Abstract
Uterine myomas (fibroids) are the most common pelvic tumors occurring in women, and are the leading cause of hysterectomy. Symptoms can be severe, and traditional treatments involve either surgical removal of the uterus (hysterectomy), or the fibroids (myomectomy). Interstitial ultrasound technologies have demonstrated potential for hyperthermia and high temperature thermal therapy in the treatment of benign and malignant tumors. These ultrasound devices offer favorable energy penetration allowing large volumes of tissue to be treated in short periods of time, as well as axial and angular control of heating to conform thermal treatment to a targeted tissue, while protecting surrounding tissues from thermal damage. The goal of this project is to evaluate interstitial ultrasound for controlled thermal coagulation of fibroids. Multi-element applicators were fabricated using tubular transducers, some of which were sectored to produce 180° directional heating patterns, and integrated with water cooling. Human uterine fibroids were obtained after routine myomectomies, and instrumented with thermocouples spaced at 0.5, 1.0, 1.5, 2.0, 2.5 and 3.0 cm from the applicator. Power levels ranging from 8–15 W per element were applied for up to 15 minute heating periods. Results demonstrated that therapeutic temperatures >50° C and cytotoxic thermal doses (t43) extended beyond 2 cm radially from the applicator (>4 cm diameter). It is anticipated that this system will make a significant contribution toward the treatment of uterine fibroids.
Keywords: Thermal ablation, fibroids, leiomyomas, temperature, thermal dose
1. INTRODUCTION
Uterine fibroids, also known as leiomyomas or myomas, are the most common solid pelvic tumor occurring in women. Fibroids are nodules of well-differentiated smooth muscle encased in fibrous tissue which grow in or on the wall of the uterus, and can range in size from approximately 0.5 cm to greater than 10 cm in diameter [1, 2]. It is estimated that 25–50% of women of reproductive age have one or more uterine fibroids, and depending on the size, number and location of the fibroids, symptoms can be severe, and often include excessive or persistent menorrhagia, pelvic pain and cramping, pressure, urinary problems, constipation, anemia, or infertility.
The most common and permanent treatment for uterine fibroids is surgical removal of the uterus (hysterectomy), particularly in women approaching menopause. An estimated 200,000 hysterectomies are performed in the U.S. each year for the treatment of fibroids[3]. Although a permanent solution for fibroids, hysterectomy is a major surgical procedure associated with significant risk of morbidity.
For pre-menopausal women wishing to retain their uterus for reproductive, psychological or hormonal reasons, myomectomy (surgical removal of fibroids) can be a less invasive alternative to hysterectomy. The procedure may be performed via open laparotomy, or via various advanced laparoscopic and hysteroscopic surgical techniques[4, 5].
A number of treatment options have been developed as an alternative to surgery, including hormonal therapies [6], uterine artery embolization (UAE)[7], and thermal ablation techniques (myolysis) using RF, laser, cryotherapy, and US[8–11]. All have demonstrated clinically significant reduction in fibroid volumes, potentially allowing for avoidance of open surgery and maintaining the ability to bear children.
Thermal ablation typically involves the insertion of an interstitial laser or a radiofrequency (RF) needle to thermally coagulate and necrose uterine fibroids and their vascular supply. However, coagulation of tissue is typically limited to a radial distance of 1 cm or less from the applicator for a single puncture. Thus, high power levels, multiple punctures and longer treatment times are often required to treat commonly occurring large myomas (5+ cm diameter) using either modality[12]. High-intensity focused ultrasound (HIFU) is a sophisticated method used to generate well-localized thermal damage deep within the body, while avoiding damage to the overlaying or surrounding tissues. Although this technique is non-invasive and capable of precise coagulation of tissue, long treatment times (>4 hours) are required to treat large tissue volumes, and access to fibroids located in proximity to bowel or bladder may be limited.
This study represents a work-in-progress towards the development of a clinical, minimally-invasive interstitial ultrasound system for controlled thermal therapy of uterine myomas via laparoscopic and hysteroscopic approaches (Fig. 1). The primary goal of this preliminary study was to investigate the potential of interstitial ultrasound for producing large zones of thermal coagulation in fresh, human myomas in shorter treatment times than can be achieved with other heating modalities.
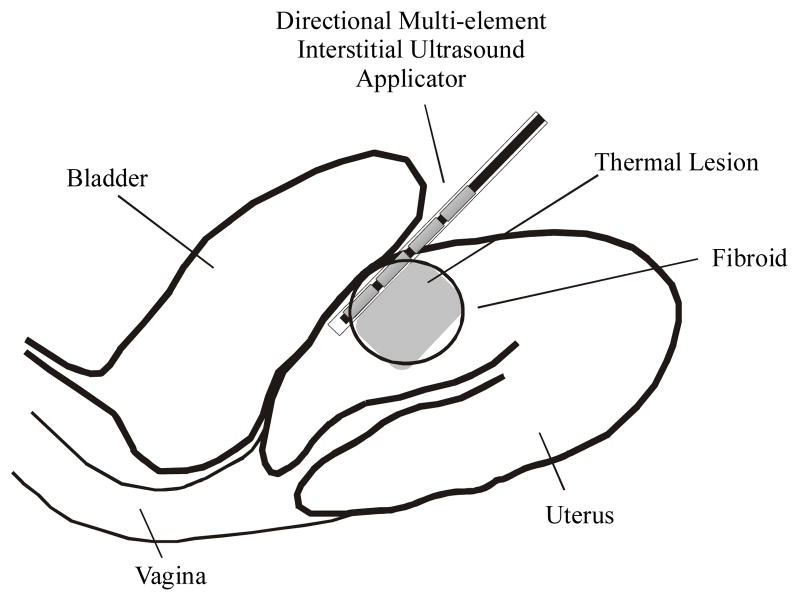
Fig. 1.
Conceptualization of a directional interstitial ultrasound applicator implanted laparoscopically into a subserous fibroid residing near the bladder.
2. APPLICATOR FABRICATION
A family of interstitial ultrasound applicators was fabricated using 2–4 cylindrical piezo-ceramic crystal transducers (PZT-4) with outer diameters (OD) of 1.5 or 2.5 mm and lengths of 10–15 mm (Fig. 2). The operating frequencies (f) of these transducers ranged from 6.5 to 8 MHz. For some of the applicators, the transducers were sectored to produce a 180° actively acoustic sector for directional power deposition[13]. The transducers were mounted on support structures, and a bio-inert plastic layer was applied for electrical and biological insulation. The 1.5 mm OD applicators are inserted into 13 gage brachytherapy catheters (2.4 mm OD), and the 2.5 mm OD applicators into custom PET catheters (3.7 mm OD). Degassed water is circulated through the applicators to cool the transducers during operation, to couple the ultrasound energy to the tissue, and to potentially control temperature at the tissue-catheter interface allowing for greater radial penetration of thermal energy.
Fig. 2.
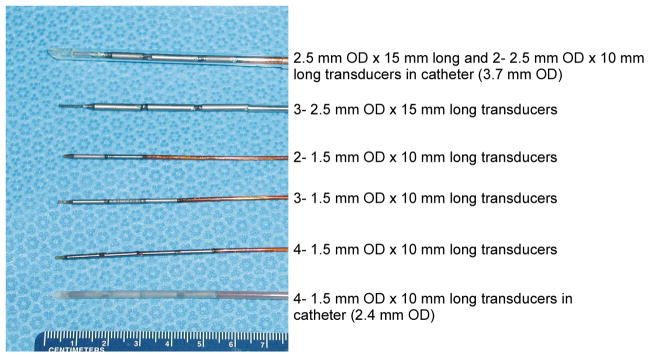
Applicators used for evaluating interstitial ultrasound for thermal ablation of uterine fibroids.
Measurements of electrical impedance (Z) and acoustic efficiency (η) were obtained for each transducer. Z was measured as a function of frequency (5 ≤ f ≤ 10 MHz) using a network analyzer (Hewlett Packard Model #3577A). η was measured as a function of frequency using the force balance technique for cylindrical radiators, and is determined as the ratio of acoustic output power to the applied electrical power[14]. Measurements for the applicators were made with no catheters in place then repeated with the applicators inserted in catheters with a water flow rate of 40 ml·min−1. These measurements are used to determine the optimal driving frequencies, and to determine how much acoustic energy is being delivered to the tissue. Acoustic efficiency data for each transducer type is summarized in Table 1. As expected, there is a 30–40% decrease in η when the applicators are in the catheters due to loss of acoustic energy in the catheter wall.
Table 1.
Acoustic efficiency (η) data for the three transducer geometries used in this study. Measurements were made without catheters, then repeated with catheters (flow rate = 40 ml/min).
| Transducer Description | f (MHz) | η (no catheter) | η (in catheter) | Catheter |
|---|---|---|---|---|
| 1.5 mm OD × 10 mm long | 7.2 | 52% | 32% | 2.4 mm OD |
| 2.5 mm OD × 10 mm long | 6.6 | 59% | 35% | 3.7 mm OD |
| 2.5 mm OD × 15 mm long | 7.6 | 62% | 36% | 3.7 mm OD |
3. EX VIVO HEATING TRIALS
Human uterine fibroids were obtained immediately after removal during routine surgical open myomectomies. The fibroids were instrumented with an interstitial ultrasound applicator and six 20 gage thin-walled spinal needles placed at radial distances of 0.5, 1.0, 1.5, 2.0, 2.5, and 3.0 cm from the applicator, and scattered in angle for thermometry (Fig. 3). A 6 cm × 8 cm × 1 cm plexiglass template was used to ensure alignment of the applicator and spinal needles. The instrumented fibroid was then placed in a 37°C circulating waterbath, and allowed to reach equilibrium. Custom, multi-junction contantan-manganin thermocouple probes consisting of linear arrays of either four 50 μm junctions spaced at 2.5 mm, or seven 50 μm junctions spaced at 5 mm, were inserted into the spinal needles. A 4 channel amplifier with built-in function generator and power monitoring (Advanced Surgical Systems, Inc.) was used to drive the transducers.
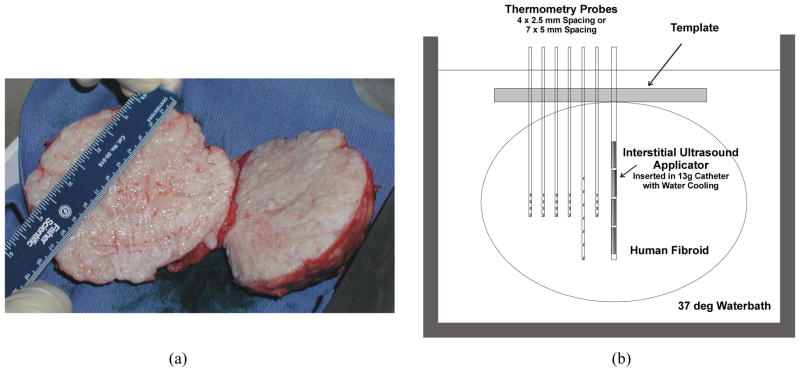
Fig. 3.
(a) Single human uterine leiomyoma (10 cm × 11.5 cm × 10 cm) cut in half, (b) experimental setup for recording temperature data during heating human myomas with interstitial ultrasound. Multi-junction thermocouple probes were spaced at radial distances of 0.5, 1.0, 1.5, 2.0, 2.5 and 3.0 cm from the applicator and staggered in angle.
Several heating trials were performed to investigate the effects of applicator size (2.4 mm OD vs. 3.7 mm OD), directional heating capability (180° vs. 360° heating patterns), and number of active elements (2–4 transducers) on thermal lesion formation (see Table 2). Temperatures were recorded every 3 s at each sensor location (up to 27 data points) using a computer controlled data acquisition system with in-line RF filtering. Typical transient temperature curves, and radial and axial temperature distributions are shown in Fig 4. The accumulated iso-effect thermal dose was calculated from the temperature-time history at each point according to Sapareto and Dewey[15]:
where t43 is the equivalent time at 43°C, T is the average temperature during time Δt, and R is a constant based on the activation energy and absolute temperature from the Arrhenius relationship (R = 2 for T ≥ 43°C, R = 4 for T < 43° C).
Table 2.
Thermal lesion dimensions measured using different applicator configurations (dia = diameter, rad = radius).
| # Elements | Applicator/Catheter | Power (W) | Time (min) | Lesion Dimensions (cm) |
|---|---|---|---|---|
| 4 | 1.5 mm OD/2.4 mm OD | 15 per chan. | 8 | 3.5 dia. × 5.0 longa |
| 3 | 1.5 mm OD/2.4 mm OD | 15 per chan. | 8 | 3.5 dia. × 3.9 longa |
| 2 | 1.5 mm OD/2.4 mm OD | 12 per chan. | 8 | 1.5 rad. × 2.5 longb |
| 3 | 2.5 mm OD/3.7 mm OD | 15 per chan. | 15 | 1.7 rad.b |
| 2 | 2.5 mm OD/3.7 mm OD | 15 per chan. | 7 | 1.2 rad.b,c |
Notes:
360 degree heating pattern;
180 degree directional heating pattern;
Tissue was at thermal equilibrium in a 28° C waterbath rather than a 37° C waterbath resulting in smaller lesion size
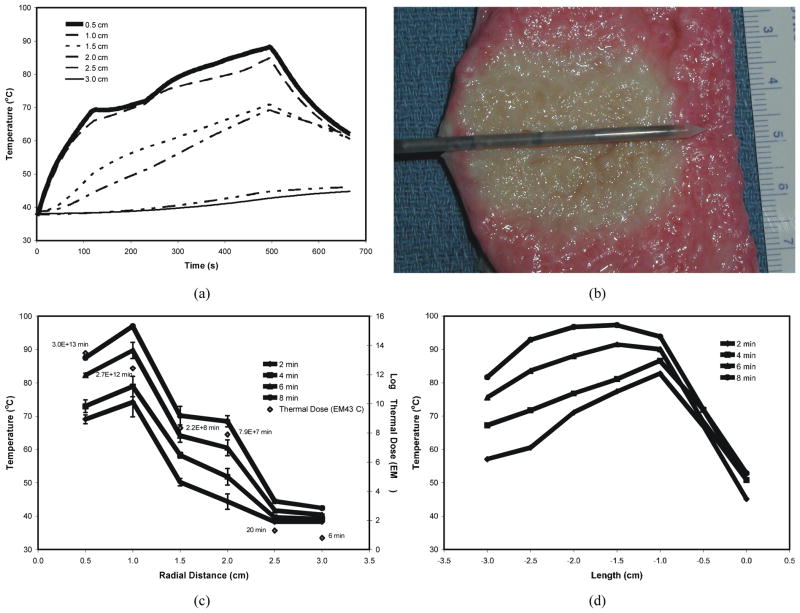
Fig. 4.
Heating trial in a human uterine fibroid using a 4-element applicator with 360 degree heating pattern inserted in a 13 g catheter with 60 ml/min flow rate (f = 8.2–8.5 MHz, 15 W to three elements for 8 minutes). (a) Transient temperature curves (each curve represents the average of 4 sensors at each radial depth of 0.5, 1.0, 1.5, 2.0, 2.5, and 3.0 cm), (b) sagittal slice through thermal lesion, visualized after 20 minutes in a 2% TTC solution (dimensions = 3.5 cm diameter × 3.9 cm long), (c) radial temperature distribution after heating for 2, 4, 6 and 8 minutes, and average accumulated thermal dose at each radial depth after heating for 8 minutes, (d) temperature distribution measured at 1 cm radial distance along the length of the applicator with 3 active elements at 2 minute time intervals.
After heating, the tissue was sliced into sections approximately 5–10 mm thick. Since the thermal lesions were not clearly visible, the tissue sections were placed into a 2% solution of 2,3,5-triphenyltetrazolium chloride (TTC) for approximately 20 minutes. TTC is a tissue viability stain which allows for visualization of acute, lethal tissue damage at a macroscopic level[16]. Measurements of visible thermal lesions were then obtained, and the tissue sections then placed in a 10% buffered Formalin solution for fixation, and later sectioning. Standard hematoxylin and eosin (H&E) stained sections were obtained for histological evaluation.
Results from this study demonstrated that thermal lesions greater than 1.5–1.7 cm radial depth (3–3.5 cm diameter) and up to 5 cm in length (as evidenced by staining with TTC) could be produced in human fibroid tissue in less than 10 min with 15 W of applied electrical power (Fig. 4 and Fig. 5). Further, therapeutic temperatures greater than 50°C, and potentially lethal thermal doses extended beyond 2.0 cm radially from the applicator (>4 cm diameter). Histological examination of heated tissue revealed hyperchromatic nuclei with homogeneously dark chromatin, and no visible nuclear features, as compared to untreated tissue (Fig. 6).
Fig. 5.
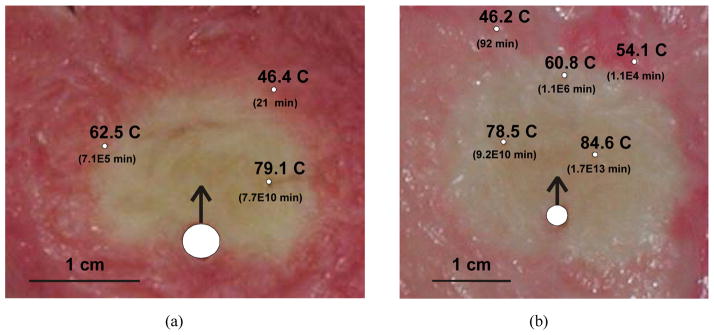
Transverse slices through thermal lesions (as visualized using TTC stain) generated in human uterine fibroids using a 3-element applicator with a 180 degree directional heating pattern, inserted in a 3.7 mm OD catheter with 60 ml/min flow rate (f = 6.6–7.6 MHz). (a) Directional lesion produced by 15 W to two elements for 7 minutes (fibroid was at thermal equilibrium in a 28°C waterbath; lesion radius = 1.2 cm). Maximum temperatures measured at radial distances of 0.5, 1.0, and 1.5 cm from the applicator are shown with corresponding accumulated thermal dose. (b) Directional lesion produced by 15 W to three elements for 15 minutes (lesion radius = 1.7 cm). Maximum temperatures measured at radial distances of 0.5, 1.0, 1.5, 2.0, and 2.5 cm from the applicator are shown with corresponding accumulated thermal dose. Position of applicator and direction of energy delivery are shown by the white circle with arrow for both cases.
Fig. 6.
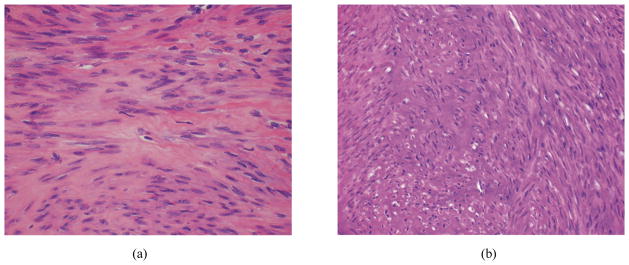
H&E stained sections of human uterine fibroid tissue (400X). (a) Untreated tissue showing lighter, heterogeneous and slightly granular chromatin, and visible nuclear features. (b) Treated tissue indicating hyperchromatic nuclei with no visible features and homogenously dark chromatin. Cytoplasm is also appears slightly darker than the untreated tissue.
4. SUMMARY
Uterine fibroids affect a large percentage of women, and require intensive clinical management which typically includes invasive surgical procedures (hysterectomy) with associated complications. Minimally invasive procedures, including thermal ablation techniques, have recently been applied as an alternative to surgery for the management of these tumors, and have demonstrated clinically significant reduction in fibroid volumes, potentially allowing for avoidance of open surgery and maintaining the ability to bear children. However, improvements are required to increase the acceptability and efficacy of thermal therapy for myomas. These include the need to produce coagulation of large volumes, precisely target specific regions such as vasculature or protect critical adjacent tissues (e.g. bladder, bone, or bowel), access and heat tumors in difficult locations, and reduce procedure times. The ultrasound devices under development in this project have unique features and capabilities which have potential to significantly improve delivery of thermal coagulation for minimally invasive treatment of myomas. These devices offer greater thermal penetration for heating larger fibroids with shorter procedure times, as well as selective heating patterns in both length and angle that can be dynamically controlled to a heat pre-defined treatment volume (e.g., fibroid boundary, feeding vasculature). Thermal lesions visible in TTC-stained specimens were greater than 1.5–1.7 cm in radial depth (3–3.5 cm diameter), however, temperatures greater than 50°C, and potentially lethal thermal doses extended beyond 2.0 cm radially from the applicator (>4 cm). Although higher power levels or longer treatment times may be required to produce similar results in vivo, it is anticipated that this interstitial ultrasound system will make a significant contribution toward thermal treatment of uterine fibroids. Furthermore, these ultrasound devices are MRI compatible, and can be coupled with non-invasive MRI thermal monitoring for precise thermal delivery and verification of treatment.
Footnotes
William H. Nau, Jr.; Chris J. Diederich; Jeff Simko; Titania Juang; Alison Jacoby; E. C. Burdette, Ultrasound interstitial thermal therapy (USITT) for the treatment of uterine myomas, Proc. SPIE. 6440, Thermal Treatment of Tissue: Energy Delivery and Assessment IV, 64400F. (February 08, 2007) doi: 10.1117/12.703220 Copyright 2011 Society of Photo‑Optical Instrumentation Engineers. One print or electronic copy may be made for personal use only. Systematic reproduction and distribution, duplication of any material in this paper for a fee or for commercial purposes, or modification of the content of the paper are prohibited. DOI abstract link: http://dx.doi.org/10.1117/12.703220
References
- 1.Treating fibroids. Harvard Womens Health Watch. 1998;5:2–3. [PubMed] [Google Scholar]
- 2.Nowak RA. Fibroids: pathophysiology and current medical treatment. Baillieres Best Pract Res Clin Obstet Gynaecol. 1999;13:223–38. doi: 10.1053/beog.1999.0019. [DOI] [PubMed] [Google Scholar]
- 3.Goldfarb HA. Myoma coagulation (myolysis) Obstetrics and Gynecology Clinics of North America. 2000;27:421–30. doi: 10.1016/s0889-8545(00)80032-7. [DOI] [PubMed] [Google Scholar]
- 4.Donnez J, Mathieu PE, Bassil S, Smets M, Nisolle M, Berliere M. Laparoscopic myomectomy today. Fibroids: management and treatment: the state of the art. Human Reproduction. 1996;11:1837–40. doi: 10.1093/oxfordjournals.humrep.a019502. [DOI] [PubMed] [Google Scholar]
- 5.Davies A, Hart R, Magos AL. The excision of uterine fibroids by vaginal myomectomy: a prospective study. Fertility and Sterility. 1999;71:961–4. doi: 10.1016/s0015-0282(99)00061-8. [DOI] [PubMed] [Google Scholar]
- 6.Felberbaum RE, Germer U, Ludwig M, Riethmüller-Winzen H, Heise S, Buttge I, Bauer O, Reissmann T, Engel J, Diedrich K. Treatment of uterine fibroids with a slow-release formulation of the gonadotrophin releasing hormone antagonist Cetrorelix. Human Reproduction. 1998;13:1660–8. doi: 10.1093/humrep/13.6.1660. [DOI] [PubMed] [Google Scholar]
- 7.Wong GC, Muir SJ, Lai AP, Goodwin SC. Uterine artery embolization: a minimally invasive technique for the treatment of uterine fibroids. Journal of Womens Health & Gender-Based Medicine. 2000;9:357–62. doi: 10.1089/15246090050020664. [DOI] [PubMed] [Google Scholar]
- 8.Bergamini V, Ghezzi F, Cromi A, Bellini G, Zanconato G, Scarperi S, Franchi M. Laparoscopic radiofrequency thermal ablation: a new approach to symptomatic uterine myomas. Am J Obstet Gynecol. 2005;192:768–73. doi: 10.1016/j.ajog.2004.10.591. [DOI] [PubMed] [Google Scholar]
- 9.Hindley JT, Law PA, Hickey M, Smith SC, Lamping DL, Gedroyc WM, Regan L. Clinical outcomes following percutaneous magnetic resonance image guided laser ablation of symptomatic uterine fibroids. Hum Reprod. 2002;17:2737–41. doi: 10.1093/humrep/17.10.2737. [DOI] [PubMed] [Google Scholar]
- 10.Exacoustos C, Zupi E, Marconi D, Romanini ME, Szabolcs B, Piredda A, Arduini D. Ultrasound-assisted laparoscopic cryomyolysis: two- and three-dimensional findings before, during and after treatment. Ultrasound Obstet Gynecol. 2005;25:393–400. doi: 10.1002/uog.1861. [DOI] [PubMed] [Google Scholar]
- 11.Tempany CM, Stewart EA, McDannold N, Quade BJ, Jolesz FA, Hynynen K. MR imaging-guided focused ultrasound surgery of uterine leiomyomas: a feasibility study. Radiology. 2003;226:897–905. doi: 10.1148/radiol.2271020395. [DOI] [PubMed] [Google Scholar]
- 12.Goldfarb HA. Laparoscopic Coagulation of Myoma (Myolysis) Obstetrics and Gynecology Clinics of North America. 1995;22:807–819. [PubMed] [Google Scholar]
- 13.Nau WH, Diederich CJ, Stauffer PR. Directional power deposition from direct-coupled and catheter-cooled interstitial ultrasound applicators. Int J Hyperthermia. 2000;16:129–44. doi: 10.1080/026567300285330. [DOI] [PubMed] [Google Scholar]
- 14.Hynynen K. Acoustic power calibrations of cylindrical intracavitary ultrasound hyperthermia applicators. Medical Physics. 1993;20:129–134. doi: 10.1118/1.597094. [DOI] [PubMed] [Google Scholar]
- 15.Sapareto SA, Dewey WC. Thermal dose determination in cancer therapy. Int J Radiat Oncol Biol Phys. 1984;10:787–800. doi: 10.1016/0360-3016(84)90379-1. [DOI] [PubMed] [Google Scholar]
- 16.Chen L, Bouley DM, Harris BT, Butts K. MRI study of immediate cell viability in focused ultrasound lesions in the rabbit brain. J Magn Reson Imaging. 2001;13:23–30. doi: 10.1002/1522-2586(200101)13:1<23::aid-jmri1004>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]