Abstract
The number of individuals with dementia is expected to increase dramatically over the next 20 years. Given the complicated clinical, sociobehavioral, and caregiving skills that are needed to comprehensively assess and manage individuals with dementia, the gold standard of care requires involvement of an interprofessional team. This systematic review examined 4,023 abstracts, finding 18 papers from 16 studies where an interprofessional dissemination program was performed. Most studies found some improvement in clinician knowledge or confidence, or patient outcomes, though methods and patient and clinician populations were disparate. While a significant evidence base for assessing and managing individuals with dementia has been developed, few studies have examined how to disseminate this research, and even fewer in an interprofessional manner. These findings suggest that greater emphasis needs to be placed on disseminating existing evidence-based care and ensuring that programs are interprofessional in nature so that excellent, patient-centered care is provided.
Introduction
It is estimated that over 7 million people in the United States currently live with dementia due to Alzheimer’s disease (AD), cerebrovascular disease, Lewy body disease and related disorders (Sloane, et al., 2002). The prevalence of dementia in those over the age of 71 has been found to be 13.9% (Plassman, et al., 2007). While the number of people with dementia is expected to increase dramatically as the population increases significantly with the aging of the baby boom generation, the infrastructure and clinical skills necessary to assess and manage dementia are considerably underdeveloped. Currently, clinicians who routinely see older adults have difficulty diagnosing dementia (Knopman, Donohue, & Gutterman, 2000; Valcour, Masaki, Curb, & Blanchette, 2000), distinguishing between dementia and delirium (Inouye, Foreman, Mion, Katz, & Cooney, 2001), and managing its sequelae including both the emergence of behavior and mood problems (e.g. agitation, depression) and the development and progression of somatic symptoms (i.e. pain) (Rhodes-Kropf, Cheng, Castillo, & Fulton, 2011).
Geriatric patients, particularly those with dementia, benefit from the multiple perspectives and teamwork provided by interprofessional team-based care (Boult, et al., 2009). Interprofessional team-based care is defined as care delivered by a small group of health professionals from different disciplines who share responsibility of caring for a group of patients (Interprofessional Education Collaborative, 2011). While it is important to implement interprofessional care teams based on evidence-based practice to provide care for patients with dementia, little work has been completed showing exactly how interprofessional teams should be formed, educated, and implemented in various settings. This review of the literature therefore examines patient and provider outcomes related to interprofessional education in dementia with the goals of: 1) examining current strengths and weaknesses of dissemination science in this area; 2) examining how to best implement effective, evidence-based interprofessional care for individuals with dementia and improve patient-centered outcomes; 3) making recommendations for researchers, funders and policy makers regarding needs for future research in this area.
Methods
Search Strategy
We performed a systematic literature review using MEDLINE, CINAHL, PsycInfo, and EMBASE following the Cochrane Handbook for Systematic Reviews of Interventions (“Cochrane Handbook for Systematic Review of Interventions Version 5.1.0,” March 2011) The search was performed on literature from January 1990 through June 2012. The search was limited to articles in peer-reviewed journals where the primary language was English. In our search strategy, we used the dementia subject heading and terms involving staff development and interprofessional, interdisciplinary and multidisciplinary education or dissemination. We also searched for education or dissemination involving individual professions such as nurse, physical therapy, and physician related to dementia. In addition, we found that many interventions that involved education or dissemination were not labeled as such so the search was broadened to include general intervention studies in dementia.
Selection Criteria
Once the searches were performed, abstracts were reviewed. If the database did not have an abstract, the entire article was downloaded and then the abstract reviewed. Articles were included in the final review if they included: 1) a dementia educational/dissemination intervention 2) more than one professional licensed discipline, and 3) either patient outcomes or health professional knowledge or behavioral outcomes. Studies had to have one of the following designs to be included in the study: controlled trial pre-post trial, interrupted time series trial. Registered nurses and licensed vocational (enrolled) nurses were considered as part of the same discipline for purposes of determining if a paper involved multiple disciplines. Studies were excluded if they focused on students, non-licensed personnel (e.g. nursing assistants, paid caregivers in the home), or forms of dementia other than Alzheimer’s, Lewy body, vascular, mixed, or frontotemporal, as the above mentioned forms are the most predominant in older adults.
Data Abstraction, Classification, and Synthesis
We abstracted as available in each manuscript the following data: study design, disciplines involved, number of providers trained, type of education provided, interprofessional or multidisciplinary in nature, focus of education, changes in professional knowledge, professional behavior (process outcomes), number of patients studied, patient outcomes, level of knowledge retention over time. Studies were considered interprofessional if two or more professional discipline took part in an education intervention at the same time and multidisciplinary if multiple professions were trained but in separate educational interventions. All abstracts were first reviewed by the first author (AAB) and then concurrence was obtained through review by the second author (JEG). Consensus was reached on all included/excluded manuscripts.
Results
The search process identified 4023 total citations. Of those, 136 papers were downloaded for further examination (see Figure 1). Of these 136 articles, 18 articles from 16 studies met the criteria for inclusion. Of these 16 studies, the methods used for the study broke down as follows: 9 pre-post studies, 3 interrupted time series studies, 1 controlled trial, 1 randomized controlled trial, 2 cluster randomized controlled trials (see Table 1). Seven of the trials occurred in the nursing home setting, six in the community, and three in the hospital. Five of the studies involved two disciplines and the remaining 11 involved three or more disciplines.
Figure 1.
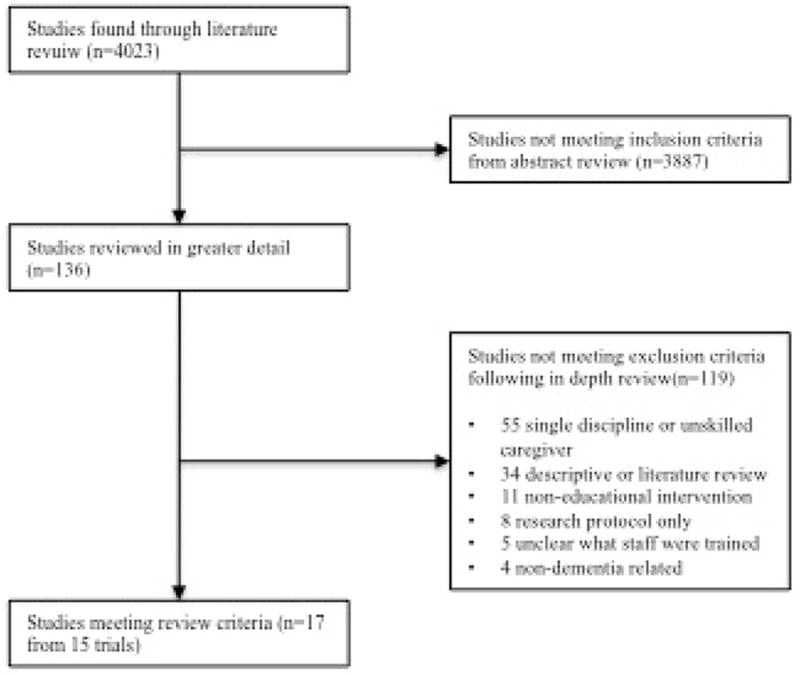
Process of Systematic Review Selection
Table 1.
Summary of Included Study Designs
| Article | Multi or Inter-Disciplinary | Study Design | Study Setting (Number of Sites) | Disciplines Involved (# providers receiving education) | Type of education provided/intervention | Focus of Education | Data Collection Method |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Arcand, 2009 | M | PP | NH (1) | P (N/A) N (N/A) | N: 45min didactic education | “Consciousness raising” of end of life care in dementia | Decedent family member interviews |
| P: 60min didactic education | |||||||
| Booklet for family of patients | |||||||
|
| |||||||
| Barton, 2006 | M | PP | NH (1) | P (N/A), N (N/A) | N: 8hrs over 3 months didactic | General dementia diagnosis, management and treatment | CR |
| P: Monthly Roundtables and didactic education, Algorithm for evaluation of CI, Guidelines for dx and management, specialist NP brought to pre-existing interdisciplinary care meeting | |||||||
|
| |||||||
| Beer, 2011 | I | RCT | NH (18) | P (27), Other (1072) | P: 7hrs didactic training | Communication, pain management, behavioral concerns, Depression, Dementia, Delirium, Effective communication, Personal care, Positive Values. | S |
| O (undefined): 13.5hrs didactic training | |||||||
| Staff Champions: 1 additional day on top of basic 13.5hr didactic program | |||||||
| Managers were also engaged. | |||||||
|
| |||||||
| Cherry, 2009 AND Cherry, 2004 | M | PP | Community (NA) | P (152), SW (2) | SW: trained to become Dementia Care Managers, received 24 hour intensive didactic session followed by 7 months of mentoring via case conferences. | Diagnose and manage dementia | CR, S |
| P: trained to diagnose and manage dementia, use of guidelines, how to screen patients didactic/interactive session, provider toolkit also provided, educational detailing by educator, checklist, volume of training not provided | |||||||
|
| |||||||
| Chodosh, 2006 AND Vickrey, 2006 | M | Cluster RCT | Community (16) | P (85), NP & PA (11), and SW (NA) | All: 100 minutes of education in 5 modules, Internet based care management software and communication system | Diagnose and manage dementia | CR, S |
|
| |||||||
| Chrzescijanski, 2007 | I | ITS | NH (4) | RN (31%), O (Therapy staff and LVN) (11%), DC (58%) | All: 40 minute video | Reduce dementia related regression | CR, S Prospective measurement of behavioral problems using the BAGS Aggression Scale |
|
| |||||||
| Downs, 2006 | I | Cluster RCT | Community clinics in Scotland (36) | P(N/A), N(N/A) | All: CD ROM OR decision support software placed in the practice electronic medical record, OR practice based workshops | Increase diagnosis and concordance with guidelines for treating dementia | CR |
|
| |||||||
| Ellis, 2010 | I | PP | Communities throughout Australia (NA) | 475 total health workers. N (77%), Aboriginal health workers (7%), O (15%) | All: Emergency mental health conditions in rural settings. Didactic, interactive 2 day workshop with workbook | Increase understanding and discerning between mental health conditions including dementia and delirium, and Improved assessment of psychotic symptoms | S |
|
| |||||||
| Gallagher,2011 | I | PP | Hospice (1) | N (12), SW (5), Chaplain (2), DC (5) | All: 60 minute didactic education session and providing hardware for performing music therapy for Alzheimer’s patients in hospice | Music therapy in dementia | S |
|
| |||||||
| Galvin, 2010 | I | PP | H (4) | N (238), T (57), O (91) | All: 5 didactic modules over 7 hours | Dementia recognition and management including medical overview, screening tools, communication, dementia friendly care, connecting the caregiver | S |
|
| |||||||
| McAiney, 2007 | I | PP | NH (439) | N(1026), SW (31), O (19) | All: Either 18 hr or 12 hr case based curriculum with homework assignments in between days. | Increase knowledge in assessing and managing physical and cognitive issues in aging. Training was to create a PRP | S |
| Over time, consultant provided for additional education and email/fax based consultation | |||||||
|
| |||||||
| Mcphail, 2009 | I | PP | H (1) | N (17), T (4), Pharm (2), SW (2), O (3) | All:10 1-hour weekly sessions | Managing dementia and its sequelae | S |
|
| |||||||
| Meuser, 2006 | I | ITS | Community (NA) | P (26), N or PA (17), T (61), SW or Psych (43) | All: 2 hour multidisciplinary didactic session | Driving assessment in dementia | S |
|
| |||||||
| Monette, 2008 | I | ITS | NH (1) | P &Pharm (6), N, (74), DC (123) | N: 1.5h didactic | Management of behavioral symptoms in dementia patients in nursing homes | S, CR, Prospective measurement of behavioral problems using the NHBPS |
| P and Pharm combined: 1.5h didactic | |||||||
| DC: 45m didactic | |||||||
| After education, pharmacists sent letters to physicians who had patients on a stable dose of antipsychotic medication for more than 3 months | |||||||
| Attendance at interdisciplinary team meetings was encouraged by researchers | |||||||
|
| |||||||
| Ray, 1993 | M | CT | NH (2) | P (NA), N (NA), DC (NA) | P: 45-60min didactic session and reference card provided | Management of behavioral symptoms | CR, Prospective measurement of behavioral problems using the NHBPS |
| N and DC: 1 hour in-service, | |||||||
| Follow up session 4 wks after initial in-service | |||||||
| Administrators: a 8 weeks after initial education care conference held regarding charts of difficult patients. | |||||||
Legend: PP=Pre-post; ITS=Interupted Time Series; CT=Controlled Trial; RCT=Randomized Controlled Trial; NH=Nursing Home; H=Hospital; P=Physician; N=Nurse; DC=Direct Care Worker (e.g. nursing assistant); T=Therapist; P=Pharmacist; O=Other; SW=Social Worker; S=Survey; CR=Chart Review; NHBPS=Nursing Home Behavioral Problem Scale; PRP= Psychogeriatric Resource Person.
Research Limitations
There were several limitations common amongst most of the studies. First, only 4 of the studies were controlled trials. Second, outcome measures varied significantly between studies (See table 2). Of the 16 studies, 5 studies examined patient outcomes exclusively, 7 examined provider knowledge and attitude outcomes, while only 3 examined both. Thus there was often an inability to understanding the connection between provider knowledge and attitudes and patient outcomes.
Table 2.
Summary of Included Study Outcomes
| Article | Changes in Professional Knowledge | Level of knowledge retention over time | Behavioral/Process Outcomes | Patient Outcomes | Limitations |
|---|---|---|---|---|---|
|
| |||||
| Arcand, 2009 | Decedent family member interviews showed no significant difference | Single site, Underpowered, outcomes are perception but patient family only, few family post-intervention received educational booklet (19%) | |||
|
|
|
||||
| Barton, 2006 | Greater identification of etiology of dementia after intervention (52% vs 91%, p=.007), treatment plan by physicians (35% vs 90%, p<.001), and management by nurses (22% vs 62%, p=.013). No statistical difference in pharmacologic management, likely due to small sample size, increase in non-pharmacolgic interventions (30% vs 100%, p<.001) | Single site, small sample size, atypical nursing home with academic attendings attached to a VA hospital. | |||
|
|
|
||||
| Beer, 2011 | 48% of general practitioners found that their learning needs were fully met, 45% partially met; 95% of staff felt it fully met their needs, 2% partially met. | Only process outcomes, few participants completed all the modules (10%) and only 29% attended at least one module. | |||
|
|
|
||||
| Cherry, 2009 AND Cherry, 2004 | MMSE reporting increased from 16% to 93% (p<.001); Increase in appropriate lab use for diagnosis of dementia increased 54% to 86% (p<.001); Referral to Alzheimers Association Safe Return program increased from 0% to 29% (p<.0001); Increased recording of ADLs, capacity, wandering potential in the medical record found. | Increased recording of depression from 11% to 57% p<.001 | Small sample size and number of clinicians trained, single atypical practice (Kaiser) in southern California | ||
| Improved caregiver satisfaction | |||||
|
|
|
||||
| Chodosh, 2006 AND Vickrey, 2006 | Greater knowledge of capacity assessment in intervention group (AOR 2.4, p=.02), more acknowledgement that managing dementia patients in primary care is difficult(4.6 vs 4.1 on 6 point likert scale, p=.03), No significant differences in knowledge of delirium evaluation, patient safety, depression treatment. No significant differences in attitude, perception of quality, utility of information, ability to improve quality of life in dementia. | 63.9% of patient guidelines were followed for intervention vs 32.9% for control (p<.001), higher level of community agency referrals in intervention group (RR 1.3); Confidence of caregiving among patient caregivers was higher for intervention group at 18 months (67.3 vs 60.3, p<.01) though the scale used was unclear. Statistically significant increases also found in caregiver use of support groups, patients receiving paid caregiver support, enrollment in the Alzheimer’s Association Safe Return program and other association services | Less measured statistically significant decline in intervention group over control group (.10 vs .03 on p=.034 on one point scale where 0 is worse),; increased cholinesterase use among intervention subjects (67.5% vs 58.8%, p=.032). | Primary care providers only, though of different disciplines. One small area of the country only, most providers only attended 1/5 modules, most of the benefit likely came from the SW case manager. | |
|
|
|
||||
| Chrzescijan ski, 2007 | No difference in staff attitudes found. | Lower frequency of aggravation after intervention (M=32.23 pre vs 28.09 post), but similar intensity. Authors found diminishing effect over time. | Small study in 4 NHs, no control, limited intervention, unclear how many staff participated | ||
|
|
|
||||
| Downs, 2006 | After intervention, an additional 31% of cases in practice with dementia were diagnosed in the workshop arm, 20% in the electronic tutorial arm, 30% in decision support arm vs 11% in control, P=.02). No changes in guideline concordance | Underpowered for measuring guideline concordance, no controlling for individual clinician difference, was analyzed at level of the practice. Differences in diagnosis could be due to external factors not related to the intervention. Intervention was primarily with general practitioners and nurses only had a small component of intervention. | |||
|
|
|
||||
| Ellis, 2010 | Increased ability to distinguish delirium from dementia (4% pre vs 74% post, p<.0001). Also significant improvements in suicide risk assessment, assessing violent or potentially violent situations, assessing psychotic symptoms, differentiating between substance intoxication and psychosis, communicating effectively with people with a mental health issue, conducting a mental status examination (p<.0001). | Only 163 participants took the post-test. Tests anonymous so no matching pre and post surveys | |||
|
|
|
||||
| Gallagher, 2011 | Improved knowledge of music therapy for patients with dementia after educational session (7.83 pre vs 9.17 post; 10 total points, higher is better, p<.0001). | Performed at a single hospice, small sample size within the hospice. Used new, untested instruments for knowledge. Descriptive statistics only, no patient outcomes | |||
|
|
|
||||
| Galvin, 2010 | Knowledge 9.97 pre vs 12.90 post, p<.001;9 item composite, total of 14 points possible), confidence (0.86 vs 2.42, p<.001; 5 item composite on 5 point likert scale, higher is more confident), and attitudes (6 questions, no composite measure 5/6 items improved) of dementia care improved immediately after completion | Slight declines in knowledge at 120 days in 3 of 4 hospitals, no change in one. Large decrease in confidence in one hospital (2.9 vs 0.9, p<.02) but no significant difference at other three hospitals. | Activity kits were implemented at ¾ hospitals after intervention. Specialized volunteer team for dementia patients created at one hospital. Elopement program created at one hospital. | 14.3% response rate to 120 day post test, thus likely significantly affecting the results at 120 days. No patient outcomes as hospitals refused | |
|
|
|
||||
| McAiney, 2007 | Improved confidence on multiple indicators of providing care to patients with dementia, no composite measure provided. | 85% of NHs still had a dementia resource person 4 years after the education session | >85% of the NH teams reported using standardized assessment tools and the template from the educational program for working with patients as necessary. Only 8% reported that the NH team was not teaching other staff in the NHs | Majority of respondents were nurses. No measurement of knowledge. No patient outcomes. Outcomes were by self-report of the PRP only, no independent data was obtained. | |
|
|
|
||||
| Mcphail, 2009 | Improved knowledge on post-test measures of knowledge reported but no numbers provided. | No p-values calculated. Small sample size at single hospital. Not all participants attended all sessions. | |||
|
|
|
||||
| Meuser, 2006 | Improved self reported clinical knowledge (4.3 vs 4.6 out of 6, p<.01), confidence (after the education (4.3 vs 6.4 unclear scale, p<.01) and practice behavior (1.7 vs 2.4 unclear scale, p<.01) | Knowledge was sustained over time, as there was no change between knowledge after the intervention and 3 and 12 months later | 27% reported a driver at 1 year vs 10% at baseline | No patient outcomes. Self report only. Multidisciplinary education, but there is no indication the participants worked with each other in usual practice. Lower response rates at 3 months and 1 year, could be selection bias. Unclear what the measurements meant. Survey was not psychometrically validated. | |
|
| |||||
| Monette, 2008 | No change in number of stressful events experienced by staff | 49.4% attempts to discontinue antipsychotics, 13.6% reduction, 12.3% failed discontinuation or reduction. 24.7% no change. No changes in other psychotropic medications, use of restraints, or number of stressful events experienced by staff. Decareased behavioral problems-NHBPS scores decreased from 16.3 to 11.4 over time (p<.0001) | Single NH in Canada, multidisciplinary but not interdisciplinary | ||
|
|
|
||||
| Ray, 1993 | Significantly Decreased antipsychotic (decreased 21 days per 100 vs 4, p<.001) and restraint use (36% reduction vs 5%, p<.001), which persisted after the education had ended per author report. No change in use of other psychotropics. Residents who had antipsychotics withdrawn did not have an increase in physical restrain use. No change in NHBPS scores between groups. | Only rural NHs, from 1990, multidisciplinary but not interdisciplinary, no changes in behavioral outcomes | |||
PT = patient; VA = Veterans Affairs; MMSE = Mini-Mental Status Exam; ADLs = activities of daily living; AOR = adjusted odds ratio; RR = risk ratio; SW = social work; NHs = nursing homes; PRP = psychogeriatric resource person; NHBPS = Nursing Home Behavioral Problem Scale.
Third, most of the interventions did not involve creating structure or process changes in care provision, only providing education to clinicians. Only four of the studies showed that knowledge, structure or process changes were maintained long-term after the educational intervention. Multiple studies have found that lasting change is rarely achieved when educational interventions are performed unless there are structure or process changes that allow the education to become ingrained into the culture (Maeck, Haak, Knoblauch, & Stoppe, 2007; Ockene & Zapka, 2000). Fourth, many of the studies were multidisciplinary in nature, not interprofessional, meaning that professions were trained separately and not in a team framework. Finally, two-thirds of the studies were vague as to what disciplines were participating, or the number of staff participating in the intervention.
Outcomes
Provider outcomes
Nine of the studies included in this review examined provider knowledge and attitude outcomes, however only four of these examined sustainability of the educational intervention as well (see Table 1). The first of these studies used a pre-post design and examined the immediate and 120 day post education benefits of a 7 hour, 5 module didactic session of 540 nurses, therapists, social workers (SW), pastors and nursing assistants (NA) in 4 hospitals (Galvin, et al., 2010). The study found improvements in provider knowledge of assessing and managing dementia and in their attitudes towards patients with the disease. The study also performed a 120 day post-test, finding that one hospital had no statistically significant loss in knowledge or confidence assessing and managing patients with dementia, one had a significant decrease in knowledge but not confidence, one had a slight loss in knowledge but not confidence, and one had slight but loss of both knowledge and confidence. The study did however have a small response rate (14.3%) on the 120 day post-test and differences between those who responded in the immediate and 120 day post-tests potentially skewed the results. The variation in retention over 120 days likely had to do with the population who took the post-test at that time, and therefore it is difficult to draw a conclusion about the retention piece of the study.
The second study using a pre-post design performed a 3-day dementia care “mini-residency” including didactic, clinical observation, and skills training techniques for rural providers caring for older adults (Galvin, Meuser, & Morris, 2011). This study was performed primarily with primary care providers including physicians, advanced practice nurses, and physician assistants, though some psychologists, social workers and “other individuals” also participated. This study found statistically significant improvement in knowledge, confidence and self-reported use of screening tests in dementia at 3 months, and improved confidence and self-reported use of screening tests in dementia at 1 year. Limitations of the study were that it was limited to a single site, though it was offered a number of times over a 9 year period, that no patient outcomes were examined, and screening test use was a self reported measure and not taken directly from patient charts. Additionally, the response rate to the follow-up surveys was only moderate at 47%, potentially causing response bias.
The third study using a pre-post design performed a two-hour multidisciplinary didactic education session with a variety of licensed, professional healthcare providers in the community to educate them about issues pertaining to driving with dementia (Meuser, Carr, Berg-Weger, Niewoehner, & Morris, 2006). This pre-post study found improved self-reported clinical knowledge and confidence related to assessing patients, and no change in retention of knowledge at 3 and 12 months. It also found increased self-reported process measures related to documentation of driving issues and referral to other disciplines or the DMV for a driving evaluation. A major limitation of this study is that it was an educational program limited to a single issue and there were no patient outcomes to confirm the self-reported process measures. Additionally there were no structural changes that would have precipitated maintenance of knowledge over the long-term.
A fourth study examining long-term retention performed either a 12 or 18 hour didactic educational program with homework between sessions to create a psychogeriatric resource person at nursing homes through Ontario Province in Canada using a pre-post design (McAiney, et al., 2007). The programs were open to licensed healthcare professionals; however a majority who received the education were nurses (95%), with only small numbers from other fields. This pre-post study found that participants increased and maintained their knowledge and confidence in assessing and managing physical and cognitive issues in aging six weeks after receiving the education intervention. Once trained, the resource staff provided consultation in their nursing home to other staff. Over time, the resource staff also received additional education and patient specific consultation from an external consultant. Four years after the initial education session, 85% of the nursing homes still had a resource staff member. Additionally, over 85% of the resource staff members reported that they and/or their teams were using standardized assessment tools to assess their patients as needed while only 8% reported that the resource staff member was not teaching other staff in their nursing home. The primary limitation of this study is that all of the results were by self-report and no independent data was obtained showing outcomes of the program. Additionally, while the authors state that many of the resource people developed teams at their institutions, they do not describe these teams, whether they were interprofessional in nature, or how they functioned.
Of the five studies that examined changes in professional knowledge but not retention over time, only one focused on diagnosis and management of dementia (Chodosh, et al., 2006; Vickrey, et al., 2006). This cluster randomized controlled trial provided a 5 module, 100 minute didactic session to physicians, nurse practitioners, and physicians assistants in 3 outpatient clinics in conjunction with a skilled geriatric social work case management program and a case management software/communication system. The study found the clinicians developed a greater knowledge of capacity assessment and more acknowledgement that managing dementia patients in primary care is difficult, however no other changes in knowledge or attitudes. This was likely due to the fact that 50% of providers only attended 1 of the 5 modules, and the average number of modules attended was only 2 out of 5.
A second study focusing on improving the management of dementia and its sequelae performed an interprofessional training program that consisted of 10 1-hour didactic sessions (Mcphail, Traynor, Wikstrom, Brown, & Quinn, 2009). This pre-post study in the acute care setting found improved knowledge on post-test measures of knowledge and skills, though the statistics were descriptive in nature and no confidence intervals or p values were provided.
Two other pre-post studies found improvement in dementia related knowledge. One single site found improved knowledge of music therapy for hospice patients with dementia following a 60 minute didactic education session (Gallagher, 2011). A second, focusing on increased understanding of mental health conditions in rural Australia, found increased ability to distinguish delirium from dementia among a variety of professional and unlicensed health workers (Ellis & Philip, 2010).
A final study used an interrupted time series format to examine the effects of a 40 minute video on reducing dementia related aggression in the nursing home (Chrzescijanski, Moyle, & Creedy, 2007). The study found no change in attitudes, as would be expected after such a limited training program.
Patient outcomes
Eight of the studies included in this review directly examined patient outcomes, generally through chart review (see Table 2). Two of these studies were cluster randomized controlled trials. The first, discussed above in provider outcomes, found that the group of providers who received the educational intervention had significantly increased adherence to dementia guidelines, higher level of community agency referrals for their patients, and that their patients had lower levels of decline than in the control group (Vickrey, et al., 2006). Additionally, confidence was higher amongst caregivers of patients seen in the intervention group, likely due to the greater support provided by the case manager and community agency resources. The study also found a higher proportion of patients in the intervention group receiving cholinesterase inhibitors.
The second cluster randomized controlled trial study examined whether one of three interventions versus control: an educational CD-ROM mailed to providers, decision support software placed in the practice electronic medical record, or a practice based workshop improved dementia diagnosis and concordance with dementia treatment guidelines (Downs, et al., 2006). This study performed these interventions with physicians and nurses at 36 general practice clinics in London and Scotland. The study found that in the workshop and decision support arms of the study a larger number of patients were diagnosed with dementia, however it found no changes in guideline adherence. The study was underpowered to measure guideline concordance and did not control for individual clinician differences as it was analyzed at the level of the practice. Additionally, there were baseline differences in patients between the groups that were not accounted for.
One non-randomized controlled trial reviewed here examined patient outcomes (Ray, et al., 1993). This study performed separate training 45 minute to 1 hour in length with physicians and nursing home staff in 1990 in 4 rural nursing homes, 2 intervention and 2 control. The education focused on management of behavioral symptoms. Educational sessions were also held with the nursing home administrators and a follow up with them eight weeks later was performed to assist with hard wiring the education into the institution. The study found significantly reduced antipsychotic use and mildly reduced restraint use that persisted for at least a year after the education had ended. The primary limitations of this study were the non-random design, as the two intervention homes were chosen for their proximity to the study authors, and that the disciplines were taught separately making it multidisciplinary, not interdisciplinary. Additionally, the age of the trial limits its applicability to today’s healthcare environment.
Two interrupted time series trials included in this review examined patient outcomes. The first, whose design was discussed above found a significantly reduced frequency of aggravation after the intervention but no change in intensity when aggravation occurred (Chrzescijanski, et al., 2007). A second interrupted time series trial involved multidisciplinary training in behavioral and pharmacologic methods for managing behavioral symptoms of dementia (Monette, et al., 2008). The study performed separate 1.5 hour training sessions for registered nurses and physician, and a 45 minute session for pharmacists at a nursing home. The study found that after the training, there were a significant number of attempts, many of them successful, to reduce or discontinue patients receiving antipsychotic medications. It also found a decrease in behavioral problems and fewer stressful events experienced by staff. While successful in its outcomes, this study was truly a multidisciplinary and not interprofessional program as the trainings were performed separately. Additionally, the single site, interrupted time series design limits the generalizability of the findings.
The remaining three outcomes studies utilized a pre-post design. The first trained social workers to become dementia care managers and physicians to diagnose and manage dementia. The physician training included providing guidelines on how to screen patients using interactive didactic sessions, a provider toolkit, educational detailing, and institutional support (Cherry, Hahn, & Vickrey, 2009; Cherry, et al., 2004). The study found improved caregiver satisfaction and increased recording of depression, decision-making capacity, activities of daily living, and wandering potential amongst dementia patients. It also found significantly increased reporting of mini-mental status exam scores, appropriate lab use prior to dementia diagnosis, and increased referral to the Alzheimer’s Association. The primary limitations of this multidisciplinary initiative were that it had a small sample size and was in an atypical integrated practice setting.
The second pre-post study, at a nursing home, performed eight hours of didactic educational sessions over a three month period to nurses (Barton, Miller, & Yaffe, 2006). Separately, physicians held monthly roundtable conferences where case studies were reviewed and a specialist nurse practitioner provided feedback. Additionally, the physicians were provided with an algorithm to evaluate cognitive impairment, and guidelines for diagnosis and management. The study found greater identification of etiology of dementia by physicians. It also found an increase in treatment plan development by physicians and nurses and an increase in non-pharmacologic interventions. No changes were found in pharmacologic management though. The primary limitations of this study were that it was performed at a small, atypical Veterans Affairs Nursing Home Care Unit attached to an academic medical center, physicians were academic attendings, and it had a small sample size.
The third and final pre-post study was also performed at a single nursing home and the intervention was a 45 minute didactic education for nurses, a separate 60 minute didactic session for physicians, and a booklet for patients/caregivers about end of life care for patients with dementia (Arcand, et al., 2009). The study found no significant differences in perception of care following interviews with decedent family members. Multiple limitations hindered the performance of this study including it being underpowered, patient outcomes were from the perception of the decedent family member, few of the family members received the educational booklet, and the education was limited and multidisciplinary.
Discussion
Several themes and limitations were found throughout this review and synthesis of the literature. First, the review found that interprofessional dementia education has the potential to provide improved knowledge and attitudes for staff. All of the studies discussed here that measured provider knowledge showed improvement in at least one area of knowledge related to dementia recognition or care. Even the studies with less robust or institutionalized education interventions appeared to show some gains in knowledge related to dementia (Chodosh, et al., 2006; Gallagher, 2011). Only one study that measured attitudes towards patients with dementia showed no change in attitudes (Chrzescijanski, et al., 2007). In this study, the measurement was specific to staff attitudes towards dementia related aggression, which is likely more difficult to change than general attitudes towards dementia. The intervention did show a decreased frequency of aggravation amongst patients however.
A second theme that emerged was that interprofessional education and structural reform has the potential to improve patient outcomes. All of the studies that measured patient outcomes with the exception of one found improvement in care for patients with dementia (Arcand, et al., 2009). The one study that did not was very limited in nature, underpowered, and used patient family perception of care as the outcome measure, which is not always a reliable indicator of quality of care in patients with dementia (Crespo, Bernaldo de Quiros, Gomez, & Hornillos, 2011; Novella, et al., 2001). In addition to knowledge attainment from education, the act of learning from educational initiatives can stimulate clinicians to think outside of the box in implementing new ways to improve care. This was particularly evident in the study by Galvin et al (2010), where clinicians were so enthusiastic about improving care for older adults with dementia that they developed their own interventions based on the education received, such as activity carts and a code “green” to minimize patients at risk for elopement from doing so, which included special precautions such as a green gown and further staff training. Other studies may have prompted similar out of the box implementation when clinicians return to their institution or practice from the education but most of the studies had no method for measuring or ascertaining that other changes were implemented due to the stimulation from the education.
While education can improve knowledge and potentially outcomes, it is important to remember that improved knowledge does not always lead to improvement in patient outcomes. While several of the studies included herein did show improvements in outcomes, many others have found that the link between knowledge and outcomes can be fleeting or non-existent (Rampatige, Dunt, Doyle, Day, & van Dort, 2009; Reeves, et al., 2008), and that those that are multi-faceted have a greater chance of changing practice and outcomes (Davis & Galbraith, 2009). Even if education is made available for free to clinicians, the chance of it being utilized is low. Despite being aware of and completing online continuing education in general, few physicians are even aware of freely available online continuing education in dementia (Galvin, Meuser, Boise, & Connell, 2011). Thus a systematic method of providing education and structural change in dementia is required; it cannot be left to individual providers or administrators. This is of particular concern for primary care practices, which especially in suburban and rural settings tend to be smaller and have fewer resources, thus limiting their potential for participation. Considering the large number of older adults living outside of cities with large primary care practices, the ability to implement evidence-based interprofessional dementia care faces significant hurdles.
A third theme that emerged was that interventions that included structural reforms within institutions have the potential to sustain long-term change in practice. All four studies that were sufficiently powered and instituted structural reform within their study found at least some level of sustainability over the long-term (Galvin, et al., 2010; McAiney, et al., 2007; Ray, et al., 1993; Vickrey, et al., 2006).
Finally, a fourth theme amongst the current literature is that while in geriatrics we have spoken frequently about performing interdisciplinary or interprofessional care, even our research studies tend to eschew those principles in this area. Most of the studies included here were multidisciplinary in nature, not interprofessional. There was minimal co-mingling between professions in education initiatives, shared learning or case study sessions. In order to truly foster an interprofessional environment that values the views of multiple disciplines, teams need not only to receive similar information, but need to be trained together. Standard practice in many nursing homes, hospices, and Alzheimer’s Disease Centers involves interprofessional case conferences, yet the research models used in the majority of these studies maintained separate programs for each discipline.
Based on these findings, we can surmise that when implementing interprofessional care teams in a variety of practice settings it is important to structure the initiative to include the following to ensure uptake, maintain changes in practice over the long run, and improve quality of care for older adults with dementia: 1) true interprofessional education experiences where all disciplines are both present and participate in the education that includes interactive elements to engage in team building; 2) structural changes must be made at the institution level to ensure education is converted to changes in practice (e.g. changing structure of care teams, adding interprofessional rounds, changing documentation and policies and procedures); 3) collect both staff knowledge and patient outcomes data in a continuous quality improvement fashion to ensure changes and remediate/reeducate where weakness still exists. While these 3 items should be implemented, we do not have enough knowledge based on these studies regarding what form interprofessional education programs should take, exactly what structural changes should occur, or what specific outcomes should be focused on. While some of this uncertainty relates to the lack of data, some relates to the principle in dissemination science that items such as these need to be customized to the individual clinic or hospital where implementation is to occur (Brownson, Colditz, & Proctor, 2012).
Limitations
Because of the limited number of studies educating multiple disciplines in dementia, this review included a wide array of studies with varying methodologies and foci within dementia care. Thus, it was impossible to perform meta-analyses or directly compare the results of one study with another.
Recommendations For Future Research
One of the primary limitations found through performing this review is that there is a significant lack of implementation studies in dementia care, particularly ones with an interprofessional intervention. While many studies have performed interventions for the recognition (Lonie, Tierney, & Ebmeier, 2009) and management (Kong, Evans, & Guevara, 2009) of dementia and its sequelae, few have examined the dissemination of this information into general practice. Similarly, few studies have examined interprofessional implementation research, despite the fact that interprofessional dementia care has been found to be extremely effective (Callahan, et al., 2006) and is the gold standard of practice in this field. Almost fifteen years after the call to increase interprofessional research in dementia care (Volicer & Hurley, 1999), we have increased the volume of interprofessional research but still do not have a great deal of evidence about how to translate it into practice. Even amongst the studies presented here, a majority of them were multidisciplinary in nature but not interdisciplinary or interprofessional, in that the disciplines were educated separately or acted separately from other disciplines. Additionally, many of the studies only performed the education with physicians and nurses and did not include other important disciplines such as physical, occupational and speech therapists, and social workers. In order to gain the full potential that having multiple health professions involved, they need to include a wide range of disciplines, and they need to work together, not in parallel.
This gap in the translation of knowledge from research to practice is present in other areas of dementia recognition and care as well, such as among unskilled caregivers and family members (Draper, Low, Withall, Vickland, & Ward, 2009). We therefore need to increase the amount of implementation research in interprofessional dementia recognition and management, and measure both in terms of provider knowledge and patient outcomes. Furthermore, we need to ensure that this research finds its way into practice through policy reform and simplicity of implementation. The current implementation of Accountable Care Organizations, and reduction in reimbursement for readmissions provides an opportunity to improve dementia care and implement evidence-based interprofessional dementia programs, however without the proper research into how best to implement this care, it will be pushed to the bottom of priorities compared to other high profile diseases like congestive heart failure or pneumonia.
Related to this issue, none of the studies examined health services outcomes such as cost effectiveness or utilization. Currently, healthcare costs are increasing unsustainably, becoming a greater and greater proportion of gross domestic product, and decreasing real family income (Auerbach & Kellermann, 2011). Given this environment, in order for interventions to be implemented in accountable care organizations and other large scale programs they need to show improved cost effectiveness.
A third major gap is related to the inadequate indexing of studies. In order to find the 18 articles from 16 studies present in this paper, we had to perform multiple searchers using a variety of keywords, as educational and interprofessional studies are not consistently labeled in databases. In the future, authors of studies performing interprofessional education interventions should ensure that interprofessional education is included as a keyword.
Summary
While significant research has been performed over the past 20 years in how to assess and manage patients with dementia, few studies have examined how best to implement this research through ongoing education in the community, and even fewer initiatives are interprofessional in nature despite the evidence that interprofessional teams are best situated to manage the care of these patients with complicated needs (Lang, et al., 2012). This review found only 18 papers from 16 studies that have examined methods for interprofessional evidence based assessment and management of dementia or its sequelae. While many of these studies showed improvement either in clinician knowledge, confidence and attitudes, or patient outcomes, few were able to link between the two, or measured the effects of the intervention over a long period of time. Given the aging of the population and the subsequent rise in dementia rates that will occur over the next 20 years, future wide scale dissemination research in this field is urgently needed to improve patient outcomes and ensure patients receive the best possible, patient centered care.
Acknowledgments
This work was supported by grants from the National Palliative Care Research Council (AAB) Mount Sinai Claude D. Pepper Older Americans Independence Center (P30 AG028741, AAB), and the National Institute on Aging (P30 AG008051, R01 AG040211, JEG).
Contributor Information
Abraham A Brody, New York University College of Nursing and the James J Peters Bronx VA Geriatric Research Education and Clinical Center, Ab.Brody@nyu.edu, 726 Broadway, 10th Floor, New York, NY 10003, USA, Tel: 212-992-7341; Fax 212-995-3143.
James E. Galvin, New York University School of Medicine, Departments of Neurology, Psychiatry, Nutrition and Public Health, and the Alzheimer Disease Center, James.Galvin@nyumc.org.
References
- Arcand M, Monette J, Monette M, Sourial N, Fournier L, Gore B, et al. Educating nursing home staff about the progression of dementia and the comfort care option: impact on family satisfaction with end-of-life care. Journal of the American Medical Directors Association. 2009;10(1):50–55. doi: 10.1016/j.jamda.2008.07.008. [DOI] [PubMed] [Google Scholar]
- Auerbach DI, Kellermann AL. A Decade Of Health Care Cost Growth Has Wiped Out Real Income Gains For An Average US Family. Health Affairs. 2011;30(9):1630–1636. doi: 10.1377/hlthaff.2011.0585. [DOI] [PubMed] [Google Scholar]
- Barton C, Miller B, Yaffe K. Improved evaluation and management of cognitive impairment: results of a comprehensive intervention in long-term care. Journal of the American Medical Directors Association. 2006;7(2):84–89. doi: 10.1016/j.jamda.2005.06.008. [DOI] [PubMed] [Google Scholar]
- Boult C, Green AF, Boult LB, Pacala JT, Snyder C, Leff B. Successful Models of Comprehensive Care for Older Adults with Chronic Conditions: Evidence for the Institute of Medicine’s “Retooling for an Aging America” Report. Journal of the American Geriatrics Society. 2009;57(12):2328–2337. doi: 10.1111/j.1532-5415.2009.02571.x. [DOI] [PubMed] [Google Scholar]
- Brownson RC, Colditz GA, Proctor EK. Dissemination and implementation research in health : translating science to practice. Oxford: Oxford University Press; 2012. [Google Scholar]
- Callahan CM, Boustani MA, Unverzagt FW, Austrom MG, Damush TM, Perkins AJ, et al. Effectiveness of Collaborative Care for Older Adults With Alzheimer Disease in Primary Care. JAMA: The Journal of the American Medical Association. 2006;295(18):2148–2157. doi: 10.1001/jama.295.18.2148. [DOI] [PubMed] [Google Scholar]
- Cherry DL, Hahn C, Vickrey BG. Educating primary care physicians in the management of Alzheimer’s disease: using practice guidelines to set quality benchmarks. International psychogeriatrics / IPA. 2009;21(Suppl 1):S44–52. doi: 10.1017/S1041610209008692. [DOI] [PubMed] [Google Scholar]
- Cherry DL, Vickrey BG, Schwankovsky L, Heck E, Plauchm M, Yep R. Interventions to improve quality of care: the Kaiser Permanente-alzheimer’s Association Dementia Care Project. The American journal of managed care. 2004;10(8):553–560. [PubMed] [Google Scholar]
- Chodosh J, Berry E, Lee M, Connor K, DeMonte R, Ganiats T, et al. Effect of a dementia care management intervention on primary care provider knowledge, attitudes, and perceptions of quality of care. Journal of the American Geriatrics Society. 2006;54(2):311–317. doi: 10.1111/j.1532-5415.2005.00564.x. [DOI] [PubMed] [Google Scholar]
- Chrzescijanski D, Moyle W, Creedy D. Reducing dementia-related aggression through a staff education intervention. Dementia. 2007;6(2):271–286. [Google Scholar]
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Review of Interventions Version 5. 1. 0. 2011 Mar; Available from http://www.cochrane-handbook.org/
- Crespo M, Bernaldo de Quiros M, Gomez MM, Hornillos C. Quality of Life of Nursing Home Residents With Dementia: A Comparison of Perspectives of Residents, Family, and Staff. The Gerontologist. 2011 doi: 10.1093/geront/gnr080. [DOI] [PubMed] [Google Scholar]
- Davis D, Galbraith R. Continuing Medical Education Effect on Practice Performance. Chest. 2009;135(3 suppl):42S–48S. doi: 10.1378/chest.08-2517. [DOI] [PubMed] [Google Scholar]
- Downs M, Turner S, Bryans M, Wilcock J, Keady J, Levin E, et al. Effectiveness of educational interventions in improving detection and management of dementia in primary care: cluster randomised controlled study. BMJ. 2006;332(7543):692–696. doi: 10.1136/bmj.332.7543.692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Draper B, Low LF, Withall A, Vickland V, Ward T. Translating dementia research into practice. International psychogeriatrics / IPA. 2009;21(Suppl 1):S72–80. doi: 10.1017/S1041610209008709. [DOI] [PubMed] [Google Scholar]
- Ellis IK, Philip T. Improving the skills of rural and remote generalists to manage mental health emergencies. Rural and remote health. 2010;10(3):1503. [PubMed] [Google Scholar]
- Gallagher M. Evaluating a protocol to train hospice staff in administering individualized music. Int J Palliat Nurs. 2011;17(4):195–201. doi: 10.12968/ijpn.2011.17.4.195. [DOI] [PubMed] [Google Scholar]
- Galvin JE, Kuntemeier B, Al-Hammadi N, Germino J, Murphy-White M, McGillick J. “Dementia-friendly Hospitals: Care not Crisis”: An Educational Program Designed to Improve the Care of the Hospitalized Patient With Dementia. Alzheimer disease and associated disorders. 2010 doi: 10.1097/WAD.0b013e3181e9f829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvin JE, Meuser TM, Boise L, Connell CM. Internet-Based Dementia Resources: Physician Attitudes and Practices. Journal of applied gerontology : the official journal of the Southern Gerontological Society. 2011;30(4):513–523. doi: 10.1177/0733464810363894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvin JE, Meuser TM, Morris JC. Improving Physician Awareness of Alzheimer Disease and Enhancing Recruitment: The Clinician Partners Program. Alzheimer Dis Assoc Disord. 2011 doi: 10.1097/WAD.0b013e318212c0df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inouye SK, Foreman MD, Mion LC, Katz KH, Cooney LM., Jr Nurses’ recognition of delirium and its symptoms: comparison of nurse and researcher ratings. Archives of Internal Medicine. 2001;161(20):2467–2473. doi: 10.1001/archinte.161.20.2467. [DOI] [PubMed] [Google Scholar]
- Interprofessional Education Collaborative. Core competencies for interprofessional collaborative practice: Report of an expect panel. Washington, D.C.: Interprofessional Education Collaborative; 2011. [Google Scholar]
- Knopman D, Donohue JA, Gutterman EM. Patterns of care in the early stages of Alzheimer’s disease: impediments to timely diagnosis. Journal of the American Geriatrics Society. 2000;48(3):300–304. doi: 10.1111/j.1532-5415.2000.tb02650.x. [DOI] [PubMed] [Google Scholar]
- Kong E-H, Evans LK, Guevara JP. Nonpharmacological intervention for agitation in dementia: A systematic review and meta-analysis. Aging & Mental Health. 2009;13(4):512–520. doi: 10.1080/13607860902774394. [DOI] [PubMed] [Google Scholar]
- Lang PO, Vogt-Ferrier N, Hasso Y, Le Saint L, Drame M, Zekry D, et al. Interdisciplinary geriatric and psychiatric care reduces potentially inappropriate prescribing in the hospital: interventional study in 150 acutely ill elderly patients with mental and somatic comorbid conditions. J Am Med Dir Assoc. 2012;13(4):406 e401–407. doi: 10.1016/j.jamda.2011.03.008. [DOI] [PubMed] [Google Scholar]
- Lonie JA, Tierney KM, Ebmeier KP. Screening for mild cognitive impairment: a systematic review. International Journal of Geriatric Psychiatry. 2009;24(9):902–915. doi: 10.1002/gps.2208. [DOI] [PubMed] [Google Scholar]
- Maeck L, Haak S, Knoblauch A, Stoppe G. Early diagnosis of dementia in primary care: a representative eight-year follow-up study in Lower Saxony, Germany. International Journal of Geriatric Psychiatry. 2007;22(1):23–31. doi: 10.1002/gps.1646. [DOI] [PubMed] [Google Scholar]
- McAiney CA, Stolee P, Hillier LM, Harris D, Hamilton P, Kessler L, et al. Evaluation of the sustained implementation of a mental health learning initiative in long-term care. International psychogeriatrics / IPA. 2007;19(5):842–858. doi: 10.1017/S1041610206004443. [DOI] [PubMed] [Google Scholar]
- Mcphail C, Traynor V, Wikstrom D, Brown M, Quinn C. Improving outcomes for dementia care in acute aged care: Impact of an education programme. Dementia. 2009;8(1):142–147. [Google Scholar]
- Meuser TM, Carr DB, Berg-Weger M, Niewoehner P, Morris JC. Driving and dementia in older adults: Implementation and evaluation of a continuing education project. The Gerontologist. 2006;46(5):680–687. doi: 10.1093/geront/46.5.680. [DOI] [PubMed] [Google Scholar]
- Monette J, Champoux N, Monette M, Fournier L, Wolfson C, du Fort GG, et al. Effect of an interdisciplinary educational program on antipsychotic prescribing among nursing home residents with dementia. International journal of geriatric psychiatry. 2008;23(6):574–579. doi: 10.1002/gps.1934. [DOI] [PubMed] [Google Scholar]
- Novella JL, Jochum C, Jolly D, Morrone I, Ankri J, Bureau F, et al. Agreement between patients’ and proxies’ reports of quality of lifein Alzheimer’s disease. Quality of Life Research. 2001;10(5):443–452. doi: 10.1023/a:1012522013817. [DOI] [PubMed] [Google Scholar]
- Ockene JK, Zapka JG. Provider Education To Promote Implementation of Clinical Practice Guidelines*. Chest. 2000;118(2 suppl):33S–39S. doi: 10.1378/chest.118.2_suppl.33s. [DOI] [PubMed] [Google Scholar]
- Plassman BL, Langa KM, Fisher GG, Heeringa SG, Weir DR, Ofstedal MB, et al. Prevalence of Dementia in the United States: The Aging, Demographics, and Memory Study. Neuroepidemiology. 2007;29(1-2):125–132. doi: 10.1159/000109998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rampatige R, Dunt D, Doyle C, Day S, van Dort P. The effect of continuing professional education on health care outcomes: lessons for dementia care. International psychogeriatrics / IPA. 2009;21(Suppl 1):S34–43. doi: 10.1017/S1041610209008746. [DOI] [PubMed] [Google Scholar]
- Ray WA, Taylor JA, Meador KG, Lichtenstein MJ, Griffin MR, Fought R, et al. Reducing Antipsychotic Drug Use in Nursing Homes: A Controlled Trial of Provider Education. Arch Intern Med. 1993;153(6):713–721. [PubMed] [Google Scholar]
- Reeves S, Zwarenstein M, Goldman J, Barr H, Freeth D, Hammick M, et al. Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2008;(1) doi: 10.1002/14651858.CD002213.pub2. CD002213. [DOI] [PubMed] [Google Scholar]
- Rhodes-Kropf J, Cheng H, Castillo EH, Fulton AT. Managing the Patient with Dementia in Long-Term Care. Clinics in Geriatric Medicine. 2011;27(2):135–152. doi: 10.1016/j.cger.2011.01.001. [DOI] [PubMed] [Google Scholar]
- Sloane PD, Zimmerman S, Suchindran C, Reed P, Wang L, Boustani M, et al. The public health impact of Alzheimer’s disease, 2000-2050: potential implication of treatment advances. Annual review of public health. 2002;23:213–231. doi: 10.1146/annurev.publhealth.23.100901.140525. [DOI] [PubMed] [Google Scholar]
- Valcour VG, Masaki KH, Curb JD, Blanchette PL. The detection of dementia in the primary care setting. Archives of Internal Medicine. 2000;160(19):2964–2968. doi: 10.1001/archinte.160.19.2964. [DOI] [PubMed] [Google Scholar]
- Vickrey BG, Mittman BS, Connor KI, Pearson ML, Della Penna RD, Ganiats TG, et al. The effect of a disease management intervention on quality and outcomes of dementia care: a randomized, controlled trial. Annals of internal medicine. 2006;145(10):713–726. doi: 10.7326/0003-4819-145-10-200611210-00004. [DOI] [PubMed] [Google Scholar]
- Volicer L, Hurley AC. Assessment of behavioral symptom management in demented individuals. Alzheimer Disease and Associated Disorders. 1999;13(Suppl 1):S59–66. doi: 10.1097/00002093-199904001-00014. [DOI] [PubMed] [Google Scholar]


