon examination of the high-frequency analysis as a whole, it was noted that in some instances the predicted values from the regression line did not meet with the mean values after the 60-month age limit. Therefore, the predicted values, including the standard deviation/error, were smoothed using a logarithmic fit, with average adult data points included. This eliminated the abrupt steps between the 36- to 37-month and 60- to 61-month points and allowed the predictive function to converge with adult RECD values at age 60 months. The smoothing strategy stops when average adult RECD values are reached.
If a clinician is unable to measure a RECD on an infant or child, the reanalyzed new normative data provide predicted RECDs for immittance/foam tips or personal earmolds in 1-month age increments. However, these new age-appropriate predictions should not replace a more precise RECD measurement.
RECD Feasibility
As reported in previous sections, RECD measurements are a reliable and valid part of the assessment stage of the hearing instrument fitting process. Therefore, it is important to discuss the feasibility of the measurement in a clinical population. Heinemann et al. (2001) attempted RECD measurements in 109 infants and children. Of this group, 90 RECD measurements were completed successfully and 19 were not. Among those subjects for whom RECDs could not be measured, it was reported that 13 were due to “behavioral issues,” 1 due to an anatomic limitation, and 5 because of other issues such as obstacles in the ear canal. Another study reported RECDs measured from 22 infants enrolled during their first 2 months of life (Tharpe et al., 2001). Six RECDs per subject were measured on each infant during monthly visits. Of the numerous RECDs obtained throughout this investigation, 1 child failed to complete the study owing to transportation difficulties and 18 measurements were not completed because of missed appointments or middle ear dysfunction.
Finally, it has been suggested that conventional probe microphone measurements may introduce more practical measurement difficulties than RECD measures in the pediatric population (Westwood and Bamford, 1995). As such, individual RECD measurements have been included as part of a thorough hearing instrument selection and verification protocol for infants and children identified through universal newborn hearing detection and management programs (Ontario Infant Hearing Program, 2002; Modernizing Children's Hearing Aid Services, 2002; American Academy of Audiology, 2003).
Modified Procedure for Infants
Within universal infant hearing detection and management programs, RECDs from young infants are used as part of a comprehensive intervention protocol (American Academy of Audiology, 2003). As demonstrated by the data from Bagatto et al. (2002), RECD values can vary by as much as 15 dB in infants younger than 6 months old, especially in the high-frequency region. This underscores the importance of measuring the RECD in this population whenever possible. Procedures for measuring the RECD in the pediatric population have been described, and probe tube insertion depth guidelines have been documented (Moodie et al., 1994; Tharpe et al., 2001). However, measurement techniques developed for toddlers may not be feasible for young infants owing to very small ear canals and the position of the infant during the measurement. Specifically, the typical RECD measurement method that involves the probe tube and tip inserted separately may not be practical in the infant population.
A recent study performed in our laboratory examined a new technique for inserting a probe tube in an infant's ear canal for the purposes of obtaining an accurate RECD measurement. The strategy involved simultaneous insertion of the probe tube and the tip into the ear canal. A probe tube was placed along an otoacoustic emission tip so that the end of the tube extended approximately 2 mm beyond the sound bore of the tip. The probe tube was then coupled along the otoacoustic tip with plastic film (as seen in Figure 3).
Figure 3.
Probe tube coupled to ER-10 3.5-mm otoacoustic emission tip using plastic film.
After the probe tube/tip unit was connected to the real-ear system, the unit was inserted into the infant's ear canal. The RECD measurement was performed according to the recommended protocol, and values were examined for appropriate high- and low-frequency representation (Dirks and Kincaid, 1987; Bagatto, 2001). The probe tube/tip unit was removed and a repeated measurement was obtained. In the second part of the study, the probe tube/tip unit from each of the 30 infants was examined to obtain a guideline for insertion depth. Findings indicated that extending the probe tube approximately 2 to 4 mm beyond the tip resulted in appropriate insertion depth, as well as reliable RECD values for infants between the ages of 2 to 6 months.
In addition, a probe tube insertion depth of approximately 11 mm from the opening of the ear canal was determined to be suitable. This technique and insertion depth provides practical information to those clinicians involved in providing amplification to young infants. The strategy may also increase the likelihood that the RECD will be measured by clinicians working with this population.
Using Electrophysiologic Threshold Estimations
Because of the growing number of EHDI programs worldwide, it is not uncommon for audiologists to assess the hearing abilities of very young infants. Behavioral audiometry is not an appropriate strategy for assessing the hearing of infants aged 6 months old and younger; therefore, electrophysiologic procedures are typically used (American Speech Language and Hearing Association, 2004). The auditory brainstem response (ABR) is a common clinical procedure that has been shown to be feasible for estimating hearing thresholds in young infants (Stapells, 2000a; American Speech Language and Hearing Association, 2004). Although much research has focused on the development of frequency-specific ABR procedures for threshold estimation in infants, little work has been done to investigate how the data are used in hearing instrument prescription. To ensure an accurate prescription is calculated from ABR threshold estimates, it is important to account for several variables.
First, auditory evoked potential systems do not currently have standardized calibration. Behavioral audiometry is referenced to a normative dB HL scale, and the audiometer is calibrated using RETSPL values. In contrast, threshold estimations obtained from auditory evoked potentials are referenced in dB normalized HL (nHL), and the method for obtaining this nHL reference is not standardized. There are two common approaches for determining the nHL reference of an ABR system.
One is to obtain a normative reference for ABR thresholds in dB nHL from normal hearing subjects. This is accomplished by comparing the subjects’ behavioral thresholds, obtained using ABR stimuli (brief tone), with those obtained using pure tones. The pure tone thresholds are subtracted from the brief tone thresholds to provide a reference for 0 dB nHL, which is incorporated into the ABR system (Gorga et al., 1993). Variations of this method between different clinics will result in different points of reference for 0 dB nHL (Stapells and Ruben, 1989).
Another common approach of calibrating ABR equipment is to use an acoustic reference by measuring ABR thresholds from subjects in dB SPL rather than dB nHL. This approach requires that the stimuli be calibrated. Similar to the previous method, no standard exists for the SPL calibration of short duration tone bursts (Burkard and Secor, 2002). Some researchers quantify tone bursts by measuring their peak equivalent SPL (pe SPL), and others measure the peak pressure equivalent of the stimuli over a sustained period of time (ppe SPL) (Burkard and Secor, 2002). The procedures will result in different SPL values and therefore a different reference point for calibration. Because no standard calibration method exists for ABR systems, it is important to consider this when applying ABR threshold estimations to derive a hearing instrument prescription.
Another variable to consider when ABR threshold estimates are used for hearing instrument fitting is the disparity between the results of behavioral and electrophysiologic methods of threshold measurement for a given patient (Stapells, 2000a). The methods of calibration are different for audiometers and evoked potential systems, so it is not surprising that the resulting thresholds are dissimilar. In addition, behavioral audiometry reflects responses of the entire auditory system, whereas ABR elicits auditory threshold information up to the level of the brainstem (Elberling and Don, 1987). Because different parts of the auditory system are being assessed in each procedure, the detection threshold is likely to be different. Also, the long-duration stimuli used for behavioral audiometry result in a lower detection threshold than the short-duration stimuli used for ABR assessments owing to temporal integration (Zwislocki, 1960). The inherent differences between the two procedures contribute to the variation noted between the results of behavioral and electrophysiologic measures of threshold.
Several researchers have investigated the degree to which thresholds obtained from behavioral and ABR procedures differ (Stapells, 2000b). ABR threshold estimations collected from adults with sensorineural hearing loss have been shown to be 5 to 30 dB higher than their behavioral thresholds (Picton et al., 1979; Suzuki et al., 1984; Purdy and Abbas, 1989; Munnerley et al., 1991; Stapells et al., 1995; Beattie et al., 1996; Nousak and Stapells, 1999). For infants and young children with sensorineural hearing loss, it has been demonstrated that ABR threshold estimations are 10 to 15 dB higher than their behavioral thresholds (Hayes and Jerger, 1982; Stapells et al., 1995; Balfour et al., 1998). The discrepancy between ABR and behavioral thresholds must be considered when fitting hearing instruments to infants as over- or under-amplification is a possible outcome. A recommended clinical procedure to account for ABR-behavioral differences will be summarized later in this chapter.
Finally, it is important to consider the effect of individual ear canal acoustics on the differences between frequency-specific ABR threshold estimates and behavioral thresholds. Sininger et al. (1997) have demonstrated that some of the infant/adult differences observed between ABR threshold estimates and behavioral thresholds are accounted for by the large ear canal resonances associated with small infant ear canals. To date, this variable has not been accounted for when ABR threshold estimates are compared with behavioral thresholds in listeners with hearing loss. This is likely a significant factor when an ABR measured at approximately 3 months of age is compared with behavioral thresholds at 7 to 9 months of age or later, as discussed earlier in this chapter. In this situation, significant growth of the child's ear canal would have occurred between 3 and 7 months of age. By comparing ABR threshold estimates (nHL) with behavioral thresholds (HL) without accounting for changes in ear canal acoustics, one may see a difference between nHL and HL values that may not be attributed to a change in sensitivity but to a change in individual ear canal acoustics. Ideally, changes in ear canal acoustics owing to growth would be either controlled or computationally removed from comparisons of ABR and behavioral data. The following section describes a study that was recently carried out in our laboratory. The goal of the study was to control for the role of ear canal acoustics in an ABR-to-behavioral comparison. Two strategies were used: (1) we measured the acoustic properties of each subject's ear canal; and (2) both the frequency-specific ABR and the behavioral thresholds were tested at the same age.
Study Overview
This study2 investigated the relationship between ABR and behavioral threshold estimates, accounting for individual ear canal acoustics. The main goal of the study was to assess the accuracy of applying a set of published corrections and a measured RECD to predict behavioral ear canal SPL thresholds.
A total of 30 subjects participated in this study; 15 had normal hearing and 15 had sensorineural hearing loss (range, 30 to 80 dB HL). The mean age of the normal hearing subjects was 24.3 years (range, 21 to 43) and the mean age of the hearing impaired subjects was 15.3 years (range, 9 to 27 years). At the time of data collection, all subjects had normal otoscopic and immittance findings. The participants were recruited from the student and staff population of University of Western Ontario, the H.A. Leeper Speech and Hearing Clinic, and the subject pool from Siemens Child Amplification Laboratory at the National Centre for Audiology.
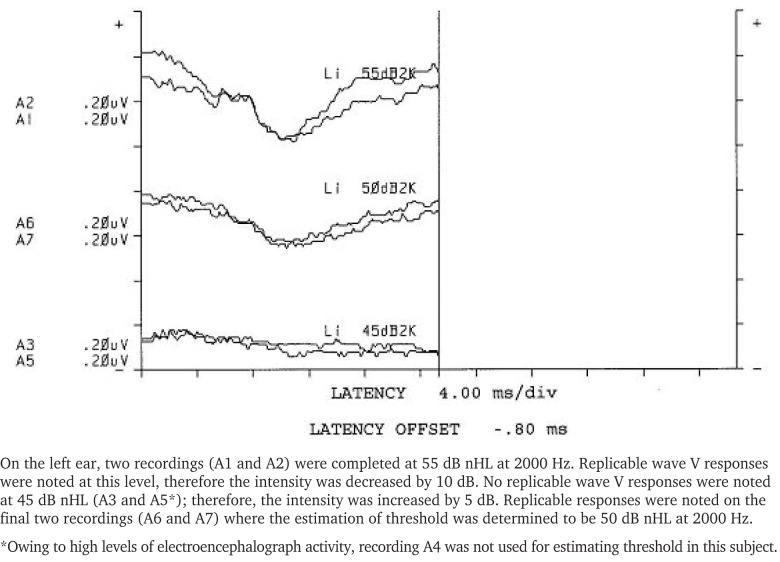
RECD measurements were obtained from one ear of each subject following the procedure described by Moodie et al. (1994). In addition, hearing thresholds from the test ear of each subject were obtained at 500, 1000, 2000, and 4000 Hz using insert earphones coupled to foam tips. Thresholds were determined using both conventional behavioral audiometry and frequency-specific ABR. The Biologic Navigator Pro Evoked Potential system was set up to deliver linearly gated 2-1-2 cycle tone bursts. Other stimulus and recording parameters were arranged to follow published recommendations and are summarized in Appendix A (Stapells, 1989; Stapells and Ruben, 1989; Stapells et al., 1990; Stapells and Oates, 1997; Stapells, 2000a; Stapells, 2000b). Subjects fell into natural sleep for the ABR procedure to keep individual noise levels as low as possible.
The presentation strategy of tone-burst stimuli was similar to behavioral audiometry. Initially, the stimulus was presented at 30 dB estimated HL (eHL)3 and the presence or absence of the response was replicated at least once (Stapells, 2000a). If a replicable response was noted, the intensity was decreased in 10-dB steps until no replicable response was noted, then up in 5-dB steps until a replicable threshold could be determined. If no response was noted at the initial starting level, the level was increased in 10-dB steps until a replicable response was noted. Bracketing in 5-dB steps was completed until reliable threshold estimation was determined. An example of this procedure is shown in Appendix B.
Strategies for the conversion of HL data to ear canal SPL using the RECD have been well documented (Bentler and Pavlovic, 1989; Revitt, 1997; Scollie et al., 1998; Munro and Davis, 2003). For the purposes of this study, the HL-to-SPL conversions described earlier in this chapter were applied to behavioral data using the following equation:
For ABR threshold estimations, a similar calculation was applied with the exception of one difference. Published behavioral corrections (Stapells et al., 1990) were applied to ABR threshold estimations to obtain an estimated behavioral hearing threshold, which will be referred to in this document as eHL and is used to denote a corrected nHL value that represents a behavioral threshold. The eHL value was then converted to SPL using the following equation:
This calculation allowed for ABR threshold estimations to be compared to behavioral thresholds in ear canal SPL.
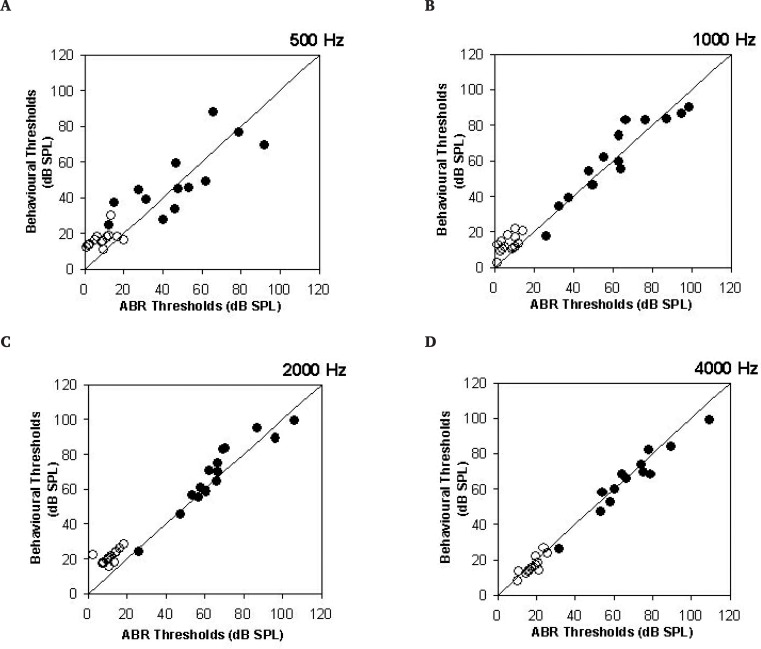
Figure 4 shows the comparison between the ABR and behavioral thresholds in ear canal SPL at 500, 1000, 2000, and 4000 Hz using a measured RECD. The average error between the ABR threshold estimates and the behavioral thresholds was 6.5 dB, once the behavioral and acoustic corrections were both applied. This error amount is smaller than the typical audiometric step size of 10 dB used during a clinical frequency-specific ABR procedure (Ontario Infant Hearing Program, 2002). Differences across frequency generally decreased with increasing frequency. For example, the average difference between ABR threshold estimates and behavioral thresholds at 500 Hz was 10.62 dB compared with 3.97 dB at 4000 Hz. Overall, 85% of the ABR threshold estimates were within 10 dB of the behavioral thresholds and 96% were within 15 dB. Significant correlations were noted across frequency (r = 0.91 to 0.99; p < .001).
Figure 4.
Comparison of derived behavioral and auditory brainstem response (ABR) thresholds in dB SPL for (A) 500 Hz, (B) 1000 Hz, (C) 2000 Hz and (D) 4000 Hz. Filled circles indicate data for hearing impaired subjects and open circles indicate data for subjects with normal hearing. The diagonal line represents perfect correspondence.
Previous evaluation of differences between frequency-specific ABR threshold estimates and behavioral thresholds have indicated that the frequency-specific ABR procedure provides valid estimates of audiometric threshold (Stapells et al., 1995). However, this and other work also indicates that corrections should be applied to the frequency-specific ABR threshold estimates to convert them from nHL to HL (Stapells, 2000a). The study reported here applied a specific set of corrections (see Appendix C), providing additional validation of this concept. Therefore, one primary finding is that the proposed corrections appeared to provide reasonable accuracy across the relatively broad range of hearing losses evaluated in this study. Further validation of this approach on infants is necessary, with longitudinal measures of growth-related changes in ear canal acoustics, to further confirm the validity of the overall approach.
The procedures used in this study also illustrate a potential method for merging the HL-to-SPL transform approach described above with the data collection procedures typically used with infants. This study used insert earphones and individually measured RECDs to convert both nHL and HL data to real-ear SPL thresholds for evaluation. Good agreement was obtained, indicating that it may be possible to convert frequency-specific ABR threshold estimates to ear canal SPL for use in hearing instrument prescription and fitting. For the DSL Method, this is an important consideration, because prescriptive targets are calculated from ear canal SPL thresholds rather than from nHL or HL thresholds.
Based on these findings, version 5.0 of the DSL Method supports infant hearing instrument fitting based on electrophysiologic threshold estimates. Specifically, clinicians may enter data referenced to nHL or eHL. If the threshold estimates are measured in the nHL reference, corrections will be applied within the DSL software to convert the nHL data to eHL. These corrections can be default values that are stored within the software, or clinicians can enter their own custom nHL to eHL correction values. In version 5.0, the default values are appropriate for use with frequency-specific ABR procedures that comply with the calibration and stimulus parameters shown in Appendix A. Several other alternatives exist to this approach, however, as will be described below.
Some clinicians may use electrophysiologic equipment that has a built-in behavioral correction (Gorga et al., 1993; Eiten, 2005). This is achieved by comparing a group of normal-hearing subjects’ behavioral thresholds with ABR stimuli (brief tone) to those obtained using pure tones. Subtraction of pure tone from the brief tone thresholds provides a reference for 0 dB nHL. The resulting ABR threshold estimations are thus referenced to eHL and therefore do not need further correction. In this case, the clinician should choose “estimated HL” in DSL v5.0 to ensure no further behavioral correction will be applied. The eHL value entered into DSL will then be converted to ear canal SPL using RECD values for a more accurate prediction of threshold.
Clinicians who assess the hearing of infants by using ASSR procedures are advised to ensure that the ASSR system is applying an nHL-to-HL correction that is valid for use with infants who have hearing loss (Stapells et al., 2005). If this is the case, data may be entered directly into DSL by using the eHL reference.
Clinical Verification Procedures
Simulated Real Ear Aided Response/Gain
As discussed by Seewald et al. (2005) in this issue, the preferred verification format used in the DSL Method is the SPLogram, or a display of the real-ear aided responses (REAR) (ANSI, 1997) with accompanying curves for threshold and upper limit of comfort. This preferred display allows meaningful interpretation of the audibility of various aided and unaided speech signals, permitting the use of electroacoustic verification measures to predict the aided audibility of speech as a function of speech input level and frequency (Scollie and Seewald, 2002). In cases where direct measurement of the REAR is not possible, measurement of coupler gain or SPL can be used to predict the REAR by using a measured or predicted age-appropriate set of RECD values (see below for details and protocols).
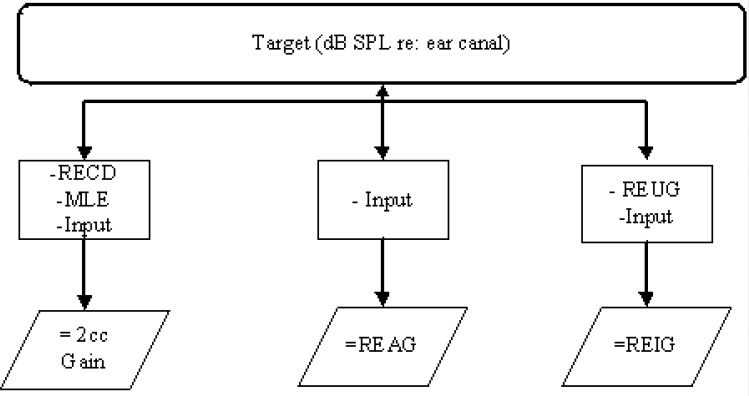
The DSL multistage input/output (m[i/o]) formula computes targets in ear canal SPL, assuming an input of running speech. The levels are defined as 1/3-octave band levels, integrated over enough samples to obtain a stable estimate of the long-term average speech spectrum. Other target formats or other test signals can be generated by applying various corrections (Figure 5). These correction strategies follow well-accepted methods that are generally used by most prescriptive formulae, hearing instrument fitting modules, and probe-microphone equipment. Specific details of correction and conversion strategies will be discussed within the following sections.
Figure 5.
Schematic diagram of the transformation processes used to convert target values from sound pressure level in the ear canal to other formats commonly used in the electroacoustic evaluation of hearing instruments. RECD = real-ear-to-coupler difference; REAG = real-ear aided gain; REUG = real-ear unaided gain; REIG = real-ear insertion gain.
Moodie et al. (1994) developed an RECD measurement procedure for use in fitting hearing instruments for infants and young children. This modification of an adult-based RECD measurement procedure described by Fikret-Pasa and Revit (1992) provided an alternative to conventional probe microphone measures for those situations in which infants and young children either could not or would not provide the passive cooperation needed for real-ear measures of behind-the-ear (BTE) hearing instrument performance. They recommended a procedure in which an insert earphone transducer was coupled to the child's earmold to measure the SPL in the ear canal. The same insert earphone transducer was subsequently used to measure corresponding SPLs developed in a 2-cc coupler for the same test signal. Moodie et al. (1994) provided procedural details on real-ear system setup, probe tube insertion depth, and measurement interpretation.
One of the primary advantages to this coupler-based approach is that it allows clinicians to perform all electroacoustic response shaping using an SPLogram format, within the highly controlled acoustic conditions of the test box. As such, it is correctly thought of as a procedure that can be used to facilitate coupler-assisted verification. Additional advantages to the RECD measurement procedure described by Moodie et al. (1994) include:
eliminating the variability associated with sound field probe tube microphone measurements with young children and enabling us to fit them with amplification in infancy;
reducing the amount of measurement time and degree of cooperation required from the infant or child; and
reducing the amount of measurement time and degree of cooperation required from children for whom conventional sound field probe microphone measures can not be obtained.
In 1999, Seewald et al. examined the predictive validity of the procedure described by Moodie et al. (1994) for predicting the real-ear aided gain (REAG) and real-ear saturation response of hearing instruments. The REAG was both measured and predicted for 14 participants in the study. Results indicated that, on average, the REAG values were predicted using the individualized RECD values to within ± 2.3 dB across the five frequencies included in the analysis in 95% of the cases. Similarly, the average error range for the predictions of real-ear saturation response for seven subjects was 4.4 dB. A similar study, with similar findings, was recently reported by Munro and Hatton (2000).
As new real-ear measurement systems have become commercially available, procedures for measuring the RECD have been implemented as part of their application of the DSL Method. Most manufacturers of these real-ear systems have provided comprehensive RECD measurement protocols, with some modifications, for development of their own signal delivery transducers used in place of the ER3A insert earphone recommended by Moodie et al. (1994) and to meet the individual needs of the measurement stimuli and procedures that were unique to their systems.
Recently, data have been reported that suggest the RECD measurement with a custom earmold may vary according to the transducer with which it is measured (Munro and Salisbury, 2002) and may not accurately predict real-ear hearing instrument performance (Munro and Toal, 2005). This transducer specificity may affect the validity of using coupler-based predictions of real-ear aided responses, under certain circumstances. The following sections of this chapter will provide a review of the parameters that must be considered when measuring a RECD and will provide a discussion of their potential impact on the validity of coupler-assisted verification.
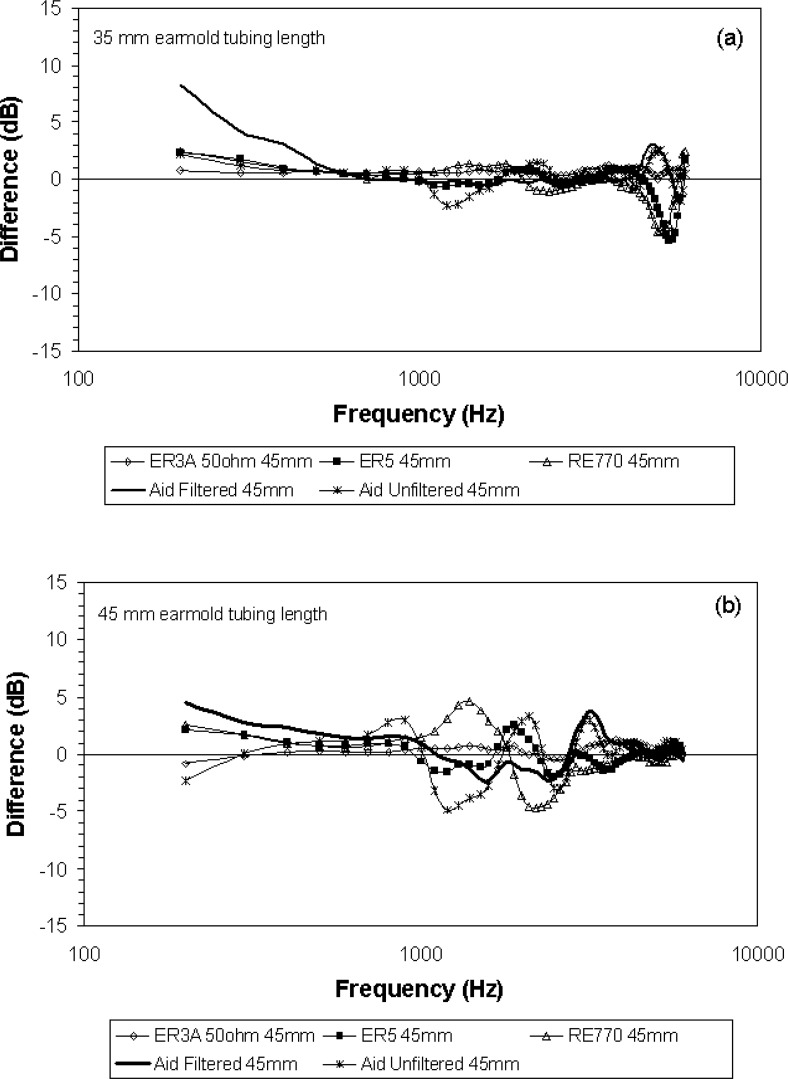
Varying the RECD Transducer
Munro and Salisbury (2002) have shown that the RECD is somewhat dependent on the measurement transducer. Comparisons of mean RECDs obtained with ER3A insert earphones and the Audioscan RE770 RECD transducer were made using a foam eartip and earmolds with three lengths of tubing. The results of this study indicated a mean difference value between the RE770 and ER3A RECD of 9 dB at 1.5 kHz when the earmold tubing was at a length that would be appropriate for adult subjects. The mean RECD difference decreased as earmold tubing length decreased. This finding may have clinical significance. That is, the validity of the coupler-assisted approach to verification is likely greatest for earmolds with shorter lengths of tubing as would be used in the case of a pediatric fitting. Munro and Salisbury (2002) postulated that the differences could be related to the interaction between the acoustic impedance of the earphone and the coupling system to the ear.
Methods for Coupling to the Ear
The recommended method for RECD measurement in children typically couples the transducer to the ear using the child's custom earmold. This recommendation evolved because children will often accept their custom earmold over alternative earphone couplings (i.e., foam or immitance tips). Also, it can provide a more accurate estimation of low-frequency RECD values caused by slit leak venting, provided the earmold is not vented. Munro and Hatton (2000) reported that the mean difference between measured and derived real-ear aided responses were greatest when the RECD was measured with foam or immitance tip coupling to the ear. The differences could be due to acoustic leakage (low frequencies), depth of earmold insertion (mid frequencies), and length of the earmold sound bore (high frequencies) (Munro, 2004). When the custom earmold was used, the mean difference between the measured and predicted real-ear performance rarely exceeded 5 dB in any subject. This finding led to the recommendation that predictions of real-ear hearing instrument performance using temporary ear couplings, such as foam or immitance tips, should only be used to guide the initial hearing instrument selection. In other words, electroacoustic predictions of hearing instrument performance should be regarded as only approximate until the real-ear portion of the RECD measurement can be made using the custom earmold.
Effects of Different Couplers
The recommended method for RECD measurement in children typically uses the HA2 coupler. This recommendation evolved for reasons of clinical feasibility. The initial development of the RECD measurement procedure included earmolds that provided a good seal to the ear because they were made of soft silicone material. This type of earmold material is more comfortable to wear for long periods of time and provides a good acoustic seal to the ear. However, soft silicone material does not adhere well to the putty commonly used with the HA1-2-cc coupler. Therefore, use of the HA1 coupler was abandoned for most measurement protocols involving the RECD with custom earmolds and consequently led to our recommendation to use the HA2-2-cc coupler in RECD measures for BTE hearing instrument fittings.
A recent study has demonstrated that the RECD values obtained using the HA1 vs the HA2 coupler will differ (Munro, 2004; Munro and Toal, 2005). However, Munro and Toal found that despite the difference in the mean RECDs, the predicted real-ear performance of a hearing instrument obtained using the ER3A insert earphone RECD is a clinically acceptable procedure. They also reported that the RECDs measured using ER3A insert earphones and the HA1 and HA2 couplers were similar to those reported for the same couplers by Munro and Davis (2003) and Munro and Hatton (2000). Results of their work led to the recommendation to continue to measure the RECD with an insert earphone and an HA2-2-cc coupler, as the errors in predicting real-ear hearing instrument performance appeared to be restricted to a limited frequency range and, for most hearing instruments, appeared to be no more than 5 dB (Munro and Toal, 2005).
Which RECD is Correct?
A hearing instrument is a signal delivery system and as such could be considered an RECD measurement transducer. Therefore, the non-hearing instrument transducer and coupler combination that best predicts the hearing instrument/earmold RECD is likely the most valid measurement. Validity is also greatest when the RECD is defined for the same coupler that will be used in later coupler-assisted verification measures.
Unfortunately, accurate measurement of the RECD with a BTE hearing instrument can be difficult to obtain. During the real-ear portion of the RECD measurement in this condition, the microphone location effects for the BTE instrument have to be measured or eliminated, and the effects of the calibration method (i.e., substitution or modified pressure) must be carefully considered. More important, however, is the potential effect of acoustic feedback occurring during the measurement process. Acoustic feedback, which can be either subaudible or just audible, may occur during the real-ear portion of the measurement simply owing to loose or poor earmold fit, or slit venting caused by the placement of the probe tube microphone. The following section will present the results of a study that attempted to replicate the findings of Munro and Toal (2005), while attempting to ensure that the BTE gold standard RECD was conducted without feedback confounds. A second goal of the study was to examine the effects of varying the impedance of the hearing instrument by measuring the BTE RECD with and without an acoustically filtered ear hook.
Six RECD measurement transducers were included in the study: the ER3A 10-ohm, the ER3A 50-ohm, the ER5A, the RE770, a BTE hearing instrument with an unfiltered ear hook, and a BTE hearing instrument with an acoustically filtered ear hook. Measurements of the coupler portion of the RECD procedure were made on an HA2-2-cc coupler. Finally, 35 mm and 45 mm lengths of earmold tubing were used with a soft silicone earmold. These lengths of earmold tubing were chosen to reflect typical lengths used for young children and for adults respectively. The measurements were obtained at 100 Hz intervals from 200 to 6000 Hz for an adult ear.
A Unitron Icon AOHPa hearing instrument was set for a flat 45 dB HL hearing loss using the DSL Method. The earhook of the hearing instrument was alternated between an unfiltered hook and one with a 1500-ohm filter. The test signal was delivered directly from the Fonix 6500 hearing instrument analyzer speaker output to the auxiliary input of the Phonic Ear Solaris FM system transmitter. This signal was delivered to the FM receiver coupled to the BTE hearing instrument worn on the ear of an adult. The output of the FM/hearing instrument combination was set to match as closely as possible the initial output of the hearing instrument. The hearing instrument microphone was deactivated for all measurements. Using the FM transmitter and deactivating the hearing instrument microphone eliminates the variability associated with performing free-field real-ear measurements. In addition, deactivation of the hearing instrument microphone eliminates the potential interference of subaudible (or audible) acoustic feedback in the real-ear portion of the RECD measurement. A 50 dB SPL composite signal output was used for all measures.
Differences were calculated between the conventional ER3A/HA2 RECD values and those measured with the hearing instruments, the ER5, and the RE770 transducers. Values close to 0 dB indicate higher validity. Figure 6 shows the RECD differences for the 35 and 45 mm tubing length. The largest difference is seen for the 45 mm tubing length, regardless of earhook filter. The greatest relative difference is seen at 200 Hz for the filtered hearing instrument transducer, where the RECD value is approximately 8 dB higher than the RECD value obtained at the same frequency for the ER3A/HA2 RECD measurement procedure. At most other frequencies, the difference between the ER3A/HA2 RECD measurement procedure and the five other conditions was less than 5 dB for both the 35 mm and 45 mm tubing lengths. This relationship between earmold tubing length and RECD variance with transducers is consistent with other studies reported in the literature (Munro and Salisbury, 2002; Munro and Davis, 2003).
Figure 6.
The mean difference between real-ear-to-coupler difference (RECD) values that were measured using the gold standard procedure (ER3A Insert Earphone [10 ohm]/HA2 2-cc coupler) and five other RECD measurement transducers as a function of frequency for 15 subjects. Panel A shows results when the custom earmold used has 35 mm of tubing. Panel B shows results when the custom earmold used has 45 mm of tubing. A value closer to 0 indicates little difference between the two measurement conditions was noted.
The Coupler-Assisted Approach and Adult Earmolds
The previous sections have reviewed several measurement issues associated with using the RECD in a coupler-assisted verification protocol. Specifically, we measure the RECD so that we can transform coupler measurements of hearing instrument performance to predicted ear canal levels. This is a useful procedure, in that it allows simulated real-ear measurement, either as a substitute for individual probe microphone verification or for presetting hearing instruments. However, the RECD has been shown to vary from the presumed response under normal aided conditions, particularly when the earmold tubing is relatively long (i.e., >45 mm). This is unlikely to present a problem in our work with infants and toddlers. For older children and adults, however, earmold tubing length issues may need to be considered. The following section will describe the amount of error associated with using the insert earphone RECD procedure with older patients.
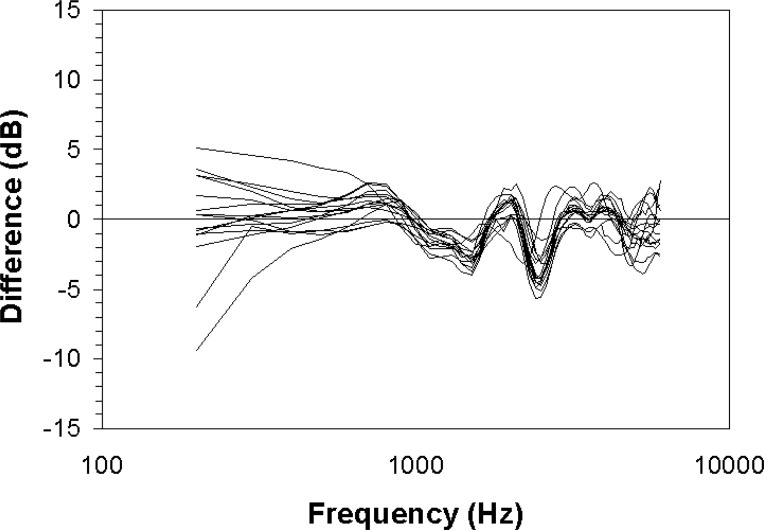
RECD measurements were obtained for 15 subjects who used their personal earmolds and two measurement transducers (ER3A and a BTE hearing instrument). Earmold tubing length was measured for each subject and ranged from 34 mm to 50 mm. The coupler portion of the RECD measurement was performed for both procedures on an HA2-2-cc coupler. The real-ear portion of the RECD measurement was made using a Phonak Claro 311 dAz hearing instrument with a 1500-ohm filtered ear hook. The hearing instrument was set for a flat 45 dB HL hearing loss. The test signal was delivered from the speaker output of the Fonix 6500 hearing instrument analyzer to the auxiliary input of a Phonak Campus-S FM system transmitter. The signal was delivered from the FM transmitter to the receiver of a MicroLink FM system attached to the BTE hearing instrument worn on the ear. The electroacoustic output of the FM system/hearing instrument combination was set as closely as possible to match that of the initial electroacoustic hearing instrument output across frequencies. The hearing instrument microphone was deactivated to eliminate issues associated with free-field real-ear measurements and potential acoustic feedback. Measurements were obtained at 100 Hz intervals for the frequencies 200 to 6000 Hz. Difference values were calculated between the RECD obtained using the BTE hearing instrument transducer and the ER3A/HA2-2-cc coupler procedure described by Moodie et al. (1994).
Figure 7 shows the relative difference values obtained for the two transducers as a function of frequency for the 15 subjects. A positive value indicates that the RECD measured using the hearing instrument transducer generated a higher RECD value at that frequency than the ER3A/HA2 RECD measurement procedure. The greatest difference was seen at 200 Hz. Most of the differences, across frequencies, were within 5 dB of the BTE measured RECD values.
Figure 7.
The relative difference values obtained for the ER3A/HA2 2-cc coupler real-ear-to-coupler difference (RECD) measurement procedure and the hearing instrument RECD measurement procedure as a function of frequency for 15 subjects. A positive value indicates that the RECD measured using the hearing instrument transducer generated a higher RECD value at that frequency than the ER3A/HA2 RECD measurement procedure.
Clinical Implications
Coupler-assisted verification is a useful procedure, particularly when working with infants and young children; however, limitations to its validity have been identified. Specifically, the RECD measurement is not independent of the transducer when custom earmolds are used if the tubing length exceeds approximately 35 or 45 mm. The associated predictive errors will not exceed 5 dB for most frequencies, however, and will be reduced when filtered ear hooks are used in BTE devices.
In summary, the use of coupler-assisted verification is likely not a concern for infants, toddlers, and other BTE users with earmold tubing length less than about 45 mm. Concerns may be present for coupler-assisted verification in other populations, but can be expected to be less than 5 dB when the ER3A transducer is used, and likely less when the earhook of the hearing instrument has been acoustically filtered. For hearing instrument users with large earmolds, large vents, or both, direct measurement of the real-ear aided response would be preferable to the coupler-assisted approach.
Insertion Gain
DSL targets in the real-ear insertion gain (REIG) (American National Standards Institute, 1997) format were not typically available in past versions of DSL. The REIG format was omitted largely out of concern regarding the lack of utility and feasibility of the REIG measurement format in the pediatric population (Scollie and Seewald, 2002). Typical REIG target implementations use an average adult REUG when computing targets, but the user's own REUG when computing measured curves. This mismatch of REUG responses can introduce significant error, particularly in the 2000 through 4000 Hz frequency region for children (Scollie and Seewald, 2002) or for adults with aberrant external ear canal resonances (Byrne and Upfold, 1991). For this reason, DSL v5.0 will compute REIG targets, with incorporation of either individual or age-appropriate REUG values, rather than assume an average adult ear canal. Specifically, the hearing instrument user's own REUG will be used to generate REIG targets, if it is available. Otherwise, an age-appropriate REUG will be applied.
Test Signals
Targets from the DSL m[i/o] algorithm are appropriate for comparison with the aided long-term average speech spectrum, measured in 1/3 octave bands. These targets can be converted for use with pure tone or speech noise signals using the gain correction proposed by Scollie et al (2002). This correction has the advantage of being robust and generic to the channel structure of the hearing instrument and only requires a minimal amount of information from the clinician about the signal processing characteristics of the hearing instrument. However, it has the disadvantage of being accurate only to within about 5 dB and only for input levels between 50 and 70 dB SPL. Therefore, targets for nonspeech test signals are only generated for inputs between 50 and 70 dB SPL, with the exception of output limiting targets for 90 dB pure tones. Clinicians are advised to use speech-based verification whenever possible (Scollie, 2003). If speech is not available as a verification test signal, the next preferred signal is a speech-weighted noise, followed by pure tones.
Venting Corrections
Venting corrections are applied in DSL m[i/o] v5.0 using values reported by Dillon (2001), but with two venting effect paths: sound lost through the vent; and sound coming in through the vent (Hoover et al., 2000). A lower limit of venting reduction is defined, in real-ear SPL, that is equivalent to the test level plus the real-ear unaided gain. If the test frequency is below 1000 Hz, the venting reduction is limited to not fall below this unaided level. Therefore, the venting correction is computed individually for each input level. Venting corrections are only applied in the 2-cc transform and will not affect the targets in real ear formats (REAR, REAG, REIG).
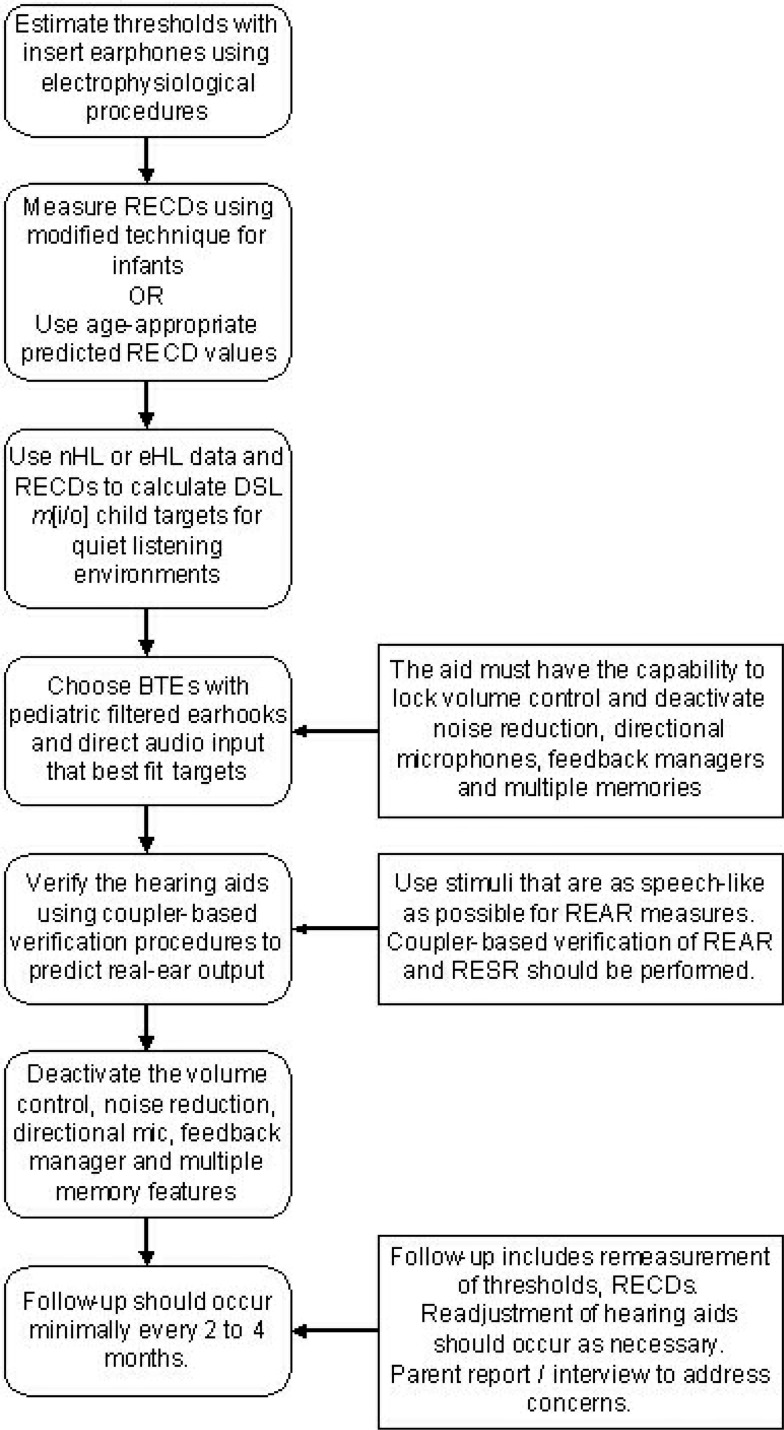
A Suggested Clinical Protocol
Recognizing that the specifics may vary depending on the equipment, location, and individual needs of services, general guidelines for hearing instrument fitting are helpful in guiding systematic practice. In modern audiologic practice, hearing instrument fitting guidelines tend to vary in terms of the age of the client. In Figures 8 through 10, we have attempted to summarize the general process of hearing instrument fitting and also to customize this process for application to the different needs of infants, children, and adults. In general, these stages follow the assessment, selection, verification, and validation schemes commonly cited in the literature and discussed in this issue (Seewald et al., 2005). The clinical procedures discussed here are intended to be used in conjunction with version 5.0 of the DSL prescriptive algorithm, also discussed in this issue (Scollie et al., 2005).
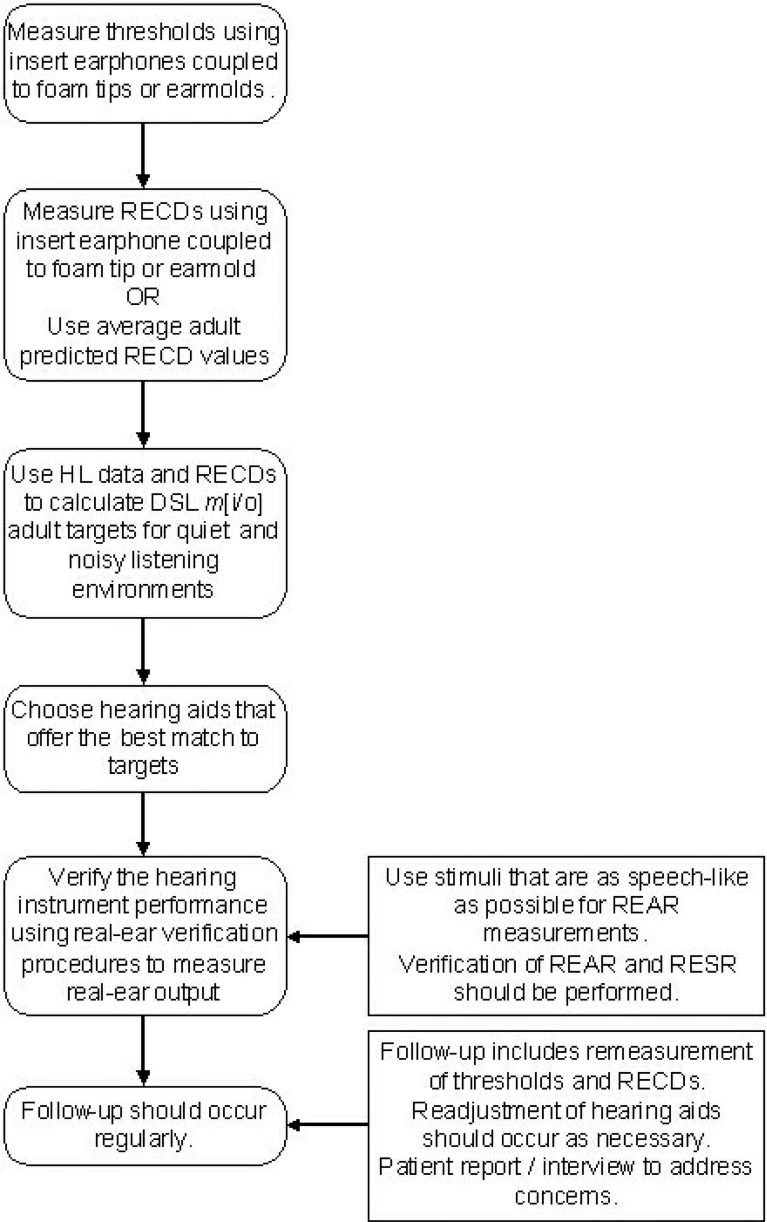
Figure 8.
The Desired Sensation Level (DSL) recommended protocol for hearing instrument fitting to infants. RECD = real-ear-to-coupler difference; DSL m[i/o] = Desired Sensation Level multistage input/output; nHL = normalized hearing level; eHL = estimated hearing level; BTE = behind-the-ear; REAR = real-ear aided response; RESR = real-ear saturation response.
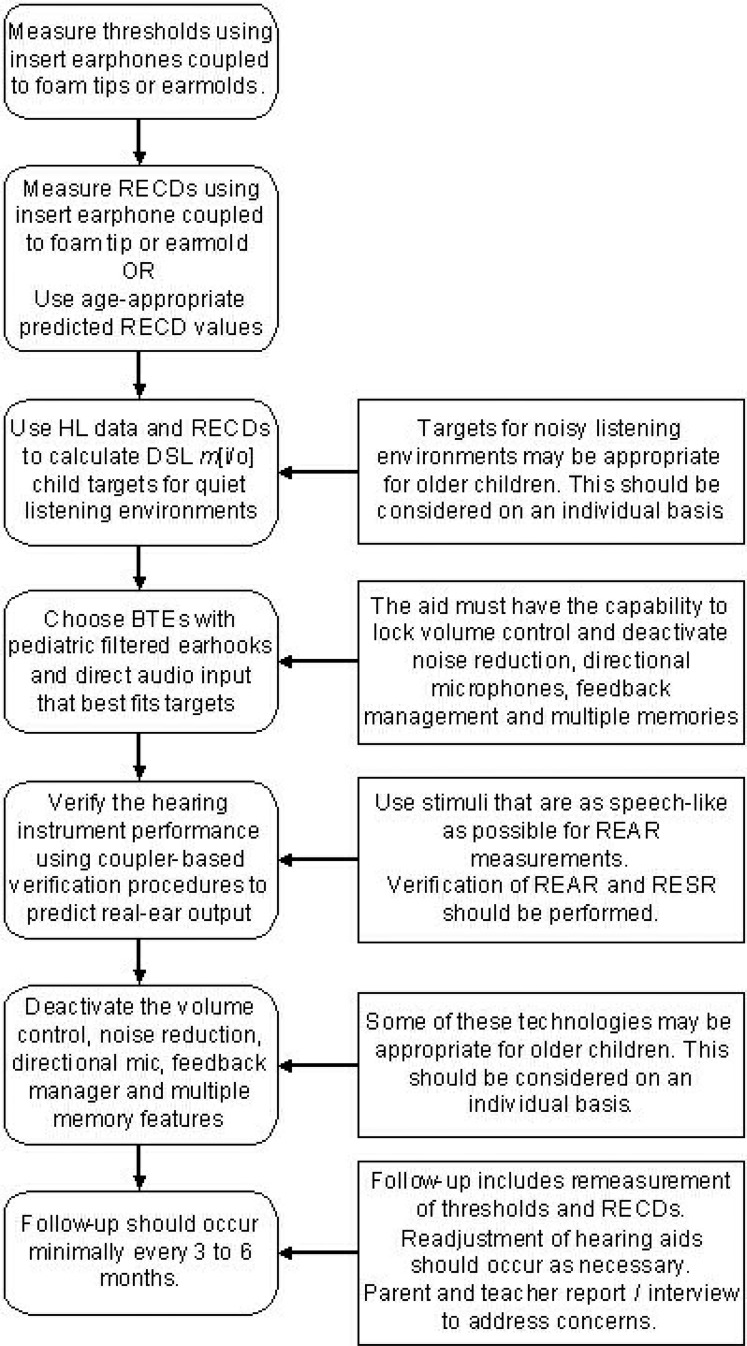
Figure 10.
The Desired Sensation Level (DSL) recommended protocol for hearing instrument fitting to adults. RECD = real-ear-to-coupler difference; DSL m[i/o] = Desired Sensation Level multistage input/output; HL = hearing level; REAR = real-ear aided response; RESR = real-ear saturation response.
Figure 9.
The Desired Sensation Level (DSL) recommended protocol for hearing instrument fitting to children. RECD = real-ear-to-coupler difference; DSL m[i/o] = Desired Sensation Level multistage input/output; HL = hearing level; BTE = behind-the-ear; REAR = real-ear aided response; RESR = real-ear saturation response.
Acknowledgments
We would particularly like to thank Martyn Hyde, Judith Gravel and David Stapells for their helpful contributions to the work that is described within this chapter. We gratefully acknowledge the assistance of Jeff Crukley, Carol Van Evera, Andreas Seelisch, and Julianne Tenhaaf in the preparation of this chapter.
Appendix A.
Stimulus and Recording Parameters Used to Obtain Frequency-Specific Auditory Brainstem Response (ABR) Threshold Estimations in the Study Comparing ABR Thresholds With Behavioral Thresholds in Real-Ear Sound Pressure Level
| Stimulus calibration | 500 Hz: 22 dB ppe SPL |
| (ER-3A) | 1000Hz: 25 dB ppe SPL |
| 2000 Hz: 20 dB ppe SPL | |
| 4000 Hz: 26 dB ppe SPL | |
| Filters | High pass: 30 Hz |
| Low pass: 1500 Hz | |
| 6 or 12 dB/octave | |
| Analog | |
| Stimuli | 2-1-2 cycle, linearly gated tones |
| Window length | 25 msec |
| Polarity | Alternating |
| Rate | 37–41 sweeps/sec |
| Artifact reject | Trials exceeding 25 muV or ± 2 SD of quietest EEG signal, whichever is smaller |
| Average | 2000 sweeps per average |
| At least 2 averages |
ppe SPL = peak pressure equivalent sound pressure level.
Appendix B.
Auditory Brainstem Response Waveform Bracketing Procedure for Threshold Estimation Using Tone-Burst Stimuli
Appendix C.
Corrections Used in the Study Described in this Chapter That Investigated the Relationship Between Behavioral Thresholds and Frequency Specific Auditory Brainstem Response Threshold Estimates*
| Frequency (Hz) | ||||
|---|---|---|---|---|
| 500 | 1000 | 2000 | 4000 | |
| Normal hearing | 16.3 | 11.0 | 9.5 | 2.5 |
| Hearing impaired | 7.0 | 1.3 | 3.0 | −1.0 |
Values are from Stapells et al., 1990 and were subtracted from normalized hearing level values to obtain estimated hearing level.
Footnotes
We gratefully acknowledge helpful discussions with Volker Kuehnel and Martyn Hyde regarding data screening.
We gratefully acknowledge Martyn Hyde, David Stapells, and Judith Gravel for their invaluable contributions to this study.
See later in this section for definition and discussion of eHL versus nHL.
References
- American Academy of Audiology (2003). Pediatric Amplification Protocol, Draft American Academy of Audiology.
- American National Standards Institute (1997). Methods of Measurement of Real-Ear Performance Characteristics of Hearing Aids. ANSI S3.46–1997. New York: Acoustical Society of America [Google Scholar]
- American National Standards Institute (1996). Specification for Audiometers. ANSI S3.6–1996. New York: Acoustical Society of America [Google Scholar]
- American Speech Language and Hearing Association (2004). Guidelines for the audiologic assessment of children from birth to 5 years of age. http://www.asha.org/members/deskref.journals/deskref/default [retrieved on-line May 2005].
- Bagatto MP. (2001). Optimizing your RECD measurements Hear J 54(9): 32, 34–36 [Google Scholar]
- Bagatto MP, Scollie SD, Seewald RC, et al. (2002). Real-ear-to-coupler difference predictions as a function of age for two coupling procedures. J Am Acad Audiol 13: 407–415 [PubMed] [Google Scholar]
- Balfour PB, Pillion JP, Gaskin AE. (1998). Distortion product otoacoustic emission and auditory brain stem response measures of pediatric sensorineural hearing loss with islands of normal sensitivity Ear Hear 19: 463–472 [DOI] [PubMed] [Google Scholar]
- Beattie RC, Garcia E, Johnson A. (1996). Frequency-specific auditory brainstem responses in adults with sensorineural hearing loss. Audiolog 35: 194–203 [DOI] [PubMed] [Google Scholar]
- Bentler RA. (1989). External ear resonance characteristics in children J Speech Hear Res 54: 264–268 [DOI] [PubMed] [Google Scholar]
- Bentler RA, Pavlovic CV. (1989). Transfer functions and correction factors used in hearing aid evaluation and research Ear Hear 10: 58–63 [DOI] [PubMed] [Google Scholar]
- Burkard RF, Secor C. (2002). Overview of auditory evoked potentials. In: Katz J. ed. Handbook of Clinical Audiology. New York: Lippincott; Williams and Wilkins, 233–248 [Google Scholar]
- Byrne D, Dillon H, Ching T, et al. (2001). The NAL-NL1 procedure for fitting non-linear hearing aids: Characteristics and comparisons with other procedures. J Am Acad Audiol 12: 37–51 [PubMed] [Google Scholar]
- Byrne D, Upfold G. (1991). Implications of ear canal resonance for hearing aid fitting Sem Hear 12: 34–41 [Google Scholar]
- Chaiklin JB. (1967). Interaural attenuation and cross-hearing in air conduction audiometry J Aud Res 7: 413–424 [Google Scholar]
- Cox RM. (1985). A structured approach to hearing aid selection. Ear Hear 6: 226–239 [DOI] [PubMed] [Google Scholar]
- Dillon H. (2001). Hearing Aids. New York: Thieme [Google Scholar]
- Dirks DD, Kincaid GE. (1987). Basic acoustic considerations of ear canal probe measurements Ear Hear 8: 60S–67S [DOI] [PubMed] [Google Scholar]
- Eiten LR. (2005). The challenges and rewards of early identification. In: Seewald RC, Bamford J, eds, A Sound Foundation through Early Amplification: Proceedings of the 3rd International Conference. Stäfa, Switzerland: Phonak AG, 231–246
- Elberling C, Don M. (1987). Threshold characteristics of the human auditory brain stem response J Acoust Soc Am 81: 115–121 [DOI] [PubMed] [Google Scholar]
- Feigin JA, Kopun JG, Stelmachowicz PG, et al. (1989). Probe-tube microphone measures of ear-canal sound pressure levels in infants and children. Ear Hear 10: 254–258 [DOI] [PubMed] [Google Scholar]
- Fikret-Pasa S, Revit LJ. (1992). Individualized correction factors in the preselection of hearing aids J Speech Hear Res 35: 384–400 [DOI] [PubMed] [Google Scholar]
- Gagne JP, Seewald RC, Zelisko DL, et al. (1991). Procedure for defining the auditory area of hearing-impaired adolescents with severe/profound hearing loss I: Detection thresholds J Speech-Lang Pathol Audiol 12: 13–20 [Google Scholar]
- Gengel RW, Pascoe D, Shore I. (1971). A frequency-response procedure for evaluating and selecting hearing aids for severely hearing-impaired children. J Speech Hear Dis 36: 341–353 [DOI] [PubMed] [Google Scholar]
- Gorga MP, Kaminski JR, Beauchaine KL, et al. (1993). A comparison of auditory brain stem response thresholds and latencies elicited by air- and bone-conducted stimuli. Ear Hear 14: 85–94 [DOI] [PubMed] [Google Scholar]
- Hayes D, Jerger J. (1982). Auditory brainstem response (ABR) to tone-pips: Results in normal and hearing-impaired subjects Scand Audiol 11: 133–142 [DOI] [PubMed] [Google Scholar]
- Heinemann M, Bohnert A, Lippert KL, et al. (2001). Fitting of childrens' hearing aids on the basis of RECD-measurements and the DSL-procedure Zeitschrift fur Audiologie 40: 104–112 [Google Scholar]
- Hoover BM, Stelmachowicz PG, Lewis DE. (2000). Effect of earmold fit on predicted real ear SPL using a real ear to coupler difference procedure Ear Hear 21: 310–317 [DOI] [PubMed] [Google Scholar]
- International Standards Organization (1996). Acoustics—Reference zero for the calibration of audiometric equipment—Part 7: Reference threshold of hearing under free-field and diffuse-field listening conditions (ISO 389-7: 1996).
- Kiessling J. (1987). In situ audiometry (ISA): A new frontier in hearing aid selection Hear Instr 38: 28–29 [Google Scholar]
- Kruger B. (1987). An update on the external ear resonance in infants and young children. Ear Hear 8: 333–336 [DOI] [PubMed] [Google Scholar]
- Lewis DE, Stelmachowicz PG. (1993). Real ear to 6-cm3 coupler differences in young children. J Speech Hear Res 36: 204–209 [DOI] [PubMed] [Google Scholar]
- Modernizing Children's Hearing Aid Services (2002). Hearing aids for children: Fitting, verification and evaluation guidelines. Manchester, UK: Human Communication and Deafness Group, University of Manchester. [Google Scholar]
- Moodie KS, Seewald RC, Sinclair ST. (1994). Procedure for predicting real-ear hearing aid performance in young children Am J Audiol 3: 23–31 [Google Scholar]
- Moodie KS, Sinclair ST, Fisk T, et al. (1998). Case study: Individualizing hearing instrument fitting for infants. In: Seewald RC. ed. A Sound Foundation through Early Amplification: Proceedings of an International Conference. Stäfa, Switzerland: Phonak AG, 213–217
- Munnerley GM, Greville KA, Purdy SC, et al. (1991). Frequency-specific auditory brainstem responses relationship to behavioral thresholds in cochlear-impaired adults. Audiol 30: 25–32 [DOI] [PubMed] [Google Scholar]
- Munro KJ. (2004). Update on RECD measures in chidlren. In: Seewald RC, Bamford J. eds. A Sound Foundation through Early Amplification: Proceedings of the 3rd International Conference. Stäfa, Switzerland: Phonak AG, 71–89
- Munro KJ, Davis J. (2003). Deriving the real-ear SPL of audiometric data using the “coupler to dial difference” and the “real ear to coupler difference.” Ear Hear 24: 100–110 [DOI] [PubMed] [Google Scholar]
- Munro KJ, Hatton N. (2000). Customized acoustic transform functions and their accuracy at predicting real-ear hearing aid performance Ear Hear 21: 59–69 [DOI] [PubMed] [Google Scholar]
- Munro KJ, Lazenby A. (2001). Use of the “real-ear-to-dial difference” to derive real-ear SPL from hearing level obtained with insert earphones Br J Audiol 35: 297–306 [DOI] [PubMed] [Google Scholar]
- Munro KJ, Salisbury VA. (2002). Is the real-ear-to-coupler difference independent of the measurement earphone? Intl J Audiol 41: 408–413 [DOI] [PubMed] [Google Scholar]
- Munro KJ, Toal S. (2005). Measuring the RECD transfer function with an insert earphone and a hearing instrument: Are they the same? Ear Hear 26(1): 27–34 [DOI] [PubMed] [Google Scholar]
- Nelson Barlow NL, Auslander MC, et al. (1988). Probe-tube microphone measures in hearing-impaired children and adults. Ear Hear 9: 243–247 [DOI] [PubMed] [Google Scholar]
- Nousak JK, Stapells DR. (1999). Estimation of 1000-Hz behavioral threshold by tone-evoked auditory brainstem and middle-latency responses: Noise-masked normal-hearing subjects and subjects with sensorineural hearing loss Am Speech-Lang-Hear Assoc 41:204. [Google Scholar]
- Ontario Infant Hearing Program (2002). Prescription of amplification protocol and guidelines. Infant Hearing Program Implementation Support Document, Ministry of Children and Youth Services.
- Pediatric Working Group (1996). Amplification for infants and children with hearing loss Am J Audiol 5: 53–68 [Google Scholar]
- Picton TW, Ouellette J, Hamel G, et al. (1979). Brainstem evoked potentials to tonepips in notched noise J Otolaryngol 8: 289–314 [PubMed] [Google Scholar]
- Purdy SC, Abbas PJ. (1989). Auditory brainstem response audiometry using linearly and Blackmangated tonebursts Am Speech-Lang-Hear Assoc 31: 115–116 [Google Scholar]
- Revit LJ. (1997). The circle of decibels: Relating the hearing test, to the hearing instrument, to the real ear response Hear Rev 4: 35–38 [Google Scholar]
- Saunders GH, Morgan DE. (2003). Impact of measuring threshold in dB HL versus dB SPL on hearing aid targets Intl J Audiol 6: 319–326 [DOI] [PubMed] [Google Scholar]
- Scollie SD. (2003). Hearing aid test signals: What's new and what's good for kids? Hear J 56: 10–15 [Google Scholar]
- Scollie SD, Seewald RC. (2002). Hearing aid fitting and verification procedures for children. In: Katz J. ed. Handbook of Clinical Audiology. New York: Lippincott; Williams and Wilkins, 687–706 [Google Scholar]
- Scollie SD, Seewald RC, Cornelisse LE, et al. (1998). Validity and repeatability of level-independent HL to SPL transforms Ear Hear 19(5): 407–413 [DOI] [PubMed] [Google Scholar]
- Scollie SD, Steinberg MJ, Seewald RC. (2002). Evaluation of electroacoustic test signals II: Development and cross-validation of correction factors Ear Hear 23: 488–498 [DOI] [PubMed] [Google Scholar]
- Seewald RC. (1992). The desired sensation level method for fitting children: Version 3.0 Hear J 13: 460–463 [Google Scholar]
- Seewald RC, Cornelisse LE, Ramji KV, et al. (1997). DSL v4.1 for Windows: A software implementation of the desired sensation level (DSL[i/o]) method for fitting linear gain and wide-dynamic-range compression hearing instruments. Users' manual. London, ON: Hearing Health Care Research Unit [Google Scholar]
- Seewald RC, Moodie KS, Sinclair ST, et al. (1999). Predictive validity of a procedure for pediatric hearing instrument fitting AM J Audiol 8(2): 143–152 [DOI] [PubMed] [Google Scholar]
- Sinclair ST, Beauchaine KL, Moodie KS, et al. (1996). Repeatability of a real-ear-to-coupler difference measurement as a function of age Am J Audiol 5: 52–56 [Google Scholar]
- Sininger YA, Abdala C, Cone-Wesson B. (1997). Auditory threshold sensitivity of the human neonate as measured by the auditory brainstem response Hear Res 104: 27–38 [DOI] [PubMed] [Google Scholar]
- Stapells DR. (1989). Auditory brainstem response assessment of infants and children Sem Hear 10: 229–251 [Google Scholar]
- Stapells DR. (2000a). Frequency-specific evoked potential audiometry in infants. In: Seewald RC. ed. A Sound Foundation through Early Amplification: Proceedings of an International Conference. Stäfa, Switzerland: Phonak AG, 13–32
- Stapells DR. (2000b). Threshold estimation by the tone-evoked auditory brainstem response: A literature meta-analysis J Speech-Lang Pathol Audiol 24: 74–83 [Google Scholar]
- Stapells DR, Gravel JS, Martin BE. (1995). Thresholds for auditory brain stem responses to tones in notched noise from infants and young children with normal hearing or sensorineural hearing loss Ear Hear 16: 361–371 [DOI] [PubMed] [Google Scholar]
- Stapells DR, Herdman A, Small SA, et al. (2005). Current status of the auditory steady state responses for estimating an infant's audiogram. In Seewald RC, Bamford J, eds: A Sound Foundation through Early Amplification: Proceedings of the 3rd International Conference. Stäfa, Switzerland: Phonak AG, 43–59
- Stapells DR, Oates P. (1997). Pure-tone behavioral threshold estimates obtained using the auditory brainstem response. A review. Audiol Neuro-Otol 2: 257–280 [DOI] [PubMed] [Google Scholar]
- Stapells DR, Picton TW, Durieux-Smith A, et al. (1990). Thresholds for short-latency auditory-evoked potentials to tones in notched noise in normal-hearing and hearing-impaired subjects Audiol 29: 262–274 [DOI] [PubMed] [Google Scholar]
- Stapells DR, Ruben RJ. (1989). Auditory brain stem responses to bone-conducted tones in infants Annals Otol Rhinol Laryngol 98: 941–949 [DOI] [PubMed] [Google Scholar]
- Suzuki JI, Kodera K, Yamada O. (1984). Brainstem response audiometry in newborns and hearing impaired infants. In Starr A, Rosenberg C, Don M, Davis H. eds. Sensory Evoked Potentials 1. An International Conference on Standards for Auditory Brainstem Response (ABR) Testing. Milan: CRS Amplifon, 85–93 [Google Scholar]
- Tabachnick BG, Fidell LS. (1996). Cleaning up your act: Screening data prior to analysis. Using Multivariate Statistics (3rd ed.). New York: Harper Collins College Publishers, 57–126 [Google Scholar]
- Tharpe AM, Sladen D, Huta HM, et al. (2001). Practical considerations of real-ear-to-coupler difference measures in infants Am J Audiol 10: 41–49 [DOI] [PubMed] [Google Scholar]
- Valente M, Potts LG, Valente M, et al. (1994). Intersubject variability of real-ear sound pressure level: Conventional and insert earphones J Am Acad Audiol 5: 390–398 [PubMed] [Google Scholar]
- Westwood GF, Bamford JM. (1995). Probe-tube microphone measures with very young infants: Real ear to coupler differences and longitudinal changes in real ear unaided response. Ear Hear 16: 263–273 [DOI] [PubMed] [Google Scholar]
- Zelisko DL, Seewald RC, Gagné JP. (1992). Signal delivery/real-ear measurement system for hearing aid fitting. Ear Hear 13(6): 460–463 [PubMed] [Google Scholar]
- Zwislocki J. (1960). Theory of temporal auditory summation J Acoust Soc Am 32: 1046–1060 [Google Scholar]