Abstract
Study Design Case report and literature review.
Objective To describe a case of nontraumatic atlantoaxial rotatory subluxation (Grisel syndrome) and to review clinical and radiologic aspects, physiopathology, and treatment of this lesion. There is no well-established protocol in the management of patients without spontaneous reduction. The authors discuss the available strategies to achieve reduction and when to operate on these patients.
Methods Case presentation of a 7-year-old patient who presented with torticollis ∼1 week after the onset of an upper airway infection. There was no history of head or neck trauma. Computed tomography demonstrated atlantoaxial rotatory subluxation and a normal atlantodental interval.
Results The patient was treated with nonsteroidal anti-inflammatory drugs and antibiotics and by progressively increasing the soft cervical collar height. Clinical reduction of the subluxation occurred after 48 hours. He wore the rigid collar for 6 weeks. At that moment, the patient was completely asymptomatic and follow-up cervical spine radiograph demonstrated an anatomical C1–C2 relation. The patient was instructed to return to daily life activities in a gradual manner.
Conclusions Grisel syndrome should be considered in the differential diagnosis of torticollis, especially in children. The management can be planned according to the classification of Fielding and Hawkins. The initial treatment involves medicines, injury reduction, and cervical spine immobilization. Surgical treatment is indicated only in cases of failure of conservative treatment, recurrences of subluxation, and irreducible subluxations.
Keywords: Grisel syndrome, atlantoaxial rotatory subluxation
Introduction
Nontraumatic atlantoaxial rotatory subluxation was first described by Charles Bell in 1830, in a patient with syphilis and pharyngitis who developed compression of the spinal cord and died. It was defined by Grisel as a syndrome in 1951 after the report of two cases of nontraumatic atlantoaxial rotatory subluxation with a recent history of pharyngitis.1 2 Thus, Grisel syndrome refers to atlantoaxial rotatory subluxation not triggered by trauma, affecting patients with a history of head and/or neck infections or occurring after otorhinolaryngology procedures.3 4 It is a rare syndrome predominantly occurring in pediatric patients (∼68% of cases involve children younger than 12 years and ∼90% involve subjects younger than 21 years).3 5 6 7 The diagnosis is established by the association of clinical and radiologic findings.2 The authors report a case of atlantoaxial rotatory subluxation involving torticollis 2 days after the beginning of signs and symptoms of pharyngotonsillitis.
Case Report
A 7-year-old boy was admitted to the sector of pediatric emergency with torticollis in the preceding 24 hours. There was no history of head or neck trauma. The patient presented cough, halitosis, and odynophagia lasting about 1 week, without fever. Physical examination revealed posture in complete cervical rotation to the right accompanied by subtle flexion. There was spasm of the ipsilateral sternocleidomastoid muscle associated with nuchal pain that was exacerbated by the attempt to perform contralateral active rotation (Fig. 1). Oroscopy revealed tonsil hypertrophy (2+/4+) with hyperemia and with no exudation or abscess. The neurologic examination was normal. Laboratory exams showed absence of leukocytosis (9,800/mm3) and normal C-reactive protein (<6.0 mg/L).
Fig. 1.

Photograph of the patient taken at admission, demonstrating anomalous rotation of the head to the right.
Computed tomography (CT) of the cervical spine demonstrated atlantoaxial rotatory subluxation to the right, with anterior dislocation of the left articular facet of the atlas and a normal atlantodental interval (ADI) of 2 mm (Fig. 2). Head and neck contrast tomographies did not detect abscesses. Treatment consisted of immobilization with a soft cervical collar (molded for neck size and position), analgesia (dipyrone and ibuprofen), a muscle relaxant (cyclobenzaprine), and empirical antibiotic treatment (Ceftriaxone for 14 days). Partial relaxation of the cervical musculature occurred after 24 hours, and the collar was replaced with a larger one to reduce the posture in flexion. Clinical reduction of the subluxation occurred after 48 hours, with centralization of the head (Fig. 3). The patient then received a rigid cervical collar (Philadelphia). He showed significant improvement of cervical pain and of difficulty in eating. No complaints or signs of neurologic involvement were observed at any time. The reduction of atlantoaxial rotatory subluxation was confirmed by imaging exams. Magnetic resonance of the cervical spine was performed 20 days after reduction and demonstrated that the odontoid process was slightly shifted to the right (Fig. 4), with the presence of fluid on the C1–C2 articular facets. The ADI was normal, with no signs of injury to the transverse ligament of the atlas. The patient was discharged from the hospital after 3 weeks. He wore the rigid collar for 6 weeks. Isometric exercises were indicated during this period to maintain the strength of the cervical musculature. Six weeks after reduction, the patient was completely asymptomatic and the radiograph demonstrated an anatomical C1–C2 relation (Fig. 5). The patient was instructed to return to daily life activities, including sports, in a gradual manner.
Fig. 2.
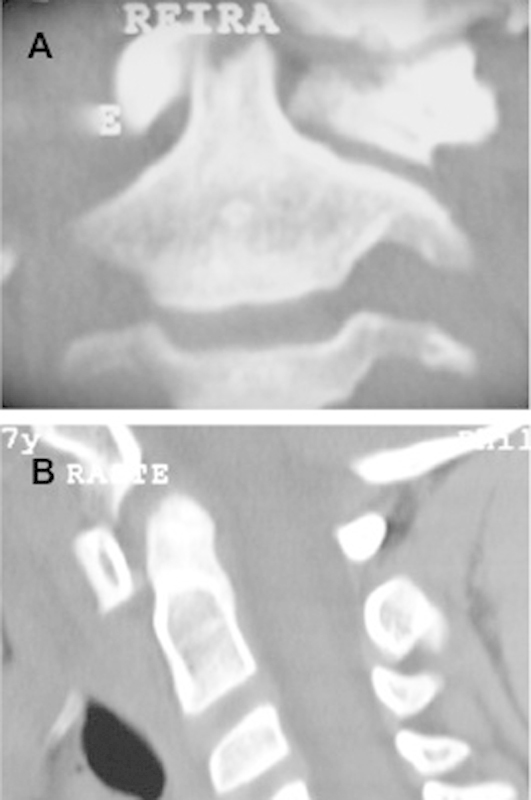
Computed tomography of the cervical spine. The coronal image demonstrates asymmetry of the lateral masses of the atlas, with apparent “increase of the left lateral mass” dislocated anteriorly (A). The sagittal image demonstrates normal distance of the atlantodental interval (B).
Fig. 3.

Three-dimensional reconstruction reveals rotatory subluxation between C1 and C2. Note the articular facet of C1 anteriorly dislocated to the left and blocked.
Fig. 4.

Photograph of the patient on day 3 of conservative treatment demonstrating the head in a neutral position, indicating clinical reduction of atlantoaxial rotatory subluxation. The restoration of neutral position left the cervical collar loose.
Fig. 5.
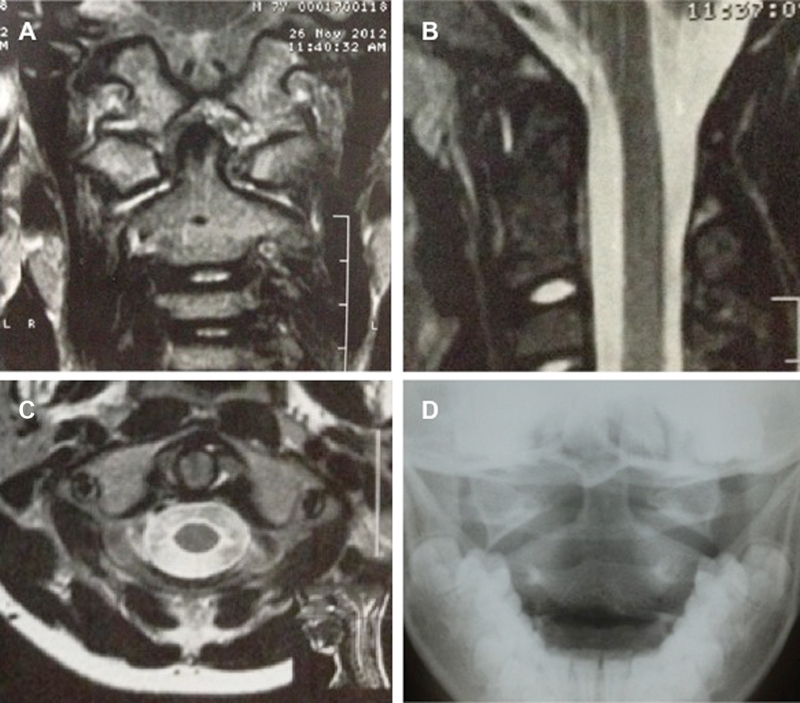
Magnetic resonance of the cervical spine, T2 sequence, after spontaneous reduction of the lesion. Observe the joint effusion on the anterior and posterior facets of the dens on the axial image. Intact transverse ligament of the axis (A). Joint effusion anterior to the dens on the sagittal image (B). Note the joint effusion in the atlantoaxial joint in the coronal image (C). Anteroposterior radiograph taken after 6 months demonstrates a reduced atlantoaxial joint (D).
Discussion
Grisel syndrome is a rare entity characterized by nontraumatic atlantoaxial rotatory subluxation, which usually occurs after infections of head and neck or after otolaryngology procedures such as adenoidectomy, tonsillectomy, and repair of choanal atresia, among others.8 This disease is more common during childhood, and only rare cases involving adults have been reported.9 This is the consequence of the relative weakness of ligaments and joint capsules, horizontal joint articulation, and small supporting muscles.5 Congenital conditions that involve ligamentous laxity such as Down and Marfan syndromes present a higher risk of atlantoaxial subluxation.10 11 Kawasaki disease is a very frequent acute febrile vasculitis of childhood that has also been related to Grisel syndrome.12 After the introduction of monopolar suction electrocautery in adenoidectomy, an increased incidence of Grisel syndrome has been observed when compared with bipolar coagulation for bleeding control.13
Karkos et al conducted a systematic review of 71 articles, which included 96 patients with C1–C2 subluxation with no history of previous trauma.14 Of these, 48% had a recent history of infection mostly affecting the upper airways and 40% were in the postoperative period after head and neck procedures. The clinical picture consists of torticollis and cervical pain, mainly in the nape, associated with oropharyngeal pain, suggesting infection of the upper airways, and/or a recent history of head or neck surgical procedures. Upon physical examination, three signs define the clinical diagnosis of atlantoaxial rotatory subluxation: palpable deviation of the spinous process of the axis in the same direction of head rotation, spasm of the sternocleidomastoid muscle ipsilateral to the rotation,5 and inability to turn the head beyond the midline in the direction of the side opposite to the lesion.15 Nuchal pain increases when an attempt is made to perform active contralateral neck rotation. Thus, the patient keeps his or her head motionless, in subtle rotation and flexion, with the chin in a position opposite to that of the affected side, characterizing the pathologic posture denoted “cock robin posture,” a term coined in reference to the posture of a robin with its head in rotation (Fig. 6).4 The reported case showed complete contralateral cervical rotation not typical of cock robin posture. However, the absence of spasm of the sternocleidomastoid muscle contralateral to the rotation might alert that this posture may not correspond to a torticollis elicited by muscle spasm.
Fig. 6.

A 9-year-old boy with Grisel syndrome. Typical cock robin posture. (Reproduced and used with permission from Deichmueller CM, Welkoborsky HJ. Grisel's syndrome—a rare complication following “small” operations and infections in the ENT region. Eur Arch Otorhinolaryngol 2010;267(9):1467–1473.)
The physiopathological mechanism of the condition is unknown. Grisel emphasized the role of muscle spasm.1 Tedesco et al proposed that cervical lymphadenitis subsequent to a nasopharyngeal infection induced irritative spastic contraction of suboccipital and paravertebral muscles causing torticollis.16 However, the most accepted theory was described by Parke et al, who studied the vascularization of the cervical spine, cranial base, and peripharyngeal tissues in human perinatal cadavers.17 The authors demonstrated that veins of the posterosuperior region of the pharynx communicate with the periodontoid venous plexus and the epidural suboccipital venous sinuses through the pharyngovertebral veins, providing a hematogenic transport route for septic exudates to structures of the upper cervical spine, a fact that would explain the atlantoaxial inflammatory reactions of Grisel syndrome in anatomical terms. Then, transverse and alar ligament laxity and edema of the atlantoaxial articular capsules would cause rotational atlantoaxial hypermobility and further subluxation after a rotational movement.
C1–C2 subluxation can be seen in simple standard radiographs of the cervical spine.18 The radiographic findings in transoral incidence include asymmetry and deletion of the C1–C2 articular surfaces, increase of a lateral C1 mass (the one anteriorly dislocated), and reduction of the contralateral one (the one posteriorly dislocated ipsilateral to cervical rotation). However, posture of the head in rotation causes technical difficulties for obtaining a radiograph of quality. On this basis, the gold standard exam for the diagnosis of atlantoaxial rotatory subluxation is the three-dimensional CT of the craniocervical transition. The pediatrician may erroneously consider a diagnosis of atlantoaxial rotatory subluxation when evaluating a CT scan after head trauma performed with the child with the head turned. If there is no neck pain or rigidity, the CT scan must be performed with the head in neutral position to avoid misdiagnosis and unnecessary referral to tertiary centers. The three-dimensional reconstruction of CT permits a clear visualization of C1–C2 rotation, including the loss of congruence of the articular facets. The axial images permit the measurement of ADI. The normal measurement is 2 to 3 mm in adults and up to 5 mm in children.19 An increase in this distance is an indirect result of injury to the transverse ligament, which is related to greater instability of the lesion, with the possible need for surgical treatment.
The fundamental diagnostic findings are the nontraumatic atlantoaxial rotatory subluxation itself and a recent history of upper airway infections and/or head and neck surgeries (Table 1). The diagnosis of the syndrome should be prompt. Diagnosis after 3 weeks is related to failure of conservative treatment, including closed reduction, greater risks of recurrence and permanent craniofacial and/or cervical deformities, and the need for surgical treatment.15 20 21 22 These might occur because of chronic changes in the transverse and alar ligaments.5 The recurrence rate is not well established. It is necessary to rule out differential diagnoses with torticollis due to muscle spasms, tumors of the posterior fossa, Chiari malformation, syringomyelia, and C1–C2 fractures.5
Table 1. Diagnostic findings of Grisel syndrome.
| History of upper airway infections and/or head and neck surgeries |
| Complaint of torticollis a few days after onset of infection/surgery |
| Anomalous rotation and mild flexion of the head, with the chin turned toward the contralateral side |
| Pain with active or passive head rotation |
| Elevation of C reactive protein and of leukocytes during the first days of torticollis, with later normalization of these parameters, usually without a fever |
| Anteroposterior radiograph may show enlargement of the C1 lateral mass that is dislocated forward (contralateral to neck rotation) |
| Lateral radiograph of the cervical spine may show an atlantodental interval larger than 5 mm in severe cases |
| Computed tomography showing rotatory subluxation of C1–C2 |
Source: Adapted from Deichmueller CM, Welkoborsky HJ. Grisel's syndrome—a rare complication following “small” operations and infections in the ENT region. Eur Arch Otorhinolaryngol 2010;267(9):1467–1473.
Fielding and Hawkins classified traumatic atlantoaxial rotatory subluxation into four types depending on the distance between the atlas and the odontoid process of the axis.23 In type I, there is pure rotation of the atlas in relation to the axis and ADI is normal. In type II, there is both rotation and anterior dislocation of the atlas with ADI of 3 to 5 mm, suggesting mild dysfunction of the transverse ligament. Type III consists of rotation and anterior dislocation of more than 5 mm, indicating complete dysfunction of the transverse ligament. Type IV is characterized by rotation and posterior dislocation of the atlas (Fig. 7). Type I and II subluxations are the most frequent and do not involve neurologic deficits, whereas types III and IV may be associated with spinal cord compression and neurological injury.
Fig. 7.
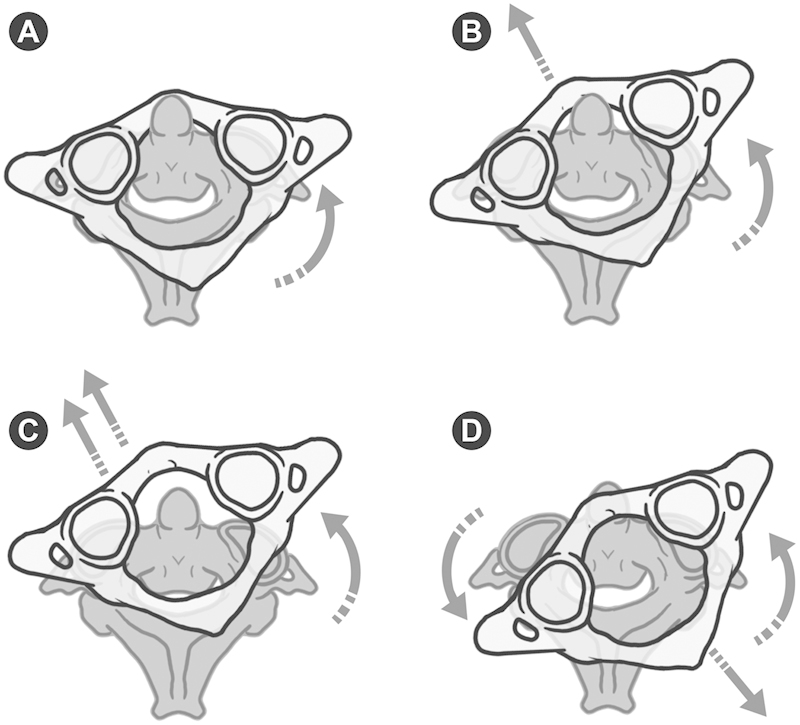
Schematic illustration of Fielding and Hawkins' classification of traumatic atlantoaxial rotatory subluxation. Type I: pure rotation of the atlas in relation to the axis without anterior displacement (A). Type II: atlas rotated with 3- to 5-mm anterior displacement (B). Type III: rotation of the atlas with anterior displacement greater than 5 mm (C). Type IV: rotatory fixation with posterior displacement of atlas (D).
The treatment of Grisel syndrome is controversial. The initial treatment is usually conservative, including bed rest, a cervical collar, analgesics, anti-inflammatory medications, muscle relaxants and, when pertinent, antibiotic therapy and abscess drainage.5 At first, the cervical posture usually prevents the use of a rigid cervical collar. Therefore, we recommend the use of a soft cervical collar molded to the height of the neck at that time. As greater relaxation of the cervical muscles occurs, the authors recommend increasing the height of the collar until reduction of the lesion occurs. Then, the soft collar is replaced with a rigid one. The waiting period for the occurrence of spontaneous reduction has not been established. However, most cases usually resolve spontaneously up to 7 days after the beginning of treatment.20 Once the injury is reduced and the inflammatory process is completely solved, stability is recovered. Although there is no consensus, the authors recommend the use of a rigid collar for at least 2 weeks to treat neck pain and to prevent early recurrence and the return to normal recreation and sports activities after 4 to 6 weeks. The reported case showed a slight deviation of the odontoid process to the right and presence of fluid on the C1–C2 articular facets in the magnetic resonance 3 weeks after reduction, and the authors chose to keep the cervical collar for 3 more weeks.
If spontaneous reduction of the lesion does not occur, closed reduction under mild sedation is recommended, with analgesia in the surgical block. The options are: manual traction in mild flexion followed by cervical extension and contralateral rotation, Jeszenszky transoral technique consisting of locking the spinous process of the axis with one hand while pressing with the index finger of the other hand the lateral mass dislocated anteriorly through the posterior wall of the oropharynx, or halo-cranial traction.15 21 24 Definitive treatment should be instituted after reduction. Wetzel and La Rocca proposed a treatment protocol for nontraumatic atlantoaxial rotatory subluxation (Grisel syndrome) based on the classification of Fielding and Hawkins. Conservative treatment for type I, II, and III lesions with a soft collar, a rigid collar (Philadelphia collar), and a halo-vest, respectively. For type IV lesions, they recommend surgical treatment.25 Surgical treatment is indicated also in cases of failure of conservative treatment, recurrence of subluxation, and irreducible subluxations. Craniocervical fusions in children present unique challenges even in the absence of craniovertebral malformations. The diminutive osseous and ligamentous structures, especially in children younger than 5 to 6 years, limit the use of internal fixation. In these cases, Menezes recommends a small craniectomy and upper cervical laminectomy with a bilateral interlaminar and occipital rib graft anchored with titanium cables (Fig. 8). After this age, the size and anatomy of craniovertebral structures may allow the use of screw fixations such as C1–C2 transarticular screw fixation, lateral mass screws at C1, and rod fixation with either C2 pars interarticular screw fixation, pedicle screw fixation, or C2 translaminar screw fixation.26
Fig. 8.
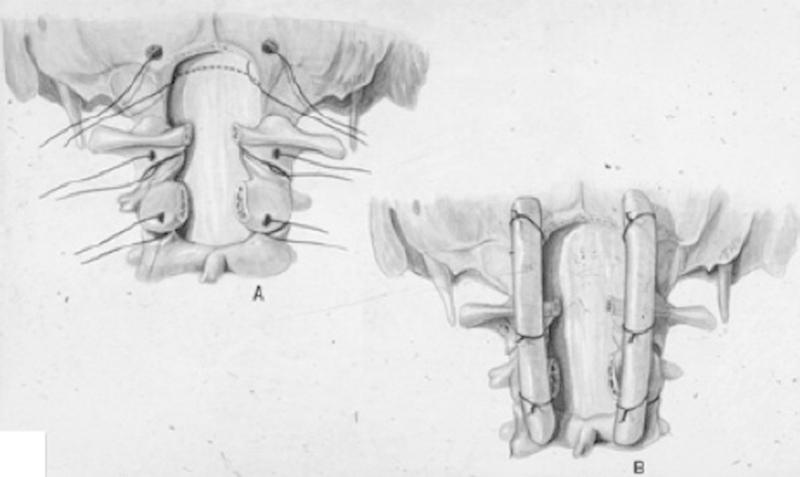
Schematic illustration of craniocervical fusion recommended by Menezes in children younger than 5 to 6 years. (Reproduced and used with permission from Menezes AH. Craniocervical fusions in children. J Neurosurg Pediatr 2012;9(6):573–585.)
Conclusion
Grisel syndrome is a rare complication of upper airway infections and otorhinolaryngology procedures, more commonly occurring in children. The present case underscores the importance of an early diagnosis and treatment of Grisel syndrome. Conservative treatment is indicated in most cases. Surgical treatment is indicated only in cases of failure of conservative treatment, recurrences of subluxation, and irreducible subluxations.
Acknowledgment
The author is grateful to Fernando Mosca for his skillful illustrations.
Footnotes
Disclosures None
References
- 1.Grisel P Enucleation de l'atlas et torticollis nasopharyngien Presse Med 1951591647–1648.14900152 [Google Scholar]
- 2.Guleryuz A, Bagdatoglu C, Duce M N, Talas D U, Celikbas H, Köksel T. Grisel's syndrome. J Clin Neurosci. 2002;9(1):81–84. doi: 10.1054/jocn.2001.0944. [DOI] [PubMed] [Google Scholar]
- 3.Bocciolini C, Dall'Olio D, Cunsolo E, Cavazzuti P P, Laudadio P. Grisel's syndrome: a rare complication following adenoidectomy. Acta Otorhinolaryngol Ital. 2005;25(4):245–249. [PMC free article] [PubMed] [Google Scholar]
- 4.Rinaldo A, Mondin V, Suárez C, Genden E M, Ferlito A. Grisel's syndrome in head and neck practice. Oral Oncol. 2005;41(10):966–970. doi: 10.1016/j.oraloncology.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 5.Fernández Cornejo V J, Martínez-Lage J F, Piqueras C, Gelabert A, Poza M. Inflammatory atlanto-axial subluxation (Grisel's syndrome) in children: clinical diagnosis and management. Childs Nerv Syst. 2003;19(5–6):342–347. doi: 10.1007/s00381-003-0749-6. [DOI] [PubMed] [Google Scholar]
- 6.Gourin C G, Kaper B, Abdu W A, Donegan J O. Nontraumatic atlanto-axial subluxation after retropharyngeal cellulitis: Grisel's syndrome. Am J Otolaryngol. 2002;23(1):60–65. doi: 10.1053/ajot.2002.28781. [DOI] [PubMed] [Google Scholar]
- 7.Grobman L R, Stricker S. Grisel's syndrome. Ear Nose Throat J. 1990;69(12):799–801. [PubMed] [Google Scholar]
- 8.Samuel D TD, Thomas D M, Tierney P A, Patel K S. Atlanto-axial subluxation (Grisel's syndrome) following otolaryngological diseases and procedures. J Laryngol Otol. 1995;109(10):1005–1009. doi: 10.1017/s0022215100131883. [DOI] [PubMed] [Google Scholar]
- 9.Youssef K, Daniel S. Grisel syndrome in adult patients. Report of two cases and review of the literature. Can J Neurol Sci. 2009;36(1):109–113. doi: 10.1017/s0317167100006430. [DOI] [PubMed] [Google Scholar]
- 10.Yamazaki M, Someya Y, Aramomi M, Masaki Y, Okawa A, Koda M. Infection-related atlantoaxial subluxation (Grisel syndrome) in an adult with Down syndrome. Spine (Phila Pa 1976) 2008;33(5):E156–E160. doi: 10.1097/BRS.0b013e3181657eca. [DOI] [PubMed] [Google Scholar]
- 11.Herzka A, Sponseller P D, Pyeritz R E. Atlantoaxial rotatory subluxation in patients with Marfan syndrome. A report of three cases. Spine (Phila Pa 1976) 2000;25(4):524–526. doi: 10.1097/00007632-200002150-00022. [DOI] [PubMed] [Google Scholar]
- 12.Nozaki F, Kusunoki T, Tomoda Y. et al. Grisel syndrome as a complication of Kawasaki disease: a case report and review of the literature. Eur J Pediatr. 2013;172(1):119–121. doi: 10.1007/s00431-012-1858-6. [DOI] [PubMed] [Google Scholar]
- 13.Tschopp K. Monopolar electrocautery in adenoidectomy as a possible risk factor for Grisel's syndrome. Laryngoscope. 2002;112(8 Pt 1):1445–1449. doi: 10.1097/00005537-200208000-00022. [DOI] [PubMed] [Google Scholar]
- 14.Karkos P D, Benton J, Leong S C, Mushi E, Sivaji N, Assimakopoulos D A. Grisel's syndrome in otolaryngology: a systematic review. Int J Pediatr Otorhinolaryngol. 2007;71(12):1823–1827. doi: 10.1016/j.ijporl.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Subach B R, McLaughlin M R, Albright A L, Pollack I F. Current management of pediatric atlantoaxial rotatory subluxation. Spine (Phila Pa 1976) 1998;23(20):2174–2179. doi: 10.1097/00007632-199810150-00006. [DOI] [PubMed] [Google Scholar]
- 16.Tedesco B, Grisel P, Desfosses P, Tassin M. Deux nouveaux cas d'énucléation de l'atlas par torticolis nasopharyngien. Bull Soc Pediat. 1930;28:252–262. [Google Scholar]
- 17.Parke W W, Rothman R H, Brown M D. The pharyngovertebral veins: an anatomical rationale for Grisel's syndrome. J Bone Joint Surg Am. 1984;66(4):568–574. [PubMed] [Google Scholar]
- 18.Deichmueller C M, Welkoborsky H J. Grisel's syndrome—a rare complication following “small” operations and infections in the ENT region. Eur Arch Otorhinolaryngol. 2010;267(9):1467–1473. doi: 10.1007/s00405-010-1241-z. [DOI] [PubMed] [Google Scholar]
- 19.Diethelm L, Heuck F, Olsson O, Berlin, Germany: Springer Verlag; 1976. Handbuch der medizinischen Radiologie [Encyclopedia of Medical Radiology] p. 195. [Google Scholar]
- 20.Phillips W A, Hensinger R N. The management of rotatory atlanto-axial subluxation in children. J Bone Joint Surg Am. 1989;71(5):664–668. [PubMed] [Google Scholar]
- 21.Martinez-Lage J F, Martinez Perez M, Fernandez Cornejo V, Poza M. Atlanto-axial rotatory subluxation in children: early management. Acta Neurochir (Wien) 2001;143(12):1223–1228. doi: 10.1007/s007010100018. [DOI] [PubMed] [Google Scholar]
- 22.Yu K K, White D R, Weissler M C, Pillsbury H C. Nontraumatic atlantoaxial subluxation (Grisel syndrome): a rare complication of otolaryngological procedures. Laryngoscope. 2003;113(6):1047–1049. doi: 10.1097/00005537-200306000-00024. [DOI] [PubMed] [Google Scholar]
- 23.Fielding J W, Hawkins R J. Atlanto-axial rotatory fixation (fixed rotatory subluxation of the atlanto-axial joint) J Bone Joint Surg Am. 1977;59(1):37–44. [PubMed] [Google Scholar]
- 24.Park S W, Cho K H, Shin Y S. et al. Successful reduction for a pediatric chronic atlantoaxial rotatory fixation (Grisel syndrome) with long-term halter traction: case report. Spine (Phila Pa 1976) 2005;30(15):E444–E449. doi: 10.1097/01.brs.0000172226.35474.fe. [DOI] [PubMed] [Google Scholar]
- 25.Wetzel F T, La Rocca H. Grisel's syndrome. Clin Orthop Relat Res. 1989;(240):141–152. [PubMed] [Google Scholar]
- 26.Menezes A H. Craniocervical fusions in children. J Neurosurg Pediatr. 2012;9(6):573–585. doi: 10.3171/2012.2.PEDS11371. [DOI] [PubMed] [Google Scholar]


