Abstract
The purpose of this study was to determine the trajectories of depressive symptoms as older youths from the foster care system mature while also examining the correlates of these trajectories. Data came from a longitudinal study of 404 youths from the foster care system in Missouri, who were interviewed nine times between their 17th and 19th birthdays. Depression was assessed with the Depression Outcomes Module and the Diagnostic Interview Schedule for DSM-IV. Data best fit a model of three trajectory classes, describing young people (1) maintaining low levels of depressive symptoms (never depressed class, 78%), (2) with increasing symptoms (increasing class, 6%), and (3) with decreasing symptoms (decreasing class, 15%). The increasing depression group was mostly male youths who were working or in school; the decreasing class was mostly highly maltreated female youths exiting the foster care system from residential care, with low levels of employment, and in school. Implications for social work practice are discussed.
Keywords: depression, foster cate, trajectories, transition
Foster youths are at increased risk of depression due to a variety of factors, including inherited vulnerability, child maltreatment, and the potential insults of the foster care system itself, including multiple moves and repeated relationship losses (Kaufman, 1991; McMillen et al., 2005). The over 26,000 young people who “age out” of the U.S. foster care system each year (U.S. Department of Health and Human Services, 2008), however, are thought to be at even greater risk for depression when they leave care. Some reasons for this may be the density of life transitions they experience, including the loss of mental health services, and a potential realization that their skills and resources are not adequate to meet the demands of living life more independently. The purpose of this study was to understand the nature of depressive symptoms among older youths transitioning from one midwestern state’s foster care system. This was achieved through examination of the rates of past-year depression at ages 17 and 19, depressive symptom trajectories, the correlates of trajectory classes, and the relationships between trajectory class membership and functional outcomes. Social work plays a leading role in serving older youths exiting foster care, and this study informs the field on how their depressive symptoms present during the transition to adulthood.
BACKGROUND
Clinical Course of Depression during the Transition Years
Older adolescence is often filled with dense transitions in education, living situation, employment, and relationships (Rindfuss, 1991). Scholars have suggested that this can be a time when “things come undone” for vulnerable youths, especially if the resources and supports necessary to make the transition to adulthood are not available (Osgood, Foster, Flanagan, & Ruth, 2005). Epidemiological research has revealed high prevalence rates of depressive disorders during the transition years, roughly ages 16 to 25 (Giaconia et al., 1994; Kessler et al., 1994; Newman et al., 1996). Prevalence rates for depression steadily increase with age, peaking during adolescence and into adulthood (Burke, Burke, Regier, & Rae, 1990). Although depression is treatable, scores of youths with depression do not seek treatment (Keller, Lavori, Beardslee, Wunder, & Ryan, 1991), and many with mental disorders often drop out of services prematurely (Kazdin, 1996). This magnifies concerns, given that depression among adolescents has been associated with substance use, academic underachievement, unemployment, and teenage pregnancy (Diego, Field, & Sanders, 2003; Fergusson & Woodward, 2002; Lewinsohn, Rohde, Seeley, Klein, & Gotlib, 2003). Increasing knowledge about depression during the transition years for our most vulnerable citizens is critical to understanding how to best target both depression prevention and management efforts.
Theories of Depression
There are multiple pathways to experiencing the onset of a depressive episode. One of the most empirically supported theoretical perspectives on the etiology of depression is the stress-diathesis model (Abramson, Metalsky, & Alloy, 1989; Beck, 1976; see Stark et al., 2006, for a review), which purports that stressful life circumstances—such as poverty, victimization, or family dysfunction—interact with a genetic vulnerability to cause depression (Costello et al., 2002; Garber, Keiley, & Martin, 2002; Stark, Laurent, Livingston, Boswell, & Swearer, 1999). Behavior geneticists add support to the gene—environment theory, as they have found that response to stressful environmental situations is moderated by a person’s genes (Caspi et al., 2003). Of particular interest for the present study is the relationship between victimization and depression (Turner, Finkelhor, & Ormrod, 2006; Widom, DuMont, & Czaja, 2007; Wise, Zierler, Krieger, & Harlow, 2001). Widom et al. (2007) used prospective data and found that childhood abuse and neglect were associated with roughly a 1.5 increase in the odds of adult depression, with even higher odds when adults had experienced multiple types of abuse.
The present study, with its focus on foster youths, involved a highly victimized sample. It is probable that leaving foster care carries different risks for older youths, depending on their genetic makeup, their pre- and postnatal environments, their early childhood experiences, and their adolescent experiences. Although not testing the stress-diathesis model, we used an integrative framework to understand depressive symptom trajectories among older youths exiting foster care by modeling individual, parental, and environmental factors to examine depressive symptom changes as these youths move toward adulthood.
Depression among Older Youths Nearing Their Exit from Foster Care
Child welfare professionals have long viewed young people in and leaving the foster care system as particularly vulnerable to depression. Even before the burdens of transitioning out of the care system, these children are thought to be at increased risk for depression as a result of both the adversities they have faced and the potential genetic liability inherited from parents who struggled to care for them (Kaufman, 1991; Widom et al., 2007). A recent study by McMillen et al. (2005) supports this view, as they found a lifetime prevalence rate of 27% for major depression among a group of 17-year-old youths in the foster care system, a rate higher than those found in the general population—that is, 18% (Lewinsohn, Hops, Roberts, Seeley, & Andrews, 1993) and 16.8% (Newman et al., 1996). In an earlier article, Anderson and Simonitch (1981) suggested that reactive depression was likely common among these youths as they left foster care. They speculated that older youths initially feel elated at leaving controlling public systems, but this is quickly followed up by fear, loneliness, irritability, and, ultimately, depression as they realize their resources are not adequate to meet life’s demands. In a small volunteer sample of older youths who left the foster care system approximately three years prior, Barth (1990) found that the mean score on the Center for Epidemiologic Studies Depression Scale was above the clinical cutoff score. To further investigate the reactive depression hypothesis, the present study examined whether there is a spike in depressive symptoms as older youths leave foster care. Understanding the prevalence of reactive depression among older youths leaving public service systems can help determine the need for depression prevention or depression management efforts that can be implemented for young people while they are in public care.
Trajectories of Depression
As methods to investigate depression have improved, studies examining depressive trajectories, or patterns of symptoms over time, have come to the forefront. Studies often identify three or four distinct paths of depressive symptoms, namely a consistently high group, a consistently low group, and one or two other groups that vary depending on the study.
Stoolmiller, Kim, and Capaldi (2005) reported that negative life events and parental depression predicted a greater likelihood of membership in a trajectory class evidencing high-persistent depressive symptoms during the transition to adulthood. Garber et al. (2002) found that adolescents with mothers who live with mood disorders had higher initial levels of depressive symptoms when compared with those with mothers who had no such history. Although research has shown that girls have higher rates of depression during adolescence (Birmaher et al., 1996), the evidence regarding gender and growth in depressive symptoms has been mixed. In an early study of adolescents, there were no significant gender differences in the presentation of depressive symptoms over a two-year period (DuBois, Felner, Bartels, & Silverman, 1995); however, another study found that depressive symptoms among girls increased at an earlier age and among boys they remained more stable (Ge, Conger, & Elder, 2001). The present study further examined gender as a predictor of trajectory class. As the literature on depression trajectories remains in its infancy, this Study drew from literature examining factors related to depression, including minority race status (that is, Rushton, Forcier, & Schcctman, 2003) and substance use (that is, Schuckit et al., 1997). We examined other potential predictors of depressive trajectories among foster care youths, such as living situation, juvenile justice involvement, teenage parenthood, and changes in mental health service use.
Finally, this study examined whether depressive trajectory class is associated with functional outcomes. Dekker et al. (2007) found that among boys, those in the elevated trajectory classes had lower educational attainment. As reviewed earlier, research has shown that the presence of depression, or depressive symptoms, is related to functioning in other important key areas of adult life. Understanding these relationships can help determine the importance of depression trajectories and what outcomes may be improved by altering them.
The present study examined the following six questions among older youths exiting foster care: (1) How do the rates of past-year major depression compare from age 17 to age 19? (2) Do depression symptoms change over time and as youths leave the system? (3) What are the trajectories of depression symptoms? (4) What factors are related to depression trajectory classes? (5) Do trajectories look different when examining them in relation to mental health service use? (6) Are outcomes associated with trajectory classes? There were four hypotheses: (1) Depression symptoms will increase from age 17 to age 19; (2) depression symptom scores will spike after youths leave care; (3) depression trajectory classes will vary by gender; and (4) trajectories of depression will be associated with developmental young adult functional outcomes, with those experiencing more depression symptoms having poorer outcomes at age 19.
METHOD
Participants
The present study was a longitudinal survey study of 404 older youths from the foster care system in Missouri, originally conceived to study the menial health service use of these youths as they transitioned toward adulthood. The protocol called for nine quarterly interviews by professional interviewers between participants’ 17th and 19th birthdays. All participants were in the legal custody of the state child welfare authority at first interview. From December 2001 to May 2003 the Missouri Children’s Division (MCD) provided to the research team lists of the names of youths who would be turning 17 the following month, along with the names of their caseworkers. Youths were recruited from eight counties, accounting for four of the seven administrative regions of the MCD. These counties included the St. Louis metro area, surrounding counties, and counties in rural Missouri. Potential participants were screened by their caseworkers for exclusion criteria, which included an IQ score less than 70, placement over 100 miles from any of the eight counties, and continual runaway status for 45 days after the youth’s 17th birthday. Caseworkers provided informed consent for those who met the criteria for participation in the study. Four-hundred and fifty youths were eligible for the study at interview 1, and 90% (407) of those eligible were enrolled in the study. Most of the nonenrolled youths had declined to enroll; however, in the case of a few of the youths, caseworkers did not return phone calls from the research team. Interviews 1 and 9 were conducted in person. Interviews 2 through 8 were conducted via phone when possible. All procedures were approved in advance by our university’s Committee for the Protection of Human Subjects.
The sample included 226 female youths (55.94%) and 226 (55.94%) youths of color, almost all of whom were African American or African American with mixed race. There was almost no variation in age at first interview, as youths were interviewed as near as possible to their 17th birthday. At the age-19 interview (ninth data point), 325 participants were interviewed. 80% of those who were interviewed at age 17. Most participants not retained were lost because we were unable to locate them (62 participants, 15%). One participant died, and one became ineligible due to a disability. Seven youths (2%) chose to leave the study. Seven (2%) were incarcerated, and we were unable to gather required protections or permissions to conduct interviews with them. Two were not interviewed due to overseas military service. Two youths became ineligible for the study as the research team later found out that their IQs were lower than 70. Multivariate logistic regression analyses to predict retention revealed that the following characteristics were associated with decreased odds of being retained in the study: being male (odds ratio [OR] = 0.34, p < .001), having past-year posttraumatic stress disorder at initial interview (OR = 0.36, p = .025), having a history of juvenile detention by first interview (OR = 0.26, p = .016), and being released from the state’s custody prior to age 19 (OR = 0.26, p < .0001). In the present study, we used multiple imputation in SAS 9.1 (five data sets) to compute the best estimates of data for those with missing data at age 19 (see details of the procedures in the Data Analysis section), with the exception of the two youths who should have been excluded initially due to low IQ and the one participant who died. This brought the sample for the current study to 404 youths. Of particular interest for this study of depressive trajectories, previous studies of this sample revealed that at age 17, 27% met criteria for lifetime history of major depression (McMillen et al., 2005).
Measurement
Depression Measures
Depressive symptoms were assessed at each of the nine interviews with the 11-item Depression—Arkansas Scale (D-ARK) from the Depression Outcomes Module (Smith, Burman, Burns, Cleary, & Rost, 1994). The measure was developed specifically to assess the presence of DSM—IV (American Psychiatric Association, 1994) major depressive disorder (Walter, Meresman, Kramer, & Evans, 2003). Participants rated symptom frequency in the past four weeks using a response range varying from not at all = 1 to nearly every day for at least 2 weeks = 4. Although the D-ARK is less well known than other depression symptom measures, we chose it because of its unique combination of brevity (11 items), excellent psychometrics, and ease of interpretability (scoring algorithm transposes scores to a 100-point scale, with higher scores representing greater depressive symptomatology). The D-ARK has been tested in culturally diverse populations and has evidenced good convergent validity, with depression severity on the D-ARK being correlated with scores on the longer Hamilton-D, symptoms on the Structured Clinical Interview for DSM (SCID) (Smith et al., 2002), number of depressive symptoms on the Diagnostic Interview Schedule (DIS) (Smith, Ross, & Rost, 1996), and most recently with the Beck Depression Inventory (Walter et al., 2003). A validity study examining the D-ARK scale and the SCID reported that those who were clinically depressed on the basis of the SCID scored 30 to 79 on the D-ARK scale, and those who were not depressed on the basis of the SCID scored in the range of 0 to 33 (Smith et al., 2002). In the present study, internal consistency coefficients ranged from .73 to .80 across the nine waves. Computed depression trajectories, using the nine data points of depression symptoms, served as the main dependent variable for most analyses. The DIS for DSM—IV (Robins, Cottier, Bucholz, & Compton, 1995) was used to assess whether youths met past-year criteria for a major depressive episode at the age-17 and age-19 interviews.
Measures Included in Modeling Trajectory Classes
Gender was coded as observed by interviewers. Race was recoded into a dichotomous variable called “youths of color” because the sample included small numbers of Asian, American Indian, and Latino youths. Physical abuse and physical neglect histories were assessed with the Childhood Trauma Questionnaire (Bernstein & Fink, 1998). For clarity of results, Bernstein and Fink’s cutoff score of 10 or above was used to identify cases of moderate or severe abuse and neglect. Youths were considered sexually victimized if they reported molestation or vaginal, oral, or anal intercourse against their wishes. History of juvenile detention at age 17 was assessed with a single item. Living situation at time 1 was categorized into living with family, in nonkin foster care, in congregate care (for example, residential facilities, shelters, inpatient hospitals), or more independently. Time out of care was collapsed into six-month intervals, with some youths leaving care at 17 and some youths remaining in care throughout the study. Family history of mental health was assessed with two single items asking youths whether their parents have a history of using psychiatric treatment for an emotional problem such as anxiety or depression and whether there is a history of suicidal behavior (attempt or completion) in the family. Also, being drunk in the past six months and past-month marijuana use at 17 were used in model building. One time-varying measure was included in the model building, namely past-month mental health service use. Youths were considered to be in receipt of mental health services if they were using any of the following services: outpatient therapy, psychotropic medication prescribed by a physician, or residential treatment services.
Age-19 Outcomes
Current employment status, being in school (currently attending high school, college, vocational training, or GED classes), being a parent, and having been charged with a crime in the past 12 months were assessed by self-report. Youths were considered “productive” if they were working or in school. Substance use was measured with three dichotomous items, past-month marijuana use, use of other drugs, and being drunk in the past six months. Transience was measured by the number of places that a youths lived from age 17 to age 19.
Data Analysis
Data were imputed using IVEware (Raghunathan, Solenberger, & Van Hoewyk, 2002), a general purpose multivariate imputation method that can handle-complex data structures where full information models cannot be easily formulated. The imputed values for each individual are fully conditional on all the values observed for that individual, with imputation conducted on a variable-by-variable basis using a sequence of regression models, varying the types of regression model by the type of variable being imputed (Raghunathan, Lepkowski, Van Hoewyk, & Solenberger, 2001). This is superior to most full information imputation procedures as it allows for proper subsetting of variables, only imputing values where it is reasonable to do so and within specified ranges. Five implicates of imputed data were generated on the basis of available information.
To assess whether depression symptom scores changed over time, and whether when youths left the foster care system was related to variation in depression symptom scores over time, we used Taylor series linearization with proc surveyreg in SAS 9.1 (Woodruff, 1971). This is a model-agnostic procedure that does not require specification of the error covanance structure and yields the same result as the Huber-White sandwich estimator.
Depression trajectories were categorized using latent growth mixture modeling (LGMM) (B. Muthén, 2004; B. Muthén & Muthén, 2000) with Mplus (version 4.2) software (L. K. Muthén & Muthén, 1998–2006). LGMM is a person-centered method of longitudinal analysis that offers a means of identifying subgroups of research participants following similar trajectories over time. This method is thought to be more appropriate than determining trajectory categories a priori, as it treats the existence of subtypes of participants as an empirical question (Connell & Frye, 2006). It is also thought to be superior to variable-centered methods of longitudinal analyses that address variation in developmental trajectories of a population as a whole (B. Muthén & Muthén, 2000).
In our LGMM models, the intercept parameter (depression scores and variance at time 1) and the slope parameter (mean and variance of the linear rate of change in depression scores) were regressed on a categorical latent trajectory class variable, representing unobserved groupings of youths with optimally similar intercept and slope parameters. Models were built with depression scores, predictor variables from the initial interview, and distal outcome variables included as determinants of trajectory class. All variables were allowed to covary, and all growth parameter intercepts and residual variances were allowed to vary across classes, as were the covariance between intercept and slope and the time-specific residual variances of the observed depression scores at each interview. These analyses yield latent classes of participants who are optimally similar with respect to depression trajectories and with respect to the influence of covariates. We used 50 random starts and the five best results from these starts.
We used the four general criteria suggested by B. Muthén and Muthén (2000) for selecting the optimal number of latent trajectory classes: (1) indices of relative model fit, especially the Bayesian information criterion, for which a lower number indicates better fit; (2) the Lo-Mendell-Rubin likelihood test, which provides a comparison of fit of a given model with a model with one fewer classes, for which a low p value indicates a better fit; (3) the quality of classification across groups, represented by entropy, a summary measure of the probability of membership in the most likely class for each individual, for which a number closer to one indicates better fit; and (4) the usefulness and interpretability of the latent trajectory classes. Model fit results were examined in all five implicates (see Table l). We examined trajectories across all implicates to be assured they were similar (they were) and interpretable. Then we assessed model results to pick the best class solution, using information from all implicates. Given that there are no guidelines for “rolling up” trajectory class results across multiple implicates of imputed data, we chose to present the solution from the implicate with the best log likelihood. We then reran the model including a quadratic slope function to assess whether the model performance improved when allowing for nonlinear trajectories.
Table 1.
Model Statistics for Latent Growth Mixture Models Implicates 1 through 5
| Solution | BIC | Entropy | LMR-LRT |
|---|---|---|---|
| IM 1 – 2-category solution | 41,069 | 0.880 | NS |
| IM 1 – 3-category solution | 41,093 | 0.963 | NS |
| IM 1 – 4-category solution | 41,196 | 0.995 | NS |
| IM 2 – 2-category solution | 40,784 | 0.908 | NS |
| IM 2 – 3-category solution | 40,792 | 0.967 | NS |
| IM 2 – 4-category solution | 40,888 | 0.980 | NS |
| IM 3 – 2-category solution | 40,911 | 0.998 | Sig. |
| IM 3 – 3-category solution | 40,973 | 0.964 | NS |
| IM 3 – 4-category solution | 41,008 | 0.977 | Sig. |
| IM 4 – 2-category solution | 40,955 | 0.950 | NS |
| IM 4 – 3-category solution | 40,987 | 0.966 | NS |
| IM 4 – 4-category solution | 41,060 | 0.982 | NS |
| IM 5 – 2-category solution | 41,052 | 0.931 | NS |
| IM 5 – 3-category solution | 41,020 | 0.935 | NS |
| IM 5 – 4-category solution | 41,153 | 0.968 | NS |
| IM 2 – 3-category solution (quadratic slope function) | 40,818 | 0.945 | NS |
Notes: BIC = Bayesian information criterion; LMR-LRT = Lo-Mendell-Rubin likelihood test; IM = implicate; NS = not significant; Sig. = significant. Boldfaced text represents the implicate and category solution chosen on the basis of the various model fit statistics.
Predictors of depression trajectory class membership and the relationship between class and distal outcomes were assessed in SAS 9.1, using the most likely trajectory class based on posterior probabilities generated from the Mplus output. In several cases, we deemed the logit and standard error estimates describing the relationships between trajectory classes and their correlates from the Mplus results unreliable and inconsistent with the proportions of respondents with certain characteristics in each class. Therefore, we chose to use the SAS results, recognizing that these analyses may overestimate between-class differences as they do not account for the uncertainty of class membership. This concern abates somewhat when using trajectory class solutions with high entropy scores, which we achieved. Only variables that were significant at the bivariate level were included in multivariate models.
We then reran the LGMM analyses in all five implicates, this time including the time-varying mental health service use covariate. We visually assessed the differences in appearance in trajectory class models, with and without mental health service use included. Finally, we examined the percentages of youths receiving mental health services at each time point by trajectory class to unpack how mental health services were affecting the second set of LGMM results.
RESULTS
Rates of Past-year Depression at Ages 17 and 19
At the initial interview at age 17, 17.6% of youths (n = 71) reported symptoms that qualified for a past-year episode of major depression. At 19, using imputed data, 10.6% of youths (n = 43) reported meeting criteria for a past-year major depressive episode. (Using unimputed data, 34 youths of 324, or 10.5%, met these criteria, with one missing value.)
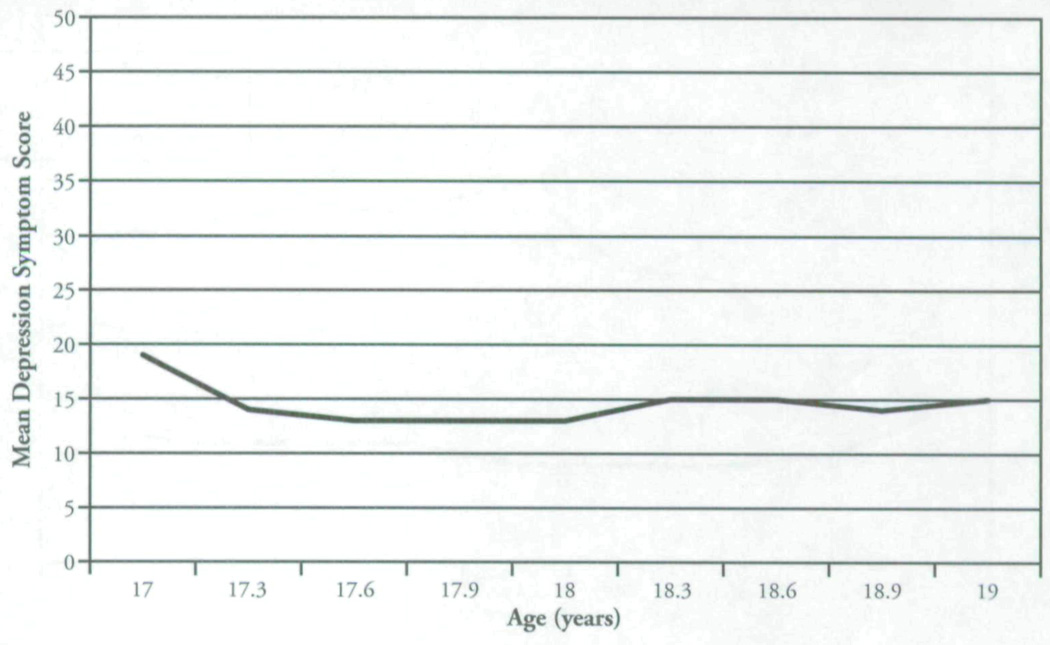
Depression Symptoms across the Two Years
As shown in Figure 1, mean depression estimates from the rolled-up imputed data sets showed a slight dip from the first to second interview and remained somewhat flat from the second through the ninth interview. The curve of this line is different from zero, showing a slight decrease over time (estimate = –1.47, t = –14.49, p < .0001). Estimated standard errors ranged from .77 to .95.
Figure 1.
Mean Depression Symptom Scores of Entire Sample (N = 404)
Do Depression Symptoms Spike after Youths Leave the Foster Care System?
First, we looked at whether depression growth curves were different based on when youths left foster care by examining the time by exit period interaction. It suggests that depression over time differs by when youths left foster care (t = −2.42, p = .02). However, an examination of the growth curves by five categories of when youths left care (not shown for reasons of graphic complexity) did not reveal a spike soon after youths left care. Instead, there was a gradual separation, so that by the age-19 interview, youths who remained in care were less depressed than those who had left custody, irrespective of when those who left custody left care.
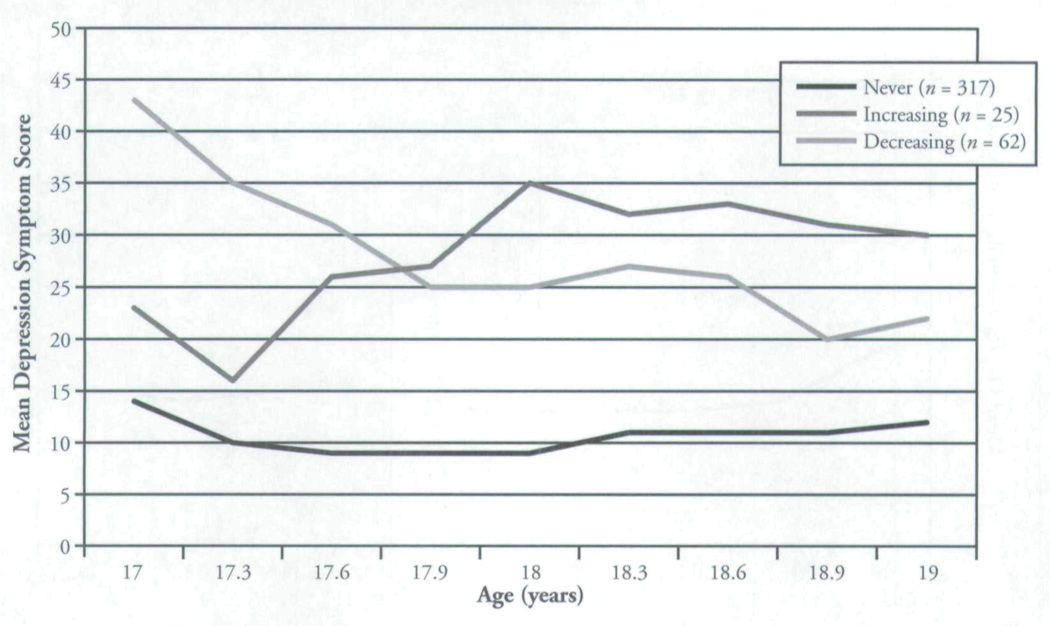
Depression Trajectory Classes
The model statistics for the two-, three-, and four-category LGMM results from each of the five implicates when time-varying mental health service use is not in the model are presented in Table 1. A case could be made for the two- or three-category solution. We chose the three-class solution after examining all the relative fit statistics and the usefulness and interpretability of the classes. Although the BIC is slightly better in the two-class solution for four of the five implicates, the entropy significantly improves from the two- to the three-class solutions in the majority of implicates. In the three-class solution using the implicate with the lowest log likelihood,. 78% (n = 317) of the youths had a trajectory that represented a never-depressed class, with 15% (n = 62) in a trajectory that represented a sharp decrease in depression over time, including a move from clinically significant symptom scores (M = 43.73, SD = 23.90) to scores indicative of not being depressed, and 6% (n = 25) in a class that represented a modest increase in depression symptom scores, moving toward a score that could represent clinical depression (M = 34.63, SD = 18.57) (see Figure 2). The two-class solution classified 79% (n = 318) of the youths in the never depressed group and 21% (n = 85) in the decreasing group. We favored the three-class solution over the two-class solution because it makes sense that participants’ depression could increase or decrease, and the youths whose-scores increased are of clinical interest. Furthermore, we examined the relative fit results for the three-class solution from the best implicate after entering a quadratic slope function in the model statement, and the results suggest that the model did not improve.
Figure 2.
Mean Depression Symptoms Scores Over Time, by Trajectory Class (N = 404)
Factors Associated with Trajectory Classes
As shown in Table 2, a number of variables measured at the first interview were associated bivariately with trajectory class membership. Male youths were more likely to be in the increasing and never depressed groups, with female youths overrepresented in the decreasing depression class. The highest proportions of youths with histories of each type of maltreatment were members of the decreasing class. Youths living in congregate care settings (for example, residential facilities) at 17 were overrepresented in the decreasing class, whereas a higher proportion of youths living more on their own at age 17 were in the increasing class. Substance use at age 17 was related to being in the increasing class. Having a family history of mental health problems was related to being in the classes with greater change in depression symptoms across the two years, particularly the increasing class, of which over 88% had a family history of receiving psychiatric treatment. Those who left care were overrepresented in the increasing class. Youths who had met criteria for a disruptive behavioral disorder (DBD) in their lifetime were overrepresented in the groups with fluctuating symptoms. A juvenile record was related to being in the decreasing class.
Table 2.
Factors Associated with Depression Trajectory Classes (N = 404)
| Predictor | Overall % (n) |
Never Depressed Class n = 317 % (n) |
Decreasing Depression Class n = 62 % (n) |
Increasing Depression Class n = 25 % (n) |
χ2 (df) | P |
|---|---|---|---|---|---|---|
| Male gender | 44.06 (178) | 46.69 (148) | 16.39 (10) | 80.00 (20) | 32.91 (2) | 00*** |
| Person of color | 55.94 (226) | 57.41 (182) | 60.66 (37) | 24.00 (6) | 11.19 (2) | 00** |
| Physically abused | (186) | 42.27 (134) | 67.21 (41) | 40.00 (10) | 13.19 (2) | 00** |
| Sexually abused | 34.74 (140) | 32.18 (102) | 50.82 (31) | 28.00 (7) | 22.09 (2) | 02* |
| Physically neglected | 46.04 (186) | 42.90 (136) | 63.93 (39) | 44.00 (11) | 9.16 (2) | 01* |
| Living situation age 17 | ||||||
| Relative care | 26.73 (108) | 28.08 (89) | 14.75 (9) | 36.00 (9) | ||
| Nonkin foster care | 28.47 (115) | 30.60 (97) | l6.39 (10) | 32.00 (8) | ||
| Congregare care | 41.58 (168) | 39.43 (125) | 63.93 (39) | 16.00 (4) | ||
| More independent | 3.22 (13) | 1.89 (6) | 4.92 (3) | 16.00 (4) | 34.57 (6) | 00*** |
| Got drunk at age 17 | 13.15 (53) | 6.31 (20) | 29.51 (18) | 60.00 (15) | 75.32 (2) | 00*** |
| Marijuana use at 17 | 9.69 (39) | 6.94 (22) | 8.20(5) | 48.00 (12) | 44.87 (2) | 00*** |
| Ever DBD at age 17 | 45.66 (184) | 37.54 (119) | 75.41 (46) | 72.00 (18) | 37.20 (2) | 00*** |
| Family history of MHSU | 44.42 (179) | 40.69 (129) | 45.90 (28) | 88.00 (22) | 21.07(2) | 00*** |
| Family history of suicidal behavior | 29.03 (117) | 23.97 (76) | 47.54 (29) | 48.00 (12) | 18.44 (2) | 00*** |
| Left care | (254) | 59.62 (1 89) | 70.49 (43) | 84.00(21) | 7.72 (2) | 02* |
| Juvenile history at 17 | 37.47 (151) | 34.38 (109) | 52.46 (32) | 40.00 (10) | 7.21 (2) | 03* |
Note: DBD = disruptive behavioral disorder; MHSU = mental health service use.
p < .05.
p< .01.
p < .001.
Multivariate logistic regression analysis suggested that being female (not male) (OR = 0.09, p < .0001), being a youth of color (OR = 1.98, p < .05), having experienced neglect (OR = 2.31, p < .05), using alcohol in excess (OR = 8.65, p < .0001), and having a lifetime history of a DBD (OR = 3.705, p < .001) were positively associated with membership in the decreasing class (see Table 3).
Table 3.
Logistic Regression Modeling Membership in Decreasing Depression Class
| Variable | OR | CI | SE | P |
|---|---|---|---|---|
| Person of color | 1 98 | 0.98, 4.00 | .36 | .05* |
| Male | 0.09 | 0.03, 0.24 | .50 | .00**** |
| Sexually abused | 0.88 | 0.42, 1.83 | .37 | .73 |
| Physically abused | 1.46 | 0.68,3.12 | .39 | .33 |
| Neglected | 2.31 | 1.11, 4.84 | .38 | .02* |
| Time in care | 1.04 | 0.49, 2.19 | .38 | .92 |
| Drunk (past 6 months) | 8.65 | 3.23, 23.13 | .50 | .00*** |
| Marijuana (past month) | 0.53 | 0.15, 1.93 | .66 | .33 |
| luvenile detention | 1.89 | 0.94, 3.79 | .36 | .07 |
| Living at 17 | 1.46 | 0.97, 2.18 | .21 | .07 |
| Disruptive behavioral disorder | 3.70 | 1.79, 7.66 | .37 | .00*** |
| Family history of psychiatric treatment | 0.45 | 0.21, 0.90 | .39 | .04* |
| Family history of suicide | 1.71 | 0.78–3.75 | .40 | .18 |
| Model statist | 100.15**** | C statistic = .86 |
Notes: OR = odds ratio; CI = confidence interval.
p < .05.
p < .001.
p <.0001.
Is Depression Trajectory Class Associated with Early Adult Functional Outcomes?
We examined nine functional outcomes at age 19 (see Table 4). Depression trajectory class was associated with being employed, being in school, substance use, being charged with a crime, and transience at the bivariate level. More specifically, a higher proportion of the youths in the increasing class were employed, using alcohol and other drugs, and committing crimes. Youths in school at age 19 were overrepresented in the never depressed group. In multivariate models, membership in the increasing (OR = 4.54, p < .05) and decreasing (OR = 2.99, p < .05) classes were both associated with a greater likelihood of being charged with a crime when compared with those who were in the never depressed class. In a multivariate model of transience, the decreasing class evidenced more transience than the other groups (b = 2.20, SE = 0.59, p < .001).
Table 4.
Differences in Age-19 Functional Outcomes, by Depression Trajectory Class (N = 404)
| Group | Employed % (n) |
In School % (n) |
Productive (in School or Working) % (n) |
Parent % (n) |
Drunk Past 6 Months % (n) |
Marijuana Use Past Month %(n) |
Other Drug Use Past Month % (n) |
Charged with Crime Past 12 Months % (n) |
Transience (Times Moved over Two Years) M (SD) |
|---|---|---|---|---|---|---|---|---|---|
| Overall | 41.19 (166) | 30.02 (121) | 56.08 (226) | 22.08 (89) | 30.27 (122) | 18.86 (76) | 4.22 (17) | 13.90 (56) | 5 (3.79) |
| Never depressed (n = 317) | 42.90 (136) | 32.81 (104) | 57.41 (182) | 21.14 (67) | 28.08 (89) | 18.93 (60) | 2.84 (9) | 10.73 (34) | 4.42 (3.17) |
| Decreasing depression (n = 62) | 27.87 (17) | 18.03 (11) | 45.90 (28) | 21.31 (13) | 31.15 (19) | 19.67 (12) | 8.20 (5) | 19.67 (12) | 7.72 (5.14) |
| Increasing depression (n = 25) | 52.00 (13) | 24.00 (6) | 64.00 (16) | 36.00 (9) | 56.00 (14) | 16.00 (4) | 12.00 (3) | 40.00 (10) | 5.68 (4.31) |
| .05* | .00*** | .18 | .22 | .00*** | .92 | .00*** | .00*** | .00**** |
p < .05.
p < .001.
p < .0001.
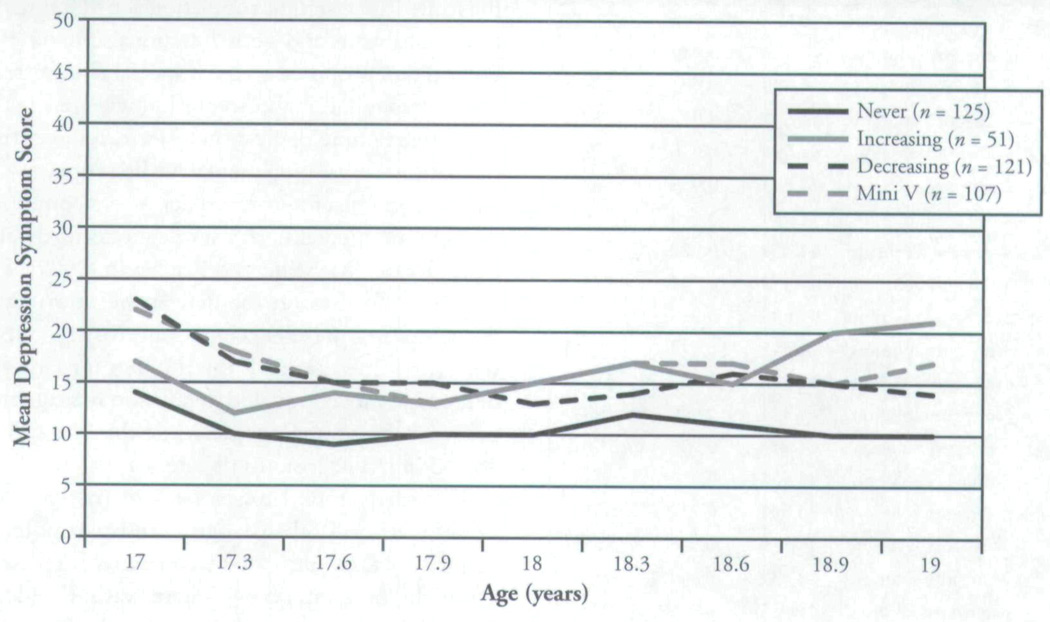
Do Trajectory Classes Look Different When Accounting for Time-varying Mental Health Service Use?
The relative fit indices for LGMM across the five implicates that were generated when the time-varying mental health service use variables were included in the model are presented in Table 5. With these variables included, models with a larger number of classes were needed to describe the data. We chose a four-class solution and present the model from implicate 2, which had the lowest log likelihood. Compared with the LGMM results without including mental health services, trajectories were somewhat compressed (see Figure 3). No trajectory class showed youths with high levels of depression at any point. Although there is a clear never depressed class, other classes display small decreases and increases over time. Investigators examined Figures 2 and 3 to explore interpretations of the differences in depression trajectory classes when mental health service use is added to the model as a time-varying covariate. What appears to differentiate these groups is their receipt of mental health services. Investigators examined the percentages of youths using mental health services by trajectory class. Twenty percent of the youths in the never depressed class were receiving services at age 17, but by 17 years and 9 months of age, nobody in this class was receiving services. The large majority of youths in the class whose depression scores over time are shaped in a miniature V (slightly decreasing then slightly increasing) were in receipt of services across the two years. The group that most resembled a reactive depression group, but with only a modest increase in symptoms, increased service use over time, with up to 70% receiving services by age 19. Finally, one class, which revealed a small decrease in symptoms, also decreased service use over time. The differences among the classes by service use status suggest that service use over time was driving the generation of these trajectory classes when time-varying mental health service use was included in the model.
Table 5.
Model Statistics for Latent Growth Mixture Models Implicates 1 through 5 (with Mental Health Service Use)
| Solution | BIC | Entropy | LMR-LRT |
|---|---|---|---|
| IM 1 – 2-category solution | 44,779 | 0.949 | Sig. |
| IM 1 – 3-category solution | 44.679 | 0.902 | NS |
| IM 1 – 4-category solution | 44,653 | 0.917 | NS |
| IM 1 – 5-category solution | 44,680 | 0.936 | NS |
| IM 2 – 3-category solution | 44,543 | 0.939 | Sig. |
| IM 2 – 3-category solution | 44,454 | 0.900 | NS |
| IM 2 – 4-category solution | 44,432 | 0.922 | NS |
| IM 2 – 5-category solution | 44,459 | 0.934 | NS |
| IM 3 – 2-category solution | 44,633 | 0.949 | Sig. |
| IM 3 – 3-category solution | 44.545 | 0.943 | Sig. |
| IM 3 – 4-category solution | 44,496 | 0.930 | Sig. |
| IM 3 – 5-category solution | 44.534 | 0.940 | NS |
| IM 4 – 2-category solution | 44,643 | 0.953 | Sig. |
| IM 4 – 3-category solution | 44,562 | 0.914 | NS |
| IM 4 – 4-category solution | 44,541 | 0.919 | NS |
| IM 4 – 5-category solution | 44.579 | 0.948 | NS |
| IM 5 – 2-category solution | 44,837 | 0.944 | Sig. |
| IM 5 – 2-category solution | 44,715 | 0.940 | NS |
| IM 5 – 4-category solution | 44,685 | 0.931 | NS |
| IM 5 – 5-category solution | 44,737 | 0.955 | NS |
| IM 2 – 4 - category solution (quadratic slope function) | 44,459 | 0.936 | NS |
Notes; BIC = Bayesian information criterion; LMR-LRT = Lo-Mendell-Rubin likelihood test; IM = implicate, Sig. = significant; NS = not significant. Boldfaced text represents the implicate and category solution chosen on the basis of the various model fit statistics.
Figure 3.
Depression Symptom Scores, by Trajectory Class (with Mental Health Service Use) (N = 404)
DISCUSSION
This is the first study to examine depression symptom trajectories in a sample of older youths from the foster care system, a population at risk for mental health problems and poor functional outcomes in general and proposed to be at special risk for reactive depression. It is also, to our knowledge, the first study to examine depression trajectories over time in relation to changing mental health service use, an issue of particular interest, as older youths commonly discontinue mental health service use shortly after leaving care (McMillen & Raghavan, 2009). This discussion focuses on the descriptive information on depression prevalence and trajectories, coupled with the implications of the findings for targeting depression prevention and depression management programs for young people while they are still involved in public systems of care.
This study found lower rates of past-year depression at age 19 than at age 17. Furthermore, the majority of the youths showed no signs or depression across the nine interviews. There was no evidence of a spike in symptoms as youths left the foster care system, although depression scores were higher at age 19 for those who had left foster cue compared with those who had stayed in care. These results suggest that the published clinical lore that youths regularly experience reactive depression as they leave the foster care system (Anderson & Simonitch, 1981) should not be accepted without caution and deserves further investigation. One possibility is that professionals may have tended to overpathologize this group:We expect depression because we assume that the youths are unprepared and miserable. They may be struggling, but without depression. A second possibility is that we have simply underestimated these young people’s emotional resilience. Young people without the generic predisposition toward depression may be able to experience substantial hardship without the onset of depression. Another possibility is that depression may await some of these young people as they spend more time out of care and fully experience the hardships of living on their own with little preparation. The fact that those who left care had more symptoms than those who stayed in care may suggest incipient depression for those who left care. They may become stressed with the demands of life and experience a slow onset of low-level depression.
This may explain some interesting results in relation to the increasing class. This small group of mostly male youths who reported family histories that included a history of psychiatric treatment had the highest rates of being employed and being productive, yet they also had the highest rates of getting drunk and of being charged with a crime. A large percentage of youths in this group had left care, and 72% of them had a history of a DBD. They may be motivated to function as productive adults in society yet be struggling with the emotional demands of doing so. Reactive depression may occur as a result of struggling to cope with the demands of adulthood, but only for those with a genetic disposition toward depression.
The group of youths in the decreasing class also represent a clinically distinguishable group that moved from clinically significant depression scores at age 17 to the subclinical level at age 19. This group had high transience and had the lowest rates of employment and being in school at age 19. They also tended to be female, be victims of multiple forms of maltreatment, and have histories of DBD, and they were often living in congregate care settings at age 17. For this group, simply leaving a care system they perceive as oppressive may be enough to lift their depression, at least temporarily, even though they are struggling to become productive adults. These youths may be experiencing the elation reaction to leaving care (Anderson & Simonitch, 1981). Their history of behavior problems and lack of involvement in school, however, may put them at risk of later mental health problems.
When mental health service use was entered as a time-varying covariate in prediction of trajectory classes, results looked very different. More classes emerged, but their determination was dominated by the service use variables. The never depressed group stopped using services quickly. A group with slightly increasing depression scores gained in service use over time. A group with slightly decreasing scores stopped using services. The fact that some young people stop mental health services with little to no change in depression may suggest that they were not well served by these interventions or that these interventions had other therapeutic targets. We should note that although mental health services and depression both varied over time, the results are not causal. We cannot infer that services changed depression scores over time.
In sum, our most maltreated youths were in the decreasing class, and those with the highest rates of family history of mental health problems were in the increasing class. This study adds support to the notion that depression trajectories differ by gender, although results were not completely anticipated, with male youths more likely to be in the increasing class and female youths more likely to be in the decreasing class. Our data also suggest that, conceptually, additional predictors should be Considered when modeling depression among high-risk youths involved with public care systems, such as where youths are living and whether they remain in custody of the state.
The low rates of depression suggest that it may not be efficient to universally deliver depression prevention and management programs to youths leaving public care. Results suggest that in addition to focusing efforts on developing depression programs for youths with histories of major depression, it may also be prudent to target youths with family histories of mental health problems, youths with conduct problems, and those who use substances. A curriculum that could be adapted for this group of youths is Illness Management and Recovery (Mueser et al., 2006), which attempts to build hope for the future, build coping skills, increase understanding of depression, and build awareness of help-seeking when it is needed. Clinicians working individually with older youths from the foster care system can emphasize these themes.
It may also make sense to develop support programs for female youths of color who have experienced depression in the past, along with multiple forms of maltreatment, to prevent a recurrence of clinical depression during the transition to adulthood. Support groups cofacilitated by mental health providers and trusted community members may help engage women to come and talk about their life transitions while they are receiving support and education geared toward keeping them aware of the possibility of recurring depression.
Study Limitations
Results of this study are not generalizable to all older youths exiting the foster care system. The sample included youths from one midwestern state; however, a strength of these data are that they represent urban, suburban, and rural participants, which may make them more closely resemble other states’ foster cue youths. Also, the present findings are based on self-report data, which can lead to problems of recall and social desirability. Also, the fact that we used methods to assess the relationships between trajectory class and other variables that did not account for the uncertainty in depression class may have increased the chance of a type I error in these analyses. These results should be interpreted with caution and need replication. It is also important to keep in mind the relatively small number of youths in the increasing depression group (n = 25) when interpreting the results of the study. Finally, a large number of covariates were examined in relation to depression trajectories without regard to the increased risk of type I errors.
CONCLUSION
The results of this longitudinal study of depression symptoms among older youths transitioning out of the foster care system suggest that this transition is not typically accompanied by a spike in depression symptoms, as has been suggested. In fact, the majority of youths in this study were in a class that did not evidence high depression symptoms at any point from age 17 to age 19. Results suggest that interesting subgroups of youths with increasing and decreasing depression may exist and that these groupings may be somewhat counterintuitive. Some youths may have their depression lifted by virtue of leaving congregate care settings, even it they are struggling to be productive young adults; others who are working or in school may be prone to increasing depression. These data provide some initial insights about how to begin targeting prevention and depression management strategies in social work practice settings among specific subgroups of older youths in foster care.
Acknowledgments
This study was funded by a grant from the NIMH (R01 MH 61404).
Contributor Information
Michelle R. Munson, Silver School of Social Work, New York University, 1 Washington Square North, New York, NY 10003; michelle.munson@nyu.edu.
Curtis McMillen, George Warren Brown School of Social work. Washington University in St. Louis.
REFERENCES
- Abramson LY, Metalsky GI, Alley LB. Hopelessness depression: A theory-based sub-type of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- Anderson JL, Simonitch B. Reactive depression in youths experiencing emancipation. Child Welfare. 1981;40:383–390. [PubMed] [Google Scholar]
- Barth RP. On their own:The experiences of youth after foster care. Child and Adolescent Social Work Journal. 1990;7:419–440. [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. New York: International Universities Press; 1976. [Google Scholar]
- Bernstein DP, Fink L. The Childhood Trauma Questionnaire manual. San Antonio, TX: Psychological Corporation; 1998. [Google Scholar]
- Birmaher B, Ryan ND, Williamson DE, Brent D, Kaufman J, Dahl RE, et al. Childhood and adolescent depression: A review of the past 10 years, Part I. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:1427–1439. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- Burke KC, Burke JD, Regier DA, Rae DS. Age at onset of selected mental disorders in five community populations. Archives of General Psychiatry. 1990;47:511–518. doi: 10.1001/archpsyc.1990.01810180011002. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Connell AM, Frye AA. Growth mixture modeling in developmental psychology: Overview and demonstration of heterogeneity in developmental trajectories of adolescent antisocial behaviour. Infant and Child Development. 2006;15:609–621. [Google Scholar]
- Costello EJ, Pine DS, Hammen C, March JS, Plotsky PM, Weissman MM, et al. Development and natural history of mood disorders. Biological Psychiatry. 2002;52:529–542. doi: 10.1016/s0006-3223(02)01372-0. [DOI] [PubMed] [Google Scholar]
- Dekker MC, Ferdinand RF, van Lang NDJ, Bongers IL, vander Ende J, Verhulst FC. Developmental trajectories of depressive symptoms from early childhood to late adolescence: Gender differences and adult outcome. Journal of Child Psychology and Psychiatry. 2007;48:657–666. doi: 10.1111/j.1469-7610.2007.01742.x. [DOI] [PubMed] [Google Scholar]
- Diego M, Field T, Sanders C. Academic performance, popularity, and depression predict adolescent substance use. Adolescence. 2003;38(149):35–42. [PubMed] [Google Scholar]
- DuBois DL, Felner RD, Barrels CL, Silverman MM. Stability of self-reported depressive symptoms in a community sample of children and adolescents. Journal of Clinical Child Psychology. 1995;24:286–396. [Google Scholar]
- Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Archives of General Psychiatry. 2002;59:225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- Garber J, Keiley M, Martin NC. Developmental trajectories of adolescents’ depressive symptoms: Predictors of change. journal of Consulting and Clinical Psychology. 2002;10:79–95. doi: 10.1037//0022-006x.70.1.79. [DOI] [PubMed] [Google Scholar]
- Ge X, Conger RD, Elder GH., Jr Pubertal transition, stressful life events, and the emergence of gender differences in adolescent depressive symptoms. Developmental Psychology. 2001;37:404–417. doi: 10.1037//0012-1649.37.3.404. [DOI] [PubMed] [Google Scholar]
- Giaconia RM, Reinherz HZ, Silverman AB, Pakiz B, Frost AK, Cohen E. Ages of onset of psychiatric disorders in a community population of older adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:706–717. doi: 10.1097/00004583-199406000-00012. [DOI] [PubMed] [Google Scholar]
- Kaufman J. Depressive disorders in maltreated children. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;50:257–265. doi: 10.1097/00004583-199103000-00014. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Dropping out of child psychotherapy: Issues for research and implications for practice. Clinical Child Psychology and Psychiatry. 1996;1(1):133–156. [Google Scholar]
- Keller MB, Lavori PW, Beardslee WR, Wunder J, Ryan N. Depression in children and adolescents: New data on “undertreatment” and a literature review on the efficiency of available treatments. Journal of Affective Disorders. 1991;21:163–171. doi: 10.1016/0165-0327(91)90037-s. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. Journal of Abnormal Psychology. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Psychosocial functioning of young adults who have experienced and recovered from major depressive disorder during adolescence. Journal of Abnormal Psychology. 2003;112:353–363. doi: 10.1037/0021-843x.112.3.353. [DOI] [PubMed] [Google Scholar]
- McMillen JC, Raghavan R. Pediatric to adult mental health service use of young people leaving the foster care system. Journal of Adolescent Health. 2009;44:7–13. doi: 10.1016/j.jadohealth.2008.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillen JC, Zima BT, Scott LD, Auslander WP, Munson MR, Ollie EL, Spitznagel E. Prevalence of psychiatric disorders among older youths in the foster care system. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:88–95. doi: 10.1097/01.chi.0000145806.24274.d2. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Mever PS, Perm DL, Clancy R, Clancy DM, Saylers MP. The illness management and recovery program: Rationale, development, and preliminary findings. Schizophrenia Bulletin. 2006;32(1):32–43. doi: 10.1093/schbul/sbl022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B. Latent variable analysis: Growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of quantitative methodology for the social sciences. Newbury Park, CA: Sage Publications; 2004. pp. 345–368. [Google Scholar]
- Muthén B, Muthén L. Integrating person-centered and variable-centered analysis: Growth mixture modeling with latent trajectory classes. Alcohol: Clinical and Experimental Research. 2000;6:882–891. [PubMed] [Google Scholar]
- Muthén LK, Muthen BO. Mplus user’s guide. 4th ed. Los Angeles: Author; 1998–2006. [Google Scholar]
- Newman DL, Moffitt TE, Caspi A, Magdon L, Silva PA, Stanton WR. Psychiatric disorder in a birth cohort of young adults: Prevalence, comorbidity, clinical significance, and new case incidence from 11-21. Journal of Consulting and Clinical Psychology. 1996;64:352–362. [PubMed] [Google Scholar]
- Osgood DW, Foster EM, Flanagan C, Ruth GR. On your own without a net: The transition to adulthood for vulnerable populations. Chicago: University of Chicago Press; 2005. [Google Scholar]
- Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001;21:85–95. [Google Scholar]
- Raghunathan TE, Solenberger PW, Van Hoewyk J. IVEware: Imputation and variance estimation software user guide. Ann Arbor, MI: Survey Research Center, Institute for Social Research; 2002. [Google Scholar]
- Rindfuss RR. The young adult years: Diversity, structural change and fertility. Demography. 1991;28:493–512. [PubMed] [Google Scholar]
- Robins L, Cottier L, Bucholz K, Compton W. Diagnostic interview schedule for DSM–IV. St. Louis: Washington University in St. Louis; 1995. [Google Scholar]
- Rushton JL, Forcier M, Schectman RM. Epidemiology of depressive symptoms in the national longitudinal study of adolescent health. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;41:199–205. doi: 10.1097/00004583-200202000-00014. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Tipp JE, Bergman M, Reich W, Hesselbrock VM, Smith TL. Comparison of induced and independent major depressive disorders in 2945 alcoholics. American Journal of Psychiatry. 1997;154:948–957. doi: 10.1176/ajp.154.7.948. [DOI] [PubMed] [Google Scholar]
- Smith GR, Kramer TL, Hollenberg JA, Mosely CL, Ross RL, Burman A. Validity of the Depression–Arkansas (D–ARK) Scale: A tool for measuring major depressive disorder. Mental Health Services Research. 2002;4(3):167–173. doi: 10.1023/a:1019763130150. [DOI] [PubMed] [Google Scholar]
- Smith GR, Ross RL, Rost KM. Psychiatric outcomes module: Depression (DOM) In: Sederer LI, Dickey B, editors. Outcomes assessment in clinical practice. Baltimore: Williams & Wilkins; 1996. pp. 88–84. [Google Scholar]
- Stark KD, Laurent J, Livingston R, Boswell J, Sweater S. Implications of research for the treatment of depressive disorders during childhood. Applied and Preventive Psychology. 1999;8:79–102. [Google Scholar]
- Stark KD, Sander J, Hauser M, Simpson J, Sclmoebelen S, Glenn R, et al. In: Depressive disorders during childhood and adolescence. Mash EJ, Barkley RA, editors. New York: Guilford Press; 2006. pp. 336–407. Treatment of childhood disorders. [Google Scholar]
- Stoolmiller M, Kim HK, Capaldi DM. The course of depressive symptoms in men from early adolescence to young adulthood: Identifying latent. trajectories and early predictors. Journal of Abnormal Psychology. 2005;114:331–345. doi: 10.1037/0021-843X.114.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner HA, Finkehor D, Ormrod R. The effect of lifetime victimization on the mental health of children and adolescents. Social Science and Medicine. 2006;62:13–27. doi: 10.1016/j.socscimed.2005.05.030. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Adoption and fostet care analysis and reporting system (AFCARS) report: Preliminary FY 2006 estimates as of January 2008 (14) Washington: DO Administration for Children and Families, Children’s Bureau; 2008. [Google Scholar]
- Walter LJ, Meresman JF, Kramer TL, Evans RB. The Depression—Arkansas Scale: A validation study of a nevi brief depression scale in an HMO. Journal of Clinical Psychology. 2003;59:465–481. doi: 10.1002/jclp.10137. [DOI] [PubMed] [Google Scholar]
- Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Archives of General Psychiatry. 2007;64:49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]
- Wise LA, Zierler S, Krieger N, Harlow B. Adult onset of major depressive disorder in relation to early life violent victimization: A case control study. Lancet. 2001;358:KX1–KX887. doi: 10.1016/S0140-6736(01)06072-X. [DOI] [PubMed] [Google Scholar]
- Woodruff RS. A simple method for approximating the variance of a complicated estimate. Journal of the American Statistical Association. 1971;66:411–414. [Google Scholar]