Abstract
The disease burden in the United States has changed radically in the past 100 years. A striking decrease in infectious diseases as causes of morbidity and mortality has been followed by a steady increase in morbidity and mortality rates from chronic disease, which is now the dominant health issue facing the country, at levels justifying considering chronic disease as having reached epidemic proportions. Research in recent years has shown that many of the common chronic diseases are malleable, i.e., susceptible to therapeutic or preventive efforts aimed at risk factors and susceptible age eras and populations. Although clinical and population-oriented interventions have been increasingly successful in recent decades, more intensive and coordinated preventive efforts will be required, including effective partnerships between clinical medicine and other sectors, particularly at-risk individuals, government, and public health. Robust joint efforts are not only needed, but are likely to be successful.
INTRODUCTION
Over the course of the 20th century, health in the United States has improved substantially: life expectancy increased 56% and the mortality rate decreased by 75% (1). But inside these figures, an extraordinary change occurred. We moved from an era in which infections caused most of the morbidity and most of the mortality to one in which chronic diseases reached epidemic proportions and became the dominant health challenge facing the country.
In the United States a small cluster of chronic diseases, namely heart disease, cancer, stroke, diabetes, and chronic obstructive lung disease together now account for 60% to 70% of deaths and 75% of health care costs (2). This shift in the disease burden, the so-called epidemiologic transition of the 20th century (3), implies a need for new perspectives on how and when diseases arise and how and when we can best intervene, particularly because new knowledge has made it possible to do so earlier and more effectively and in the process reduce individual risk as well as population prevalence. Furthermore, the biology and natural history of these diseases suggest that a sharpened focus on prevention would be a feasible and effective approach to reduction in their prevalence, a particularly important effort because our ability to cure them is sharply limited. To do that, new joint clinical and public health approaches are needed, and chronic disease prevention must move to higher priority for us in the clinical community.
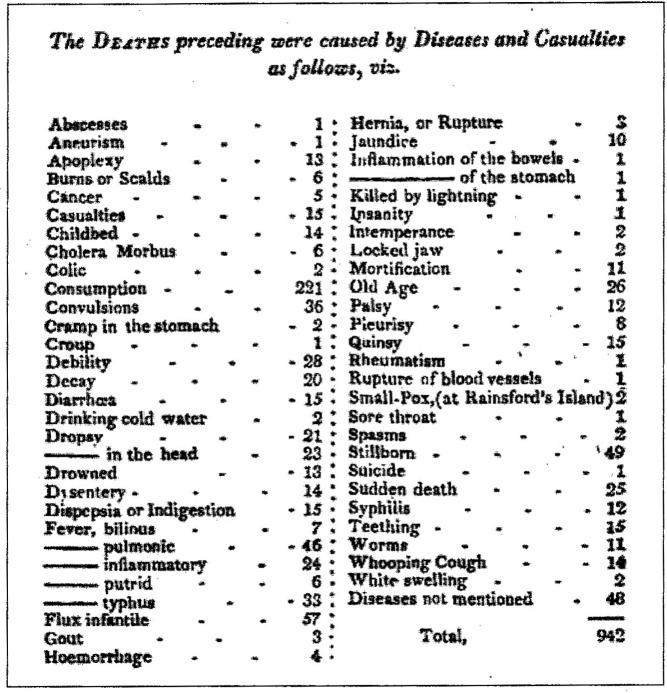
The change in the disease pattern has been dramatic (Figure 1). The Boston Bill of Mortality for 1811 shows that more than 50% of deaths were caused by infections. “Consumption” alone, surely almost entirely tuberculosis, was responsible for a quarter of the deaths, and a cluster of “fevers” identified by their major clinical characteristics caused almost half as many.
Fig. 1.
Causes of death in 1811. Abstract of the Bill of Mortality for the town of Boston. (Source: Ref. 2)
By 100 years later, at the turn of the 20th century, a progressive and dramatic decrease in mortality from infectious diseases was beginning (Figure 2), driven largely by improved nutritional status of the population and a variety of public health measures.
Fig. 2.
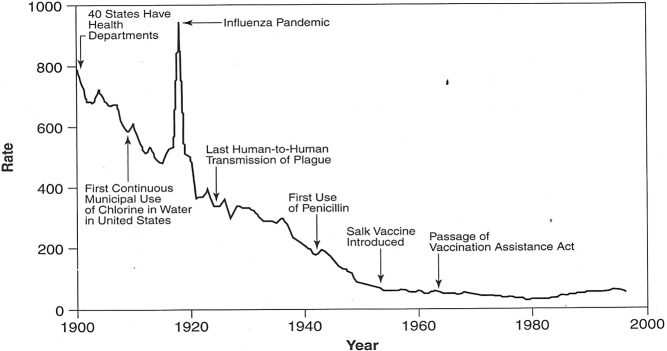
Crude death rate for infectious disease, United States 1900–1996. (Adapted from Armstrong, GL, et al. JAMA 1999:281:61–6)
Two hundred years after the Boston Bill of Mortality was published, i.e., at the outset of the 21st century, the leading causes of death are all chronic diseases; infections do not appear on the list. The “800-pound gorilla in the waiting room” is and will remain chronic disease.
Three major derivatives of these trends can be identified:
> Largely due to the decrease in infectious disease mortality—and public health interventions, life expectancy has increased approximately 30 years in the past century to 78.4 years (an average increase of more than 7 hours per day!), with striking associated aging of the population.
> There has been a major shift in deaths from childhood, when most of the deaths from infections occurred, to older ages.
> An urgent need has developed for an increased focus by the clinical community on prevention, driven by the etiologic, epidemiologic, and relevant clinical characteristics of chronic diseases.
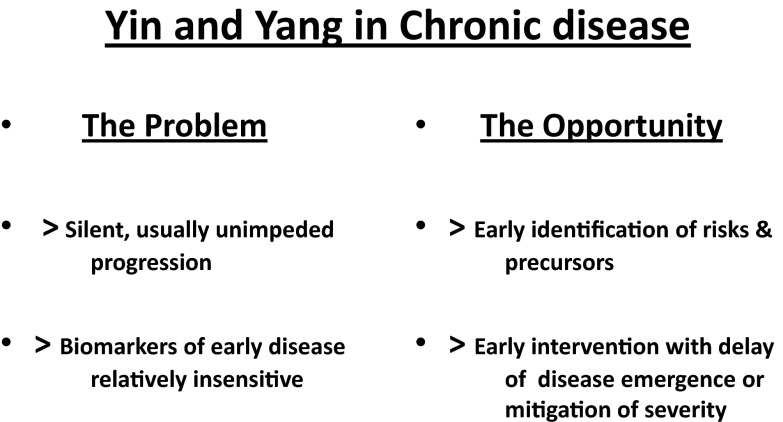
In considering the complexities of prevention in chronic diseases, there are two related premises. First, these are very slow diseases, with long presymptomatic courses, often lasting for decades. Second, presentation with clinical manifestations is a very late event. Within these statements are both the problem and the opportunity (Figure 3).
Fig. 3.
Yin and yang in chronic disease.
IMPORTANT FEATURES OF CHRONIC DISEASES
Chronic diseases are different from acute infections in important respects (Table 1). For example, the unitary microbial causes of infections usually act alone and are disease-specific; exposures are ordinarily brief and either do or do not result in infection. The risk factors involved in the major chronic diseases, in contrast, frequently act in multiples and are often polyvalent, i.e., common to several diseases. Exposures tend to be prolonged; their effects often persist and are expressed in altered probabilities of disease or of its clinical expression. Prevention of infections is often possible through immunizations, vector control, or other modalities; prevention of chronic diseases is more difficult to accomplish and reduction of the probability of ultimate clinical expression through risk mitigation is frequently the most realistic goal.
TABLE 1.
Major Differences Between Acute Infections and Chronic Diseases
| Acute Infections | Chronic Diseases |
| Unitary causes | Risk factors |
| Short courses | Prolonged courses |
| Curability | Management |
| Prevention | Risk reduction |
| Stochastic | Ubiquitous |
Chronic diseases share a number of additional characteristics relevant to prevention (Table 2). Because they arise from determinants and exposures shared by large segments of the population, they are ubiquitous. For example, coronary artery atheroma, frequently advanced, was found in some 77% of routinely autopsied combat deaths during the Korean War (4); the lifetime risk of developing clinically apparent coronary heart disease in the United States is now 49% for men and 32% for women (5); from 1980 through 2011 the crude prevalence of diabetes increased 176% (6), and the lifetime risk of developing diabetes for individuals born in 1980, i.e., 23-year olds, is now 32.8% for men and 38.5% for women (7); prostate cancer was found during 7 years of surveillance in 15.2% of men age 62 to 91 years who had never had a prior prostate-specific antigen level in excess of 4 ng/mL or an abnormal digital rectal examination (8); the lifetime risk of breast cancer in US women is greater than 12% (9); and chronic respiratory disease has now surpassed stroke as the third leading cause of death (10). In addition to their ubiquity, these diseases are frequently multiple: among sexagenarians, for example, 22% have had two diagnosed, 16% have three and 16% have four (11). On the basis of such trends, calling chronic disease ubiquitous, even epidemic, seems a reasonable perspective.
TABLE 2.
Major Features of Chronic Diseases Relevant to Prevention
| Ubiquity |
| Risk factors |
| Early onset |
| Long latency |
| Silent progression |
| Clinical threshold |
| Overt progression |
| Periodic exacerbations |
| Malleability |
| Fluidity |
Genetic determinants probably contribute to all chronic diseases, but in almost all cases exogenous causes (risk factors) are more immediately involved. The array of implicated risk factors is large. Among the most important are health-adverse personal behaviors, now responsible for approximately 40% of deaths in this country (10, 12), especially smoking, dysnutrition, and inadequate physical exercise. It has become fashionable in recent years to refer to the major chronic diseases as noncommunicable, an unfortunate and inaccurate formulation. Not only are a number of cancers clearly infectious in origin and thus communicable in the traditional sense, but the major health-adverse behaviors are also communicable, transmitted from individual to individual largely through social networks, and the diseases they cause are therefore communicable as well.
Smoking, usually initiated in adolescence, causes more than 90% of lung cancer deaths in men, 80% in women, and is contributory or causative in cancers of the larynx, mouth, pharynx, esophagus, bladder, kidney, pancreas, cervix, stomach, and acute myeloid leukemia (12), in addition to its role in atheromatous disease and chronic obstructive lung disease. Compared with nonsmokers, men who smoke are 23 times more likely to get lung cancer, women 13 times (12).
The major health outcome of excessive caloric intake and inadequate physical exercise is obesity, now affecting one third of the American population and increasing in incidence (13). Importantly, childhood obesity is also epidemic and tracks into adult life, with large impacts on the risk of hypertension, ischemic heart disease, colon cancer, and osteoarthritis. Overweight (body mass index of 25–30), about which the data are somewhat conflicting, appears to cost nonsmokers 3.1 to 3.3 years of life expectancy; the impact of obesity (BMI 30+) is clearer—5.8 to 7.1 years on average (13). For smokers the costs are higher.
Health-adverse behaviors are important, but numerous other, less personally induced risk factors are also operative in chronic disease. The risk of individual exposure to behavioral and environmental risk factors is unevenly distributed across the population and is strikingly affected by larger scale determinants, including gender, race, ethnicity, socioeconomic status, class, education, literacy, and severe ongoing psychological and social stress, as well as others at still larger scale, such as the quality of the physical environment, access to high-quality health care, and its relation to national policy.
Social factors are powerful determinants of chronic disease risk (Table 3). These effects are mediated in part through central nervous system mechanisms including the hypothalamic-pituitary-adrenal axis and by effects on the immune system and other pathways contributing to allostatic mechanisms in maintaining stability of the organism in the face of stress (14).
TABLE 3.
Social Factors Are Major Contributors to Chronic Disease Mortality
| Social Factor | No.(%) | Cause of Death | No.(%) |
|---|---|---|---|
| Low education | 193,626 (8.3) | Acute MI | 192,898 (8.0) |
| Low social support | 179,937 (7.7) | Stroke | 167,661 (7.0) |
| Racial segregation | 153,796 (6.6) | Lung cancer | 155,521 (6.5) |
| Income inequality | 145,388 (6.2) | Chronic lower respiratory disease | 122,009 (5.1) |
| Poverty | 102,672 (4.4) | Unintentional injuries | 97,900 (4.1) |
| Area-level poverty | 39,553 (1.7) | Renal failure | 36,471 (1.5) |
The course of chronic diseases is long. Most are characterized by early onset, years or even decades before becoming clinically apparent. The Bogalusa Heart Study (15) and the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Study (16), for example, showed fatty streaks and early raised atheromatous lesions in the aortas and coronary arteries of children as young as 6 years, progressing with age and with clear relation to established risk factors for atherosclerosis. In addition, established coronary artery disease, often severe, was found at autopsy in more than three fourths of a sample of soldiers killed in Korea, men of average age 22 years with normal blood pressures and body weights, selected for military service on the basis of their apparent good health (4). Studies of a number of cancers suggest similar long latencies and prolonged preclinical courses, in the case of colon cancer some 2 to 4 decades (17), with similar estimates for many others (18). Chronic obstructive pulmonary disease follows a similar course. Again, these are slow diseases.
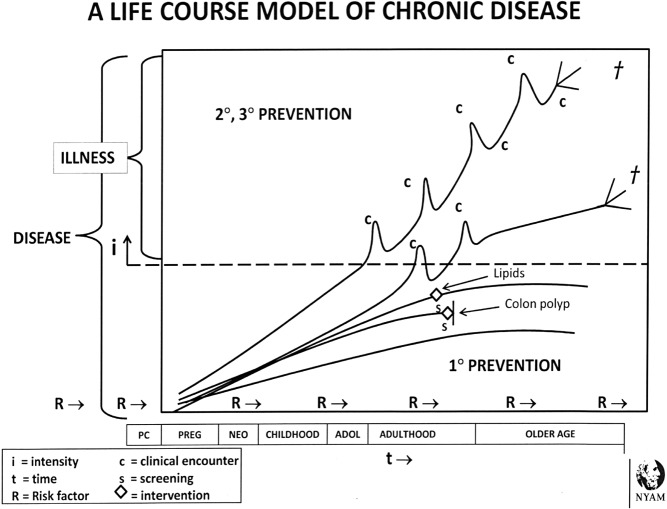
A schematic course (Figure 4) applicable to most chronic diseases indicates early onset, irregular appearance of risk factors across the life course, variable rates of clinical emergence and irregular, complex courses with progression. The schema indicates the late stages and stochastic timing of interfaces with the clinical care system, and long periods of opportunity for secondary and tertiary interventions. It implies a need to re-examine our concepts of health and disease, which we have traditionally considered largely in terms of events above the clinical threshold. Health is clearly not simply the absence of clinically evident disease.
Fig. 4.
Schematic life course model of chronic disease.
Although long thought refractory to interventions, important decreases in mortality from lung cancer, ischemic heart disease, hemorrhagic stroke, and a number of other chronic diseases as well as advances in secondary prevention in hypertensive cardiovascular disease, colon cancer, congestive heart failure, and embolic stroke make it clear that these disorders are malleable and that an expanded preventive agenda is justified. That malleability is a two-way street has however become evident in type II diabetes, the increasing prevalence of which, in addition to its shift from older to younger age groups, threatens to reverse the steady gains in life expectancy of the past century (19).
The concept of fluidity refers to the instability of diagnostic categories over time, shifts that reflect changes in causative factors or therapeutic or preventive efforts and that must be considered in studies of causation, incidence, population distribution, and outcomes. Examples include striking changes in heart disease during the past 75 years, from a high incidence of rheumatic valvular disease, now ended, followed by an era dominated by ischemic heart disease, now apparently past its peak and overlapping with an increasing incidence of heart failure and the re-emergence of valvular disease, now chiefly aortic stenosis. Equally striking changes have occurred in stroke, formerly predominantly hemorrhagic and now largely embolic. At more fundamental levels, colon cancer has been migrating to more proximal sites in the colon (20), and type II diabetes has emerged as an especially powerful additional example of fluidity in diagnostic categories formerly thought to be stable.
PREVENTING CHRONIC DISEASES
The great challenge before us is reducing the prevalence of these diseases. How can we move to evidence-based chronic disease prevention or, if not prevention, management of the earliest stages so that the level of clinical consequence is delayed or never reached? The issues are complex: risk factors are usually multiple, in most cases common to several diseases, emerge irregularly across the life span and persist. In addition, host vulnerability to them is not uniform over time; the life course is marked by a number of especially vulnerable eras, notably intrauterine life, the neonatal period and early childhood, adolescence, and older age. In each of these times, profound biologic change is accompanied by major pressures in the physical and psychosocial environments, with significant implications for long-term health.
The life course approach (21) has emerged in recent years as a powerful perspective that can be organized around an alternative preventive dynamic, namely the preservation of health, an idea more consistent with the characteristics of the major chronic diseases. The central idea of the health preservation paradigm (22) is slowing the irregular but progressive erosion of health over the life course by focusing on the identification of chronic disease risks and precursors as they emerge, and managing them starting at the earliest biologically germane and clinically sensible junctures, especially during particularly vulnerable life eras, and maintaining risk mitigation efforts thereafter.
It was difficult for clinicians to promote prevention to the major focus it needed before effective measures were available. We can do better now. The most basic requirement is the long view. For the individual clinician, each patient at any age presents both the opportunity and the need for an iterative, age-related view of his or her disease-related future (Figure 5) and the mitigation of long-term risk.
Fig. 5.
Chronic disease prevention involves the health of all later iterations of the individual.
In addition, for the clinical community as a whole and for any of its components, partnerships will be crucial to reducing chronic disease prevalence. Active engagement of the patient or the proto-patient is critical particularly with reference to health-related behaviors. Helping patients to become literate about chronic diseases and helping them to also take the long view is difficult but it works—smoking rates among US adults have decreased by half, to less than 20% in recent decades; attention to diet is widespread, and active exercise is a national phenomenon. But more is needed. Obesity is rampant, millions still smoke, health-adverse diets are introduced in childhood and promoted throughout life by powerful stimuli, including electronic media, and abuse of alcohol and other drugs is still a substantial problem for many. More active engagement with the ambient population by the wider clinical community, not only individual clinicians but hospitals, health systems, and the clinical societies, is needed.
These efforts can be amplified through additional partnerships. One, with government at various levels, makes it possible to take health preservation and chronic disease prevention activities to scale at the municipal and state levels. In addition, because health protection/preservation activities command less than 10% of federal health funding (23), the health professions, including the academic sector, can and should bring biologic and clinical evidence to bear as national policy is developed, emphasizing the fact that basic biomedical research, clinical care and the protection of health are not separate enterprises but linked beads on the same string.
The other partnership, potentially very powerful but still underdeveloped, is the one between the clinical and public health enterprises, between individual and population health approaches. A more biologically and clinically informed public health cadre and a clinical enterprise thinking more easily in terms of life course risk mitigation would facilitate joint approaches to earlier intervention in the causal pathways, well proximal to the late stages of disease with which these patients now present. Together clinical medicine and public health can bring the power of a joint perspective to the increasing epidemics of Alzheimer-type dementia or obesity, as examples; together they can develop collaborative research pathways in longitudinal studies of disease or exploration of population heterogeneity in disease expression or therapeutic responsiveness, or the role of gene-environment interactions in pathogenesis.
Clinical and public health perspectives are complementary, in fact overlapping. Biologic and epidemiologic trends make clear that we must move closer together. The chronic disease epidemic is the overriding health issue of our time. It is to a considerable degree and paradoxically a complication of scientific, clinical, and public health success in dealing with infectious disease. It will yield to an analogous approach.
Footnotes
Potential Conflicts of Interest: None disclosed.
REFERENCES
- 1.Guyer B, Freedman MA, Strobino DM, Sondik EJ. Annual summary of vital statistics: trends in the health of Americans during the 20th century. Pediatrics. 2000;106:1307–17. doi: 10.1542/peds.106.6.1307. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Chronic diseases cause 7 in 10 deaths each year in the US; more than 75% of health care costs are due to chronic conditions. Available at: http//;www.cdc.gov/chronicdisease/resources/publications/aag/chronic.htm.
- 3.Omran AR. The epidemiologic transition; a theory of population change. Milbank Q. 1971;49:509–38. [PubMed] [Google Scholar]
- 4.Enos WF, Holmes RF, Beyer J. Coronary disease among US soldiers killed in action in Korea: preliminary report. JAMA. 1953;152:1090–3. doi: 10.1001/jama.1953.03690120006002. [DOI] [PubMed] [Google Scholar]
- 5.Lloyd-Jones DM, Larsen MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet. 1999;353:89–92. doi: 10.1016/S0140-6736(98)10279-9. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Crude and age-adjusted percentage of civilian, non-institutionalized population with diagnosed diabetes, United States, 1980–2011. Available at: http://www.cdc.gov/diabetes/statistics/prev/national/figage.htm.
- 7.Narayan KM, Boyle JP, Thompson TJ, et al. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290:1884–90. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 8.Thompson IM, Panter DK, Goodman PJ, et al. Prevalence of prostate cancer among men with prostate-specific antigen < or = 4 ng per milliliter. N Engl J Med. 2004;350:2239–46. doi: 10.1056/NEJMoa031918. [DOI] [PubMed] [Google Scholar]
- 9.National Cancer Institute, National Institutes of Health. Breast cancer in American women. [Accessed September 24, 2012]. Available at: http://www.cancer.gov/cancertopics/factsheet/detection/probability-breastcancer.
- 10.Hoyert DL, Xu J. Deaths: preliminary data for 2011. National Vital Statistics Reports Oct 10, 2012;61(6):1–51. [PubMed] [Google Scholar]
- 11.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures and complications of multiple chronic diseases in the elderly. Arch Int Med. 2002;162:2269–76. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 12.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270:2207–12. [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Chronic Diseases and Health Promotion. Available at: http://www.cdc.gov/chronicdisease/overview/index.htm.
- 14.Peeters A, Barendregt JJ, Willekens F, et al. Obesity in adulthood and its consequences for life expectancy: a life table analysis. Ann Int Med. 2003;138:24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 15.McEwen B. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–9. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 16.Berenson GS, Srinivasan SR, Welhang B, et al. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. N Engl J Med. 1998;338:1650–6. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 17.Young JP, Malcom GT, McMahan AQ, et al. Prevalence and extent of atherosclerosis in adolescents and young adults. JAMA. 1999;281:727–35. doi: 10.1001/jama.281.8.727. [DOI] [PubMed] [Google Scholar]
- 18.Vogelstein B, Papadopoulos N, Velescu VE, Zhou S, Diaz A, Jr, Kinzler KW. Cancer genome landscapes. Science. 2013;339:1546–58. doi: 10.1126/science.1235122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olshansky SJ, Passaro DJ, Hershow RC, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352:1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 20.National Cancer Institute, National Institutes of Health, Bethesda, Md. SEER Cancer Institute Factsheets: Colon and Rectum cancer. Available at: http://seer.cancer.gov/ststfacts/html/colorect.
- 21.Kuh D, Ben-Shlomo Y. A Life Course Approach to Chronic Disease Epidemiology. New York, NY: Oxford University Press; 2004. [Google Scholar]
- 22.Barondess JA. Toward reducing the prevalence of chronic disease: a life course perspective on health preservation. Perspect Biol Med. 2008;51:616–29. doi: 10.1353/pbm.0.0053. [DOI] [PubMed] [Google Scholar]
- 23.McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff. 2002;21:78–93. doi: 10.1377/hlthaff.21.2.78. [DOI] [PubMed] [Google Scholar]