Abstract
Background
The Borg RPE scale is widely used for many patient populations, but the ability of patients to accurately report their RPE without visual feedback has not been studied. However, it is needed in clinical settings.
Objective
The objective was to investigate if the Borg scale could be used as a measure of perceived isometric exertion in healthy subjects and in patients who have suffered a stroke.
Methods
In experiment (Exp) 1, young and healthy subjects (n=15) were instructed 1) to perform spontaneous pushes (i.e., self-selected effort) without visual feedback, and 2) to produce and hold self-determined isometric finger flexion at five Borg levels (i.e., very light, light, somewhat hard, hard and very had) without visual feedback. In Exp 2, chronic stroke subjects (n=10) were instructed to produce self-determined isometric elbow flexion at four perceptual levels (comfortable, light, somewhat hard and hard) on the impaired and non-impaired side.
Results
In Exp 1, young and healthy subjects demonstrated that 1) when asked to self-select without visual feedback (spontaneous push), subjects tended to exert at “somewhat hard” level, about 12%MVC; 2) The blinded self-selection of forces ranged from 2% of MVC (i.e., Very light) up to only 39% of MVC (i.e., Very hard), instead of evenly distributing from 0–100% MVC as instructed. In Exp 2, stroke subjects were able to distinguished different levels of perceived exertion among light (19% MVC), somewhat hard (moderate) (33%MVC), and hard (63%MVC); this ability was not different between the impaired and non-impaired limb; a “light” level was equivalent to a “comfortable” level for stroke subjects.
Conclusion
Both healthy and stroke subjects are able to differentiate distinct levels of perceived exertion during isometric force when prompted with the Borg scale. Efforts at smaller %MVC levels are perceived by stroke subjects as greater-than-normal Borg PRE levels.
Keywords: Borg scale, isometric force, force perception, fingers, stroke
Introduction
A patient’s subjective experience of physical exertion during rehabilitation can greatly impact the course of their recovery. In a clinical setting, direct measurements of the magnitude of forces being exerted are not always available. Clinicians must rely on estimates based on observation and patient’s subjective report. Simply, how strenuous a given exercise feels to a patient is directly related to the amount of effort exerted. Such considerations are especially important for patients with neurological impairments (e.g., stroke, TBI). These patients are characteristically prone to physical and motivational fatigue 1,2. In addition, they may have reduced somatosensation as part of their impairment, which is associated with worse functional outcomes 3.
The Borg scale was first developed by Gunnar Borg in the 1960s to quantify perceived exertion and allow for inter-individual comparisons 4. The original Borg RPE Scale (range: 6–20), although subjective, has been found to correlate well with the objective measures of workload level and heart rate4,5. It continues to be one of the most widely utilized measures of perceived exertion, especially in cardiovascular rehabilitation 6. Several recent studies in the field of ergonomics have reported strong correlations between the Borg scale and isometric hang grip forces 7–9. The primary focus of these studies was to develop a cost-effective way to monitor workplace exertion and prevent injury, however. In these studies, a simplified category ratio scale, called a CR-10 scale (range: 0–10) 5, was used without visual feedback to estimate the grip forces pre-calibrated by the subjects. Visual targets were presented to subjects at predefined percentages of their maximal voluntary contraction (MVC) for pre-calibration7–9. We found little discussion in the literature regarding the subjective experience of subjects at these levels and how hard subjects would push if visual targets were not provided. Furthermore, no such studies have been investigated in the patient populations, including patients who have suffered a stroke.
In order to understand perceived exertion of patients with neurological impairment in complex motor tasks, one must first investigate perceived exertion of healthy individuals in simple motor tasks. Isometric finger flexion has proven to be a useful experimental paradigm for studying the neuromuscular system 10–13. The objectives of this study were 1) to investigate if the Borg RPE scale could be used as a measure of perceived isometric exertion using the finger flexion paradigm in healthy subjects, and 2) to examine how well stroke subjects can differentiate efforts at different levels of exertion during isometric elbow flexion of the impaired and non-impaired arms.
Methods
Participants
In Experiment (Exp) 1, fifteen healthy subjects (6 male, 9 female; mean age: 28.3 years; age range: 24–43) without neurological or musculoskeletal diseases participated in the experiment. All subjects were right hand dominant according to hand usage during routine activities such as writing and eating. In Exp 2, there was a convenience sample of ten chronic hemiparetic stroke patients (history of stroke: mean: 66.2 months, range: 22–132months; 7 male, 3 female; mean age: 60.1 years; range: 37–79 years; 5 right and 5 left hemiplegia). Inclusion criteria for Exp 2 were: 1) hemiplegia secondary to an ischemic or hemorrhage stroke; 2) at least 6 months post-stroke; 3) residual voluntary elbow flexion force; 4) full passive range of motion in the impaired shoulder and elbow joints; 5) spastic hypertonia in elbow flexors of the impaired side, rated as Modified Ashworth Scale (MAS) less than 3; and 6) able to understand and follow instructions related to the experiments. Exclusion criteria for Exp 2 included: 1) a history of multiple strokes or bilateral involvement; 2) presence of contracture that would limit full elbow range of motion on the impaired side; 3) visual spatial neglect; or 4) elbow flexor MAS score of 3 or 4 in the impaired shoulder side. All subjects gave informed consent and all procedures were approved by our institutional review board and conformed to the Declaration of Helsinki.
Exp 1 – Finger force estimation in healthy subjects
Experimental setting
We adopted the previous experimental settings10–13. All healthy subjects were seated comfortably on an adjustable chair in front of a table. The right forearm was secured to a wooden board on the table with Velcro straps (Figure 1). The right shoulder was abducted to approximately 15° in the frontal plane and flexed to 45° in the sagittal plane. The elbow joint was flexed to approximately 90°. The fingers of the right hand were positioned onto four force sensors (208C02, PCB Piezotronics, Depew, NY). The force sensors were mounted on the wooden board and their two-dimensional position was adjustable to optimize the comfort of subjects.
Figure 1.
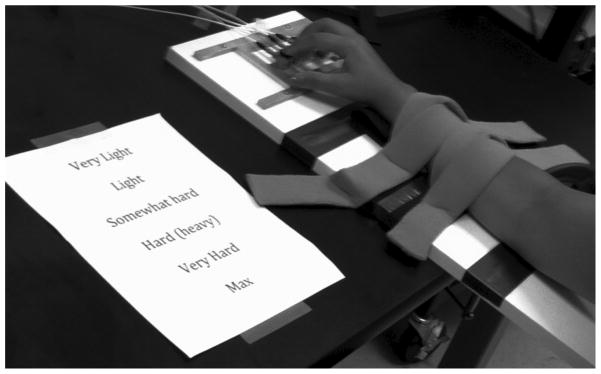
Experimental setting for finger flexion tasks. Note that after the spontaneous push and MVC measurement, they were presented with verbal cues of the Borg RPE Scale.
Tasks
The finger flexion tasks were divided into three parts in the following order: 1) a spontaneous push of self-selected force during which subjects were told to press the sensors at that level and hold for 10 seconds; 2) maximal voluntary contraction (MVC). Subjects were instructed to press and hold the sensors with their fingers as hard as possible for about 5 seconds. The highest peak value from three trials was recorded as the MVC for each subject; and 3) perceptual levels of force using the Borg scale. For the RPE Borg Scale measurements, subjects were provided with an 8″×10″ sheet of paper listing five levels: (from bottom to top) Very Light, Light, Somewhat Hard, Hard, Very Hard, Maximum (Figure 1). They were instructed to imagine these 6 levels of force were evenly distributed through their maximal ability to push. Subjects then practiced producing these self-determined perceptual levels without visual feedback. When they felt confident in their ability to distinguish and reproduce these levels of force, the subjects were presented with each level in a randomized order. For all tasks, each task was repeated six times. A rest period of at least 30 seconds was observed between each 10-second trial, and the next trial did not begin until the subject verbalized their readiness to continue. Standard verbal encouragement was provided, but subjects did not receive visual or auditory feedback of their performance.
Exp 2 – elbow flexion force estimation in stroke patients
Experimental setting
We adopted the experimental setting we used in a recent study14. Briefly, stroke subjects were seated on a height-adjustable chair with upper arm support in a symmetrical position. The shoulders were slightly flexed and abducted to 45°, the elbow flexed to 90°, and the forearm in a neutral position on the table. Additional trunk stabilization was provided using shoulder straps. The tested arm and wrist were secured firmly on a customized apparatus. A force sensor (Model 208C02, PCB Piezotronics, Depew, NY) was placed perpendicular to the distal end of each forearm (about 2 cm proximal to the wrist joint) to measure isometric elbow flexion force.
Tasks
Similarly, two elbow flexion tasks were performed by each limb: 1) the elbow flexion MVC was first determined for each side as the highest of three trials; 2) perceptual levels of force. As in Exp 1, subjects produced the following perceptual levels of elbow flexion on each side without visual feedback: Comfortable, Light, Somewhat hard (moderate) and Hard. The order of testing on each side was alternated and balanced across subjects. To minimize the potential fatiguing effect, subjects were instructed to produce and maintain a constant elbow flexion force for 6 seconds in each trial. Similarly, Standard verbal encouragement was provided, but subjects did not receive visual or auditory feedback of their performance.
Data analysis
In both experiments, signals the force sensors were amplified by conditioners (484B11, PCB Piezotronics, Depew, New York), digitized by a 16-bit analog-to-digital converter (PCI-6229, National Instruments, Austin, Texas), and saved to a desktop computer running customized LabVIEW software (National Instruments, Austin, Texas). Force signals were sampled at 1,000 Hz. Data analysis was performed off-line using a customized Matlab program (MathWorks, Natick, MA). To minimize the impact of variable force propagation and release, trials were averaged from 3 to 9 seconds in Exp 1. In Exp 2, force data were averaged over a 2-second window till 0.5 second prior to the end of a 6-second trial. Usually, force was most stable visually during this period. Force measurements were normalized to individual MVCs for inter-subject comparisons.
Statistics
Descriptive statistics were used. In Exp 1, effort (i.e., relative force, % MVC) for the spontaneous push and the Borg scale levels were analyzed using one-way ANOVA with Tukey’s Post Hoc analysis. In Exp 2, A two-way ANOVA was performed to compare effort of force production between two limbs (SIDE, 2 levels, impaired vs. non-impaired) across different levels (LEVEL, 4 levels). The level of significance was set at a p-value of 0.05.
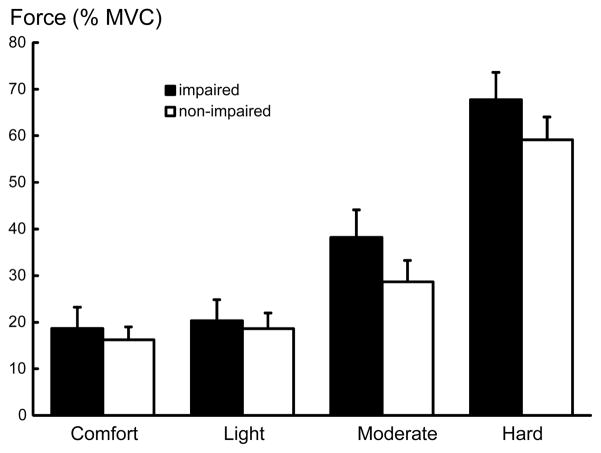
Results
In Exp 1, the average finger flexion MVC was 62.7±4.4 N with a range of 35.3 to 85 N. As shown in Figure 2, the subjects were able to maintain a relatively stable level of isometric force, even without visual feedback. The average force produced in the spontaneous push was (mean % MVC ± standard error) 12.4%±1.7. For the Borg perceptual levels average force produced at each level was: Very light 2.0%±0.3, Light 5.6%±0.9, Somewhat hard 12.8%±1.5, Hard 23.4%±2.4, and Very hard 39.0%±3.7. Subjects were able to significantly distinguish between different perceptual force levels (Figure 3), according to one-way ANOVA results (F [5,14]=43.51, p<0.01). In post-hoc Tukey’s analysis, the perceptual Borg scale levels were significantly different from one another (p<0.01), except for Somewhat hard and Light (p=0.14) and Light and Very light (p=0.82). The spontaneous push was significantly different from all other levels (p<0.01), except for Somewhat hard (p=1.00) and Light (p=0.19).
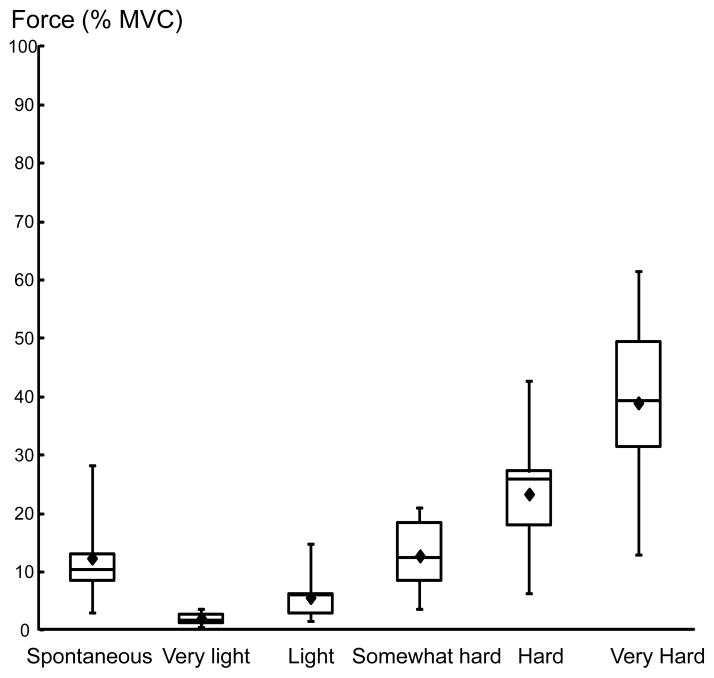
Figure 2.
Raw data from a representative subject for the spontaneous (left) and somewhat hard (right) force levels. The thin lines represent single trials and the thick lines represent the average of 6 trials for that level.
Figure 3.
Box plots of relative force (%MVC). The dots represent the mean force for each individual at that perceptual level.
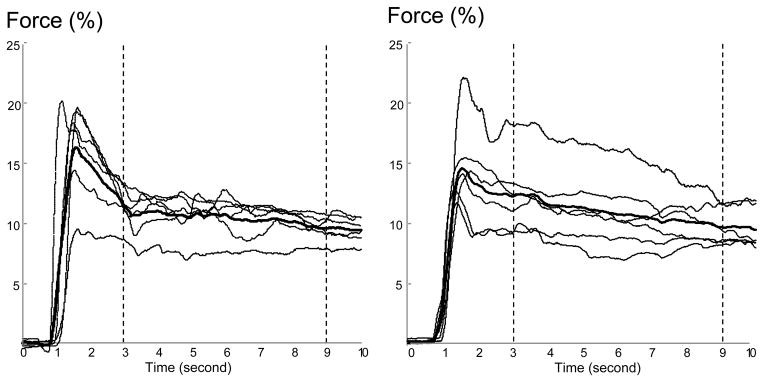
In Exp 2, the average elbow flexion MVC was 49.4±8.9N on the impaired side, 106.8±15.4N on the non-impaired side. Without visual feedback, stroke subjects were able to differentiate different levels of effort (F[3, 27]=52.803, p<0.0001) (Figure 4). Efforts for the perceptual levels of Comfort, Light, Somewhat hard (moderate) and Hard exertions were not significantly different between the impaired and non-impaired arms, specifically, they were 18.7±4.5%, 20.3±4.5%, 38.2±5.9%, and 67.7±5.9% MVC for the impaired side, and 16.2±2.8%, 18.6±3.3%, 28.7±4.6%, and 59.2±5.9%MVC for the non-impaired side. These results indicated that chronic stroke survivors were able to accurately differentiate their levels of effort during light, moderate and hard physical exertion on the impaired and non-impaired arms.
Figure 4.
averaged relative force (%MVC) at different perceptual levels on the impaired and non-impaired side. Standard error bars are shown.
Discussion
In the present study, we confirmed previous work 8,7,15–18,9 that the Borg scale could be used as a measure of perceived exertion during isometric contraction in both healthy and stroke subjects. To our knowledge, we were the first to apply more than three levels of the Borg RPE scale to isometric contraction without any visual feedback to guide subjects. This experimental design led to novel findings. In Exp 1, young and healthy subjects demonstrated that 1) when asked to self-select without visual feedback, subjects tended to exert at a “somewhat hard” level; 2) although subjects were explicitly asked to produce forces evenly distributed from 0–100%MVC on the Borg RPE scale, they produced forces ranging from 2% MVC (i.e., Very light) up to only 39%MVC (i.e., Very hard). The results suggest a reserve in perceptual levels of exertion. In Exp 2, stroke subjects were able to distinguish different levels of perceived exertion. This ability was not different between the impaired and non-impaired limb. The actual amount of force produced at the “light” level was equivalent to the force at the “comfortable” level for stroke subjects.
It is interesting in Exp 1 that the spontaneous push by healthy subjects with a self-selected amount of force fell closest to the “Somewhat hard” level. This perceptual level is only about 12% of their force ability. In cardiovascular rehabilitation, the “somewhat hard” level, or Borg 13, is clinically important, where patients are exerting themselves but still report being comfortable and able to speak11. Our study shows that this level for cardiovascular rehabilitation also applies to rating perceived exertion during isometric force production. Despite instructions to imagine the Borg RPE levels as evenly spread between no effort and MVC, healthy subjects only pushed at 39% of MVC for “Very hard”. Thus, even with encouragement to exert oneself very hard, subjects may hold as much as 60% of their strength in reserve. In contrast, earlier studies using the CR-10 Borg scale have reported strong correlations between the Borg scale and isometric hang grip forces 7–9. It is important to point out that subjects first experienced force exertion with feedback prior to subsequent force estimation tasks in these studies 7–9. Reportedly, subjects produced approximately 25% MVC for a level of 2 (“weak” or “light”) and 80% MVC for a level 7 (“very strong”) and on the CR-10 Borg scale.8 In our study, no feedback on force production was available as in most clinical settings. Surprisingly, subjects produced only 5.6% MVC for the “light” level. 23.4% MVC was reported as “Hard” in the present study. The striking difference suggests that without feedback, subjects are able to differentiate different levels of physical exertion. But these levels are not evenly distributed.
The findings that stroke subjects were able to distinguish different levels of perceived exertion and there was no difference in subjective rating of perceived exertion between the impaired and non-impaired limbs are of clinical significance. The results indicate that stroke patients could perceive their effort on the impaired side as accurately as on the non-impaired side across different levels. Clinicians could rely on patient’s subjective reports when visual feedback is not available, to encourage patients with stroke to work at relatively high RPEs, since there is growing evidence that patients with stroke receive more neuromechanical and function gains after high-intensity training19. However, because of weakness and lack of coordination of motor control in people with stroke, their work efforts at smaller %MVC levels are perceived as greater-than-normal Borg PRE levels. In young and healthy subjects, a spontaneous push at about 12.8% MVC was closest to the “Somewhat hard” level, while a “Comfortable” level was the “Light” level, about 19%MVC during elbow flexion in stroke subjects. Similarly, the actual force level was higher in stroke subjects than in healthy subjects for “Somewhat hard (moderate)” and “Hard” levels. In healthy subjects, estimation of effort has been consistent across different muscles of different strengths 20. The difference between healthy and stroke subjects may be attributable to possible sensory dysfunction in stroke subjects. It is a limitation that sensory function was not examined in the present study, though sensory impairment is common on the impaired side3. It has been shown in healthy subjects if somatosensory feedback is reduced by applying a tourniquet to one forearm, subjects overestimate their grip forces with that hand and squeeze significantly harder with the opposing hand if told to match the forces of both hands 21.
Conclusions
Both healthy and stroke subjects are able to differentiate distinct levels of perceived exertion during isometric finger or elbow flexion force when prompted with the Borg scale. Without a visual target, healthy subjects spontaneously choose to push around a “Somewhat hard” level (i.e. 12.8% MVC) while stroke subjects choose to push around a “light” level (19%MVC). There is no difference in subjective rating of perceived exertion between the impaired and non-impaired limbs in stroke subjects. These results suggest that strengthening programs need more aggressive instructions or specified targets. An efficient measure of perceived exertion, such as the Borg scale, could provide a meaningful outcome measure for rehabilitation. For example, improvement could be documented as a reduction in perceptual effort in the same task over time.
Acknowledgments
This study was supported in part by NIH grants (NIH/NINDS R01NS060774; NIH/NICHD/NCMRR R24 HD050821-08 under subcontract with Rehabilitation Institute of Chicago). The authors thank Jasper Yen, PhD for his assistance in analysis of part of the data.
References
- 1.Beaulieu-Bonneau S, Morin CM. Sleepiness and fatigue following traumatic brain injury. Sleep Med. 2012;13(6):598–605. doi: 10.1016/j.sleep.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 2.Brainin M, Pinter M. Poststroke fatigue: a hint, but no definite word on therapy yet. Stroke. 2012;43(4):933–934. doi: 10.1161/STROKEAHA.111.644856. [DOI] [PubMed] [Google Scholar]
- 3.Sullivan JE, Hedman LD. Sensory dysfunction following stroke: incidence, significance, examination, and intervention. Top Stroke Rehabil. 2008;15(3):200–217. doi: 10.1310/tsr1503-200. [DOI] [PubMed] [Google Scholar]
- 4.Borg E, Kaijser L. A comparison between three rating scales for perceived exertion and two different work tests. Scand J Med Sci Sports. 2006;16(1):57–69. doi: 10.1111/j.1600-0838.2005.00448.x. [DOI] [PubMed] [Google Scholar]
- 5.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 6.Braverman DL. Cardiac rehabilitation: a contemporary review. Am J Phys Med Rehabil. 2011;90(7):599–611. doi: 10.1097/PHM.0b013e31821f71a6. [DOI] [PubMed] [Google Scholar]
- 7.Spielholz P. Calibrating Borg scale ratings of hand force exertion. Appl Ergon. 2006;37(5):615. doi: 10.1016/j.apergo.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 8.Li KW, Yu R. Assessment of grip force and subjective hand force exertion under handedness and postural conditions. Appl Ergon. 2011;42(6):929–933. doi: 10.1016/j.apergo.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Buchholz B, Park JS, Gold JE, Punnett L. Subjective ratings of upper extremity exposures: inter-method agreement with direct measurement of exposures. Ergonomics. 2008;51(7):1064–1077. doi: 10.1080/00140130801915220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park WH, Leonard CT, Li S. Perception of finger forces within the hand after index finger fatiguing exercise. Exp Brain Res. 2007;182(2):169–177. doi: 10.1007/s00221-007-0978-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park WH, Leonard CT, Li S. Finger force perception during ipsilateral and contralateral force matching tasks. Exp Brain Res. 2008;189(3):301–310. doi: 10.1007/s00221-008-1424-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kruger ES, Hoopes JA, Cordial RJ, Li S. Error compensation during finger force production after one- and four-finger voluntarily fatiguing exercise. Exp Brain Res. 2007;181(3):461–468. doi: 10.1007/s00221-007-0942-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li S. Perception of individual finger forces during multi-finger force production tasks. Neurosci Lett. 2006;409(3):239–243. doi: 10.1016/j.neulet.2006.09.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang S-H, Francisco GE, Zhou P, Rymer WZ, Li S. Weakness, spasticity, force variability and spontaneous motor unit discharges of resting spastic-paretic biceps brachii in chronic stroke. Muscle & Nerve. doi: 10.1002/mus.23699. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pincivero DM. Older adults underestimate RPE and knee extensor torque as compared with young adults. Med Sci Sports Exerc. 2011;43(1):171–180. doi: 10.1249/MSS.0b013e3181e91e0d. [DOI] [PubMed] [Google Scholar]
- 16.Pincivero DM, Coelho AJ, Campy RM. Perceived exertion and maximal quadriceps femoris muscle strength during dynamic knee extension exercise in young adult males and females. Eur J Appl Physiol. 2003;89(2):150–156. doi: 10.1007/s00421-002-0768-0. [DOI] [PubMed] [Google Scholar]
- 17.Pincivero DM, Coelho AJ, Campy RM. Gender differences in perceived exertion during fatiguing knee extensions. Med Sci Sports Exerc. 2004;36(1):109–117. doi: 10.1249/01.MSS.0000106183.23941.54. [DOI] [PubMed] [Google Scholar]
- 18.Woods S, Bridge T, Nelson D, Risse K, Pincivero DM. The effects of rest interval length on ratings of perceived exertion during dynamic knee extension exercise. J Strength Cond Res. 2004;18(3):540–545. doi: 10.1519/1533-4287(2004)18<540:TEORIL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Patten C, Condliffe EG, Dairaghi CA, Lum PS. Concurrent neuromechanical and functional gains following upper-extremity power training post-stroke. J NeuroEng Rehab. doi: 10.1186/1743-0003-10-1. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jones LA. Perceptual constancy and the perceived magnitude of muscle forces. Exp Brain Res. 2003;151(2):197–203. doi: 10.1007/s00221-003-1434-4. [DOI] [PubMed] [Google Scholar]
- 21.Takarada Y, Nozaki D, Taira M. Force overestimation during tourniquet-induced transient occlusion of the brachial artery and possible underlying neural mechanisms. Neurosci Res. 2006;54(1):38–42. doi: 10.1016/j.neures.2005.10.004. [DOI] [PubMed] [Google Scholar]