Abstract
Nonalcoholic fatty liver disease (NAFLD), defined as abnormal accumulation (> 5%) of hepatic triglyceride without excess alcohol intake, is the most common form of chronic liver disease in adults and children in the United States. NAFLD encompasses a spectrum of histologic findings including uncomplicated steatosis, steatosis with inflammation and steatohepatitis [nonalcoholic steatohepatitis (NASH)]; the latter can advance to cirrhosis and hepatocellular carcinoma. NASH is currently accepted as the hepatic manifestation of the set of cardiovascular risk factors collectively known as metabolic syndrome. In 1999 a system for histologic grading and staging for NASH was proposed; this was revised by the NASH Clinical Research Network in 2005 for the entire spectrum of lesions in NAFLD, including the lesions and patterns of pediatric NAFLD, and for application in clinical research trials. Diagnosis remains distinct from grade and stage. A recent European proposal separates steatosis from activity to derive a numeric diagnosis of NASH. Even though there have been promising advancements in non-invasive testing, these tests are not yet detailed enough to replace the full range of findings provided by liver biopsy evaluation. Limitations of biopsy are acknowledged, but liver biopsy remains the “gold standard” for diagnosis and determination of amounts of necroinflammatory activity, and location of fibrosis, as well as remodeling of the parenchyma in NASH. This review focuses on the specific histologic lesions of NAFLD and NASH, grading and staging, differential diagnoses to be considered, and the continuing role of the liver biopsy in this important liver disease.
Keywords: Nonalcoholic fatty liver disease, Nonalcoholic steatohepatitis, Liver biopsy, Histopathology, Grading and staging
Core tip: Nonalcoholic fatty liver disease (NAFLD) is the most common form of chronic liver disease; no clinical or serologic tests have yet replaced liver biopsy for definitive diagnosis. The histologic spectrum includes steatosis, steatohepatitis, and cirrhosis with or without active steatohepatitis. Hepatocellular carcinoma may occur in cirrhosis, or prior to cirrhosis. Liver biopsy provides vital data for patient care, clinical trials, and for ongoing research into nuances of the disease process. The histologic spectrum of NAFLD, features with co-existent diseases, differential diagnoses, grading and staging methods and the role of liver biopsy, as well as a brief description of non-invasive alternatives, are discussed.
INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD), defined as abnormal accumulation of triglycerides in the liver (i.e., > 5%) in the absence of significant alcohol intake, is recognized as the most common cause of chronic liver disease, and is estimated to affect 30% of adults and 10% of children in United States[1]. The prevalence of NAFLD parallels that of metabolic syndrome, insulin resistance, type 2 diabetes and central obesity[2]. It is currently recognized that mortality in the majority of individuals with NAFLD is more likely from cardiovascular diseases than from liver disease[3], thus, even though recent studies have documented similar epidemiologic and histologic features of NAFLD and nonalcoholic steatohepatitis (NASH) in the geriatric population[4,5], this age group will not be further discussed in this review. The prevalence is highest in the ethnic Hispanic population, followed by non-Hispanic whites, Asians and African Americans[6,7]. The prevalence increases significantly up to 80%-90% in obese adults, 60% in patients with hyperlipidemia, and 30%-50% in diabetics[2]. Only a minority of subjects with steatohepatitis actually progress to fibrosis or cirrhosis[8]. Currently, however, NAFLD is the third most common cause of liver transplantation in United States[9], and is projected to be the leading cause of liver transplantation in the United States by 2020[1]. In addition, approximately 4%-22% of hepatocellular carcinomas in the Western world are attributed to NAFLD[10]. Hepatocellular carcinoma may develop in either cirrhosis or non-cirrhotic NAFLD, as recently reviewed[10,11].
NAFLD is a spectrum of histologic lesions of steatosis at one end, and steatohepatitis and cirrhosis at the other[12]. However, whether in a given patient there is actual “progression” from steatosis to steatohepatitis without concurrent clinical complications such as weight gain, or new onset diabetes, has not been adequately studied. What is accepted is that steatosis itself is considered “non-progressive” whereas steatohepatitis is the constellation of lesions with potential to progress; this was first shown in a seminal series of Matteoni et al[13]. Thus, the ability of the liver biopsy is to separate individuals with steatohepatitis from those with “only” steatosis (which includes steatosis with inflammation); this is an important goal that any diagnostic test should meet. NASH is defined histopathologically by the presence of a constellation of features: steatosis, lobular and portal inflammation and liver cell injury in the form of hepatocyte ballooning. Initially, in adults, the ballooning and fibrosis are in a zone 3 distribution; once abnormal matrix is deposited (i.e., fibrosis), and architectural remodeling occurs, the zonality of injury is less apparent.
Many advances have occurred since the initial recognition that fatty liver disease could occur in overweight and/or diabetic subjects who weren’t over-exposed to alcohol by several researchers including Thaler[14], Klatskin et al[15], Schaffner et al[16] and Ludwig et al[17] in the late 1970’s and early 1980’s. These include histopathologic work in humans with careful clinical correlations discerning the prevalence of NAFLD and NASH[18], the roles of progenitor cells and the ductular reaction in fibrogenesis[18-21], and the role of innate and adaptive immune-mediated mechanisms in steatohepatitis[22], progression of steatohepatitis to cirrhosis and hepatocellular carcinoma[10,23,24] and genetic and genomic underpinnings of disease susceptibility and progression[25,26].
LIVER BIOPSY: ROLE, INDICATIONS, AND DRAWBACKS
The general indications for performing a liver biopsy in patients with NAFLD are to confirm or exclude the diagnosis, diagnose other liver diseases, and to determine amounts of damage to the liver for treatment and prognosis. The last includes necroinflammatory activity, which is potentially reversible, and collagen deposition with varying degrees of remodeling, which is potentially less reversible. More specific indications have been recently stated. According to the 2012 guidelines from American Association for the Study of Liver Disease (AASLD), liver biopsy should be reserved for subjects who will “benefit”, for subjects with potentially competing diagnoses, and for children with either an unclear diagnosis or in whom consideration is being given for medication[27]. The European Association for the Study of Liver Disease position statement on liver biopsy differed slightly and recommended liver biopsy in all bariatric surgery subjects, and as an endpoint in all clinical trials[28]. Liver biopsy remains the standard against which noninvasive (serologic and imaging) methods are judged in order to assess these features. By histologic evaluation, one is able to distinguish between NASH, a lesion with progressive potential, and no NASH, lesions without potential to progress[28-33].
Performing a liver biopsy on every patient with suspected NAFLD remains a controversial subject in daily practice, and clearly is not a practical consideration as a “screening” tool. There are studies, however, that support the value of liver biopsy. A frequently cited albeit older study by Skelly et al[34] showed that of 354 biopsied patients with otherwise unexplained abnormal liver tests 66% had fatty liver, 50% of those had steatohepatitis, approximately 19% of the remaining biopsies had other treatable causes diagnosed by the pathology evaluation including autoimmune hepatitis (AIH), primary biliary cirrhosis (PBC), hemochromatosis and alcoholic liver disease (ALD).
A more recent study used a modeling system to show that obtaining a liver biopsy could provide survival benefit to patients with NAFLD. Gaidos et al[35] evaluated the long-term benefit of biopsy vs no biopsy. The study showed that performing an early liver biopsy resulted in a higher percentage of having mild liver disease ultimately in NAFLD patients. Early diagnosis and treatment resulted in decrease in progression to severe disease or transplant and a predicted survival advantage in NAFLD patients. In addition, the risk of death related to liver biopsy did not offset the survival advantage. Others have demonstrated the benefits of liver biopsy in NAFLD by demonstrating the presence of NAFLD or NASH in “atypical settings” such as concurrent disease processes such as Hepatitis C[36-38], AIH, PBC, hereditary hemochromatosis (HH)[36], as well as drugs and occupational exposures[39-41]. Liver biopsy studies proved the validity of the concept of the presence of all ranges of necroinflammatory activity and fibrosis, including cirrhosis, in the presence of normal alanine aminotransferase values in adults[42-44], and children[45]. The current state of investigation for pathologists is to evaluate which subjects will develop fibrosis and why, and which findings on early biopsies, if any, may be predictive of future outcomes.
Liver biopsy studies have given insight into natural history of NASH, albeit in a selected group of primarily adult subjects. The prevalence of NASH, 12.2% of over 300 multi-ethnic adult subjects, was established in a Texas city by liver biopsy in an unbiased community who were willing to undergo ultrasound and subsequent liver biopsy. Nearly 30% had evidence of NAFLD by ultrasound[18]. This was the first study of its kind in adults, as all prior studies had been done either in living donors, who did not have evidence of steatohepatitis, or in autopsies. Liver pathology evaluation was the first to establish the remarkable incidence of fatty liver of up to 13% in an autopsy study of children who died from accidental deaths[46]. Liver biopsy further characterized the association of cardiovascular disease and biopsy proven NAFLD in 150 overweight children compared with 150 overweight children without NAFLD[47].
At the current time, it remains common practice to attribute cases of cryptogenic cirrhosis to burned out “NASH”. This is not altogether appropriate unless there is prior biopsy proof of NASH because clinically it is known that other forms of liver injury can “burn out”, in particular alcoholic liver disease and autoimmune liver disease. It was liver biopsy studies that indicated that NASH may be one of the underlying causes of cryptogenic cirrhosis, which, by definition, has no serologic markers for determination of cause of liver disease. This was shown in a small case series[48] then larger case studies comparing NAFLD-related cirrhosis to cirrhosis related to other forms of serologically diagnosed chronic liver disease[49], and finally in kindred studies[50]. Liver biopsy in cirrhosis of otherwise unknown etiology can show evidence of ongoing steatohepatitis, or burned out disease without any activity or steatosis in subjects with clinical features of metabolic syndrome. Additionally, not only will NASH progress to advanced fibrosis and cirrhosis in a subset of individuals if the underlying metabolic conditions are unchanged, but several studies have verified that NASH may also regress spontaneously, as reviewed[51]. This phenomenon has largely been observed in either placebo arms or in the non-responders of treatment trials[52-54].
In 2009, an AASLD sponsored workshop raised important questions for advancement in the field of NAFLD, providing guidance for investigators for clinical design and end points including pathologic and laboratory data[55]. As evidenced by published recommendations, liver biopsy is an important tool in clinical trials. Outcomes remain based on histologic features which provide information regarding the effects of intervention on extent and severity of hepatocellular injury, inflammation, and architectural alterations as well as the ultimate diagnosis. To date, histologic evaluation remains the “hard endpoint” that can be measured with the most reliability[12]. The most commonly used tool for histologic evaluation is the nonalcoholic fatty liver disease activity score (NAS) (Details will be discussed in later in the text). The NAS was not intended to replace the diagnosis but to provide a sensitive tool to assess the changes that might occur with treatment[56]. However, unintended use of this score has been noted by the investigators[56]. A study by NASH clinical research network (CRN), including 976 adult liver biopsies, challenged this concept and demonstrated that while the NAS correlated with the diagnosis, it was in the lower and higher ends of the spectrum. Therefore, if NAS were to reflect the diagnosis, a significant portion of these patients would be misclassified[56]. Most importantly diagnosis of NASH was strongly associated with the presence of diabetes, quantitative insulin sensitivity check index (QUICKi) and homeostasis model assessment-estimated insulin resistance (HOMA-IR)[56] while the diagnosis and the NAS both correlated with aminotransferases. This data further supported the concept that scoring lesions and diagnosing patterns of injury are different processes for a pathologist[29,56].
LIVER BIOPSY LIMITATIONS
Liver biopsy, as useful as it is, however, does have limitations. The major limitation of liver biopsy is the invasive nature of the procedure. Though considered “minimal”, liver biopsy is an invasive procedure and can have complications even in the ideal clinical conditions, including pain, minor and major bleeding (0.3%). Organ perforation is uncommon, but more likely in blind biopsy. Death albeit rare, has been reported at 0.01%[57]. Currently, the majority of liver biopsies are performed under ultrasound guidance. As with liver biopsy interpretation, operator experience is an important factor in success[58].
As in other chronic liver diseases, biopsy size is an important, but often unrecognized consideration in diagnostic accuracy[12,59,60]. A biopsy, at least 1.6 cm in length with 1.2-1.8 mm diameter, containing approximately 10 portal tracts is considered adequate[61,62]. Even then an adequate liver biopsy represents approximately 1:50.000 of the entire organ[63].
Some limitations of liver biopsy are due to variability of the disease process itself, as with all other forms of chronic liver disease. NAFLD, while a diffuse process of the liver, can have differences particularly in fibrosis due to the location of the samples under evaluation. The subcapsular liver tissue is generally more fibrotic, and the left lobe has larger portal areas near the capsule than the right. Thus, it is important, particularly for studies, that both pre and post study biopsies are done in a similar fashion and from the same region of the liver[12]. Authors have not always agreed on the amounts of histologic sampling variability in NAFLD. Larson et al[62] found minimal variability in steatosis, NAS ≥ 5 and fibrosis between two samples in bariatric subjects. The study also emphasized the need for not only appropriate length, but also width of liver biopsy needle. Another study in morbidly obese individuals undergoing bariatric surgery found moderate histologic variability between lobes[64]. In two additional studies, one in bariatrics and one in non-morbidly obese subjects, two separate biopsies from the same location in the same lobe were graded and staged independently and showed one or more points in discordance in fibrosis stage[59,60]. In addition hepatocyte ballooning, one of the diagnostic requirements of NASH, was not present in 24% of patients in one study in one set of the biopsies[60]. The implications for clinical studies for evaluating pre and post treatment biopsies are apparent.
The experience of the pathologist also plays a significant role in making the diagnosis of NAFLD; this is similar to other liver diseases[58]. The interobserver agreements on steatosis, ballooning and fibrosis were good amongst pathologists in the study of Kleiner et al[65] that included 32 adult biopsies and 9 pathologists but not so strong for location of steatosis and for inflammation[66]. Similar observations were reported in a study of 21 liver biopsies read by eight experienced Japanese hepatopathologists with good agreement on fibrosis and extent of steatosis. Younossi et al[67], showed good concordance for extent of steatosis and degree of fibrosis along with ballooned hepatocytes in 53 liver biopsies interpreted by 4 experienced liver pathologists.
The high prevalence of NAFLD in the population and the limitations, risks and cost of liver biopsy have led investigators to seek for non-invasive methods to diagnose, and stage NALFD. The ideal test would be cheap, reproducible, and would be able to diagnose the full spectrum of NAFLD, predict fibrosis, and also reflect changes that occur with treatment[31,32]. Several different methodologies including imaging modalities, serum markers and combined tests are currently being investigated. Even though advancements are being made in these fields, none of these can provide detailed and accurate enough information to replace the liver biopsy. For a more comprehensive summary of recent non-invasive tests, the reader is referred to current reviews[31,32].
In summary an adequate liver biopsy, with appropriate clinical history, interpreted by a trained liver pathologist, is not only pivotal for an accurate and complete diagnosis (or exclusion) of NAFLD (or NASH), but also is optimal for obtaining detailed information regarding disease pattern, severity and fibrosis. It provides important information with respect to subtypes, potential future risks, possible etiology, and natural history of disease, and sets the ground work for future molecular studies and clinical trials, assisting clinical colleagues and patients with treatments and follow-up.
HISTOLOGIC FEATURES, GRADING, AND STAGING OF NAFLD: ADULTS
In NAFLD, 5% or more macrovesicular steatosis is required for the diagnosis. This may occur with or without other findings, but without it, the diagnosis cannot be entertained. Steatosis initially is found predominantly in hepatocytes around the terminal hepatic venule (zone 3); when abundant, steatosis can be panacinar, and when resolving, may be irregular, or azonal. The type of triglyceride accumulation that is observed in NAFLD is predominantly macrovesicular and is typically characterized by a single or a few lipid droplets within the affected hepatocytes, displacing the nucleus peripherally within the cell (Figure 1A). When the droplets are smaller, i.e., “small droplet” steatosis, they are well-defined and easily delineated from one another. Small droplets often form droplets around the larger droplets and may coalesce to form the macrodroplet. Albeit small, these types of droplets should not be confused for true “microvesicular” steatosis, as the pathophysiology and thus implications for liver function differ (Figure 1B). Microvesicular steatosis may occur in a patchy distribution in up to 10 % of NASH cases[68,69], and has been shown in a large study to be associated with ballooned hepatocytes, and advanced fibrosis[69].
Figure 1.
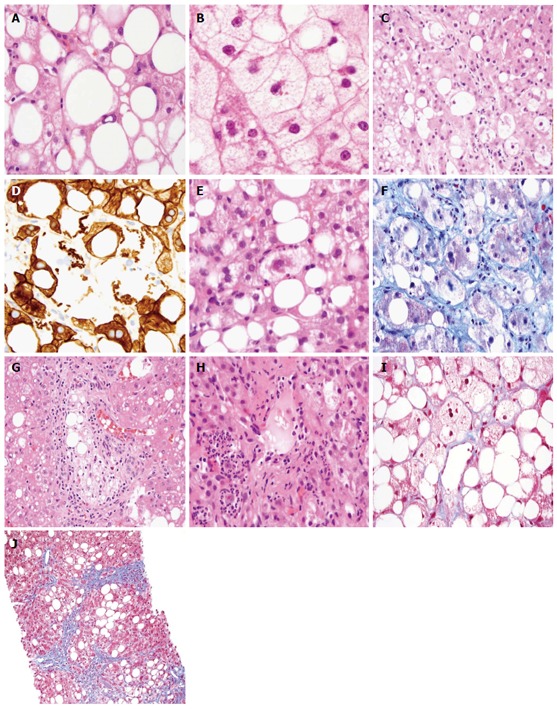
Histologic features, grading, and staging of nonalcoholic fatty liver disease. A: Mixed large and small droplet steatosis, single droplet, with nucleus pushed to one side, HE stain, 600 ×; B: Microvesicular steatosis, nuclei in the center with foamy cytoplasm, and megamitochondria HE stain, 600 ×; C: Ballooned hepatocytes with flocculent cytoplasm, HE stain, 600 ×; D: Loss of cytoplasmic expression of keratin 8/18 in ballooned hepatocytes, 600 ×; E: Mallory-Denk body, HE stain, 600 ×; F: Mallory-Denk body in blue-green color and dense perisinusoidal fibrosis, Trichrome stain, 600 ×; G: Portal lipogranuloma, HE stain, 400 ×; H: Mallory-Denk bodies and satellitosis HE stain, 600 ×; I: Delicate perisinusoidal fibrosis, Trichrome stain, 600 ×; J: Bridging fibrosis, Trichrome stain, 200 ×.
There are a constellation of histopathologic lesions required for the diagnosis of steatohepatitis. These include steatosis, inflammation (lobular and portal) and hepatocyte injury, commonly in the form of ballooning. Ballooned hepatocytes appear as enlarged hepatocytes with a flocculent, cleared appearance of the cytoplasm with irregular cytoplasmic borders[30,70] (Figure 1C). Often the nucleus is hyperchromatic. Hepatocyte ballooning has been shown to correlate with oxidative damage[71] and microtubule disruption[30,70], and loss of normal structure of the cytoskeleton[71,72]. In adult NASH, ballooned hepatocytes are most commonly seen in zone 3 and if fibrosis is present, they are intermixed with perisinusoidal collagen fibers. Keratins 8/18, present throughout the cytoplasm of all normal hepatocytes[72], are damaged in ballooned hepatocytes; this is manifest with loss of cytoplasmic immunoexpression (Figure 1D), movement to submembranous location, and highlighting of Mallory-Denk bodies (MDB)[73]. MDB are ubiquitinated keratins and cytoskeletal structures within the proteosome (Figure 1E). p62 and ubiquitin are immunomarkers that label MDB[74]. By trichrome stain, MDB can be blue or green (Figure 1F). In NASH, MDBs are often less well-formed than in alcoholic hepatitis or alcoholic steatohepatitis[75]. Finally, ballooning has been associated with several relevant clinical markers such as measures of insulin resistance[76], increased serum cholesterol[76,77] and serum markers of necroinflammation[78]. Similar correlations have also been noted in the pediatric population[79].
Lobular inflammation, typically more prominent than portal inflammation in uncomplicated adult NAFLD, is mostly mononuclear, but also includes Kupffer cell clusters, microgranulomas with or without lipid droplets, and larger lipogranulomas (Figure 1G). Lefkowitch noted prominent enlargement and aggregation of Kupffer cells around terminal hepatic venules in NASH, in contrast to the even distribution in normal livers and uncomplicated steatosis[80]. Kupffer cells, the largest resident macrophage population in liver, are an important component of the innate immune system[81] and are implicated in the development and the progression of steatohepatitis[82,83] as well as in fibrosis[83].
Occasional polymorphonuclear leukocytes may also occur as a part of lobular inflammation. When intense and encircling hepatocytes (i.e., satellitosis), one should consider alcoholic hepatitis (Figure 1H). The intensity and distribution of the inflammation varies within the lobule. In some cases, the intense inflammation in zone 3 may be confused with a portal area with the duct obscured by inflammation. This may be particularly true in the cases when an artery branch is readily appreciated in zone 3[84].
Portal inflammation in NAFLD/NASH can be seen in 4 situations in increased amounts. In most cases, however, it is usually milder than lobular inflammation, and mononuclear cells are typically predominant[85]. Increased portal inflammation in active NASH has been associated with increased steatosis, ballooning and fibrosis in a series of 728 adult and 205 pediatric biopsies[86]. Additionally, portal inflammation was noted to predominate along with portal fibrosis in a study of 100 pediatric NAFLD biopsies[87]. When portal inflammation is unusually prevalent, or when lymphoid aggregates occur in adult NAFLD or NASH, one should consider the possibility of a concurrent liver disease such as viral hepatitis, autoimmune liver disease, as examples[36,88]. Liver biopsy data has shown that pathologists are capable of diagnosing NASH concurrently with another serologically positive liver disease, in particular, HCV, but the criteria may differ. This concept was shown by 3 separate studies; 2 retrospective reviews of large biopsy series[36,38] and a prospective study[89]. One group emphasized the necessity of stricter histologic criteria when evaluating NASH with other diseases by focusing on the characteristic zone 3 perisinusoidal fibrosis of the former that does not occur in the latter[36]. The fourth consideration is increased portal inflammation compared to lobular in adult patients following otherwise effective intervention[29]. Finally, a different type of portal inflammation, i.e., polymorphonuclear leukocytes accompanying periportal ductular reaction may be indicative of ALD with pancreatitis or other forms of biliary obstruction.
Studies have demonstrated expansion of the periportal progenitor cell compartment in NASH. Hepatic progenitor cells (HPC) reside within the canal of Hering, along the limiting plate. They are rarely visualized by light microscopy unless activated. HPC are characterized by high N:C, round to spindled cytoplasm, ovoid nuclei and positivity for keratin 7 and 19; these characteristics are altered with progressive stages of development towards hepatocellular or biliary epithelium. In certain circumstances of liver injury and repair, stem cell markers, Hedgehog pathway markers and others are also reported in activated HPC[90]. Roskams et al[91] demonstrated increased number of progenitor cells in patients with NASH and ALD; the study further showed correlation between numbers of hepatic progenitor cells and fibrosis stage. In a multi-center study of subjects before and after various forms of treatment, the investigators demonstrated expansion of progenitor cell component, correlation between ductular reaction, steatosis, amount of portal inflammation, and NASH activity grade[19]. The group went on to demonstrate that the ductular reaction correlated with p21 positive replicative arrest in hepatocytes which was also associated with NASH activity and with insulin resistance. This area of epithelial-mesenchymal communication is one of ongoing interest in NASH.
Apoptotic hepatocytes are common both in NASH and ALD. Investigators have found that increased apoptosis is associated with disease severity[92,93], as well as fibrosis in NASH[92].
Isolated arteries observed in zone 3 correlated with advanced fibrosis in NASH[84]. Care must be taken to not confuse this region for a portal tract when there is marked inflammation.
Iron deposition, typically mild, can be noted as punctate granules within reticuloendothelial lining cells and as granules or blush within hepatocytes. It has been reported in 15%-55% of cases[94]. Reticuloendothelial iron deposition was associated with steatosis, ballooning, portal inflammation, and fibrosis in a study of 849 patient biopsies from the NASH CRN[95,96]. The relationships of iron deposition, hepcidin, iron regulatory genetics, advanced fibrosis and insulin resistance in fatty liver disease are complex and under intense investigation[96-99].
The typical pattern of fibrosis in adult NASH is initially located in zone 3 in the perisinusoidal spaces in a pattern that is described as pericellular. When delicate, it is best appreciated with Masson trichrome or other collagen stains (Figure 1I). As the disease progresses, the fibrosis becomes denser in zone 3 perisinusoidal spaces and, with further progression, portal and periportal fibrosis can be appreciated. At that point, ductular reaction is often present. In time, central-central, central-portal, or portal-portal bridging, architectural remodeling and finally cirrhosis may occur (Figure 1J). In the advanced stages of fibrosis and remodeled architecture, perisinusoidal fibrosis may no longer be present. Cartoon depiction of progression may be seen in texts[100].
GRADING AND STAGING THE LESIONS OF NAFLD/NASH
In 1999, a semi-quantitative grading and staging system to describe and unify the approach of pathologists to the histopathologic lesions of NASH and fibrosis along with architectural alterations, was proposed by Brunt et al[101]. The system was developed from evaluation of 51 liver biopsies of NASH, and followed the broad method recently developed for chronic hepatitis of separating activity (grade) from fibrosis (stage), with the recognition that NASH was not a portal-based process[102]. A semi-quantitative activity grade was assigned by a combination of parameters including steatosis, lobular and portal inflammation, and hepatocyte ballooning (Table 1). Fibrosis staging was based on fibrosis patterns of adult NASH, and reflects the progression of fibrosis as well as subsequent architectural remodeling. Figures 1I and J illustrate Stages 1 and 3. The details of staging system can be seen in Table 2.
Table 1.
Brunt grading system
| Grade | Steatosis | Ballooning | Inflammation |
| Mild (1) | 1-2 (< 66%) | Minimal | L: 1-2 P: 0-1 |
| Moderate (2) | 2-3 | Present-zone 3 | L: 2 P: 1-2 |
| Severe (3) | 2-3 | Marked-zone 3 | L: 3 P: 1-2 |
Reproduced with permission[101]. Steatosis: grade 1: < 33%; grade 2: > 33%-66%; grade 3: > 66%. Lobular inflammation: grade 1: < 2 foci per 200 × field; grade 2: 2-4 foci per 200 × field; grade 3: > 4 foci per 200 × field. Portal inflammation: grade 0: None; grade 1: Mild; grade 2: Moderate; grade 3: Severe. Ballooning: grade 1: Rare; grade 2: Prominent ballooning. L: Lobular/acinar inflammation; P: Portal inflammation.
Table 2.
Brunt staging system
| Stage | Zone 3 PSF, focal or extensive | Portal, periportal | Bridging | Cirrhosis |
| 1 | + | 0 | 0 | 0 |
| 2 | + | + | 0 | 0 |
| 3 | +/- | +/- | + | 0 |
| 4 | +/- | +/- | +/- | + |
Reproduced with permission[101]. PSF: Perisinusoidal fibrosis.
In 2002 the Brunt grading and staging was revised by NASH CRN for use as a feature-based system in clinical trials. The system was published in 2005, and has come to be known as “NAFLD Activity Score (NAS)”[65]. The NASH CRN Scoring system includes the entire spectrum of lesions that can be seen in the full range of NAFLD and NASH, including pediatric liver disease (Table 3). The disease activity score represents the unweighted sum of scores for steatosis, hepatocyte ballooning, and lobular inflammation. The fibrosis stage is an expansion of the Brunt scoring, with additional subdivisions to stage 1 (1a-mild perisinusoidal fibrosis, 1b-moderate perisinusoidal fibrosis, and 1c-portal fibrosis only, as occurs in pediatric NAFLD).
Table 3.
Nonalcoholic steatohepatitis clinical research network nonalcoholic fatty liver disease scoring system
| Steatosis grade | Lobular inflammation | Liver cell ballooning |
| 0: < 5% | 0: No foci | 0: None |
| 1: 5%-33% | 1: < 2 foci per 200 × field | 1: Few ballooned hepatocytes |
| 2: 34%-66% | 2: 2-4 foci per 200 × field | 2: Many ballooned hepatocytes |
| 3: > 66% | 3: > 4 foci per 200 × field |
Reproduced with permission[65]. Nonalcoholic fatty liver disease activity score (NAS): Steatosis + inflammation + ballooning. Fibrosis, 0: None; 1: Perisinusoidal or periportal; 1A: Mild, zone 3 perisinusoidal; 1B: Moderate, zone 3 perisinusoidal; 1C: Portal, periportal; 2: Perisinusoidal and portal/periportal; 3: Bridging fibrosis; 4: Cirrhosis.
Alkhouri et al[103] recently published a calculated pediatric NAFLD histological score (PNHS), using the histologic parameters in NAS. The PNHS consists of weighted sum of steatosis, hepatocyte ballooning, lobular inflammation and portal inflammation. The “borderline NASH” category has been eliminated from the pediatric scoring system and high scores are associated with a diagnosis of NASH in this patient group[103]. The reader is referred to the reference for the calculation.
Most recently, an algorithmic approach to scoring has been proposed by Bedossa et al[104] based on over 600 bariatric patient liver biopsies. The SAF (steatosis, activity, fibrosis) system is a sum of scores of steatosis, activity (hepatocyte ballooning + lobular inflammation) and fibrosis. Many details are modeled on the criteria by NASH CRN[65]. The SAF system differs from NAS in three major areas: it includes fibrosis into the final score, it excludes steatosis from the activity score and one is able to derive a diagnosis of NASH from a numeric value of SAF. It is noteworthy that the proponents of this system do not take patterns of any of the lesions or any assessments of portal inflammation into account. Further validation of this method in non-morbidly obese subjects is awaited.
In summary, grading and staging systems are useful tools in terms of providing a standard in pathology reporting, monitoring response to treatment and/or progression of disease both in patient care and clinical trials. However, the diagnosis of NAFLD depends on interpreting a variety of histologic findings and patterns and, cannot be replaced or reflected with a single number or score.
PEDIATRIC NAFLD
One of the most consistent observations of pediatric NAFLD that differed from adults was the difference in distribution of the fat, and the preferential accentuation of portal inflammation and fibrosis (Figure 2A, B). Steatosis is commonly either panacinar or distinctly periportal (zone 1)[87,105-107]. From a study that resulted in a hierarchical analysis of 100 pediatric biopsies, Schwimmer proposed two dominant subtypes of pediatric NAFLD: Type 1, the least common, but seen in Caucasian girls and with the similar zone 3 accentuation as with adult NAFLD, and Type 2, the most common, seen more often in boys and characterized by either panacinar or periportal steatosis, portal-predominant inflammation and portal-based fibrosis, and most commonly encountered in Asian, Hispanic or Native American ethnic groups. The remainder of the biopsies were “overlap” or steatosis[87]. Carter-Kent et al[108] studied a large multi-ethnic overweight biopsy population from several North American centers and found less ability to clearly separate the biopsies into discrete patterns with an overlap of the two main patterns in 82% of cases. Nobili et al[109] also noted more overlap (52.4%) than either Type 1 or 2 in a series of 84 Italian overweight subjects. The NASH CRN refers to zone 1 (periportal) pattern as “borderline, zone 1”, and zone 3 pattern as “borderline, zone 3”, and has found similar ethnic correlations to Patton et al[110]. Both patterns have been seen in blinded biopsy reviews by the Central Pathology Committee in adult biopsies, albeit in small numbers. Interestingly, to date, there is yet to be a definitive agreement amongst expert pathologists in the field for pediatric NASH histology, unless there are the very same characteristics found in adult NASH, as described above. There is also no knowledge about when or how a transition may occur from pediatric patterns to adult patterns of disease, but an initial retrospective cross-sectional review of 186 NASH CRN biopsies has shown that comparing biopsies from children during prepuberty, puberty and post puberty, there is less steatosis and portal inflammation, but increased steatohepatitis and Mallory-Denk bodies with the change in age[111]. These findings are strongly suggestive that with the changes of aging and associated hormonal alterations and shifts of insulin sensitivity, the liver is more susceptible to the injury of increased free fatty acids and lipotoxicity. Natural history studies with prospective biopsies are needed in this growing population.
Figure 2.
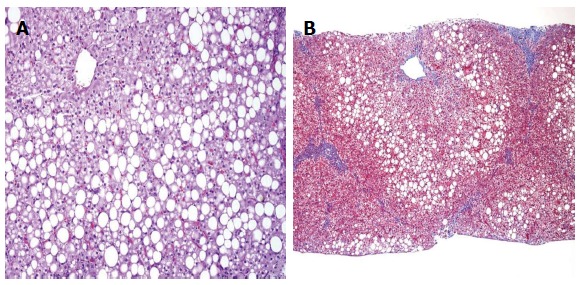
Pediatric nonalcoholic fatty liver disease. A: Periportal accentuation of steatosis with sparing of zone 3, pediatric nonalcoholic fatty liver disease (NAFLD), HE stain, 200 ×; B: Portal fibrosis without zone 3 perisinusoidal fibrosis, pediatric NAFLD, Trichrome stain, 100 ×.
DIFFERENTIATION FROM ALCOHOLIC LIVER DISEASE
Some histologic features of NASH and ALD such as steatosis, hepatocyte injury (including ballooning, necrosis and apoptosis, MDBs), and lobular inflammation are shared[112]. However, in ALD lobular inflammation may show clusters of PMNs; when present, the lesion is known as “satellitosis”. The lesion is a clue to the presence of MDB, often in apoptotic hepatocytes (Figure 1H). Steatosis is not a diagnostic requirement for ALD. An unusual form of ALD is nearly all microvesicular steatosis and is referred as “alcoholic foamy degeneration”; there is no equivalent described in NASH. Canalicular cholestasis and features of pancreatitis or biliary obstruction (ductular reaction accompanied by marked acute inflammation and edema) can occur in ALD; these lesions have not been described in NASH. Thickening and perivenular fibrosis of terminal hepatic venules and, veno-occlusive lesions are described in ALD[113]. Sclerosing hyaline necrosis (obliteration of terminal hepatic venules, hepatocyte necrosis and MDBs) is exclusive to severe alcoholic hepatitis[112,113].
Footnotes
P- Reviewers: Penkova-Radicheva MP, Sanal MG, Streba LAM S- Editor: Gou SX L- Editor: A E- Editor: Ma S
References
- 1.Wree A, Broderick L, Canbay A, Hoffman HM, Feldstein AE. From NAFLD to NASH to cirrhosis-new insights into disease mechanisms. Nat Rev Gastroenterol Hepatol. 2013;10:627–636. doi: 10.1038/nrgastro.2013.149. [DOI] [PubMed] [Google Scholar]
- 2.Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10:686–690. doi: 10.1038/nrgastro.2013.171. [DOI] [PubMed] [Google Scholar]
- 3.Rafiq N, Bai C, Fang Y, Srishord M, McCullough A, Gramlich T, Younossi ZM. Long-term follow-up of patients with nonalcoholic fatty liver. Clin Gastroenterol Hepatol. 2009;7:234–238. doi: 10.1016/j.cgh.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Koehler EM, Schouten JN, Hansen BE, van Rooij FJ, Hofman A, Stricker BH, Janssen HL. Prevalence and risk factors of non-alcoholic fatty liver disease in the elderly: results from the Rotterdam study. J Hepatol. 2012;57:1305–1311. doi: 10.1016/j.jhep.2012.07.028. [DOI] [PubMed] [Google Scholar]
- 5.Zois CD, Baltayiannis GH, Bekiari A, Goussia A, Karayiannis P, Doukas M, Demopoulos D, Mitsellou A, Vougiouklakis T, Mitsi V, et al. Steatosis and steatohepatitis in postmortem material from Northwestern Greece. World J Gastroenterol. 2010;16:3944–3949. doi: 10.3748/wjg.v16.i31.3944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weston SR, Leyden W, Murphy R, Bass NM, Bell BP, Manos MM, Terrault NA. Racial and ethnic distribution of nonalcoholic fatty liver in persons with newly diagnosed chronic liver disease. Hepatology. 2005;41:372–379. doi: 10.1002/hep.20554. [DOI] [PubMed] [Google Scholar]
- 7.Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, Grundy SM, Hobbs HH. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–1395. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 8.Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013;10:330–344. doi: 10.1038/nrgastro.2013.41. [DOI] [PubMed] [Google Scholar]
- 9.Charlton MR, Burns JM, Pedersen RA, Watt KD, Heimbach JK, Dierkhising RA. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology. 2011;141:1249–1253. doi: 10.1053/j.gastro.2011.06.061. [DOI] [PubMed] [Google Scholar]
- 10.Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol. 2013;10:656–665. doi: 10.1038/nrgastro.2013.183. [DOI] [PubMed] [Google Scholar]
- 11.Baffy G, Brunt EM, Caldwell SH. Hepatocellular carcinoma in non-alcoholic fatty liver disease: an emerging menace. J Hepatol. 2012;56:1384–1391. doi: 10.1016/j.jhep.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 12.Kleiner DE, Brunt EM. Nonalcoholic fatty liver disease: pathologic patterns and biopsy evaluation in clinical research. Semin Liver Dis. 2012;32:3–13. doi: 10.1055/s-0032-1306421. [DOI] [PubMed] [Google Scholar]
- 13.Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116:1413–1419. doi: 10.1016/s0016-5085(99)70506-8. [DOI] [PubMed] [Google Scholar]
- 14.Thaler H. Relation of steatosis to cirrhosis. Clin Gastroenterol. 1975;4:273–280. [PubMed] [Google Scholar]
- 15.Miller DJ, Ishimaru H, Klatskin G. Non-Alcoholic liver disease mimicking alcoholic hepatitis. Gastroenterology. 1979;77:A27. [Google Scholar]
- 16.Adler M, Schaffner F. Fatty liver hepatitis and cirrhosis in obese patients. Am J Med. 1979;67:811–816. doi: 10.1016/0002-9343(79)90740-x. [DOI] [PubMed] [Google Scholar]
- 17.Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55:434–438. [PubMed] [Google Scholar]
- 18.Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, Landt CL, Harrison SA. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140:124–131. doi: 10.1053/j.gastro.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 19.Richardson MM, Jonsson JR, Powell EE, Brunt EM, Neuschwander-Tetri BA, Bhathal PS, Dixon JB, Weltman MD, Tilg H, Moschen AR, et al. Progressive fibrosis in nonalcoholic steatohepatitis: association with altered regeneration and a ductular reaction. Gastroenterology. 2007;133:80–90. doi: 10.1053/j.gastro.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 20.Carpino G, Renzi A, Onori P, Gaudio E. Role of hepatic progenitor cells in nonalcoholic fatty liver disease development: cellular cross-talks and molecular networks. Int J Mol Sci. 2013;14:20112–20130. doi: 10.3390/ijms141020112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nobili V, Carpino G, Alisi A, Franchitto A, Alpini G, De Vito R, Onori P, Alvaro D, Gaudio E. Hepatic progenitor cells activation, fibrosis, and adipokines production in pediatric nonalcoholic fatty liver disease. Hepatology. 2012;56:2142–2153. doi: 10.1002/hep.25742. [DOI] [PubMed] [Google Scholar]
- 22.Radwan MM, Radwan BM, Nandipati KC, Hunter WJ, Agrawal DK. Immunological and molecular basis of nonalcoholic steatohepatitis and nonalcoholic fatty liver disease. Expert Rev Clin Immunol. 2013;9:727–738. doi: 10.1586/1744666X.2013.816484. [DOI] [PubMed] [Google Scholar]
- 23.Jou J, Choi SS, Diehl AM. Mechanisms of disease progression in nonalcoholic fatty liver disease. Semin Liver Dis. 2008;28:370–379. doi: 10.1055/s-0028-1091981. [DOI] [PubMed] [Google Scholar]
- 24.Tian Y, Wong VW, Chan HL, Cheng AS. Epigenetic regulation of hepatocellular carcinoma in non-alcoholic fatty liver disease. Semin Cancer Biol. 2013;23:471–482. doi: 10.1016/j.semcancer.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 25.Anstee QM, Daly AK, Day CP. Genetics of alcoholic and nonalcoholic fatty liver disease. Semin Liver Dis. 2011;31:128–146. doi: 10.1055/s-0031-1276643. [DOI] [PubMed] [Google Scholar]
- 26.Sookoian S, Pirola CJ. The genetic epidemiology of nonalcoholic fatty liver disease: toward a personalized medicine. Clin Liver Dis. 2012;16:467–485. doi: 10.1016/j.cld.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 27.Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592–1609. doi: 10.1053/j.gastro.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 28.Ratziu V, Bellentani S, Cortez-Pinto H, Day C, Marchesini G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol. 2010;53:372–384. doi: 10.1016/j.jhep.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 29.Brunt EM. Nonalcoholic fatty liver disease: what the pathologist can tell the clinician. Dig Dis. 2012;30 Suppl 1:61–68. doi: 10.1159/000341127. [DOI] [PubMed] [Google Scholar]
- 30.Brunt EM, Neuschwander-Tetri BA, Burt A. Fatty liver disease: alcoholic and non-alcoholic. In: Burt A, Portmann B, Ferrell L, editors. MacSween’s Pathology of the Liver. 6th ed. Amsterdam: Elsevier; 2012. p. 1020. [Google Scholar]
- 31.Grandison GA, Angulo P. Can NASH be diagnosed, graded, and staged noninvasively? Clin Liver Dis. 2012;16:567–585. doi: 10.1016/j.cld.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Torres DM, Harrison SA. Noninvasive methods of assessing nonalcoholic fatty liver disease: what the clinician needs to know. Clin Gastroenterol Hepatol. 2013;11:1205–1207. doi: 10.1016/j.cgh.2013.05.040. [DOI] [PubMed] [Google Scholar]
- 33.Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology. 2003;37:1202–1219. doi: 10.1053/jhep.2003.50193. [DOI] [PubMed] [Google Scholar]
- 34.Skelly MM, James PD, Ryder SD. Findings on liver biopsy to investigate abnormal liver function tests in the absence of diagnostic serology. J Hepatol. 2001;35:195–199. doi: 10.1016/s0168-8278(01)00094-0. [DOI] [PubMed] [Google Scholar]
- 35.Gaidos JK, Hillner BE, Sanyal AJ. A decision analysis study of the value of a liver biopsy in nonalcoholic steatohepatitis. Liver Int. 2008;28:650–658. doi: 10.1111/j.1478-3231.2008.01693.x. [DOI] [PubMed] [Google Scholar]
- 36.Brunt EM, Ramrakhiani S, Cordes BG, Neuschwander-Tetri BA, Janney CG, Bacon BR, Di Bisceglie AM. Concurrence of histologic features of steatohepatitis with other forms of chronic liver disease. Mod Pathol. 2003;16:49–56. doi: 10.1097/01.MP.0000042420.21088.C7. [DOI] [PubMed] [Google Scholar]
- 37.Ong JP, Younossi ZM, Speer C, Olano A, Gramlich T, Boparai N. Chronic hepatitis C and superimposed nonalcoholic fatty liver disease. Liver. 2001;21:266–271. doi: 10.1034/j.1600-0676.2001.021004266.x. [DOI] [PubMed] [Google Scholar]
- 38.Sanyal AJ, Contos MJ, Sterling RK, Luketic VA, Shiffman ML, Stravitz RT, Mills AS. Nonalcoholic fatty liver disease in patients with hepatitis C is associated with features of the metabolic syndrome. Am J Gastroenterol. 2003;98:2064–2071. doi: 10.1111/j.1572-0241.2003.07640.x. [DOI] [PubMed] [Google Scholar]
- 39.Farrell GC, Liddle C. Drugs and the liver updated, 2002. Semin Liver Dis. 2002;22:109–113. [PubMed] [Google Scholar]
- 40.Cotrim HP, Andrade ZA, Parana R, Portugal M, Lyra LG, Freitas LA. Nonalcoholic steatohepatitis: a toxic liver disease in industrial workers. Liver. 1999;19:299–304. doi: 10.1111/j.1478-3231.1999.tb00053.x. [DOI] [PubMed] [Google Scholar]
- 41.Cotrim HP, Carvalho F, Siqueira AC, Lordelo M, Rocha R, De Freitas LA. Nonalcoholic fatty liver and insulin resistance among petrochemical workers. JAMA. 2005;294:1618–1620. doi: 10.1001/jama.294.13.1618-b. [DOI] [PubMed] [Google Scholar]
- 42.Sorrentino P, Tarantino G, Conca P, Perrella A, Terracciano ML, Vecchione R, Gargiulo G, Gennarelli N, Lobello R. Silent non-alcoholic fatty liver disease-a clinical-histological study. J Hepatol. 2004;41:751–757. doi: 10.1016/j.jhep.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 43.Fracanzani AL, Valenti L, Bugianesi E, Andreoletti M, Colli A, Vanni E, Bertelli C, Fatta E, Bignamini D, Marchesini G, et al. Risk of severe liver disease in nonalcoholic fatty liver disease with normal aminotransferase levels: a role for insulin resistance and diabetes. Hepatology. 2008;48:792–798. doi: 10.1002/hep.22429. [DOI] [PubMed] [Google Scholar]
- 44.Mofrad P, Contos MJ, Haque M, Sargeant C, Fisher RA, Luketic VA, Sterling RK, Shiffman ML, Stravitz RT, Sanyal AJ. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology. 2003;37:1286–1292. doi: 10.1053/jhep.2003.50229. [DOI] [PubMed] [Google Scholar]
- 45.A-Kader HH, Henderson J, Vanhoesen K, Ghishan F, Bhattacharyya A. Nonalcoholic fatty liver disease in children: a single center experience. Clin Gastroenterol Hepatol. 2008;6:799–802. doi: 10.1016/j.cgh.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 46.Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118:1388–1393. doi: 10.1542/peds.2006-1212. [DOI] [PubMed] [Google Scholar]
- 47.Schwimmer JB, Pardee PE, Lavine JE, Blumkin AK, Cook S. Cardiovascular risk factors and the metabolic syndrome in pediatric nonalcoholic fatty liver disease. Circulation. 2008;118:277–283. doi: 10.1161/CIRCULATIONAHA.107.739920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Abdelmalek M, Ludwig J, Lindor KD. Two cases from the spectrum of nonalcoholic steatohepatitis. J Clin Gastroenterol. 1995;20:127–130. doi: 10.1097/00004836-199503000-00011. [DOI] [PubMed] [Google Scholar]
- 49.Caldwell SH, Lee VD, Kleiner DE, Al-Osaimi AM, Argo CK, Northup PG, Berg CL. NASH and cryptogenic cirrhosis: a histological analysis. Ann Hepatol. 2009;8:346–352. [PMC free article] [PubMed] [Google Scholar]
- 50.Struben VM, Hespenheide EE, Caldwell SH. Nonalcoholic steatohepatitis and cryptogenic cirrhosis within kindreds. Am J Med. 2000;108:9–13. doi: 10.1016/s0002-9343(99)00315-0. [DOI] [PubMed] [Google Scholar]
- 51.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 52.Neuschwander-Tetri BA, Brunt EM, Wehmeier KR, Oliver D, Bacon BR. Improved nonalcoholic steatohepatitis after 48 weeks of treatment with the PPAR-gamma ligand rosiglitazone. Hepatology. 2003;38:1008–1017. doi: 10.1053/jhep.2003.50420. [DOI] [PubMed] [Google Scholar]
- 53.Lindor KD, Kowdley KV, Heathcote EJ, Harrison ME, Jorgensen R, Angulo P, Lymp JF, Burgart L, Colin P. Ursodeoxycholic acid for treatment of nonalcoholic steatohepatitis: results of a randomized trial. Hepatology. 2004;39:770–778. doi: 10.1002/hep.20092. [DOI] [PubMed] [Google Scholar]
- 54.Adams LA, Sanderson S, Lindor KD, Angulo P. The histological course of nonalcoholic fatty liver disease: a longitudinal study of 103 patients with sequential liver biopsies. J Hepatol. 2005;42:132–138. doi: 10.1016/j.jhep.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 55.Sanyal AJ, Brunt EM, Kleiner DE, Kowdley KV, Chalasani N, Lavine JE, Ratziu V, McCullough A. Endpoints and clinical trial design for nonalcoholic steatohepatitis. Hepatology. 2011;54:344–353. doi: 10.1002/hep.24376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brunt EM, Kleiner DE, Wilson LA, Belt P, Neuschwander-Tetri BA. Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: distinct clinicopathologic meanings. Hepatology. 2011;53:810–820. doi: 10.1002/hep.24127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Piccinino F, Sagnelli E, Pasquale G, Giusti G. Complications following percutaneous liver biopsy. A multicentre retrospective study on 68,276 biopsies. J Hepatol. 1986;2:165–173. doi: 10.1016/s0168-8278(86)80075-7. [DOI] [PubMed] [Google Scholar]
- 58.Rousselet MC, Michalak S, Dupré F, Croué A, Bedossa P, Saint-André JP, Calès P. Sources of variability in histological scoring of chronic viral hepatitis. Hepatology. 2005;41:257–264. doi: 10.1002/hep.20535. [DOI] [PubMed] [Google Scholar]
- 59.Janiec DJ, Jacobson ER, Freeth A, Spaulding L, Blaszyk H. Histologic variation of grade and stage of non-alcoholic fatty liver disease in liver biopsies. Obes Surg. 2005;15:497–501. doi: 10.1381/0960892053723268. [DOI] [PubMed] [Google Scholar]
- 60.Ratziu V, Charlotte F, Heurtier A, Gombert S, Giral P, Bruckert E, Grimaldi A, Capron F, Poynard T. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128:1898–1906. doi: 10.1053/j.gastro.2005.03.084. [DOI] [PubMed] [Google Scholar]
- 61.Goldstein NS, Hastah F, Galan MV, Gordon SC. Fibrosis heterogeneity in nonalcoholic steatohepatitis and hepatitis C virus needle core biopsy specimens. Am J Clin Pathol. 2005;123:382–387. doi: 10.1309/EY72-F1EN-9XCB-1KXX. [DOI] [PubMed] [Google Scholar]
- 62.Larson SP, Bowers SP, Palekar NA, Ward JA, Pulcini JP, Harrison SA. Histopathologic variability between the right and left lobes of the liver in morbidly obese patients undergoing Roux-en-Y bypass. Clin Gastroenterol Hepatol. 2007;5:1329–1332. doi: 10.1016/j.cgh.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 63.Theise ND, Bodenheimer HC, Ferrel L. Acute and chronic viral hepatitis. In: Burt AD, Portmann B, Ferrel L, editors. MacSween’s pathology of the liver. 6th ed. Amsterdam: Elsevier; 2012. pp. 361–402. [Google Scholar]
- 64.Merriman RB, Ferrell LD, Patti MG, Weston SR, Pabst MS, Aouizerat BE, Bass NM. Correlation of paired liver biopsies in morbidly obese patients with suspected nonalcoholic fatty liver disease. Hepatology. 2006;44:874–880. doi: 10.1002/hep.21346. [DOI] [PubMed] [Google Scholar]
- 65.Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, Ferrell LD, Liu YC, Torbenson MS, Unalp-Arida A, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 66.Fukusato T, Fukushima J, Shiga J, Takahashi Y, Nakano T, Maeyama S, Masayuki U, Ohbu M, Matsumoto T, Matsumoto K, et al. Interobserver variation in the histopathological assessment of nonalcoholic steatohepatitis. Hepatol Res. 2005;33:122–127. doi: 10.1016/j.hepres.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 67.Younossi ZM, Gramlich T, Liu YC, Matteoni C, Petrelli M, Goldblum J, Rybicki L, McCullough AJ. Nonalcoholic fatty liver disease: assessment of variability in pathologic interpretations. Mod Pathol. 1998;11:560–565. [PubMed] [Google Scholar]
- 68.Aly FZ, Kleiner DE. Update on fatty liver disease and steatohepatitis. Adv Anat Pathol. 2011;18:294–300. doi: 10.1097/PAP.0b013e318220f59b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tandra S, Yeh MM, Brunt EM, Vuppalanchi R, Cummings OW, Unalp-Arida A, Wilson LA, Chalasani N. Presence and significance of microvesicular steatosis in nonalcoholic fatty liver disease. J Hepatol. 2011;55:654–659. doi: 10.1016/j.jhep.2010.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Brunt EM. Nonalcoholic steatohepatitis. Semin Liver Dis. 2004;24:3–20. doi: 10.1055/s-2004-823098. [DOI] [PubMed] [Google Scholar]
- 71.Caldwell S, Ikura Y, Dias D, Isomoto K, Yabu A, Moskaluk C, Pramoonjago P, Simmons W, Scruggs H, Rosenbaum N, et al. Hepatocellular ballooning in NASH. J Hepatol. 2010;53:719–723. doi: 10.1016/j.jhep.2010.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ku NO, Strnad P, Zhong BH, Tao GZ, Omary MB. Keratins let liver live: Mutations predispose to liver disease and crosslinking generates Mallory-Denk bodies. Hepatology. 2007;46:1639–1649. doi: 10.1002/hep.21976. [DOI] [PubMed] [Google Scholar]
- 73.Lackner C, Gogg-Kamerer M, Zatloukal K, Stumptner C, Brunt EM, Denk H. Ballooned hepatocytes in steatohepatitis: the value of keratin immunohistochemistry for diagnosis. J Hepatol. 2008;48:821–828. doi: 10.1016/j.jhep.2008.01.026. [DOI] [PubMed] [Google Scholar]
- 74.Stumptner C, Fuchsbichler A, Heid H, Zatloukal K, Denk H. Mallory body--a disease-associated type of sequestosome. Hepatology. 2002;35:1053. doi: 10.1053/jhep.2002.32674. [DOI] [PubMed] [Google Scholar]
- 75.Ludwig J, McGill DB, Lindor KD. Review: nonalcoholic steatohepatitis. J Gastroenterol Hepatol. 1997;12:398–403. doi: 10.1111/j.1440-1746.1997.tb00450.x. [DOI] [PubMed] [Google Scholar]
- 76.Guy CD, Suzuki A, Burchette JL, Brunt EM, Abdelmalek MF, Cardona D, McCall SJ, Ünalp A, Belt P, Ferrell LD, et al. Costaining for keratins 8/18 plus ubiquitin improves detection of hepatocyte injury in nonalcoholic fatty liver disease. Hum Pathol. 2012;43:790–800. doi: 10.1016/j.humpath.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Law K, Brunt EM. Nonalcoholic fatty liver disease. Clin Liver Dis. 2010;14:591–604. doi: 10.1016/j.cld.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 78.Brunt EM, Neuschwander-Tetri BA, Oliver D, Wehmeier KR, Bacon BR. Nonalcoholic steatohepatitis: histologic features and clinical correlations with 30 blinded biopsy specimens. Hum Pathol. 2004;35:1070–1082. doi: 10.1016/j.humpath.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 79.Patton HM, Yates K, Unalp-Arida A, Behling CA, Huang TT, Rosenthal P, Sanyal AJ, Schwimmer JB, Lavine JE. Association between metabolic syndrome and liver histology among children with nonalcoholic Fatty liver disease. Am J Gastroenterol. 2010;105:2093–2102. doi: 10.1038/ajg.2010.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lefkowitch JH, Haythe JH, Regent N. Kupffer cell aggregation and perivenular distribution in steatohepatitis. Mod Pathol. 2002;15:699–704. doi: 10.1097/01.MP.0000019579.30842.96. [DOI] [PubMed] [Google Scholar]
- 81.Vonghia L, Michielsen P, Francque S. Immunological mechanisms in the pathophysiology of non-alcoholic steatohepatitis. Int J Mol Sci. 2013;14:19867–19890. doi: 10.3390/ijms141019867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Maher JJ, Leon P, Ryan JC. Beyond insulin resistance: Innate immunity in nonalcoholic steatohepatitis. Hepatology. 2008;48:670–678. doi: 10.1002/hep.22399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rivera CA, Adegboyega P, van Rooijen N, Tagalicud A, Allman M, Wallace M. Toll-like receptor-4 signaling and Kupffer cells play pivotal roles in the pathogenesis of non-alcoholic steatohepatitis. J Hepatol. 2007;47:571–579. doi: 10.1016/j.jhep.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gill RM, Belt P, Wilson L, Bass NM, Ferrell LD. Centrizonal arteries and microvessels in nonalcoholic steatohepatitis. Am J Surg Pathol. 2011;35:1400–1404. doi: 10.1097/PAS.0b013e3182254283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Brunt EM. Nonalcoholic steatohepatitis: definition and pathology. Semin Liver Dis. 2001;21:3–16. doi: 10.1055/s-2001-12925. [DOI] [PubMed] [Google Scholar]
- 86.Brunt EM, Kleiner DE, Wilson LA, Unalp A, Behling CE, Lavine JE, Neuschwander-Tetri BA. Portal chronic inflammation in nonalcoholic fatty liver disease (NAFLD): a histologic marker of advanced NAFLD-Clinicopathologic correlations from the nonalcoholic steatohepatitis clinical research network. Hepatology. 2009;49:809–820. doi: 10.1002/hep.22724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Schwimmer JB, Behling C, Newbury R, Deutsch R, Nievergelt C, Schork NJ, Lavine JE. Histopathology of pediatric nonalcoholic fatty liver disease. Hepatology. 2005;42:641–649. doi: 10.1002/hep.20842. [DOI] [PubMed] [Google Scholar]
- 88.Clouston AD, Powell EE. Interaction of non-alcoholic fatty liver disease with other liver diseases. Best Pract Res Clin Gastroenterol. 2002;16:767–781. doi: 10.1053/bega.2002.0329. [DOI] [PubMed] [Google Scholar]
- 89.Bedossa P, Moucari R, Chelbi E, Asselah T, Paradis V, Vidaud M, Cazals-Hatem D, Boyer N, Valla D, Marcellin P. Evidence for a role of nonalcoholic steatohepatitis in hepatitis C: a prospective study. Hepatology. 2007;46:380–387. doi: 10.1002/hep.21711. [DOI] [PubMed] [Google Scholar]
- 90.Roskams TA, Theise ND, Balabaud C, Bhagat G, Bhathal PS, Bioulac-Sage P, Brunt EM, Crawford JM, Crosby HA, Desmet V, et al. Nomenclature of the finer branches of the biliary tree: canals, ductules, and ductular reactions in human livers. Hepatology. 2004;39:1739–1745. doi: 10.1002/hep.20130. [DOI] [PubMed] [Google Scholar]
- 91.Roskams T, Yang SQ, Koteish A, Durnez A, DeVos R, Huang X, Achten R, Verslype C, Diehl AM. Oxidative stress and oval cell accumulation in mice and humans with alcoholic and nonalcoholic fatty liver disease. Am J Pathol. 2003;163:1301–1311. doi: 10.1016/S0002-9440(10)63489-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Feldstein AE, Canbay A, Angulo P, Taniai M, Burgart LJ, Lindor KD, Gores GJ. Hepatocyte apoptosis and fas expression are prominent features of human nonalcoholic steatohepatitis. Gastroenterology. 2003;125:437. doi: 10.1016/s0016-5085(03)00907-7. [DOI] [PubMed] [Google Scholar]
- 93.Wieckowska A, Zein NN, Yerian LM, Lopez AR, McCullough AJ, Feldstein AE. In vivo assessment of liver cell apoptosis as a novel biomarker of disease severity in nonalcoholic fatty liver disease. Hepatology. 2006;44:27–33. doi: 10.1002/hep.21223. [DOI] [PubMed] [Google Scholar]
- 94.Yeh MM, Brunt EM. Pathology of nonalcoholic fatty liver disease. Am J Clin Pathol. 2007;128:837–847. doi: 10.1309/RTPM1PY6YGBL2G2R. [DOI] [PubMed] [Google Scholar]
- 95.Nelson JE, Wilson L, Brunt EM, Yeh MM, Kleiner DE, Unalp-Arida A, Kowdley KV. Relationship between the pattern of hepatic iron deposition and histological severity in nonalcoholic fatty liver disease. Hepatology. 2011;53:448–457. doi: 10.1002/hep.24038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Turlin B, Mendler MH, Moirand R, Guyader D, Guillygomarc’h A, Deugnier Y. Histologic features of the liver in insulin resistance-associated iron overload. A study of 139 patients. Am J Clin Pathol. 2001;116:263–270. doi: 10.1309/WWNE-KW2C-4KTW-PTJ5. [DOI] [PubMed] [Google Scholar]
- 97.O’Brien J, Powell LW. Non-alcoholic fatty liver disease: is iron relevant? Hepatol Int. 2011:Epub ahead of print. doi: 10.1007/s12072-011-9304-9. [DOI] [PubMed] [Google Scholar]
- 98.Kowdley KV, Belt P, Wilson LA, Yeh MM, Neuschwander-Tetri BA, Chalasani N, Sanyal AJ, Nelson JE. Serum ferritin is an independent predictor of histologic severity and advanced fibrosis in patients with nonalcoholic fatty liver disease. Hepatology. 2012;55:77–85. doi: 10.1002/hep.24706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nelson JE, Brunt EM, Kowdley KV. Lower serum hepcidin and greater parenchymal iron in nonalcoholic fatty liver disease patients with C282Y HFE mutations. Hepatology. 2012;56:1730–1740. doi: 10.1002/hep.25856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology. 2006;43:S99–S112. doi: 10.1002/hep.20973. [DOI] [PubMed] [Google Scholar]
- 101.Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999;94:2467–2474. doi: 10.1111/j.1572-0241.1999.01377.x. [DOI] [PubMed] [Google Scholar]
- 102.Brunt EM. Grading and staging the histopathological lesions of chronic hepatitis: the Knodell histology activity index and beyond. Hepatology. 2000;31:241–246. doi: 10.1002/hep.510310136. [DOI] [PubMed] [Google Scholar]
- 103.Alkhouri N, De Vito R, Alisi A, Yerian L, Lopez R, Feldstein AE, Nobili V. Development and validation of a new histological score for pediatric non-alcoholic fatty liver disease. J Hepatol. 2012;57:1312–1318. doi: 10.1016/j.jhep.2012.07.027. [DOI] [PubMed] [Google Scholar]
- 104.Bedossa P, Poitou C, Veyrie N, Bouillot JL, Basdevant A, Paradis V, Tordjman J, Clement K. Histopathological algorithm and scoring system for evaluation of liver lesions in morbidly obese patients. Hepatology. 2012;56:1751–1759. doi: 10.1002/hep.25889. [DOI] [PubMed] [Google Scholar]
- 105.Baldridge AD, Perez-Atayde AR, Graeme-Cook F, Higgins L, Lavine JE. Idiopathic steatohepatitis in childhood: a multicenter retrospective study. J Pediatr. 1995;127:700–704. doi: 10.1016/s0022-3476(95)70156-7. [DOI] [PubMed] [Google Scholar]
- 106.Rashid M, Roberts EA. Nonalcoholic steatohepatitis in children. J Pediatr Gastroenterol Nutr. 2000;30:48–53. doi: 10.1097/00005176-200001000-00017. [DOI] [PubMed] [Google Scholar]
- 107.Molleston JP, White F, Teckman J, Fitzgerald JF. Obese children with steatohepatitis can develop cirrhosis in childhood. Am J Gastroenterol. 2002;97:2460–2462. doi: 10.1111/j.1572-0241.2002.06003.x. [DOI] [PubMed] [Google Scholar]
- 108.Carter-Kent C, Yerian LM, Brunt EM, Angulo P, Kohli R, Ling SC, Xanthakos SA, Whitington PF, Charatcharoenwitthaya P, Yap J, et al. Nonalcoholic steatohepatitis in children: a multicenter clinicopathological study. Hepatology. 2009;50:1113–1120. doi: 10.1002/hep.23133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Nobili V, Marcellini M, Devito R, Ciampalini P, Piemonte F, Comparcola D, Sartorelli MR, Angulo P. NAFLD in children: a prospective clinical-pathological study and effect of lifestyle advice. Hepatology. 2006;44:458–465. doi: 10.1002/hep.21262. [DOI] [PubMed] [Google Scholar]
- 110.Patton HM, Lavine JE, Van Natta ML, Schwimmer JB, Kleiner D, Molleston J. Clinical correlates of histopathology in pediatric nonalcoholic steatohepatitis. Gastroenterology. 2008;135:1961–1971.e2. doi: 10.1053/j.gastro.2008.08.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Suzuki A, Abdelmalek MF, Schwimmer JB, Lavine JE, Scheimann AO, Unalp-Arida A, Yates KP, Sanyal AJ, Guy CD, Diehl AM. Association between puberty and features of nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2012;10:786–794. doi: 10.1016/j.cgh.2012.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Brunt EM. Alcoholic and nonalcoholic steatohepatitis. Clin Liver Dis. 2002;6:399–420, vii. doi: 10.1016/s1089-3261(02)00002-8. [DOI] [PubMed] [Google Scholar]
- 113.Yip WW, Burt AD. Alcoholic liver disease. Semin Diagn Pathol. 2006;23:149–160. doi: 10.1053/j.semdp.2006.11.002. [DOI] [PubMed] [Google Scholar]


