Abstract
Intravital 2-photon microscopy, along with the development of fluorescent probes and innovative software, has rapidly advanced the study of intracellular and intercellular processes at the organ level. Researchers can quantify the distribution, behavior, and dynamic interactions of up to four labeled chemical probes and proteins simultaneously and repeatedly in four dimensions (3D + time) with subcellular resolution in real time. Transgenic fluorescently labeled proteins, delivery of plasmids, and photo-activatable probes enhance these possibilities. Thus, multi-photon microscopy has greatly extended our ability to understand cell biology intra-vitally at cellular and subcellular levels. For example, evaluation of rat surface glomeruli and accompanying proximal tubules has shown the long held paradigm regarding limited albumin filtration under physiologic conditions is to be questioned. Furthermore, the role of proximal tubules in determining albuminuria under physiologic and disease conditions was supported by direct visualization and quantitative analysis.
INTRODUCTION
Multiphoton microscopy (MPM) has equipped investigators with novel techniques to uniquely address biologically important questions that can only be accomplished at the organ level (1–6). In parallel, advances in fluorophores with increased quantum yields and ease of labeling (7–9), molecular and transgenic approaches, and new delivery techniques have allowed for the development of intravital studies with remarkable spatial and temporal resolution and sensitivity at subcelluar levels (5, 10, 11). MPM is uniquely positioned to complement other in vivo biochemical and molecular techniques. However, MPM lacks deep tissue penetration, limiting its use in clinical situations. Exponential developments in computer software and hardware have removed many obstacles previously limiting the use of MPM to observe and quantify dynamic cellular and subcellular processes (12, 13). In particular, developments in hardware, software, bandwidth, and data storage now provide systems that possess the necessary speed to effectively and efficiently approach data intensive processes using digital imaging analysis. These imaging technologies enable the dynamic measurement of four-dimensional (3-D plus time) using fluorescently labeled molecular agents including drugs and proteins. Of paramount importance, it allows for simultaneous quantification of the rates of multiple physiological processes and correlation with structural events. This disruptive technology has already brought into question many previously held paradigms and many more will follow.
THE GLOMERULAR-TUBULAR UNIT
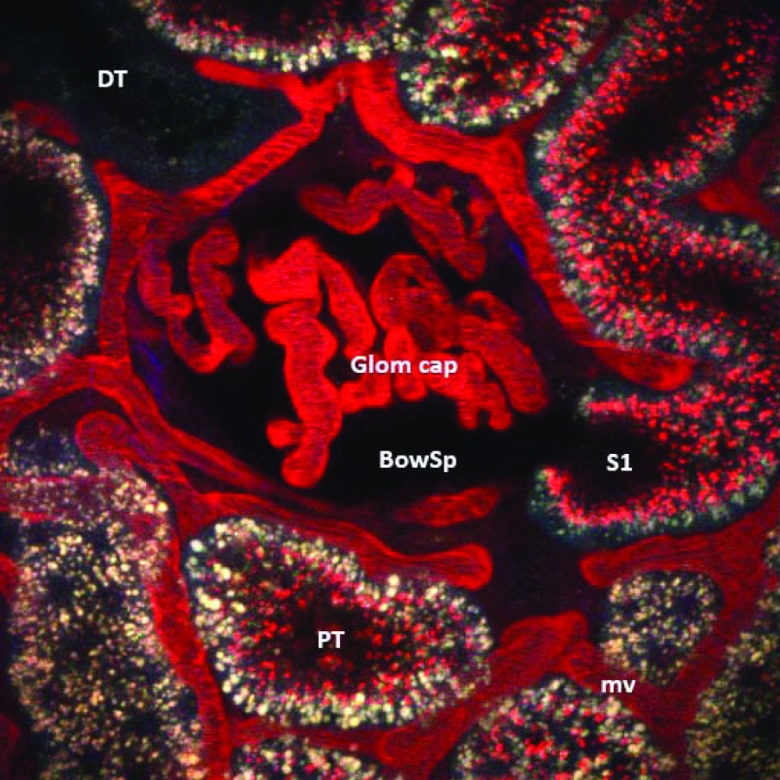
Figure 1 shows the glomerulus and proximal tubule (PT) portion of the nephron. Although universally considered two distinct functional units, the function of each component is dependent on the other. For instance, blood flow to peritubular capillaries must first go through the glomerulus. Furthermore, interruption of function of either component results in paralysis of the other, and fine tuning of each component's function is determined by the other. Renal physiologists have prided themselves in understanding these interactions and dependencies, and yet the assignment of pathologic processes to one or the other component has been the dogma.
Fig. 1.
Texas Red Rat Serum Albumin uptake by proximal tubule cells. A 12-micron volume of a superficial glomerulus given a single bolus of labeled albumin (red) ∼20 minutes post-infusion shows avid uptake in the early S1 segment and other proximal tubules (PT). Note the absence of labeled albumin in distal tubules (DT), corroborating the high capacity of PTs to internalize and transcytose filtered albumin. (Abbreviations: mv, microvasculature; Glom cap, glomerular capillary loops; BowSp, Bowman's space; Bar = 20 μm.)
Proteinuria is an excellent example of this approach. Proteinuria has been defined as glomerular or tubular depending on the size of the proteins involved. If a protein is greater than say 40 kDa, then by definition it must have leaked through the glomerular filter otherwise known as the glomerular filtration barrier. By definition, only proteins in the 20-kDa range end up in the urine following minimally restricted filtration and subsequent proximal tubule dysfunction and lack of endocytic uptake. The idea that albumin (69 kDa) would end up in the urine due to tubular dysfunction is still considered heresy by many. Yet, isolated proximal tubule studies, dating back to the 1970s, documented proximal tubule uptake and transcytosis of albumin (14). Furthermore, early studies using selective pharmacologic-induced PT injury documented nephrotic range proteinuria (15). Now, in the past year, using molecular approaches to selective injury to the PT, three different investigative groups have shown that selective injury to the PT results in nephrotic range proteinuria that increases as PT cell (PTC) dysfunction occurs and resolves with PT repair (16–18). Finally, recent data using enhanced scanning electron microscopy have shown that podocyte slit diaphragm pore size is much larger than previously thought, and is sufficiently large enough to allow for albumin filtration (19).
ALBUMIN FILTRATION ACROSS THE GLOMERULUS: QUANTITATION
Numerous techniques and experimental approaches have been used to determine the quantitative role of glomerular albumin permeability and PTC reabsorption/catabolism in albuminuria. Values for the glomerular sieving coefficient of albumin have ranged from 0.000077 to 0.07 under various physiologic and pathologic conditions (20). Of particular importance has been the use of Munich-Wistar (MW) rats that have surface glomeruli allowing for direct dynamic visualization, instrumentation, and manipulation. Munich-Wistar Fromter (MWF) rats have a large number of surface glomeruli, have been used in micropuncture studies, and spontaneously develop hypertension and progressive albuminuria beginning by week 8 and increasing to >300 mg/24h urinary albumin excretion by week 32. By week 40, 50% of glomeruli are sclerotic (21–23). Munich-Wistar Simonsen (MWS) rats have fewer surface glomeruli and do not develop spontaneous kidney failure or albuminuria under physiologic conditions. These rat models are useful in helping to identify structural and functional changes in disease states in which excess protein is found in the urine. Mice and other strains of rats unfortunately lack surface glomeruli; therefore, direct visualization methods cannot be utilized, unless pathologic processes, such as ureteral obstruction for several days, are used (24).
Prior micropuncture studies in Sprague-Dawley or MWF rats with surface glomeruli measured low glomerular filtration of albumin in fasting states, with a glomerular sieving coefficient (GSC) of 0.00057–0.00062, consistent with low amounts of measured albumin observed in excreted urine (<30 mg/d) (25–27). This has been attributed to the charge barrier and size selectivity at the glomerular filtration barrier. Previous in vivo rat filtration studies and noninvasive studies by one group using isolated perfused rat kidneys showed a much higher GSC of albumin using [3H]-albumin. By measuring total radioactivity in urine, and by inhibiting protein uptake in the PTC, it was shown that the GSC of albumin may actually be approximately 0.074 — more than 120-fold greater than previously thought (28). High GSCs for albumin were also observed by another group using glomerular volumetric analysis in rat glomeruli (0.02 ± 0.01) (29). This finding was strengthened by other investigators showing that high–molecular weight dextrans, with similar radii and molecular weights as albumin (3.6 nm, 66 kDa) and not reabsorbed through receptor-mediated endocytosis, had comparable high GSCs in normal kidneys: pancreatic isoamylase (3.4 nm, 45 kDa, GSC 0.03) (30); horseradish peroxidase (3.0 nm, 40 kDa, GSC 0.06); Bence-Jones protein (2.8 nm, 44 kDa, GSC 0.09) (31). Furthermore, large single-wall carbon nanotubes, which are 100–500 nm and ∼350–500 kDa in size, were shown to be filtered through the normal glomerulus and remain intact before being taken up partially by PTCs (32).
Intravital 2-photon microscopy allows direct visualization and quantification of GSCs of albumin (GSCA) and proximal tubule endocytosis of the filtered albumin. It has also allowed direct visualization of subcellular trafficking, transcytosis, catabolism, and reclamation of proteins and other molecules from glomerular filtrate by PTCs (3, 33). It provides real-time imaging and is minimally invasive (the kidney is exteriorized yet remains itself completely intact and fully functional), is non-toxic, non-disruptive, and mirrors normal physiology most closely, compared to other techniques. MWS rats, which do not develop spontaneous albuminuria, have a GSCA of 0.034 under physiologic fed states, while simultaneously measuring a GSC of 1.0 for inulin and approximately a 500-fold lower GSC for high–molecular weight dextrans (34, 35). The GSCA for MWS rats in fasting states is considerably lower at 0.016 (36). MWF rats, which develop albuminuria spontaneously with aging, have a lower fed GSCA of 0.010 and also display a GSCA reduction in fasting states to 0.007. These studies indicate that the GSC for albumin is higher than previously thought, that feeding has significant impact on glomerular albumin filtration (36), and albumin filtration differs markedly in two genetically related rat strains.
The MPM data documenting a higher than anticipated GSC for albumin immediately caused great skepticism within the nephrology community (26, 37, 38). Indeed, conflicting MPM data were generated indicating that the GSC for albumin is lower than we have reported (39–41). However, these data were subsequently shown to be inaccurate primarily based on using a background cut-off that removed important fluorescent data, thus reducing sensitivity and resulting in an erroneously low GSC (42). However, the controversy remains and one must proceed with caution.
THE PROXIMAL TUBULE: ALBUMIN REABSORPTION AND TRANSCYTOSIS
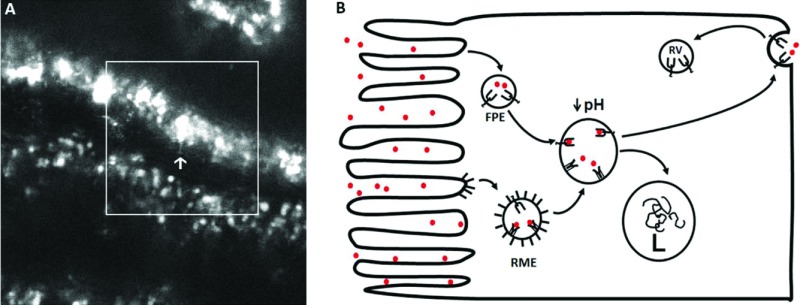
Classically, proximal tubule uptake of proteins and other molecules by endocytic pathways has been attributed to receptor-mediated endocytosis by apical membrane-bound receptors, such as megalin and cubilin clustering into clathrin-coated pits. These pathways have been studied extensively and numerous reviews exist (43, 44). In addition, other mechanisms of protein internalization have also been described, including caveolin-dependent internalization and fluid-phase endocytosis (Figure 2). Molecules endocytosed in this manner are similarly routed to the sorting endosomal compartment and are either degraded through lysosomal pathways or undergo transcytosis back into circulation (45). Albumin uptake by nonselective fluid-phase endocytosis is likely a quantitatively important process in PTCs as shown by the rapid cellular uptake of molecules not having receptors on the apical membrane such as neutral fluorescent dextrans — markers of fluid-phase endocytosis (46, 47).
Fig. 2.
Transcytosis of albumin across proximal tubule cells in vivo using 2-photon microscopy. (A) Two-photon intra-vital time image taken in a Simonsen Munich Wistar rat given 2 mg of Alexa 568-RSA intravenously 24 hours before imaging shows vesicular and tubular structures containing albumin. A single frame with a large accumulation of albumin is indicated by the arrow; note the orientation of the apical membrane is opposite the arrow. The formation of a tubular structure extending from an intracellular compartment toward the basal pole of the PTC is shown at the end of the arrow. (B) Schematic of albumin entering into a PTC either via unbound in a fluid phase vesicle/endosome (FPE) or bound to megalin-cubulin as a receptor mediated endosome (RME) at the apical surface via a clatherin coated pit. With acidification to a pH of less than or equal to 6, the megalin-cubulin binding of albumin diminishes while that of FcRn increases dramatically. As such, there is an exchange of albumin from megalin-cubulin to binding to FcRn and this carrier then mediates transcytosis. When the transcytotic vesicle unites with the basolateral membrane, the increase in pH of the interstitial compartment releases albumin to diffuse into the interstitium and be transcytosed across endothelial cells again using FcRn as the carrier. FcRn then recycles to the apical membrane area via the recycling vesicle (RV). L stands for lysosome.
The endocytic apparatus is found throughout the proximal tubule, although clathrin-coated pits and vesicles are notably less in the S3 segment (48). Protein reabsorption and degradation are greatest in the S1 segment of the PTC and least in the S3 segment (49). Kinetic studies of the rat PT have shown that internalization of cargo at the brush border is highly active. The amount of membrane contained in the apical membrane invaginations is internalized within 78 seconds (50). This rapid rate of turnover means that a great deal of luminal fluid is internalized via endocytic vesicles and likely indicates an important role for fluid phase endocytosis. However, there has been great difficulty in quantifying the overall importance of fluid phase endocytosis as all endocytic vesicles contain fluid and thus luminal contents.
The megalin-cubilin receptor complex is well studied and recent reviews to describe its function and role in protein absorption and metabolism (43, 51). The dissociation coefficient (Kd) of albumin to cubilin is very low and is estimated at 0.63 μM at pH 7.0 (52), resulting in a high-affinity, low-capacity pathway of endocytosis that primarily targets proteins to the lysosome for degradation. Megalin and cubilin work in concert to reabsorb more than 40 filtered molecules (51). In megalin knockout models, the internalization of endogenous ligands bound to apical cubilin, especially cubilin-albumin complexes, is markedly reduced. Urinary albumin excretion is increased 6-fold in cubilin knockout mouse models (53) and in humans (54), although neither reaches nephrotic range; this suggests that an additional mechanism(s) for albumin reabsorption exists. In Dab2 knockout mice — a protein involved in coated pit formation — mild proteinuria was found (55). Type I diabetic patients with albuminuria were found to have significantly elevated urinary levels of megalin and cubilin, suggesting possible proximal tubule shedding of these proteins as a contributing factor to albuminuria (56). Also, in early streptozoticin-induced diabetes in rats, the GSCA was unchanged but PTC uptake of albumin was markedly reduced (34).
The Neonatal Fc Receptor and Its Role in Albumin Transcytosis
The neonatal Fc receptor (FcRn) is a heterodimer with class I major histocompatibility (MHC)–like properties, containing a membrane-bound heavy chain and a β2-microglobulin light chain. Wild-type FcRn has two separate and distinct binding sites for albumin and immunoglobulin G (IgG) (57), with binding being low-affinity and high-capacity at physiologic pH with increasing affinity occurring dramatically at lower pH. It is known to be resident on vascular endothelium; epithelial cells of the proximal small intestine, liver, spleen, and lung; placental syncytiotrophoblasts; polymorphonuclear neutrophils, monocytes, and phagocytes; dendritic cells; and in the kidney (58, 59). Within the kidney, FcRn is found in the vascular endothelia, podocytes, cortical collecting duct, and PT epithelial cells (60). In human kidney sections, it is found at the brush border of PTCs and in endosomes (60).
FcRn is known to transport albumin across membranes, preserving albumin's function and life span as a carrier protein, colloid, buffer, and one that maintains oncotic hemostasis. Overexpression of FcRn in transgenic mice and rabbits increases serum albumin concentrations and generates a 3- to 10-fold increase in IgM and IgG concentrations in serum (61). FcRn is believed to mediate transcytosis and recycling of IgG by PTCs back into circulation (62). The mechanism of FcRn-mediated transcytosis has been well studied in the small intestine and its role in IgG endocytosis via clathrin-coated pits at low luminal pH is known (63, 64).
The FcRn receptor mediates intracellular selection, sorting, and preservation of reabsorbed albumin and IgG. FcRn is concentrated into the apical area in the PT. Whether it participates in luminal albumin binding is not known, but this would not be favored by luminal pH. However, at the low pH found in endosomes, albumin dissociates from megalin-cubilin, whereas FcRn's albumin-binding affinity increases from 34–408 μM at pH 7 to 0.2–0.7 μM at pH 5 (65). Thus, albumin is likely capable of moving from a low-capacity lysosomal degradation pathway (66) to enter a high-capacity pathway of transcytosis and recycling mediated by FcRn based on inherent binding properties of the receptors (67, 68). When the trancytotic vesicle fuses with the plasma membrane and encounters neutral physiological pH, a rapid dissociation of albumin from FcRn would occur releasing it to the interstitium.
The first direct evidence for transcytosis of albumin came from PT microperfusion studies (14). Subsequent studies using transmission electronic microscopy immunogold studies revealed albumin uptake across the apical membrane and release across the basolateral membrane of PTC (35). Multiphoton studies showed actual intracellular vesicles and tubules uniting with the basolateral membrane and releasing fluorescently labeled albumin into the interstitium (36). Finally, Tenten (69) showed a definitive role for FcRn mediating albumin transcytosis in PTC (Figure 2). However, the magnitude of this process remains to be determined. Finally, additional information highlighting the role of FcRn in albumin reabsorption by PTC comes from FcRn knockout mice lacking the neonatal Fc receptor. In these mice, the plasma albumin half-lives were reduced to 75% of wild-type and plasma concentrations were reduced by ∼50% (70–72). This new equilibrium state probably results from the lack of transcytosis by PTC after filtration and a new set point for serum albumin concentration and glomerular filtration is achieved.
CLINICAL SIGNIFICANCE
These data imply that both glomerular permeability and PT reabsorption and transcytosis play significant and likely interactive roles in determining albuminuria. Under physiologic states, the amount of albumin filtered by the glomerulus can be effectively and efficiently reabsorbed by the PTC. Whether the PTC process is saturated or inducible remains to be determined. We have shown that an increase in albumin filtration mediated by endothelin infusion can be compensated for by increased PTC endocytosis (73). Also, data indicate that feeding and genetics influence the GSCA (36). This could be playing a role in diabetic kidney disease and variability in GSCA could influence progression in chronic kidney disease. Finally, that selective injury to PTCs has been shown by three investigative teams to lead to massive proteinuria and albuminuria in a time course consistent with PTC dysfunction highlights the potential importance of the PTC in albumin homeostasis (16, 17).
ACKNOWLEDGMENTS
The authors acknowledge grant support to BAM from the National Institutes of Health, DK 091623, 088934, and 079312, and support from the Veterans Administration through a Merit Review award.
Footnotes
Potential Conflicts of Interest: None disclosed
DISCUSSION
Zeidel, Boston: Bruce, absolutely wonderful work. I know how long it took to get the technical aspects of this to work. When you can make new measurements and look at things in new ways, you come up with new information, which is what's really terrific. So, there are a lot of models of kidney injury that have been studied over the years — including things like crush injury with injection of glycerol into the muscle and puromycin and other things — which have been touted as glomerular injuries but, in fact, probably aren't. So, if you take your work and what Joe was showing us, it's sounding more and more like often the first injury we are talking about is something in the tubule, which then results in glomerular damage. Are you beginning to use this to look at specific injury models? That's the first question; and the second question: is there any way that you can get a mouse into your machine and watch this going on in mice, because obviously the ability to do mutagenesis and other studies would be really powerful?
Molitoris, Indianapolis: So first question — and thank you, Mark, for those questions — is are we looking at other models. Two of the models we've studied pretty extensively include the albumin overload, that may reduce neonatal Fc receptor (FcRn), and in CKD we find both an increased glomerular sieving coefficient and reduced proximal tubule uptake. We also have Roger Wiggin's rats where he has put diphtheria toxin into the podocytes and we can give small, medium, and large doses, and we can regulate the sieving coefficient across the glomerulus and then look at the proximal tubular cell response. So, yes, we are trying to rip this apart. Also, mice can be studied.
DuBose, Winston Salem: Thank you very much, Bruce, for a spectacular presentation. Something of a modification of Mark's question, but in the initial uptake step at the apical membrane endocytosis, the H+ ATPase is playing a major role in regulating that pH that is so critical to the transcytosis of albumin. I wonder if you have considered examining some of the models of knockouts of various subunits of the H+ ATPase to see if it modifies or impedes transcytosis.
Molitoris, Indianapolis: You could evaluate those animals. We're still trying to determine the disease-specific aspects of this before we dive off into the molecular mechanisms.
REFERENCES
- 1.Dunn KW, Sandoval RM, Kelly KJ, et al. Functional studies of the kidney of living animals using multicolor two-photon microscopy. Am J Physiol Cell Physiol. 2002;283(3):C905–16. doi: 10.1152/ajpcell.00159.2002. Epub 2002/08/15. doi: 10.1152/ajpcell.00159.2002. PubMed PMID: 12176747. [DOI] [PubMed] [Google Scholar]
- 2.Hall AM, Rhodes GJ, Sandoval RM, Corridon PR, Molitoris BA. In vivo multiphoton imaging of mitochondrial structure and function during acute kidney injury. Kidney Int. 2013;83(1):72–83. doi: 10.1038/ki.2012.328. doi: 10.1038/ki.2012.328. PubMed PMID: 22992467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Molitoris BA, Sandoval RM. Intravital multiphoton microscopy of dynamic renal processes. Am J Physiol Renal Physiol. 2005;288(6):F1084–9. doi: 10.1152/ajprenal.00473.2004. Epub 2005/05/11. doi: 10.1152/ajprenal.00473.2004. PubMed PMID: 15883167. [DOI] [PubMed] [Google Scholar]
- 4.Peti-Peterdi J, Burford JL, Hackl MJ. The first decade of using multiphoton microscopy for high-power kidney imaging. Am J Physiol Renal Physiol. 2012;302(2):F227–33. doi: 10.1152/ajprenal.00561.2011. doi: 10.1152/ajprenal.00561.2011. PubMed PMID: 22031850; PubMed Central PMCID: PMC3340919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanner GA, Sandoval RM, Molitoris BA, Bamburg JR, Ashworth SL. Micropuncture gene delivery and intravital two-photon visualization of protein expression in rat kidney. Am J Physiol Renal Physiol. 2005;289(3):F638–43. doi: 10.1152/ajprenal.00059.2005. doi: 10.1152/ajprenal.00059.2005. PubMed PMID: 15886277. [DOI] [PubMed] [Google Scholar]
- 6.Zipfel WR, Williams RM, Christie R, Nikitin AY, Hyman BT, Webb WW. Live tissue intrinsic emission microscopy using multiphoton-excited native fluorescence and second harmonic generation. Proc Natl Acad Sci U S A. 2003;100(12):7075–80. doi: 10.1073/pnas.0832308100. doi: 10.1073/pnas.0832308100. PubMed PMID: 12756303; PubMed Central PMCID: PMC165832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lidke DS, Arndt-Jovin DJ. Imaging takes a quantum leap. Physiology. 2004;19:322–5. doi: 10.1152/physiol.00030.2004. doi: 10.1152/physiol.00030.2004. PubMed PMID: 15546848. [DOI] [PubMed] [Google Scholar]
- 8.Miyawaki A, Sawano A, Kogure T. Lighting up cells: labelling proteins with fluorophores. Nature Cell Biol. 2003;(suppl):S1–7. PubMed PMID: 14562844. [PubMed] [Google Scholar]
- 9.Zipfel WR, Williams RM, Webb WW. Nonlinear magic: multiphoton microscopy in the biosciences. Nature Biotech. 2003;21(11):1369–77. doi: 10.1038/nbt899. doi: 10.1038/nbt899. PubMed PMID: 14595365. [DOI] [PubMed] [Google Scholar]
- 10.Brown EB, Campbell RB, Tsuzuki Y, et al. In vivo measurement of gene expression, angiogenesis and physiological function in tumors using multiphoton laser scanning microscopy. Nature Med. 2001;7(7):864–8. doi: 10.1038/89997. doi: 10.1038/89997. PubMed PMID: 11433354. [DOI] [PubMed] [Google Scholar]
- 11.Hadjantonakis AK, Dickinson ME, Fraser SE, Papaioannou VE. Technicolour transgenics: imaging tools for functional genomics in the mouse. Nature Rev Genetics. 2003;4(8):613–25. doi: 10.1038/nrg1126. doi: 10.1038/nrg1126. PubMed PMID: 12897773. [DOI] [PubMed] [Google Scholar]
- 12.Swedlow JR, Goldberg I, Brauner E, Sorger PK. Informatics and quantitative analysis in biological imaging. Science. 2003;300(5616):100–2. doi: 10.1126/science.1082602. doi: 10.1126/science.1082602. PubMed PMID: 12677061; PubMed Central PMCID: PMC3522889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weijer CJ. Visualizing signals moving in cells. Science. 2003;300(5616):96–100. doi: 10.1126/science.1082830. doi: 10.1126/science.1082830. PubMed PMID: 12677060. [DOI] [PubMed] [Google Scholar]
- 14.Park CH, Maack T. Albumin absorption and catabolism by isolated perfused proximal convoluted tubules of the rabbit. J Clin Invest. 1984;73(3):767–77. doi: 10.1172/JCI111270. Epub 1984/03/01. doi: 10.1172/JCI111270. PubMed PMID: 6707203; PubMed Central PMCID: PMC425079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carone FA, Ganote CE. D-serine nephrotoxicity. The nature of proteinuria, glucosuria, and aminoaciduria in acute tubular necrosis. Arch Pathol. 1975;99(12):658–62. Epub 1975/12/01. PubMed PMID: 1203037. [PubMed] [Google Scholar]
- 16.Grgic I, Campanholle G, Bijol V, et al. Targeted proximal tubule injury triggers interstitial fibrosis and glomerulosclerosis. Kidney Int. 2012;82(2):172–83. doi: 10.1038/ki.2012.20. Epub 2012/03/23. doi: 10.1038/ki.2012.20. PubMed PMID: 22437410; PubMed Central PMCID: PMC3480325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sekine M, Monkawa T, Morizane R, et al. Selective depletion of mouse kidney proximal straight tubule cells causes acute kidney injury. Transgenic Res. 2012;21(1):51–62. doi: 10.1007/s11248-011-9504-z. Epub 2011/03/25. doi: 10.1007/s11248-011-9504-z. PubMed PMID: 21431867; PubMed Central PMCID: PMC3264875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang MZ, Yao B, Yang S, et al. CSF-1 signaling mediates recovery from acute kidney injury. J Clin Invest. 2012;122(12):4519–32. doi: 10.1172/JCI60363. doi: 10.1172/JCI60363. PubMed PMID: 23143303; PubMed Central PMCID: PMC3533529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gagliardini E, Conti S, Benigni A, Remuzzi G, Remuzzi A. Imaging of the porous ultrastructure of the glomerular epithelial filtration slit. J Am Soc Nephrol. 2010;21(12):2081, 9. doi: 10.1681/ASN.2010020199. Epub 2010/10/30. doi: 10.1681/ASN.2010020199. PubMed PMID: 21030599; PubMed Central PMCID: PMC3014021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Comper WD, Osicka TM, Russo LM. Seldin and Gievisch's The Kidney. Amsterdam: Elsevier, Inc; 2008. pp. 2081–112. [Google Scholar]
- 21.Fassi A, Sangalli F, Maffi R, et al. Progressive glomerular injury in the MWF rat is predicted by inborn nephron deficit. J Am Soc Nephrol. 1998;9(8):1399–406. doi: 10.1681/ASN.V981399. Epub 1998/08/11. PubMed PMID: 9697661. [DOI] [PubMed] [Google Scholar]
- 22.Macconi D, Bonomelli M, Benigni A, Plati T, Sangalli F, Longaretti L, et al. Pathophysiologic implications of reduced podocyte number in a rat model of progressive glomerular injury. Am J Pathol. 2006;168(1):42–54. doi: 10.2353/ajpath.2006.050398. Epub 2006/01/10. doi: 10.2353/ajpath.2006.050398. PubMed PMID: 16400008; PubMed Central PMCID: PMC1592676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schulz A, Hansch J, Kuhn K, et al. Nephron deficit is not required for progressive proteinuria development in the Munich Wistar Fromter rat. Physiol Genomics. 2008;35(1):30–5. doi: 10.1152/physiolgenomics.90270.2008. Epub 2008/07/24. doi: 10.1152/physiolgenomics.90270.2008. PubMed PMID: 18647879. [DOI] [PubMed] [Google Scholar]
- 24.Forbes MS, Thornhill BA, Chevalier RL. Proximal tubular injury and rapid formation of atubular glomeruli in mice with unilateral ureteral obstruction: a new look at an old model. Am J Physiol Renal Physiol. 2011;301(1):F110, 7. doi: 10.1152/ajprenal.00022.2011. Epub 2011/03/25. doi: 10.1152/ajprenal.00022.2011. PubMed PMID: 21429968; PubMed Central PMCID: PMC3129891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lund U, Rippe A, Venturoli D, Tenstad O, Grubb A, Rippe B. Glomerular filtration rate dependence of sieving of albumin and some neutral proteins in rat kidneys. Am J Physiol Renal Physiol. 2003;284(6):F1226–34. doi: 10.1152/ajprenal.00316.2002. doi: 10.1152/ajprenal.00316.2002. PubMed PMID: 12620929. [DOI] [PubMed] [Google Scholar]
- 26.Remuzzi A, Sangalli F, Fassi A, Remuzzi G. Albumin concentration in the Bowman's capsule: multiphoton microscopy vs micropuncture technique. Kidney Int. 2007;72(11):1410–1. doi: 10.1038/sj.ki.5002501. author reply 1. Epub 2007/11/16. doi: 10.1038/sj.ki.5002501. PubMed PMID: 18004314. [DOI] [PubMed] [Google Scholar]
- 27.Tojo A, Endou H. Intrarenal handling of proteins in rats using fractional micropuncture technique. Am J Physiol. 1992;263(4 pt 2):F601–6. doi: 10.1152/ajprenal.1992.263.4.F601. PubMed PMID: 1415732. [DOI] [PubMed] [Google Scholar]
- 28.Osicka TM, Strong KJ, Nikolic-Paterson DJ, Atkins RC, Jerums G, Comper WD. Renal processing of serum proteins in an albumin-deficient environment: an in vivo study of glomerulonephritis in the Nagase analbuminaemic rat. Nephrol Dial Transplant. 2004;19(2):320–8. doi: 10.1093/ndt/gfg226. Epub 2004/01/23. PubMed PMID: 14736954. [DOI] [PubMed] [Google Scholar]
- 29.Dileepan KN, Sharma R, Stechschulte DJ, Savin VJ. Effect of superoxide exposure on albumin permeability of isolated rat glomeruli. J Lab Clin Med. 1993;121(6):797–804. Epub 1993/06/01. PubMed PMID: 8389394. [PubMed] [Google Scholar]
- 30.Fox JG, Quin JD, O'Reilly DS, Boulton-Jones JM. Assessment of glomerular charge selectivity in man by differential clearance of isoamylases. Clin Sci (Lond) 1993;84(4):449–54. doi: 10.1042/cs0840449. Epub 1993/04/01. PubMed PMID: 7683259. [DOI] [PubMed] [Google Scholar]
- 31.Gregoire F, Lambert PP. The biosynthesis of a labelled Bence-Jones-protein and its glomerular permeability in the normal dog. Clin Sci. 1963;25:243–8. Epub 1963/10/01. PubMed PMID: 14070909. [PubMed] [Google Scholar]
- 32.Ruggiero A, Villa CH, Bander E, et al. Paradoxical glomerular filtration of carbon nanotubes. Proc Natl Acad Sci U S A. 2010;107(27):12369–74. doi: 10.1073/pnas.0913667107. Epub 2010/06/23. doi: 10.1073/pnas.0913667107. PubMed PMID: 20566862; PubMed Central PMCID: PMC2901461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sandoval RM, Kennedy MD, Low PS, Molitoris BA. Uptake and trafficking of fluorescent conjugates of folic acid in intact kidney determined using intravital two-photon microscopy. Am J Physiol Cell Physiol. 2004;287(2):C517–26. doi: 10.1152/ajpcell.00006.2004. Epub 2004/04/23. doi: 10.1152/ajpcell.00006.2004. PubMed PMID: 15102609. [DOI] [PubMed] [Google Scholar]
- 34.Russo LM, Sandoval RM, Campos SB, Molitoris BA, Comper WD, Brown D. Impaired tubular uptake explains albuminuria in early diabetic nephropathy. J Am Soc Nephrol. 2009;20(3):489–94. doi: 10.1681/ASN.2008050503. Epub 2009/01/02. doi: 10.1681/ASN.2008050503. PubMed PMID: 19118149; PubMed Central PMCID: PMC2653682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Russo LM, Sandoval RM, McKee M, et al. The normal kidney filters nephrotic levels of albumin retrieved by proximal tubule cells: retrieval is disrupted in nephrotic states. Kidney Int. 2007;71(6):504–13. doi: 10.1038/sj.ki.5002041. Epub 2007/01/18. doi: 10.1038/sj.ki.5002041. PubMed PMID: 17228368. [DOI] [PubMed] [Google Scholar]
- 36.Sandoval RM, Wagner MC, Patel M, et al. Multiple factors influence glomerular albumin permeability in rats. J AmSoc Nephrol. 2012;23(3):447–57. doi: 10.1681/ASN.2011070666. Epub 2012/01/10. doi: 10.1681/ASN.2011070666. PubMed PMID: 22223875; PubMed Central PMCID: PMC3294301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Christensen EI, Birn H, Rippe B, Maunsbach AB. Controversies in nephrology: renal albumin handling, facts, and artifacts! Kidney Int. 2007;72(10):1192–4. doi: 10.1038/sj.ki.5002526. doi: 10.1038/sj.ki.5002526. PubMed PMID: 17805237. [DOI] [PubMed] [Google Scholar]
- 38.Gekle M. Renal albumin handling: a look at the dark side of the filter. Kidney Int. 2007;71(6):479–81. doi: 10.1038/sj.ki.5002123. doi: 10.1038/sj.ki.5002123. PubMed PMID: 17344895. [DOI] [PubMed] [Google Scholar]
- 39.Nakano D, Kobori H, Burford JL, et al. Multiphoton imaging of the glomerular permeability of angiotensinogen. J Am Soc Nephrol. 2012;23(11):1847–56. doi: 10.1681/ASN.2012010078. doi: 10.1681/ASN.2012010078. PubMed PMID: 22997258; PubMed Central PMCID: PMC3482730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peti-Peterdi J. Independent two-photon measurements of albumin GSC give low values. Am J Physiol Renal Physiol. 2009;296(6):F1255–7. doi: 10.1152/ajprenal.00144.2009. Epub 2009/03/20. doi: 10.1152/ajprenal.00144.2009. PubMed PMID: 19297453; PubMed Central PMCID: PMC2692442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tanner GA. Glomerular sieving coefficient of serum albumin in the rat: a two-photon microscopy study. Am J Physiol Renal Physiol. 2009;296(6):F1258–65. doi: 10.1152/ajprenal.90638.2008. Epub 2009/02/13. doi: 10.1152/ajprenal.90638.2008. PubMed PMID: 19211688. [DOI] [PubMed] [Google Scholar]
- 42.Sandoval RM, Wang E, Molitoris MA. Finding the bottom and using it. Intravital. 2013;2:1–9. doi: 10.4161/intv.23674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Christensen EI, Birn H. Megalin and cubilin: multifunctional endocytic receptors. Nat Rev Mol Cell Biol. 2002;3(4):256–66. doi: 10.1038/nrm778. Epub 2002/05/08. doi: 10.1038/nrm778. PubMed PMID: 11994745. [DOI] [PubMed] [Google Scholar]
- 44.Grant BD, Donaldson JG. Pathways and mechanisms of endocytic recycling. Nat Rev Mol Cell Biol. 2009;10(9):597–608. doi: 10.1038/nrm2755. Epub 2009/08/22. doi: 10.1038/nrm2755. PubMed PMID: 19696797; PubMed Central PMCID: PMC3038567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Racoosin EL, Swanson JA. Macropinosome maturation and fusion with tubular lysosomes in macrophages. J Cell Biol. 1993;121(5):1011–20. doi: 10.1083/jcb.121.5.1011. Epub 1993/06/01. PubMed PMID: 8099075; PubMed Central PMCID: PMC2119679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mansson LE, Melican K, Molitoris BA, Richter-Dahlfors A. Progression of bacterial infections studied in real time—novel perspectives provided by multiphoton microscopy. Cell Microbiol. 2007;9(10):2334–43. doi: 10.1111/j.1462-5822.2007.01019.x. doi: 10.1111/j.1462-5822.2007.01019.x. PubMed PMID: 17662072. [DOI] [PubMed] [Google Scholar]
- 47.Melican K, Boekel J, Mansson LE, et al. Bacterial infection-mediated mucosal signalling induces local renal ischaemia as a defence against sepsis. Cell Microbiol. 2008;10(10):1987–98. doi: 10.1111/j.1462-5822.2008.01182.x. doi: 10.1111/j.1462-5822.2008.01182.x. PubMed PMID: 18549455. [DOI] [PubMed] [Google Scholar]
- 48.Christensen EI, Nielsen S. Structural and functional features of protein handling in the kidney proximal tubule. Semin Nephrol. 1991;11(4):414–39. Epub 1991/07/01. PubMed PMID: 1947495. [PubMed] [Google Scholar]
- 49.Clapp WL, Park CH, Madsen KM, Tisher CC. Axial heterogeneity in the handling of albumin by the rabbit proximal tubule. Lab Invest. 1988;58(5):549–58. Epub 1988/05/01. PubMed PMID: 3367637. [PubMed] [Google Scholar]
- 50.Birn H, Christensen EI, Nielsen S. Kinetics of endocytosis in renal proximal tubule studied with ruthenium red as membrane marker. Am J Physiol. 1993;264(2 pt 2):F239–50. doi: 10.1152/ajprenal.1993.264.2.F239. PubMed PMID: 7680532. [DOI] [PubMed] [Google Scholar]
- 51.Moestrup SK, Verroust PJ. Megalin- and cubilin-mediated endocytosis of protein-bound vitamins, lipids, and hormones in polarized epithelia. Annu Rev Nutr. 2001;21:407–28. doi: 10.1146/annurev.nutr.21.1.407. Epub 2001/05/26. doi: 10.1146/annurev.nutr.21.1.407. PubMed PMID: 11375443. [DOI] [PubMed] [Google Scholar]
- 52.Birn H, Fyfe JC, Jacobsen C, et al. Cubilin is an albumin binding protein important for renal tubular albumin reabsorption. J Clin Invest. 2000;105(10):1353–61. doi: 10.1172/JCI8862. Epub 2000/05/17. doi: 10.1172/JCI8862. PubMed PMID: 10811843; PubMed Central PMCID: PMC315466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Amsellem S, Gburek J, Hamard G, et al. Cubilin is essential for albumin reabsorption in the renal proximal tubule. J Am Soc Nephrol. 2010;21(11):1859–67. doi: 10.1681/ASN.2010050492. Epub 2010/08/28. doi: 10.1681/ASN.2010050492. PubMed PMID: 20798259; PubMed Central PMCID: PMC3014001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Storm T, Emma F, Verroust PJ, Hertz JM, Nielsen R, Christensen EI. A patient with cubilin deficiency. N Engl J Med. 2011;364(1):89–91. doi: 10.1056/NEJMc1009804. Epub 2011/01/07. doi: 10.1056/NEJMc1009804. PubMed PMID: 21208123. [DOI] [PubMed] [Google Scholar]
- 55.Morris SM, Tallquist MD, Rock CO, Cooper JA. Dual roles for the Dab2 adaptor protein in embryonic development and kidney transport. EMBO J. 2002;21(7):1555–64. doi: 10.1093/emboj/21.7.1555. Epub 2002/04/03. doi: 10.1093/emboj/21.7.1555. PubMed PMID: 11927540; PubMed Central PMCID: PMC125955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thrailkill KM, Nimmo T, Bunn RC, et al. Microalbuminuria in type 1 diabetes is associated with enhanced excretion of the endocytic multiligand receptors megalin and cubilin. Diabetes Care. 2009;32(7):1266–8. doi: 10.2337/dc09-0112. Epub 2009/04/16. doi: 10.2337/dc09–0112. PubMed PMID: 19366958; PubMed Central PMCID: PMC2699744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chaudhury C, Brooks CL, Carter DC, Robinson JM, Anderson CL. Albumin binding to FcRn: distinct from the FcRn-IgG interaction. Biochemistry. 2006;45(15):4983–90. doi: 10.1021/bi052628y. Epub 2006/04/12. doi: 10.1021/bi052628y. PubMed PMID: 16605266. [DOI] [PubMed] [Google Scholar]
- 58.Blumberg RS, Koss T, Story CM, et al. A major histocompatibility complex class I-related Fc receptor for IgG on rat hepatocytes. J Clin Invest. 1995;95(5):2397–402. doi: 10.1172/JCI117934. Epub 1995/05/01. doi: 10.1172/JCI117934. PubMed PMID: 7738203; PubMed Central PMCID: PMC295868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vidarsson G, Stemerding AM, Stapleton NM, et al. FcRn: an IgG receptor on phagocytes with a novel role in phagocytosis. Blood. 2006;108(10):3573–9. doi: 10.1182/blood-2006-05-024539. Epub 2006/07/20. doi: 10.1182/blood-2006-05-024539. PubMed PMID: 16849638. [DOI] [PubMed] [Google Scholar]
- 60.Haymann JP, Levraud JP, Bouet S, et al. Characterization and localization of the neonatal Fc receptor in adult human kidney. J Am Soc Nephrol. 2000;11(4):632–9. doi: 10.1681/ASN.V114632. Epub 2000/04/07. PubMed PMID: 10752522. [DOI] [PubMed] [Google Scholar]
- 61.Cervenak J, Bender B, Schneider Z, et al. Neonatal FcR overexpression boosts humoral immune response in transgenic mice. J Immunol. 2011;186(2):959–68. doi: 10.4049/jimmunol.1000353. Epub 2010/12/15. doi: 10.4049/jimmunol.1000353. PubMed PMID: 21148035. [DOI] [PubMed] [Google Scholar]
- 62.Kobayashi N, Suzuki Y, Tsuge T, Okumura K, Ra C, Tomino Y. FcRn-mediated transcytosis of immunoglobulin G in human renal proximal tubular epithelial cells. Am J Physiol Renal Physiol. 2002;282(2):F358–65. doi: 10.1152/ajprenal.0164.2001. Epub 2002/01/15. doi: 10.1152/ajprenal.0164.2001. PubMed PMID: 11788451. [DOI] [PubMed] [Google Scholar]
- 63.He W, Ladinsky MS, Huey-Tubman KE, Jensen GJ, McIntosh JR, Bjorkman PJ. FcRn-mediated antibody transport across epithelial cells revealed by electron tomography. Nature. 2008;455(7212):542–6. doi: 10.1038/nature07255. Epub 2008/09/27. doi: 10.1038/nature07255. PubMed PMID: 18818657; PubMed Central PMCID: PMC2773227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ladinsky MS, Huey-Tubman KE, Bjorkman PJ. Electron tomography of late stages of FcRn-mediated antibody transcytosis in neonatal rat small intestine. Mol Biol Cell. 2012;23(13):2537–45. doi: 10.1091/mbc.E12-02-0093. Epub 2012/05/11. doi: 10.1091/mbc.E12-02-0093. PubMed PMID: 22573886; PubMed Central PMCID: PMC3386217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Andersen JT, Daba MB, Berntzen G, Michaelsen TE, Sandlie I. Cross-species binding analyses of mouse and human neonatal Fc receptor show dramatic differences in immunoglobulin G and albumin binding. J Biol Chem. 2010;285(7):4826–36. doi: 10.1074/jbc.M109.081828. Epub 2009/12/19. doi: 10.1074/jbc.M109.081828. PubMed PMID: 20018855; PubMed Central PMCID: PMC2836088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hilliard LM, Osicka TM, Clavant SP, Robinson PJ, Nikolic-Paterson DJ, Comper WD. Characterization of the urinary albumin degradation pathway in the isolated perfused rat kidney. J Lab Clin Med. 2006;147(1):36–44. doi: 10.1016/j.lab.2005.08.008. Epub 2006/01/31. doi: 10.1016/j.lab.2005.08.008. PubMed PMID: 16443003. [DOI] [PubMed] [Google Scholar]
- 67.Koltun M, Comper WD. Retention of albumin in the circulation is governed by saturable renal cell-mediated processes. Microcirculation. 2004;11(4):351–60. doi: 10.1080/10739680490437513. Epub 2004/07/29. doi: 10.1080/10739680490437513. PubMed PMID: 15280074. [DOI] [PubMed] [Google Scholar]
- 68.Koltun M, Nikolovski J, Strong K, Nikolic-Paterson D, Comper WD. Mechanism of hypoalbuminemia in rodents. Am J Physiol Heart Circ Physiol. 2005;288(4):H1604–10. doi: 10.1152/ajpheart.00808.2004. Epub 2004/11/13. doi: 10.1152/ajpheart.00808.2004. PubMed PMID: 15539420. [DOI] [PubMed] [Google Scholar]
- 69.Tenten V, Menzel S, Kunter U, et al. Albumin is recycled from the primary urine by tubular transcytosis. J Am Soc Nephrol. 2013;24(12):1966–80. doi: 10.1681/ASN.2013010018. doi: 10.1681/ASN.2013010018. PubMed PMID: 23970123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chaudhury C, Mehnaz S, Robinson JM, et al. The major histocompatibility complex-related Fc receptor for IgG (FcRn) binds albumin and prolongs its lifespan. J Exp Med. 2003;197(3):315–22. doi: 10.1084/jem.20021829. Epub 2003/02/05. PubMed PMID: 12566415; PubMed Central PMCID: PMC2193842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kim J, Bronson CL, Hayton WL, et al. Albumin turnover: FcRn-mediated recycling saves as much albumin from degradation as the liver produces. Am J Physiol Gastrointest Liver Physiol. 2006;290(2):G352–60. doi: 10.1152/ajpgi.00286.2005. Epub 2005/10/08. doi: 10.1152/ajpgi.00286.2005. PubMed PMID: 16210471. [DOI] [PubMed] [Google Scholar]
- 72.Sarav M, Wang Y, Hack BK, et al. Renal FcRn reclaims albumin but facilitates elimination of IgG. J Am Soc Nephrol. 2009;20(9):1941–52. doi: 10.1681/ASN.2008090976. doi: 10.1681/ASN.2008090976. PubMed PMID: 19661163; PubMed Central PMCID: PMC2736763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Saleh M, Sandoval RM, Rhodes GJ, Campos-Bilderback SB, Molitoris BA, Pollock DM. Chronic endothelin-1 infusion elevates glomerular sieving coefficient and proximal tubular albumin reuptake in the rat. Life Sci. 2012;91:634–7. doi: 10.1016/j.lfs.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]