Abstract
Objectives
Millions of U.S. adults are recipients of the high school equivalency (GED) diploma. Virtually nothing is known about the health of this large group, although literature suggests GED recipients are considerably worse off than high school graduates in numerous economic and social outcomes. We analyze general health among working-age adults with a high school diploma, GED recipients, and high school dropouts.
Methods
Ordered and binary logistic models of self-rated health and activity limitations were estimated using data from the 1997–2009 National Health Interview Surveys (N=76,703).
Results
GED recipients have significantly and substantially worse health than high school graduates, among both sexes. In fact, the GED recipients’ health is generally comparable to that of high school dropouts. Health behaviors and economic factors explain a large proportion of the difference but the gap remains significant.
Conclusions
In terms of health, adults with a terminal GED are not equivalent to high school graduates. GED recipients report considerably worse general health and activity limitations. The disadvantage is only partly due to the worse economic outcomes and health behaviors; a significant difference remains unexplained and may be due to other, unobserved pathways, or to selection mechanisms.
Over 17 million adults have earned the General Education Development (GED) diploma since its inception (American Council on Education 2009). In recent years, over half a million GEDs have been awarded annually, representing over 10% of all secondary degrees (Snyder and Dillow 2011; Heckman, Humphries, and Mader 2010). The GED is referred to as the high school equivalency diploma, under the assumption that GED recipients have comparable knowledge and skills as regular high school graduates. For instance, the Census and the National Center for Education Statistics do not distinguish the GED and high school diplomas in tabulating the educational attainment of U.S. adults.
Over the past two decades, however, education researchers and econometricians have accumulated persuasive evidence that the GED is associated with significantly worse labor market outcomes compared to high school diplomas (Cameron and Heckman 1993; Tyler 2003; Heckman and LaFontaine 2006; Heckman, Humphries, and Mader 2010; Heckman and Rubinstein 2001; Murnane, Willett, and Boudett 1997). In employment rates, wages, and other economic indicators, adults with a terminal GED were often found to be comparable to high school dropouts rather than regular high school graduates.
In population health research, much attention has been paid to the gradients in health outcomes by education in general (Ross and Mirowsky 1999; Herd 2010; Mirowsky and Ross 2003). Little is known, however, about how the two secondary credentials, GED and a regular high school diploma, translate into adult health. Is it justifiable to consider GED recipients as equivalent to high school graduates in terms of health? The health gradient literature would suggest so: different levels of education are known to be associated with correspondingly different levels of health; we could assume that two equivalent educational credentials might be associated with equivalent levels of health. Among the few papers that compared the two secondary-schooling credentials, however, there is some disagreement. A 2005 study of about 2,000 adults aged 40–45 found no significant differences between HS and GED with respect to self-reported and physician-reported illnesses (Caputo 2005). In contrast, a recent paper using a nationally-representative sample of adults aged 25 and above found that GED recipients had higher mortality than HS graduates, especially among younger birth cohorts (Rogers et al. 2010). For emotional health, GED was found associated with higher rates of depressive symptoms compared to a regular diploma among inner-city youth (Ou 2008).
Ours is the first study to focus in depth on the general health among HS graduates and GED recipients. These two groups represent millions of U.S. adults who are assumed to be comparable in their skills and thus presumably also obtain equivalent returns to their credentials in terms of outcomes like health.
THE GED AND ITS RECIPIENTS
The GED is an examination-based credential, consisting of five tests (science, reading, writing, social studies and science/mathematical skills). The credential is intended to certify that its recipients have cognitive skills and knowledge comparable to those of high school graduates (Heckman, Humphries, and Mader 2010; Tyler 2005). The GED was created in 1942 to enable young WWII veterans who interrupted their secondary education when they enrolled in the military to complete high school requirements (Tyler 2005). Over the following decades, the proportion of young adults who completed secondary education via the GED exam rather than the high school diploma has systematically increased (Heckman 2008). In recent years, up to 18% of young adults who completed high school did so via the GED (Heckman, Humphries, and Mader 2010).
In varied outcomes, GED recipients differed significantly from regular high school graduates. Although the GED is widely accepted as a satisfactory prerequisite for college admission, relatively few GED recipients enroll in and graduate from 4-year colleges (Heckman, Humphries, and Mader 2010). GED earners also appear to drop out of the military at much higher rates than conventional HS graduates (i.e., see Heckman and LaFontaine 2010; Boesel 1998). Ou (2008) examined a range of outcomes among inner-city youth, including incarceration, childbearing, life satisfaction, and substance use. She found a ‘gradient’ where high school dropouts fared worse than GED recipients, who in turn fared considerably worse than high school graduates. Caputo (2005) found a similar gradient with respect to depression in a study of mid-life adults.
PATHWAYS FROM EDUCATION TO HEALTH
Among the explanatory factors that link education and health outcomes, two stand out as important factors in the general literature, and specifically in the GED-HS comparison: economic status and health behaviors. The economic resources include higher income, greater wealth, and more stable employment, all of which are associated with better health (Adams et al. 2003; Backlund, Sorlie, and Johnson 1996; Elo, Martikainen, and Smith 2006; Sorlie and Rogot 1990). Health behaviors comprise a rich set of lifestyle factors: higher education is often associated with more exercise, moderate alcohol intake, less obesity, and less smoking (Cowell 2006; Lantz et al. 1998).
In the economics literature, studies have consistently reported that relative to regular HS graduates, GED recipients have substantially worse outcomes in employment, hourly wages, income, and other labor-market indicators (Cameron and Heckman 1993; Heckman and LaFontaine 2006; Heckman and Rubinstein 2001; Clark and Jaeger 2006; Tyler 2005; Caputo 2005). The comparison between GED recipients and other dropouts without the credential has been more inconsistent, with some (but not all) studies reporting a significant benefit of the GED for wages and earnings (Heckman and LaFontaine 2006; Heckman, Humphries, and Mader 2010; Tyler 2003).
Literature that has explicitly compared health behaviors between high school graduates and persons who have received GEDs is modest but motivates their inclusion in our analyses. With respect to smoking, high school graduates have been found to have significantly lower rates than GED earners, who were at best only marginally less likely to smoke than HS dropouts (Kenkel, Lillard, and Mathios 2006; Ou 2008; Barbeau, Krieger, and Soobader 2004). No significant differences between these three educational groups were found in being overweight (Kenkel, Lillard, and Mathios 2006). Although not traditionally conceptualized as a key health behavior, substance abuse was also reported more frequently among GED recipients than standard graduates (Ou 2008).
RESEARCH QUESTIONS
The study is organized around three questions: (1) How large are the differences in self-rated health (SRH) and activity limitations among persons with GED certificates and high school diplomas? (2) Can the observed gross differences be explained by health behaviors and labor-market characteristics of the GED and HS graduates? (3) Do the results hold for major demographic groups?
DATA AND METHOD
DATA SOURCE AND ANALYTIC SAMPLE
The analyses are based on data collected in the National Health Interview Surveys (NHIS) from 1997 to 2009. The NHIS consists of annual surveys conducted since 1957; information is collected in face-to-face interviews by the National Center for Health Statistics (NCHS). NHIS uses a complex sampling design to obtain a sample representative of the civilian non-institutionalized U.S. population. In 1997, the NHIS underwent a major redesign that included a new way of collecting education information. Prior to 1997, education was collected in completed years of schooling, so GED and high school graduates were coded identically, as 12 years of education. Since the redesign, these two credentials have been recorded separately. We obtained the data via the Integrated Health Interview Surveys (IHIS), an aggregated source of the NHIS compiled by the Minnesota Population Center (2008).
We defined the analysis sample as U.S.-born adults age 30 to 65 who reported their highest level of educational achievement as 9–12 years (high school dropouts), GED, or a high school diploma. We included high school dropouts because they are roughly comparable to the average years of schooling reported by GED recipients in other surveys – about 10 years (Tyler 2005). Respondents who reported having achieved any postsecondary education or less than 9 years of education were not pertinent to the analyses and therefore excluded from the sample. As a side note, the health of these excluded educational categories followed the gradient: those with 0–8 years of schooling had worse health and more limitations than high school dropouts, and respondents with postsecondary education had better health and fewer limitations. Results are available on request; alternatively, recent studies have reviewed general health across the educational spectrum (Zajacova, Hummer, and Rogers 2012). Foreign-born respondents were excluded because of potential confounding of the age at immigration and region of origin for our research questions. The age range, 30–65 years, was intended to capture working-age population, before the ages when transition to retirement and mortality selection complicate drawing conclusions from model findings. Two respondents from this group were missing both health outcomes and were also excluded; our final sample size was 76,703 respondents.
VARIABLES
Information about education was asked in terms of completed years of schooling for respondents with less than a high school degree and in terms of attained credentials for those with at least a high school completion or alternatives. During the interview, respondents were handed a card with all educational categories and asked to place themselves in the appropriate category. We focused on a subset of adults who reported 9–12 years of schooling (high school dropouts), GED, or a high school diploma as their highest schooling level.
The two measures of health were self-rated health (SRH) and activity limitations. SRH was ascertained with a question “Would you say your health in general is excellent, very good, good, fair, or poor?” The variable is used in analyses as the original 5-category health outcome; for the figure it is collapsed into a binary response, coded 1 for fair or poor health and 0 otherwise. Activity limitation indicated whether the respondent had any limitations versus none (reference). This variable was constructed within NHIS from seven questions that focused on specific limitations, comprising 1) needing help with personal care needs like eating or bathing, 2) needing help with routing needs like household chores, 3) health problems keeping a respondent from working, 4) health problems limiting the kind or amount of work, 5) difficulty walking, 6) difficulty remembering, and 7) limitations in any other activities.
Basic demographic variables included age (measured in single years and centered on the mean age of 47 years), sex (male=reference), and race/ethnicity (non-Hispanic white=reference, non-Hispanic black, Hispanic, and ‘other’). Census region of residence was coded as Northeast, North Central, South (reference), and West.
For the following variables, the reference was chosen to reflect the most advantageous category as it likely related to health outcomes. Marital status was coded as married (reference), widowed, divorced or separated, and never married. Health insurance was categorized as insured (reference) versus not insured. Economic status was captured by two variables: the respondent’s family poverty-income ratio and own employment status. The poverty-income ratio was defined as the ratio of a family’s income to the federally-defined poverty threshold, taking into account household composition. The variable was categorical, with levels from “under 0.5” for a family with income less than half the poverty threshold, up to “5 and over” for a family with income 5 or more times the threshold. We recoded the variable into the median value of each category and used it as a continuous predictor of health. Employment status was a nominal variable coded as employed (reference), unemployed, or not in labor force.
Finally, we included three predictors to capture health behaviors: smoking, alcohol use, and obesity. Smoking was categorized as never (reference), former, and current smoker. Alcohol use was coded as never, former use, and current use (reference). Body size was captured using the body mass index (BMI), calculated from self-reported height and weight, and used in models as a dichotomous indicator coded as non-obese (reference) versus obese (BMI ≥ 30).
ANALYSIS
First, univariate and bivariate descriptive analyses were used to examine the distribution of the variables individually and across the three education groups. Variables with significant differences across schooling categories were particularly likely to be important explanatory factors in the multivariate models. Second, we estimated a series of nested ordered logistic models of SRH and logistic models of activity limitations. Each series comprised four models; the first model controlled for age, sex, and race; the second model added marital status, region, and access to health care. The next models added the major explanatory pathways linking education and health: economic resources and health behaviors. Third, we estimated the baseline models separately by age (30–45 and 46–65 years), sex, and race/ethnicity (non-Hispanic white, non-Hispanic black, and Hispanic). The purpose of these stratified models was to examine to what degree the all-sample findings hold for demographic subgroups, an important validity check given that the effect of education on health in general is known to vary by age, sex, and race (Hill and Needham 2006; Liu and Hummer 2008; Dupre 2008).
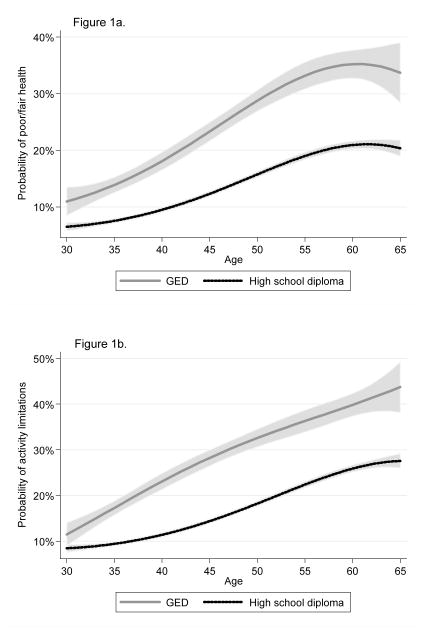
In order to provide a clear visual impression of the health differences between high school and GED credentials, we calculated predicted probability of fair/poor health and activity limitations by age for GED and high school diploma recipients. The probabilities were calculated from age, sex, and race-adjusted logistic models of each outcome. In order to allow the data to reveal the actual shape of the likelihood of an outcome by age, we fitted each model using age, age squared, age cubed, as well as the interactions of these age terms with the GED dummy.
There were no missing data on basic demographic variables. For all categorical control variables from marital status to health behaviors, we included a category of “unknown.” Most variables had a low proportion of missing observations, ranging 0.2% for employment status to 4.8% for obesity information. The poverty-income ratio was the only predictor with a high proportion missing values (20%). We imputed them using a regression-based imputation. To establish how robust the findings were to different methods of dealing with the missingness on income, we also estimated models using categorized income with a missing category, and models where adults with missing income were dropped. These different specifications yielded comparable results (all are available on request).
Additional validity checks included testing the proportional odds assumption for the ordered logistic model of SRH. The global tests (both Brant Wald test and the approximate likelihood ratio test) were significant, indicating violation of the proportional odds assumptions. The Brant test for the primary coefficient of interest, for GED versus HS diploma, however, had p-value=.83, indicating that the coefficient was statistically identical across all binary equations. Since these tests are not available for data collected using the complex sampling design, their findings are difficult to interpret. We have therefore also estimated models of dichotomized SRH (fair/poor versus excellent to good), obtaining comparable findings. The results are available on request. All analyses adjusted for complex sampling design using svy suite of commands in Stata 11.0.
RESULTS
Among adults in the analysis sample, 70% were high school graduates, about 8% had a GED, and 22% dropped out of high school without a credential. Just over half the respondents reported excellent or very good health; 18% had fair or poor health. About one in five adults reported some activity limitations. There was considerable variation across the three educational groups in both health outcomes and most control variables. The direction of the differences was as expected; a more unexpected pattern was that the GED recipients resembled high school dropouts more than high school graduates. For instance, both GED recipients and dropouts were substantially more likely than graduates to be in fair or poor health, have activity limitations, be unmarried, uninsured, unemployed, have low income, and smoke.
The descriptive analyses suggested health differences among the educational groups. Tables 2 and 3 show the differences in a multivariate context, taking into account the different distribution of explanatory factors among the three education groups. The results were similar for SRH and activity limitations so we comment on both sets of results together. Controlling for key demographic variables in Model 1, we obtained a startling finding: adults with a GED, assumed to be equivalent to the HS credential, had significantly and substantially worse health compared to high school graduates: they were about twice as likely as high school graduates to report ‘worse’ health and activity limitations. In fact, GED recipients were only slightly better off than dropouts in self-rated health and statistically indistinguishable from dropouts in activity limitations (see notes to Tables 2 and 3).
Table 2.
Ordered logistic models of SRH on select predictors, NHIS 1997–2009 (N=76,636).
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Education (ref.=HS diploma) | ||||
| HS dropouts | 2.14*** | 2.05*** | 1.56*** | 1.45*** |
| GED | 1.96*** | 1.88*** | 1.55*** | 1.39*** |
| Control variables | ||||
| Age | 1.04*** | 1.04*** | 1.03*** | 1.03*** |
| Female | 1.11*** | 1.12*** | 0.90*** | 0.92*** |
| Race/ethnicity (ref.=NH white) | ||||
| Black | 1.57*** | 1.38*** | 1.17*** | 1.17*** |
| Hispanic | 1.12*** | 1.14*** | 1.06 | 1.09* |
| Other | 1.39*** | 1.36*** | 1.19** | 1.12 |
| Year of interview | 1.03*** | 1.03*** | 1.03*** | 1.02*** |
| Marital status (ref.=married) | ||||
| Widowed | 1.20*** | 0.88*** | 0.88*** | |
| Divorced | 1.41*** | 1.24*** | 1.22*** | |
| Never married | 1.48*** | 1.17*** | 1.18*** | |
| Unknown | 1.03 | 0.85* | 0.88 | |
| Region (ref.=South) | ||||
| Northeast | 0.84*** | 0.86*** | 0.87*** | |
| North Central | 0.94** | 0.96 | 0.95* | |
| West | 0.82*** | 0.81*** | 0.84*** | |
| Health insurance (ref.=insured) | ||||
| Uninsured | 1.10*** | 0.90*** | 0.91*** | |
| Unknown | 1.17 | 0.99 | 1.02 | |
| Economic factors | ||||
| Family income | 0.80*** | 0.82*** | ||
| Employment (ref.=employed) | ||||
| Unemployed | 1.29*** | 1.27*** | ||
| Not in LF | 2.79*** | 2.71*** | ||
| Unknown | 0.98 | 1.06 | ||
| Body weight (ref=not obese) | ||||
| Obese | 1.88*** | |||
| Unknown | 1.51*** | |||
| Smoking (ref.=never smoked) | ||||
| Past smoker | 1.23*** | |||
| Current smoker | 1.72*** | |||
| Unknown | 1.19 | |||
| Alcohol use (ref.=current use) | ||||
| Never | 1.20*** | |||
| Former | 1.48*** | |||
| Unknown | 1.09 | |||
| Cutpoints | ||||
| 1 | −1.03 | −0.97 | −1.81 | −1.22 |
| 2 | 0.44 | 0.51 | −0.25 | 0.37 |
| 3 | 1.99 | 2.08 | 1.46 | 2.13 |
| 4 | 3.52 | 3.62 | 3.11 | 3.81 |
p<.05,
p<.01,
p<.001
When we re-estimate these models with GED as the omitted education category, the results show that HS dropouts have 9% higher odds of ‘worse’ health than GED recipients in Models 1 and 2 (p<.01); there are no significant difference between GEDs and dropouts in Models 3 and 4.
Table 3.
Logistic models of activity limitations on select predictors (N=76,564).
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Education (ref.=HS diploma) | ||||
| HS dropouts | 2.10*** | 2.06*** | 1.26*** | 1.17*** |
| GED | 2.09*** | 2.04*** | 1.48*** | 1.35*** |
| Control variables | ||||
| Age | 1.05*** | 1.05*** | 1.03*** | 1.03*** |
| Female | 1.04 | 1.03 | 0.67*** | 0.68*** |
| Race/ethnicity (ref.=NH white) | ||||
| Black | 1.27*** | 1.05 | 0.77*** | 0.77*** |
| Hispanic | 0.89** | 0.82*** | 0.69*** | 0.71*** |
| Other | 1.51*** | 1.35*** | 1.08 | 1.01 |
| Year of interview | 1.02*** | 1.02*** | 1.02*** | 1.01** |
| Marital status (ref.=married) | ||||
| Widowed | 1.93*** | 1.35*** | 1.38*** | |
| Divorced | 2.04*** | 1.91*** | 1.92*** | |
| Never married | 2.55*** | 1.87*** | 1.94*** | |
| Unknown | 1.32* | 1.06 | 1.21 | |
| Region (ref.=South) | ||||
| Northeast | 0.97 | 1.03 | 1.03 | |
| North Central | 1.05 | 1.14*** | 1.13*** | |
| West | 1.16*** | 1.18*** | 1.21*** | |
| Health insurance (ref.=insured) | ||||
| Uninsured | 0.74*** | 0.58*** | 0.59*** | |
| Unknown | 0.64 | 0.46** | 0.50** | |
| Economic factors | ||||
| Family income | 0.71*** | 0.73*** | ||
| Employment (ref.=employed) | ||||
| Unemployed | 1.84*** | 1.85*** | ||
| Not in LF | 8.05*** | 7.95*** | ||
| Unknown | 0.69 | 0.80 | ||
| Body weight (ref=not obese) | ||||
| Obese | 1.64*** | |||
| Unknown | 1.35*** | |||
| Smoking (ref.=never smoked) | ||||
| Past smoker | 1.28*** | |||
| Current smoker | 1.54*** | |||
| Unknown | 0.99 | |||
| Alcohol use (ref.=current use) | ||||
| Never | 1.19*** | |||
| Former | 1.72*** | |||
| Unknown | 0.96 | |||
p<.05,
p<.01,
p<.001
When we re-estimate these models with GED as the omitted education category, the results show that HS dropouts and GEDs are not significantly different in Models 1 and 2; the dropout group actually has significantly lower odds of limitations than GED recipients (OR=.85, p<.001 in Model 3; OR=.87, p<.01 in Model 4).
Figure 1 illustrates how the relative differences between HS graduates and GED recipients translate into absolute inequalities. The predicted probabilities of fair/poor self-assessed health and activity limitations by age showed an enormous health gap. Best expressed in age equivalents, 30-year-old GED recipients have health similar to that of HS graduates in their early 40s; when the GED recipients are about 42–43 years old, their health is comparable to that of 60-year-old HS graduates.
Figure 1.
Figure 1a. Predicted Probability of Poor or Fair Health, by Age
Figure 1b. Predicted Probability of Activity Limitations, by Age
Adjusting for region of residence and marital status in the second model in Tables 2 and 3 explained relatively little of the HS-GED differential: GED recipients remained about twice as likely to report ‘worse’ health and activity limitations, compared to HS graduates.
Economic status, added in Model 3, explained a much larger proportion of the HS-GED difference. The odds ratio decreased to 55% higher odds of ‘worse’ health from 88% and 48% higher odds of reporting a limitation for GED recipients relative to high school graduates from 204%, a reduction of 30–45% of the GED disadvantage from the previous model. Finally, health behaviors were also significant predictors of health, and further attenuated the HS-GED inequality. However, the differences remained significant: in Model 4, taking into account multiple potential confounders and mediators, GED recipients still reported 35–39% higher odds of worse health outcomes relative to HS graduates, a significant and considerable disadvantage.
A consistent finding across all models and both outcomes was that that the GED earners were more similar to high school dropouts than graduates. Adjusted for economic outcomes and health behaviors, adults with a GED and high school dropouts were statistically identical in terms of their self-reported health; for activity limitations, high school dropouts actually reported 13% lower odds of any limitations than adults with a GED (p<.001).
Table 4 summarizes the GED-HS differences in major demographic subgroups. The key finding was that the difference between graduates and the two other education groups was consistent in direction and significance across all demographic groups: GED recipients had worse health and more functional limitations than graduates. The health gap between HS and GED was marginally larger for older adults and women in SRH and for younger adults and men in activity limitations. Auxiliary interaction models (available on request) showed that these differences were not statistically significant. Racial/ethnic differences in the HS-GED gap were more pronounced, reaching statistical significance in the interaction models. For both health outcomes, the gap was largest among whites, smaller among Hispanics, and smallest among black adults. This variation may occur either because black and Hispanic adults gain less from a HS diploma than whites, or because they are penalized less for having a GED than white adults.
Table 4.
Models of self-rated health and activity limitations on education, for total sample and by demographic subpopulations, NHIS 1997–2009.
| By age
|
By sex
|
By race/ethnicity
|
|||||
|---|---|---|---|---|---|---|---|
| 30–45 | 46–65 | Men | Women | White | Black | Hispanic | |
| A. Self-rated health | |||||||
| Education (ref.=HS diploma) | |||||||
| 9–12 | 2.07*** | 2.20*** | 2.02*** | 2.24*** | 2.23*** | 1.82*** | 1.89*** |
| GED | 1.89*** | 2.02*** | 1.90*** | 2.00*** | 2.14*** | 1.45*** | 1.52*** |
| B. Activity limitations | |||||||
| Education (ref.=HS diploma) | |||||||
| 9–12 | 2.14*** | 2.09*** | 1.98*** | 2.21*** | 2.14*** | 1.88*** | 2.19*** |
| GED | 2.20*** | 2.00*** | 2.09*** | 2.07*** | 2.18*** | 1.63*** | 2.14*** |
p<.05,
p<.01,
p<.001
U.S.-born adults age 30–65, NHIS 1997–2009. The models also controls for age, and interview years, as well as sex and race/ethnicity in those models not stratified on these predictors. Adjusted for sampling design.
DISCUSSION
For nearly 70 years, the GED has existed as an alternative to a regular high school diploma, predicated on the equivalence between the two credentials. We asked whether these two credentials translated into equivalent health among working-age adults. Other outcomes of GED recipients have been studied for two decades, primarily focusing on labor market outcomes (Heckman and LaFontaine 2010; Cameron and Heckman 1993). Despite calls for extending the comparison of GED and high school diplomas to other areas (Tyler 2003), no previous study analyzed the general health of GED recipients and high school graduates. Using nationally-representative NHIS data, we showed that GED recipients face a substantial health disadvantage compared to high school graduates. The supposedly equivalent GED credential is associated with about twice the odds of self-reported ‘worse’ health and physical limitations than a high school diploma. This relative difference is even more clearly illustrated using absolute differentials. Adults with GEDs have health comparable to high school graduates who are up to 20 years older. In fact, GED recipients are not only systematically worse off than their high school (HS) graduate peers, but they appear worse off than high school dropouts.
The gross HS-GED difference is partly due to the lower income and employment, as well as worse lifestyle profile, of the latter group. Controlling for these mediating factors, the difference between GED and HS decreases; however, it remains significant and substantively large in both SRH and functional limitations. The explanatory inputs of economic and lifestyle variables corroborates the literature, which has established that the GED is associated with worse outcomes ranging from employment, wages, college attendance and completion, military retention, life satisfaction, depression, and smoking (Tyler and Lofstrom 2010; Kenkel, Lillard, and Mathios 2006; Ou 2008; Heckman, Humphries, and Mader 2010; Caputo 2005).
On the other hand, our findings differ from the literature in one crucial aspect. Some previous studies reported that GED recipients had advantage over high school dropouts in various educational and social outcomes (Caputo 2005; Tyler 2003; Boesel, Alsalam, and Smith 1998); we found the opposite for health outcomes. With respect to general health, GED recipients appear consistently worse than high school dropouts -- a finding that held across population subgroups and taking into account varied explanatory factors. A possible exception to these patterns occurs among black and Hispanic adults, where differences among the three educational categories were smaller than among whites. Some theorists might find this pattern consistent with expectations: racial/ethnic minorities face racism and discrimination that impedes their ability to convert higher education into other resources, including health (Williams 1997; Williams and Collins 1995). Empirical studies, however, tend to report that the effect of schooling on health is comparable for whites and blacks, or that the black disadvantage is “slight” (Zajacova 2006; Cutler and Lleras-Muney 2008). One reason for the apparent similarity might be gleaned from Christenson and Johnson’s (1995) study, which found that black adults benefited less than whites from schooling at the postsecondary level, but more at the pre-secondary to secondary level, the range we studied here.
The key question is why do the high school equivalents have such ‘non-equivalent’ health. Although our data and study design did not permit a causal analysis, we can draw on several theoretical perspectives to speculate about the findings. One explanation of the striking disadvantage of GED recipients might draw on the human capital theory, in particular its conceptualization within the health literature (Becker 1964; Ross and Mirowsky 1999). Human capital comprises both cognitive skills like writing, reading, and quantitative reasoning, and non-cognitive skills. Noncognitive factors comprise a psychological traits like the ability to defer gratification (Mischel, Shoda, and Rodriguez 1989), time preference (Barsky et al. 1997), self-control (Tangney, Baumeister, and Boone 2004), self-efficacy (Bandura 1986), personal control (Mirowsky and Ross 1998), and numerous other factors.
These non-cognitive characteristics have been linked to important outcomes, including health. For instance, Mirowsky and Ross (1998, 2003) suggest that education affects health by increasing the sense of personal control, a non-cognitive skill, which promotes a healthy lifestyle via persistence and active decisions about appropriate health behaviors. Thus, social epidemiologists have already considered how education and health may be linked via non-cognitive skills. With respect to the HS-GED comparison, Heckman and colleagues (Heckman and Rubinstein 2001; Heckman, Humphries, and Mader 2010; Heckman 2008) have shown that the cognitive skills of GED and HS diploma earners are comparable; however, they posit that the GED recipients have considerably weaker non-cognitive skills. If the GED recipients have personality characteristic that influence their time preference or the ability to defer gratification (Mischel, Shoda, and Rodriguez 1989; Barsky et al. 1997), their life choices may generally lead to a trajectory that is less optimal for health, whether via jobs, relationships, social support, or general lifestyles that may negatively impact their health in adulthood.
Given the importance of non-cognitive skills in explaining the differences among the education groups, an obvious limitation of this study is an absence of direct measures of non-cognitive characteristics. The next step in untangling the relationship between educational credentials and health depends on the availability of data, which needs to include health outcomes, detailed educational information, and valid measures of non-cognitive skills. We hope that the increasing awareness of the high-risk status of the GED recipients will help add non-cognitive measures to educational and health surveys, and conversely that existing surveys will add information about GED diploma as a separate educational category.
Another limitation concerns the self-reported nature of the health outcomes. We cannot isolate the underlying latent health differences from possible reporting biases: if adults with a GED report their health as worse, given some true level of health, compared to high school graduates, the differences we described would be biased upward. There is now a growing literature examining group differences in how respondents form health judgment (Dowd and Zajacova 2010; Subramanian, Huijts, and Avendano 2010; Zajacova and Dowd 2011; Crossley and Kennedy 2002). It is becoming clear that there are groups differences in self-ratings of health but it is not yet clear to what degree or even in what direction they may affect our research on health disparities. It is also helpful to keep in mind that there is extensive literature that has repeatedly found high predictive and concurrent validity of SRH (Mossey and Shapiro 1982; Idler, Russell, and Davis 2000; Bailis, Segall, and Chipperfield 2003).
Our findings extend economic and educational literatures, which previously documented the non-equivalent outcomes of GED recipients in labor market and other early-adulthood outcomes, to health. The substantial health gap between adults with a GED versus a high school diploma has both policy and research implications. In terms of health policy, the GED group comprises millions of adults in the United States. It is clear that their health is considerably worse than would be implied by their supposed equivalence to their HS diploma peers; consequently they may require earlier medical interventions and more health-care resources in the coming decades. In terms of research, the findings suggest that we need to exercise caution when putting adults with GED and HS diploma on equal footing in our studies. These two groups do not have comparable health, and ignoring this fact might bias findings and lead to erroneous conclusions about population health inequalities.
Table 1.
Characteristics of the analysis sample, by education (N=76,703).
| Education | 9–12 years | GED | High school grad. | Total |
|---|---|---|---|---|
| 9–12 years (dropouts) | 22.1% | |||
| GED | 7.9% | |||
| High school graduates | 70.0% | |||
| Health (N=76,636) | ||||
| Excellent | 14.7% | 15.2% | 23.6% | 21.0% |
| Very good | 23.3% | 26.8% | 33.4% | 30.6% |
| Good | 33.1% | 33.8% | 29.3% | 30.5% |
| Fair | 20.1% | 17.1% | 10.5% | 13.2% |
| Poor | 8.8% | 7.1% | 3.2% | 4.8% |
| Activity limitations (N=76,564) | ||||
| No activity limitations | 69.9% | 72.1% | 83.3% | 79.4% |
| Any activity limitations | 30.1% | 27.9% | 16.7% | 20.6% |
| Control variables | ||||
| Age -- mean (s.e.) | 47.5 (.09) | 45.7 (.15) | 47.0 (.05) | 47.0 (.04) |
| Female | 53.4% | 51.7% | 53.8% | 53.6% |
| Marital status | ||||
| Married | 44.8% | 46.8% | 56.0% | 52.8% |
| Widowed | 6.6% | 4.8% | 4.4% | 4.9% |
| Divorced | 29.2% | 32.7% | 24.6% | 26.2% |
| Never married | 18.8% | 15.1% | 14.5% | 15.5% |
| Unknown | 0.6% | 0.5% | 0.6% | 0.6% |
| Race/ethnicity | ||||
| Non-Hispanic white | 67.0% | 78.5% | 80.8% | 77.6% |
| Non-Hispanic black | 23.8% | 12.5% | 13.8% | 15.9% |
| Hispanic | 7.5% | 7.1% | 4.1% | 5.1% |
| Other | 1.8% | 2.0% | 1.3% | 1.5% |
| Geographic region | ||||
| Northeast | 15.2% | 14.7% | 19.3% | 18.1% |
| North Central | 22.8% | 25.0% | 29.5% | 27.7% |
| South | 47.6% | 44.0% | 37.1% | 39.9% |
| West | 14.4% | 16.4% | 14.0% | 14.3% |
| Health insurance | ||||
| Uninsured | 23.9% | 23.1% | 14.6% | 17.4% |
| Insured | 75.8% | 76.6% | 85.0% | 82.3% |
| Unknown | 0.3% | 0.3% | 0.3% | 0.3% |
| Employment | ||||
| Employed | 55.3% | 63.2% | 72.6% | 68.0% |
| Unemployed | 4.5% | 5.6% | 2.7% | 3.3% |
| Not in LF | 40.1% | 31.2% | 24.5% | 28.5% |
| Unknown | 0.1% | 0.1% | 0.2% | 0.2% |
| Income-to-poverty ratio | ||||
| Continuous | 2.2 | 2.5 | 3.3 | 3.0 |
| Categorized | ||||
| Low | 51.6% | 49.2% | 29.9% | 36.2% |
| Mid | 19.8% | 23.2% | 28.5% | 26.1% |
| High | 9.6% | 11.4% | 21.0% | 17.7% |
| Unknown | 19.0% | 16.2% | 20.7% | 20.0% |
| Body weight | ||||
| Not obese | 63.3% | 63.5% | 66.8% | 65.7% |
| Obese | 32.6% | 32.3% | 28.2% | 29.5% |
| Unknown | 4.1% | 4.3% | 5.0% | 4.8% |
| Smoking | ||||
| Never smoked | 32.5% | 24.7% | 44.9% | 40.5% |
| Past smoker | 20.8% | 22.9% | 22.6% | 22.2% |
| Current smoker | 45.9% | 51.6% | 31.4% | 36.2% |
| Unknown | 0.9% | 0.8% | 1.1% | 1.0% |
| Alcohol use | ||||
| Never | 22.0% | 15.4% | 18.1% | 18.7% |
| Former | 23.4% | 23.1% | 17.5% | 19.3% |
| Current | 52.2% | 59.5% | 61.7% | 59.4% |
| Unknown | 2.5% | 2.0% | 2.7% | 2.6% |
Note: U.S.-born adults age 30–65, NHIS 1997–2009. Adjusted for sampling design. All variables are significantly different across education categories at p<.001 except sex (p=.018)
Contributor Information
Anna Zajacova, University of Wyoming.
Bethany G. Everett, University of Illinois at Chicago.
References
- Adams Peter, Hurd Michael D, McFadden Daniel, Merrill Angela, Ribeiro Tiago. Healthy, Wealthy, and Wise? Tests for Direct Causal Paths Between Health and Socioeconomic Status. Journal of Econometrics. 2003;112(1):3–56. [Google Scholar]
- American Council on Education. GED testing program statistical report. Author; Washington, DC: 2009. [Google Scholar]
- Backlund Eric, Sorlie Paul D, Johnson Norman J. The Shape of the Relationship between Income and Mortality in the United States. Evidence from the National Longitudinal Mortality Study. Annals of Epidemiology. 1996;6(1):12–20. doi: 10.1016/1047-2797(95)00090-9. [DOI] [PubMed] [Google Scholar]
- Bailis Daniel S, Segall Alexander, Chipperfield Judith G. Two Views of Self-Rated General Health Status. Social Science and Medicine. 2003;56(2):203–17. doi: 10.1016/s0277-9536(02)00020-5. [DOI] [PubMed] [Google Scholar]
- Bandura Albert. Social Foundations of Thought and Action: A social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall, Inc; 1986. Self-Efficacy. [Google Scholar]
- Barbeau Elizabeth M, Krieger Nancy, Soobader Mah-Jabeen. Working Class Matters: Socioeconomic Disadvantage, Race/Ethnicity, Gender, and Smoking in NHIS 2000. Am J Public Health. 2004;94(2):269–278. doi: 10.2105/ajph.94.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barsky Robert B, Thomas Juster F, Kimball Miles S, Shapiro Matthew D. Preference Parameters and Behavioral Heterogeneity: An Experimental Approach in the Health and Retirement Study. Quarterly Journal of Economics. 1997;112(2):537–579. [Google Scholar]
- Becker Gary S. Human Capital: A Theoretical and Empirical Analysis, with Special Reference to Education. New York: Columbia University Press; 1964. [Google Scholar]
- Boesel David. The street value of the GED diploma. Phi Delta Kappan. 1998;80(1):65. [Google Scholar]
- Boesel David, Alsalam Nabeel, Smith Thomas M. Educational and Labor Market Performance of GED Recipients: Research Synthesis. Washington, DC: National Library of Education, Office of Educational Research and Improvement, US Department of Education; 1998. [Google Scholar]
- Cameron Stephen V, Heckman James J. The Nonequivalence of High School Equivalents. Journal of Labor Economics. 1993;11(1):1–47. [Google Scholar]
- Caputo Richard K. The GED as a Predictor of Mid-Life Health and Economic Well-Being. Journal of Poverty. 2005;9(4):73–97. [Google Scholar]
- Christenson Bruce A, Johnson Nan E. Educational Inequality in Adult Mortality: An Assessment with Death Certificate Data from Michigan. Demography. 1995;32(2):215–29. [PubMed] [Google Scholar]
- Clark MA, Jaeger DA. Natives, the foreign-born and high school equivalents: new evidence on the returns to the GED. Journal of Population Economics. 2006;19(4):769–793. [Google Scholar]
- Cowell Alexander J. The Relationship Between Education and Health Behavior: Some Empirical Evidence. Health Economics. 2006;15(2):125–146. doi: 10.1002/hec.1019. [DOI] [PubMed] [Google Scholar]
- Crossley Thomas F, Kennedy Steven. The reliability of self-assessed health status. Journal of Health Economics. 2002;21(4):643–658. doi: 10.1016/s0167-6296(02)00007-3. [DOI] [PubMed] [Google Scholar]
- Cutler David M, Lleras-Muney Adriana. Education and Health: Evaluating Theories and Evidence. In: Schoeni RF, House JS, Kaplan GA, Pollack H, editors. Making Americans Healthier: Social and Economic Policy as Health Policy. New York, NY: Russel Sage Foundation; 2008. [Google Scholar]
- Dowd Jennifer Beam, Zajacova Anna. Does Self-Rated Health Mean the Same Thing Across Socioeconomic Groups? Evidence From Biomarker Data. Annals of Epidemiology. 2010;20(10):743–749. doi: 10.1016/j.annepidem.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupre Matthew E. Educational Differences in Health Risks and Illness over the Life Course: A Test of Cumulative Disadvantage Theory. Social Science Research. 2008;37(4):1253–1266. doi: 10.1016/j.ssresearch.2008.05.007. [DOI] [PubMed] [Google Scholar]
- Elo Irma T, Martikainen Pekka T, Smith Kristen P. Socioeconomic Differentials in Mortality in Finland and the United States: The Role of Education and Income. European Journal of Population. 2006;22(2):179–203. [Google Scholar]
- Heckman James J, LaFontaine Paul A. The American High School Graduation Rate: Trends and Levels. Review of Economics and Statistics. 2010;92(2):244–262. doi: 10.1162/rest.2010.12366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman James J. Schools, Skills, and Synapses. Economic Inquiry. 2008;46(3):289–324. doi: 10.1111/j.1465-7295.2008.00163.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman James J, Humphries John E, Mader Nicholas S. NBER Working Paper Series. Cambridge, MA: NBER; 2010. The GED. [Google Scholar]
- Heckman James J, LaFontaine Paul A. Bias-Corrected Estimates of GED Returns. Journal of Labor Economics. 2006;24(3):661–700. [Google Scholar]
- Heckman James J, Rubinstein Yona. The Importance of Noncognitive Skills: Lessons from the GED Testing Program. American Economic Review. 2001;91(2):145–49. [Google Scholar]
- Herd Pamela. Education and Health in Late-life among High School Graduates. Journal of Health and Social Behavior. 2010;51(4):478–496. doi: 10.1177/0022146510386796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill Terence D, Needham Belinda L. Gender-Specific Trends in Educational Attainment and Self-Rated Health, 1972–2002. American Journal of Public Health. 2006;96(7):1288–92. doi: 10.2105/AJPH.2004.061119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler Ellen L, Russell Louise B, Davis Diane. Survival, Functional Limitations, and Self-Rated Health in the NHANES I Epidemiologic Follow-up Study, 1992. First National Health and Nutrition Examination Survey. American Journal of Epidemiology. 2000;152(9):874–83. doi: 10.1093/aje/152.9.874. [DOI] [PubMed] [Google Scholar]
- Kenkel Donald, Lillard Dean, Mathios Alan. The Roles of High School Completion and GED Receipt in Smoking and Obesity. Journal of Labor Economics. 2006;24(3):635–660. [Google Scholar]
- Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of US adults. JAMA. 1998;279(21):1703–8. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- Liu Hui, Hummer Robert A. Are Educational Differences in U.S. Self-Rated Health Increasing?: An Examination by Gender and Race. Social Science & Medicine. 2008;67(11):1898–1906. doi: 10.1016/j.socscimed.2008.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnesota Population Center and State Health Access Data Assistance Center. Integrated Health Interview Series: Version 2.0. University of Minnesota; 2010. 2008 [cited January 2010]. Available from http://www.ihis.us. [Google Scholar]
- Mirowsky John, Ross Catherine E. Education, Personal Control, Lifestyle and Health. Research on Aging. 1998;20(4):415–449. [Google Scholar]
- Mirowsky John, Ross Catherine E. Education, Social Status, and Health. New York: Aldine de Gruyter; 2003. [Google Scholar]
- Mischel W, Shoda Y, Rodriguez MI. Delay of gratification in children. Science. 1989;244(4907):933–938. doi: 10.1126/science.2658056. [DOI] [PubMed] [Google Scholar]
- Mischel W, Shoda Y, Rodriguez MI. Delay of gratification in children. Science. 1989;244(4907):933–938. doi: 10.1126/science.2658056. [DOI] [PubMed] [Google Scholar]
- Mossey Jana M, Shapiro Evelyn. Self-Rated Health: A Predictor of Mortality among the Elderly. American Journal of Public Health. 1982;72(8):800–8. doi: 10.2105/ajph.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murnane Richard J, Willett John B, Boudett Kathryn Parker. Does a GED Lead to More Training, Post-Secondary Education, and Military Service for School Dropouts? Industrial and Labor Relations Review. 1997;51(1):100–116. [Google Scholar]
- Ou Suh-Ruu. Do GED Recipients Differ from Graduates and School Dropouts? Findings from an Inner-City Cohort. Urban Education. 2008;43(1):83–117. [Google Scholar]
- Rogers Richard G, Everett Bethany G, Zajacova Anna, Hummer Robert A. Educational Degrees and Adult Mortality Risk in the United States. Biodemography and Social Biology. 2010;56(1):80–99. doi: 10.1080/19485561003727372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross Catherine E, Mirowsky John. Refining the Association between Education and Health: The Effects of Quantity, Credentials, and Selectivity. Demography. 1999;36(4):445–60. [PubMed] [Google Scholar]
- Snyder TD, Dillow SA. Digest of Education Statistics 2010 (NCES 2011-015) Washington, DC: National Center for Education Statistics, Institute of Education Sciences, U.S. Department of Education; 2011. [Google Scholar]
- Sorlie Paul D, Rogot Eugene. Mortality by Employment Status in the National Longitudinal Mortality Study. American Journal of Epidemiology. 1990;132(5):983–92. doi: 10.1093/oxfordjournals.aje.a115741. [DOI] [PubMed] [Google Scholar]
- Subramanian SV, Huijts T, Avendano M. Self-reported health assessments in the 2002 World Health Survey: how do they correlate with education? Bulletin of the World Health Organization. 2010;88(2):131–138. doi: 10.2471/BLT.09.067058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangney June P, Baumeister Roy F, Boone Angie Luzio. High Self-Control Predicts Good Adjustment, Less Pathology, Better Grades, and Interpersonal Success. Journal of Personality. 2004;72(2):271–324. doi: 10.1111/j.0022-3506.2004.00263.x. [DOI] [PubMed] [Google Scholar]
- Tyler JH. Economic benefits of the GED: Lessons from recent research. Review of Educational Research. 2003;73(3):369–403. [Google Scholar]
- Tyler John. The General Educational Development (GED) Credential: History, Current Research, and Directions for Policy and Practice. In: Comings J, Garner B, Smith C, editors. Review of Adult Learning and Literacy. Vol. 5. Mahwah, NJ: Lawrence Erlbaum Associates; 2005. [Google Scholar]
- Tyler John, Lofstrom Magnus. Is the GED an effective route to postsecondary education for school dropouts? Economics of Education Review. 2010;29(5):813–825. [Google Scholar]
- Williams David R. Race and health: Basic questions, emerging directions. Annals of Epidemiology. 1997;7(5):322–333. doi: 10.1016/s1047-2797(97)00051-3. [DOI] [PubMed] [Google Scholar]
- Williams David R, Collins Chiquita. US Socioeconomic and Racial Differences in Health: Patterns and Explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- Zajacova Anna. Education, Gender, and Mortality: Does Schooling Have the Same Effect on Mortality for Men and Women in the US? Social Science and Medicine. 2006;63(8):2176–90. doi: 10.1016/j.socscimed.2006.04.031. [DOI] [PubMed] [Google Scholar]
- Zajacova Anna, Dowd Jennifer Beam. Reliability of Self-Rated Health in US Adults. American Journal of Epidemiology. 2011;174(8):977–983. doi: 10.1093/aje/kwr204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajacova Anna, Hummer Robert A, Rogers Richard G. Education and health among U.S. working-age adults: A detailed portrait across the full educatonal-attainment spectrum. Biodemography and Social Biology. 2012 doi: 10.1080/19485565.2012.666122. in press. [DOI] [PubMed] [Google Scholar]