Abstract
Objective
Although there is a growing interest in the use of acupuncture during pregnancy, the safety of acupuncture is yet to be rigorously investigated. The objective of this review is to identify adverse events (AEs) associated with acupuncture treatment during pregnancy.
Methods
We searched Medline, Embase, Cochrane Central Register of Controlled Trials, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Allied and Complementary Medicine Database (AMED) and five Korean databases up to February 2013. Reference lists of relevant articles were screened for additional reports. Studies were included regardless of their design if they reported original data and involved acupuncture needling and/or moxibustion treatment for any conditions in pregnant women. Studies of acupuncture for delivery, abortion, assisted reproduction or postpartum conditions were excluded. AE data were extracted and assessed in terms of severity and causality, and incidence was determined.
Results
Of 105 included studies, detailed AEs were reported only in 25 studies represented by 27 articles (25.7%). AEs evaluated as certain, probable or possible in the causality assessment were all mild/moderate in severity, with needling pain being the most frequent. Severe AEs or deaths were few and all considered unlikely to have been caused by acupuncture. Total AE incidence was 1.9%, and the incidence of AEs evaluated as certainly, probably or possibly causally related to acupuncture was 1.3%.
Conclusions
Acupuncture during pregnancy appears to be associated with few AEs when correctly applied.
Keywords: Acupuncture, Gynaecology, Obstetrics, Systematic Reviews
Introduction
During pregnancy, women may suffer from various conditions which could affect pregnant women's health as well as normal development and delivery of the infant. Concerns over drug use during pregnancy have helped increase the use of other non-pharmacological treatments. Among them, acupuncture is increasingly practised in pregnant women. In a recent survey of 575 women seeking Chinese medical care, 17.4% received acupuncture for reproductive conditions.1 Another survey in North Carolina reported that acupuncture was used by 19.5% of nurse midwives during pregnancy.2 Evidence of effectiveness of acupuncture during pregnancy is emerging for various conditions.3 4 Recommending acupuncture as a treatment option then depends on its safety, so research on safety of acupuncture for pregnant women is needed urgently.
According to a recent prospective survey on adverse events (AEs) associated with acupuncture,5 the risk of a serious AE with acupuncture is estimated to be 0.01 per 10 000 acupuncture sessions and 0.09 per 10 000 individual patients, which are regarded as ‘very low’. A systematic review on the safety of paediatric acupuncture recently reported that a majority of AEs were mild, and rare serious harms were identified.6 However, sporadic data on the safety of acupuncture during pregnancy are available. Although acupuncture is regarded as highly safe in the general population,5 7 the risk–benefit profile in pregnant women may differ.
This systematic review therefore aimed to summarise and critically evaluate all available reports on AEs associated with acupuncture treatment during pregnancy to safeguard against avoidable AEs.
Methods
Search strategy
Electronic searches were conducted in the following databases from inception to February 2013: Ovid Medline, Cochrane Central Register of Controlled Trials, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and the Allied and Complementary Medicine Database (AMED). We also searched Korean databases including Korean Studies Information Service System (KISS), Korea Institute of Science and Technology Information (KISTI), DBPIA, Korea National Assembly Library and Korean Traditional Knowledge Portal (KTKP). Reference lists of reviews and relevant articles were screened for additional studies. For commentaries, letters, responses or editorials, the original articles were sought.
The following search terms were used: ‘acupunct*’, ‘moxibustion’, ‘moxa’, and ‘pregnan*’ in the title and abstract for Ovid Medline and modified terms and limits were used for other databases. As we were concerned that most articles poorly report AEs and are poorly indexed, we decided not to combine search terms for AEs at the cost of sensitivity. Trials published in English, Korean and Chinese were considered.
Study selection
Studies were included if they (1) had original patient data; (2) involved pregnant women treated for any condition; (3) involved acupuncture treatment which includes needling and/or moxibustion as they are often used together; and (4) included reporting of AEs. Studies reporting that no AEs had occurred were also included. We also kept records of reports that did not mention harms. We excluded studies investigating the effect of acupuncture on delivery, abortion, assisted reproductive technology or postpartum conditions. There was no restriction to the type of studies —that is, we included randomised controlled trials (RCTs), non-randomised controlled clinical trials (CCTs), case series/reports or surveys if they contained unique data. We further sought original articles included or referenced in the reviews, editorials or commentaries for potentially relevant studies.
Data extraction
Two authors (JP and YS) extracted data regarding author(s), publication year, country, study design, sample size, gestational week, condition/symptom for acupuncture treatment, details of acupuncture treatment based on the Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) guidelines,8 control treatment if applicable, practitioner information and detailed information on AEs.
AEs were classified into maternal and fetal outcomes because we deemed both to be clinically relevant and important. The original authors were contacted when further information was needed. Extracted data were validated by another reviewer (HL).
Quality assessment of the included studies
The quality assessment of AE data from RCTs and CCTs included in our review was performed on the following items, which were adopted and modified from previous suggestions.9–12
Was the definition of AEs given?
Was the method used to monitor or collect AEs reported?
Were the type and frequency of AEs in each group reported in detail?
Was the severity of AEs assessed?
Was the causality between acupuncture and AEs assessed?
Were the participant withdrawals or drop-outs due to AEs described adequately?
Each item was given Y for yes, N for no and U for unclear reporting. Disagreements were resolved by discussion.
Data analysis
AE data from divergent sources such as different study designs and data collection methods may be better summarised in a qualitative manner than combining them using meta-analysis.13 Hence, the results were presented descriptively by categorising the data according to the study design. AEs were analysed in terms of severity, causality and incidence.
Severity of the AEs was assessed by the two reviewers (JP and YS) based on the Common Terminology Criteria for AEs (CTCAEs) scale V.4.0.14 The following 5-point grading categories were applied: grade 1, mild (asymptomatic or mild symptoms; clinical or diagnostic observations only; intervention not indicated); grade 2, moderate (minimal, local, or non-invasive intervention indicated; limiting age-appropriate instrumental activities of daily living (ADL)); grade 3, severe or medically significant but not immediately life-threatening (hospitalisation or prolongation of hospitalisation indicated; disabling; limiting self-care ADL); grade 4, life-threatening consequences (urgent intervention indicated); grade 5, death ‘related to AE’.
Causality —that is, the strength of the relationship between AEs and acupuncture treatment—was assessed by two reviewers (JP, acupuncture specialist and YS, obstetrics/gynaecology specialist) in accordance with the causality categories in the World Health Organisation-Uppsala Monitoring Centre system for standardised case causality assessment.15 The causality categories used were certain, probable/likely, possible, unlikely, conditional/unclassified and unassessable/unclassifiable.
The incidence of AEs was presented as the number of AEs per number of acupuncture sessions (%). As we expected that there would be few articles that clearly stated the number of treatment sessions, we adopted the following rules. First, we used the reported mean/median value when a range and the mean/median value were all available in the original study. Second, when the number of treatments varied across participants and only a range value was available, we took the midpoint value between the two extremes. Third, when participants withdrew or dropped out but the number of treatments that they had received was not reported, we considered they were treated once because we judged that the incidence of AEs should be calculated in a conservative manner. Finally, when the number of treatments was not reported at all, we put the number of participants as the denominator. Studies reporting that there were no AEs were included in our incidence analysis.
For sensitivity analysis we compared the incidence of AEs that were originally reported as such in the primary studies with the incidence calculated by including poor pregnancy outcomes which were not reported as AEs. Poor outcomes included perinatal outcomes (eg, miscarriage, stillbirth and neonatal death), congenital abnormalities, pregnancy complications (eg, pre-eclampsia and gestational diabetes) and fetal outcomes.16
Results
Description of studies
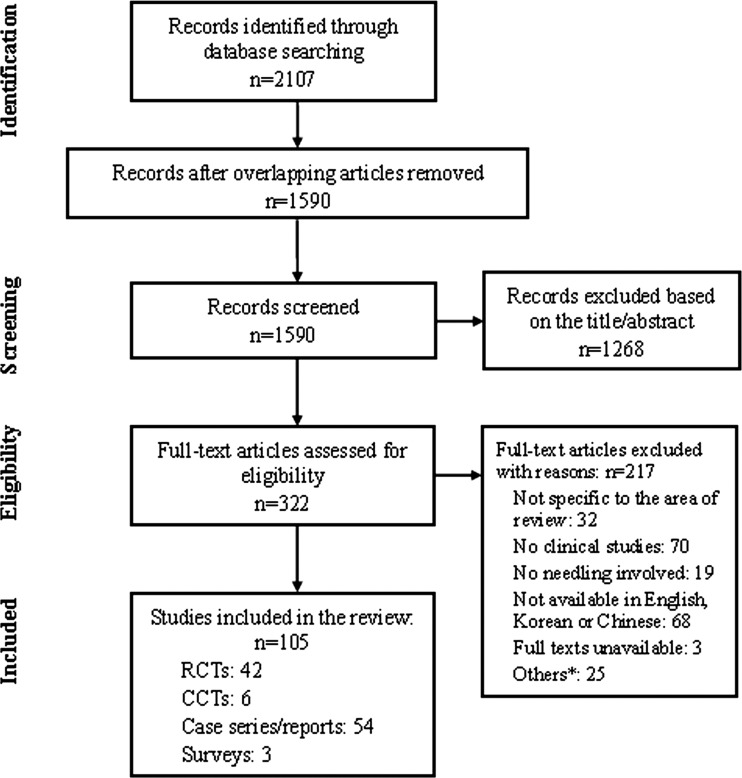
A total of 2107 references were initially identified. Of these, 517 duplicates were removed and 1268 articles were excluded based on the title and abstract. After 217 of the 322 full-text articles were read and further excluded, 105 articles were included in this review: RCTs (n=42), CCTs (n=6), case series/reports (n=54) and surveys (n=3). Figure 1 shows a flow diagram as recommended in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).17 A complete list of included and excluded articles is available by request from the corresponding author.
Figure 1.
Flow diagram of studies included in the systematic review. *Includes 23 commentaries/summary articles, one retracted article and one article with a healthy pregnant woman. CCT, controlled clinical trial; RCT, randomised controlled trial.
Study characteristics
Of the 105 included articles, detailed AEs were extracted from 27 reports (25.7%; 25 studies and 2 additional reports18 19 of the included studies20 21). Of these, the most frequent design was case reports/series (51.4%) followed by RCTs (40.0%), CCTs (5.7%) and surveys (2.9%). A complete list of the other studies which did not mention AEs or reported that no AEs had occurred is provided in online supplementary table S1. Among them, 55 studies did not mention AEs, 22 studies reported there were no AEs and one study22 reported that fewer AEs had occurred in the acupuncture group without a detailed description of AEs. Details of AEs are summarised in online supplementary tables S2 and S3 based on the severity of AEs (mild/moderate AEs in online supplementary table S2 and severe AEs/death in online supplementary table S3); 18 were RCTs,4 18–21 23–36 2 were CCTs37 38 and 5 were case series/reports.39–43
Studies were conducted across several countries: five each in Sweden and Brazil, four in the UK, three in China, two each in the USA and Italy and one each in Australia, Spain, Switzerland and Korea.
The most frequent condition treated with acupuncture was low back pain and/or pelvic pain (n=9) followed by fetal malposition (n=7). The others included nausea and vomiting, tension-type headache, depression, dyspepsia, insomnia, emotional complaints, lateral epicondylitis and back pain, sciatica, rib flare and symphysis pubis dysfunction.
Details of acupuncture interventions are summarised in online supplementary table S4 based on the revised STRICTA.8 Regarding the style of acupuncture, manual acupuncture was most commonly used (n=14), followed by moxibustion to treat fetal malposition (n=7); manual acupuncture plus electroacupuncture, auricular acupuncture alone or auricular acupuncture with or without manual acupuncture were tested in three studies of low back and/or pelvic pain, respectively; one study used manual acupuncture plus bee venom pharmacopuncture for lateral epicondylitis.
The number of acupuncture sessions ranged from 2 to 40 over 5 days to 8 weeks; 12 used fixed treatment, 10 used partially individualised treatment, two used individualised treatments and one did not report detailed information.
Twelve studies used 12 meridian points only, two studies used 12 meridian points, extra meridian points and trigger/tender points, three studies used 12 meridian points and local tender points, three studies used standardised points (12 meridian points and extra meridian points) plus additional points (but the additional points were not clearly reported), two studies used auricular acupuncture with or without local tender points, one study used 12 meridian points and extra meridian points, one used tender or trigger points only and one did not report the acupuncture points used.
In 17 trials involving acupuncture treatment only, the acupuncture treatment was given by acupuncturists in 10 trials, by midwives in three studies and in four studies the practitioner was not stated. In seven moxibustion trials, pregnant women with or without her partner/helper performed moxibustion treatment in three trials, a family member alone provided moxibustion treatment in one study and three trials did not report the relevant information. One study that tested acupuncture plus bee venom pharmacopuncture did not report the relevant information but it was assumed that a doctor gave the treatment.
Severity and causality of AEs associated with acupuncture
We identified a total of 429 AEs in the 27 reports (online supplementary tables S2 and S3). From approximately 22 283 sessions of acupuncture in 2460 pregnant women, 322 AEs were regarded as mild, 6 as moderate, 99 as severe, 2 as death related to AE and 2 were not assessable due to a lack of information. With regard to causality, the AEs were evaluated as certain (n=144), probable (n=15), possible (n=132), unlikely (n=124) or unassessable (n=14). AEs evaluated as certain, probable and possible in the causality assessment were all evaluated as mild or moderate in severity. Severe AEs or death related to AEs were all considered unlikely to have been caused by acupuncture treatment.
Mild/moderate AEs
Among the 322 mild AEs, 302 involved maternal complications: needle or unspecified pain (n=48), local bleeding (n=40), haematoma, tiredness, headache and/or drowsiness (n=21 for each), worsened symptom/condition (n=19), dizziness, discomfort at needling points (n=15 for each), ecchymosis/bruise, uterine contractions with or without abdominal pain, and unpleasant odour with or without nausea and throat problems (n=14 for each), heat or sweating (n=10), nausea (n=9), unpleasantness with treatment (n=5), feeling faint (n=4), sleep disturbance and excessive fatigue (n=3 for each), irritability/agitation, heaviness of arms, rash at needling points, feeling energised, local anaesthesia, itching and unspecified problems (n=2 for each), weakness, altered taste, pressure in nose, transient ear tenderness, bed rest, thirst, sadness, oedema, tattooing of the skin at needling points, shooting sensation with intense paraesthaesia down the leg to the foot by needling, breech engagement, and threatened preterm labour which spontaneously disappeared completely within a day followed by a normal delivery in the 42nd week (n=1 for each). Cardini et al35 reported a sense of tenderness and pressure in the epigastric region and epigastric crushing but they did not state the number of AEs nor the group that experienced the AEs.
Of the mild AEs, fetal adverse outcomes occurred in 20: small for date (n=13) and multiple twists of the umbilical cord around the neck (n=4) or shoulder (n=3).
Six AEs were evaluated as moderate: fainting (n=5) and transient fall in blood pressure (n=1).
Severe AEs
Ninety-nine severe AEs were all considered unlikely to have been caused by acupuncture treatment. In severe AEs, maternal complications were 86: hypertension and/or pre-eclampsia (n=37), preterm delivery between 20 and 37 weeks of pregnancy (n=19), miscarriage (n=15), premature rupture of the membranes (n=5), antepartum haemorrhage/abruption or placenta praevia (n=6), pregnancy termination due to unspecified reasons (n=2), cesaerean delivery (n=1), and tachycardia and atrial sinus arrhythmia (n=1). The 15 miscarriages were all reported from one study19 21 in which the participants received five sessions of acupuncture over a month for nausea and vomiting in early pregnancy. The reported miscarriage rate of 5% (15/293 in the acupuncture in addition to usual care group, 6/147 in the sham acupuncture in addition to usual care group and 9/143 in the usual care only group) was lower than the population risk estimate of 11% in Australia, suggesting that acupuncture was not associated with a higher risk of miscarriage.
Fetal complications were congenital defects (n=12) and admission to neonatal intensive care unit due to preterm delivery (n=1).
Death related to AE
Two deaths were reported: one stillbirth and one neonatal death. Manber et al28 reported premature delivery of twins with one unexpected neonatal death which was classified as unrelated to acupuncture by the study investigators and the Data Safety and Monitoring Board. We also evaluated them as unlikely in the causality assessment. The lack of acupuncture-related maternal mortality is worthy of note.
Incidence of AEs
The incidence of AEs based on study design is shown in online supplementary table S5. The total incidence of AEs in the acupuncture group was 1.9% (429 AEs in 22 283 sessions), and limiting the calculation to AEs evaluated as certain, probable and possible in the causality assessment resulted in an incidence of 1.3% (291 AEs in 22 283 sessions). In other words, the incidence of AEs amounted to 193 and 131 AEs per 10 000 acupuncture sessions, respectively. The risk of mild or moderate AEs was 1.5%, estimated to be 147 per 10 000 treatments. There were no serious AEs or deaths probably causally related to acupuncture in 10 000 treatments.
Sensitivity analysis
When poor outcomes that were not reported as AEs in the original articles were counted as AEs, the total AE incidence in the acupuncture group was 4.8% (1067 AEs in 22 283 sessions) and limiting this to AEs evaluated as certain, probable and possible in the causality assessment resulted in 1.9% (418 AEs in 22 283 sessions). This is more than twice that of our original analysis (total AE incidence 1.9%) which included reported AEs only. Nevertheless, these values are comparable to or lower than those investigated in the general population receiving acupuncture treatment (table 1).
Table 1.
Estimated AE incidences associated with acupuncture treatment compared with previous studies*
| Author (year) Country |
Design | Condition | No. of patients | AE incidence (per 10 000 sessions) | Most frequent AEs | Authors’ comments |
|---|---|---|---|---|---|---|
| Yamashita (2000)44 Japan |
Prospective survey | NR† | 391 | 6849 | Tiredness, drowsiness, symptom aggravation, minor bleeding on needle withdrawal | ‘Although some adverse reactions associated with acupuncture were common even in standard practice, they were transient and mild.’ |
| White (2001)45 UK |
Prospective survey | NR‡ | NR | 671 | Bleeding or haematoma, needling pain | ‘All AEs were mild and no serious AE occurred.’ |
| Witt (2009)5 Germany |
Prospective survey | Chronic OA, LBP, neck pain, headache, allergic rhinitis, asthma or dysmenorrhoea | 229 230 | 111 | Bleeding or haematoma, pain | ‘Acupuncture provided by physicians is a relatively safe treatment.’ |
| Park (2009)7 Korea |
Retrospective survey | CVA, headache, hypertension, dizziness, numbness and others | 1095 | 339 | Minor bleeding | ‘Acupuncture treatment is safe if the practitioners are well educated, trained, and experienced.’ |
| Present study (2013) Various |
Systematic review | Various conditions in pregnant women | 2460 | 131§/188¶ | Needling pain | ‘Acupuncture during pregnancy appears to be associated with few AEs when correctly applied.’ |
*Incidence rate may slightly vary as definition of AEs, survey methods or acupuncture methods are all different across studies.
†Patients receiving acupuncture treatments at Tsukuba College of Technology Clinic in Japan.
‡Patients receiving acupuncture treatments from medical doctors and physiotherapists in the UK.
§AE incidence varies: 193 per 10 000 acupuncture sessions when the analysis included reported AEs in the original reports; 131 per 10 000 acupuncture sessions when the calculation is limited to the AEs evaluated as certain, probable or possible in the causality assessment.
¶AE incidence varies: 479 per 10 000 when the calculation is expanded to poor pregnancy outcomes which were not originally reported as acupuncture-related AEs and, among them, 188 were evaluated as certain, probable or possible in the causality assessment.
AE, adverse event; CVA, cerebrovascular accident; LBP, low back pain; NR, not reported; OA, osteoarthritis.
Quality assessment of AE data from RCTs and CCTs
We assessed the quality of AE data from RCTs and CCTs based on six predetermined items (table 2). The quality of data reporting was mostly poor. Only one study (5.0%)19 21 provided a definition of AEs. Eight out of 20 studies (40.0%) reported the method used to collect AEs: three studies used direct questioning,1,8 20 26 3,4 two used patient diaries,28 33 one used a questionnaire,36 Vas et al4 used patient case notes, direct questioning and a questionnaire and Smith et al19 21 used direct questioning and patient case notes. Ninety percent of studies reported the type and frequency of AEs in each group but none stated the severity; only Elden et al18 20 assessed the severity of some but not all of the reported AEs. Two studies4 35 did not state in which group the AEs had occurred. Only one of the included studies assessed the causality between acupuncture treatment and reported AEs.28 Seventeen of the 20 trials adequately described the participant withdrawals and drop-outs due to AEs. In two studies it was impracticable to extract data on withdrawals and drop-outs relevant to AEs; one study29 did not report the reason for withdrawals and another32 did not mention the withdrawals and drop-outs at all. Cardini et al31 stated the reason for withdrawals but it was not sufficiently clear.
Table 2.
Assessment of the quality of AE data from RCTs and CCTs included in the review
| Author (year) | Was the definition of AEs given? | Was the method used to monitor or collect AEs reported? | Were the type and frequency of AEs in each group reported in detail? | Was the severity of AEs assessed? | Was the causality between acupuncture and AEs assessed? | Were the participant withdrawals and drop-outs due to AEs described adequately? |
|---|---|---|---|---|---|---|
| RCTs/quasi-RCTs | ||||||
| Vas (2013)4 | N | Y | N | N | N | Y |
| Guerreiro da Silva (2012)23 | N | N | Y | N | N | Y |
| Manber (2010)28 | N | Y | Y | N | Y | Y |
| Guerreiro da Silva (2009)24 | N | N | Y | N | N | Y |
| Wang (2009)29 | N | N | Y | N | N | N |
| Elden (2008)46 | N | N | Y | N | N | Y |
| Guittier (2008)36 | N | Y | Y | N | N | Y |
| Guerreiro da Silva (2007)25 | N | N | Y | N | N | Y |
| Guerreiro da Silva (2005)26 | N | Y | Y | N | N | Y |
| Elden (2005)18 20 | N | Y | Y | N | N | Y |
| Du (2005)30 | N | N | Y | N | N | Y |
| Cardini (2005)31 | N | N | Y | N | N | U |
| Guerreiro da Silva (2004)27 | N | N | Y | N | N | Y |
| Kvorning (2004)32 | N | N | Y | N | N | N |
| Smith (2002)19 21 | Y | Y | Y | N | N | Y |
| Knight (2001)33 | N | Y | Y | N | N | Y |
| Wedenberg (2000)34 | N | Y | Y | N | N | Y |
| Cardini (1998)35 | N | N | N | N | N | Y |
| CCTs | ||||||
| Liang (2004)37 | N | N | Y | N | N | Y |
| Cardini (1993)38 | N | N | Y | N | N | Y |
AE, adverse event; CCT, controlled clinical trial; N, no; RCT, randomised controlled trial; U, unclear; Y, yes.
Discussion
Main findings
This systematic review has found that the majority of AEs associated with acupuncture during pregnancy are mild and transient, and serious AEs are very rare. Needling or unspecified pain was the most commonly reported mild AE, followed by bleeding. AEs were largely mild in severity. We found acupuncture treatment during pregnancy was associated with few serious AEs and all of them were evaluated as unlikely to have been caused by acupuncture treatment. The estimated incidence of AEs associated with acupuncture in pregnant women was 193 per 10 000 acupuncture sessions. Limiting the calculation to AEs evaluated as certain, probable or possible in the causality assessment resulted in an incidence of 131 per 10 000 treatments. These values are comparable to or less serious than those investigated in the general population receiving acupuncture treatment (table 1).
Interpretation of review findings
There are some specific issues worth mentioning in this review. Rare AEs associated with treatment are difficult to study and are usually published as case reports. The incidence of AEs is best estimated in large prospective surveys and, in acupuncture research, there are some large surveys from the general population.5 45 47 In general, commonly reported mild AEs associated with acupuncture include bleeding or haematoma, pain and tiredness or drowsiness.5 44 Pneumothorax, infection and nerve lesions have been reported as serious AEs, although they are rare.5 48 In our review, needling pain and bleeding were the most common mild AEs and the incidence was similar to those from previous studies. Severe AEs (primarily hypertension and/or pre-eclampsia in the mother and congenital defects in the baby) were all evaluated as unlikely to have been caused by acupuncture treatment. While the incidence of serious AEs is higher than those from other trials,7 45 49 this may be attributable to special characteristics of pregnant women. Deaths related to AEs were all stillbirths or neonatal deaths which were unlikely to have been due to acupuncture. What should be noted here is that AEs did occur in pregnant women but most of them were mild and transient, and severe AEs such as pneumothorax and nerve lesions were not recorded at all.
Strengths and limitations of this review
The assessment of the benefit–harm profile should also be considered in the context of the nature of the condition for which the intervention is applied.13 This review looks at the important population of pregnant women who may be different from the general population in several respects. As pregnant women have relatively limited treatment options for pregnancy-specific and/or general health problems because of the fear of miscarriage, premature delivery or teratogenicity, solid evidence on the safety of acupuncture is all the more needed. To our knowledge, this is the first systematic review dealing with this topic.
Some limitations of this review should be noted. There is a lack of appropriate information regarding obstetric complications, particularly in the case of the most serious complications such as maternal and perinatal mortality. It may be difficult to make any meaningful conclusions about these important AEs. Hemminki et al50 found that unpublished trials gave more information on AEs than published trials. We may have missed relevant articles or unpublished data. Due to limited resources, we only included trials published in English, Korean and Chinese. However, as the AE results did not significantly differ across countries,5 7 45 the excluded studies may not have significantly reversed the overall picture.
Although every medical intervention carries some risk of AEs, the research focus has been on the benefit of the intervention and information on harm has been neglected. Inadequate reporting of harms has been ubiquitous in conventional medicine as well as in complementary and alternative medicine.51 52 The absence of reported AEs thus does not mean that there are not any. In our review, AEs were reported from only 25.7% of the included studies, the most frequent design being case reports/series followed by RCTs, CCTs and surveys. Each of the different designs has pros and cons: observational studies are useful to identify AEs which have long latent periods or are unusual, but these reports do not provide information on the incidence due to a lack of denominator data. Clinical trials are useful in determining the incidence but are unsuitable for new, rare or long-term AEs and may only provide limited information on AEs due to exclusion of patients at high risk because of comorbidity. Surveys also have limitations such as recall bias which occurs intentionally or unintentionally in the recollection and reporting process. The overall incidence of AEs associated with acupuncture for pregnant women in this review therefore may be just an approximation of the true value. All but one19 21 of the included RCTs and CCTs did not predefine potential AEs, and the definition of AEs may have been different across studies. Methods of monitoring or collecting AE data were not clear in 60% of studies. Evidence from our review therefore may be incomplete and susceptible to reporting and publication bias.
While most included trials satisfactorily reported the type and frequency of AEs and the withdrawals or drop-outs due to AEs in each group, the definition and severity of AEs, causality between the intervention and AEs and the collecting and monitoring methods of AEs were generally poorly reported. Only 25.7% provided safety information and 52.4% did not mention AEs at all. For studies reporting that there were no AEs (21%) it is assumed that they were not ascertained or recorded.13 Thus we may not be entirely free from risk of having underestimated the AE incidence.
Clinical implications of this review
Controversies about so-called ‘forbidden points in pregnancy’ exist.53 Some experimental studies suggest no evidence on harm by needling LI4, SP6 or sacral points54 55 while others argue that the classic literature should be taken into consideration on the basis of the potential physiological mechanisms whereby acupuncture may adversely affect pregnancy.56 However, the suggested mechanisms have been refuted,53 and a recent literature review failed to find any plausible explanation for repeatedly or differently mentioned forbidden points across books.57 In this context, this systematic review found that AEs associated with acupuncture during pregnancy are generally mild, and serious AEs are rare. The present findings should be given to pregnant women together with effectiveness data so that they can make an informed decision. In addition, future large prospective studies would give us better information and a more accurate estimate of AEs associated with acupuncture in pregnant women.
Supplementary Material
Acknowledgments
We thank the original authors who sent us their articles when contacted.
Footnotes
Contributors: HL and JP designed the review, searched databases and screened studies for inclusion. JP and YS extracted data and evaluated the quality of AE data, which was checked by HL. HL and JP performed analyses and discussed with ARW. All authors read and approved the final manuscript.
Funding: This research was supported by the National Research Foundation of Korea (NRF) grants funded by the Korea government (Ministry of Science, ICT & Future Planning) (Nos. 2005-0049404&2013R1A6A6029251).
Competing interests: ARW receives editorial fees, lecture fees and travel expenses from BMAS and royalties from Elsevier in relation to acupuncture but not in relation to the present work.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Cassidy CM. Chinese medicine users in the United States. Part I: utilization, satisfaction, medical plurality. J Altern Complement Med 1998;4:17–27 [DOI] [PubMed] [Google Scholar]
- 2.Allaire AD, Moos MK, Wells SR. Complementary and alternative medicine in pregnancy: a survey of North Carolina certified nurse-midwives. Obstet Gynecol 2000;95:19–23 [DOI] [PubMed] [Google Scholar]
- 3.Pennick V, Liddle SD. Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database Syst Rev 2013;8:CD001139. [DOI] [PubMed] [Google Scholar]
- 4.Vas J, Aranda-Regules JM, Modesto Met al. Using moxibustion in primary healthcare to correct non-vertex presentation: a multicentre randomised controlled trial. Acupunct Med 2013;31:31–8 [DOI] [PubMed] [Google Scholar]
- 5.Witt CM, Pach D, Brinkhaus Bet al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forsch Komplementmed 2009;16:91–7 [DOI] [PubMed] [Google Scholar]
- 6.Adams D, Cheng F, Jou Het al. The safety of pediatric acupuncture: a systematic review. Pediatrics 2011;128:e1575–87 [DOI] [PubMed] [Google Scholar]
- 7.Park SU, Ko CN, Bae HSet al. Short-term reactions to acupuncture treatment and adverse events following acupuncture: a cross-sectional survey of patient reports in Korea. J Altern Complement Med 2009;15:1275–83 [DOI] [PubMed] [Google Scholar]
- 8.MacPherson H, Altman DG, Hammerschlag Ret al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. PLoS Med 2010;7:e1000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centre for Reviews and Dissemination (CRD). Chapter 4: Systematic reviews of adverse effects . In: Systematic Reviews: CRD's guidance for undertaking reviews in health care. York: Center for Reviews and Dissemination, 2009:177–97 [Google Scholar]
- 10.Loke Y. Chapter 14: Adverse effects. In: Higgins J, Green S. eds Cochrane handbook for systematic reviews of interventions version 5.1.0. Chichester, UK: The Cochrane Collaboration, John Wiley & Sons, 2011:1–13 [Google Scholar]
- 11.Ioannidis JP, Evans SJ, Gotzsche PCet al. Better reporting of harms in randomised trials: an extension of the CONSORT statement. Ann Intern Med 2004;141:781–8 [DOI] [PubMed] [Google Scholar]
- 12.Edwards JE, McQuay HJ, Moore RAet al. Reporting of adverse effects in clinical trials should be improved: lessons from acute postoperative pain. J Pain Symptom Manage 1999;18:427–37 [DOI] [PubMed] [Google Scholar]
- 13.Loke YK, Price D, Herxheimer A. Systematic reviews of adverse effects: framework for a structured approach. BMC Med Res Methodol 2007;7:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Cancer Institute. Grading: General Characteristics of the CTCAE (Common Terminology Criteria for Adverse Events) Grading (Severity) Scale. 2012. http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5×7.pdf (accessed 19 Jul 2012).
- 15.World Health Organization (WHO)-Uppsala Monitoring Centre. The use of the WHO-UMC system for standardized case causality assessment. 2012. http://www.who-umc.org/Graphics/24734.pdf (accessed 19 Jul 2012).
- 16.Scheil W, Scott J, Catcheside B,et al. Pregnancy outcome in South Australia 2010. Adelaide: Pregnancy Outcome Unit, SA Health, Government of South Australia, 2012 [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff Jet al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264–9, W64 [DOI] [PubMed] [Google Scholar]
- 18.Elden H, Ostgaard HC, Fagevik-Olsen Met al. Treatments of pelvic girdle pain in pregnant women: adverse effects of standard treatment, acupuncture and stabilizing exercises on the pregnancy, mother, delivery and the fetus/neonate. BMC Complement Altern Med 2008;8:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith C, Crowther C, Beilby J. Pregnancy outcome following women's participation in a randomised controlled trial of acupuncture to treat nausea and vomiting in early pregnancy. Complement Ther Med 2002;10:78–83 [DOI] [PubMed] [Google Scholar]
- 20.Elden H, Ladfors L, Olsen MFet al. Effects of acupuncture and stabilizing exercises as adjunct to standard treatment in pregnant women with pelvic girdle pain: randomised single blind controlled trial. BMJ 2005;330:761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith C, Crowther C. The placebo response and effect of time in a trial of acupuncture to treat nausea and vomiting in early pregnancy. Complement Ther Med 2002;10:210–16 [DOI] [PubMed] [Google Scholar]
- 22.Manyande A, Grabowska C. Factors affecting the success of moxibustion in the management of a breech presentation as a preliminary treatment to external cephalic version. Midwifery 2009;25:774–80 [DOI] [PubMed] [Google Scholar]
- 23.Guerreiro da Silva JB, Nakamura MU, Cordeiro JAet al. Acupuncture for tension-type headache in pregnancy: a prospective, randomised, controlled study. Eur J Integr Med 2012;4:366–70 [Google Scholar]
- 24.Guerreiro da Silva JB, Nakamura MU, Cordeiro JAet al. Acupuncture for dyspepsia in pregnancy: a prospective, randomised, controlled study. Acupunct Med 2009; 27:50–3 [DOI] [PubMed] [Google Scholar]
- 25.Guerreiro da Silva JB. Acupuncture for mild to moderate emotional complaints in pregnancy—a prospective, quasi-randomised, controlled study. Acupunct Med 2007;25:65–71 [DOI] [PubMed] [Google Scholar]
- 26.Guerreiro da Silva JB, Nakamura MU, Cordeiro JAet al. Acupuncture for insomnia in pregnancy—a prospective, quasi-randomised, controlled study. Acupunct Med 2005;23:47–51 [DOI] [PubMed] [Google Scholar]
- 27.Guerreiro da Silva JB, Nakamura MU, Cordeiro JAet al. Acupuncture for low back pain in pregnancy—a prospective, quasi-randomised, controlled study. Acupunct Med 2004;22:60–7 [DOI] [PubMed] [Google Scholar]
- 28.Manber R, Schnyer RN, Lyell Det al. Acupuncture for depression during pregnancy: a randomized controlled trial. Obstet Gynecol 2010;115:511–20 [DOI] [PubMed] [Google Scholar]
- 29.Wang SM, Dezinno P, Lin ECet al. Auricular acupuncture as a treatment for pregnant women who have low back and posterior pelvic pain: a pilot study. Am J Obstet Gynecol 2009;201:271 e1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Du YH, Xue AJ. Clinical observation of integrative medicine to correct malposition in 50 cases. Modern J Integr Trad Chin West Med 2005;14:2727 [Google Scholar]
- 31.Cardini F, Lombardo P, Regalia ALet al. A randomised controlled trial of moxibustion for breech presentation. BJOG 2005;112:743–7 [DOI] [PubMed] [Google Scholar]
- 32.Kvorning N, Holmberg C, Grennert Let al. Acupuncture relieves pelvic and low-back pain in late pregnancy. Acta Obstet Gynecol Scand 2004;83:246–50 [DOI] [PubMed] [Google Scholar]
- 33.Knight B, Mudge C, Openshaw Set al. Effect of acupuncture on nausea of pregnancy: a randomized, controlled trial. Obstet Gynecol 2001;97:184–8 [DOI] [PubMed] [Google Scholar]
- 34.Wedenberg K, Moen B, Norling A. A prospective randomized study comparing acupuncture with physiotherapy for low-back and pelvic pain in pregnancy. Acta Obstet Gynecol Scand 2000;79:331–5 [PubMed] [Google Scholar]
- 35.Cardini F, Weixin H. Moxibustion for correction of breech presentation: a randomized controlled trial. JAMA 1998;280:1580–4 [DOI] [PubMed] [Google Scholar]
- 36.Guittier MJ, Klein TJ, Dong Het al. Side-effects of moxibustion for cephalic version of breech presentation. J Altern Complement Med 2008;14:1231–3 [DOI] [PubMed] [Google Scholar]
- 37.Liang JL, Chen SR, Li YP. Comparative analysis of moxibustion at Zhiyin acupoint and knee-chest posture in correcting breech presentation, report of 320 cases. Chin Med 2004;17:11–12 [Google Scholar]
- 38.Cardini F, Marcolongo A. Moxibustion for correction of breech presentation: a clinical study with retrospective control. Am J Chin Med 1993;21:133–8 [DOI] [PubMed] [Google Scholar]
- 39.Ahn BJ, Song HS. A case report of patient in pregnancy with external epicondylitis. J Kor Acupunct Moxibust Soc 2011;28:137–41 [Google Scholar]
- 40.Bourne A. The use of acupuncture as a treatment for pelvic girdle pain during pregnancy in a multiparous woman. AACP 2007;2007:77–85 [Google Scholar]
- 41.Cummings M. Acupuncture for low back pain in pregnancy. Acupunct Med 2003;21:42–6 [DOI] [PubMed] [Google Scholar]
- 42.De Jonge-Vors C. Reducing the pain: midwifery acupuncture service audit in Birmingham. Practising Midwife 2011;14:22–6 [Google Scholar]
- 43.Kvorning N, Grennert L, Aberg Aet al. Acupuncture for lower back and pelvic pain in late pregnancy: a retrospective report on 167 consecutive cases. Pain Med 2001;2:204–7 [DOI] [PubMed] [Google Scholar]
- 44.Yamashita H, Tsukayama H, Hori Net al. Incidence of adverse reactions associated with acupuncture. J Altern Complement Med 2000;6:345–50 [DOI] [PubMed] [Google Scholar]
- 45.White A, Hayhoe S, Hart Aet al. Adverse events following acupuncture: prospective survey of 32000 consultations with doctors and physiotherapists. BMJ 2001;323:485–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Elden H, Fagevik-Olsen M, Ostgaard HCet al. Acupuncture as an adjunct to standard treatment for pelvic girdle pain in pregnant women: randomised double-blinded controlled trial comparing acupuncture with non-penetrating sham acupuncture. BJOG 2008;115:1655–68 [DOI] [PubMed] [Google Scholar]
- 47.MacPherson H, Thomas K, Walters Set al. The York acupuncture safety study: prospective survey of 34000 treatments by traditional acupuncturists. BMJ 2001;323:486–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ernst E. Deaths after acupuncture: a systematic review. Int J Risk Saf Med 2010;22:131–6 [Google Scholar]
- 49.Melchart D, Weidenhammer W, Streng Aet al. Prospective investigation of adverse effects of acupuncture in 97733 patients. Arch Intern Med 2004;164:104–5 [DOI] [PubMed] [Google Scholar]
- 50.Hemminki E. Study of information submitted by drug companies to licensing authorities. BMJ 1980;280:833–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Turner LA, Singh K, Garritty Cet al. An evaluation of the completeness of safety reporting in reports of complementary and alternative medicine trials. BMC Complement Altern Med 2011;11:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ioannidis JP, Lau J. Completeness of safety reporting in randomised trials: an evaluation of 7 medical areas. JAMA 2001;285:437–43 [DOI] [PubMed] [Google Scholar]
- 53.Cummings M. ‘Forbidden points’ in pregnancy: no plausible mechanism for risk. Acupunct Med 2011;29:140–2 [DOI] [PubMed] [Google Scholar]
- 54.Guerreiro da Silva AV, Nakamura MU, Cordeiro JAet al. The effects of so-called 'forbidden acupuncture points’ on pregnancy outcome in wistar rats. Forsch Komplementmed 2011;18:10–14 [DOI] [PubMed] [Google Scholar]
- 55.Guerreiro da Silva AV, Nakamura MU, Guerreiro da Silva JBet al. Could acupuncture at the so-called forbidden points be harmful to the health of pregnant Wistar rats? Acupunct Med 2013;31:202–6 [DOI] [PubMed] [Google Scholar]
- 56.Betts D, Budd S. Forbidden points’ in pregnancy: historical wisdom? Acupunct Med 2011;29:137–9 [DOI] [PubMed] [Google Scholar]
- 57.Chang L, Sohn YJ, Lee YBet al. A traditional literature review on acupuncture and moxibustion during pregnancy. Kor J Acupunct 2011;28:87–104 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.