Abstract
Background and aims: Photodynamic therapy with aminolevulinic acid (ALA-PDT) is effective therapy for acne vulgaris; however, relatively strong side effects limit its wide usage. We have previously demonstrated that ALA-induced protoporphyrin IX distribution with lower concentrations and shorter contact time of ALA resulted in focused damage in sebaceous glands in vivo. We have formulated a protocol for ALA-PDT using 5% ALA with 2 hours contact time. The objective of this study was to establish the effectiveness and side effect profile of the new protocol in humans. Subjects and Methods: Eleven Japanese patients (Fitzpatrick's skin type III – IV, mean age 23.7±7.2) with facial acne received topical application of 5% ALA for 2 hours with subsequent illumination by a broadband light (600 – 1100 nm, 15J/cm2, 60 mW/cm2). Subjects were evaluated prior to the procedure, 1 month, and 3 months after the treatment by a blinded dermatologist using the global acne grading system (GAGS). Side effects were monitored through the treatment period.
Results: The mean GAGS score decreased from 22.1±3.8 at baseline to 19.4 at 1 month, and to 16.3 at 3 months after PDT (P<0.05). Ten of eleven patients experienced local side effects, such as erythema, which were of minimal to mild severity. However, most side effects were of minimal to mild severity, and all of them resolved within several days without post inflammatory hyper pigmentation.
Conclusion: Our protocol was effective for acne in Japanese and did not exhibit severe side effects.
Keywords: acne vulgaris, ALA-PDT, photodynamic therapy, rhino mouse, sebaceous gland
Introduction
Acne vulgaris is one of the most common skin disorders, affecting approximately 85% of young people between 12 and 24 years of age 1). While many different treatments are available for acne, such as antibiotics, retinoids, exfoliative techniques etc, gradual resistance to these therapies is a hallmark of this dermatosis. Thus, the search for new therapeutics for acne is an active and actual topic of dermatologic investigations.
Photodynamic therapy (PDT) using 5-aminolevulinic acid (ALA)-induced protoporphyrin IX (PpIX) (ALA-PDT) for acne was initially reported in 2000 2), and since then many clinical trials have been attempted to provide durable response in patients with acne 3–16). The effectiveness of ALA-PDT for acne has been proven; while the treatment outcome was found to be influenced by various factors, such as concentration and contact time of ALA, wavelength, and/or emitted energy. Moreover, relatively strong side effects, such as pain, erythema, and post inflammatory hyperpigmentation (PIH) have hindered the usage of ALA-PDT for acne. The efficacy of ALA-PDT for acne is based on selectivity of ALA-PpIX for sebaceous glands, while side effects are related to extensive surrounding tissue damage 2, 3). In this context, we believe that a reduction of side effects could be achieved by increasing the selectivity of ALA-PpIX for sebaceous glands but limiting the ALA-PpIX accumulation in surrounding tissue. Recently, we performed a series of in vivo experiments in rhino mice (a common model of acne) and showed that sebaceous gland-targeted accumulation of ALAPpIX and selective damage of sebaceous glands by PDT can be achieved by shortening the incubation time and decreasing ALA concentration 17).
Based on these results, we proposed a new protocol of ALA-PDT, and performed a pilot clinical trial of with 5% ALA for 2 hours of contact time using the same irradiation setting.
Methods
Patients
Eleven Japanese patients with facial acne vulgaris were enrolled in this study after written informed consent was obtained. The study was approved by the ethical committee of Nippon Medical School Hospital. Seven females and four males were enrolled in our study (Table 1). The average age of the patients was 23.7±7.2 years old. The Fitzpatrick skin types of the patients were type III (n=2) or IV (n=9). The duration of acne varied from 1 to 17 years (5.4±4.4 years).
Table 1: Patient characteristics at baseline.
| case | age (y.o.)/sex | skin type | Duration of acne (years) | GAGS score | severity |
| 1 | 14/M | III | 1 | 27 | moderate |
| 2 | 23/F | IV | 6 | 21 | moderate |
| 3 | 21/F | IV | 8 | 27 | moderate |
| 4 | 38/M | IV | 3 | 17 | mild |
| 5 | 22/F | IV | 3 | 26 | moderate |
| 6 | 18/M | IV | 2 | 20 | mild |
| 7 | 32/F | IV | 3 | 18 | mild |
| 8 | 20/F | IV | 5 | 18 | mild |
| 9 | 22/F | III | 7 | 26 | moderate |
| 10 | 32/F | IV | 17 | 21 | moderate |
| 11 | 19/M | IV | 4 | 22 | moderate |
Photodynamic therapy
Hydrophilic ALA hydrochloride ointment (Cosmo Oil, Tokyo, Japan) was freshly prepared before the application at 5% concentration. ALA ointment was applied to the facial skin for two hours. A broadband (600 to 1100 nm) light system (TheraBeam®VR630; Ushio, Tokyo, Japan and M&M Co., Tokyo, Japan) was used for a light delivery at a fluence of 15 J/cm2 (fluence rate 60 mW/cm2). Two peaks, at 612 nm and 674 nm, in the emission spectrum were purposely designed to be absorbed by both ALA-PpIX and photoproducts produced in the photochemical reaction.
Clinical evaluation
The severity of acne was evaluated by a blinded dermatologist before PDT, one month, and three months after the treatment. Global acne grading score (GAGS) was used for evaluation 18). The severity of acne was accessed as: 0 none, 1–20 minimal, 21–30 moderate, 31–38 severe, and 39- very severe. Adverse effects (pain, erythema, edema, and PIH) were graded as none, minimal, mild, or severe.
Statistical analysis
The statistical analysis was based on the calculation of arithmetic mean and standard deviation. Statistical significance was determined using two-way ANOVA with Bonferroni post test. Values of p<0.05 were considered to be statistically significant.
Results
The patient characteristics are presented in Table 1. The average GAGS score before treatment was 22.1±3.8; four patients had mild acne, and seven patients had acne of moderate severity. In all patients except one who showed the same score before and after PDT, the GAGS score decreased, and the average score of GAGS score dropped to 19.48 one month after ALA-PDT and to 16.3 three months after PDT (data not shown). The decreasing rate of moderate acne at three months after treatment was 31.8%, showing greater improvement compared to mild acne which improved in 13.7% (P <0.05, Fig. 1a). Efficacy of the therapy was also evident by decreasing the number of patients with moderate severity of acne from 7 to 0, and an increase of number of patients with mild acne from 4 to 11 three months after ALA-PDT (Fig. 1b). Representative pictures of the patients with mild acne (Fig.2) and moderate acne (Fig.3) before and after therapy were presented.
Figure 1:
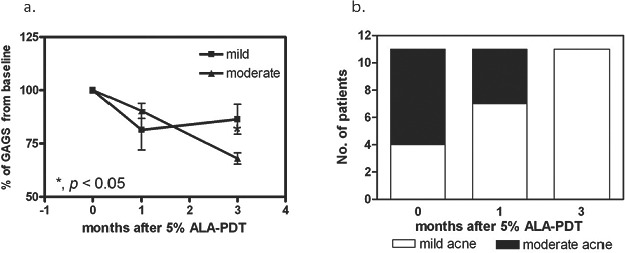
a. The average GAGS score of mild (square) and moderate (triangle) acne at baseline, one month after, and three months after PDT. (*P <0.05)
b. The number of patients with mild and moderate severity of acne during the course of therapy with ALA-PDT.
Figure 2:
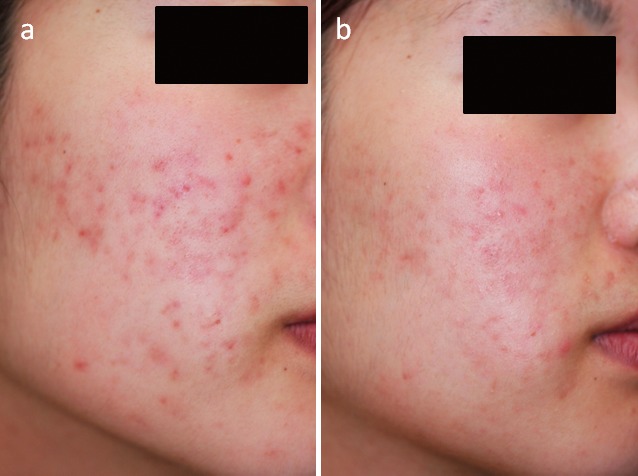
Patient eight (mild acne) a) at baseline (GAGS=18); b) at 3 months after ALA-PDT (GAGS=12)
Figure 3:
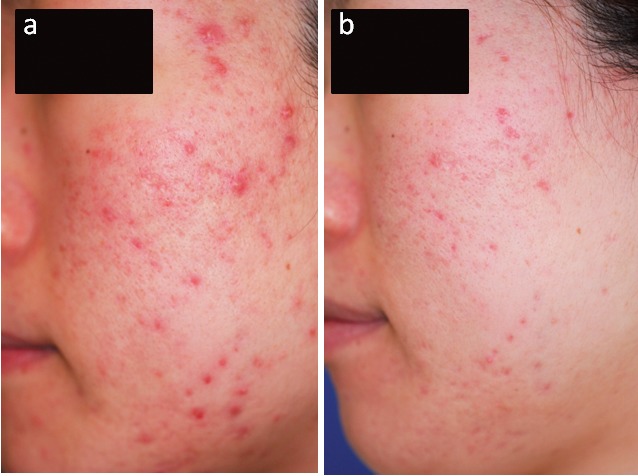
Patient nine (moderate acne) a) at baseline (GAGS=26); b) at 3 months after ALA-PDT (GAGS=15)
Ten out of 11 patients experienced some local side effects during or after PDT. The most frequent symptom was erythema, which was observed in ten patients. However, most of them except one were of minimal to mild severity, and all of them resolved within several days without PIH. Three out of 11 experienced minimal pain, while none required local anesthesia (Fig.4).
Figure 4:
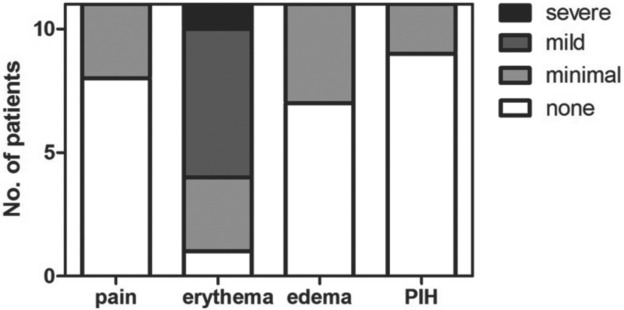
Side effects after ALA-PDT. Pain, erythema, edema, and post inflammatory hyperpigmentation (PIH) were graded as none, minimal, mild, and severe.
According to the protocol, the last evaluation of the study subjects was 3 months after single ALA-PDT. However, we were able to follow up eight out of 11 patients for period up to 12 months. Four out of those eight patients experienced recurrence at four to 12 months, and 5 patients requested and received the second ALA-PDT at three to 12 months after first PDT being highly satisfied with previous results expecting to get further improvement. The average time to disease progression in our study was 6 months.
Discussion
Acne vulgaris is one of the most common, multi-factorial diseases in dermatologic practice. Abnormal keratinization of sebaceous isthmus (comedogenesis), androgen-induced excessive sebum excretion, excessive colonization by Propionibacterium acnes (P. acnes) and bacteria-induced inflammation, hereditary factors, and follicular reactivity all play a pivotal role in the development of acne lesions. In spite of the complexity of the etiology, it can be simply stated that acne vulgaris is a disorder of sebaceous glands. The main mechanism by which ALA-PDT is effective in acne is destruction of the affected sebaceous glands by means of the relatively selective accumulation of ALA-PpIX in sebocytes 2). P. acnes was also considered to contribute to the efficacy of ALA-PDT for acne, since high accumulation of porphyrins by P. acnes may be responsible for the enhancement of the phototoxicity 19).
Previously, we attempted to achieve more selectivity of ALA-PpIX for sebaceous glands by altering the concentration and contact time of ALA. Using rhino mouse model, we found that selective accumulation of ALA-PpIX in sebaceous glands and subsequent destruction after irradiation could be accomplished by relatively low concentration (5%) of ALA and short contact time (1 to 2 hours) 17). We were encouraged to evaluate the efficacy and the side effect profile of our new protocol in Japanese patients, who have darker skin compared to the patients in most published reports. We found good efficacy and tolerability of proposed protocol in patients with skin type III to IV using lower concentration and shorter contact time of ALA compared to the established protocols. Although, we did not verify level of PDT damage histologically, we expect that this was due to improved selectivity of ALA-PpIX to sebaceous glands.
The total decreasing rate was 26.3% at 3 months after treatment; 31.8% in moderate acne and 13.7% in mild acne. It is significant that we could achieve such reduction after single PDT. Moreover there was no severe PIH in patients even with relatively darker skin types, although most of the patients experienced minimal to mild transient erythema. Previous PDT trials demonstrated high efficacy of multiple PDT administration showing improvement from 53% to 87% sometimes accompanied by severe side effects 9–12,14,16). We assumed that subsequent treatments might bring even higher curative rate. It was shown that the time interval for consecutive PDT treatments was one of important parameters for PDT efficacy. Additional study may be required to establish the optimal interval for subsequent treatments. While many strategies have been proposed to improve the therapeutic outcome and decrease the side effects of ALA-PDT (estreification of ALA 20), skin stripping/microdermabrasion 21,22), iontoforesis/electoroporation 23) etc), we believe that our strategy choosing the optimal concentration and contact time for ALA is one of the most straight forward approaches. Recently, Yin et al reported a paper 16)comparing the efficacy and the side effects using 5% to 20% of ALA and suggested that consecutive ALA-PDT with 10% or 15% ALA would be the ideal regimen in Chinese patients who have similar skin type of Japanese. Further clinical studies could be directed towards establishing the efficacy of multitreatment protocol of ALA-PDT for acne as well as comparing efficacy of established regiment vs. traditional one.
Acknowledgements
A broadband light system (TheraBeam®VR630) was provided by Ushio, Tokyo, Japan and M&M Co., Tokyo, Japan.
References
- 1: Plewig G, Kligman AM. Acne, Prevalence. In: Acne and Rosacea 3rd edn. 2000, Springer,Germany: pp 27 [Google Scholar]
- 2: Hongcharu W, Taylor CR, Chang Y, Aghassi D, Suthamjariya K, Anderson RR. (2000): Topical ALA-photodynamic therapy for the treatment of acne vulgaris. Jounal of Investigative Dermatology, 115: 183∼192 [DOI] [PubMed] [Google Scholar]
- 3: Itoh Y, Ninomiya Y, Tajima S, Ishibashi A. (2000): Photodynamic therapy for acne vulgaris with topical 5-aminolevulinic acid. Archives of Dermatology, 115: 1093∼1095 [DOI] [PubMed] [Google Scholar]
- 4: Pollock B, Turner D, Stringer MR, Bojar RA, Goulden V, Stables GI, Cunliffe WJ. (2004): Topical aminolevulinic acid-photodynamic therapy for the treatment of acne vulgaris: a study of clinical efficacy and mechanism of action. British Journal of Dermatology, 151: 616∼622 [DOI] [PubMed] [Google Scholar]
- 5: Hong S-B, Lee M-H. (2005): Topical aminolevulinic acid-photodynamic therapy for treatment of acne vulgaris. Photodermatology, Photoimmunology and Photomedicine, 21: 322∼325 [DOI] [PubMed] [Google Scholar]
- 6: Santos MAV, Belo VG, Santos G. (2005). Effectiveness of photodynamic therapy with topical 5-aminolevulinic acid and intense pulsed light versus intense pulsed light alone in the treatment of acne vulgaris: comparative study. Dermatologic Surgery, 31: 910∼915 [DOI] [PubMed] [Google Scholar]
- 7: Wiegell SR, Wulf HC. (2006). Photodynamic therapy of acne vulgaris using methyl aminolevulinate: a blinded, randomized, controlled trial. British Journal of Dermatology, 154: 969∼976 [DOI] [PubMed] [Google Scholar]
- 8: Hörfelt C, Stenquist B, Larkö O, Faergemann J, Wennberg A-M. (2007). Photodynamic therapy for acne vulgaris: a pilot study of the dose-response and mechanism of action. Acta Dermato-Venereologica, 87: 325∼329 [DOI] [PubMed] [Google Scholar]
- 9: Wiegell SR, Wulf HC. (2006). Photodynamic therapy of acne vulgaris using 5-aminolevulinic acid versus methyl aminolevulinate. J Am Acad Dermatol, 54: 647∼651 [DOI] [PubMed] [Google Scholar]
- 10: Rojanamatin J, Choawawanich P. (2006). Treatment of inflammatory facial acne vulgaris with intense pulsed light and short contact of topical 5-aminolevulinic acid: a pilot study. Dermatologic Surgery, 32: 991∼997 [DOI] [PubMed] [Google Scholar]
- 11: Hörfelt C, Funk J, Frohm-Nilsson M, WieglebEdström D, Wennberg A-M. (2006). Topical methyl aminolevulinate photodynamic therapy for treatment of facial acne vulgaris: results of a randomized, controlled study. British Journal of Dermatology, 151: 608∼611 [DOI] [PubMed] [Google Scholar]
- 12: Marvilia L, Malara G, Moretti G, LoRe M, Puglisi_Guerra A. (2007). Photodynamic therapy of acne using methyl aminolevulinate diluted 4% together with low doses of red light. British Journal of Dermatology, 157: 810∼811 [DOI] [PubMed] [Google Scholar]
- 13: Akaraphanth R, Kanjanawanitchkul W, Gritiyarangsan P. (2007). Efficacy of ALA-PDT vs blue light in the treatment of acne. Photodermatology, Photoimmunology and Photomedicine, 23: 186∼190 [DOI] [PubMed] [Google Scholar]
- 14: Yeung CK, Shek SY, Bjerring P, Yu CS, Kono T, Chan HH. (2007). A comparative study of intense pulse light alone and its combination with phorodynamic therapy for the treatment of facial acne in Asian skin. Lasers in Surgery and Medicine, 39: 1∼6 [DOI] [PubMed] [Google Scholar]
- 15: Haedersdal M, Togsvers-Bo K, Wiegell SR, Wulf HC. (2008). Long-pulsed dye laser versus longpulsed dye laser-assisted photodynamic therapy for acne vulgaris: a randomized controlled trial. Journal of the American Academy of Dermatology, 58: 387∼394 [DOI] [PubMed] [Google Scholar]
- 16: Yin R, Hao F, Deng J, Yang XC, Yan H. (2010). Investigation of optimal aminolevulinic acid concentration applied in topical aminolevulinic acid-photodynamic therapy for treatment of moderate to severe acne: a pilot study in Chinese subjects. British Journal of Dermatology, 163: 1064∼1071 [DOI] [PubMed] [Google Scholar]
- 17: Kosaka S, Miyoshi N, Alilov OE, Hasan T, Kawana S. (2011). Targeting of sebaceous glands by delta-aminolevulinic acid-based photodynamic therapy: an in vivo study. Lasers in Surgery and Medicine, 43: 376-381 [DOI] [PubMed] [Google Scholar]
- 18: Doshi A, Zaheer A, Stiller MJ. (1997). A comparison of current acne grading systems and proposal of a novel system. International Journal of Dermatology, 36: 416∼418 [DOI] [PubMed] [Google Scholar]
- 19: Ashkenazi H, Malik Z, Harth Y, Nitzan Y. (2003). Eradication of Propionibacterium acnes by its endogenic porphyrins after illumination with high intensity blue light. FEMS Immunology and Medical Microbiology, 35: 17∼24 [DOI] [PubMed] [Google Scholar]
- 20: Gerscher S, Connelly JP, Griffiths J, Brown SB, MacRobert AJ, Wong G, Rhodes LE. (2000). Comparison of the pharmacokinetics and photo-toxicity of protoporphyrin IX metabolized from 5-aminolevulinic acid and two derivatives in human skin in vivo. Photochemical and Photobiological Sciences, 72: 569∼574 [DOI] [PubMed] [Google Scholar]
- 21: Soler A, Warloe MT, Berner A, Giercksky KE. (2001). A follow-up study of recurrence and cosmesis in completely responding superficial and nodular basal cell carcinomas treated with methyl 5-aminolevulinate-based photodynamic therapy alone with prior curettage. British Journal of Dermatology, 145: 167∼471 [DOI] [PubMed] [Google Scholar]
- 22: Donnelly RF, McCarron PA, Woolfson AD. (2005). Drug delivery of aminolevulinic acid from topical formulations intended for photodynamic therapy. Photochemical and Photobiological Sciences, 81: 750∼767 [DOI] [PubMed] [Google Scholar]
- 23: Fang JY, Lee WR, Shen SC, Fang YP, Hu CH. (2004). Enhancement of topical 5-aminolevulinic acid delivery by erbium:YAG laser and microdemabrasion: a comparison with iontophoresis and electroporation. British Journal of Dermatology, 151: 132∼140 [DOI] [PubMed] [Google Scholar]


