Abstract
Study Design Retrospective population-based observational study.
Objective To assess the growth of cervical spine surgery performed in an outpatient setting.
Methods A retrospective study was conducted using the United States Healthcare Cost and Utilization Project's State Inpatient and Ambulatory Surgery Databases for California, New York, Florida, and Maryland from 2005 to 2009. Current Procedural Terminology, fourth revision (CPT-4) and International Classification of Diseases, ninth revision Clinical Modification (ICD-9-CM) codes were used to identify operations for degenerative cervical spine diseases in adults (age > 20 years). Disposition and complication rates were examined.
Results There was an increase in cervical spine surgeries performed in an ambulatory setting during the study period. Anterior cervical diskectomy and fusion accounted for 68% of outpatient procedures; posterior decompression made up 21%. Younger patients predominantly underwent anterior fusion procedures, and patients in the eighth and ninth decades of life had more posterior decompressions. Charlson comorbidity index and complication rates were substantially lower for ambulatory cases when compared with inpatients. The majority (>99%) of patients were discharged home following ambulatory surgery.
Conclusions Recently, the number of cervical spine surgeries has increased in general, and more of these procedures are being performed in an ambulatory setting. The majority (>99%) of patients are discharged home but the nature of analyzing administrative data limits accurate assessment of postoperative complications and thus patient safety. This increase in outpatient cervical spine surgery necessitates further discussion of its safety.
Keywords: cervical spine surgery, ambulatory surgery, complications, safety
Introduction
The performance of ambulatory surgical procedures is on the rise across all surgical fields, from cholecystectomy1 to orthopedic procedures ranging from outpatient knee arthroscopy2 to lumbar spine surgery.3
The number of surgeries performed for degenerative cervical spine disease is also increasing in the United States. Notably, Medicare data demonstrate that cervical fusions alone rose 206% from 1992 to 2005.4 5 More recently, cervical spine surgery performed on an ambulatory basis has received attention in the literature.4 6 7 8 9 10
One study examining the United States Nationwide Inpatient Sample from 1993 to 2002 analyzed 58,049 patients undergoing cervical spinal fusion for cervical spondylotic myelopathy.5 The data showed that although the number of cervical spinal fusions had increased sevenfold and the percentage of patients with two or more major medical comorbidities had increased from 20 to 37% during the study period, the rate of complications remained stable at 10.3% and mortality remained steady at 0.6%. In addition, a prospective cohort study of 390 patients undergoing anterior cervical diskectomy and fusion (ACDF) found that all potentially life-threatening complications were discovered in the early postoperative period (<6 hours) and concluded that patients could be safely discharged home after an initial 6-hour observation period.7 In contrast to these findings, others have found that airway swelling and the potential for respiratory compromise peaked at the second and third postoperative days.11 12
The purpose of this study was to examine large administrative data from four U.S. states to assess the increase in performance of cervical spine surgery on an outpatient basis. Recent trends in types of cervical procedures, patient demographics, postoperative disposition, and reported complications were investigated.
Patients and Methods
Data Source
We conducted a retrospective cohort study using the United States Healthcare Cost and Utilization Project's State Ambulatory Surgery Databases for California, New York, Florida, and Maryland from 2005 to 2009.13 Data from government, psychiatric, chemical dependency, or long-term hospitals were excluded. It should be noted that this database does not distinguish between truly ambulatory care and 23-hour monitoring, meaning that relying upon this disposition classification could substantially overestimate the number of ambulatory procedures.
Inclusions
We included patients 20 years of age or older who underwent surgery for degenerative conditions of the cervical spine. Current Procedural Terminology, fourth revision (CPT-4) and International Classification of Diseases, ninth revision Clinical Modification (ICD-9-CM) procedure/diagnosis codes were used as previously described.4 Given our inclusion criteria, the database yielded data on 21,533 ambulatory and 170,974 inpatient surgeries. The diagnosis codes were grouped into subcategories, such as herniated disk (722.0), cervical spondylosis with myelopathy (721.1, 722.71), cervical spondylosis without myelopathy (721.0, 722.4, 723.7), and spinal stenosis (723.0). Cervical procedure codes were anterior fusion (ICD-9; CPT-4) (81.02; 22554), posterior fusion (81.03; 22600), cervical disk arthroplasty (84.62; 22856), diskectomy without fusion (80.51; 63075), decompression (03.09; 63040, 63045, 63001, 63015), and laminoplasty (03.09; 63050, 63051).
We also examined reported complications by identifying ICD-9 codes within the cohort for the following complications found in the postoperative period: cardiac (997.1), respiratory (997.3), peripheral vascular (997.2), central nervous system (997.0), hematoma (998.1), carotid or vertebral artery injury (997.7), and other complications not otherwise specified (998.9). Furthermore, we included dysphagia (787.2), dysphonia (784.4), and wound infection (998.5).14 The Healthcare Cost and Utilization Project has been employed in this manner for assessing outcomes and complications in several previous studies.15 16
Exclusions
We excluded patients younger than 20 years and those who were pregnant or presented with cancer, trauma, infection, or inflammatory disease.
Analysis
Continuous variables were analyzed using t test and categorical variables with the chi-square test. The Cochrane-Armitage test was used to examine trends, and p values less than 0.05 were considered statistically significant. The comorbidity index was calculated with the Charlson algorithm as modified by Deyo et al.17 18 All statistical analyses were performed using SAS 9.2 (SAS Institute, Inc., Cary, North Carolina, United States).
Results
Among the four states studied, there has been a steady rise in cervical spine surgeries in both inpatient (56.1 in 2005 to 60.9 per 100,000 capita in 2009) and outpatient (5.6 in 2005 to 9.0 per 100,000 capita in 2009) settings (Table 1). Utilization of cervical spine surgery per 100,000 capita by state was as follows (ambulatory and inpatient, respectively): California 1.2 and 37.5; Florida 15.1 and 86.7; Maryland 12.7 and 88.4; New York 9.8 and 61.0 (Fig. 1). Notably, all the states except California demonstrated an increase in the utilization of cervical spine surgery per 100,000 capita over the study period (Fig. 2).
Table 1. Trend in ambulatory and inpatient cervical spine surgeries per 100,000 capita of 4 states combined (California, Florida, Maryland, New York).
| 2005 | 2006 | 2007 | 2008 | 2009 | p Values | |
|---|---|---|---|---|---|---|
| Ambulatory | 5.6 | 6.5 | 7.4 | 8.2 | 9.0 | <0.001 |
| Inpatient | 56.1 | 57.1 | 58.3 | 59.7 | 60.9 | <0.001 |
| % Ambulatory surgeries | 9.1 | 10.2 | 11.3 | 12.1 | 12.9 | <0.001 |
Fig. 1.
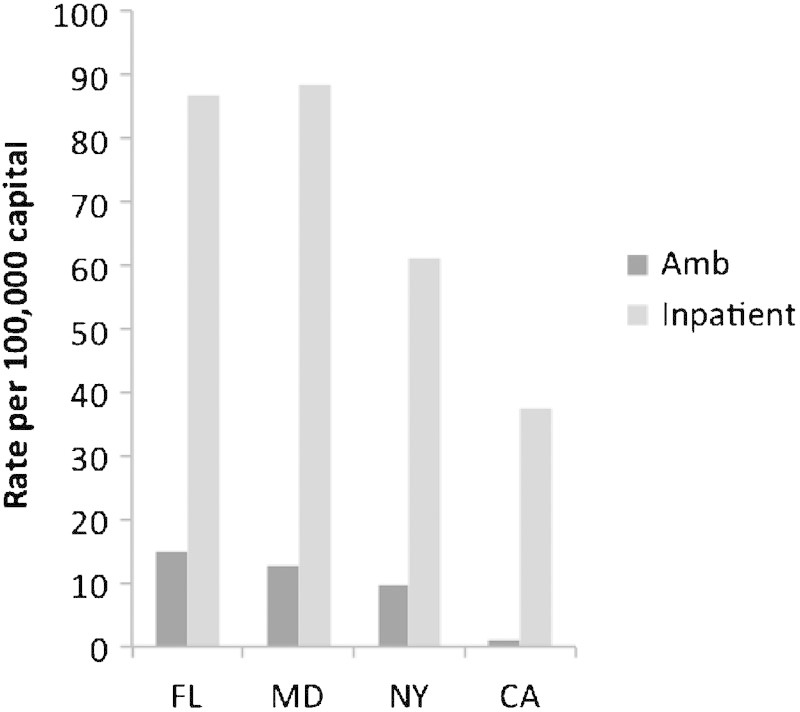
Geographic variation in usage of ambulatory and inpatient cervical spine surgeries for degenerative diseases. Abbreviations: Amb, ambulatory; CA, California; FL, Florida; MD, Maryland; NY, New York.
Fig. 2.

Trend in utilization of cervical spine surgery from 2005 to 2009 by state. Abbreviations: Amb, ambulatory; CA, California; FL, Florida; Inp, inpatient; MD, Maryland; NY, New York.
Ambulatory surgery comprised 9% (5.6 per 100,000 capita) of all cervical procedures in 2005 and 13% (9.0 per 100,000 capita) in 2009, constituting a 60.5% increase; there was an 8.7% increase in inpatient surgeries over the same period (p < 0.001, Table 1). During the study period, outpatient ACDF accounted for 68% of procedures, and posterior decompression comprised 21% (Fig. 3). In 2005, there were no codes for artificial disk replacement. By 2009, this increased to 279 cases (Fig. 3). More procedures were performed in the fifth and sixth decades of life than any other time and accounted for 32 and 30% of procedures, respectively (Fig. 4), and gender distribution was similar with female patients comprising 48.8 to 52.6%, depending on the year. Younger patients (third, fourth, and fifth decades) were more likely to have anterior fusions than older patients (eighth and ninth decades), and older patients were more likely to have posterior decompression than younger patients (p < 0.05; Fig. 5). Notably, ambulatory procedures performed in octogenarians accounted for 0.4% of all ambulatory procedures, and the same age group comprised 3.1% of all inpatient cervical procedures. Patients in the ambulatory setting had fewer comorbidities than those who had similar procedures in inpatient settings (Charlson comorbidity index 0.15 versus 0.53, p < 0.001).
Fig. 3.
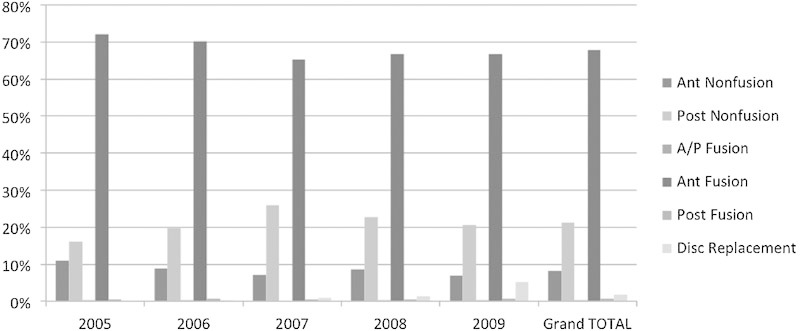
Ambulatory surgeries by procedure type, four states combined. Abbreviations: Ant, anterior; A/P, anterior/posterior; Post, posterior.
Fig. 4.
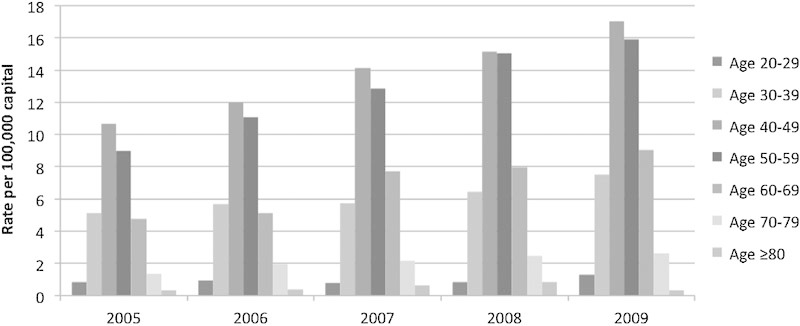
Trends in utilization of cervical spine surgery overall by age group, 2005 to 2009.
Fig. 5.
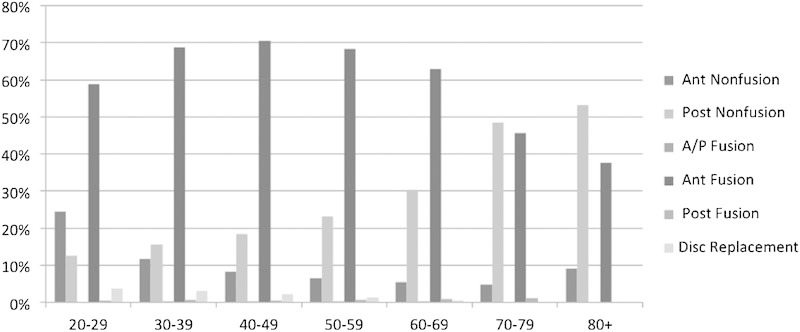
Utilization of cervical spine surgery by age and procedure type. Abbreviations: Ant, anterior; A/P, anterior/posterior; Post, posterior.
The data demonstrated that 99% of patients were discharged home following surgery, with the remaining 1% split among short-term hospitalization (0.1%), transfer to another health care facility (0.2%), home with health care assistance (0.3%), and unknown (0.3%; Table 2).
Table 2. Trend in patient disposition following ambulatory procedures.
| 2005 | 2006 | 2007 | 2008 | 2009 | Overall | |
|---|---|---|---|---|---|---|
| Number of procedures | 3,199 | 3,722 | 4,324 | 4,869 | 5,419 | 21,533 |
| Home for self-care (%) | 98.0 | 98.6 | 99.6 | 99.4 | 99.0 | 99.0 |
| Short-term hospitalization (%) | 0.1 | 0.3 | 0.0 | 0.0 | 0.1 | 0.1 |
| Transfer to another institution (%) | 0.1 | 0.1 | 0.0 | 0.2 | 0.4 | 0.2 |
| Home health care (%) | 0.3 | 0.2 | 0.2 | 0.3 | 0.5 | 0.3 |
| AMA (%) | 0.0 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 |
| Death (%) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Unknown (%) | 1.5 | 0.7 | 0.1 | 0.0 | 0.0 | 0.3 |
Abbreviation: AMA, left against medical advice.
Complication data for the cohort are listed in Table 3. It was not possible to determine the time course for the development of complications. The reported complication rate for the cohort was 0.67%, including other complications not otherwise specified (998.9); the complication rate for the inpatient cohort was 9.58% (p < 0.001).
Table 3. Complications of outpatient and inpatient cervical surgery.
| Ambulatory (n = 21,533) | Inpatient (n = 170,974) | p Value | |||
|---|---|---|---|---|---|
| Complication | % | n | % | n | |
| Cardiac | 0.05 | 11 | 0.75 | 1,290 | <0.001 |
| Respiratory | ≤0.05a | ≤10a | 0.93 | 1,584 | <0.001 |
| Peripheral vascular | 0.00 | 0 | 0.05 | 86 | <0.001 |
| Central nervous system | ≤0.05a | ≤10a | 0.46 | 792 | <0.001 |
| Hematoma | 0.06 | 12 | 0.84 | 1,432 | <0.001 |
| Durotomy | ≤0.05a | ≤10a | 0.54 | 924 | <0.001 |
| CSF leak/fistula | ≤0.05a | ≤10a | 0.18 | 309 | <0.001 |
| Other wound complication | 0.00 | 0 | 0.10 | 163 | <0.001 |
| Other complications | 0.19 | 41 | 1.43 | 2,443 | <0.001 |
| Carotid/vertebral injury | 0.00 | 0 | 0.09 | 153 | <0.001 |
| Postoperative infection | 0.00 | 0 | 0.36 | 607 | <0.001 |
| Dysphonia | 0.05a | 10a | 0.48 | 823 | <0.001 |
| Dysphagia | 0.22 | 48 | 3.37 | 5,770 | <0.001 |
Abbreviation: CSF, cerebrospinal fluid.
Per state database guidelines, observations are not reported if the number of observations (i.e., individual discharge records) in the cell is less than or equal to 10.
Discussion
The number of spine procedures performed each year continues to increase,3 4 5 not only due to an increase in population but also on a per-capita basis, as demonstrated in our data. Largely due to the development of more minimally invasive surgical techniques in all fields of surgery as well as the productivity and financial incentives afforded by ambulatory surgery centers, the practice of performing procedures on an outpatient basis has gained significant attention recently.1 8
Similar to previous reports,4 19 we also found an overall increase in cervical spine surgery in recent years. Although most published studies have been on a small scale,6 8 9 10 20 we examined data from four states,13 which we believe to be more representative of general trends.3 The overwhelming majority of cervical spine procedures were performed on an inpatient basis (Fig. 1). However, the proportion of outpatient cervical spine surgery, ranging from 3% (California) to nearly 15% (Florida), was significant. Furthermore, the overall trend was that of an increase toward more procedures per 100,000 capita, with utilization of ambulatory care increasing by a larger percentage than inpatient care (Table 1).
The state of California was the exception, where ambulatory surgery per capita remained relatively constant throughout the 2005 to 2009 study period. The difference in surgical rates in California in comparison to the other states we examined has been alluded to previously in the spine literature in reference to regional differences.4 21 22 23
The trends outlined in Figs. 3 to 5 with respect to age and surgical approach were consistent with the results by Wang et al.4 Even patients who were in their 70s and beyond (although comprising only 2.5% of the total number of cases) underwent surgery in an ambulatory setting. Advanced age has been associated with increased postoperative complications following spine surgery.14 Because elderly patients may require more postoperative care than middle-aged patients, the safety of performing such procedures in an ambulatory setting needs more clinical investigation.
There are several limitations to this study. The most significant of these is undoubtedly the inability to obtain data from all 50 states. This was a result of both the availability of data as well as the cost of obtaining such data. More specifically, during the specified study period, only 15 states made available their respective ambulatory surgery data.13 Moreover, each year of each state's ambulatory surgery database is available separately, which is cost-prohibitive. We therefore had to be selective as to which states and which data to use. We chose four states from different regions in an attempt to represent different regions of the country, as demonstrated by Gray et al.3 There are further significant limitations present when working with administrative data. Our primary intention was to investigate general trends in ambulatory cervical spine surgery and to provide broad surgical and demographic perspectives, rather than offer specific clinical information or guidelines. We found that most patients were discharged home after ambulatory cervical spine surgery (>99%), implying a low unplanned admission rate, and the calculated complication rate was low at 0.67%. These findings, at first glance, seem to suggest that cervical spine surgery can be performed safely in an ambulatory setting, especially when compared with the significantly higher rate of complications in the inpatient cohort. However, we caution readers that these values most likely underreport the actual complication rates for the following reasons.
The time course of complications could not be determined due to lack of patient identifiers for longitudinal follow-up. Although we attempted to focus on complications frequently observed in the immediate postoperative period, which in turn may be reflected in the patient being transferred to another health care facility rather than being discharged home, it is likely that some complications did not occur in the immediate postoperative period. It is also possible that many complications were not recorded in the data set because treatment for a complication may have occurred only after the patient was transferred to another facility; this may also be true for complications that did not require hospitalization or a further procedure to adequately treat. Furthermore, due to limitations inherent to using this database, we did not have a way to tell which patients, if any, returned to the hospital after discharge, or to keep track of the treatment of complications on an outpatient basis at another location, both of which could have significantly affected the reporting of complications. Moreover, there is potential for discrepancy in the definition of ambulatory, which may denote a procedure performed in a hospital with subsequent discharge in less than 24 hours or in an ambulatory surgery center where the patient must be transferred to a hospital if the stay is longer than 24 hours. Although the data set does provide the number of patients who were transferred to either a hospital or other facility, this could be a source of misclassification in the analysis of our data.
The complication rate in the inpatient cohort was 9.58% (p < 0.001), but comparison of complication rates between cohorts is limited. Patients in the inpatient cohort were in poorer health (implying selection bias), and the time course of care received in the inpatient setting significantly exceeded that in the ambulatory setting, which allowed detection and reporting of more complications (denoting a lead time bias).
Complication rates reported in studies examining outpatient cervical spine surgery have varied considerably from 0.39 to 10%.6 Silvers et al retrospectively reviewed their outpatient ACDFs and demonstrated similar rates of relief of neck and arm pain and weakness, return to normal activities and work, and patient satisfaction with surgery as with inpatient procedures, with no change in complication rates between the two groups.20 Similarly, in 2009, Liu et al retrospectively showed no complications associated with 45 single-level ACDF outpatients.8 Their findings may have been tempered by selection bias, as evidenced by the fact that the number of major medical comorbidities of outpatients was significantly less than that of inpatients (120 comorbidities in 64 inpatients versus 63 comorbidities in 45 outpatients). Of note, our cohort demonstrated a low medical comorbidities score (0.15) as calculated by the Charlson Comorbidity Index17 and subsequently modified by Deyo et al.18 Though we did not have data on Charlson Comorbidity Index scores from other studies for comparison, the number of comorbidities demonstrated in our study is lower than that reported by Liu et al.8
Of the potential complications following a cervical procedure, one important complication deserves discussion. Airway compromise, a potentially life-threatening complication encountered in anterior cervical spine surgery, has been reported in several studies.7 12 24 Sagi et al conducted a retrospective cohort study of 311 patients undergoing ACDF and found a 6.1% (n = 19) incidence of airway complication12; 1.6% (n = 6) of the patients required reintubation as a direct result of the complications. In this study, symptoms of airway compromise developed an average of 36 hours postoperatively, in contrast to the 6-hour window reported by Lied et al.7 Sagi et al also found that exposing more than three vertebral levels, exposures involving any level above C5, surgical time greater than 5 hours, and estimated blood loss of greater than 300 mL all correlated positively with the development of airway compromise.12 Other studies have demonstrated that smoking, asthma, prolonged operative time, obesity, transfusion requirement, and multilevel surgery or procedures involving C2 were linked to the development of significant postoperative prevertebral swelling but did not examine whether this had a causative effect on the development of airway complications.25 26 Fountas et al, in a retrospective cohort study examining 1,015 patients undergoing inpatient ACDF, noted that 5.6% of patients developed postoperative hematoma, with 2.4% requiring surgical evacuation due to airway compromise or threat of airway compromise.24 However, they did not indicate a time course for the development of complications. Garringer and Sasso conducted a prospective cohort study comprising 645 patients (83% of whom were outpatients) who underwent one-level ACDF from 1993 to 2006.9 In the outpatient group, patients were required to remain in the observation unit for at least 4 hours after surgery before being allowed to go home. The investigators reported a 0.3% (n = 2) incidence of complications, both of which were epidural hematomas and were identified within the mandatory 4-hour observation period. One of these required emergent evacuation, and the other patient was given systemic steroids and experienced improvement of symptoms within an hour.
In conclusion, we found an increase in cervical spine procedures performed in an ambulatory setting in recent years. Middle-aged patients were more likely to undergo an anterior procedure, whereas older patients were more likely to receive posterior surgery and comprised a small percentage of surgeries performed. Although the data suggest that the majority of patients were discharged home (>99%) after the procedure and the calculated complication rate was low, certain limitations inherent when analyzing administrative data make it impossible to assess its validity. Further investigation is needed to ensure the safety of cervical spine surgery in the ambulatory setting.
Footnotes
Disclosures Evan O. Baird, none Natalia N. Egorova, none Steven J. McAnany, none Sheeraz A. Qureshi, none Andrew C. Hecht, none Samuel K. Cho, none
References
- 1.Rathore M A, Andrabi S I, Mansha M, Brown M G. Day case laparoscopic cholecystectomy is safe and feasible: a case controlled study. Int J Surg. 2007;5(4):255–259. doi: 10.1016/j.ijsu.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 2.Kim S, Bosque J, Meehan J P, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93(11):994–1000. doi: 10.2106/JBJS.I.01618. [DOI] [PubMed] [Google Scholar]
- 3.Gray D T Deyo R A Kreuter W et al. Population-based trends in volumes and rates of ambulatory lumbar spine surgery Spine (Phila Pa 1976) 200631171957–1963., discussion 1964 [DOI] [PubMed] [Google Scholar]
- 4.Wang M C Kreuter W Wolfla C E Maiman D J Deyo R A Trends and variations in cervical spine surgery in the United States: Medicare beneficiaries, 1992 to 2005 Spine (Phila Pa 1976) 2009349955–961., discussion 962–963 [DOI] [PubMed] [Google Scholar]
- 5.Lad S P Patil C G Berta S Santarelli J G Ho C Boakye M National trends in spinal fusion for cervical spondylotic myelopathy Surg Neurol 200971166–69., discussion 69 [DOI] [PubMed] [Google Scholar]
- 6.Stieber J R, Brown K, Donald G D, Cohen J D. Anterior cervical decompression and fusion with plate fixation as an outpatient procedure. Spine J. 2005;5(5):503–507. doi: 10.1016/j.spinee.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Lied B Sundseth J Helseth E Immediate (0-6 h), early (6-72 h) and late (>72 h) complications after anterior cervical discectomy with fusion for cervical disc degeneration; discharge six hours after operation is feasible Acta Neurochir (Wien) 20081502111–118., discussion 118 [DOI] [PubMed] [Google Scholar]
- 8.Liu J T, Briner R P, Friedman J A. Comparison of inpatient vs. outpatient anterior cervical discectomy and fusion: a retrospective case series. BMC Surg. 2009;9:3. doi: 10.1186/1471-2482-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garringer S M, Sasso R C. Safety of anterior cervical discectomy and fusion performed as outpatient surgery. J Spinal Disord Tech. 2010;23(7):439–443. doi: 10.1097/BSD.0b013e3181bd0419. [DOI] [PubMed] [Google Scholar]
- 10.Trahan J Abramova M V Richter E O Steck J C Feasibility of anterior cervical discectomy and fusion as an outpatient procedure World Neurosurg 2011751145–148., discussion 43–44 [DOI] [PubMed] [Google Scholar]
- 11.Suk K S, Kim K T, Lee S H, Park S W. Prevertebral soft tissue swelling after anterior cervical discectomy and fusion with plate fixation. Int Orthop. 2006;30(4):290–294. doi: 10.1007/s00264-005-0072-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sagi H C, Beutler W, Carroll E, Connolly P J. Airway complications associated with surgery on the anterior cervical spine. Spine (Phila Pa 1976) 2002;27(9):949–953. doi: 10.1097/00007632-200205010-00013. [DOI] [PubMed] [Google Scholar]
- 13.Healthcare Cost and Utilization Project state inpatient and ambulatory surgery databases Available at: http://www.hcup-us.ahrq.gov/. Accessed October 2011
- 14.Wang M C, Chan L, Maiman D J, Kreuter W, Deyo R A. Complications and mortality associated with cervical spine surgery for degenerative disease in the United States. Spine (Phila Pa 1976) 2007;32(3):342–347. doi: 10.1097/01.brs.0000254120.25411.ae. [DOI] [PubMed] [Google Scholar]
- 15.Friedman A L Cheung K Roman S A Sosa J A Early clinical and economic outcomes of patients undergoing living donor nephrectomy in the United States Arch Surg 20101454356–362., discussion 362 [DOI] [PubMed] [Google Scholar]
- 16.Fry D E Pine M Jones B L Meimban R J Comparative effectiveness and efficiency in peripheral vascular surgery Am J Surg 20112013363–367., discussion 367–368 [DOI] [PubMed] [Google Scholar]
- 17.Charlson M E, Pompei P, Ales K L, MacKenzie C R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 18.Deyo R A, Cherkin D C, Ciol M A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 19.Marawar S, Girardi F P, Sama A A. et al. National trends in anterior cervical fusion procedures. Spine (Phila Pa 1976) 2010;35(15):1454–1459. doi: 10.1097/BRS.0b013e3181bef3cb. [DOI] [PubMed] [Google Scholar]
- 20.Silvers H R, Lewis P J, Suddaby L S, Asch H L, Clabeaux D E, Blumenson L E. Day surgery for cervical microdiscectomy: is it safe and effective? J Spinal Disord. 1996;9(4):287–293. [PubMed] [Google Scholar]
- 21.Angevine P D Arons R R McCormick P C National and regional rates and variation of cervical discectomy with and without anterior fusion, 1990-1999 Spine (Phila Pa 1976) 2003289931–939., discussion 940 [DOI] [PubMed] [Google Scholar]
- 22.Chassin M R Explaining geographic variations. The enthusiasm hypothesis Med Care 199331(5, Suppl):YS37–YS44. [DOI] [PubMed] [Google Scholar]
- 23.Lurie J D, Birkmeyer N J, Weinstein J N. Rates of advanced spinal imaging and spine surgery. Spine (Phila Pa 1976) 2003;28(6):616–620. doi: 10.1097/01.BRS.0000049927.37696.DC. [DOI] [PubMed] [Google Scholar]
- 24.Fountas K N, Kapsalaki E Z, Nikolakakos L G. et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007;32(21):2310–2317. doi: 10.1097/BRS.0b013e318154c57e. [DOI] [PubMed] [Google Scholar]
- 25.Emery S E, Smith M D, Bohlman H H. Upper-airway obstruction after multilevel cervical corpectomy for myelopathy. J Bone Joint Surg Am. 1991;73(4):544–551. [PubMed] [Google Scholar]
- 26.Epstein N E Hollingsworth R Nardi D Singer J Can airway complications following multilevel anterior cervical surgery be avoided? J Neurosurg 200194(2, Suppl):185–188. [DOI] [PubMed] [Google Scholar]


