Abstract
Study Design Literature review.
Objective Atlantoaxial dislocation (AAD) is a rare and potentially fatal disturbance to the normal occipital-cervical anatomy that affects some populations disproportionately, which may cause permanent neurologic deficits or sagittal deformity if not treated in a timely and appropriate manner. Currently, there is a lack of consensus among surgeons on the best approach to diagnose, characterize, and treat this condition. The objective of this review is to provide a comprehensive review of the literature to identify timely and effective diagnostic techniques and treatment modalities of AAD.
Methods This review examined all articles published concerning “atlantoaxial dislocation” or “atlantoaxial subluxation” on the PubMed database. We included 112 articles published between 1966 and 2014.
Results Results of these studies are summarized primarily as defining AAD, the normal anatomy, etiology of dislocation, clinical presentation, diagnostic techniques, classification, and recommendations for timely treatment modalities.
Conclusions The Wang Classification System provides a practical means to diagnose and treat AAD. However, future research is required to identify the most salient intervention component or combination of components that lead to the best outcomes.
Keywords: atlantoaxial dislocation, atlantoaxial subluxation, comprehensive review, classification, diagnosis, treatment
Introduction
Atlantoaxial dislocation refers to a loss of stability between the atlas and axis (C1–C2), resulting in loss of normal articulation (Fig. 1). The atlantoaxial joints can lose stable articulation from traumatic, inflammatory, idiopathic, or congenital abnormalities.1 The mechanism of injury typically remains unidentified with several theories proposed in the literature.2 Although it occurs in all age groups, atlantoaxial dislocation is most often seen in adolescents. Atlantoaxial dislocations have been previously studied extensively and reported in the literature with subsequent treatment recommendations published using older, less relevant classification systems. However, given recent advances in diagnostics and surgical techniques, this systematic review provides a concise summary of our current knowledge of atlantoaxial dislocation and offers treatment guidelines based on the most recent clinical evidence.
Fig. 1.
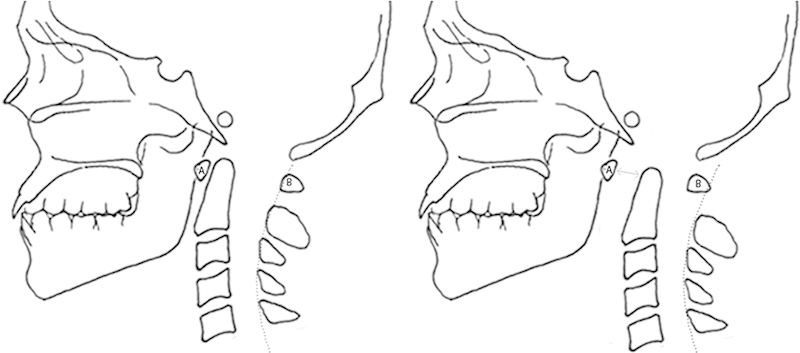
Schematic representation of atlantoaxial dislocation. Lateral view of the normal cervical spine in relation to the occiput (left) compared with an abnormal relationship between the cervical spine and occiput representing an atlantoaxial dislocation (right). An increase in the distance between the anterior surface of the dens and the posterior surface of the C1 tubercle (A) as measured by the gray arrowed line is shown. The dotted line represents an imaginary line connecting the spinolaminar white lines (the junction between the lamina and the spinous process) and shows that the body of C1 (B) is displaced anteriorly relative to the cervical spine. The atlantodental interval (ADI) is measured between the posterior aspect of the anterior atlas ring and the anterior aspect of the odontoid process. The ADI is often constant in distance during movement of the head and generally does not exceed 3 mm for adults and 5 mm for children. Atlantoaxial dislocation is defined as ADI greater than 3 mm in adults older than 18 years of age and greater than 5 mm in children.
Anatomy of the Atlantoaxial Region
The atlantoaxial joint allows complex movements of the cervical spine while providing sufficient mechanical strength to stabilize the head. About 50% of total cervical spine flexion and extension occurs at the occiput–C1 articulation.3 4 Flexibility is provided by the dens (odontoid process) of C2 (the axis), which articulates with the C1 (atlas) and transverse ligaments, accounting for over 50% of all cervical spine rotation.3 4 To provide this flexibility, the synovial joints at these segments do not have the same osseous and intervertebral disk-related stability mechanisms as the rest of the spinal column, relying more on ligamentous stabilizers.5 The region is unique in that the occiput–C1 articulation and the C1–C2 articulation are the only vertebral segments without intervertebral disks, and the vertebral bodies do not directly bear the load distribution from the occiput. The occipital condyles transfer the load at the articulation with the C1 lateral masses, which transfers the load onto the C2 lateral masses.4
Stability against anterior translation is provided by the transverse ligament, which runs across the posterior dens, attaching on either side at the lateral masses of C1 and holding the dens in position. A small fascicular vertical portion of the transverse ligament articulates with the occiput superiorly and body of the axis inferiorly.6 Additional stabilization of the dens comes from the alar ligaments, which extend off the odontoid in a lateral and cephalad direction to the basilar portion of the occiput. The transverse ligament is larger and stronger than the alar ligaments, thus providing a greater portion of the stability, with the alar ligaments providing secondary support.6 7 Unlike in the lower cervical spine, the C1–C2 facets are oriented in the axial plane and have no bony structure between them preventing dislocation. This joint thus relies solely on the integrity of the transverse ligament to prevent anterior dislocation of C1 and the odontoid process abutting the anterior arch of the atlas to prevent posterior dislocation.
Etiology of Atlantoaxial Dislocation
Atlantoaxial dislocation can be broadly categorized into separate traumatic, congenital, or inflammatory etiologies, although the cause is commonly multifactorial.
Traumatic Causes
A purely traumatic atlantoaxial dislocation in the absence of another predisposing risk factor is extremely rare. A literature review by Venkatesan et al in 2012 found only 12 adult case reports.8 Traumatic atlantoaxial dislocation is due to forced displacement of the neck resulting in disruption of the transverse ligament. Rarely, injury of the transverse ligament can also involve simultaneous disruption of the alar and apical ligaments. Such injuries may be seen in head injuries, which may occur during tackling in football or rugby. In these ligamentous dislocations, the atlas will lose articulation with the dens, and the anterior atlantal arch may translate completely superiorly and posteriorly with significant damage to the ligaments.9
Traumatic osseous injuries may also result in atlantoaxial instability. Type II odontoid fractures occur at the base between the transverse ligament and body of C2 body.10 11 12 Type II fractures are the most common odontoid fracture and the only type normally associated with atlantoaxial dislocation.10 Traditionally believed to be a congenital anomaly, os odontoideum may in fact be caused by an early traumatic injury in which the odontoid is separated completely from the axis and then heals to resemble a separate ossicle. The resulting condition predisposes patients to dislocation.13 14
Congenital Causes
Certain congenital conditions are associated with craniocervical region abnormalities that predispose these populations to developing atlantoaxial dislocation.15 One particularly well-studied condition is Down syndrome. Down syndrome (trisomy 21) is the most common inherited chromosomal disorder.16 Predisposing sequela include hypermobility and instability caused by ligamentous laxity and osseous abnormalities,17 18 resulting in an increased incidence of atlantoaxial dislocation (15 to 20%).19 Ligamentous laxity may be due to an inflammatory process or to an intrinsic defect in collagen fibers that form ligaments.20 Alternatively, chronic environmental trauma seen in these population superimposed on congenitally weakened ligaments can lead to spondylitis with subsequent atlantoaxial dislocation.18
Skeletal dysplasias are a heterogeneous group of disorders with resulting abnormal cartilage and bone formation, growth, and remodeling. Craniocervical junction abnormalities, atlantoaxial dislocation, and kyphoscoliotic deformities are among the common spinal problems that are found in certain skeletal dysplasias.16 Examples of skeletal dysplasias that have been linked with atlantoaxial dislocation include Goldenhar syndrome, spondyloepiphyseal dysplasia, and Morquio syndrome.16
Goldenhar syndrome is a clinically heterogeneous disorder characterized by spinal defects, hemifacial microsomia, and epibulbar dermoid appendages. An increased frequency of hypoplasia of the dens with atlantoaxial instability has been reported in children with Goldenhar syndrome.16 In one series of eight children with Goldenhar syndrome, three had atlantoaxial instability greater than 5 mm with upward migration of the odontoid process. Two of the patients had atlantoaxial instability greater than 7 mm and required surgical treatment.21
Spondyloepiphyseal dysplasia encompasses several disorders characterized by abnormal growth of the spinal vertebrae and epiphysis. Typically, individuals with spondyloepiphyseal dysplasia have short-trunk dwarfism, with short proximal and middle limbs but normal-sized hands and feet.16 Atlantoaxial instability associated with hypoplasia of the dens or ligamentous laxity is the most common spinal manifestation of congenital spondyloepiphyseal dysplasia in children. An increased incidence, as high as 35% of cervical myelopathy in children with congenital spondyloepiphyseal dysplasia, may be attributable to atlantoaxial dislocation.22
Mucopolysaccharidosis type IV (Morquio syndrome) is an autosomal recessive lysosomal storage disease characterized by an inability to metabolize keratan sulfate. These patients often have normal growth and development during the first 2 years of life with abnormalities progressing rapidly after 2 years of life.16 Atlantoaxial dislocation has been identified in up to 42 to 90% of cases of Morquio syndrome,23 24 likely due to an increased incidence of odontoid dysplasia (hypoplasia, aplasia, or os odontoideum) and increased ligamental laxity.23 Other syndromes that have been associated with the development of atlantoaxial dislocation are listed in Table 1.
Table 1. Congenital conditions associated with atlantoaxial dislocation.
| Congenital condition | Class | Etiology | Incidence |
|---|---|---|---|
| Down syndrome16 17 | Chromosomal disorder | Inflammatory process or an intrinsic defect in collagen fibers that form ligaments20 | 15–20%19 |
| Goldenhar syndrome | Skeletal dysplasia | Hypoplasia of the dens with atlantoaxial instability16 | 3 of 8 in one case series21 |
| Spondyloepiphyseal dysplasia | Skeletal dysplasia | Abnormal growth of the spinal vertebrae and epiphysis,16 hypoplasia of the dens or ligamentous laxity22 | 35%22 |
| Morquio syndrome (mucopolysaccharidosis type IV) | Skeletal dysplasia | Autosomal recessive lysosomal storage disease, resulting in odontoid dysplasia | 42–90%23 24 |
| Occipitalization of the atlas | Congenital osseous abnormalities | Abnormal motility in the joint region26 | – |
Congenital osseous abnormalities, in the absence of an underlying genetic abnormality, are also frequently associated with atlantoaxial dislocation. Wang et al documented a rate of 18% among 904 patients in the largest published series to date.25 Failures in segmentation, such as occipitalized atlas, C2–C3 fusion, and asymmetrical occiput–C3 facet joints, can predispose to dislocation.14 26 Occipitalization of the atlas occurs when the inferior neural arch and superior spinal sclerotome form improperly. Patients with occipitalization of the atlas may also have asymmetrical occipitoatlantal facet joints because the same sclerotomal segments contribute to development of the facets.
Inflammatory Causes
Another notable population that is disproportionately affected by atlantoaxial dislocation is chronic rheumatoid arthritis patients, particularly adults. The atlantoaxial joint is frequently affected in rheumatoid arthritis with studies showing incidence rates ranging from 23 to 86% of patients with rheumatoid arthritis.27 28 29 The rates we present here are based on traditional rates. Although it is not well documented, it is likely the rate has declined in conjunction with advancements in medical treatment of rheumatoid arthritis (i.e., biologics and immunoregulatory medications). The cervical spine often becomes involved early in the course of rheumatoid arthritis, leading to three different patterns of instability: atlantoaxial dislocation, atlantoaxial impaction, and subaxial subluxation.30 Chronic systemic inflammation in these patients leads to chronic synovitis resulting in bony erosion and ligamentous laxity that may result in instability and atlantoaxial dislocation. In patients with rheumatoid arthritis, anterior atlantoaxial dislocation is the most frequently occurring deformity due to laxity of the ligamentous restraints.3 31 32
Resulting Pathology
When the upper cervical spine is destabilized and sagittal balance is compromised, the lower cervical spine compensates, which may lead to subaxial pathology and deformities.1 33 34 35 When atlantoaxial dislocation causes diminished lordosis at the C0–C2 segment, the subaxial cervical region compensates with increased lordosis to maintain balance.33 35 Some patients with end-stage changes can develop kyphosis at the occipitoaxial segment together with extreme hyperlordosis subaxially, resulting in swan neck deformity.33
Clinical Presentation
The presentation of atlantoaxial dislocation may range from minor axial neck pain to death. Approximately 50% of patients present with neck pain and/or neck movement restriction, 70% with weakness and/or numbness, and 90% with pyramidal signs.33 36 37 Other preoperative clinical presentations include sphincter disturbances, lower cranial nerve dysfunction, and respiratory distress. Other serious sequelae include myelopathy, respiratory failure, vertebral artery dissection, neurologic compromise, and rarely quadriplegia or death if left untreated.38 39 40 The differential diagnosis of atlantoaxial dislocation includes torticollis, atlantoaxial rotary fixation, and odontoid fractures without atlantoaxial dislocation.
Most cases of atlantoaxial dislocation appear in the adolescent population and should be considered in a child with inability or unwillingness to turn their head when history and physical examination are inconsistent with torticollis.41 Typically, congenital atlantoaxial dislocation presents in childhood as chronically progressive spinal canal compression and associated with neurologic and respiratory symptoms.42 Less commonly, a patient with a congenital yet asymptomatic unstable atlantoaxial joint may have an acute presentation after minor acute trauma. In one study, 9 of 15 patients who presented after acute trauma with congenital atlantoaxial dislocation presented with quadriplegia.41 The symptoms may also present as relapsing and remitting episodes due to the motion of day-to-day life.26 38 42
Atlantoaxial dislocation presenting in adulthood has historically been the result of rheumatoid arthritis, with some patients experiencing few symptoms and others experiencing gross instability and neurologic compromise. Clinical findings can be confounded by the severity of systemic involvement. Radiographic changes are common, and the prevalence of neurologic injury is relatively low.30 More recent series have found a decreased prevalence of atlantoaxial dislocation among patients with rheumatoid arthritis, especially with various immunoregulatory medications showing promising outcomes preventing cervical spine lesions in patients with rheumatoid arthritis.43 44 One study that investigated a total of 904 patients with a diagnosis of atlantoaxial dislocation over a period of 12 years showed that only 36 patients (4%) had rheumatoid arthritis.25 Regardless of the etiology, the clinical consequences of atlantoaxial dislocation have clear potential for neurologic compromise. Therefore, a careful history is critical to identify symptoms of cervical disease, and physical and neurologic examinations should be performed in all at-risk patients.3
Diagnosis
There are several different approaches to diagnosing atlantoaxial dislocation; however, no consensus exists. Atlantoaxial dislocation can be defined with radiographic measurements of atlantoaxial joint articulation using the atlantodental interval (ADI). The ADI is a small slitlike space between the posterior aspect of the anterior atlas ring and the anterior aspect of the odontoid process. Flexion and extension radiographs of the neck allow for the measurement of the ADI and to determine whether the atlantoaxial joint reduces itself in these positions.38
The ADI is measured from a line projected superiorly along the anterior border to the axis body to the anterior arch of the atlas (Figs. 1 and 2).45 The ADI is normally constant in distance during movement of the head and generally does not exceed 3 mm for adults and 5 mm for children.33 45 46 In this article, we define atlantoaxial dislocation as ADI greater than 3 mm in adults older than 18 years of age and greater than 5 mm in children. The majority (70%) of clinical atlantoaxial dislocation presentations are due to anterior dislocations.41 Anterior dislocation increases the ADI, decreasing the space available for the spinal cord, which is measured from the posterior aspect of the dens to the anterior aspect of the posterior atlantal ring.41 A decrease in the space available for the spinal cord increases the risk of spinal cord compression as well as neurologic sequelae. Of note, the space available for the spinal cord of less than 14 mm predicts the development of paralysis47 48 and has been shown to correlate with severity of paralysis.48
Fig. 2.
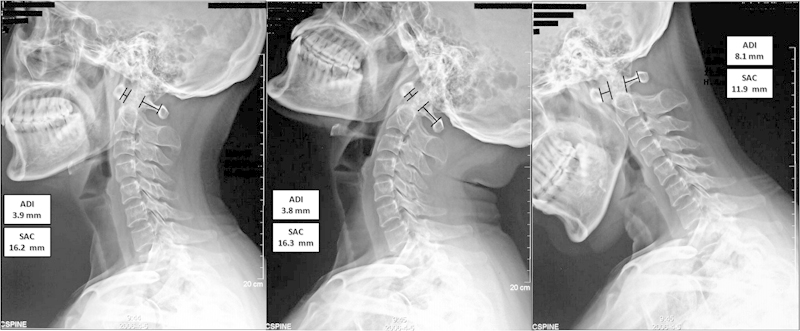
Neutral (left), extension (center), and flexion (right) lateral X-rays showing the atlantodental interval (ADI) anterior to the odontoid process and the space available for spinal cord posteriorly. The ADI is above the average for adults of 3 mm and is slightly reduced in extension, but severely increased in flexion. This patient's space available for spinal cord (SAC) reducing to below 14 mm indicates risk of paralysis.
Neutral and dynamic cervical radiographs are often used to diagnose atlantoaxial instability and dislocation, but the diagnostic sensitivity is low. Some studies report decreased false-negative diagnostic rate when using dynamic radiography, with some studies also reporting the necessity for magnetic resonance imaging (MRI) to obtain information on soft tissues, joints, and the spinal cord with high sensitivity and specificity and to possibly provide early warnings signs of instability.41 When evaluating trauma patients with concerns about cervical spine involvement, it is important to most efficiently and effectively evaluate the cervical spine to avoid missing the injury. The NEXUS study group reported reliability of a standard three-view imaging of the cervical spine that included an open-mouth odontoid view, an anterior-posterior view, and a cross-table lateral view.49 Another study supports the use of cervical computed tomography (CT) for diagnosis given the higher specificity.50
Classification of Atlantoaxial Dislocations
Atlantoaxial dislocation was initially classified by Greenberg into two subcategories—reducible and irreducible.46 Greenberg further devised a treatment strategy based on this system. For irreducible atlantoaxial dislocation, Greenberg specifically stated that the treatment must be aimed at immediate decompression and achieving stabilization.46 Greenberg's work has been considered a landmark publication and is considered by many to be the gold standard for atlantoaxial dislocation treatment in the subsequent literature.51 Fielding and Hawkins subsequently developed a new classification system according to the direction of dislocation—anterior, posterior, lateral, and rotational.52 This classification, known as the Fielding classification system, has been widely accepted for clinical application. Unfortunately, it was not found to have clinical significance in treatment or grading severity of injuries as the majority of clinical dislocations encountered were anterior.45 Wang has recently proposed a novel classification system that aims to standardize atlantoaxial dislocation classification and treatment strategy.51 Referred to as the “Wang classification system” in this article, it draws from Greenberg's system and is primarily based on classifying dislocations as reducible or irreducible atlantoaxial dislocation. According to this treatment algorithm, which includes preoperative evaluation using dynamic radiographs, reconstructive CT, and skeletal traction test, the Wang classification (Table 2) categorizes atlantoaxial dislocation into four types: instability (type I), reducible dislocation (type II), irreducible dislocation (type III), and bony dislocations (type IV).51 This novel classification system offers a unique diagnosis and treatment protocol for clinicians suspecting atlantoaxial dislocation in a patient.
Table 2. Wang classification system of atlantoaxial dislocations.
| Type | Description | Diagnosis | Incidence (%) | Treatment |
|---|---|---|---|---|
| I | Instability | Reducible in dynamic X-rays | 52.2 | Posterior fusion procedure |
| II | Reducible | Reducible with skeletal traction under general anesthesia | 17.7 | Posterior fusion procedure |
| III | Irreducible | Irreducible with skeletal traction under general anesthesia | 29.6 | Transorally released anteriorly before posterior fusion |
| IV | Bony dislocations | Dislocations with bony anomalies that are visualized by reconstructive computed tomography scan | 0.4 | Transoral odontoidectomy |
Treatments
Treatment of atlantoaxial dislocation is aimed at the correction of the sagittal alignment of the upper cervical spine and the stabilization in near anatomical alignment.45 There is no uniformly accepted method for determining treatment strategies, with extremely varying opinion on indications of nonoperative versus operative treatment modalities and on which operative techniques are more appropriate.19 26 53 54 55 56 Some resources state that surgical treatment is recommended even in asymptomatic atlantoaxial dislocation to avoid development of myelopathy due to concerns about increased morbidity and mortality associated with atlantoaxial dislocation in patients presenting with myelopathy.38 39 40 57 Recently, Wang et al have provided treatment recommendations based on the Wang classification system previously described.25 Although not uniformly adopted, the classification system is unique in that it offers clear clinical and radiographic parameters for the clinician to reference.51
The main procedures reported in the literature are posterior occipitocervical/C1–C2 fusion after transoral odontoidectomy or periodontoid tissue release. Fusion of the atlantoaxial joint greatly reduces the range of motion by preventing rotation of the occipitocervical region.41 These procedures have many disadvantages, such as increasing hospitalization costs and length of stay, which may discount their effectiveness.36 Surgical reduction and fixation of atlantoaxial dislocation is not without risk. One of the most serious complications is vertebral artery injury as it can have serious sequelae with poor prognosis such as exsanguination or catastrophic injury if not treated rapidly.58 Both anterior and posterior approaches can pose a risk for vertebral artery injury, reported incidences ranging from 0 to 8.2% for posterior atlantoaxial transarticular screw fixation.44 Dickman et al reported an overall complication rate of 9.4% during transoral surgery, even in experienced hands including cerebrospinal fluid leakage, wound dehiscence, wound infection, pneumonia, and death.108
Obtaining physiologic alignment is of particular importance. Normal upper cervical alignment differs between children, male adults, and female adults. Mean sagittal spinal angles according to group are provided in Table 3 . Fusion of the atlantoaxial joint or occipitoaxial segment in hyperlordosis can place patients at high risk for postoperative iatrogenic subaxial loss of lordosis, or even kyphosis. According to a study by Matsunaga et al, a small number of patients (13%) with atlantoaxial dislocation developed postoperative kyphosis and swan neck deformity and more patients (32%) experienced subaxial subluxation after surgery.34 High postoperative incidence of degenerative disk disease after fixation for atlantoaxial dislocation has also been reported in the setting of fusion in nonphysiologic lordosis.35 Several authors have reported on the development of subaxial subluxation following occipitocervical fusion.34 35 In such cases, degenerative disk disease was found near the apex of the subaxial sagittal curvature (C6–7) rather than at levels adjacent to the fusion.33
Table 3. Mean sagittal spinal angles according to age group.
| Oc–C2 (°) | C1–C2 (°) | C2–C7 (°) | C1–C7 (°) | C7 slope | |
|---|---|---|---|---|---|
| Pediatric (average 8.8 y)106 | −15.2 (±6.7) | −26.0 (±6.2) | −6.5 (±11.7) | −32.7 (±11.3) | 21.3 (±6.9) |
| Pediatric (average 14.2 y)106 | −18.3 (±6.1) | −30.3 (±6.0) | −0.7 (±11) | −30.5 (±10.1) | 17.4 (±6.6) |
| Male adults107 | 14.5 (±8) | 26.5 (±7) | 16.2 (±12.9) | n/a | n/a |
| Female adults107 | 16 (±8.5) | 28.9 (±6.7) | 10.5 (±10.3) | n/a | n/a |
Nonoperative Treatment
Nonoperative treatment for atlantoaxial dislocation consists of cervical halter traction in the supine position and active range-of-motion exercises for 24 to 48 hours first, followed by ambulatory orthotic immobilization with active range-of-motion exercises until free motion returns.59 Particular conditions and patient populations are recommended for nonoperative treatment. For example, children presenting acutely with evidence of transverse ligament disruption, diagnosed within 3 weeks, can be treated nonoperatively in the absence of neurologic injury.60 The vast majority of patients with Grisel syndrome will improve spontaneously, and thus may be treated with halter traction if the atlantoaxial dislocation does not improve spontaneously. However, with persistent instability, stabilization with posterior arthrodesis is required.21 Nonoperative treatment in symptomatic adults is generally not advised in the absence of surgical contraindications.
Certain patient populations predisposed to atlantoaxial dislocation also have recommendations for preventative treatment and screening as well. For example, it is recommended that patients with Down syndrome obtain cervical radiographs between 3 and 5 years of age and have their cervical canal width measured.61 Controversy exists regarding optimal management in the subset of patients with Down syndrome with asymptomatic atlantoaxial dislocation. The Special Olympics mandated screening all potential participants with Down syndrome in 1983 for atlantoaxial dislocation and limiting the participation of those patients found to have radiographic evidence of instability.16 Although supported by the Committee on Sports Medicine of the American Academy of Pediatrics, controversy about appropriate interventions in these asymptomatic patients still remains.62 In fact, it is unclear if asymptomatic patients with Down syndrome with an ADI greater than 4.5 mm are at higher risk for neurologic sequelae.61
Management of patients with rheumatoid arthritis is aimed at preventing permanent neurologic injury while avoiding potentially dangerous and unnecessary surgery. Strategies include patient education, lifestyle modification, regular radiographic follow-up, and early surgical intervention when indicated. MRI is indicated when myelopathic symptoms are present or when plain radiographs show atlantoaxial dislocation with the space available for the spinal cord less than or equal to 14 mm, any degree of atlantoaxial impaction, or subaxial stenosis with a canal diameter less than or equal to 14 mm.30 There is evidence that the incidence of upper cervical abnormalities is lessened by early, aggressive drug treatment, specifically administration of disease-modifying antirheumatic drugs in combination with newer immunologic mediators such as tumor necrosis factor-α blockers.3 32 When administered before the onset of cartilage destruction, these drugs may actually prevent or significantly mitigate the development of changes in the cervical spine.3 These patients generally have better outcomes when treated before the onset of myelopathy.3 32 Not as well established, however, is whether immunoregulatory drugs have the potential to interrupt the onset of ongoing degenerative changes. Radiographs of the cervical spine with lateral flexion-extension dynamic views should be obtained periodically and used to evaluate the cervical spine before elective surgery requiring general anesthesia. Advanced imaging, such as MRI, myelography, and CT, may be necessary to evaluate neuraxis.3
Patients with Goldenhar syndrome with an ADI less than 6 mm should get cervical flexion-extension films every 6 months and be advised against contact sports. Surgical treatment is recommended in any child with instability greater than 6 mm to reduce the possibility of catastrophic spinal cord impingement. Moreover, the relatively high frequency of cervical malformations in patients with Goldenhar syndrome may warrant extensive radiographic investigation and planning before surgery.21 Likewise, not all patients with atlantoaxial dislocation secondary to Morquio syndrome have spinal cord compression or require surgery. Asymptomatic patients or patients with a less than 50% reduction in spinal cord diameter may not require surgical treatment. However, the preferred time for elective surgery is between 3 and 8 years of age when skeletal anomalies are well developed.24
Indications for Surgical Treatment
Surgical treatment for patients with symptomatic atlantoaxial dislocation is widely accepted to protect against potential respiratory failure, progressive neurologic symptoms, and death.63 However, there is a lack of consensus on surgical indications for asymptomatic atlantoaxial dislocation as these patients are at risk for new-onset severe neurologic and respiratory compromise from a minor acute trauma.42 64 Different suggestions exist in the literature for these asymptomatic patients depending on patient age and underlying diagnosis. For adults, surgical treatment can be considered if ADI is greater than 5 mm. Surgical fusion is indicated in children when one or more of the following is present: neurologic involvement, persistent anterior displacement with ADI greater than 4 mm,65 deformity present for more than 3 months, or recurrence of deformity following 6 weeks of immobilization. In young adults, fusion is recommended when moderate displacement is seen in flexion and extension cervical radiographs or instability with or without pain is present.51 60 66 67
In patients with rheumatoid arthritis, surgery should be considered promptly in an asymptomatic patient with atlantoaxial dislocation for any of the following: chronic neck pain in the setting of radiographic instability that does not respond to nonnarcotic pain medication, any degree of atlantoaxial impaction or cord stenosis seen radiographically, the space available for the spinal cord less than or equal to 14 mm, atlantoaxial impaction represented by odontoid migration less than or equal to 5 mm rostral to McGregor line, sagittal canal diameter < 14 mm, or cervicomedullary angle < 135 degrees.30 For patients with Down syndrome or os odontoideum, there is no clear surgical indication in the literature, but it is recommended to monitor with annual lateral and flexion/extension cervical radiograph due to the possibility of sudden change from spinal cord compression in this patient population.68 69 Due to the paucity of universally accepted guidelines in the literature, more research on the relative risks of surgery versus neurologic deterioration due to an asymptomatic atlantoaxial dislocation is needed given the lack of patient-derived outcome data.42 64
Methods for Surgical Treatment
Attempt at Conversion of Irreducible to Reducible Atlantoaxial Dislocation via Traction
The first step in correcting atlantoaxial dislocation is attempting reduction of the dislocation. When the dislocation is not easily reduced by neck flexion or extension, different intraoperative or preoperative approaches can be utilized to attempt reduction via traction (Fig. 3). Traction lengthens and relaxes muscles around the dislocation, thereby enabling settling into normal anatomical position. Some surgeons choose to curarize back and neck muscles to alleviate tension and to briefly apply skeletal traction with the patient under general anesthesia for a rapid reduction before fixation in the same surgical session.19 55 The entire reduction procedure with curarization takes ∼10 minutes. Traction weight should start at 7 to 8% of body weight and gradually increase to a maximum of ∼7 kg, and reduction should be monitored by sequential lateral radiographs.26 64
Fig. 3.
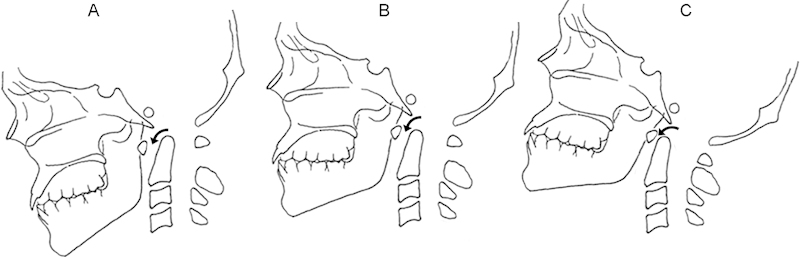
A schematic representation of the traction technique involving three stages to reposition the joint. In the initial distraction phase (A), the patient is placed in slight flexion to keep the ring of C1 opposed to the posterior odontoid and to avoid hitting the spinal cord as traction weight is gradually added. After full distraction, the realignment phase (B) will occur when C1 slips back over the odontoid. Excessive flexion during distraction could cause the ring to slip too far forward. The release phase (C) consists of switching to an extension posture and slowly releasing traction over several hours with gradual weight reduction. Note the gradual realignment of the occiput to the cervical spine, as denoted by the decreasing atlantodental interval (black arrows).
It is also possible to apply traction over a longer period preoperatively without general anesthesia and muscle curarization to slowly elongate muscles and reduce the joint.19 53 Reductions without such relaxation techniques are less likely to be successful and have been shown to take longer traction durations even when successful.9 Three stages of reduction have been described in complete C1–C2 dislocations. In the initial distraction phase, the patient is placed in slight flexion to keep the ring of C1 opposed to the posterior odontoid and to avoid hitting the spinal cord as traction weight is gradually added. After full distraction, the realignment phase will occur when C1 slips back over the odontoid. Excessive flexion during distraction could cause the ring to slip too far forward, so care must be taken through these stages to properly position C1 and C2. Finally, the release phase consists of switching to an extension posture and slowly releasing traction over several hours with gradual weight reduction.9
Traction may induce an increase in canal diameter due to the distraction of the odontoid from the foramen magnum.70 71 Several studies report successful reduction of irreducible atlantoaxial dislocation up to 80% with traction,71 with others reporting equally high failure rates.15 If the reduction procedure is successful, defined by achieving an ADI measuring less than 3 mm in adults and 5 mm in children, the operation may proceed with a posterior fusion to stabilize the reduced reducible atlantoaxial dislocation. Reducible atlantoaxial dislocation requires posterior fusion alone while an irreducible atlantoaxial dislocation requires an anterior transoral decompression plus posterior fusion.14 51 72 Posterior decompression and fusion alone are not sufficient in irreducible atlantoaxial dislocation as they may only achieve partial decompression while stabilizing the upper cervical spine in a suboptimal position. Assessment of the reducibility of the atlantoaxial dislocation is critical prior to proceeding with posterior fusion alone to optimize adequate decompression and restoration of physiologic alignment.73
Anterior Methods
An irreducible dislocation with persistent compression causing profound neurologic deficit after traction may necessitate an anterior approach.51 Although it is possible that neurologic status can improve simply with a successful fusion, it is generally accepted that irreducible atlantoaxial dislocation must be either released or decompressed prior to fixation. Currently, the most accepted treatment for irreducible atlantoaxial dislocation is transoral odontoidectomy.74 Most techniques that are approached anteriorly, such as transoral anterior release and transoral atlantoaxial reduction plate (TARP), have shown positive results (Table 4).
Table 4. Select clinical series.
| Authors | Study design | Demographics | Etiology | Surgery | Outcomes and complications |
|---|---|---|---|---|---|
| Wang et al (2007)54 | Retrospective clinical and radiologic case series | n = 57; 35 M, 22 F; mean age: 35 y (range, 13–66 mo); average follow-up 47 mo (range, 24–76) | Reducible atlantoaxial dislocation (AAD): os odontoideum (n = 26) | Transarticular screw fixation with morselized autograft (n = 57) | 2 screw malplacements: 1 penetrated to occipitoatlantal joint, 1 slightly breached vertebral artery groove, no clinical sequelae |
| Reducible AAD: transverse ligament disruption/relaxation (n = 20) | |||||
| Reducible AAD: odontoid fracture nonunion (n = 6) | |||||
| Irreducible AAD: os odontoideum (n = 1) | Transoral anterior AA joint release and reduction for irreducible AAD (n = 5) | No screw fracture, loosening, or backing out | |||
| Irreducible AAD: transverse ligament relaxation (n = 1) | No pseudarthrosis | ||||
| Irreducible AAD: malunion of odontoid fracture (n = 3) | 2 cases of postoperative iatrogenic C2–C3 instability | ||||
| Harms and Melcher (2001)88 | Retrospective clinical and radiologic case series | n = 37; 19 M, 18 F; mean age: 49 y (range, 2–90) | Fractures (n = 20) | Polyaxial C1L-C2PSF (n = 37) | 1 deep wound infection |
| Symptomatic os odontoideum (n = 6) | No cases of implant failure | ||||
| Rheumatoid arthritis (n = 4) | Solid fusion in all patients | ||||
| Rotary subluxation (n = 3) | Transoral odontoidectomy (n = 2) | ||||
| Osteoarthritis C1–C2 (n = 2) | Satisfactory screw placement in all patients | ||||
| Congenital malformation (n = 2) | No dural laceration or vertebral artery injury |
Abbreviations: AA, atlantoaxial; AAD, atlantoaxial dislocation; C1L-C2PSF, C1 lateral mass screw and C2 pedicle screw fixation.
In the transoral odontoidectomy, the apical and alar ligaments are detached with a curette before removing the dens from top down.74 More recent advances have made it possible to do a less invasive odontoidectomy endoscopically via a transnasal, transoral, or retropharyngeal approach. The endoscopic transoral odontoidectomy procedure obtains access through an incision in the midline pharyngeal wall, avoiding any palatal splitting or use of self-retaining retractors. The transoral endoscopic approach has yielded promising results with improvement in neurologic status after surgery.75 However, cerebrospinal fluid leakage, incomplete decompression, infection, abscess formation, vertebral artery injury, and spinal cord injury have been reported during transoral decompression, and other more serious complications such as death from vertebral artery injury and respiratory distress should be considered and discussed with the patient.1 55 74 76 Moreover, excessive bone removal of the odontoid and parts of the C2 body is a possible adverse effect as it compromises the C2 pedicle, which can disrupt posterior fixation.55 Less invasive endoscopic approaches may become more popular as the techniques advance. An endoscopic expanded endonasal approach has been explored previously in a cadaveric study.77 78 Similarly, an endoscopically assisted retropharyngeal approach with a small incision in the angle of the mandible has been performed with positive results.79 All 21 patients undergoing the retropharyngeal approach in one prospective study had an uneventful recovery with significant improvement in neurologic function and radiographic parameters.79
The TARP technique eliminates the need for a two-step operation. This technique uses a reduction plate capable of anterior decompression, reduction, and fusion for anterior irreducible atlantoaxial dislocation in one stage.80 81 82 In this procedure, incision of the posterior pharynx and exposure of C1 and C2 are completed similar to the other transoral approaches. The TARP is placed on the anterior aspect of C1, and the reduction screw is then inserted into the C2 body. One notch of the TARP system engages the TARP at the midline and the other engages the protruding reduction screw, causing distraction forces between C1 and C2, pushing C1 superiorly with the reduction screw serving as a base. The joint is then fused with bone graft.80 81 This procedure is advantageous because it is able to reduce and provide adequate internal fixation and stabilization, making a posterior procedure unnecessary and reducing the duration of hospitalization and surgery as well total cost. In a 2- to 4-year follow-up study, adequate anatomical reduction was seen in 100% of patients with 73.3% having improved spinal cord function.81
Anterior transarticular screw fixation is yet another option to reduce fixed atlantoaxial dislocation. It provides a safer and more appropriate environment with high fusion rates and only minor complications for challenging cases such as patients with osteolysis in infectious or tumorous conditions, aberrant vertebral artery, and/or narrow pars interarticularis.83 However, there are concerns about safe screw dimension, insertion, and trajectory. One study analyzed the feasibility of anterior transarticular screw fixation in 100 patients and recommended reliable fluoroscopic landmarks with minor complications and threshold lengths of C1 purchase screws during this procedure.83
Posterior Methods
The most common posterior surgical methods include C1–C2 transarticular screw fixation, C1 lateral mass screw–to–C2 pedicle screw fixation, and C1 lateral mass screw–to–C2 laminar screw fixation. Posterior techniques can be used alone for reducible atlantoaxial dislocation treatment or in conjunction with anterior transoral decompression to treat certain types of irreducible atlantoaxial dislocation. In many cases, the posterior instrumentation extends to the occiput or fuses the occiput to the axis, especially if there is a congenital anomaly causing instability that extends beyond the atlantoaxial joint or if anatomical anomalies preclude screw placement into the atlas (Table 5).33 For cases in which placement of a C1 lateral mass screw is difficult, recently described procedures such as open, posterior-only, and instrumented reduction of a fixed C1–2 subluxation using occipital and C2/C3 fixation as reported by Meals et al provide surgeons more options.84
Table 5. Summary of posterior surgical techniques.
| Method | Stability | Complications | Surgical procedure |
|---|---|---|---|
| Transarticular screw fixation with sublaminar wiring | Very high fusion rates, up to 100%, due to direct fusion and stability | Neurologic damage can occur due to wire loosening, which has been reported in up to 50% of patients (Matsumoto et al 200595) | Transarticular screw fixation placement risks damage to vertebral artery, hypoglossal nerve; most difficult posterior procedure. |
| One of the gold standard treatments | Procedure risks damage to vertebral artery | Articular screw placement requires steep angle and joint exposure that can cause C2–C3 instability | |
| Transarticular screw fixation with C1 hook | Added stability compared with transarticular screw fixation alone, three-point fixation | Minimizes risk of neurologic damage (no wire) and subaxial instability (from dissection for wire insertion) | Fluoroscopic imaging required for proper placement of screws to avoid complications |
| Transarticular screw fixation with morselized autograft | Less stable than other transarticular screw fixation constructs | Minimizes risk of neurologic damage (no wire) | Wiring risks neurologic damage, and tissue dissection for wiring can cause weakness or longer healing process |
| Sufficient biomechanical stability | Instrumentation breakage has been reported, maybe due to screw | C1 hook or autograft obviates risk of tissue dissection | |
| C1L-C2PSF | Best overall stability; more stable than intact spine on axial rotation, lateral bending, and AP translation; less stable on flexion/extension | No complications reported in main clinical series of this procedure | Extension to occiput or subaxially is simple if necessary |
| C1L is compatible with most anatomical variations, imaging unnecessary | |||
| C2P pedicle variations make placement challenging; ∼20% of patients have insufficient pedicles for placement | |||
| Intraoperative reduction is possible | |||
| C1L-C2LSF | Not as stiff as transarticular screw fixation and C1L-C2PSF, especially on lateral bending | Early hardware failure | Weaker in extension to occiput than C1L-C2PSF construct |
| Less stable than C1L-C2PSF on axial rotation as well | Relatively safe regarding neurovascular injury, probably safest of the techniques | C1L is compatible with most anatomical variations; intraoperative imaging unnecessary | |
| Should be reserved for when anatomy restricts to this construct (Finn et al 200863) | C2L key structures can be visualized during procedure, less challenging | ||
| Technically less complicated procedure, but less stability |
Abbreviations: AP, anteroposterior; C1L, C1 lateral mass screw; C1L-C2PSF, C1 lateral mass screw and C2 pedicle screw fixation; C2L, C2 lateral mass screw; C1L-C2LSF, C1 lateral mass screw and C2 laminar screw fixation; C2P, C2 pedicle screw.
Historical Methods
Some surgical procedures that have been used in the past are highlighted here as historical notes and in comparison with contemporary procedures. The earliest surgical treatments for atlantoaxial dislocation used the Gallie or Brooks methods of wiring and bone grafting to fuse and stabilize the atlantoaxial joint.85 This practice has fallen out of favor because posterior wiring requires external immobilization (bracing) of the head and neck postoperatively and longer hospitalizations and has a nonunion rate of up to 30%.12 86 87 88 Sublaminar wiring has also been implicated as a cause of neural injury and disruption of ligamentous tissue that supports the spinal column.13 Posterior wiring may still be used for secondary fixation with transarticular screws in certain salvage procedures,89 or in cases with highly abnormal anatomy.
The Magerl technique, or C1–C2 transarticular screw fixation with posterior wiring, was first described in 1986 and became popular for cervical fixations including treatment of atlantoaxial dislocation because of its superior biomechanical strength and high fusion rates compared with posterior wiring,12 with fusion rates as high as 100% reported.90 91 92 This technique is successful because it provides immediate and direct fixation at the atlantoaxial joint. A midline incision is made to expose the posterior arch of C1 and lamina of C2.90 91 The screw is positioned anteriorly through the C2 pars, across the C1–C2 joint, and into the anterior aspect of the lateral mass of the atlas. In 1995, McGuire and Harkey introduced a modification of this technique to minimize tissue dissection in which a smaller midline incision is supplemented with two bilateral 1-cm caudal percutaneous incisions ∼2 cm lateral to the T1 spinous process.90 93 94 Once the C1–C2 joint is positioned and adequately reduced and the screws are placed, a bone graft is placed between C1 and C2 and wiring goes around the posterior arches to resist torsional and flexion forces.91 However, one study found that up to 50% of the wires were loosened after using the Magerl technique with a 95% fusion rate after a mean follow-up of 45 months,95 suggesting that posterior wiring is not required for successful fusion. Loosening of posterior wiring can violate the spinal cord and cause neurologic deficits.95
Recently, a modified Magerl technique that uses transarticular screw fixation with morselized autograft without posterior wiring has been described.54 Although this technique has less biomechanical strength than the Magerl technique, the authors reported that patients maintained a high fusion rate and avoided the risk of neurologic complications and loosening of cables associated with posterior wiring.54 Similarly, the Magerl technique has recently been used in combination with a transarticular screw fixation with C1 hook fixation for reducible atlantoaxial dislocation.13 96 97 With this method, transarticular screws are placed through the C2 pars and connected ipsilaterally with a rod to a hook grasping the posterior arch of C1. Bone graft is placed in between the C1 posterior arch and C2 lamina. This modified technique is easier and less invasive than sublaminar wiring because the posterior arch of C1 does not need to be exposed.13 Additionally, this three-point fixation provides high biomechanical stability while also preserving the ligamentous tissue between C2 and C3. However, ∼20% of patients requiring atlantoaxial fusion have anatomical variations that would interfere with safe placement of transarticular screws and must undergo a different fusion technique.88
The C1 lateral mass screw and C2 pedicle screw fixation (C1L-C2PSF) utilizes a C1 lateral mass screw technique in combination with a C2 pedicle screw fixation connected by rods to stabilize the atlantoaxial joint, although certain centers prefer plates connecting the fixation points.88 98 99 The technique enables extension to the occiput or subaxially if needed, and screw placement is more precise.89 100 Additionally, it allows for intraoperative reduction after screw fixation.88 C1 lateral mass screw placement has an advantage over the Magerl technique because it is compatible with most anatomical variations and does not require posterior wiring.89 101 The trajectory and placement of the C1 lateral mass screws is guided mostly by anatomical landmarks and does not require fluoroscopic imaging as does the Magerl technique.88 Additionally, C1L-C2PSF permits individual placement of screws in C1 and C2 to allow direct intraoperative manipulation for corrective alignment of the head and reduction of the dislocation.88 89 Neural complications associated with posterior wiring of the Gallie and Magerl techniques are mostly eliminated because sublaminar wiring is not required for C1L-C2PSF.88 Although longer fusion is required due to the involvement of levels adjacent to the atlantoaxial dislocation, this technique can also be applied for patients with an underlying rheumatic or ligamental cause for their atlantoaxial dislocation.88 In up to 20% of patients, the pedicles of C2 are too narrow for pedicle screws to be placed, and overall great care must be taken in pedicle screw placement. Additionally, the close proximity of the vertebral artery laterally, the spinal cord medially, and nerve roots vertically put patients at high risk for neurovascular complications.102 Yeom et al compared the risk of vertebral artery injury by C1–C2 transarticular screw versus C2 pedicle screw and found that the two techniques did not differ in risk of vertebral artery injury but recommended the use of pedicle screw over transarticular screw in cases of high-riding vertebral artery.41
Alternatively, the C1 lateral mass screw and C2 laminar screw fixation (C1L-C2LSF) technique was described in 2004 by using a crossed screw approach through the C2 lamina. This technique minimizes the risk of vertebral artery injury compared with transarticular screw fixation and C1L-C2PSF and allows direct visualization of the lamina to guide screw placement intraoperatively.8 20 37 Because there is no need for intraoperative fluoroscopy, the C1L-C2LSF procedure minimizes radiation exposure and reduces intraoperative time.103 It appears to be the safest of all available constructs with regards to vertebral artery injury. However, the biomechanical strength is similar to that of the transarticular screw fixation and C1L-C2PSF construct, but it cannot resist lateral bending as well.63 103 104 Additionally, there is a high incidence of early hardware failure with this technique.41
A 2008 report compared the three most commonly used constructs for atlantoaxial dislocation fixation (transarticular screw fixation, C1L-C2PSF, C1L-C2LSF), determining that both transarticular screw fixation and C1L-C2PSF showed greater stability, relative to C1L-C2LSF, with no significant biomechanical differences between these two constructs.63 Thus, the two are interchangeable depending on the opinion of the surgeon and the anatomy of the patient. A detailed biomechanical analysis of the C1L-C2PSF versus C1L-C2LSF techniques across four domains of motion (anteroposterior translation, lateral bending, axial rotation, and flexion/extension) revealed that the C1L-C2PSF is a structurally superior construct because it is stiffer in lateral bending and axial rotation when compared with C1L-C2LSF.105 Both of these constructs were found to be stronger than an intact spine. However, the C1L-C2LSF was only stronger in anteroposterior translation and lateral bending, whereas the C1L-C2PSF construct also resisted axial rotation better.105 C2 laminar screws have also been demonstrated to be weaker in occipitocervical construct extensions.
Conclusion
Atlantoaxial dislocation is a rare but dangerous condition that affects particular patient populations disproportionately. A variety of etiologies contributes to atlantoaxial dislocation, and the underlying causes or predisposing factors must be taken into consideration to maximize timely and effective treatment. The recent Wang classification system offers a practical and clinically proven means to effectively diagnose and treat atlantoaxial dislocation. Several anterior and posterior surgical techniques are suitable for atlantoaxial fusion. Each technique has its own indications, contraindications, risks, and technical difficulty. Future prospective clinical trials are necessary to more adequately determine which surgical technique is optimal based for respective clinical presentations.
Footnotes
Disclosures The authors have received no sources of any financial support and no personal assistance for the work being published. The authors of this manuscript have no conflicts of interest.
References
- 1.Subin B, Liu J F, Marshall G J, Huang H Y, Ou J H, Xu G Z. Transoral anterior decompression and fusion of chronic irreducible atlantoaxial dislocation with spinal cord compression. Spine (Phila Pa 1976) 1995;20(11):1233–1240. doi: 10.1097/00007632-199506000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Wheeless C R Atlantoaxial subluxation Available at: www.wheelessonline.com/ortho/atlantoaxial_subluxation. Accessed December 22, 2011
- 3.Wasserman B R, Moskovich R, Razi A E. Rheumatoid arthritis of the cervical spine—clinical considerations. Bull NYU Hosp Jt Dis. 2011;69(2):136–148. [PubMed] [Google Scholar]
- 4.Klimo P Jr, Rao G, Brockmeyer D. Congenital anomalies of the cervical spine. Neurosurg Clin N Am. 2007;18(3):463–478. doi: 10.1016/j.nec.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Tulsi R S. Some specific anatomical features of the atlas and axis: dens, epitransverse process and articular facets. Aust N Z J Surg. 1978;48(5):570–574. doi: 10.1111/j.1445-2197.1978.tb00049.x. [DOI] [PubMed] [Google Scholar]
- 6.Tubbs R S, Hallock J D, Radcliff V. et al. Ligaments of the craniocervical junction. J Neurosurg Spine. 2011;14(6):697–709. doi: 10.3171/2011.1.SPINE10612. [DOI] [PubMed] [Google Scholar]
- 7.Dvorak J, Schneider E, Saldinger P, Rahn B. Biomechanics of the craniocervical region: the alar and transverse ligaments. J Orthop Res. 1988;6(3):452–461. doi: 10.1002/jor.1100060317. [DOI] [PubMed] [Google Scholar]
- 8.Venkatesan M, Bhatt R, Newey M L. Traumatic atlantoaxial rotatory subluxation (TAARS) in adults: a report of two cases and literature review. Injury. 2012;43(7):1212–1215. doi: 10.1016/j.injury.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 9.Wong D A, Mack R P, Craigmile T K. Traumatic atlantoaxial dislocation without fracture of the odontoid. Spine (Phila Pa 1976) 1991;16(5):587–589. doi: 10.1097/00007632-199105000-00021. [DOI] [PubMed] [Google Scholar]
- 10.Grauer J N, Shafi B, Hilibrand A S. et al. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J. 2005;5(2):123–129. doi: 10.1016/j.spinee.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 11.Guiot B Fessler R G Complex atlantoaxial fractures J Neurosurg 199991 (2, Suppl):139–143. [DOI] [PubMed] [Google Scholar]
- 12.Guo X, Ni B, Zhao W. et al. Biomechanical assessment of bilateral C1 laminar hook and C1-2 transarticular screws and bone graft for atlantoaxial instability. J Spinal Disord Tech. 2009;22(8):578–585. doi: 10.1097/BSD.0b013e31818da3fe. [DOI] [PubMed] [Google Scholar]
- 13.Ni B, Zhou F, Xie N. et al. Transarticular screw and C1 hook fixation for os odontoideum with atlantoaxial dislocation. World Neurosurg. 2011;75(3–4):540–546. doi: 10.1016/j.wneu.2010.07.021. [DOI] [PubMed] [Google Scholar]
- 14.Salunke P, Sharma M, Sodhi H B, Mukherjee K K, Khandelwal N K. Congenital atlantoaxial dislocation: a dynamic process and role of facets in irreducibility. J Neurosurg Spine. 2011;15(6):678–685. doi: 10.3171/2011.7.SPINE1152. [DOI] [PubMed] [Google Scholar]
- 15.Menezes A H, VanGilder J C, Graf C J, McDonnell D E. Craniocervical abnormalities. A comprehensive surgical approach. J Neurosurg. 1980;53(4):444–455. doi: 10.3171/jns.1980.53.4.0444. [DOI] [PubMed] [Google Scholar]
- 16.Song D, Maher C O. Spinal disorders associated with skeletal dysplasias and syndromes. Neurosurg Clin N Am. 2007;18(3):499–514. doi: 10.1016/j.nec.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Curtis B H, Blank S, Fisher R L. Atlantoxial dislocation in Down's syndrome. Report of two patients requiring surgical correction. JAMA. 1968;205(6):464–465. doi: 10.1001/jama.205.6.464. [DOI] [PubMed] [Google Scholar]
- 18.Martel W, Tishler J M. Observations on the spine in mongoloidism. Am J Roentgenol Radium Ther Nucl Med. 1966;97(3):630–638. doi: 10.2214/ajr.97.3.630. [DOI] [PubMed] [Google Scholar]
- 19.Hedequist D, Bekelis K, Emans J, Proctor M R. Single stage reduction and stabilization of basilar invagination after failed prior fusion surgery in children with Down's syndrome. Spine (Phila Pa 1976) 2010;35(4):E128–E133. doi: 10.1097/BRS.0b013e3181bad0c2. [DOI] [PubMed] [Google Scholar]
- 20.Pueschel S M, Scola F H. Atlantoaxial instability in individuals with Down syndrome: epidemiologic, radiographic, and clinical studies. Pediatrics. 1987;80(4):555–560. [PubMed] [Google Scholar]
- 21.Healey D, Letts M, Jarvis J G. Cervical spine instability in children with Goldenhar's syndrome. Can J Surg. 2002;45(5):341–344. [PMC free article] [PubMed] [Google Scholar]
- 22.Miyoshi K, Nakamura K, Haga N, Mikami Y. Surgical treatment for atlantoaxial subluxation with myelopathy in spondyloepiphyseal dysplasia congenita. Spine (Phila Pa 1976) 2004;29(21):E488–E491. doi: 10.1097/01.brs.0000143621.37688.f3. [DOI] [PubMed] [Google Scholar]
- 23.Takeda E, Hashimoto T, Tayama M. et al. Diagnosis of atlantoaxial subluxation in Morquio's syndrome and spondyloepiphyseal dysplasia congenita. Acta Paediatr Jpn. 1991;33(5):633–638. doi: 10.1111/j.1442-200x.1991.tb01877.x. [DOI] [PubMed] [Google Scholar]
- 24.Stevens J M, Kendall B E, Crockard H A, Ransford A. The odontoid process in Morquio-Brailsford's disease. The effects of occipitocervical fusion. J Bone Joint Surg Br. 1991;73(5):851–858. doi: 10.1302/0301-620X.73B5.1910048. [DOI] [PubMed] [Google Scholar]
- 25.Wang S, Wang C, Yan M, Zhou H, Dang G. Novel surgical classification and treatment strategy for atlantoaxial dislocations. Spine (Phila Pa 1976) 2013;38(21):E1348–E1356. doi: 10.1097/BRS.0b013e3182a1e5e4. [DOI] [PubMed] [Google Scholar]
- 26.Salunke P Behari S Kirankumar M V Sharma M S Jaiswal A K Jain V K Pediatric congenital atlantoaxial dislocation: differences between the irreducible and reducible varieties J Neurosurg 2006104(2, Suppl):115–122. [DOI] [PubMed] [Google Scholar]
- 27.Bouchaud-Chabot A, Lioté F. Cervical spine involvement in rheumatoid arthritis. A review. Joint Bone Spine. 2002;69(2):141–154. doi: 10.1016/s1297-319x(02)00361-5. [DOI] [PubMed] [Google Scholar]
- 28.Neva M H, Kaarela K, Kauppi M. Prevalence of radiological changes in the cervical spine—a cross sectional study after 20 years from presentation of rheumatoid arthritis. J Rheumatol. 2000;27(1):90–93. [PubMed] [Google Scholar]
- 29.Pellicci P M, Ranawat C S, Tsairis P, Bryan W J. A prospective study of the progression of rheumatoid arthritis of the cervical spine. J Bone Joint Surg Am. 1981;63(3):342–350. [PubMed] [Google Scholar]
- 30.Kim D H, Hilibrand A S. Rheumatoid arthritis in the cervical spine. J Am Acad Orthop Surg. 2005;13(7):463–474. doi: 10.5435/00124635-200511000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Halla J T, Hardin J G, Vitek J, Alarcón G S. Involvement of the cervical spine in rheumatoid arthritis. Arthritis Rheum. 1989;32(5):652–659. doi: 10.1002/anr.1780320522. [DOI] [PubMed] [Google Scholar]
- 32.Neva M H, Kauppi M J, Kautiainen H. et al. Combination drug therapy retards the development of rheumatoid atlantoaxial subluxations. Arthritis Rheum. 2000;43(11):2397–2401. doi: 10.1002/1529-0131(200011)43:11<2397::AID-ANR4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 33.Passias P G, Wang S, Kozanek M, Wang S, Wang C. Relationship between the alignment of the occipitoaxial and subaxial cervical spine in patients with congenital atlantoxial dislocations. J Spinal Disord Tech. 2013;26(1):15–21. doi: 10.1097/BSD.0b013e31823097f9. [DOI] [PubMed] [Google Scholar]
- 34.Matsunaga S, Onishi T, Sakou T. Significance of occipitoaxial angle in subaxial lesion after occipitocervical fusion. Spine (Phila Pa 1976) 2001;26(2):161–165. doi: 10.1097/00007632-200101150-00010. [DOI] [PubMed] [Google Scholar]
- 35.Yoshimoto H, Ito M, Abumi K. et al. A retrospective radiographic analysis of subaxial sagittal alignment after posterior C1-C2 fusion. Spine (Phila Pa 1976) 2004;29(2):175–181. doi: 10.1097/01.BRS.0000107225.97653.CA. [DOI] [PubMed] [Google Scholar]
- 36.Yin Y-H, Qiao G-Y, Yu X-G, Tong H-Y, Zhang Y-Z. Posterior realignment of irreducible atlantoaxial dislocation with C1-C2 screw and rod system: a technique of direct reduction and fixation. Spine J. 2013;13(12):1864–1871. doi: 10.1016/j.spinee.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 37.Sobolewski B A, Mittiga M R, Reed J L. Atlantoaxial rotary subluxation after minor trauma. Pediatr Emerg Care. 2008;24(12):852–856. doi: 10.1097/PEC.0b013e31818ea0d3. [DOI] [PubMed] [Google Scholar]
- 38.Wadia N H. Myelopathy complicating congenital atlanto-axial dislocation. (A study of 28 cases) Brain. 1967;90(2):449–472. doi: 10.1093/brain/90.2.449. [DOI] [PubMed] [Google Scholar]
- 39.Panda S, Ravishankar S, Nagaraja D. Bilateral vertebral artery dissection caused by atlantoaxial dislocation. J Assoc Physicians India. 2010;58:187–189. [PubMed] [Google Scholar]
- 40.Reddy K R, Rao G S, Devi B I, Prasad P V, Ramesh V J. Pulmonary function after surgery for congenital atlantoaxial dislocation: a comparison with surgery for compressive cervical myelopathy and craniotomy. J Neurosurg Anesthesiol. 2009;21(3):196–201. doi: 10.1097/ANA.0b013e31819f1cce. [DOI] [PubMed] [Google Scholar]
- 41.Yeom J S, Buchowski J M, Kim H J, Chang B S, Lee C K, Riew K D. Risk of vertebral artery injury: comparison between C1-C2 transarticular and C2 pedicle screws. Spine J. 2013;13(7):775–785. doi: 10.1016/j.spinee.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 42.Bhagwati S N, Deopujari C E, Parulekar G D. Trauma in congenital atlanto-axial dislocation. Childs Nerv Syst. 1998;14(12):719–721. doi: 10.1007/s003810050304. [DOI] [PubMed] [Google Scholar]
- 43.Kaito T, Hosono N, Ohshima S. et al. Effect of biological agents on cervical spine lesions in rheumatoid arthritis. Spine (Phila Pa 1976) 2012;37(20):1742–1746. doi: 10.1097/BRS.0b013e318256b584. [DOI] [PubMed] [Google Scholar]
- 44.Kanayama Y, Kojima T, Hirano Y. et al. Radiographic progression of cervical lesions in patients with rheumatoid arthritis receiving infliximab treatment. Mod Rheumatol. 2010;20(3):273–279. doi: 10.1007/s10165-010-0276-8. [DOI] [PubMed] [Google Scholar]
- 45.Fielding J W, Hawkins R J, Ratzan S A. Spine fusion for atlanto-axial instability. J Bone Joint Surg Am. 1976;58(3):400–407. [PubMed] [Google Scholar]
- 46.Greenberg A D. Atlanto-axial dislocations. Brain. 1968;91(4):655–684. doi: 10.1093/brain/91.4.655. [DOI] [PubMed] [Google Scholar]
- 47.Yurube T, Sumi M, Nishida K. et al. Incidence and aggravation of cervical spine instabilities in rheumatoid arthritis: a prospective minimum 5-year follow-up study of patients initially without cervical involvement. Spine (Phila Pa 1976) 2012;37(26):2136–2144. doi: 10.1097/BRS.0b013e31826def1c. [DOI] [PubMed] [Google Scholar]
- 48.Boden S D, Dodge L D, Bohlman H H, Rechtine G R. Rheumatoid arthritis of the cervical spine. A long-term analysis with predictors of paralysis and recovery. J Bone Joint Surg Am. 1993;75(9):1282–1297. doi: 10.2106/00004623-199309000-00004. [DOI] [PubMed] [Google Scholar]
- 49.Mower W R Hoffman J R Pollack C V Jr Zucker M I Browne B J Wolfson A B; NEXUS Group. Use of plain radiography to screen for cervical spine injuries Ann Emerg Med 20013811–7. [DOI] [PubMed] [Google Scholar]
- 50.Bailitz J, Starr F, Beecroft M. et al. CT should replace three-view radiographs as the initial screening test in patients at high, moderate, and low risk for blunt cervical spine injury: a prospective comparison. J Trauma. 2009;66(6):1605–1609. doi: 10.1097/TA.0b013e3181a5b0cc. [DOI] [PubMed] [Google Scholar]
- 51.Wang S W A novel surgical classification and treatment strategy for atlantoaxial dislocations based on 1106 cases over 14 years Paper presented at: Cervical Spine Research Society; December 7, 2012; Chicago, IL [DOI] [PubMed]
- 52.Fielding J W, Hawkins R J. Atlanto-axial rotatory fixation. (Fixed rotatory subluxation of the atlanto-axial joint) J Bone Joint Surg Am. 1977;59(1):37–44. [PubMed] [Google Scholar]
- 53.Nordt J C, Stauffer E S. Sequelae of atlantoaxial stabilization in two patients with Down's syndrome. Spine (Phila Pa 1976) 1981;6(5):437–440. doi: 10.1097/00007632-198109000-00003. [DOI] [PubMed] [Google Scholar]
- 54.Wang C, Yan M, Zhou H, Wang S, Dang G. Atlantoaxial transarticular screw fixation with morselized autograft and without additional internal fixation: technical description and report of 57 cases. Spine (Phila Pa 1976) 2007;32(6):643–646. doi: 10.1097/01.brs.0000257539.75693.cc. [DOI] [PubMed] [Google Scholar]
- 55.Wang C, Yan M, Zhou H T, Wang S L, Dang G T. Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine (Phila Pa 1976) 2006;31(11):E306–E313. doi: 10.1097/01.brs.0000217686.80327.e4. [DOI] [PubMed] [Google Scholar]
- 56.Zhang K, Xu J, Wang Q. et al. Treatment of dens fractures with posterior atlantoaxial dislocation with transoral atlantoaxial reduction plate surgery: case report and introduction of a novel treatment option. Spine (Phila Pa 1976) 2012;37(7):E451–E455. doi: 10.1097/BRS.0b013e31823735f5. [DOI] [PubMed] [Google Scholar]
- 57.Papadopoulos S M, Dickman C A, Sonntag V KH. Atlantoaxial stabilization in rheumatoid arthritis. J Neurosurg. 1991;74(1):1–7. doi: 10.3171/jns.1991.74.1.0001. [DOI] [PubMed] [Google Scholar]
- 58.Devin C J, Kang J D. Vertebral artery injury in cervical spine surgery. Instr Course Lect. 2009;58:717–728. [PubMed] [Google Scholar]
- 59.Koval K J, Zuckerman J D, Rockwood C A. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. Handbook of Fractures. [Google Scholar]
- 60.Chechik O, Wientroub S, Danino B, Lebel D E, Ovadia D. Successful conservative treatment for neglected rotatory atlantoaxial dislocation. J Pediatr Orthop. 2013;33(4):389–392. doi: 10.1097/BPO.0b013e318279c68c. [DOI] [PubMed] [Google Scholar]
- 61.Cohen W I Current dilemmas in Down syndrome clinical care: celiac disease, thyroid disorders, and atlanto axial instability Paper presented at: American Journal of Medical Genetics Part C: Seminars in Medical Genetics; 2006 [DOI] [PubMed]
- 62.American Academy of Pediatrics . American Academy of Pediatrics. Committee on Sports Medicine. Atlantoaxial instability in Down syndrome. Pediatrics. 1984;74(1):152–154. [PubMed] [Google Scholar]
- 63.Finn M A, Fassett D R, Mccall T D, Clark R, Dailey A T, Brodke D S. The cervical end of an occipitocervical fusion: a biomechanical evaluation of 3 constructs. Laboratory investigation. J Neurosurg Spine. 2008;9(3):296–300. doi: 10.3171/SPI/2008/9/9/296. [DOI] [PubMed] [Google Scholar]
- 64.Behari S, Bhargava V, Nayak S. et al. Congenital reducible atlantoaxial dislocation: classification and surgical considerations. Acta Neurochir (Wien) 2002;144(11):1165–1177. doi: 10.1007/s00701-002-1009-3. [DOI] [PubMed] [Google Scholar]
- 65.Flynn J M, Wiesel S W. Philadelphia, PA: Lippincott Williams & Wilkins; 2010. Operative Techniques in Pediatric Orthopaedics. [Google Scholar]
- 66.Miyamoto H, Sumi M, Uno K. Outcome of surgery for rheumatoid cervical spine at one institute over three decades. Spine J. 2013;13(11):1477–1484. doi: 10.1016/j.spinee.2013.05.023. [DOI] [PubMed] [Google Scholar]
- 67.Tauchi R, Imagama S, Ito Z. et al. Surgical treatment for chronic atlantoaxial rotatory fixation in children. J Pediatr Orthop B. 2013;22(5):404–408. doi: 10.1097/BPB.0b013e3283633064. [DOI] [PubMed] [Google Scholar]
- 68.Dedlow E R, Siddiqi S, Fillipps D J, Kelly M N, Nackashi J A, Tuli S Y. Symptomatic atlantoaxial instability in an adolescent with trisomy 21 (Down's syndrome) Clin Pediatr (Phila) 2013;52(7):633–638. doi: 10.1177/0009922813482178. [DOI] [PubMed] [Google Scholar]
- 69.Arvin B Fournier-Gosselin M-P Fehlings M G Os odontoideum: etiology and surgical management Neurosurgery 201066(3, Suppl):22–31. [DOI] [PubMed] [Google Scholar]
- 70.Ogino H, Tada K, Okada K. et al. Canal diameter, anteroposterior compression ratio, and spondylotic myelopathy of the cervical spine. Spine (Phila Pa 1976) 1983;8(1):1–15. doi: 10.1097/00007632-198301000-00001. [DOI] [PubMed] [Google Scholar]
- 71.Tuite G F, Veres R, Crockard H A, Sell D. Pediatric transoral surgery: indications, complications, and long-term outcome. J Neurosurg. 1996;84(4):573–583. doi: 10.3171/jns.1996.84.4.0573. [DOI] [PubMed] [Google Scholar]
- 72.Jain V K, Behari S. Management of congenital atlanto-axial dislocation: some lessons learnt. Neurol India. 2002;50(4):386–397. [PubMed] [Google Scholar]
- 73.Di Lorenzo N. Craniocervical junction malformation treated by transoral approach. A survey of 25 cases with emphasis on postoperative instability and outcome. Acta Neurochir (Wien) 1992;118(3–4):112–116. doi: 10.1007/BF01401296. [DOI] [PubMed] [Google Scholar]
- 74.Mummaneni P V Haid R W Transoral odontoidectomy Neurosurgery 20055651045–1050., discussion 1045–1050 [PubMed] [Google Scholar]
- 75.Yadav Y, Shenoy R, Mukerji G, Sherekar S, Parihar V. Delhi, India: Byword Books; 2011. Endoscopic transoral excision of odontoid process in irreducible atlanto-axial dislocation; pp. 159–169. [Google Scholar]
- 76.Jain V K, Behari S, Banerji D, Bhargava V, Chhabra D K. Transoral decompression for craniovertebral osseous anomalies: perioperative management dilemmas. Neurol India. 1999;47(3):188–195. [PubMed] [Google Scholar]
- 77.Kassam A B Snyderman C Gardner P Carrau R Spiro R The expanded endonasal approach: a fully endoscopic transnasal approach and resection of the odontoid process: technical case report Neurosurgery 200557(1 Suppl):E213. [DOI] [PubMed] [Google Scholar]
- 78.Alfieri A Jho H-D Tschabitscher M Endoscopic endonasal approach to the ventral cranio-cervical junction: anatomical study Acta Neurochir (Wien) 20021443219–225., discussion 225 [DOI] [PubMed] [Google Scholar]
- 79.Lü G, Passias P G, Li G. et al. Endoscopically assisted anterior release and reduction through anterolateral retropharyngeal approach for fixed atlantoaxial dislocation. Spine (Phila Pa 1976) 2010;35(5):544–551. doi: 10.1097/BRS.0b013e3181bad101. [DOI] [PubMed] [Google Scholar]
- 80.Yin Q, Ai F, Zhang K. et al. Irreducible anterior atlantoaxial dislocation: one-stage treatment with a transoral atlantoaxial reduction plate fixation and fusion. Report of 5 cases and review of the literature. Spine (Phila Pa 1976) 2005;30(13):E375–E381. doi: 10.1097/01.brs.0000168374.84757.d5. [DOI] [PubMed] [Google Scholar]
- 81.Yin Q S, Ai F Z, Zhang K, Mai X H, Xia H, Wu Z H. Transoral atlantoaxial reduction plate internal fixation for the treatment of irreducible atlantoaxial dislocation: a 2- to 4-year follow-up. Orthop Surg. 2010;2(2):149–155. doi: 10.1111/j.1757-7861.2010.00077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang M Y C2 crossing laminar screws: cadaveric morphometric analysis Neurosurgery 200659(1, Suppl 1):ONS84–ONS88., discussion ONS84–ONS88 [DOI] [PubMed] [Google Scholar]
- 83.Padua M R, Yeom J S, Lee S Y. et al. Fluoroscopically guided anterior atlantoaxial transarticular screws: a feasibility and trajectory study using CT-based simulation software. Spine J. 2013;13(11):1455–1463. doi: 10.1016/j.spinee.2013.05.036. [DOI] [PubMed] [Google Scholar]
- 84.Meals C, Harrison R, Yu W, O'Brien J. Instrumented reduction of a fixed C1–2 subluxation using occipital and C2/C3 fixation: a case report. The International Journal of Spine Surgery. 2013;7(1):e20–e23. doi: 10.1016/j.ijsp.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Brooks A L, Jenkins E B. Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am. 1978;60(3):279–284. [PubMed] [Google Scholar]
- 86.Cassinelli E H, Lee M, Skalak A, Ahn N U, Wright N M. Anatomic considerations for the placement of C2 laminar screws. Spine (Phila Pa 1976) 2006;31(24):2767–2771. doi: 10.1097/01.brs.0000245869.85276.f4. [DOI] [PubMed] [Google Scholar]
- 87.Wright N M. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech. 2004;17(2):158–162. doi: 10.1097/00024720-200404000-00014. [DOI] [PubMed] [Google Scholar]
- 88.Harms J, Melcher R P. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 2001;26(22):2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 89.De Iure F, Donthineni R, Boriani S. Outcomes of C1 and C2 posterior screw fixation for upper cervical spine fusion. Eur Spine J. 2009;18 01:2–6. doi: 10.1007/s00586-009-0981-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Haid R W Jr Subach B R McLaughlin M R Rodts G E Jr Wahlig J B Jr C1-C2 transarticular screw fixation for atlantoaxial instability: a 6-year experience Neurosurgery 200149165–68., discussion 69–70 [DOI] [PubMed] [Google Scholar]
- 91.Finn M A Apfelbaum R I Atlantoaxial transarticular screw fixation: update on technique and outcomes in 269 patients Neurosurgery 201066(3, Suppl):184–192. [DOI] [PubMed] [Google Scholar]
- 92.Platzer P, Vécsei V, Thalhammer G, Oberleitner G, Schurz M, Gaebler C. Posterior atlanto-axial arthrodesis for fixation of odontoid nonunions. Spine (Phila Pa 1976) 2008;33(6):624–630. doi: 10.1097/BRS.0b013e318166dfb8. [DOI] [PubMed] [Google Scholar]
- 93.Haid R W Jr. C1-C2 transarticular screw fixation: technical aspects. Neurosurgery. 2001;49(1):71–74. doi: 10.1097/00006123-200107000-00011. [DOI] [PubMed] [Google Scholar]
- 94.McGuire R A Jr, Harkey H L. Modification of technique and results of atlantoaxial transfacet stabilization. Orthopedics. 1995;18(10):1029–1032. doi: 10.3928/0147-7447-19951001-12. [DOI] [PubMed] [Google Scholar]
- 95.Matsumoto M, Chiba K, Nakamura M, Ogawa Y, Toyama Y, Ogawa J. Impact of interlaminar graft materials on the fusion status in atlantoaxial transarticular screw fixation. J Neurosurg Spine. 2005;2(1):23–26. doi: 10.3171/spi.2005.2.1.0023. [DOI] [PubMed] [Google Scholar]
- 96.Ren Z W, Ni B, Song H T. et al. [A finite element investigation of bilateral atlantoaxial trans-articular screws and atlas laminar hooks instrumentation] Zhonghua Wai Ke Za Zhi. 2008;46(9):657–660. [PubMed] [Google Scholar]
- 97.Ni B, Guo X, Xie N. et al. Bilateral atlantoaxial transarticular screws and atlas laminar hooks fixation for pediatric atlantoaxial instability. Spine (Phila Pa 1976) 2010;35(24):E1367–E1372. doi: 10.1097/BRS.0b013e3181e8ee87. [DOI] [PubMed] [Google Scholar]
- 98.Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 1994;129(1–2):47–53. doi: 10.1007/BF01400872. [DOI] [PubMed] [Google Scholar]
- 99.Abumi K, Itoh H, Taneichi H, Kaneda K. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord. 1994;7(1):19–28. doi: 10.1097/00002517-199407010-00003. [DOI] [PubMed] [Google Scholar]
- 100.Deen H G, Birch B D, Wharen R E, Reimer R. Lateral mass screw-rod fixation of the cervical spine: a prospective clinical series with 1-year follow-up. Spine J. 2003;3(6):489–495. [PubMed] [Google Scholar]
- 101.Bransford R J, Lee M J, Reis A. Posterior fixation of the upper cervical spine: contemporary techniques. J Am Acad Orthop Surg. 2011;19(2):63–71. doi: 10.5435/00124635-201102000-00001. [DOI] [PubMed] [Google Scholar]
- 102.Nakanishi K, Tanaka M, Sugimoto Y. et al. Application of laminar screws to posterior fusion of cervical spine: measurement of the cervical vertebral arch diameter with a navigation system. Spine (Phila Pa 1976) 2008;33(6):620–623. doi: 10.1097/BRS.0b013e318166aa76. [DOI] [PubMed] [Google Scholar]
- 103.Wang M Y Cervical crossing laminar screws: early clinical results and complications Neurosurgery 200761(5, Suppl 2):311–315., discussion 315–316 [DOI] [PubMed] [Google Scholar]
- 104.Lapsiwala S B, Anderson P A, Oza A, Resnick D K. Biomechanical comparison of four C1 to C2 rigid fixative techniques: anterior transarticular, posterior transarticular, C1 to C2 pedicle, and C1 to C2 intralaminar screws. Neurosurgery. 2006;58(3):516–521, discussion 516–521. doi: 10.1227/01.NEU.0000197222.05299.31. [DOI] [PubMed] [Google Scholar]
- 105.Claybrooks R, Kayanja M, Milks R, Benzel E. Atlantoaxial fusion: a biomechanical analysis of two C1-C2 fusion techniques. Spine J. 2007;7(6):682–688. doi: 10.1016/j.spinee.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 106.Abelin-Genevois K Idjerouidene A Roussouly P Vital J M Garin C Cervical spine alignment in the pediatric population: a radiographic normative study of 150 asymptomatic patients Eur Spine J 2014; January 7 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 107.Nojiri K Matsumoto M Chiba K et al. Relationship between alignment of upper and lower cervical spine in asymptomatic individuals J Neurosurg 200399(1, Suppl):80–83. [DOI] [PubMed] [Google Scholar]
- 108.Dickman C A, Locantro J, Fessler R G. The influence of transoral odontoid resection on stability of the craniovertebral junction. J Neurosurg. 1992;77(4):525–530. doi: 10.3171/jns.1992.77.4.0525. [DOI] [PubMed] [Google Scholar]


