Abstract
Background and Aims: Vaginal relaxation syndrome (VRS) is both a physical and psychological problem for women and often their partners. Recently the 2940 nm Er:YAG laser has attracted attention for VRS treatment. The current study evaluated the clinical efficacy of this nonsurgical laser procedure.
Subjects and Methods: Thirty postpartum females with VRS or vaginal atrophy, ages from 33 – 56 yr (mean 41.7 yr) were divided randomly into two groups, Group A and Group B. Both groups were treated for 4 sessions at 1∼2-weekly intervals with a 2940 nm Er:YAG via 90° and 360° scanning scopes. In Group A the first 2 sessions were performed with the 360° scope and the final 2 with the 90° scope in multiple micropulse mode, 1.7 J delivered per shot, 3 multishots, 3 passes per session. Group B underwent multiple micropulse mode treatment with the 90° scope in all 4 sessions (same parameters as Group A) then during the final 2 sessions an additional 2 passes/session were delivered with the 360° scope, long-pulsed mode, 3.7 J delivered per shot. Perineometer assessments were performed at baseline and at 2 months post-treatment for vaginal tightness. Histological specimens were taken at baseline and at 2 months post-procedure. Subjective satisfaction with vaginal tightening was assessed together with improvement in sexual satisfaction. Results were tested for statistical significance with the paired Student's t-test.
Results: All subjects successfully completed the study with no adverse events. Significant improvement in vaginal wall relaxation was seen in all subjects at 2 months post-procedure based on the perineometer values, on the partners' input for vaginal tightening (76.6%) and for sexual satisfaction as assessed by the subjects themselves (70.0%). The histological findings suggested better elasticity of the vaginal wall with tightening and firming.
Conclusions: Both regimens of Er:YAG laser treatment for VRS produced significant improvement in vaginal relaxation. With multishots delivered in the multiple micropulse mode via scanning scopes, nonsurgical Er:YAG laser treatment was pain-free, safe, side effect free, easily tolerated and effective.
Keywords: Multishot micropulse mode, vaginal tightening, 360° scanning scope, 90° scanning scope, perineometer, sexual satisfaction, elastinogenesis, collagenesis, tissue remodeling
Introduction
As women age, relaxing of the vaginal wall can lead to vaginal relaxation syndrome (VRS), which is exacerbated by childbirth, especially multiple pregnancies and deliveries, and the vaginal atrophy associated with menopause-related hormonal changes. VRS can lead to a number of problems, both physical and psychological, a major one of which is lessening of sexual satisfaction for both the female and her partner, often referred to as “loose vagina”. Urinary incontinence (UI) is another problem associated with VRS, either of the stress or urge type, and can be mildly irritating or totally debilitating. The quality of life of affected women can decline dramatically as they become afraid to go out socially or even to work because of the humiliation of an unpredictable and involuntary loss of urinary control. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health (NIH) in the USA, UI occurs in women at least twice as often as in men. The combination of loss of sexual satisfaction for both partners and the psychological and social problems associated with UI mandate that a real, lasting and consistent solution for the underlying condition of VRS is required.
A variety of VRS treatment options exists spanning the spectrum from noninvasive approaches to frankly invasive surgical procedures. For the noninvasive approaches, behavioral training such as Kegel exercises can tighten up relaxed musculature in the pelvic floor and to a lesser extent in the vaginal wall; “tightening creams”, hormonal creams, sprays and other pharmacological approaches are also available. However, although these are noninvasive and innocuous, the effectiveness is somewhat limited and the latency period temporary, requiring continuous application in the case of the pharmacotherapies. Surgical procedures, in which vaginal and associated tissues are incised and rearranged, 1) can offer a much better and longer lasting final result. The results of surgical vaginoplasties, however, have to be balanced against the much greater risks involved in any surgery performed on the extremely sensitive vaginal tissues. Downtime for recovery is longer, and there are recognized risks associated with scar formation or nerve damage leading to dysesthesia. 2,3)
The laser has recently been added to the traditional armamentarium associated with surgical approaches for VRS because of its precision and the ability to limit damage depth with particular wavelengths having high water absorption, such as the CO2 (10600 nm) and particularly the Er:YAG (2940 nm). This approach was called laser-assisted vaginoplasty. Taking the bulk laser beam and splitting it into multiple microbeams has provided even more control of the depth of the microablative columns (MACs), resulting in better efficacy with less downtime for the subject, and has become popularized as so-called “vaginal tightening”. Compared with a vaginoplasty, this approach encompasses non-reconstructive strategies aimed at restoring the muscle tone of the vagina by tightening the supportive structures of the vulvovaginal complex, in an effort either to at least reduce the effects of aging and childbirth.
Fractional Er:YAG systems with a dedicated gynecological delivery system recently became commercially available offering a nonsurgical approach falling under the concept of vaginal tightening. In the system used in the present study, special scanning scopes, one allowing 360° beam delivery and the other a 90° side-firing scope, were designed to deliver selective and precise ablation with controlled coagulative damage to the entire vaginal wall for the treatment of all symptoms of VRS, or to the wall of the anterior vaginal canal for the treatment of UI, or both. The present study was designed to assess the efficacy of the multiple micropulse mode Er:YAG laser fitted with such scanning scopes in the treatment of VRS, and compared two different treatment protocols.
Subjects and Methods
Subjects
The study subjects comprised 30 postpartum females with VRS or vaginal atrophy, ages from 33 – 56 yr (mean 41.7 yr) who were divided randomly into two groups, Group A and Group B. Five subjects had given birth once, 20 twice, and 5 had undergone 3 deliveries. There was no significant difference between the groups as regards mean age (Group A, 42.93 yr; Group B, 40.53 yr), body mass index (BMI) (Group A 22.3; Group B, 22.6) or parous status. Regarding the menstrual status, in Group A, pre-, peri- and post-menopausal females accounted for 9, 1 and 5 subjects, respectively; in group B, 14, 1 and 0. Group A was thus at a more advanced menopausal status than group B. One subject in Group A had undergone a cesarean section, compared with 5 subjects in Group B. The subject demographics and relevant histories are given in Table 1. Regarding the degree of VRS, 3, 9 and 3 subjects were graded mild, moderate and severe, respectively, in Group A, compared with 7, 3 and 5 in Group B (Table 2). Levator ani muscle (LAM) power as assessed with a digital examination was respectively good, moderate, poor and very poor in 5, 2, 7 and 1 subjects in Group A, compared with 4, 7, 3 and 1 subjects, respectively, in Group B (Table 2). A perineometer (ExTT-101, APIMEDS Inc, South Korea) was used for objective measurement of the strength of voluntary contractions of the pelvic floor muscles at baseline and after treatment. Table 2 also shows the baseline perineometer readings for the maximum (Pm) pressures and average (Pa) pressures (in mmHg) and the time for which pressure was maintained (Pt in seconds).
Table 1: Patient characteristics.
| Serial No | Age | BMI(%) | Parous status | Delivery type | Menstrual status | Remarks |
|---|---|---|---|---|---|---|
| Group A (n = 15) | ||||||
| P-1 | 36 | 21.9 | 2 | NSVD | premen | |
| P-2 | 38 | 23.2 | 2 | C-sec | premen | |
| P-3 | 35 | 22.6 | 2 | NSVD | premen | previous p-repair Hx(+) |
| P-4 | 40 | 20.1 | 2 | NSVD | premen | Previous sexual assault Hx(+) |
| P-5 | 41 | 24.1 | 3 | NSVD | premen | |
| P-6 | 53 | 27.1 | 2 | NSVD | postmen | atrophic vaginitis case |
| P-7 | 56 | 25 | 2 | NSVD | postmen | atrophic vaginitis case |
| P-8 | 35 | 19.7 | 1 | NSVD | premen | previous LEEP Hx(+) |
| P-9 | 35 | 19.7 | 1 | NSVD | premen | |
| P-10 | 56 | 24.4 | 3 | NSVD | postmen | |
| P-11 | 51 | 24.3 | 2 | NSVD | perimen | |
| P-12 | 52 | 22.4 | 3 | NSVD | postmen | atrophic vaginitis case |
| P-13 | 43 | 20.4 | 2 | NSVD | premen | |
| P-14 | 36 | 22 | 2 | NSVD | premen | |
| P-15 | 37 | 20.6 | 2 | NSVD | premen | |
| Group B (n=15) | ||||||
| P-16 | 49 | 20 | 3 | NSVD | premen | |
| P-17 | 42 | 24.3 | 1 | C-sec | premen | |
| P-18 | 42 | 25 | 2 | NSVD | premen | |
| P-19 | 33 | 22 | 2 | C-sec | premen | |
| P-20 | 38 | 19.1 | 2 | C-sec | premen | |
| P-21 | 40 | 20.6 | 1 | NSVD | premen | |
| P-22 | 34 | 32.2 | 2 | C-sec | premen | |
| P-23 | 42 | 23.2 | 2 | NSVD | premen | |
| P-24 | 44 | 24.3 | 2 | C-sec | premen | |
| P-25 | 41 | 20.8 | 1 | NSVD | premen | previous TOT op(+) |
| P-26 | 33 | 17.6 | 3 | NSVD | premen | |
| P-27 | 33 | 18.4 | 2 | NSVD | premen | |
| P-28 | 52 | 26.7 | 2 | NSVD | perimen | previous TOT op(+) / HRT(+) |
| P-29 | 38 | 22.8 | 2 | NSVD | premen | |
| P-30 | 47 | 21.4 | 2 | NSVD | premen | |
KEY: BMI, body mass index; NSVD, normal spontaneous vaginal delivery; C-sec, cesarean section; Premen, premenstrual; perimen, perimenstrual; postmen, postmenstrual; p-repair, posterior vaginal repair; LEEP, loop electrosurgical excision procedure; TOT, transobturator tape surgery; HRT, hormone replacement therapy
Table 2: Vaginal wall relaxation status at baseline as assessed by digital examination, at baseline and after treatment tested with a perineometer, postprocedural partners' assessment of vaginal tightening and patients' assessment of postprocedural sexual satisfaction.
| Pat. No | Degree of VWRS | LAM power (digital exam) | Perineometer test values | Vaginal tightening (Partner) | Sexual satisfaction (Patient) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| B/L | Post-2 months | |||||||||
| Pm (mmHg) | Pa (mmHg) | Pt (s) | Pi (mmHg) | Pa (mmHg) | Pt (s) | |||||
| Group A | ||||||||||
| P-1 | mild | good | 39 | 34 | 10 | 41 | 35 | 17 | 3 | 3 |
| P-2 | mild | good | 48 | 38 | 9 | 61 | 44 | 10 | 2 | 3 |
| P-3 | moderate | poor | 13 | 6 | 20 | 17 | 6 | 36 | 0 | 0 |
| P-4 | moderate | good | 28 | 21 | 6 | 49 | 42 | 8 | 0 | 3 |
| P-5 | moderate | poor | 12 | 7 | 6 | 22 | 16 | 19 | 2 | 2 |
| P-6 | moderate | good | 28 | 19 | 20 | 50 | 40 | 21 | 3 | 3 |
| P-7 | mild | poor | 7 | 3 | 21 | 13 | 7 | 19 | 0 | 3 |
| P-8 | moderate | good | 11 | 6 | 23 | 32 | 24 | 23 | 1 | 1 |
| P-9 | moderate | poor | 8 | 6 | 7 | 15 | 11 | 25 | 3 | 3 |
| P-10 | severe | moderate | 19 | 14 | 2 | 27 | 20 | 14 | 1 | 0 |
| P-11 | severe | poor | 13 | 8 | 2 | 19 | 9 | 6 | 1 | 1 |
| P-12 | moderate | moderate | 8 | 4 | 10 | 31 | 25 | 16 | 3 | 3 |
| P-13 | moderate | poor | 8 | 4 | 16 | 14 | 8 | 26 | 2 | 2 |
| P-14 | moderate | poor | 20 | 10 | 49 | 22 | 10 | 53 | 3 | 3 |
| P-15 | severe | very poor | 0 | 0 | 0 | 15 | 10 | 8 | 1 | 1 |
| Group B | ||||||||||
| P-16 | severe | moderate | 21 | 15 | 21 | 20 | 14 | 23 | 1 | 1 |
| P-17 | moderate | moderate | 8 | 5 | 11 | 10 | 6 | 10 | 1 | 0 |
| P-18 | mild | good | 19 | 9 | 46 | 15 | 8 | 40 | 0 | 0 |
| P-19 | mild | moderate | 15 | 5 | 37 | 24 | 16 | 25 | 0 | 0 |
| P-20 | mild | good | 20 | 12 | 8 | 28 | 19 | 8 | 0 | 0 |
| P-21 | mild | good | 37 | 30 | 13 | 38 | 24 | 17 | 1 | 1 |
| P-22 | mild | poor | 26 | 19 | 14 | 34 | 26 | 15 | 3 | 3 |
| P-23 | moderate | very poor | 0 | 0 | 0 | 20 | 12 | 14 | 3 | 3 |
| P-24 | mild | moderate | 17 | 14 | 22 | 22 | 18 | 56 | 2 | 2 |
| P-25 | moderate | good | 22 | 15 | 36 | 32 | 24 | 17 | 1 | 1 |
| P-26 | severe | moderate | 31 | 24 | 5 | 34 | 28 | 5 | 0 | 0 |
| P-27 | severe | poor | 18 | 12 | 25 | 19 | 12 | 33 | 0 | 0 |
| P-28 | severe | moderate | 27 | 21 | 4 | 65 | 54 | 8 | 2 | 2 |
| P-29 | mild | poor | 10 | 7 | 24 | 14 | 10 | 58 | 1 | 1 |
| P-30 | severe | moderate | 22 | 18 | 30 | 15 | 9 | 56 | 2 | 2 |
Pat. No, patient reference No; VWRS, vaginal wall relaxation status; LAM, levator ani muscle; BL, baseline values; Post-2 months, values 2 months after the final treatment; Pm, maximum pressure; Pa, average pressure; Pt, time for which pressure was maintained; Vaginal tightening (Partner), assessment by the patient's partner of the degree of improvement in vaginal tightness post-treatment using the following scale: little or no improvement, 0; some improvement, 1; good improvement, 2; excellent improvement, 3.
Patient sexual satisfaction was self-rated using the following scale: dissatisfied, 0; somewhat satisfied, 1; satisfied, 2; extremely satisfied, 3.
Laser system
The laser system used was the ACTION II™ Er:YAG (Lutronic, Goyang, South Korea) delivering a wavelength of 2940 nm. When fitted with the dedicated vaginal scanning scopes (Petit Lady™ system, Lutronic) the laser can be operated in the multiple micropulse mode (pulse width of 250 µs, selectable number of multipulses), or in the long-pulsed mode (1000 ms, single pulse). There were two scopes comprising the dedicated vaginal scanning scope system (Figure 1): one scope delivered a 360° ring-shaped beam with an approximate beam width at target of 2–3 mm (Petit 360), and the other delivered around-shaped 90° beam with an approximate beam width at target of 5 mm (Petit 90), both scopes being supported in the vagina by a specially designed guide (Figure 2). In general, for the 360° scope the supporting guide is inserted, then the scope is fully inserted into the guide. The body of the scope is marked with 2.5 mm gradations. The laser parameters are set including the multiple pulse option, the laser is fired, the probe is withdrawn by 1 gradation (2.5 mm) marked on the probe body, and the process repeated for the entire length of the vaginal canal. Multiple passes may be made. For the 90° scope in the treatment of UI, following insertion of the supporting cage the probe is inserted with the active part of the scope at the 12 o'clock position. The laser is fired, and the scope turned to the 2 o'clock position, fired again, then turned to the 10 o'clock position and fired again. The scope is withdrawn by 2 gradations (5 mm), returned to the 12 o'clock position, and the process is repeated for the required number of passes. To treat the entire vaginal wall with the 90° scope, however, for each set of shots the active part of the scope is set at the 12 o'clock, then 2 o'clock, 4 o'clock, 6 o'clock, 8 o'clock and 10 o'clock positions, the scope is withdrawn by 2 gradations, and the process repeated.
Fig. 1:

The 360° scanning scope (left) and the 90° scanning scope (right).
Fig. 2:
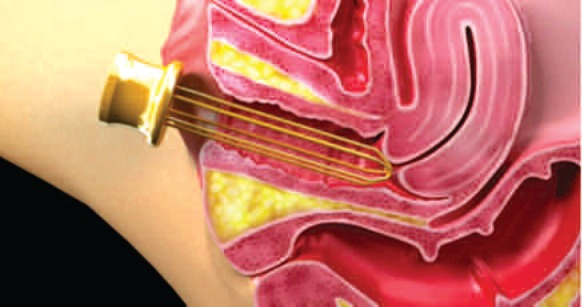
Illustration showing the special support for the scanning scopes inserted in the vagina.
Treatment protocol by group (N=15 for both groups)
Group A: The protocol called for four treatment sessions, 1–2 weeks apart. In sessions 1 and 2, treatment was applied with the 360° scope as described above using the multiple micropulse mode. The multishot option was set to 3 multishots and 1.7 J/shot was selected by manually setting the pulse energy at 15 mJ on the screen display in Fractional Mode to convert the display screen settings to the gynecological scope settings. Three passes were delivered along the entire length of the vaginal canal in each treatment session. In sessions 3 and 4, the 90° scope was used at the same parameters as for sessions 1 and 2. For each set of shots the active part of the scope was set at the 12 o'clock, then 2 o'clock, 4 o'clock, 6 o'clock, 8 o'clock and 10 o'clock positions to treat the entire circumference of the vaginal wall, as described above.
Group B: Four treatment sessions were delivered, 1–2 weeks apart. Sessions 1–4 called for the 90° scope used as in Group A, multiple micropulse mode, 3 multishot setting (pulse width of 250 µs), and 1.7 J/shot. Three passes were delivered for each treatment session. In sessions 3 and 4 an additional 2 passes per session were delivered with the 360° scope in long-pulsed mode, pulse width of 1000 ms (1 s), 3.7 J/shot (manually set as 11 J/cm2 on the display screen with a spot size of 6.4 mm in Long Pulsed mode).
Assessments
Punch biopsies were taken at baseline and at 2 months after the final session, formalin fixed and routinely prepared for light microscopy with hematoxylin and eosin and elastica van Giesen staining. Perineometer reading were repeated at the same time point and compared with the baseline values. Subjective assessments at the same time point included the subject's partner's evaluation of the degree of vaginal tightening, and the subject's own evaluation of the degree of improvement in sexual satisfaction. Subjective scoring was on 4-point scales as follows: For vaginal tightening, little or no improvement, 0; some improvement, 1; good improvement, 2; excellent improvement, 3. For patient sexual satisfaction, dissatisfied, 0; somewhat satisfied, 1; satisfied, 2; extremely satisfied, 3.
Statistical analysis
Perineometer readings of all subjects were compared at baseline and 2 months after the final session with the paired Student's t-test. The same test was used to compare between Groups A and B for perineometer readings, partner's assessment of vaginal tightening and subject's assessment of improvement in sexual satisfaction. A P value equal to or less than 0.05 was considered statistically significant, with marginal significance at P equal to or less than 0.1. The statistical software used was STATISTICA V10, StatSoft, OK, USA.
Results (Table 2)
All subjects completed the treatment and the 2-month assessment. All patients were aware of some heating in the vagina during treatment, and a very few patients (3: 1 from Group A and 2 from Group B) felt mild vaginal ecchymosis with a mild burning sensation which lasted for 24–48 hr and evolved spontaneously. No subject reported any major or lasting adverse side effects after any of the treatments. Improvement was seen in all perineometer scores, in the majority of subjects (76.6%) for the partner's assessment of vaginal tightening and in the subjects' own assessment of improved sexual satisfaction (70.0%).
Statistical assessments (Table 3)
Table 3: Statistical analyses of the data comparing the baseline and post-procedure results for the entire patient population, and between Groups A and B.
| Groups | Pm (mmHg) | S-Sig (p) | Pa (mmHg) | S-Sig (p) | Pt (s) | S-Sig (p) | VT | SS | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| BL (SEM) | Post (SEM) | BL (SEM) | Post (SEM) | BL (SEM) | Post (SEM) | ||||||
| Total | 18.50 (2.04) | 27.27 (2.60) | *< 0.01 (=0.0052) | 12.87 (1.76) | 19.57 ](2.3) | *< 0.05 (=0.013) | 16.57 (2.4) | 22.87 (2.9) | < 0.1 (=0.097) | □ | □ |
| Grp A* vs Grp B** | 17.47 (3.4) | 28.53 (3.9) | *<0.1 (= 0.091) | 12.00 (2.92) | 20.47 (3.55) | NS (=0.330) | 13.4 (3.19) | 20.07 (3.13) | NS (=0.539) | NS (=0.101) | *< 0.05 (=0.011) |
| 13.73 (2.05) | 18.67 (2.09) | 13.73 (2.06) | 18.67 (3.09) | 19.73 (3.49) | 25.67 (4.81) | ||||||
BL, baseline; Pm, maximum pressure; Pa, average pressure; Pt, time for which pressure was maintained, in seconds; SEM, standard error of means; Post, 2 months post-treatment; S-Sig, statistical significance; (p), P value (paired Student's t-test); VT, vaginal tightening (assessed by patients' partners); SS, sexual satisfaction (patients' subjective assessment); NS, no significance
Overall values in the vaginal wall relaxation status for the total subject population showed a statistically significant improvement between the baseline and findings at 2 months after treatment for the maximum perineometer pressure (p <0.01), and the average pressure (p < 0.05), with marginal significance noted in the time for which the pressure was maintained (p < 0.1).
Fig. 6:
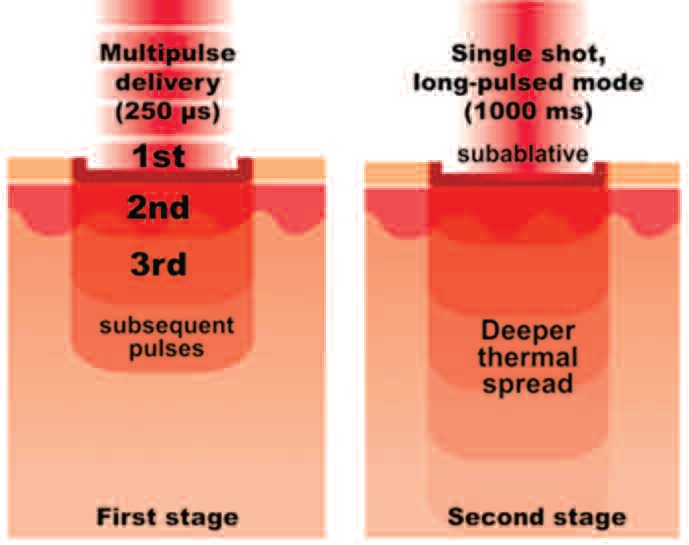
Schematic representation of the dual-mode technique. In the first stage (left panel) the 1st shot of the 250 µs multipulse delivers controlled and minimal ablation opening a window in the epidermal tissue, allowing the thermal effect of subsequent shots to penetrate into the lamina propria. In the second stage, the subablative single shot in the 1000 ms long-pulsed mode delivers thermal damage deep into the lamina propria through the existing epidermal window.
In the comparison of results between groups, Group A had slightly better results than Group B with marginal significance in the maximum pressure (p <0.1) and an increased trend without significant difference seen in the average perineometer pressure or the time for which pressure was maintained. As for vaginal tightening as assessed by the subject's partner, Group A showed an increasing trend without significance compared with Group B, but with a statistically significant difference seen for the increase in sexual satisfaction assessed by the subjects themselves (p <0.05).
Histological assessment
The histological findings in general showed evidence of a thicker and more cellular epithelium and a more compact lamina propria with a denser arrangement of connective tissue. Figures 3 (Patient 1) and 4 (Patient 2) show representative specimens at baseline and two months after the final treatment under hematoxylin and eosin and elastica van Giesen staining, respectively. Taken together, the results of the histological analysis suggest tightening and firming of the vaginal wall. Both specimens came from comparatively young patients, but even in these young patients improvements in and rejuvenation of the vaginal structures can be seen 2 months after the final Petit Lady treatment.
Fig. 3:
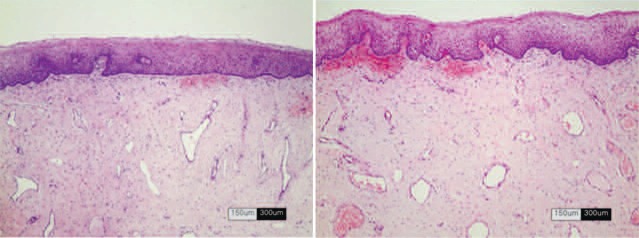
Hematoxylin and eosin stained specimens of the vaginal wall from patient 1 (Left) at baseline, and (right) 2 months after treatment with the system used in the present study showing improved mucosal architecture in both the epithelium and lamina propria. Scale units are as shown on the bars.
Fig. 4:
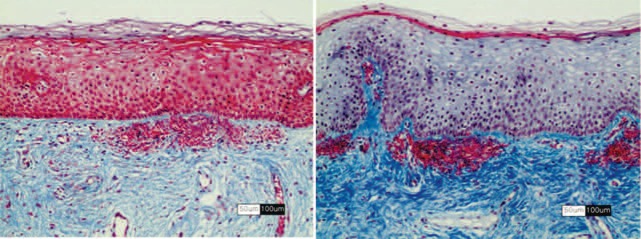
In these elastica van Giesen stained specimens from the vaginal wall of patient 2 at a higher magnification than in Fig 3, the findings can be seen comparing the baseline (left) with the situation 2 months post-treatment (right) where a thicker epithelium and denser lamina propria are observed. Scale units are as shown on the bars.
Subject assessments
As seen in Table 2, in the case of the subjects' partners, 23 out of 30 (76.6%) noted improvement in vaginal tightening as follows: some improvement, 9; good improvement, 6; and excellent improvement, 7. There was no statistical significance in these results between groups A and B. As for the patient sexual satisfaction compared with the preoperative condition, 21 out of the 30 patients were satisfied (70.0%), made up as follows: somewhat satisfied, 7; satisfied, 5; and extremely satisfied, 9. Group A subjects were significantly more satisfied than subjects in group B (p < 0.05)
Discussion
The important fact from the present study, based on the results of the nonsurgical multiple micropulse mode Er:YAG treatment for vaginal relaxation syndrome, was that all patients completed the study, improvement was seen in both vaginal tightening for all subjects and increased sexual satisfaction was reported for the majority of the total patient population and their partners. The choice of the Er:YAG with its 2940 nm wavelength for this gynecological scanning probe-based system was predicated on the absorption peak of water at that wavelength. As human tissue, especially mucous membranes, has a very high percentage of water, it is a good target for this wavelength. Because of the extremely high absorption in water, the incident photon energy is almost totally quenched in the first few micrometers of tissue, producing at appropriate parameters a very controlled column of ablation with an extremely narrow band of secondary coagulation, known as residual thermal damage (RTD). 4) This translates into shorter downtime with quicker healing, and was the cornerstone of the use of the Er:YAG in full-face ablative laser resurfacing compared with the CO2 laser, which had a much larger RTD zone. 5) For many clinicians practicing laser resurfacing, however, this larger zone of RTD actually made the CO2 laser superior to the Er:YAG in terms of the latency and degree of the result, although use of the CO2 laser dramatically increased the downtime. In the case of the very delicate vaginal canal, however, the depth control associated with the Er:YAG wavelength offers major benefits.
Splitting an Er:YAG laser beam into multiple micropulses further controls the depth of the ablative columns (referred to as microablative columns [MACs]), which allows the deposition of adequate RTD to ensure a healthy and swift wound healing process while leaving undamaged normal tissue between the MACs and thereby speeds up tissue recovery even more because of the participation in the process of the normal tissue. In the delicate tissues of the vaginal canal, it is imperative that the ablative damage depth is minimized, but that enough RTD is created in the target tissue to induce actively the wound healing process, plumping up and rejuvenating the squamous epithelial component of the mucosa, while firming up the connective tissue of the lamina propria (Figure 4) and thus causing tightening of the supportive structures of the vulvovaginal complex.
In the case of the approach in the present study, there were two scanning scopes to deliver the multiple micropulses: the 360° and the 90° scope. The 360° scope delivered a ring-shaped circular beam with micropulse beam width at the target of 2–3 mm, whereas the 90° scope delivered a round beam with a micropulse beam width of around 5 mm at the tissue. For both scopes, the first set of multiple micropulses cleanly created a few µm-thick epidermal window in the vaginal epithelium with minimal RTD, and subsequent micropulses created a pulse-stacking effect without further ablation, but with thermal build-up down into the lamina propria, increasing the RTD zone and ensuring a good wound healing response (Figure 5, left panel). Therefore, taking the respective beam diameters into consideration, to ensure even coverage of the target tissue the 360° scope was withdrawn by 1 increment marked on the scope body after each set of shots, and the 90° scope was withdrawn by 2 increments for each set of shots, each increment representing a distance of 2.5 mm.
Fig. 5:
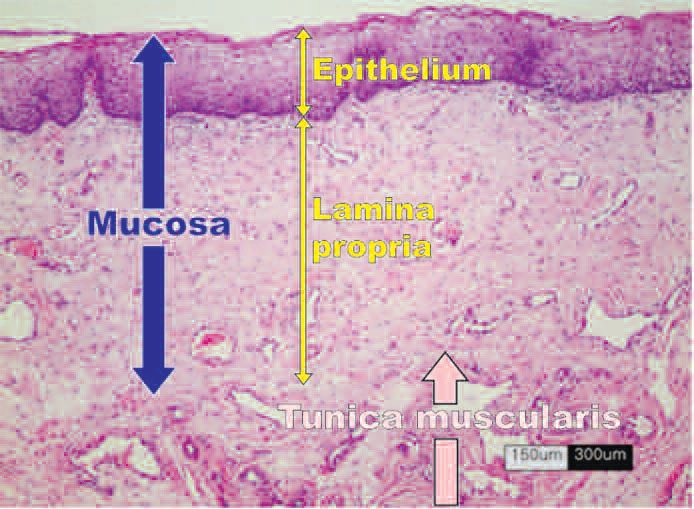
Hematoxylin and eosin-stained section of the anatomy of the vaginal wall, with the various zones labeled.
In the present study, to attempt even better tightening of the vaginal canal through induced enhanced tissue remodeling, it was considered that a more “CO2-like” effect should be delivered to the tissue, i.e. more residual thermal damage with minimal controlled ablation. It was shown as early as 2001 by Trelles and colleagues that the Er:YAG at appropriate parameters could deliver almost as good a coagulative effect as the CO2 through an ablated epidermal window, 6) so for the Group B subjects the 1000 ms long-pulsed mode was added for the last 2 sessions as an adjunct to the 250 µs multiple micropulse mode treatment to deliver more of a thermal effect (Figure 5, right panel).
This protocol actually represents a potential limitation of the present study, because the protocol for group A was not exactly repeated in Group B with the addition of the long-pulsed mode, and this makes it more difficult to compare the effect accurately between the groups with and without the long-pulsed mode. Groups A and B both received 4 sessions, 1–2 weeks apart. However in Group A the first 2 sessions were delivered with the 360° scope, and sessions 3 and 4 with the 90° scope, multiple micropulse mode in all cases. For group B, on the other hand, all 4 sessions were delivered with the 90° scope in multiple micropulse mode, but in the last 2 sessions patients were additionally treated with the 360° scope in the long-pulsed mode. Another limitation was the fact that no specific attention was paid to the urinary incontinence (UI) status of any individual patients, so no conclusions can be drawn as to the efficacy of this approach for UI. However, as UI is one of the major symptoms associated with VRS, improvement in the VRS status could be correlated with improvement of the UI: future studies should address this separately.
When the results in the group of 30 patients are looked at as a whole, significantly better results were seen in the perineometer readings, vaginal tightening and sexual satisfaction. However, the author expected to see better results in Group B because of the additional long-pulsed mode treatment, but as the data show, it was Group A subjects who had the statistically significantly better results, both from the perineometer readings and the subjects' own assessment of sexual satisfaction. This was not a little surprising, especially as Group A was at a more advanced menopausal state than Group B, and so might have had more vaginal atrophy. In addition, subjects in Group A had experienced more natural childbirths than in Group B, with 1 C-section in the former compared to 5 C-sections in the latter: A C-section obviously puts much less strain on the birth canal, especially the vulvovaginal complex. In short, a better result was achieved in Group A whose vaginal canal was in potentially worse physiological condition than Group B.
Overall, however, the objective perineometry readings clearly showed high statistical significance between the baseline and the 2-month post-procedural readings for the entire patient population, as did the patient and partner assessments of sexual satisfaction and vaginal tightening, respectively, so both treatment protocols were efficacious and safe. It is an accepted fact that a fluence delivered by a larger spot size penetrates better and deeper than the same fluence with a small spot size. Why was the result superior in Group A when the pulse energy for the multiple micropulse mode was identical at 15 mJ? The answer is uncertain. Perhaps the order of treatment was important, with the 2-3 mm spot size of the 360° scope for the first 2 sessions, followed by the 90° scope with its 5 mm beam diameter in the Group A protocol. Future studies need to be designed to take these considerations into account, with the addition if possible of histological assessment immediately after treatment to help compare the morphology at baseline with changes in the vaginal architecture following Er:YAG laser treatment with the scanning scope system, and further related with the follow-up results.
Conclusions
Both regimens of Er:YAG laser treatment for VRS and vaginal atrophy with the multiple micropulse mode (Group A) and dual mode (multiple micropulse mode with 2 additional sessions of long-pulse mode, Group B) produced significant improvement in vaginal relaxation with tightening in both the objective perineometer readings, from the results of the partners' assessments of improved vaginal tightness (76.6%), and from the subjects' own improvements in perceived sexual satisfaction (70.0%). This nonsurgical treatment involving multiple micropulse and dual Er:YAG modes with the Er:YAG laser and gynecological probes used in the present study was safe, easily tolerated, pain- and side effect free and effective in the treatment of VRS.
References
- 1: Goodman MP. Female cosmetic genital surgery. Obstet Gynecol, 2009;113:154-159 [DOI] [PubMed] [Google Scholar]
- 2: Davies MC, Creighton SM, Woodhouse CR. The pitfalls of vaginal construction. BJU Int, 2005;95:1293-1298 [DOI] [PubMed] [Google Scholar]
- 3: American College of Obstetricians and Gynecologists (ACOG). Vaginal “Rejuvenation” and Cosmetic Vaginal Procedures (in PDF) (2007)
- 4: Price CR, Carniol PJ, Glaser DA. Skin resurfacing with the erbium:YAG laser. Facial Plast Surg Clin North Am. 2001; 9: 291-302 [PubMed] [Google Scholar]
- 5: Newman JB, Lord JL, Ash K, McDaniel DH. Variable pulse erbium:YAG laser skin resurfacing of perioral rhytides and side-by-side comparison with carbon dioxide laser. Lasers Surg Med, 2000;26:208-214 [DOI] [PubMed] [Google Scholar]
- 6: Trelles MA, Mordon S, Benítez V, Levy JL. Er:YAG laser resurfacing using combined ablation and coagulation modes. Dermatol Surg, 2001; 27:727-34 [DOI] [PubMed] [Google Scholar]


