Abstract
Irritable bowel syndrome (IBS) is a highly prevalent functional disorder that reduces patients’ quality of life. It is a chronic disorder characterized by abdominal pain or discomfort associated with disordered defecation in the absence of identifiable structural or biochemical abnormalities. IBS imposes a significant economic burden to the healthcare system. Alteration in neurohumoral mechanisms and psychological factors, bacterial overgrowth, genetic factors, gut motility, visceral hypersensitivity, and immune system factors are currently believed to influence the pathogenesis of IBS. It is possible that there is an interaction of one or more of these etiologic factors leading to heterogeneous symptoms of IBS. IBS treatment is predicated upon the patient’s most bothersome symptoms. Despite the wide range of medications and the high prevalence of the disease, to date no completely effective remedy is available. This article reviews the literature from January 2008 to July 2013 on the subject of IBS peripherally acting pharmacological treatment. Drugs are categorized according to their administration for IBS-C, IBS-D or abdominal pain predominant IBS.
Keywords: Irritable bowel syndrome, Irritable bowel syndrome constipation, Irritable bowel syndrome-diarrhea, Constipation, Diarrhea, Irritable bowel syndrome treatment, Irritable bowel syndrome-pain
Core tip: Irritable bowel syndrome (IBS) is a highly prevalent functional disorder that reduces patients’ quality of life and imposes a significant economic burden to the healthcare system. This article extensively reviews the literature from January 2008 to July 2013 on the subject of IBS peripherally acting pharmacological treatment. Pathophysiology background and mode of action in IBS of each substance are also discussed.
INTRODUCTION
Irritable bowel syndrome (IBS) is a highly prevalent (10%-20% of the United States adult population)[1] functional disorder that reduces patients’ quality of life. IBS is defined in the Rome III criteria as a chronic disorder characterized by abdominal pain or discomfort associated with disordered defecation [either constipation (IBS-C), diarrhea (IBS-D), or mixed/ alternating symptoms of constipation and diarrhea (IBS-M)][2]. Symptoms should begin at least 6 mo before and abdominal pain or discomfort should be present at least 3 d per month for 3 mo during last 6 mo and should be associated with two or more of the following: improvement with defecation, onset associated with a change in stool frequency and/or change in stool form. Bloating and abdominal distention are also frequently reported by IBS patients reflecting sensitivity to normal amounts of intestinal gas. By definition, no disease that could explain the symptoms should be present[2].
IBS represents important costs for the healthcare system. One should look carefully for alert signs [i.e., anemia, unintentional weight loss, gastrointestinal (GI) bleeding, nausea/vomiting, family history of cancer] of a serious underlying disorder to differentiate functional symptoms from organic disorders. Thus, for younger patients who meet criteria for IBS with normal physical examination and no “red flags”, an extensive laboratory work up should not be considered[3].
It is likely that the definition of IBS represent an auspice of different conditions/disease states for which we lack specific biomarkers. Alteration in neurohumoral mechanisms and psychological factors, bacterial overgrowth, genetic factors, gut motility, visceral hypersensitivity, and immune system factors are currently believed to influence the pathogenesis of IBS[4-6]. It is possible that there is an interaction of one or more of these etiologic factors leading to heterogeneous symptoms of IBS.
Since IBS is not a single disease entity, but rather likely consists of several different disease states, IBS treatment is predicated upon the patient’s most bothersome symptoms. Specifically, our treatment strategy seems to target constipation, diarrhea, bloating or pain[7]. A wide range of medications (prokinetiks, antispasmodics, sedatives, tranquilizers, laxatives, fecal bulking agents, probiotics and antibiotics) along with life style and diet modifications have been proposed for this highly prevalent condition; however to date there is no definite effective cure for this state[7].
In the present review, we report the results of our search in PubMed, Scopus, and Google Scholar databases from January 2008 to July 2013 on the subject of IBS peripherally acting pharmacological treatment. MeSH terms “irritable bowel syndrome treatment” and “IBS treatment” were used as search terms. English-written articles only were included. Data from metanalysis and clinical studies were included. Abstracts, case reports, comments/reviews, in vitro studies, animal studies and pharmacogenetic studies were excluded from the review. The search resulted in 1018 papers after omission of duplicate articles; finally 86 papers were included after omission of non-relevant articles. Flowgram of the search is presented in Figure 1. Drugs are categorized according to their administration for IBS-C, IBS-D or abdominal pain predominant IBS.
Figure 1.
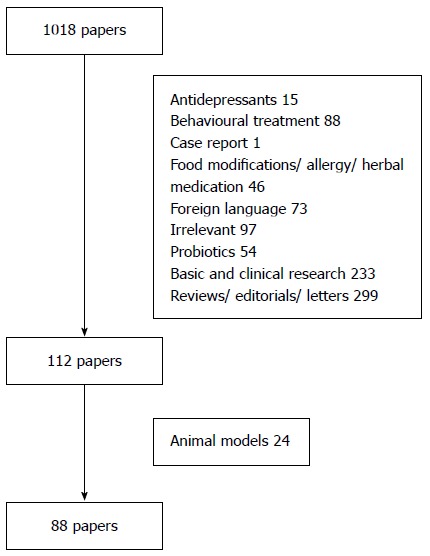
Flowgram of the selected studies for the review.
IBS-C
The evaluated studies in each category are reported in Table 1. Below is a list of available treatment methods based on the findings.
Table 1.
Pharmacological treatment irritable bowel syndrome-C studies and clinical efficacy during last 5 years
| Category/No. of studies/Ref. | No. of patients | vs Placebo | Abdominal distention/pain | SBMs | Stool consistency | Recommendation vs placebo |
| Laxatives/2 | ||||||
| Awad et al[11] 2010 | Yes | NS | NS | SS | Equal | |
| Chapman et al[12] 2013 | Yes | NS | SS | SS | Equal | |
| Linaclotide/5 | ||||||
| Johnston et al[19] 2010 | Yes | SS | SS | SS | Superior | |
| Chey et al[20] 2012 | Yes | SS | SS | - | Superior | |
| Rao et al[21] 2012 | Yes | SS | SS | - | Superior | |
| Quigley et al[22] 2013 | Yes | SS | Superior | |||
| Videlock et al[23] 2013 | Yes | SS | SS | SS | Superior | |
| 5-HT4 agonists | ||||||
| Renzapride/2 | ||||||
| Lembo et al[49] 2010 | Yes | SS | SS | SS | Superior but AE | |
| Ford et al[82] 2009 | 726 | Yes | NS | NS | NS | Equal |
| Cisapride/1 | ||||||
| Ford et al[82] 2009 | 726 | Yes | NS | NS | NS | Equal |
| Lubiprostone/4 | ||||||
| Johanson et al[57] 2008 | Yes | SS (16/32/48 μg) | SS (16/32/48 μg) | SS (16/32/48 μg) | Superior | |
| Fukudo et al[58] 2011 | Yes | SS (48 μg) | SS (48 μg) | SS (48 μg) | Superior(48 μg) | |
| Drossman et al[59] 2009 | Yes | SS (16 μg) | SS (16 μg) | SS (16 μg) | Superior | |
| Chey et al[60] 2012 | No, extention study, comparison to inclusion | SS | SS | SS | Favourable profile of effectiveness, safety, tolerability | |
| CDCA/1 | ||||||
| Rao et al[65] 2010 | Yes | - | SS | SS | Superior |
SBMs: Spontaneous bowel movements; SS: Statistically significant; NS: Not significant; 5-HT: 5-hydrodytryptamine; CDCA: Chenodeoxycholic acid.
Laxatives
Several clinical observations have reported a decrease in bowel motility and a prolonged transit time in patients with IBS-C compared with controls[8,9]. Also, some IBS-M patients report an alternation in bowel habits with extended periods with small, hard bowel movements or no bowel movement followed by periods with loose stools. Osmotic agents, stimulants, and stool softeners are all comprised in the category of laxatives. Polyethylene glycol (PEG) is the only laxative that has been evaluated in the treatment of IBS. The first study published in 2006 assessed the effects of PEG 3350 in patients with IBS-C (Rome II criteria)[10]. Mean bowel movement frequency was significantly increased; however, there was no change in mean pain level for the group with the PEG therapy. In the last 5 years 2 new studies evaluated the efficacy of PEG in IBS-C. The first study[11], a randomized, double-blind, placebo-controlled trial used fasting and postprandial (PP) perception of rectal distension as measurements. Symptoms were also recorded. Forty two patients with IBS-C (Rome II criteria) and with a pain threshold of < 32 mmHg participated. Patients received either oral PEG, 3.45 g t.i.d. orally for 30 d or placebo. PEG improved consistency of faeces. Both, PEG and placebo increased bowel movements per week (P < 0.001), and relieved symptoms without significant side-effects. However, there were not significant differences in fasting and PP rectal tone and thresholds for first sensation, gas sensation, urge to defecate, and pain between PEG and placebo. The investigators concluded that changes in rectal tone and sensation were not related to PEG 3350 and placebo effects. Patients with IBS-C gained some relief from their symptoms both with PEG and placebo. In the second study[12], following a 14-d run-in period without study medication, 139 adult patients with IBS-C were randomized to receive PEG 3350+E or placebo for 28 d. The primary endpoint was the mean number of spontaneous bowel movements per day in the last treatment week. In both groups there was an increase in mean bowel movement frequency compared to run-in. The difference between the groups in week 4 from 4.40 (PEG 3350+E) to 3.11 (placebo) was statistically significant (95%Cl: 1.17- 1.95; P < 0.0001). However, although mean severity score for abdominal discomfort/pain was significantly reduced compared with run-in with PEG 3350+E, there was no difference vs placebo. Spontaneous bowel movements (SBMs), responder rates, stool consistency, and severity of straining also showed superior improvement in the PEG 3350+E group over placebo in the fourth week. The authors concluded that PEG 3350+E was superior to placebo for relief of constipation but resulted in no improvement to abdominal discomfort/pain compared to placebo in spite of the presence of a statistical significant improvement in abdominal discomfort/pain that was observed compared with baseline.
Guanylate cyclase-c receptor agonists
Linaclotide is a guanylin peptide. Guanylin peptides are a family of peptides with similar structure to the heat-stable enterotoxin produced by Escherichia coli and other enteric bacteria that cause secretory diarrhea. They have a conformation to bind with guanylate cyclase-c (GC-C) receptors. Binding of GC-C receptors, which are abundantly expressed on enterocytes lining the intestine, stimulates production of cyclic guanosine monophosphate[13]. This leads to a cascade of intracellular events resulting in the activation of the cystic fibrosis transmembrane conductance regulator (CFTR) and the subsequent transepithelial chloride (Cl-) and potassium (K-) ion efflux from enterocytes, with secondary passive water secretion into the intestinal lumen[14]. Linaclotide is minimally absorbed and therefore believed to act locally[15]. In animal models linaclotide has been shown to stimulate intestinal secretion, accelerate GI transit time and reduce visceral pain through GC-C dependent activation[13].
Clinical studies have investigated linaclotide in patients with IBS-C and chronic constipation (CC). In an earlier phase IIa study[16] 36 women with IBS-C that received a 5-d course of linaclotide 1000 mg. The result was a significantly accelerated ascending colon (P = 0.004) and total colonic transit time at 48 h (P = 0.01). Linaclotide had no effect on gastric emptying or small bowel transit time; however, it accelerated the time to first bowel movement, decreased stool consistency, and enhanced ease of stool passage. Data from CC studies have demonstrated improvement of weekly SBMs and various other constipation-related clinical parameters, including stool consistency and straining in a dose-dependent fashion. In addition, patients treated with linaclotide experienced improvements in abdominal discomfort, bloating, and constipation severity. Constipation symptoms tended to return to baseline, without evidence of a rebound, after discontinuation of linaclotide[17,18]. The overall frequency of adverse events reported with linaclotide and placebo were similar[18], with diarrhea the most common adverse event (AE) reported with linaclotide.
In the recent years 4 studies and 1 meta-analysis were published regarding linaclotide efficacy in IBS. Specifically, a phase IIb study[19] published in 2010 the efficacy, safety, and dose response of linaclotide administered at 75, 150, 300, and 600 μg once daily for 12 wk. Four hundred twenty patients with IBS-C were assessed. The study recorded changes from baseline in daily bowel habits and daily abdominal symptoms. There were also weekly global assessments. All doses of linaclotide significantly improved the frequency of SBMs and complete spontaneous bowel movements (CSBM). They also improved the severity of straining, stool consistency and abdominal pain compared with placebo. Mean changes in abdominal pain (assessed on a 5-point scale) from baseline were -0.71, -0.71, -0.90, and -0.86 for linaclotide doses of 75, 150, 300, and 600 μg, respectively, compared with -0.49 for placebo. Other abdominal symptoms and global measures of IBS-C were also improved compared with placebo. The drug presented effect within the first week that sustained during the 12 wk of treatment. Diarrhea was the only dose-dependent adverse event and was usually of mild or moderate severity. Although all linaclotide doses were associated with a statistically significant improvement compared with placebo for most end points, the higher doses of linaclotide (i.e., 300 and 600 μg) were generally more effective across most parameters. Because the 300 and 600 μg doses provided comparable efficacy and the higher dose was associated with an increase in side effects, a dosage of 300 μg per day was selected for continued evaluation in phase III trials. In 2012, 2 studies were published together. The first, a phase III trial[20] included 804 patients with IBS-C (Rome II criteria). Participants were randomized to linaclotide 290 μg orally or placebo once daily for 26 wk. The study had the rigorous end point to be a “responder” as recommended for IBS-C in the Food and Drug Administration guidelines for IBS clinical trials (May 2012); the percentage of responders was 33.7% in the linaclotide group compared with 13.9% in the placebo group (P < 0.0001). Significant differences in favor of linaclotide (P < 0.0001) were also observed for an even more rigorous end point which required that patients meet the ≥ 30 % of improvement in worst abdominal pain and both ≥ 3 CSBMs/wk and an increase of ≥ 1 CSBM/wk from baseline for a minimum of 9 out of 12 wk. The effects of linaclotide on abdominal and bowel symptoms were manifested within the first week of treatment and sustained over the entire 26-wk treatment period. The second study[21] randomized 800 patients with IBS-C to 290 μg linaclotide orally or placebo once daily, for 12 wk. This was followed by a 4-wk withdrawal period after randomization. The same FDA end points that were used in the former trial were used as primary end points. In the linaclotide group 33.6% of patients compared with 21% of patients in the placebo group (P < 0.0001) [number needed to treat (NNT) = 8.0, 95 %CI: 5.4-15.5] met the FDA end points. A statistically significant percentage of patients treated with linaclotide vs placebo met the rest of end points (primary and secondary, P < 0.05 and P < 0.001 respectively). During the withdrawal period, after randomization, patients remained improved as long as they were receiving linaclotide whereas those that were re-randomized to placebo presented relapse of symptoms. Symptoms did not become worse relative to baseline. In both studies AEs were generally comparable between linaclotide and placebo groups, with the exception of diarrhea, which occurred more commonly with linaclotide than with placebo, and was mostly mild or moderate in severity. Recently further analysis on the data of these 2 trials was performed[22]. Overall, 803 and 805 patients were randomized. A significantly greater proportion of patients in the linaclotide group vs placebo patients presented improvement in abdominal pain/discomfort during the 12 wk treatment period. Similarly, significantly more linaclotide-treated patients compared to placebo-treated patients were responders for ≥ 13 wk (abdominal pain/discomfort: 53.6% vs 36.0%; IBS degree-of-relief: 37.2% vs 16.9%; P < 0.0001). The proportion of sustained responders was also significantly greater with linaclotide vs placebo in both trials (P < 0.001). In these trials, treatment-emergent AEs were reported by more than half of those receiving linaclotide, with the most noteworthy being a greater incidence of diarrhea in one of five subjects. These observations are obviously related to the secretagogue mechanism of the drug.
Finally a meta-analysis to determine the efficacy of linaclotide, compared with placebo, for patients with IBS-C or CC was published in 2013[23]. The search identified seven trials of linaclotide in patients with IBS-C or CC with six finally included in the analysis. The relative risk (RR) for the response to treatment with 290 mg linaclotide, compared with placebo, was 1.95 (95%CI: 1.3-2.9), and the NNT was 7 (95%CI: 5-11). Linaclotide also improved the stool form and reduced abdominal pain, bloating, and overall symptom severity in patients with IBS-C or CC.
Therefore, linaclotide has the potential to offer relief for the multiple symptoms from which patients with IBS-C suffer.
Serotonin receptor modulators
Serotonin (5-hydrodytryptamine; 5-HT) is predominantly (90%-95% of the body’s 5-HT) produced in the enterochromaffin (EC) cells in the intestinal mucosa, and also by a subpopulation of enteric neurons[24]. Acting as a signaling molecule through the intrinsic and extrinsic afferent nervous system of the GI tract, 5-HT plays an important role in various aspects of GI sensory, secretory, absorptive, and motility function[24]. Abnormal levels have been shown in individuals with IBS. Several studies describe increased serotonergic activity in association with IBS-D[25-28]. Similarly, a decrease in serotonergic activity has been observed in IBS-C[26,27]. Pharmaceutical agents acting on 5-HT receptors have, therefore, evolved to ameliorate the smooth muscle spasm, abdominal pain, and change in bowel habit that IBS patients experience. Of the identified serotonin-receptor subtypes, the 5-HT1p, 5-HT3, 5-HT4, and 5-HT7 receptors seem to play an important role in GI tract functioning[29]. Intraluminal distension of the intestine (translated to abdominal pain in IBS patients) stimulates 5-HT release from EC cells and activates 5-HT3 receptors of primary afferent neurons. 5-HT3 receptors activation results in the release of various neurotransmitters, such as acetylcholine. This induces colonic transit acceleration and abnormal water transport, which in turn leads to defecation abnormalities. Receptor antagonists of 5-HT3 have been reported to slow small bowel and colonic transit, decrease intestinal secretion and colonic tone[29]. Of great relevance to IBS-C and CC are the 5-HT4 receptors. In the gastrointestinal tract, 5-HT4 receptors are located on enteric neurons and smooth muscle cells, and their stimulation leads to acetylcholine release causing prokinetic effects. Based on biochemical structure, 5-HT4 agonists can be broadly categorized as benzamides (metoclopramide, cisapride, renzapride, mosapride, clebopride, and ATI-7505), carbazimidamides (tegaserod), benzofurancarboxamides (prucalopride), and other agonists such as velusetrag[15].
5-HT4 agonists
Tegaserod is a selective 5-HT4 receptor partial agonist with promotility effects in the small and large intestine[30-32] and modulation of visceral sensation[33,34]. The efficacy and tolerability of tegaserod in the treatment of women with IBS-C was initially reported in 2 multicenter, double-blind, placebo-controlled trials. More than 2000 patients from the Western hemisphere were involved[35,36]. These clinical trials consistently reported the superiority of tegaserod over placebo in improving IBS symptoms (abdominal pain, stool frequency, stool consistency, straining, and bloating). Later, other trials have confirmed the safety and tolerability of tegaserod[37-40]. Side effects included headache, abdominal pain and diarrhea. Although there were no reports of ischemic colitis in the clinical trials, 26 events of possible colonic ischemia were identified during postmarketing surveillance. This was translated to an estimated incidence of 7 cases of colonic ischemia per 100000 patient-years of tegaserod use[41]. Cardiovascular and cerebrovascular events in the group receiving tegaserod were also reported later[42] in a pooled analysis[13] cardiovascular ischemic events in 11614 patients receiving tegaserod compared with 1 out of 7031 patients in the placebo group (0.1% vs 0.01% respectively, P = 0.02)]. A pathogenetic mechanism that was proposed was that tegaserod may induce platelet aggregation through 5-HT4 receptors located on platelets[43]. Later retrospective studies found no relationship between tegaserod and cardiovascular events; however the drug was definitely withdrawn from the market in 2009.
Mosapride has stimulatory effects on gastric and colonic motility[44]. Unlike cisapride, mosapride does not bind to K1 channels or D2 dopaminergic receptors. Mosapride was primarily developed for upper GI tract conditions, such as functional dyspepsia, gastroesophageal reflux disease, and nausea and vomiting[15]. Data from animal models show that mosapride accelerates colonic transit time[45], augments motility in the proximal and distal colon in a dose-dependent manner[45] and has a stimulatory effect on the defecatory reflex[46,47]. In humans a study showed that mosapride changes rectosigmoid motility and perception in patients with IBS[48].
In 2010, the efficacy and safety of renzapride were assessed in a study of 1798 women with IBS-C. Patients were randomized to a 4 mg daily dosage of renzapride, 2 mg b.i.d. or placebo for 12 wk[49]. The primary end point was global relief of IBS symptoms. A subset of patients (n = 971) were enrolled in a 12-mo, open-label study of oral intake of renzapride 4 mg daily. Relief of overall IBS symptoms was achieved at (mean ± SD) 0.55 ± 0.04, 0.60 ± 0.04 and 0.44 ± 0.04 in the renzapride 4 mg daily, 2 mg b.i.d. and placebo groups (P = 0.027 and P = 0.004 respectively). Stool consistency and frequency were statistically significantly improved in the renzapride group, as well as bloating and abdominal distension. Three episodes of ischemic colitis were reported. The authors concluded that due to the limited benefit of renzapride over placebo and the reported cases of ischemic colitis, no further study with renzapride as possible treatment of IBS-C should be conducted.
Lubiprostone (chloride channel stimulators)
Lubiprostone is a bicyclic fatty acid derivative of prostaglandin E1. The underlying mechanism of lubiprostone is stimulation of electrogenic chloride secretion by activating chloride channel type-2 (ClC-2)[50] and CFTR[51] in the intestinal epithelial cells apical membrane. Primary functions of ClC-2 channels include maintenance of the membrane potential of the cell, regulation of pH and cell volume, and regulation of chloride ion channel transport and fluid secretion. Dose-dependent ClC-2 activation of ClC-2 channels or CFTR chloride channels in intestinal epithelial cells produces an active secretion of chloride ions from cells into the intestinal lumen followed by a passive secretion of electrolytes and water which increases the liquidity of the luminal contents. The luminal distension increased by intestinal fluid promotes the GI tract motility which in turn increases the intestinal and colonic transit[41]. Besides this mechanism, lubiprostone enhances and stimulates contraction in colonic as well as gastric muscles through prostaglandin E receptors (EP1 or EP4)[52], suggesting the modulatory effects of lubiprostone on GI motility through the activation of prostaglandin receptors.
Previous work has demonstrated that lubiprostone accelerates small bowel and colonic transit and increases the frequency of bowel movement in healthy adults[53]; however, the thresholds for pain do not seem to be affected by lubiprostone. Multiple randomized controlled trials (RCTs) have demonstrated the efficacy of lubiprostone in idiopathic CC[54-56]. In these trials, lubiprostone was consistently found to be superior to placebo at increasing the number of weekly SBMs as well as improving stool consistency, straining, constipation severity, bloating, and treatment effectiveness. The most commonly reported side effects included nausea, headache, and diarrhea. A pooled analysis of 91 patients meeting diagnostic criteria for IBS-C from the 2 phase III constipation trials revealed significant improvements in constipation symptoms as well as abdominal symptoms due to lubiprostone as compared to placebo. This observation led to further evaluation of lubiprostone in the treatment of IBS-C[41].
The efficacy and tolerability of lubiprostone have been assessed in several RCTs. First, 195 IBS-C patients received daily doses of 16 (8 μg twice daily), 32 (16 μg b.i.d.) or 48 μg (24 μg b.i.d.) lubiprostone or placebo for 3 mo[57]. In the lubiprostone group mean abdominal discomfort/pain scores were significantly improved compared to placebo after 1 and 2 mo (P = 0.023 and P = 0.039, respectively). All 3 doses of lubiprostone were superior to placebo with regard to frequency of SBM (P = 0.0499), constipation severity (P = 0.0056), stool consistency (P < 0.0001), and straining (P = 0.0094) in each of the 3 mo of treatment. Treatment with lubiprostone showed significantly higher rates of GI AEs (P = 0.020), especially diarrhea and nausea. The 16 μg/d dose demonstrated the optimal combination of efficacy and safety and was therefore the dose selected for further study in subsequent phase III clinical trials. Another Japanese trial[58] studied adequate dosing of lubiprostone for the treatment of constipation in CC or IBS-C patients. One hundred seventy patients (128 without IBS and 42 with IBS) randomly received a placebo or 16 μg, 32 μg, or 48 μg of lubiprostone daily for two weeks. There was a dose-dependent increase in weekly average number of SBM compared to baseline in the first week (placebo: 1.5; 16 μg: 2.3, 32 μg: 3.5; and 48 μg: 6.8, per week, P < 0.0001). The 32 and 48 μg dosage treatments had a significantly higher primary efficacy endpoint than the placebo treatment (P = 0.0017, P < 0.0001, respectively). The 16 μg treatment showed no significant increase in change in SBMs during the first week over placebo. The primary endpoint was significantly better only in patients with IBS treated with 48 μg of lubiprostone than those treated with placebo (P = 0.0086).
There was a combined analysis of two phase-III RCTs of lubiprostone 8 μg twice daily vs placebo for 12 wk that reported data of 1171 patients with IBS-C [Rome II criteria][59]. Patients responded with respect to relief of IBS symptoms over the past week. Patients were characterized monthly responders (moderate relief in 4/4 wk or significant relief in 2/4 wk) or overall responders (a monthly responder in 2/3 mo of the trial). The primary efficacy endpoint was the percentage of overall responders. Significantly more patients in the lubiprostone group were considered overall responders compared with the placebo group (17.9% vs 10.1%, P = 0.001). Lubiprostone was also superior to placebo in improving individual IBS symptoms (abdominal discomfort/pain, stool consistency, straining, constipation severity), and quality of life (QOL). A similar incidence of AEs to those treated with placebo and lubiprostone was observed. Another recent study[60] evaluated the long-term safety, tolerability and patient outcomes of lubiprostone in patients with IBS-C. This was an extension study analyzing the data of 476 IBS-C patients who had completed one of two randomized phase III studies. Patients received placebo or lubiprostone orally for 36-wk (8 μg, twice daily). Those receiving lubiprostone during the initial 12-wk phase III trial experienced an increase in response from 15% to 37% and those initially receiving placebo experienced an increase in response from 8% to 31% at the conclusion of the 36-wk extension period. The overall safety profile of lubiprostone during this study was similar to that observed in the preceding phase III studies. AEs were diarrhea (11.0%), nausea (11.0%), urinary tract infection (9.0%), sinusitis (9.0%) and abdominal distention (5.8%). Diarrhea and nausea were the most common treatment-related AEs.
An evidence-based systematic review was performed by the ACG IBS Task Force that evaluated lubiprostone in the treatment of IBS-C[61] concluding that “Lubiprostone in a dose of 8mg twice daily is more effective than placebo in relieving global IBS symptoms in women with IBS-C.” Regarding men with IBS-C, the ACG task force suggested a need for further studies before a recommendation for use in this population. Lubiprostone is contraindicated in patients with mechanical bowel obstruction and should be avoided in patients with preexisting diarrhea; there have also been postmarketing reports of dyspnea (typically resolves over several hours but sometimes reoccurs with subsequent dosing)[41].
Bile acid modulators
Bile acids have been used in the treatment of patients with gallstones and cholestatic liver diseases. Longterm treatment is generally well tolerated other than the consistent side effect of diarrhea[62], which mimics the chronic loose stools observed in patients with a disrupted enterohepatic circulation from ileal disease resulting in spillage of bile acid into the colon[63]. In the setting of bile acid-related diarrhea after ileal resection or disease, high concentrations of bile acids decrease net colonic fluid and electrolyte absorption and induce secretion[64]. The mechanisms involved in promoting secretion include intracellular activation of adenylate cyclase, increased mucosal permeability, and inhibition of apical Cl-/OH- exchange[65]. Furthermore, instillation of bile acids directly into the colon increases intracolonic pressure and motility index[66].
Chenodeoxycholic acid (CDCA), a primary bile acid previously used for dissolution of gallstones, elicited diarrhea at dosages of 750 to 1000 mg/d[67]. CDCA (with hydroxyl groups in the 3α, 7α positions) promoted colonic secretion in comparison to its 3α, 7β epimer, ursodeoxycholic acid[68]. Previous studies in healthy volunteers[69] and in patients with gallstones who had CC receiving CDCA demonstrated a significant increase in the frequency of bowel movements and loosening of stools[70]. CDCA also accelerated colonic transit time resulting in ease of stool passage, and sense of complete evacuation[69].
Recently a double-blind placebo-controlled study[65] evaluated pharmacodynamics (colonic transit, bowel function) and pharmacogenetics of CDCA in 36 female patients with IBS-C. Participants were randomized to treatment with delayed-release oral formulations of placebo, 500 mg CDCA, or 1000 mg CDCA for 4 d. Colonic transit and ascending colon emptying were significantly accelerated in the CDCA group compared to the placebo group (P = 0.005 and P = 0.028, respectively). Looser stool consistency (P = 0.003), increased stool frequency (P = 0.018), and greater ease of passage (P = 0.024) were noted with CDCA compared with placebo. The investigators also found a correlation between fasting serum 7 alpha-hydroxy-4-cholesten-3-one (7aC4), a biomarker of bile acid synthesis, and colonic transit time in the placebo group: subjects with an increased 7aC4 showed a faster overall colonic transit time. In the CDC group, 7aC4 showed a modest influence on colonic transit at 24 h (P = 0.055) and 48 h (P = 0.019).
IBS-D
The evaluated studies in each category are reported in Table 2. Below is a list of available treatment methods based on the findings.
Table 2.
Pharmacological treatment irritable bowel syndrome-C studies and clinical efficacy during last 5 years
| Category/No. of studies/Ref. | n | vs Placebo | Abdominal distention/pain | QOL/patient satisfaction/global improvement | Stool consistency/bowel habits | Recommendation vs placebo |
| 5-HT3 antagonists | ||||||
| Alosetron, cilansetron/4 | ||||||
| Cremonini et al[79] 2012 | 705 | Yes | - | SS | - | Superior |
| Rahimi et al[80] 2008 | 4.17 | Yes | SS | SS | - | Superior |
| Metanalysis | ||||||
| Andresen et al[81] 2008 | 7487 Metanalysis | Yes or mebeverine | SS | SS | - | Superior |
| Ford et al[82] 2009 | 7216 | Yes | SS | SS | - | Superior |
| Metanalysis | ||||||
| Ramosetron/3 | ||||||
| Matsueda et al[85] 2008 | 418 | Yes | SS (5/10 μg) | SS (5/10 μg) | - | Superior |
| Matsueda et al[86] 2008 | 539 | Yes | SS (5 μg) | SS (5 μg) | SS (5 μg) | Superior |
| Lee et al[87] 2011 | 343 | Mebeverine | NS(5 μg) | NS (5 μg) | NS(5 μg) | Equal |
| 135 mg t.i.d | ||||||
| LX-1031/1 | ||||||
| Brown et al[92] 2011 | 155 | Yes | SS only the 1st week (1000 mg 4 times/d) | - | SS (1000 mg 4 times/d) | Superior |
| Crofelemer/1 | ||||||
| Angel et al[94] 2008 | 246 | Yes | SS 500 mg b.i.d | SS | SS | Superior |
| Antibiotics | ||||||
| Rifaximin/2 | ||||||
| Pimentel et al[105] 2011 | 1260 | Yes | SS | SS | SS | Superior |
| Menees et al[106] 2012 | 1803 | Yes | SS | SS | - | Superior |
| Metanalysis | ||||||
| 5ASA compounds, mesalazine/3 | ||||||
| Corinaldesi et al[108] 2009 | 20 | Yes | NS | SS | NS | Equal |
| Andrews et al[109] 2011 | 12 | No | SS | SS | - | - |
| Comparison to baseline | ||||||
| Tuteja et al[110] 2012 | 17 | Yes | NS | NS | NS | Equal |
QOL: Quality of life; ASA: Aminosalicylic acid; SS: Statistically significant; NS: Not significant.
Antidiarrheals
As mentioned above alterations in bowel habits in IBS are in part a result of altered GI motility. Accelerated small bowel and colon transit times as well as exaggerated motility patterns have been demonstrated in those with IBS-D compared with controls[8,9]. Consequently, antidiarrheals remain among the more commonly used gut-acting agents used in the treatment of patients with IBS-D.
Among the class of antidiarrheals, loperamide is the only substance that has been evaluated in RCTs for the treatment of IBS. In total, four studies have been published[71-74] showing an improvement in the number of bowel movements and stool consistency compared to placebo in IBS-D patients; however results were rather disappointing regarding pain. The ACG Task Force recently performed a systematic review of antidiarrheals in the treatment of IBS and concluded that “The antidiarrheal agent loperamide is not more effective than placebo at reducing abdominal pain or global symptoms of IBS, but is an effective agent for treatment of diarrhea, improving stool frequency and stool consistency. RCTs with other antidiarrheal agents have not been performed. Safety and tolerability data on loperamide are lacking”[61].
5-HT3 antagonist (alosetron, cilansetron, ramosetron)
As already mentioned receptor antagonists of 5-HT3 have been reported to slow colonic and small bowel transit and decrease intestinal secretion and colonic tone[29]. Early, rigorous, large clinical trials with alosetron 1 mg b.i.d. have all demonstrated the efficacy of alosetron in the global and individual symptoms of IBS-D in women. Alosetron decreases urgency, reduces stool frequency, and increases stool consistency. Improvement is seen within 1 wk of therapy, which persists throughout the treatment period[75,76]. The use of alosetron also demonstrated improvement in 3 QOL domains (including food/diet, social functioning, and role-physical on the validated generic QOL instrument, the SF-36 75)[77] and in the global IBS symptoms[78]. Recently a total of 705 women (severe IBS-D, Rome II criteria) were randomized to alosetron 0.5 mg q.d., 1 mg q.d., 1 mg b.i.d., or placebo for 12 wk[79]. IBSQOL, treatment satisfaction, daily activities, and lost workplace productivity were evaluated. The authors concluded that in women with severe IBS-D, alosetron treatment, including 0.5 mg q.d., resulted in statistically significant and clinically relevant improvements in health-related QOL, restriction of daily activities and treatment satisfaction over placebo.
During the last 5 years 3 metanalyses have been published on this subject. The first[80] included 8 multicenter, randomized, placebo-controlled, 12-wk clinical trials with 4170 patients with IBS randomized to receive either alosetron or placebo. Alosetron was significantly more effective in global improvement in symptoms than placebo (RR = 1.60; 95%CI: 1.44-1.76; P < 0.001), in adequate relief of IBS pain and discomfort (RR = 1.31; 95%CI: 1.20-1.43; P < 0.001). In the alosetron group, there were 4 cases of ischemic colitis (0.16%) and 2 cases of serious complications of constipation (0.08%). The second[81] trial collected data from 14 RCTs [alosetron (n = 3024) or cilansetron (n = 1116) vs placebo (n = 3043) or mebeverine (n = 304)]. 5-HT3 antagonists were more effective than mebeverine and placebo in achieving global IBS symptoms improvement (pooled RR = 1.60; 95%CI: 1.49-1.72), abdominal pain and discomfort relief (pooled RR = 1.30; 95%CI: 1.22-1.39). Superiority of both agents was demonstrated in patients of either sex. Nine patients (0.2%) in the 5-HT3 antagonists group were reported with possible ischemic colitis vs none in control groups. The third meta-analysis[82] pooled the data from eight clinical trials of alosetron and three clinical trials of cilansetron. This analysis, which included a total of 7216 patients with IBS, found 5-HT3 antagonists more effective than placebo in treating IBS-D. The RR of IBS symptoms persisting with 5-HT3 antagonists was 0.78 (95%CI: 0.71-0.86) compared to placebo.
Severe complications of constipation and ischemic colitis have emerged as significant side effects with alosetron use and this led to the drug’s withdrawal from the United States marketplace in 2000. An expert panel reviewed the postmarketing data[83] reporting similar incidence rates for ischemic colitis and constipation (0.95 and 0.36 cases per 1000 patient-years, respectively) to rates during the postmarketing cycle before alosetron withdrawal. No mesenteric ischemia, surgeries, transfusions, or deaths occurred in patients with ischemic colitis and no cases of contipation were associated with toxic megacolon, perforation, surgeries, transfusions, or deaths. AEs were typically of short duration and all improved on prompt withdrawal of alosetron.
Ramosetron, is also a selective serotonin 5-HT3-receptor antagonist that possesses a specific three dimensional chemical conformation able to bind long lastingly to 5-HT3 receptors. Traditionally it has been used in oncology as a medication for hyperemesis due to chemotherapy[84]. The first double-blind, RCT[85] randomized 418 IBS-D patients to ramosetron 5 μg, 10 μg or placebo. Significantly higher rates of patients treated with both doses of ramosetron reported relief of IBS symptoms compared to placebo; the outcome measure was “global assessment of relief of IBS symptoms” in a monthly basis with similar benefits in men and women. The second study was also double-blind RCT. Five hundred thirty nine IBS-D patients received 5 μg ramosetron or placebo once daily. Ramosetron was shown effective for discomfort, altered bowel habits (44% vs 24%, for ramosetron vs placebo respectively, P = 0.001) and abdominal pain (46% vs 33%, for ramosetron vs placebo respectively, P = 0.005), without any serious AEs[86]. Overall 47% of individuals treated with ramosetron reported a positive response to treatment compared to 27% of placebo-treated patients (P = 0.001). Ramosetron was compared to mebeverine in another study with male IBS-D patients[87]. Patients (n = 343) were randomized to receive 5 μg ramosetron once daily or 135 mg mebeverine t.i.d for four weeks. Adequate relief of IBS symptoms at the last week of treatment was the primary end point and this was measured as the proportion of patients reporting relief in an intention to treat analysis. Both in the ramosetron and mebeverine groups, responder rates for global IBS symptoms, altered bowel habits and abdominal pain significantly increased during treatment. Although abdominal pain/discomfort and urgency (severity scores), the stool form score, and the stool frequency in both treatment arms significantly improved compared to baselines, statistical significance was not reached. Furthermore, in the comparison between ramosetron and mebeverine groups, the responder rates were similar (37% vs 38% on ITT analysis) as well as AEs. Events of severe constipation or ischemic colitis were not reported. When the oral administration of 5 μg ramosetron was prolon data analysis of the postmarketing survey[88]. Further RCTs studies ged for a minimum of 28 wk (up to 52 wk) the responder rate was increased as well as the overall improvement of IBS symptoms. The rate was further increased subsequently in the to evaluate ramosetron are needed.
LX-1031
As already mentioned 5-HT is an important neurotransmitter in the GI tract released from EC cells and interneurons[24]. 5-HT is synthesized through the actions of the rate-limiting enzyme tryptophan hydroxylase (TPH), of which 2 different types, TPH1 and TPH2, are expressed by EC cells and neurons. After release of 5-HT from EC cells or neurons, it is inactivated by uptake into enterocytes or neurons through the 5-HT reuptake transporter, followed by metabolization to 5-hydroxyindole acetic acid (5-HIAA), which is excreted in the urine. Abnormalities of serotonergic signaling, including altered expression of TPH-1 and 5-HT reuptake transporter, and altered release of 5-HT, have been implicated in IBS pathogenesis[24,89]. Specifically, patients with IBS-D have increased platelet-depleted 5-HT concentrations during fasting and postprandial conditions compared with healthy volunteers and patients with IBS-C[27].
LX-1031 is an orally administrable, TPH inhibitor, with poor systemic absorption and low penetration through the blood-brain barrier that decreases serotonin synthesis[90,91]. Among healthy volunteers, LX-1031 was well tolerated and dose dependently inhibited 5-HIAA levels, supporting the potential of the drug to inhibit 5-HT synthesis in the human GI tract upon oral administration[91]. Brown et al[92] reported the results of a phase IIa study with LX-1031 in patients with non-constipating IBS. A total of 155 patients were randomized to a 4-wk treatment with placebo or 250 mg or 1000 mg LX-1031 q.d. After 1 wk, a significantly greater number of patients obtained adequate relief of IBS symptoms with the high dose of LX-1031 compared with placebo (48% vs 22%, P = 0.02). In weeks 2-4, the response to LX-1031 was higher compared with placebo, but no statistical significance was reached. As a result, the therapeutic gain (adequate relief) decreased from 25% to 10%. Stool consistency measured with the Bristol Stool Form Scale improved significantly with the high dose compared with placebo during weeks 1, 2, and 4. In a subset of patients, urinary 5-HIAA was measured as a marker of 5-HT synthesis before and after 4 wk of treatment with LX-1031. Overall, the high dosage decreased 5-HIAA excretion by approximately 25%. In this subgroup, a significant correlation was found between the percent decrease in urinary 5-HIAA excretion and the adequate relief response at the end of the treatment, indicating that decreased 5-HT synthesis is the mechanism underlying the symptomatic benefit. This is supported further by a post hoc analysis that showed a significantly higher symptomatic benefit in those who achieved a > 15% decrease in urinary 5-HIAA excretion during treatment. LX-1031 was well tolerated and no safety issues were observed; however, more studies are needed to establish fully the safety and tolerance profile of this drug[89].
Crofelemer
Crofelemer is a proanthocyanidin oligomer. Crofelemer acts through an antisecretory mechanism by reducing excess intestinal chloride ion secretion. It exerts an antisecretory action on two distinct chloride channel targets on the luminal membrane of intestinal epithelial cells, namely the CFTR and calcium-activated chloride channel[93]. The drug is being investigated for the treatment of acute infectious diarrhea, chronic diarrhea associated with human immunodeficiency virus/acquired immunodeficiency syndrome, and IBS-D.
A randomized, double-blind, placebo-controlled, phase IIa 12-wk treatment study evaluated crofelemer for IBS-D. A total of 246 patients with IBS-D received either placebo or crofelemer at dosages of 125, 250, or 500 mg twice daily[94]. The primary end point was improvement in stool consistency. The study found that none of the doses of crofelemer improve d stool consistency, stool frequency, or urgency, or provided adequate relief of IBS symptoms. However, the 500-mg twice-daily dosage of crofelemer significantly increased pain- and discomfort-free days especially in women with IBS-D. Large clinical trials are necessary to evaluate the effectiveness and safety of crofelemer.
Antibiotics
The potential utility of antibiotics in IBS treatment has been supported by a growing body of evidence demonstrating the important role of bacteria in IBS pathogenesis. It has been proposed that small intestinal bacterial overgrowth (SIBO) might explain the physiological hallmarks of altered gut motility, visceral hypersensitivity, abnormal brain-gut interaction and immune activation seen in IBS[95]. This is supported by multiple lines of evidence; first, gas analysis is abnormal in 10%-84% of IBS patients undergoing lactulose breath testing[96,97]; second, the distribution of inflammatory mediators and⁄or inflammatory cells have been shown to be disturbed in some patients with IBS[98]. It is thought that SIBO may contribute to many of the clinical manifestations of IBS through bacterial fermentation and stimulation of a gut immune response, characterized by release of inflammatory mediators, such as interleukins and tumour necrosis factor-α, which may affect motility, secretion and sensation[95,99]. Postinfectious IBS, which occurs in 4%-31% of individuals assessed up to 12 mo after an episode of acute gastroenteritis[100], also supports an aetiological role of bacteria in IBS.
In earlier studies[97,101] the systemic antibiotic neomycin has been evaluated and was found to improve global symptoms compared with placebo. The non-absorbed (< 0.4%), oral antibiotic rifaximin is the most thoroughly studied antibiotic for the treatment of IBS. Rifaximin appears to be well suited for the treatment of IBS because of its broad-spectrum bactericidal activity in vitro, its efficacy for SIBO in vivo, its favorable tolerability profile and its lack of association with clinically relevant resistance or Clostridium difficile colitis[99,102]. Rifaximin has demonstrated its efficacy in RCTs evaluating IBS patients[103,104]. IBS trials utilized high doses of rifaximin: 400 mg three times daily for 10 d[104], 400 mg twice daily for 10 d[103], and 550 mg twice daily for 14 d[105]. Rifaximin, at these high doses, demonstrated statistically significant improvement in symptoms whereas patients reported at significantly greater rate global improvement in IBS symptoms and/or bloating compared to patients treated with placebo. Pimentel et al[105] evaluated rifaximin as treatment for IBS in TARGET 1 and TARGET 2 studies. These were phase III, double-blind, placebo-controlled trials, identically designed. Patients who suffered from IBS without constipation were included in the studies and were randomized to receive for two weeks 550 mg rifaximin or placebo, three times daily. Patients were then followed for an additional period of 10 wk. The study measured (weekly assessments) the proportion of patients that responded reporting adequate relief of global IBS symptoms and IBS-related bloating. A significantly higher rate of patients in the rifaximin group reported adequate relief of global IBS symptoms and bloating during the first 4 wk after treatment compared to patients in the placebo group (40.7% vs 31.7%, P < 0.001 and 40.2% vs 30.3%, P < 0.001, respectively). AEs were similar between the two groups. A metanalysis[106] that included 5 trials reporting data from 1803 patients was published in 2012. Rifaximin was found to be more efficacious than placebo for global IBS symptom improvement (OR = 1.57; therapeutic gain = 9.8%; NNT = 10.2). Rifaximin was significantly more likely to improve bloating than placebo (OR = 1.55; therapeutic gain = 9.9 %; NNT = 10.1). The authors noticed that studies with older patients and more females demonstrated higher response rates, which was consistent regardless of treatment group. Although therapeutic gain offered by rifaximin is modest, it was similar to that yielded by other currently available therapies for IBS.
The American Task Force systematic review[61] concludes that rifaximin has shown improvement of global IBS symptoms and bloating in trials included in their analysis. Rifaximin has mostly been offered in patients with IBS-D; therefore it seems as a reasonable option for IBS patients with bloating and patients with IBS-D. The suggested dose is 400 mg three times a day for 10-14 d; however symptoms may recur over three to nine months.
5ASA compounds
Mesalamine is an anti-inflammatory agent, effective in the treatment of inflammatory bowel disease. It has been proposed for IBS-D on the basis of treatment of the underlying chronic inflammation. Bowel infections, bacterial overgrowth syndrome, antibiotics, stress and unfavorable dietary habits can precede visceral hypersensitivity and lead to a clinical manifestation of IBS. Although there is no specific morphologic correlate of IBS, these predictors can affect the colon microbiota and the local immune system, decrease the protective properties of the bowel mucosa, impair mucus production, and may be caused by only minimal alterations on the cellular level. The detection of minor lesions is often accompanied by a decrease of proliferation and enhanced apoptosis of colonocytes[107]. Progression of the disease leads to more pronounced morphological changes of the colon mucosa epithelium: reduced frequency of serotonin-producing cells and mast cells and increased frequency of secondary cells and increasing number of cellular infiltrations by eosinophils, neutrophils, lymphocytes, plasmocytes and fibroblasts of stroma[107]. These morphological criteria are signs of inflammatory processes and activation of immune mechanisms. In this context mesalazine has been evaluated in a RCT trial in 20 IBS patients[108]. Patients received 800 mg mesalazine or placebo three times daily for eight weeks. The primary outcome measure was changes in the number of colonic immune cells on biopsies obtained at baseline and at the end of treatment. Symptom severity, changes in subsets of immune cells and inflammatory mediators were also evaluated. In the group of mesalazine the total count of immune cells and specifical the mast cells were reduced as compared with placebo (P = 0.0082 and P = 0.0014, respectively). General well-being was also improved in the group of mesalazine (P = 0.038), but did not seem to have an impact on abdominal pain (P = 0.084), bowel habits or bloating (P = 0.177). The drug was well tolerated with no serious AEs reported. In another study[109] 12 women with diarrhoea-predominant IBS received oral mesalazine (1.5 g b.i.d.) for four weeks followed by a 4-wk washout phase. Molecular profiling of stool bacterial communities and IBS symptoms were assessed before, during and after mesalazine treatment. Qualitative and quantitative effects of mesalazine on stool microbiota, mucosal proteolytic activity and IBS symptoms were assessed. Faecal bacteria decreased by 46% on mesalazine treatment (P = 0.014), but returned to baseline during washout. Eight of 12 (67%) patients responded favorably to mesalazine based on a global relief questionnaire, with significant decreases in the number of days with discomfort and increases in bowel movement satisfaction. In a recent trial[110] 17 patients who developed IBS-D after gastroenteritis were randomized to receive mesalamine 1.6 gm b.i.d. or placebo for 12 wk. Mesalamine was not associated with significant improvement in global symptoms, abdominal pain, bloating, stool urgency, frequency, or consistency (all P ≥ 0.11) or QOL (P ≥ 0.16). At this point, data from all these studies seem inconclusive. Further study of the bacteriological and anti-inflammatory properties of mesalazine in IBS is necessary.
ABDOMINAL PAIN
Antispasmodics
Exaggerated motility response of the small bowel and colon to environmental stimuli may be responsible for the symptoms, especially pain, experienced in IBS[111-113]. For this reason antispasmodics have been used for the symptoms of IBS. Antispasmodics encompass several different drug classes (smooth-muscle relaxants, antimuscarinics, anticholinergics) and unique agents (pinaverium, trimebutine). Given their mechanism of action, these agents are directed at those subgroups of IBS, with a predominant symptom of abdominal pain and stool patterns that are either mixed or more diarrheal in nature. The propensity of these agents to promote constipation makes them a less attractive option for patients with IBS-C. The anticholinergic properties of these agents restrict their usefulness in clinical practice. Common side effects that often limit these drugs usefulness in the treatment of IBS are dizziness, dry mouth, confusion (particularly in elderly patients), blurry vision, urinary retention, and constipation[41].
A systematic review and meta-analysis of antispasmodics as a class was performed by the ACG IBS Task Force[61]. The Task Force identified 22 studies suitable for inclusion in their systematic review. Most of these clinical trials are dated, with only 3 of the studies performed in the last 10 years. Studies evaluated hyoscine, hyoscyamine, otilonium, cimetropium, pinaverium, trimebutine, alverine, mebeverine, pirenzipine, prifinium, propinox, and a trimebutine/rociverine combination. The 22 trials collectively included data from 1778 patients with IBS. The pooled analysis of these studies revealed a RR of symptoms persisting with antispasmodics compared with placebo of 0.68 (95%CI: 0.57-0.81) and a NNT of 5. The pooled analysis that was performed on the 13 studies, included 1379 patients in whom AEs were reported. There was significant heterogeneity among these patients; moreover these clinical trials were collectively fraught with methodological flaws, including diagnostic criteria used, inclusion criteria used, dosing schedule used, duration of therapy studied, study end points used to assess response, and study size (only three studies enrolled more than 100 patients). The review concluded that some drugs in the antispasmodics class (cimetropium, hyoscine, pinaverium) may be an option for relief of abdominal discomfort and pain in IBS-patients. Older systematic reviews have yielded mixed results regarding the efficacy of antispasmodics for IBS[114,115].
Mebeverine is an antispasmodic that has been successfully used in the management of IBS for many years. Mebeverine is a musculotropic agent that has antispasmodic activity and regulatory effects on the bowel function[116]. During oral administration at doses of 135-270 mg t.i.d., it shows no typical anticholinergic side effects. There is no indication that the incidence of side effects caused by mebeverine is higher than that of a placebo[114]. In 2010, a metanalysis was published on the efficacy and tolerability of mebeverine in IBS in its usual dosages[117]. Eight randomized trials including 555 patients with all IBS subtypes, randomized to receive either mebeverine or placebo, met the metanalysis criteria. The pooled RR for clinical improvement of mebeverine was 1.13 (P = 0.7) and 1.33 (P = 0.12) for relief of abdominal pain. The efficacy of mebeverine 200 mg compared to mebeverine 135 mg indicated RRs of 1.12 (P = 0.168) for clinical or global improvement and 1.08 (P = 0.463) for relief of abdominal pain. Thus, mebeverine was shown to be well tolerated with no significant AEs; however, its efficacy in global improvement of IBS did not reach statistical significance. Recently the results of an exploratory RCT of mebeverine, methylcellulose, placebo and a self-management online (website) treatment method (cognitive behavior treatment) were published[118]. One hundred thirty-five patients, with IBS symptoms fulfilling Rome III criteria were randomized to over-encapsulated mebeverine, methylcellulose or placebo for six weeks and to 1 of 3 website conditions. Mean IBS SSS (symptom severity scale) decreased by 35 points from baseline to 12 wk of treatment. There was no significant difference in IBS SSS or IBS-QOL score between medication and website groups. However, IBS SSS at six weeks was lower in the No-website group than the website groups (P = 0.037). In the end of the study, the global relief of IBS symptoms was significantly improved in the website groups compared to the non-website group at 12 wk of treatment (Enablement and Subjects Global Assessment of relief P = 0.001 and P = 0.035 respectively).
Otilonium bromide (OB) has been shown to reduce the pain severity in IBS patients effectively[61]. OB is an ammonium derivative with spasmolytic activity in GI smooth muscle by inhibiting the calcium ion influx through L-type voltage operated calcium channels. OB pharmacologically has been demonstrated to inhibit central/peripheral tachykinin-2 receptor; in this way it reduces the sensory signals afferent transmission from the periphery to central nervous system[119]. Additionally, OB binds with high affinity to muscarinic receptor subtypes M1, M2, M3, M4 and M5[120,121]. M3 sub-receptor is located in human colonic crypt cells to mediate secretion coupled with calcium channels. Due to its potent muscarinic blockade of M3, OB exhibits its antisecretory properties, thus improving stool consistency[121]. Among researches on the OB efficacy on IBS patients, early studies indicated that OB is effective for abdominal pain and bloating but there was a difficulty in demonstrating efficacy over placebo[122,123]. A review based on four OB trials was eventually conducted in 2008. Various antispasmodics were studied, but OB (four trials, 435 patients, RR of persistent symptoms 0.55, 0.31 to 0.97) showed consistent evidence of efficacy over placebo[124]. Subsequently, two RCTs were published. The first multi-center phase IV double-blind study[125] randomized 356 patients with various IBS subtypes to receive OB (40 mg t.d.s.) or placebo for 15 weeks, and follow-up was extended 10 additional weeks. The effect of OB was significantly greater than placebo in the reduction of weekly frequency of episodes of abdominal pain at the end of treatment period (P = 0.03); similarly OB was superior to placebo in the reduction of abdominal bloating (P = 0.02) and in the global efficacy by patient assessment (P = 0.047). However, no difference between the effect of OB and placebo was found in the intensity of abdominal pain, the proportion of patient responders, and the safety and quality of life scores. During follow-up, the therapeutic effect of OB remained greater than placebo in terms of withdrawal rate due to symptom relapse (P = 0.009), global efficacy of treatment and relapse-free probability (P = 0.038). Therefore, the study demonstrated superiority of OB vs placebo in the reduction of pain and bloating, and in protection from relapse as a result of the long-lasting effect. These symptoms improved progressively during the study. It should be pointed out that IBS trials are subjected to high placebo effect, typically between 30% and 60% thus making difficult to detect the therapeutic gain and interpretation of the results[126]. The second trial was an Asian study[127] which randomized 117 participants to receive 40 mg OB or 100 mg mebeverine, thrice daily for eight weeks. The abdominal pain/discomfort frequency score (APDFS) and safety profile were assessed. Compared to baselines, the APDFSs in OB and mebeverine were significantly reduced (0.55; P = 0.011 and 0.37; P = 0.042 respectively). However, when the improved results of the two treatments were compared between them, statistical significance was not reached). One hundred eighteen AEs were reported (OB = 65 and mebeverine = 53); these comprised mostly dry mouth in both arms, followed by nausea and dizziness (particularly in OB).
Similarly, solifenacin, a muscarinic type 3 receptor antagonist, that is used to treat overactive bladder in adults has been evaluated in a recent study for the symptomatic relief of diarrhea in 20 IBS-D patients[128]. After a 2-wk observation period, all participants received solifenacin for six weeks. Subsequently, the administration of solifenacin was discontinued and ramosetron, a serotonin 3 receptor antagonist, was administered for four weeks. Two weeks after initiation of solifenacin, an overall improvement was observed in 16 out of 20 participants (80%). The efficacy of solifenacin in the treatment of IBS with diarrhea was not inferior to that of ramosetron. However, the study had the limitation of not being placebo-controlled.
In recent years, increasing attention has been given to the role of the nonadrenergic and noncholinergic (NANC) nervous system for the regulation of colonic motility. Nitric oxide (NO) has been identified as an important component of the NANC nervous system and as an inhibitory neurotransmitter in the colon[129]. NO mediates the relaxation of smooth muscle cells in the GI tract by production of intracellular guanosine 3,5-cyclic monophosphate (cGMP)[129] and is also involved in nociception[130]. Sildenafil is an orally administered drug that has been used to augment NO activity and is widely used as a treatment for erectile dysfunction. In an earlier study[131] stimulation of the NO-cGMP pathway by sildenaifil administration decreased rectal tone but did not influence rectal distensibility. Relaxation of the rectum was accompanied by an increase in rectal volumes to reach perception thresholds in healthy subjects and in patients with IBS, but no direct effect on rectal perception could be demonstrated. Recently, another small study[132] evaluated the effects of sildenafil tone inhibition on rectal sensitivity. Eight control subjects and 21 IBS patients (Rome II) were enrolled in a double-blinded study, after dosing with placebo or sildenafil (50 mg p.o.). Sildenafil increased the first desire to defecate and the pain in the hypersensitive IBS patients. It also increased rectal compliance, but only in diarrhea-IBS. No trials regarding the effectiveness of sildenafil on the relief of the IBS symptoms and the quality of life are available.
Opioid receptor agonists
Opioid receptors, including m, d, and k, are expressed along the GI tract and play a key role in regulating GI motility, secretion, and visceral sensation. Recently, exogenous opioids have been shown to reduce GI transit through activation of m-opioid receptor (MOR) and they can treat diarrhea in acute situations. Agents that simultaneously activate MOR and antagonize d-opioid receptor (DOR) have differential GI effects and can possess increased analgesic potency compared to pure MOR agonists[133]. Eluxadoline is a locally active, mixed MOR agonist/DOR antagonist with low oral bioavailability that is being developed for the treatment of IBS-D. In vitro, eluxadoline reduces contractility in intestinal tissue and inhibits neurogenically mediated secretion[134]. In a recent phase II study[135] 807 patients were randomly assigned to groups receiving twice daily 5, 25, 100, or 200 mg oral eluxadoline or oral placebo for 12 wk. The primary end point was clinical response at week four, defined by a mean reduction in daily pain score of more than 30% from baseline and of at least 2 points on 0-10 scale, as well as a stool consistency score of 3 or 4 on the Bristol Stool Scale (1-7) for at least 66% of daily diary entries during that week. The authors concluded that patients given eluxadoline were significantly more likely to be clinical responders, based on a combination of improvement in abdominal pain and stool consistency. Another selective, potent k-opioid agonist, asimadoline, which has been shown to improve pain and abnormal bowel function, has been evaluated in a trial[136]. Asimadoline has low permeability through the blood-brain barrier. In this trial, 596 patients with varying IBS subtypes were randomized to receive 0.15, 0.5, 1.0 mg asimadoline or placebo b.i.d for twelve weeks. Asimadoline (0.5 mg) significantly prolonged the total time (number of mo) with adequate relief of IBS pain or discomfort (46.7% vs 20.0%), adequate relief of IBS symptoms (46.7% vs 23.0%). It also significantly reduced pain scores (week 12: -1.6 vs -0.7), increased pain free days (42.9% vs 18.0%), and improved urgency and stool frequency (-2.3 vs -0.3). These positive results were observed in IBS-D patients with at least moderate pain in baseline. However, no significant difference was observed in the percentage of months with adequate relief. Asimadoline failed to show a benefit in IBS-C.
Drugs acting through the endocannabinoid system have also been studied. Two types of G-protein- coupled cannabinoid receptors, CB1 and CB2, have been identified and cloned[137]. CB1-immunoreactivity is located on the normal colonic epithelium, smooth muscle, and the myenteric plexus. Dronabinol, a nonselective CB receptor agonist, has been shown to inhibit and colonic motility in healthy humans[138]. In a recent study[139], the effect of dronabinol on colonic sensory and motor functions in 75 patients with mixed IBS subtypes who were cannabinoid naïve was assessed. Patients were randomly assigned to groups that were given a single dose of placebo or 2.5 mg or 5.0 mg dronabinol. Single nucleotide polymorphisms CNR1 rs806378, fatty acid amide hydrolase (FAAH) rs324420, and MGLL rs4881 were also studied. In all patients, dronabinol decreased fasting proximal left colonic motility index compared with placebo and increased the colonic compliance. The effects of dronabinol were greatest in IBS patients with diarrhea or IBS alternating. Dronabinol did not alter sensation or tone but it affected fasting distal motility index in patients, regardless of FAAH rs324420 variant (CA/AA vs CC) (P = 0.046)
GLP-1 (Rose-10)
GLP-1(glucagon-like peptide 1) is normally released after food intake. It stimulates insulin release and reduces gastric emptying and small intestinal motility[140]. GLP-1 has been reported to inhibits small intestinal motility in IBS patients[141] and to prolong colonic transit[142]. The initial use of GLP-1 analogues was to normalize blood glucose levels in patients with diabetes; however, based on the aforementioned observation,s are now being studied to treat abdominal pain attacks in patients with IBS. The GLP-1 analog ROSE-010 has been demonstrated to reduce acute IBS pain in a RCT involving 166 IBS patients[143]. Participants were assigned to receive single subcutaneous injections of ROSE-010 100 μg, 300 μg and placebo in a cross-over design. Patient-rated pain relief and intensity were evaluated with a visual-analog scale. The primary outcome measure was the proportion of patients with a minimum 50% pain reduction from 10 to 60 min after treatment. A significantly higher proportion of patients reported greater than 50% of the maximum total pain relief response after 100 and 300 μg of ROSE-010 treatments than after placebo (23% and 24% vs 12%; P =0.011 and P = 0.005, respectively). Times to meaningful and total pain relief were shorter for both doses of active drug vs placebo. A second single-center RCT evaluated safety, pharmacodynamics, and pharmacokinetics in women with IBS-C[144]. Patients were administered once daily 30, 100, or 300 μg ROSE-010 subcutaneously or placebo for three consecutive days as well as a single repetitive dose after 2-10 d. Validated scintigraphy was used to measure GI and colonic transit. Single-photon emission computed tomography was used to measure gastric volumes. The primary outcome measures were gastric emptying of solids half time, the colonic transit geometric center at 24 h, and the gastric accommodation volume. Gastric emptying was significantly retarded at the doses of 100 and 300 μg ROSE-010. Gastric volumes, small bowel or colonic transit at 24 h and bowel functions were not significantly altered by ROSE-010. Colonic transit at 48 h was accelerated with the 30 and 100 μg ROSE-010 doses. AEs were vomiting (P = 0.008) and nausea nausea (P < 0.001). Based on the observation that at the doses of 30 and 100 μg the drug accelerated colonic transit time, the authors concluded that it could be a candidate for relief of constipation in IBS-C. More in-depth assessments of the IBS pain attack characteristics are ongoing and future clinical trials with ROSE-010 are being planned[15].
Ketotifen
Experimental studies have shown that mast cells play an important role in IBS through visceral hypersensitivity[145]. Patients with IBS excibit an increased number of mast cells in the small intestine[146], large intestine[147,148] and rectum[149]. The number of mucosal mast cells and their proximity to sensory nerves in colonic tissue has also been studied and found positively correlated to abdominal pain[148]. Mast cells activation results in degranulation; thus mediators pre-stored in vesicles such as tryptase, histamine and several cytokines are rapidly released inducing an inflammatory response. Sodium cromoglycate and ketotifen are well known membrane stabilizers that act by blocking mast cell degranulation[145]. Klooker et al[145] conducted a RCT to assess the effect of ketotifen on IBS. Sixty patients with various IBS subtypes (Rome II criteria) were included in the study. The idea was to evaluate whether increased number of mast cells and/or increased spontaneous mucosal tryptase release is associated with visceral hypersensitivity and whether mast cell stabilization with ketotifen had an impact on visceral perception; this was estimated by measurements of rectal distension in hypersensitive patients with IBS. Abdominal symptoms were also monitored. The trial consisted of two weeks of screening/observation, then a treatment period of eight weeks and a follow-up period of another two weeks. Barostat measurements were performed at baseline and then after eight weeks of treatment with ketotifen or placebo. Rectal biopsies were also collected before and after treatment. Ketotifen was shown to be superior to placebo in increasing the threshold for discomfort in patients with IBS with visceral hypersensitivity; it also significantly improved abdominal pain and quality of life. Mast cells and spontaneous release of tryptase were lower in patients with IBS than in healthy volunteers. However, ketotifen did not histamine and tryptase release. Further studies are needed to confirm the beneficial effect of ketotifen in IBS symptoms and clarify its way of action.
CONCLUSION
IBS is a highly prevalent functional disorder that reduces patients’ quality of life. IBS is not a single disease entity, but rather likely consists of several different disease states; currently, treatment is predicated upon the patient’s most bothersome symptoms. Various drug categories (antispasmodics, laxatives, dopamine antagonists, 5-HT3 antagonists and/or 5-HT4 agonists, sedatives, antibiotics, probiotics), modifications in diet and lifestyle, and complementary and alternative therapies have been proposed as symptomatic treatment. It is difficult to draw conclusions from previous studies since IBS trials are subjected to high placebo effect, typically between 30% and 60% thus complicating the detection of the therapeutic gain and interpretation of the results. For IBS-C, linaclotide and lubiprostone seem promising for the relief of multiple symptoms from which patients with IBS-C suffer. Regarding IBS-D, although the 5-HT3 antagonist alosetron was shown to be superior than placebo at relieving global IBS symptoms in male and female with a high level of evidence, it was withdrawn from the market due to complications (ischemic colitis). Newer 5-HT3 antagonists (cilansetron, ramosetron) have emerged; however there is lack of consistent data demonstrating whether the drug is superior over placebo. In the category of antibiotics, rifaximin has been presented as efficacious in RCTs evaluating IBS patients. It has emerged as a strong option for the treatment of IBS because of its broad-spectrum bactericidal activity in vitro, its efficacy for SIBO in vivo, its favorable tolerability profile and the lack of association with clinically relevant resistance or Clostridium difficile colitis. Among the antispasmodics, OB showed consistent evidence of efficacy over placebo. Other molecules, i.e. NO donors, Opioid Receptor Agonists, ketotifen, as well as GLP-1 have been proposed for IBS treatment as well.
Footnotes
P- Reviewers: Kuo SM, Mansour-Ghanaei F, Marsh MN S- Editor: Qi Y L- Editor: A E- Editor: Ma S
References
- 1.Longstreth GF, Wilson A, Knight K, Wong J, Chiou CF, Barghout V, Frech F, Ofman JJ. Irritable bowel syndrome, health care use, and costs: a U.S. managed care perspective. Am J Gastroenterol. 2003;98:600–607. doi: 10.1111/j.1572-0241.2003.07296.x. [DOI] [PubMed] [Google Scholar]
- 2.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 3.Lacy BE, Weiser K, De Lee R. The treatment of irritable bowel syndrome. Therap Adv Gastroenterol. 2009;2:221–238. doi: 10.1177/1756283X09104794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crowell MD, Harris L, Jones MP, Chang L. New insights into the pathophysiology of irritable bowel syndrome: implications for future treatments. Curr Gastroenterol Rep. 2005;7:272–279. doi: 10.1007/s11894-005-0019-8. [DOI] [PubMed] [Google Scholar]
- 5.Hasler WL. Traditional thoughts on the pathophysiology of irritable bowel syndrome. Gastroenterol Clin North Am. 2011;40:21–43. doi: 10.1016/j.gtc.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Pimentel M, Chang C. Inflammation and microflora. Gastroenterol Clin North Am. 2011;40:69–85. doi: 10.1016/j.gtc.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 7.Salari P, Abdollahi M. Systematic review of modulators of benzodiazepine receptors in irritable bowel syndrome: is there hope? World J Gastroenterol. 2011;17:4251–4257. doi: 10.3748/wjg.v17.i38.4251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manabe N, Wong BS, Camilleri M, Burton D, McKinzie S, Zinsmeister AR. Lower functional gastrointestinal disorders: evidence of abnormal colonic transit in a 287 patient cohort. Neurogastroenterol Motil. 2010;22:293–e82. doi: 10.1111/j.1365-2982.2009.01442.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deiteren A, Camilleri M, Burton D, McKinzie S, Rao A, Zinsmeister AR. Effect of meal ingestion on ileocolonic and colonic transit in health and irritable bowel syndrome. Dig Dis Sci. 2010;55:384–391. doi: 10.1007/s10620-009-1041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khoshoo V, Armstead C, Landry L. Effect of a laxative with and without tegaserod in adolescents with constipation predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2006;23:191–196. doi: 10.1111/j.1365-2036.2006.02705.x. [DOI] [PubMed] [Google Scholar]
- 11.Awad RA, Camacho S. A randomized, double-blind, placebo-controlled trial of polyethylene glycol effects on fasting and postprandial rectal sensitivity and symptoms in hypersensitive constipation-predominant irritable bowel syndrome. Colorectal Dis. 2010;12:1131–1138. doi: 10.1111/j.1463-1318.2009.01990.x. [DOI] [PubMed] [Google Scholar]
- 12.Chapman RW, Stanghellini V, Geraint M, Halphen M. Randomized clinical trial: macrogol/PEG 3350 plus electrolytes for treatment of patients with constipation associated with irritable bowel syndrome. Am J Gastroenterol. 2013;108:1508–1515. doi: 10.1038/ajg.2013.197. [DOI] [PubMed] [Google Scholar]
- 13.Bryant AP, Busby RW, Bartolini WP, Cordero EA, Hannig G, Kessler MM, Pierce CM, Solinga RM, Tobin JV, Mahajan-Miklos S, et al. Linaclotide is a potent and selective guanylate cyclase C agonist that elicits pharmacological effects locally in the gastrointestinal tract. Life Sci. 2010;86:760–765. doi: 10.1016/j.lfs.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 14.Shailubhai K. Therapeutic applications of guanylate cyclase-C receptor agonists. Curr Opin Drug Discov Devel. 2002;5:261–268. [PubMed] [Google Scholar]
- 15.Maneerattanaporn M, Chang L, Chey WD. Emerging pharmacological therapies for the irritable bowel syndrome. Gastroenterol Clin North Am. 2011;40:223–243. doi: 10.1016/j.gtc.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 16.Andresen V, Camilleri M, Busciglio IA, Grudell A, Burton D, McKinzie S, Foxx-Orenstein A, Kurtz CB, Sharma V, Johnston JM, et al. Effect of 5 days linaclotide on transit and bowel function in females with constipation-predominant irritable bowel syndrome. Gastroenterology. 2007;133:761–768. doi: 10.1053/j.gastro.2007.06.067. [DOI] [PubMed] [Google Scholar]
- 17.Johnston JM, Kurtz CB, Drossman DA, Lembo AJ, Jeglinski BI, MacDougall JE, Antonelli SM, Currie MG. Pilot study on the effect of linaclotide in patients with chronic constipation. Am J Gastroenterol. 2009;104:125–132. doi: 10.1038/ajg.2008.59. [DOI] [PubMed] [Google Scholar]
- 18.Lembo AJ, Kurtz CB, Macdougall JE, Lavins BJ, Currie MG, Fitch DA, Jeglinski BI, Johnston JM. Efficacy of linaclotide for patients with chronic constipation. Gastroenterology. 2010;138:886–895.e1. doi: 10.1053/j.gastro.2009.12.050. [DOI] [PubMed] [Google Scholar]
- 19.Johnston JM, Kurtz CB, Macdougall JE, Lavins BJ, Currie MG, Fitch DA, O’Dea C, Baird M, Lembo AJ. Linaclotide improves abdominal pain and bowel habits in a phase IIb study of patients with irritable bowel syndrome with constipation. Gastroenterology. 2010;139:1877–1886.e2. doi: 10.1053/j.gastro.2010.08.041. [DOI] [PubMed] [Google Scholar]
- 20.Chey WD, Lembo AJ, Lavins BJ, Shiff SJ, Kurtz CB, Currie MG, MacDougall JE, Jia XD, Shao JZ, Fitch DA, et al. Linaclotide for irritable bowel syndrome with constipation: a 26-week, randomized, double-blind, placebo-controlled trial to evaluate efficacy and safety. Am J Gastroenterol. 2012;107:1702–1712. doi: 10.1038/ajg.2012.254. [DOI] [PubMed] [Google Scholar]
- 21.Rao S, Lembo AJ, Shiff SJ, Lavins BJ, Currie MG, Jia XD, Shi K, MacDougall JE, Shao JZ, Eng P, et al. A 12-week, randomized, controlled trial with a 4-week randomized withdrawal period to evaluate the efficacy and safety of linaclotide in irritable bowel syndrome with constipation. Am J Gastroenterol. 2012;107:1714–1724; quiz p.1725. doi: 10.1038/ajg.2012.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quigley EM, Tack J, Chey WD, Rao SS, Fortea J, Falques M, Diaz C, Shiff SJ, Currie MG, Johnston JM. Randomised clinical trials: linaclotide phase 3 studies in IBS-C - a prespecified further analysis based on European Medicines Agency-specified endpoints. Aliment Pharmacol Ther. 2013;37:49–61. doi: 10.1111/apt.12123. [DOI] [PubMed] [Google Scholar]
- 23.Videlock EJ, Cheng V, Cremonini F. Effects of linaclotide in patients with irritable bowel syndrome with constipation or chronic constipation: a meta-analysis. Clin Gastroenterol Hepatol. 2013;11:1084–1092.e3; quiz e68. doi: 10.1016/j.cgh.2013.04.032. [DOI] [PubMed] [Google Scholar]
- 24.Hasler WL. Serotonin and the GI tract. Curr Gastroenterol Rep. 2009;11:383–391. doi: 10.1007/s11894-009-0058-7. [DOI] [PubMed] [Google Scholar]
- 25.Houghton LA, Atkinson W, Whitaker RP, Whorwell PJ, Rimmer MJ. Increased platelet depleted plasma 5-hydroxytryptamine concentration following meal ingestion in symptomatic female subjects with diarrhoea predominant irritable bowel syndrome. Gut. 2003;52:663–670. doi: 10.1136/gut.52.5.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dunlop SP, Coleman NS, Blackshaw E, Perkins AC, Singh G, Marsden CA, Spiller RC. Abnormalities of 5-hydroxytryptamine metabolism in irritable bowel syndrome. Clin Gastroenterol Hepatol. 2005;3:349–357. doi: 10.1016/s1542-3565(04)00726-8. [DOI] [PubMed] [Google Scholar]
- 27.Atkinson W, Lockhart S, Whorwell PJ, Keevil B, Houghton LA. Altered 5-hydroxytryptamine signaling in patients with constipation- and diarrhea-predominant irritable bowel syndrome. Gastroenterology. 2006;130:34–43. doi: 10.1053/j.gastro.2005.09.031. [DOI] [PubMed] [Google Scholar]
- 28.Zuo XL, Li YQ, Yang XZ, Guo M, Guo YT, Lu XF, Li JM, Desmond PV. Plasma and gastric mucosal 5-hydroxytryptamine concentrations following cold water intake in patients with diarrhea-predominant irritable bowel syndrome. J Gastroenterol Hepatol. 2007;22:2330–2337. doi: 10.1111/j.1440-1746.2006.04772.x. [DOI] [PubMed] [Google Scholar]
- 29.Gershon MD, Tack J. The serotonin signaling system: from basic understanding to drug development for functional GI disorders. Gastroenterology. 2007;132:397–414. doi: 10.1053/j.gastro.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 30.Grider JR, Foxx-Orenstein AE, Jin JG. 5-Hydroxytryptamine4 receptor agonists initiate the peristaltic reflex in human, rat, and guinea pig intestine. Gastroenterology. 1998;115:370–380. doi: 10.1016/s0016-5085(98)70203-3. [DOI] [PubMed] [Google Scholar]
- 31.Degen L, Matzinger D, Merz M, Appel-Dingemanse S, Osborne S, Lüchinger S, Bertold R, Maecke H, Beglinger C. Tegaserod, a 5-HT4 receptor partial agonist, accelerates gastric emptying and gastrointestinal transit in healthy male subjects. Aliment Pharmacol Ther. 2001;15:1745–1751. doi: 10.1046/j.1365-2036.2001.01103.x. [DOI] [PubMed] [Google Scholar]
- 32.Prather CM, Camilleri M, Zinsmeister AR, McKinzie S, Thomforde G. Tegaserod accelerates orocecal transit in patients with constipation-predominant irritable bowel syndrome. Gastroenterology. 2000;118:463–468. doi: 10.1016/s0016-5085(00)70251-4. [DOI] [PubMed] [Google Scholar]
- 33.Jiao HM, Xie PY. Tegaserod inhibits noxious rectal distention induced responses and limbic system c-Fos expression in rats with visceral hypersensitivity. World J Gastroenterol. 2004;10:2836–2841. doi: 10.3748/wjg.v10.i19.2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sabaté JM, Bouhassira D, Poupardin C, Wagner A, Loria Y, Coffin B. Sensory signalling effects of tegaserod in patients with irritable bowel syndrome with constipation. Neurogastroenterol Motil. 2008;20:134–141. doi: 10.1111/j.1365-2982.2007.01030.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Müller-Lissner SA, Fumagalli I, Bardhan KD, Pace F, Pecher E, Nault B, Rüegg P. Tegaserod, a 5-HT(4) receptor partial agonist, relieves symptoms in irritable bowel syndrome patients with abdominal pain, bloating and constipation. Aliment Pharmacol Ther. 2001;15:1655–1666. doi: 10.1046/j.1365-2036.2001.01094.x. [DOI] [PubMed] [Google Scholar]
- 36.Novick J, Miner P, Krause R, Glebas K, Bliesath H, Ligozio G, Rüegg P, Lefkowitz M. A randomized, double-blind, placebo-controlled trial of tegaserod in female patients suffering from irritable bowel syndrome with constipation. Aliment Pharmacol Ther. 2002;16:1877–1888. doi: 10.1046/j.1365-2036.2002.01372.x. [DOI] [PubMed] [Google Scholar]
- 37.Chey WD, Paré P, Viegas A, Ligozio G, Shetzline MA. Tegaserod for female patients suffering from IBS with mixed bowel habits or constipation: a randomized controlled trial. Am J Gastroenterol. 2008;103:1217–1225. doi: 10.1111/j.1572-0241.2008.01808.x. [DOI] [PubMed] [Google Scholar]
- 38.Kellow J, Lee OY, Chang FY, Thongsawat S, Mazlam MZ, Yuen H, Gwee KA, Bak YT, Jones J, Wagner A. An Asia-Pacific, double blind, placebo controlled, randomised study to evaluate the efficacy, safety, and tolerability of tegaserod in patients with irritable bowel syndrome. Gut. 2003;52:671–676. doi: 10.1136/gut.52.5.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nyhlin H, Bang C, Elsborg L, Silvennoinen J, Holme I, Rüegg P, Jones J, Wagner A. A double-blind, placebo-controlled, randomized study to evaluate the efficacy, safety and tolerability of tegaserod in patients with irritable bowel syndrome. Scand J Gastroenterol. 2004;39:119–126. doi: 10.1080/00365520310006748. [DOI] [PubMed] [Google Scholar]
- 40.Tougas G, Snape WJ, Otten MH, Earnest DL, Langaker KE, Pruitt RE, Pecher E, Nault B, Rojavin MA. Long-term safety of tegaserod in patients with constipation-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2002;16:1701–1708. doi: 10.1046/j.1365-2036.2002.01347.x. [DOI] [PubMed] [Google Scholar]
- 41.Saad RJ. Peripherally acting therapies for the treatment of irritable bowel syndrome. Gastroenterol Clin North Am. 2011;40:163–182. doi: 10.1016/j.gtc.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 42.Thompson CA. Novartis suspends tegaserod sales at FDA’s request. Am J Health Syst Pharm. 2007;64:1020. doi: 10.2146/news070044. [DOI] [PubMed] [Google Scholar]
- 43.Serebruany VL, El Mouelhi M, Pfannkuche HJ, Rose K, Marro M, Angiolillo DJ. Investigations on 5-HT4 receptor expression and effects of tegaserod on human platelet aggregation in vitro. Am J Ther. 2010;17:543–552. doi: 10.1097/MJT.0b013e3181b63f21. [DOI] [PubMed] [Google Scholar]
- 44.Liu Z, Sakakibara R, Odaka T, Uchiyama T, Uchiyama T, Yamamoto T, Ito T, Asahina M, Yamaguchi K, Yamaguchi T, et al. Mosapride citrate, a novel 5-HT4 agonist and partial 5-HT3 antagonist, ameliorates constipation in parkinsonian patients. Mov Disord. 2005;20:680–686. doi: 10.1002/mds.20387. [DOI] [PubMed] [Google Scholar]
- 45.Kim HS, Choi EJ, Park H. The effect of mosapride citrate on proximal and distal colonic motor function in the guinea-pig in vitro. Neurogastroenterol Motil. 2008;20:169–176. doi: 10.1111/j.1365-2982.2007.00996.x. [DOI] [PubMed] [Google Scholar]
- 46.Kojima Y, Fujii H, Katsui R, Nakajima Y, Takaki M. Enhancement of the intrinsic defecation reflex by mosapride, a 5-HT4 agonist, in chronically lumbosacral denervated guinea pigs. J Smooth Muscle Res. 2006;42:139–147. doi: 10.1540/jsmr.42.139. [DOI] [PubMed] [Google Scholar]
- 47.Kojima Y, Nakagawa T, Katsui R, Fujii H, Nakajima Y, Takaki M. A 5-HT4 agonist, mosapride, enhances intrinsic rectorectal and rectoanal reflexes after removal of extrinsic nerves in guinea pigs. Am J Physiol Gastrointest Liver Physiol. 2005;289:G351–G360. doi: 10.1152/ajpgi.00532.2004. [DOI] [PubMed] [Google Scholar]
- 48.Kanazawa M, Watanabe S, Tana C, Komuro H, Aoki M, Fukudo S. Effect of 5-HT4 receptor agonist mosapride citrate on rectosigmoid sensorimotor function in patients with irritable bowel syndrome. Neurogastroenterol Motil. 2011;23:754–e332. doi: 10.1111/j.1365-2982.2011.01732.x. [DOI] [PubMed] [Google Scholar]
- 49.Lembo AJ, Cremonini F, Meyers N, Hickling R. Clinical trial: renzapride treatment of women with irritable bowel syndrome and constipation - a double-blind, randomized, placebo-controlled, study. Aliment Pharmacol Ther. 2010;31:979–990. doi: 10.1111/j.1365-2036.2010.04265.x. [DOI] [PubMed] [Google Scholar]
- 50.Lacy BE, Levy LC. Lubiprostone: a chloride channel activator. J Clin Gastroenterol. 2007;41:345–351. doi: 10.1097/01.mcg.0000225665.68920.df. [DOI] [PubMed] [Google Scholar]
- 51.Bijvelds MJ, Bot AG, Escher JC, De Jonge HR. Activation of intestinal Cl- secretion by lubiprostone requires the cystic fibrosis transmembrane conductance regulator. Gastroenterology. 2009;137:976–985. doi: 10.1053/j.gastro.2009.05.037. [DOI] [PubMed] [Google Scholar]
- 52.Chan WW, Mashimo H. Lubiprostone Increases Small Intestinal Smooth Muscle Contractions Through a Prostaglandin E Receptor 1 (EP1)-mediated Pathway. J Neurogastroenterol Motil. 2013;19:312–318. doi: 10.5056/jnm.2013.19.3.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Camilleri M, Bharucha AE, Ueno R, Burton D, Thomforde GM, Baxter K, McKinzie S, Zinsmeister AR. Effect of a selective chloride channel activator, lubiprostone, on gastrointestinal transit, gastric sensory, and motor functions in healthy volunteers. Am J Physiol Gastrointest Liver Physiol. 2006;290:G942–G947. doi: 10.1152/ajpgi.00264.2005. [DOI] [PubMed] [Google Scholar]
- 54.Johanson JF, Ueno R. Lubiprostone, a locally acting chloride channel activator, in adult patients with chronic constipation: a double-blind, placebo-controlled, dose-ranging study to evaluate efficacy and safety. Aliment Pharmacol Ther. 2007;25:1351–1361. doi: 10.1111/j.1365-2036.2007.03320.x. [DOI] [PubMed] [Google Scholar]
- 55.Johanson JF, Morton D, Geenen J, Ueno R. Multicenter, 4-week, double-blind, randomized, placebo-controlled trial of lubiprostone, a locally-acting type-2 chloride channel activator, in patients with chronic constipation. Am J Gastroenterol. 2008;103:170–177. doi: 10.1111/j.1572-0241.2007.01524.x. [DOI] [PubMed] [Google Scholar]
- 56.Barish CF, Drossman D, Johanson JF, Ueno R. Efficacy and safety of lubiprostone in patients with chronic constipation. Dig Dis Sci. 2010;55:1090–1097. doi: 10.1007/s10620-009-1068-x. [DOI] [PubMed] [Google Scholar]
- 57.Johanson JF, Drossman DA, Panas R, Wahle A, Ueno R. Clinical trial: phase 2 study of lubiprostone for irritable bowel syndrome with constipation. Aliment Pharmacol Ther. 2008;27:685–696. doi: 10.1111/j.1365-2036.2008.03629.x. [DOI] [PubMed] [Google Scholar]
- 58.Fukudo S, Hongo M, Kaneko H, Ueno R. Efficacy and safety of oral lubiprostone in constipated patients with or without irritable bowel syndrome: a randomized, placebo-controlled and dose-finding study. Neurogastroenterol Motil. 2011;23:544–e205. doi: 10.1111/j.1365-2982.2011.01668.x. [DOI] [PubMed] [Google Scholar]
- 59.Drossman DA, Chey WD, Johanson JF, Fass R, Scott C, Panas R, Ueno R. Clinical trial: lubiprostone in patients with constipation-associated irritable bowel syndrome--results of two randomized, placebo-controlled studies. Aliment Pharmacol Ther. 2009;29:329–341. doi: 10.1111/j.1365-2036.2008.03881.x. [DOI] [PubMed] [Google Scholar]
- 60.Chey WD, Drossman DA, Johanson JF, Scott C, Panas RM, Ueno R. Safety and patient outcomes with lubiprostone for up to 52 weeks in patients with irritable bowel syndrome with constipation. Aliment Pharmacol Ther. 2012;35:587–599. doi: 10.1111/j.1365-2036.2011.04983.x. [DOI] [PubMed] [Google Scholar]
- 61.Brandt LJ, Chey WD, Foxx-Orenstein AE, Schiller LR, Schoenfeld PS, Spiegel BM, Talley NJ, Quigley EM. An evidence-based position statement on the management of irritable bowel syndrome. Am J Gastroenterol. 2009;104 Suppl 1:S1–S35. doi: 10.1038/ajg.2008.122. [DOI] [PubMed] [Google Scholar]
- 62.Iser JH, Sali A. Chenodeoxycholic acid: a review of its pharmacological properties and therapeutic use. Drugs. 1981;21:90–119. doi: 10.2165/00003495-198121020-00002. [DOI] [PubMed] [Google Scholar]
- 63.Mitchell WD, Findlay JM, Prescott RJ, Eastwood MA, Horn DB. Bile acids in the diarrhoea of ileal resection. Gut. 1973;14:348–353. doi: 10.1136/gut.14.5.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Aldini R, Roda A, Festi D, Sama C, Mazzella G, Bazzoli F, Morselli AM, Roda E, Barbara L. Bile acid malabsorption and bile acid diarrhea in intestinal resection. Dig Dis Sci. 1982;27:495–502. doi: 10.1007/BF01296727. [DOI] [PubMed] [Google Scholar]
- 65.Rao AS, Wong BS, Camilleri M, Odunsi-Shiyanbade ST, McKinzie S, Ryks M, Burton D, Carlson P, Lamsam J, Singh R, et al. Chenodeoxycholate in females with irritable bowel syndrome-constipation: a pharmacodynamic and pharmacogenetic analysis. Gastroenterology. 2010;139:1549–1558, 1558.e1. doi: 10.1053/j.gastro.2010.07.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kirwan WO, Smith AN, Mitchell WD, Falconer JD, Eastwood MA. Bile acids and colonic motility in the rabbit and the human. Gut. 1975;16:894–902. doi: 10.1136/gut.16.11.894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mok HY, Bell GD, Dowling RH. Effect of different doses of chenodeoxycholic acid on bile-lipid composition and on frequency of side-effects in patients with gallstones. Lancet. 1974;2:253–257. doi: 10.1016/s0140-6736(74)91415-9. [DOI] [PubMed] [Google Scholar]
- 68.Caspary WF, Meyne K. Effects of chenodeoxy- and ursodeoxycholic acid on absorption, secretion and permeability in rat colon and small intestine. Digestion. 1980;20:168–174. doi: 10.1159/000198436. [DOI] [PubMed] [Google Scholar]
- 69.Odunsi-Shiyanbade ST, Camilleri M, McKinzie S, Burton D, Carlson P, Busciglio IA, Lamsam J, Singh R, Zinsmeister AR. Effects of chenodeoxycholate and a bile acid sequestrant, colesevelam, on intestinal transit and bowel function. Clin Gastroenterol Hepatol. 2010;8:159–165. doi: 10.1016/j.cgh.2009.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fromm H, Roat JW, Gonzalez V, Sarva RP, Farivar S. Comparative efficacy and side effects of ursodeoxycholic and chenodeoxycholic acids in dissolving gallstones. A double-blind controlled study. Gastroenterology. 1983;85:1257–1264. [PubMed] [Google Scholar]
- 71.Cann PA, Read NW, Holdsworth CD, Barends D. Role of loperamide and placebo in management of irritable bowel syndrome (IBS) Dig Dis Sci. 1984;29:239–247. doi: 10.1007/BF01296258. [DOI] [PubMed] [Google Scholar]
- 72.Hovdenak N. Loperamide treatment of the irritable bowel syndrome. Scand J Gastroenterol Suppl. 1987;130:81–84. doi: 10.3109/00365528709091004. [DOI] [PubMed] [Google Scholar]
- 73.Lavö B, Stenstam M, Nielsen AL. Loperamide in treatment of irritable bowel syndrome--a double-blind placebo controlled study. Scand J Gastroenterol Suppl. 1987;130:77–80. doi: 10.3109/00365528709091003. [DOI] [PubMed] [Google Scholar]
- 74.Efskind PS, Bernklev T, Vatn MH. A double-blind placebo-controlled trial with loperamide in irritable bowel syndrome. Scand J Gastroenterol. 1996;31:463–468. doi: 10.3109/00365529609006766. [DOI] [PubMed] [Google Scholar]
- 75.Camilleri M, Northcutt AR, Kong S, Dukes GE, McSorley D, Mangel AW. Efficacy and safety of alosetron in women with irritable bowel syndrome: a randomised, placebo-controlled trial. Lancet. 2000;355:1035–1040. doi: 10.1016/S0140-6736(00)02033-X. [DOI] [PubMed] [Google Scholar]
- 76.Camilleri M, Chey WY, Mayer EA, Northcutt AR, Heath A, Dukes GE, McSorley D, Mangel AM. A randomized controlled clinical trial of the serotonin type 3 receptor antagonist alosetron in women with diarrhea-predominant irritable bowel syndrome. Arch Intern Med. 2001;161:1733–1740. doi: 10.1001/archinte.161.14.1733. [DOI] [PubMed] [Google Scholar]
- 77.Watson ME, Lacey L, Kong S, Northcutt AR, McSorley D, Hahn B, Mangel AW. Alosetron improves quality of life in women with diarrhea-predominant irritable bowel syndrome. Am J Gastroenterol. 2001;96:455–459. doi: 10.1111/j.1572-0241.2001.03525.x. [DOI] [PubMed] [Google Scholar]
- 78.Lembo T, Wright RA, Bagby B, Decker C, Gordon S, Jhingran P, Carter E. Alosetron controls bowel urgency and provides global symptom improvement in women with diarrhea-predominant irritable bowel syndrome. Am J Gastroenterol. 2001;96:2662–2670. doi: 10.1111/j.1572-0241.2001.04128.x. [DOI] [PubMed] [Google Scholar]
- 79.Cremonini F, Nicandro JP, Atkinson V, Shringarpure R, Chuang E, Lembo A. Randomised clinical trial: alosetron improves quality of life and reduces restriction of daily activities in women with severe diarrhoea-predominant IBS. Aliment Pharmacol Ther. 2012;36:437–448. doi: 10.1111/j.1365-2036.2012.05208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rahimi R, Nikfar S, Abdollahi M. Efficacy and tolerability of alosetron for the treatment of irritable bowel syndrome in women and men: a meta-analysis of eight randomized, placebo-controlled, 12-week trials. Clin Ther. 2008;30:884–901. doi: 10.1016/j.clinthera.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 81.Andresen V, Montori VM, Keller J, West CP, Layer P, Camilleri M. Effects of 5-hydroxytryptamine (serotonin) type 3 antagonists on symptom relief and constipation in nonconstipated irritable bowel syndrome: a systematic review and meta-analysis of randomized controlled trials. Clin Gastroenterol Hepatol. 2008;6:545–555. doi: 10.1016/j.cgh.2007.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ford AC, Brandt LJ, Young C, Chey WD, Foxx-Orenstein AE, Moayyedi P. Efficacy of 5-HT3 antagonists and 5-HT4 agonists in irritable bowel syndrome: systematic review and meta-analysis. Am J Gastroenterol. 2009;104:1831–1843; quiz 1844. doi: 10.1038/ajg.2009.223. [DOI] [PubMed] [Google Scholar]
- 83.Chang L, Tong K, Ameen V. Ischemic colitis and complications of constipation associated with the use of alosetron under a risk management plan: clinical characteristics, outcomes, and incidences. Am J Gastroenterol. 2010;105:866–875. doi: 10.1038/ajg.2010.25. [DOI] [PubMed] [Google Scholar]
- 84.Ohta M, Suzuki T, Nagashima S, Tokunaga T, Miyata K, Mase T. Novel 5-hydroxytryptamine (5-HT3) receptor antagonists. IV. Synthesis and pharmacological evaluation of the oxidation products of (-)-(R)-5-[(1-methyl-1H-indol-3-yl)carbonyl] -4,5,6,7-tetrahydro-1H-benzimidazole hydrochloride (YM060: ramosetron) Chem Pharm Bull (Tokyo) 1996;44:1717–1722. doi: 10.1248/cpb.44.1717. [DOI] [PubMed] [Google Scholar]
- 85.Matsueda K, Harasawa S, Hongo M, Hiwatashi N, Sasaki D. A phase II trial of the novel serotonin type 3 receptor antagonist ramosetron in Japanese male and female patients with diarrhea-predominant irritable bowel syndrome. Digestion. 2008;77:225–235. doi: 10.1159/000150632. [DOI] [PubMed] [Google Scholar]
- 86.Matsueda K, Harasawa S, Hongo M, Hiwatashi N, Sasaki D. A randomized, double-blind, placebo-controlled clinical trial of the effectiveness of the novel serotonin type 3 receptor antagonist ramosetron in both male and female Japanese patients with diarrhea-predominant irritable bowel syndrome. Scand J Gastroenterol. 2008;43:1202–1211. doi: 10.1080/00365520802240255. [DOI] [PubMed] [Google Scholar]
- 87.Lee KJ, Kim NY, Kwon JK, Huh KC, Lee OY, Lee JS, Choi SC, Sohn CI, Myung SJ, Park HJ, et al. Efficacy of ramosetron in the treatment of male patients with irritable bowel syndrome with diarrhea: a multicenter, randomized clinical trial, compared with mebeverine. Neurogastroenterol Motil. 2011;23:1098–1104. doi: 10.1111/j.1365-2982.2011.01771.x. [DOI] [PubMed] [Google Scholar]
- 88.Chiba T, Yamamoto K, Sato S, Suzuki K. Long-term efficacy and safety of ramosetron in the treatment of diarrhea-predominant irritable bowel syndrome. Clin Exp Gastroenterol. 2013;6:123–128. doi: 10.2147/CEG.S32721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tack J, Janssen P, Wouters M, Boeckxstaens G. Targeting serotonin synthesis to treat irritable bowel syndrome. Gastroenterology. 2011;141:420–422. doi: 10.1053/j.gastro.2011.06.024. [DOI] [PubMed] [Google Scholar]
- 90.Liu Q, Yang Q, Sun W, Vogel P, Heydorn W, Yu XQ, Hu Z, Yu W, Jonas B, Pineda R, et al. Discovery and characterization of novel tryptophan hydroxylase inhibitors that selectively inhibit serotonin synthesis in the gastrointestinal tract. J Pharmacol Exp Ther. 2008;325:47–55. doi: 10.1124/jpet.107.132670. [DOI] [PubMed] [Google Scholar]
- 91.Camilleri M. LX-1031, a tryptophan 5-hydroxylase inhibitor, and its potential in chronic diarrhea associated with increased serotonin. Neurogastroenterol Motil. 2011;23:193–200. doi: 10.1111/j.1365-2982.2010.01643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Brown PM, Drossman DA, Wood AJ, Cline GA, Frazier KS, Jackson JI, Bronner J, Freiman J, Zambrowicz B, Sands A, et al. The tryptophan hydroxylase inhibitor LX1031 shows clinical benefit in patients with nonconstipating irritable bowel syndrome. Gastroenterology. 2011;141:507–516. doi: 10.1053/j.gastro.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Tradtrantip L, Namkung W, Verkman AS. Crofelemer, an antisecretory antidiarrheal proanthocyanidin oligomer extracted from Croton lechleri, targets two distinct intestinal chloride channels. Mol Pharmacol. 2010;77:69–78. doi: 10.1124/mol.109.061051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mangel AW, Chaturvedi P. Evaluation of crofelemer in the treatment of diarrhea-predominant irritable bowel syndrome patients. Digestion. 2008;78:180–186. doi: 10.1159/000185719. [DOI] [PubMed] [Google Scholar]
- 95.Lin HC. Small intestinal bacterial overgrowth: a framework for understanding irritable bowel syndrome. JAMA. 2004;292:852–858. doi: 10.1001/jama.292.7.852. [DOI] [PubMed] [Google Scholar]
- 96.Pimentel M, Chow EJ, Lin HC. Eradication of small intestinal bacterial overgrowth reduces symptoms of irritable bowel syndrome. Am J Gastroenterol. 2000;95:3503–3506. doi: 10.1111/j.1572-0241.2000.03368.x. [DOI] [PubMed] [Google Scholar]
- 97.Pimentel M, Chow EJ, Lin HC. Normalization of lactulose breath testing correlates with symptom improvement in irritable bowel syndrome. a double-blind, randomized, placebo-controlled study. Am J Gastroenterol. 2003;98:412–419. doi: 10.1111/j.1572-0241.2003.07234.x. [DOI] [PubMed] [Google Scholar]
- 98.O’Mahony L, McCarthy J, Kelly P, Hurley G, Luo F, Chen K, O’Sullivan GC, Kiely B, Collins JK, Shanahan F, et al. Lactobacillus and bifidobacterium in irritable bowel syndrome: symptom responses and relationship to cytokine profiles. Gastroenterology. 2005;128:541–551. doi: 10.1053/j.gastro.2004.11.050. [DOI] [PubMed] [Google Scholar]
- 99.Frissora CL, Cash BD. Review article: the role of antibiotics vs. conventional pharmacotherapy in treating symptoms of irritable bowel syndrome. Aliment Pharmacol Ther. 2007;25:1271–1281. doi: 10.1111/j.1365-2036.2007.03313.x. [DOI] [PubMed] [Google Scholar]
- 100.Connor BA. Sequelae of traveler’s diarrhea: focus on postinfectious irritable bowel syndrome. Clin Infect Dis. 2005;41 Suppl 8:S577–S586. doi: 10.1086/432956. [DOI] [PubMed] [Google Scholar]
- 101.Pimentel M, Chatterjee S, Chow EJ, Park S, Kong Y. Neomycin improves constipation-predominant irritable bowel syndrome in a fashion that is dependent on the presence of methane gas: subanalysis of a double-blind randomized controlled study. Dig Dis Sci. 2006;51:1297–1301. doi: 10.1007/s10620-006-9104-6. [DOI] [PubMed] [Google Scholar]
- 102.Robins GW, Wellington K. Rifaximin: a review of its use in the management of traveller’s diarrhoea. Drugs. 2005;65:1697–1713. doi: 10.2165/00003495-200565120-00011. [DOI] [PubMed] [Google Scholar]
- 103.Sharara AI, Aoun E, Abdul-Baki H, Mounzer R, Sidani S, Elhajj I. A randomized double-blind placebo-controlled trial of rifaximin in patients with abdominal bloating and flatulence. Am J Gastroenterol. 2006;101:326–333. doi: 10.1111/j.1572-0241.2006.00458.x. [DOI] [PubMed] [Google Scholar]
- 104.Pimentel M, Park S, Mirocha J, Kane SV, Kong Y. The effect of a nonabsorbed oral antibiotic (rifaximin) on the symptoms of the irritable bowel syndrome: a randomized trial. Ann Intern Med. 2006;145:557–563. doi: 10.7326/0003-4819-145-8-200610170-00004. [DOI] [PubMed] [Google Scholar]
- 105.Pimentel M, Lembo A, Chey WD, Zakko S, Ringel Y, Yu J, Mareya SM, Shaw AL, Bortey E, Forbes WP. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364:22–32. doi: 10.1056/NEJMoa1004409. [DOI] [PubMed] [Google Scholar]
- 106.Menees SB, Maneerattannaporn M, Kim HM, Chey WD. The efficacy and safety of rifaximin for the irritable bowel syndrome: a systematic review and meta-analysis. Am J Gastroenterol. 2012;107:28–35; quiz 36. doi: 10.1038/ajg.2011.355. [DOI] [PubMed] [Google Scholar]
- 107.Clouse RE, Alpers DH, Hockenbery DM, DeSchryver-Kecskemeti K. Pericrypt eosinophilic enterocolitis and chronic diarrhea. Gastroenterology. 1992;103:168–176. doi: 10.1016/0016-5085(92)91110-p. [DOI] [PubMed] [Google Scholar]
- 108.Corinaldesi R, Stanghellini V, Cremon C, Gargano L, Cogliandro RF, De Giorgio R, Bartesaghi G, Canovi B, Barbara G. Effect of mesalazine on mucosal immune biomarkers in irritable bowel syndrome: a randomized controlled proof-of-concept study. Aliment Pharmacol Ther. 2009;30:245–252. doi: 10.1111/j.1365-2036.2009.04041.x. [DOI] [PubMed] [Google Scholar]
- 109.Andrews CN, Griffiths TA, Kaufman J, Vergnolle N, Surette MG, Rioux KP. Mesalazine (5-aminosalicylic acid) alters faecal bacterial profiles, but not mucosal proteolytic activity in diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2011;34:374–383. doi: 10.1111/j.1365-2036.2011.04732.x. [DOI] [PubMed] [Google Scholar]
- 110.Tuteja AK, Fang JC, Al-Suqi M, Stoddard GJ, Hale DC. Double-blind placebo-controlled study of mesalamine in post-infective irritable bowel syndrome--a pilot study. Scand J Gastroenterol. 2012;47:1159–1164. doi: 10.3109/00365521.2012.694903. [DOI] [PubMed] [Google Scholar]
- 111.Chey WY, Jin HO, Lee MH, Sun SW, Lee KY. Colonic motility abnormality in patients with irritable bowel syndrome exhibiting abdominal pain and diarrhea. Am J Gastroenterol. 2001;96:1499–1506. doi: 10.1111/j.1572-0241.2001.03804.x. [DOI] [PubMed] [Google Scholar]
- 112.Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108–2131. doi: 10.1053/gast.2002.37095. [DOI] [PubMed] [Google Scholar]
- 113.Clemens CH, Samsom M, Roelofs JM, van Berge Henegouwen GP, Smout AJ. Association between pain episodes and high amplitude propagated pressure waves in patients with irritable bowel syndrome. Am J Gastroenterol. 2003;98:1838–1843. doi: 10.1111/j.1572-0241.2003.07541.x. [DOI] [PubMed] [Google Scholar]
- 114.Poynard T, Regimbeau C, Benhamou Y. Meta-analysis of smooth muscle relaxants in the treatment of irritable bowel syndrome. Aliment Pharmacol Ther. 2001;15:355–361. doi: 10.1046/j.1365-2036.2001.00937.x. [DOI] [PubMed] [Google Scholar]
- 115.Jailwala J, Imperiale TF, Kroenke K. Pharmacologic treatment of the irritable bowel syndrome: a systematic review of randomized, controlled trials. Ann Intern Med. 2000;133:136–147. doi: 10.7326/0003-4819-133-2-200007180-00013. [DOI] [PubMed] [Google Scholar]
- 116.Talley NJ. Drug therapy options for patients with irritable bowel syndrome. Am J Manag Care. 2001;7:S261–S267. [PubMed] [Google Scholar]
- 117.Darvish-Damavandi M, Nikfar S, Abdollahi M. A systematic review of efficacy and tolerability of mebeverine in irritable bowel syndrome. World J Gastroenterol. 2010;16:547–553. doi: 10.3748/wjg.v16.i5.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Everitt H, Moss-Morris R, Sibelli A, Tapp L, Coleman N, Yardley L, Smith P, Little P. Management of irritable bowel syndrome in primary care: the results of an exploratory randomised controlled trial of mebeverine, methylcellulose, placebo and a self-management website. BMC Gastroenterol. 2013;13:68. doi: 10.1186/1471-230X-13-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Evangelista S. Quaternary ammonium derivatives as spasmolytics for irritable bowel syndrome. Curr Pharm Des. 2004;10:3561–3568. doi: 10.2174/1381612043382972. [DOI] [PubMed] [Google Scholar]
- 120.Evangelista S, Giachetti A, Chapelain B, Neliat G, Maggi CA. Receptor binding profile of Otilonium bromide. Pharmacol Res. 1998;38:111–117. doi: 10.1006/phrs.1998.0340. [DOI] [PubMed] [Google Scholar]
- 121.Lindqvist S, Hernon J, Sharp P, Johns N, Addison S, Watson M, Tighe R, Greer S, Mackay J, Rhodes M, et al. The colon-selective spasmolytic otilonium bromide inhibits muscarinic M(3) receptor-coupled calcium signals in isolated human colonic crypts. Br J Pharmacol. 2002;137:1134–1142. doi: 10.1038/sj.bjp.0704942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Battaglia G, Morselli-Labate AM, Camarri E, Francavilla A, De Marco F, Mastropaolo G, Naccarato R. Otilonium bromide in irritable bowel syndrome: a double-blind, placebo-controlled, 15-week study. Aliment Pharmacol Ther. 1998;12:1003–1010. doi: 10.1046/j.1365-2036.1998.00397.x. [DOI] [PubMed] [Google Scholar]
- 123.Baldi F, Longanesi A, Blasi A, Monello S, Cestari R, Missale G, Corazziari E, Badiali G, Pescatori M, Anastasio G. Clinical and functional evaluation of the efficacy of otilonium bromide: a multicenter study in Italy. Ital J Gastroenterol. 1991;23:60–63. [PubMed] [Google Scholar]
- 124.Ford AC, Talley NJ, Spiegel BM, Foxx-Orenstein AE, Schiller L, Quigley EM, Moayyedi P. Effect of fibre, antispasmodics, and peppermint oil in the treatment of irritable bowel syndrome: systematic review and meta-analysis. BMJ. 2008;337:a2313. doi: 10.1136/bmj.a2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Clavé P, Acalovschi M, Triantafillidis JK, Uspensky YP, Kalayci C, Shee V, Tack J. Randomised clinical trial: otilonium bromide improves frequency of abdominal pain, severity of distention and time to relapse in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2011;34:432–442. doi: 10.1111/j.1365-2036.2011.04730.x. [DOI] [PubMed] [Google Scholar]
- 126.Ford AC, Moayyedi P. Meta-analysis: factors affecting placebo response rate in the irritable bowel syndrome. Aliment Pharmacol Ther. 2010;32:144–158. doi: 10.1111/j.1365-2036.2010.04328.x. [DOI] [PubMed] [Google Scholar]
- 127.Chang FY, Lu CL, Luo JC, Chen TS, Chen MJ, Chang HJ. The evaluation of otilonium bromide treatment in asian patients with irritable bowel syndrome. J Neurogastroenterol Motil. 2011;17:402–410. doi: 10.5056/jnm.2011.17.4.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Fukushima Y, Suzuki H, Matsuzaki J, Kiyosue A, Hibi T. Efficacy of Solifenacin on Irritable Bowel Syndrome With Diarrhea: Open-label Prospective Pilot Trial. J Neurogastroenterol Motil. 2012;18:317–323. doi: 10.5056/jnm.2012.18.3.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Mizuta Y, Takahashi T, Owyang C. Nitrergic regulation of colonic transit in rats. Am J Physiol. 1999;277:G275–G279. doi: 10.1152/ajpgi.1999.277.2.G275. [DOI] [PubMed] [Google Scholar]
- 130.Luo ZD, Cizkova D. The role of nitric oxide in nociception. Curr Rev Pain. 2000;4:459–466. doi: 10.1007/s11916-000-0070-y. [DOI] [PubMed] [Google Scholar]
- 131.Fritz E, Hammer J, Schmidt B, Eherer AJ, Hammer HF. Stimulation of the nitric oxide-guanosine 3’, 5’-cyclic monophosphate pathway by sildenafil: effect on rectal muscle tone, distensibility, and perception in health and in irritable bowel syndrome. Am J Gastroenterol. 2003;98:2253–2260. doi: 10.1111/j.1572-0241.2003.07661.x. [DOI] [PubMed] [Google Scholar]
- 132.Gonçalves de Medeiros MT, de Oliveira RB, dos Santos AA, de Leopoldino DM, Lima MC, Nobre RA, Nobre e Souza MÂ. The effects of sildenafil on rectal sensitivity and tone in patients with the irritable bowel syndrome. Aliment Pharmacol Ther. 2012;35:577–586. doi: 10.1111/j.1365-2036.2011.04977.x. [DOI] [PubMed] [Google Scholar]
- 133.Holzer P. Opioid receptors in the gastrointestinal tract. Regul Pept. 2009;155:11–17. doi: 10.1016/j.regpep.2009.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Wade PR, Palmer JM, McKenney S, Kenigs V, Chevalier K, Moore BA, Mabus JR, Saunders PR, Wallace NH, Schneider CR, et al. Modulation of gastrointestinal function by MuDelta, a mixed µ opioid receptor agonist/ µ opioid receptor antagonist. Br J Pharmacol. 2012;167:1111–1125. doi: 10.1111/j.1476-5381.2012.02068.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Dove LS, Lembo A, Randall CW, Fogel R, Andrae D, Davenport JM, McIntyre G, Almenoff JS, Covington PS. Eluxadoline benefits patients with irritable bowel syndrome with diarrhea in a phase 2 study. Gastroenterology. 2013;145:329–338.e1. doi: 10.1053/j.gastro.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 136.Mangel AW, Bornstein JD, Hamm LR, Buda J, Wang J, Irish W, Urso D. Clinical trial: asimadoline in the treatment of patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2008;28:239–249. doi: 10.1111/j.1365-2036.2008.03730.x. [DOI] [PubMed] [Google Scholar]
- 137.Howlett AC, Barth F, Bonner TI, Cabral G, Casellas P, Devane WA, Felder CC, Herkenham M, Mackie K, Martin BR, et al. International Union of Pharmacology. XXVII. Classification of cannabinoid receptors. Pharmacol Rev. 2002;54:161–202. doi: 10.1124/pr.54.2.161. [DOI] [PubMed] [Google Scholar]
- 138.Esfandyari T, Camilleri M, Busciglio I, Burton D, Baxter K, Zinsmeister AR. Effects of a cannabinoid receptor agonist on colonic motor and sensory functions in humans: a randomized, placebo-controlled study. Am J Physiol Gastrointest Liver Physiol. 2007;293:G137–G145. doi: 10.1152/ajpgi.00565.2006. [DOI] [PubMed] [Google Scholar]
- 139.Wong BS, Camilleri M, Busciglio I, Carlson P, Szarka LA, Burton D, Zinsmeister AR. Pharmacogenetic trial of a cannabinoid agonist shows reduced fasting colonic motility in patients with nonconstipated irritable bowel syndrome. Gastroenterology. 2011;141:1638–1647.e1-7. doi: 10.1053/j.gastro.2011.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hellström PM, Grybäck P, Jacobsson H. The physiology of gastric emptying. Best Pract Res Clin Anaesthesiol. 2006;20:397–407. doi: 10.1016/j.bpa.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 141.Hellström PM, Näslund E, Edholm T, Schmidt PT, Kristensen J, Theodorsson E, Holst JJ, Efendic S. GLP-1 suppresses gastrointestinal motility and inhibits the migrating motor complex in healthy subjects and patients with irritable bowel syndrome. Neurogastroenterol Motil. 2008;20:649–659. doi: 10.1111/j.1365-2982.2007.01079.x. [DOI] [PubMed] [Google Scholar]
- 142.Brubaker PL, Drucker DJ, Asa SL, Swallow C, Redston M, Greenberg GR. Prolonged gastrointestinal transit in a patient with a glucagon-like peptide (GLP)-1- and -2-producing neuroendocrine tumor. J Clin Endocrinol Metab. 2002;87:3078–3083. doi: 10.1210/jcem.87.7.8584. [DOI] [PubMed] [Google Scholar]
- 143.Hellström PM, Hein J, Bytzer P, Björnssön E, Kristensen J, Schambye H. Clinical trial: the glucagon-like peptide-1 analogue ROSE-010 for management of acute pain in patients with irritable bowel syndrome: a randomized, placebo-controlled, double-blind study. Aliment Pharmacol Ther. 2009;29:198–206. doi: 10.1111/j.1365-2036.2008.03870.x. [DOI] [PubMed] [Google Scholar]
- 144.Camilleri M, Vazquez-Roque M, Iturrino J, Boldingh A, Burton D, McKinzie S, Wong BS, Rao AS, Kenny E, Månsson M, et al. Effect of a glucagon-like peptide 1 analog, ROSE-010, on GI motor functions in female patients with constipation-predominant irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2012;303:G120–G128. doi: 10.1152/ajpgi.00076.2012. [DOI] [PubMed] [Google Scholar]
- 145.Klooker TK, Braak B, Koopman KE, Welting O, Wouters MM, van der Heide S, Schemann M, Bischoff SC, van den Wijngaard RM, Boeckxstaens GE. The mast cell stabiliser ketotifen decreases visceral hypersensitivity and improves intestinal symptoms in patients with irritable bowel syndrome. Gut. 2010;59:1213–1221. doi: 10.1136/gut.2010.213108. [DOI] [PubMed] [Google Scholar]
- 146.Santos J, Alonso C, Guilarte M, Vicario M, Malagelada JR. Targeting mast cells in the treatment of functional gastrointestinal disorders. Curr Opin Pharmacol. 2006;6:541–546. doi: 10.1016/j.coph.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 147.Piche T, Saint-Paul MC, Dainese R, Marine-Barjoan E, Iannelli A, Montoya ML, Peyron JF, Czerucka D, Cherikh F, Filippi J, et al. Mast cells and cellularity of the colonic mucosa correlated with fatigue and depression in irritable bowel syndrome. Gut. 2008;57:468–473. doi: 10.1136/gut.2007.127068. [DOI] [PubMed] [Google Scholar]
- 148.Barbara G, Stanghellini V, De Giorgio R, Cremon C, Cottrell GS, Santini D, Pasquinelli G, Morselli-Labate AM, Grady EF, Bunnett NW, et al. Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology. 2004;126:693–702. doi: 10.1053/j.gastro.2003.11.055. [DOI] [PubMed] [Google Scholar]
- 149.Park JH, Rhee PL, Kim HS, Lee JH, Kim YH, Kim JJ, Rhee JC. Mucosal mast cell counts correlate with visceral hypersensitivity in patients with diarrhea predominant irritable bowel syndrome. J Gastroenterol Hepatol. 2006;21:71–78. doi: 10.1111/j.1440-1746.2005.04143.x. [DOI] [PubMed] [Google Scholar]


