Abstract
Objective
To examine associations between modifications in parent feeding practices, child diet, and child weight status after treatment and to evaluate dietary mediators.
Design and Methods
Children classified as overweight or obese and 7-11 years old (N=170) completed a 16-session family-based behavioral treatment program (FBT). Anthropometrics (standardized body mass index (zBMI)), Child Feeding Questionnaire, and 24-hr dietary recalls were collected at baseline and post-FBT. Linear regression predicted child zBMI change. Single and multiple mediation tested child dietary modifications as mediators between change in parent feeding practices and child zBMI.
Results
Restrictive parent feeding practices significantly decreased during FBT. Reductions in parent restriction, child weight concern, child total energy intake, and percent energy from fat, and increases in parent perceived responsibility, and child percent energy from protein, predicted reductions in child zBMI. Change in child total energy intake mediated the relation between parent restriction and child zBMI change after accounting for covariates and additional dietary mediators.
Conclusions
FBT is associated with a decrease in parental restriction, which is associated with reductions in child relative weight, which was mediated by a decrease in child energy intake. Teaching parents to reduce children's energy intake without being overly restrictive may improve child weight.
Keywords: childhood obesity, parents, eating behaviors, weight loss
Introduction
Pediatric obesity represents a major health crisis, as excess weight in childhood is associated with numerous physiological and psychological consequences. 1-4 Recommendations for pediatric obesity treatment support the use of comprehensive multidisciplinary interventions that emphasize diet, activity, and behavior change.5 Family-based treatment (FBT) is an evidence based intervention for pediatric obesity, which simultaneously treats both parent and child with obesity, using a comprehensive approach aimed to reduce energy intake, increase physical activity, improve family behaviors, and modify the home environment. While there are extensive efficacy data on FBT, data are limited regarding the best parent feeding styles, an important factor that may impact child weight change during treatment.
Restrictive parent feeding practices, or excessive control over when and how much food a child eats, have drawn a great deal of attention due to their negative influence on child weight and food intake.6-8 During treatment or attempted weight loss, parents may adopt a restrictive feeding style as they attempt to eliminate the consumption and access to energy-dense foods; however, the conceptualization of specific foods as forbidden may lead to preoccupation and increased desire for and consumption of that food,6,9 hindering weight loss. An overly restrictive approach, where the child is not allowed to make independent choices and parents make all food-related decisions, may increase the reinforcing value of ‘forbidden’ foods,10,11 which has been associated with weight gain12 and blunted response to weight loss treatment in children.13 Alternatively, an overly permissive approach that relies on children to make healthful choices in unhealthy contexts makes it unlikely that children will achieve better weight management. FBT attempts to strike a balance between excessive control and permissiveness by encouraging parents to allow consumption of RED foods (high calorie, energy-dense foods) in moderation and create a healthy home environment that fosters better child self-regulation and choice. In fact, initial research has shown that FBT is associated with a reduction in parental restriction, which was associated with decreased child weight status.14 These results suggest there are other ways to foster negative energy balance to achieve weight loss than excessive parental restriction, or being the “food police,” yet the potential mechanisms have not been explored.
Restrictive parent feeding practices have shown to negatively impact child dietary intake in favor of excess calories and added sugars, which could lead to increased body weight.15,16 Accordingly, it is plausible that decreases in restrictive feeding practices while enhancing the diet quality of the home food environment may facilitate positive changes in child food intake and improve treatment response. Evidence to support the association between parental restriction and child diet comes primarily from laboratory feeding studies and may not generalize to eating in a natural environment.6,9,15,16 Consequently, examination of the influence of parent feeding practices on usual intakes within FBT is warranted.
Therefore the aims of this study were to: 1) identify modifications in parent feeding practices and child dietary intake that predict improvements in child zBMI following FBT; and 2) identify child dietary modifications that mediate the relation between change in parent feeding practices and child zBMI. We hypothesized that modifications in parent feeding practices and child diet would result in decreases in child zBMI and that the relation between parent feeding practices and child zBMI would be partially mediated by dietary changes.
Methods and Procedures
Study Design
This study evaluated data from the weight loss phase of a larger multi-site randomized controlled trial to evaluate the effects of maintenance treatments on relative weight among children with overweight/obesity. The participating parent and child were assessed at baseline and post-FBT and completed anthropometrics, questionnaires, and 24-hour recalls. Families were recruited and attended treatment sessions at two clinical sites located in the United States. Families attended sixteen weekly sessions conducted by trained interventionists. All participants provided informed consent, and the Institutional Review Boards at each site approved the study protocol.
Family-based Behavioral Treatment
FBT is an evidence-based, multicomponent intervention that targets diet, activity, behavioral techniques, and parenting skills. The Traffic Light Eating Plan, which classifies foods and activities into RED, YELLOW, and GREEN categories (defined below), was used.17 FBT modifies the shared family environment by encouraging parents to remove RED (energy-dense) foods from the home, while making GREEN (nutrient-dense) foods readily available to create an environment that promotes healthy choices and eliminates the need to be overly restrictive so the child does not feel deprived. Additionally, parents are taught to model healthy behaviors and implement household changes to create a supportive environment rather than targeting the child in isolation. Positive reinforcers for healthy behavior change, such as rewards for achieving behavioral goals were also used (i.e., increasing GREEN foods to ≥ 5 servings/day and decreasing RED foods to ≤ 15 servings/week).
Participants
Families were recruited via advertisements through fliers, newspapers, television, radio, referrals from schools and community providers, and word of mouth. Families were excluded if either child or parent were participating in another weight control program, had major psychiatric problems or previous eating disorder diagnosis, food allergies limiting diet participation, and/or physical activity limitations that impeded moderate to vigorous physical activity. Participants were 170 children with BMI≥85th percentile for age and sex, 7-11 years old, and at least one parent with BMI ≥25 kg/m2.
Measures
Parent attitude/feeding practices
Parent feeding practices were measured using the Child Feeding Questionnaire (CFQ).8 The CFQ is a validated questionnaire that assesses the following domains: perceived responsibility (parent feeling of responsibility for the quantity and quality of the child's diet); perceived child overweight (parent perception of child weight status); child weight concern (degree of parent concern for child weight gain); monitoring (degree of parent monitoring of energy-dense, high-fat food consumption); restriction (degree of parent control over access to palatable foods); and pressure to eat (degree of parent encouragement to eat more food).
Demographics
Demographics were collected via the Barratt (Hollingshead Modified) Demographics Questionnaire to assess child and parent race, ethnicity, age, sex, and household income.18
Anthropometrics
Child height and weight were measured in light clothing without shoes using a stadiometer and calibrated digital scale, to the nearest 0.1cm and 0.1kg, respectively. The average of three measurements was calculated to determine the final value. Body mass index was calculated by dividing weight (kg) by height (m2). Child zBMI was computed based on CDC normative data and the LMS method.19
Dietary Intake
Child dietary intake was assessed via three telephone-administered 24-hr recalls using the Nutrition Data System for Research (NDSR version 2009, Nutrition Coordinating Center, University of Minnesota). This assessment is considered to be the most accurate method for children aged 4-11 years.20 Parents reported on child intake and were assisted by the child if present. Recalls were conducted on non-consecutive days, using at least one weekday and one weekend day. Mean intakes for each nutrient/food group were averaged across the three days for each time point.
Dietary recall reporting status was determined using the method developed by Huang and colleagues.21 Predicted energy requirement (pER) was calculated using sex-specific equations for overweight boys and girls ages 3-18 years of age.22 To account for low fitness and physical activity levels (PAL) of children with obesity,23,24 the sedentary PAL category was used since the majority (90.2%) of our sample was classified as obese. The ±2SD cutoff was chosen to identify plausible reporters, given that the incidence of underreporting is higher in children with obesity.25 This cutoff may provide better representation of variation in daily intakes,26 and it has been used previously in both children27 and adults. 28 Thus, plausible reporters were defined as those within ±2SD of their pER (reported energy intake ≥135% and ≤65% of pER). Misreporting was also estimated using the Goldberg method,26 but since results were similar, only data using the Huang method are presented.
Statistical Methods
Differences between plausible and implausible reporters were determined using t-tests and chi-square analyses. Differences between baseline and post-FBT variables were determined using paired samples t tests or the nonparametric Related-Samples Wilcoxon signed-rank test. Change variables were calculated by subtracting baseline from post-FBT. Linear regression examined associations between parent feeding practices, child diet, and child zBMI. All models included child age, sex, race/ethnicity, baseline weight status, household income, baseline parent feeding practice (for parent attitude/feeding practice change variables) or baseline diet variable (for diet change variables), and change in energy intake (for all remaining diet change variables) as covariates. Residual diagnostics were evaluated for each model using histograms, normal P-P plots, and plots of standardized residuals against predicted values.
Single and multiple mediation assessed mediating effects of change in child diet on the relation between change in parent feeding practices and change in child zBMI.29 Models for each parent feeding practice that significantly predicted change in child zBMI were tested in both all children and plausible reporters. Parent feeding practice variables were entered as the independent variable and dietary variables associated with weight loss were included as mediators. The magnitude of the indirect effect was assessed using a nonparametric, bootstrapping procedure. Confidence intervals of the indirect effect were constructed using 20,000 bootstrap resamples from the SPSS macro INDIRECT.29 The indirect effect was considered significant if the 95% confidence interval did not contain zero. The proportion mediated was calculated by dividing indirect effect by total effect (path a * path b / path c). Alpha was set at P<0.05. Results are presented for plausible reporters and also for the full sample, since the classification of misreporting is merely an assumption and stratification may be more informative than elimination of a large portion of the sample.30 All analyses were conducted using SPSS version 19.
Results
Sample characteristics
Sample characteristics are described in Table 1. Mean (±SD) child baseline zBMI and age in the full sample were 2.16±0.39 and 9.4±1.2 years, respectively. After accounting for reporting bias, 75.3% of the sample was classified as plausible reporters. The mean age of plausible and implausible reporters was similar; however, plausible reporters had a significantly lower baseline zBMI and were more likely to be female and White as compared to implausible reporters. Plausible reporters also reported higher income than implausible reporters, which trended toward significance (P=0.061).
Table 1. Baseline characteristics of the study sample and differences by reporting status.
| Characteristic | All children (n=170) | Reporting Status | P value1 | |
|---|---|---|---|---|
|
| ||||
| Plausible (n=128) | Implausible (n=42) | |||
| zBMI2 | 2.16±0.39 | 2.10±0.41 | 2.36±0.25 | <0.001 |
| Age (years)2 | 9.4±1.2 | 9.3±1.2 | 9.7±1.2 | 0.114 |
| Sex [n(%)] | ||||
| Male | 66(38.8) | 40(31.3) | 26(61.9) | <0.001 |
| Female | 104(61.2) | 88(68.8) | 16(38.1) | |
| Race [n(%)] | ||||
| African American | 29(17.1) | 16(12.5) | 13(31.0) | 0.022 |
| White | 119(70.0) | 95(74.2) | 24(57.1) | |
| Other | 22(12.9) | 17(13.3) | 5(11.9) | |
| Ethnicity [n(%)] | ||||
| Hispanic | 17(10.0) | 15(11.7) | 2(4.8) | 0.192 |
| Non-Hispanic | 153(90.0) | 113(88.3) | 40 (95.2) | |
| Annual household income [n(%)] | ||||
| <$50,000 | 42(24.7) | 27(21.1) | 15(35.7) | 0.057 |
| ≥$50,000 | 128(75.3) | 101(78.9) | 27(64.3) | |
zBMI = Standardized body mass index.
Indicates significant differences between plausible and implausible reporters.
Mean ± standard deviation
Post-FBT changes in parent feeding practices and child dietary intake
Changes in parent feeding practices and child dietary intake were evident from before to end of treatment (Table 2). In plausible reporters, scores for parent perceived child overweight and monitoring significantly increased, and parent child weight concern and restriction significantly decreased (P<0.001). Following FBT, children had significantly reduced total energy, percent energy from fat, sugar-sweetened beverages, added sugars, and added fats, while increasing percent energy from protein, percent energy from carbohydrate, fiber, and total fruits and vegetables (P<0.001). Results in all children were similar.
Table 2. Baseline, post-FBT, and change in child dietary intake and parent attitude/feeding practices by reporting status.
| All Children (N=170) | Plausible reporters (n=128) | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Baseline | Post-FBT | Change | Baseline | Post-FBT | Change | |
| zBMI | 2.16±0.39 | 1.87±0.56*** | -0.29±0.24 | 2.10±0.41 | 1.78±0.58*** | -0.32±0.26 |
| Parent attitude/feeding practices | ||||||
| Perceived responsibility | 2.9±0.7 | 3.0±0.7 | 0.1±0.6 | 2.9±0.7 | 2.9±0.7 | 0.0±0.6 |
| Perceived child overweight | 2.5±0.4 | 3.5±0.6*** | 1.0±0.6 | 2.4±0.4 | 3.5±0.6*** | 1.1±0.6 |
| Child weight concern | 3.1±0.8 | 2.7±1.0*** | -0.4±1.0 | 3.1±0.8 | 2.6±1.0*** | -0.5±1.0 |
| Monitoring | 2.5±0.8 | 3.4±0.7*** | 0.9±1.0 | 2.6±0.8 | 3.4±0.6*** | 0.9±1.0 |
| Restriction | 2.9±0.6 | 2.5±0.7*** | -0.4±0.7 | 2.9±0.5 | 2.5±0.7*** | -0.4±0.7 |
| Pressure to eat | 0.7±0.7 | 0.7±0.7 | 0.0±0.7 | 0.6±0.7 | 0.6±0.7 | -0.0±0.7 |
| Child dietary intake | ||||||
| Energy (kcals) | 1708.4±440.8 | 1351.5±296.1*** | -357.0±444.8 | 1785.5±395.5 | 1370.7±296.9*** | -414.9±394.3 |
| Percent energy from protein (%) | 16.4±3.0 | 18.7±3.6*** | 2.3±3.7 | 16.1±2.8 | 18.5±3.6*** | 2.5±3.7 |
| Percent energy from fat (%) | 31.5±4.9 | 24.6±6.2*** | -6.9±7.0 | 31.7±4.6 | 24.4±6.1*** | -7.3±6.9 |
| Percent energy from carbohydrate (%) | 52.1±5.6 | 56.7±6.4*** | 4.6±7.2 | 52.2±5.3 | 57.1±6.4*** | 4.9±7.1 |
| Fiber (g) | 13.7±4.5 | 16.0±5.6*** | 2.3±6.1 | 14.1±4.5 | 16.2±5.6*** | 2.1±6.0 |
| Total Fruit and Vegetables (svg/d) | 2.4±1.4 | 3.8±2.1*** | 1.4±2.1 | 2.4±1.5 | 3.9±2.1*** | 1.5±2.1 |
| Sugar Sweetened Beverages (svg/d) | 0.6±0.6 | 0.2±0.4*** | -0.4±0.7 | 0.7±0.7 | 0.2±0.3*** | -0.5±0.7 |
| Added Sugars (g) | 68.3±36.1 | 35.9±21.7*** | -32.4±38.8 | 74.0±38.4 | 36.9±22.2*** | -37.2±41.3 |
| Added Fats (svg/d) | 1.8±1.4 | 1.0±0.8*** | -0.7±1.6 | 1.9±1.4 | 1.0±0.8*** | -0.8±1.6 |
All values represent mean ± standard deviation.
Significantly different between baseline and post-FBT at P <0.001.
Associations with child zBMI change
Associations with change in child zBMI are shown in Table 3. In plausible reporters, increased parent perceived responsibility and child percent energy from protein and decreased parent restriction, parent child weight concern, child total energy intake, and child percent energy from fat were associated with decreased child zBMI (P<0.05). When data from all children were analyzed, decreased child consumption of added sugars and increased total fruits and vegetables also predicted decreased child zBMI (P<0.05).
Table 3. Association between post-FBT changes in parent feeding practices and child dietary intake with child zBMI change1.
| Independent variable | All Children (N=170) | Plausible reporters (n=128) | ||
|---|---|---|---|---|
|
|
|
|||
| β | P value | β | P value | |
| Change in parent attitude/feeding practices | ||||
| Perceived responsibility | -0.153 | 0.031 | -0.160 | 0.059 |
| Perceived child overweight | -0.083 | 0.344 | -0.063 | 0.525 |
| Child weight concern | 0.229 | 0.001 | 0.242 | 0.003 |
| Monitoring | -0.177 | 0.057 | -0.183 | 0.130 |
| Restriction | 0.250 | 0.001 | 0.261 | 0.002 |
| Pressure to eat | -0.097 | 0.187 | -0.076 | 0.397 |
| Change in child dietary intake | ||||
| Energy (kcals) | 0.378 | <0.001 | 0.382 | <0.000 |
| Percent energy from protein (%) | −0.212 | 0.003 | -0.230 | 0.006 |
| Percent energy from fat (%) | 0.166 | 0.026 | 0.184 | 0.032 |
| Percent energy from carbohydrate (%) | –0.036 | 0.629 | -0.044 | 0.600 |
| Fiber (g) | –0.120 | 0.097 | -0.110 | 0.185 |
| Total Fruit and Vegetables (svg/d) | -0.144 | 0.031 | -0.127 | 0.105 |
| Sugar Sweetened Beverages (svg/d) | 0.223 | 0.060 | 0.156 | 0.343 |
| Added Sugars (g) | 0.307 | 0.008 | 0.213 | 0.145 |
| Added Fats (svg/d) | 0.208 | 0.088 | 0.235 | 0.106 |
Data are standardized regression coefficients from linear regression models adjusted for child age, child sex, child race/ethnicity, household income, child baseline weight status, baseline parent feeding practice (for parent attitude/feeding practices) or eating behavior (for change in child dietary intake variables), and change in energy intake (among the remaining child dietary intake variables).
Mediating effects of dietary modifications
Mediation models to test the mediating effects of dietary modifications on the association between parent perceived responsibility and parent concern about child weight and change in child zBMI were not significant and thus, only the results for parent restriction are presented. In plausible reporters, change in child total energy intake and child percent energy from protein significantly mediated the association between change in parent restriction and change in child zBMI when tested in single mediation models, proportion mediation 18.7% and 21.5%, respectively; indirect effects and confidence intervals for the energy model and the percent energy from protein model were 0.0181 (0.0026, 0.0447, P<0.05) and 0.0186 (0.0028, 0.0512, P<0.05), respectively. Change in percent energy from fat was not a significant mediator (data not shown) in the model using plausible reporters. These results indicate that as parents became less restrictive, children consumed less total energy and more energy from protein as a percent of total energy, which resulted in reductions in child zBMI. When single mediation models were conducted in all children, change in child total energy, child percent energy from protein, and child added sugars acted as significant mediators of the association between change in parent restriction and change in child zBMI (P<0.05), proportion mediated 17.6%, 20.4%, and 13.0%, respectively. The indirect effects and bias corrected bootstrapping confidence intervals for the energy model, percent energy from protein model, and added sugars model were 0.0144 (0.0021, 0.0346, P<0.05), 0.0167 (0.0042, 0.0390, P<0.05), and 0.0009 (0.0009, 0.0219, P<0.05), respectively. Models testing change in percent energy from fat and fruits and vegetables were not significant (data not shown).
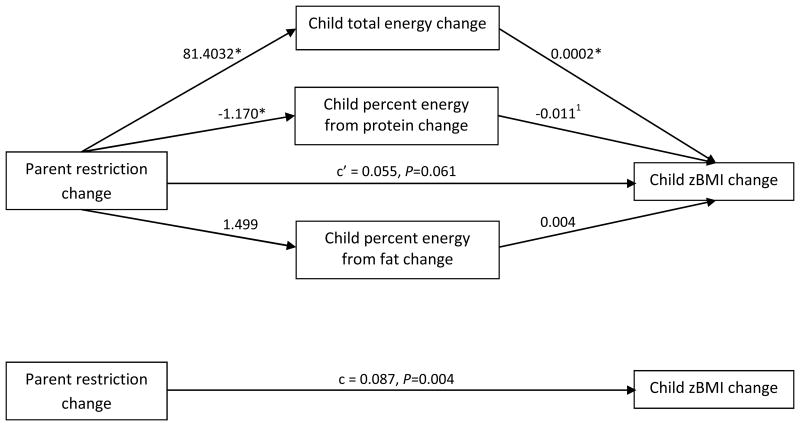
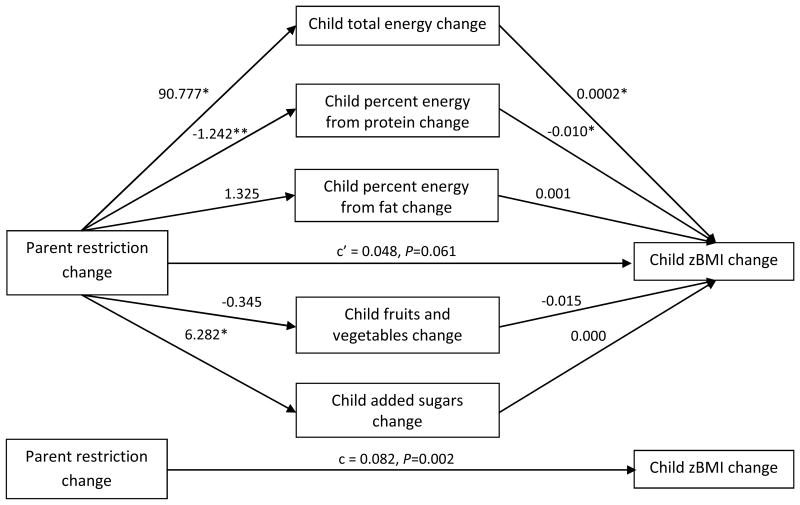
Multiple mediation models using all significant dietary predictors of change in child zBMI were also conducted. In plausible reporters (figure 1), paths a and b were significant for total energy (P≤0.05). The bootstrapped confidence intervals indicated the indirect effect of change in parent restriction on change in zBMI through change in child total energy intake was significant (P<0.05). Portion mediated by child total energy intake was 18.7%. The full model explained 47.2% of the variance in change in zBMI. In all children (figure 2), path a was significant for child total energy, percent energy from protein, and added sugars (P<0.05). Path b was significant for child total energy and percent energy from protein (P<0.05). A mediation effect for child total energy and percent energy from protein was evident (P<0.05). Proportion mediated by change in child total energy was 22.1% and that by change in percent energy from protein was 15.1%.
Figure 1.
Multiple mediation model for plausible reporters only (n=128, which tests the mediating effects of changes in dietary intake on the relationship between change in parent restriction and change in child zBMI, adjusting for child age, child gender, child race/ethnicity, household income, child baseline weight status, baseline restriction score, and baseline eating behavior. Unstandardized regression coefficients for each path are presented. The indirect effects and the bias corrected bootstrapping confidence intervals of change in energy are 0.012 (0.0002, 0.0356)*. Model R-square was 0.472.
Figure 2.
Multiple mediation model for ALL CHILDREN (n=170), which tests the mediating effects of changes in dietary intake on the relationship between change in parent restriction and change in child zBMI, adjusting for child age, child gender, child race/ethnicity, household income, child baseline weight status, baseline restriction score, and baseline eating behavior. Unstandardized regression coefficients for each path are presented. The indirect effects and the bias corrected bootstrapping confidence intervals of change in energy and change in percent energy from protein are 0.015 (0.0003, 0.0448)* and 0.012 (0.0008, 0.0361)*, respectively. Model R-square was 0.499. *P<0.05, **P<0.01
Because the mediation models testing change in parent restrictive feeding practices were significant, individual questions of the restriction subscale were examined to identify the specific aspects of parental restriction that were modified after treatment. Mean scores for individual questions are shown in Table 4. Scores for all but one question decreased after treatment. The question “I intentionally keep some foods out of my child's reach” increased, but this change was non-significant in plausible reporters.
Table 4. Baseline, post-FBT, and change in individual questions of the restriction subscale from the Child Feeding Questionnaire.
| All Children (N=170) | Plausible reporters (n=128) | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Baseline | 4 months | Change | Baseline | 4 months | Change | |
| I have to be sure that my child does not eat too many sweets (candy, ice cream, cake or pastries) | 3.6 ± 0.8 | 3.3 ± 1.0 | -0.3±1.1*** | 3.7 ± 0.7 | 3.3 ± 1.0 | -0.3±1.1** |
| I have to be sure that my child does not eat too many high-fat foods | 3.7 ±0.6 | 3.4±0.9 | -0.3±1.0*** | 3.7 ±0.6 | 3.4±0.9 | -0.3±1.0** |
| I have to be sure that my child does not eat too much of his or her favorite foods | 3.4±0.8 | 3.2±0.9 | -0.3±1.0** | 3.4±0.8 | 3.2±0.9 | -0.2±1.0* |
| I intentionally keep some foods out of my child's reach | 2.7±1.5 | 3.1±1.4 | 0.3±1.7* | 2.8±1.4 | 3.0±1.4 | 0.3±1.7 |
| I offer sweets (candy, ice cream, cake, pastries) to my child as a reward for good behavior | 1.5±1.3 | 0.6±0.9 | -0.9±1.5*** | 1.5±1.3 | 0.6±0.9 | -0.9±1.5*** |
| I offer my child his or her favorite foods in exchange for good behavior | 1.3±1.3 | 0.6±1.0 | -0.8±1.4*** | 1.4±1.3 | 0.6±1.0 | -0.8±1.4*** |
| If I did not guide or regulate my child's eating, he or she would eat too many junk foods | 3.3±1.0 | 2.9±1.3 | -0.4±1.3*** | 3.4±0.9 | 2.9±1.3 | -0.4±1.4** |
| If I did not guide or regulate my child's eating, he or she would eat too much of his or her favorite foods | 3.5±0.9 | 3.1±1.1 | -0.4±1.1*** | 3.5±0.8 | 3.1±1.1 | -0.4±1.2*** |
All values represent mean ± standard deviation.
P<0.05,
P<0.01,
P<0.001
Discussion
Reductions in restrictive parent feeding practices during treatment promoted improvements in child zBMI, and this association was mediated by reductions in child energy intake. These findings highlight the importance of targeting parental feeding practices during FBT and are in support of the existing data that suggest parent attitudes and feeding practices are modifiable constructs that can impact treatment outcomes.14 Previous research has demonstrated a link between high levels of parental restriction and increased child weight and energy intake. The present study builds upon these findings to show that modifications in parental restriction within the context of treatment may reverse these negative associations, resulting in reduced child energy intake and improvements in child relative weight.
All aspects of parental restriction decreased after treatment except intentionally keeping foods out of a child's reach. There are two aspects of the Traffic Light Eating Plan component of FBT that may have elicited these findings: 1) encouraging moderate consumption (i.e., 2 servings/day) of RED foods within energy needs, rather than elimination; and 2) eliminating RED foods in the home to limit temptation. A central tenet of contemporary FBT is the role of choice and the importance of providing a choice among many healthy foods, which can improve food selection.31 In support of this tenet, a study by Epstein and colleagues14 examined the effects of two FBT approaches targeting either increasing healthy eating or reducing high energy-dense foods on child weight loss. At 24-month follow up weight loss was significantly greater in the increase healthy eating condition than the reducing high energy-dense foods condition. The authors speculate that by focusing on increasing healthy foods, families may have altered their food purchasing habits and changed the home environment, which increased access to healthier dietary choices. These results provide support for the concept of “covert” control, a feeding style defined as controlling a child's food intake in a way that cannot be detected by the child,32 which has been associated with positive dietary behaviors.33 Therefore, the primary goal for parents is to reduce intake without creating feelings of deprivation in the child. This goal may be difficult to achieve in situations in which, prior to treatment, a family had unlimited access to unhealthy foods (e.g., potato chips or sugar sweetened beverages). Total, rapid elimination of these foods may result in greater feelings of deprivation and restriction in a child from this environment than a child who never had access to these foods at home. Similarly, effects of restriction of a particular food may differ based on the alternatives that are available. It may be easier to resist a specific food if there is a choice of palatable alternatives available than if no choice is available.31 Thus, strategies to reduce restrictive feeding practices and improve child weight include: 1) eliminating high-fat snacks from the home and replacing with readily available healthy alternatives (e.g., fruits, vegetables, and low-fat dairy products); 2) stimulus control to reduce eating prompts such as changing the daily routine to include non-sedentary after school activities in place of television, 3) making household changes so that all family members adopt the new eating habits and no one is singled out, 4) parent modeling of healthy eating and activity behaviors, and 5) moderating rather than restricting consumption of RED foods to fit within energy needs.
Increased perceived responsibility and decreased child weight concern also predicted reductions in child zBMI and complement the parent restriction findings to establish a solid parenting approach to improve child weight. The association between increased parent responsibility and improved child weight may have resulted from greater parental attention to the establishment of a healthy home environment and routines, which is a major component of FBT. Our results for parent concern about child weight are similar to those reported by Epstein et al., (2008), and may reflect a change in attitude as parent and child become actively engaged in treatment. FBT empowers children with knowledge and skills to adopt healthy behaviors independently, which may shift some responsibility for in the moment decisions from parent to child. Once parents have established a home environment that supports healthy behaviors, children are encouraged to make choices from a variety of healthy options. As the child becomes more autonomous in eating-related decisions, the parent may feel less concerned about the child's weight and be less likely to engage in controlling feeding practices.34 We did not elucidate a mechanism to explain these associations with child zBMI change. These constructs reflect parent attitudes, which are not directly related to child dietary behaviors and thus, may act through another energy balance behavior (e.g., physical activity).
To our knowledge, this is the first study to directly link improvements in child zBMI with specific dietary modifications. In particular, child modifications in total energy, percent energy from protein, and percent energy from fat were associated with zBMI change and these associations remained after accounting for reporting bias. Because successful weight loss can only be achieved during a state of negative energy balance, a reduction in caloric intake is the cornerstone of obesity treatment.35 Thus, it is not surprising that reductions in child total energy intake were associated with zBMI change. Our results regarding percent energy from protein contrast with Kirk and colleagues36 who reported no difference in weight loss between children assigned to diets that varied in macronutrient content after a 3-month intervention. In our study, increased percent energy from protein was accompanied by decreased percent energy from fat, which could have been accomplished by replacing high-fat sources of protein with low-fat sources (e.g., lean meats, low-fat dairy, and legumes). These dietary changes are encouraged in the Traffic Light Eating Plan and recommended by national nutrition guidelines, and they could potentially explain the effects on improved weight outcomes.
The strengths of this study include the large multi-site sample of treatment-seeking children with overweight/obesity and that most results remained significant after stratification by child dietary reporting status. Limitations include self-reported measures for dietary intake and parent feeding practices. Additionally, change in restriction and change in diet were measured only at baseline and post-FBT, thus the temporal order of the association to zBMI change cannot be confirmed. It is possible that parent feeding practices changed only after observing improvements in child weight.
In conclusion, these results underscore the importance of including parental feeding practices as treatment targets for pediatric weight loss, specifically, reducing restrictive parent feeding practices. For example, children should be allowed to select foods from a variety of healthy options, and parents should focus on what children can eat instead of what they cannot. Additionally, an allowance of moderate consumption of less healthful foods within energy needs may produce calorie reduction without causing children to feel overly deprived. Our results also support prescribing a diet lower in calories, fat, and added sugars, and higher in low-fat sources of protein and fruits and vegetables for pediatric obesity treatment. These results are important to consider within the framework of FBT approaches and highlight the critical role of parents in addressing pediatric obesity.
What is already known about the subject: Restrictive parent feeding practices have been associated with elevated child weight and food intake
What this study adds: Reductions in restrictive parent feeding practices during treatment were associated with greater decreases in child zBMI and this association was mediated by a decrease in energy intake
Acknowledgments
Jodi Cahill Holland carried out all data analysis and data interpretation and wrote the manuscript. Rachel Kolko, Richard Stein, and R. Robinson Welch delivered the treatment and helped manage the study. Ken Schectman approved all statistical analyses. Richard Stein, Michael Perri, Brian Saelens, Len Epstein, and Denise Wilfley designed the primary trial. All authors were involved in writing the paper and had final approval of the submitted version. The authors would like to thank Mary Bednarski and Michael Wallendorf for their contributions on management of the data. This work was supported by NIH grant 2 R01 HD036904-06 (NICHD). Jodi Cahill Holland and Rachel P. Kolko were supported by NIH grant 5T32HL007456 (NHLBI) and Richard I. Stein was supported by NIH grant KL2RR024994.
Footnotes
Conflict of Interest: The authors declared no conflict of interest.
References
- 1.Davison KK, Markey CN, Birch LL. A longitudinal examination of patterns in girls' weight concerns and body dissatisfaction from ages 5 to 9 years. Int J Eat Disord. 2003;33:320–332. doi: 10.1002/eat.10142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Latner JD, Stunkard AJ. Getting worse: the stigmatization of obese children. Obes Res. 2003;11:452–456. doi: 10.1038/oby.2003.61. [DOI] [PubMed] [Google Scholar]
- 3.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103:1175–1182. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 4.Dockray S, Susman EJ, Dorn LD. Depression, cortisol reactivity, and obesity in childhood and adolescence. J Adolesc Health. 2009;45:344–350. doi: 10.1016/j.jadohealth.2009.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 6.Fisher JO, Birch LL. Restricting access to palatable foods affects children's behavioral response, food selection, and intake. Am J Clin Nutr. 1999;69:1264–1272. doi: 10.1093/ajcn/69.6.1264. [DOI] [PubMed] [Google Scholar]
- 7.Faith MS, Berkowitz RI, Stallings VA, Kerns J, Storey M, Stunkard AJ. Parental feeding attitudes and styles and child body mass index: prospective analysis of a gene-environment interaction. Pediatrics. 2004;114:e429–436. doi: 10.1542/peds.2003-1075-L. [DOI] [PubMed] [Google Scholar]
- 8.Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36:201–210. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- 9.Jansen E, Mulkens S, Jansen A. Do not eat the red food!: prohibition of snacks leads to their relatively higher consumption in children. Appetite. 2007;49:572–577. doi: 10.1016/j.appet.2007.03.229. [DOI] [PubMed] [Google Scholar]
- 10.Epstein LH, Truesdale R, Wojcik A, Paluch RA, Raynor HA. Effects of deprivation on hedonics and reinforcing value of food. Physiol Behav. 2003;78:221–227. doi: 10.1016/s0031-9384(02)00978-2. [DOI] [PubMed] [Google Scholar]
- 11.Raynor HA, Epstein LH. The relative-reinforcing value of food under differing levels of food deprivation and restriction. Appetite. 2003;40:15–24. doi: 10.1016/s0195-6663(02)00161-7. [DOI] [PubMed] [Google Scholar]
- 12.Hill C, Saxton J, Webber L, Blundell J, Wardle J. The relative reinforcing value of food predicts weight gain in a longitudinal study of 7--10-y-old children. Am J Clin Nutr. 2009;90:276–281. doi: 10.3945/ajcn.2009.27479. [DOI] [PubMed] [Google Scholar]
- 13.Best JR, Theim KR, Gredysa DM, et al. Behavioral economic predictors of overweight children's weight loss. J Consult Clin Psychol. 2012;80:1086–1096. doi: 10.1037/a0029827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Epstein LH, Paluch RA, Beecher MD, Roemmich JN. Increasing healthy eating vs. reducing high energy-dense foods to treat pediatric obesity. Obesity (Silver Spring) 2008;16:318–326. doi: 10.1038/oby.2007.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klesges RC, Stein RJ, Eck LH, Isbell TR, Klesges LM. Parental influence on food selection in young children and its relationships to childhood obesity. Am J Clin Nutr. 1991;53:859–864. doi: 10.1093/ajcn/53.4.859. [DOI] [PubMed] [Google Scholar]
- 16.Birch LL, Fisher JO. Mothers' child-feeding practices influence daughters' eating and weight. Am J Clin Nutr. 2000;71:1054–1061. doi: 10.1093/ajcn/71.5.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Valoski A, Epstein LH. Nutrient intake of obese children in a family-based behavioral weight control program. Int J Obes. 1990;14:667–677. [PubMed] [Google Scholar]
- 18.Hollingshead AB. Four-factor Index of social status. New Haven, CT: Yale University; 1975. [Google Scholar]
- 19.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002:1–190. [PubMed] [Google Scholar]
- 20.Burrows TL, Martin RJ, Collins CE. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. Journal of the American Dietetic Association. 2010;110:1501–1510. doi: 10.1016/j.jada.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 21.Huang TT, Roberts SB, Howarth NC, McCrory MA. Effect of screening out implausible energy intake reports on relationships between diet and BMI. Obes Res. 2005;13:1205–1217. doi: 10.1038/oby.2005.143. [DOI] [PubMed] [Google Scholar]
- 22.Institute of Medicine. Food and Nutrition Board. Washington, DC: National Academy press; 2002. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein and Amino Acids. [DOI] [PubMed] [Google Scholar]
- 23.Garcia-Dominic O, Wray LA, Ledikwe JH, et al. Accuracy of self-reported energy intakes in low-income urban 4th grade minority children. Obesity (Silver Spring) 2010;18:2220–2226. doi: 10.1038/oby.2010.144. [DOI] [PubMed] [Google Scholar]
- 24.Dorsey KB, Herrin J, Krumholz HM. Patterns of moderate and vigorous physical activity in obese and overweight compared with non-overweight children. Int J Pediatr Obes. 2011;6:e547–555. doi: 10.3109/17477166.2010.490586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ventura AK, Loken E, Mitchell DC, Smiciklas-Wright H, Birch LL. Understanding reporting bias in the dietary recall data of 11-year-old girls. Obesity (Silver Spring) 2006;14:1073–1084. doi: 10.1038/oby.2006.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Black AE. Critical evaluation of energy intake using the Goldberg cut-off for energy intake:basal metabolic rate. A practical guide to its calculation, use and limitations. Int J Obes Relat Metab Disord. 2000;24:1119–1130. doi: 10.1038/sj.ijo.0801376. [DOI] [PubMed] [Google Scholar]
- 27.Kranz S, Mitchell DC, Smiciklas-Wright H, Huang SH, Kumanyika SK, Stettler N. Consumption of recommended food groups among children from medically underserved communities. J Am Diet Assoc. 2009;109:702–707. doi: 10.1016/j.jada.2008.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bailey RL, Mitchell DC, Miller C, Smiciklas-Wright H. Assessing the effect of underreporting energy intake on dietary patterns and weight status. J Am Diet Assoc. 2007;107:64–71. doi: 10.1016/j.jada.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 29.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 30.Nielsen SJ, Adair L. An alternative to dietary data exclusions. J Am Diet Assoc. 2007;107:792–799. doi: 10.1016/j.jada.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Goldfield GS, Epstein LH. Can fruits and vegetables and activities substitute for snack foods? Health Psychol. 2002;21:299–303. [PubMed] [Google Scholar]
- 32.Ogden J, Reynolds R, Smith A. Expanding the concept of parental control: a role for overt and covert control in children's snacking behaviour? Appetite. 2006;47:100–106. doi: 10.1016/j.appet.2006.03.330. [DOI] [PubMed] [Google Scholar]
- 33.Brown KA, Ogden J, Vogele C, Gibson EL. The role of parental control practices in explaining children's diet and BMI. Appetite. 2008;50:252–259. doi: 10.1016/j.appet.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 34.Webber L, Hill C, Cooke L, Carnell S, Wardle J. Associations between child weight and maternal feeding styles are mediated by maternal perceptions and concerns. European journal of clinical nutrition. 2010;64:259–265. doi: 10.1038/ejcn.2009.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Seagle HM, Strain GW, Makris A, Reeves RS. Position of the American Dietetic Association: weight management. J Am Diet Assoc. 2009;109:330–346. doi: 10.1016/j.jada.2008.11.041. [DOI] [PubMed] [Google Scholar]
- 36.Kirk S, Brehm B, Saelens BE, et al. Role of carbohydrate modification in weight management among obese children: a randomized clinical trial. J Pediatr. 2012;161:320–327 e321. doi: 10.1016/j.jpeds.2012.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]