Abstract
OBJECTIVE
We examine differences in prevalence of diabetes and rates of awareness and control among adults from diverse Hispanic/Latino backgrounds in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL).
RESEARCH DESIGN AND METHODS
The HCHS/SOL, a prospective, multicenter, population-based study, enrolled from four U.S. metropolitan areas from 2008 to 2011 16,415 18–74-year-old people of Hispanic/Latino descent. Diabetes was defined by either fasting plasma glucose, impaired glucose tolerance 2 h after a glucose load, glycosylated hemoglobin (A1C), or documented use of hypoglycemic agents (scanned medications).
RESULTS
Diabetes prevalence varied from 10.2% in South Americans and 13.4% in Cubans to 17.7% in Central Americans, 18.0% in Dominicans and Puerto Ricans, and 18.3% in Mexicans (P < 0.0001). Prevalence related positively to age (P < 0.0001), BMI (P < 0.0001), and years living in the U.S. (P = 0.0010) but was negatively related to education (P = 0.0005) and household income (P = 0.0043). Rate of diabetes awareness was 58.7%, adequate glycemic control (A1C <7%, 53 mmol/mol) was 48.0%, and having health insurance among those with diabetes was 52.4%.
CONCLUSIONS
Present findings indicate a high prevalence of diabetes but considerable diversity as a function of Hispanic background. The low rates of diabetes awareness, diabetes control, and health insurance in conjunction with the negative associations between diabetes prevalence and both household income and education among Hispanics/Latinos in the U.S. have important implications for public health policies.
Introduction
The Centers for Disease Control and Prevention (CDC) has reported that the prevalence of diabetes (self-reported and undiagnosed) in the U.S. is 10.2% for non-Hispanic whites aged 20 years or older and 18.7% for non-Hispanic blacks of the same age (1). According to the CDC, sufficient data are not yet available to estimate the total prevalence of diabetes for other U.S. racial/ethnic minority populations. This includes the 50.5 million Hispanics/Latinos who comprise 16% of the U.S. population (2). In part because of the gap in information about Hispanic/Latino health, the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) was launched by the National Heart, Lung, and Blood Institute (NHLBI) and six other institutes, centers, and offices of the National Institutes of Health to examine the prevalence and development of chronic diseases, including diabetes, among people of diverse Hispanic/Latino backgrounds living in the U.S.
Although the CDC indicated that there was insufficient information to provide a prevalence estimate for diabetes in Hispanic/Latinos, they did cite data concerning self-reported diabetes in this population obtained from 2007–2009 by the National Health Interview Survey (NHIS) (1). This study indicated that after age adjustment, 7.1% of non-Hispanic whites, 8.4% of Asian Americans, 11.8% of Hispanics/Latinos, and 12.6% of non-Hispanic blacks self-reported having diabetes. There was considerable diversity among Hispanics/Latinos, as rates for Cubans and Central and South Americans were both 7.6%, whereas the rate was 13.3% for Mexican Americans and 13.8% for Puerto Ricans. However, national prevalence estimates for Cubans, Central and South Americans, and Puerto Ricans are less precise than they are for Mexican Americans, as indicated by the relatively large SEs for the estimates (3). In the HCHS/SOL, it was possible to obtain more precise prevalence estimates for the various Hispanic/Latino groups using objective criteria for assessing diabetes. The aim of this article is to describe the prevalence of diabetes in U.S. Hispanics/Latinos from diverse Hispanic backgrounds. Further, we describe the prevalence of diabetes in the HCHS/SOL by age, sex, BMI, length of time living in the U.S. and socioeconomic status. Among these participants with diabetes, we present data on diabetes awareness, glycemic control, and health insurance.
Research Design and Methods
The HCHS/SOL is a study of 16,415 women and men aged 18–74 years at screening from randomly selected households recruited during 2008–2011 from Bronx, NY; Chicago, IL; Miami-Dade County, FL; and San Diego, CA. The HCHS/SOL cohort was selected through a stratified multistage area probability sample of four communities (4). The selected communities are diverse regions of the U.S., from 4 of the 11 urban metropolitan areas with the largest number of Hispanics/Latinos (5). Even though the target population for the HCHS/SOL is the four selected communities, not the entire U.S. Hispanic/Latino population, each community has high concentrations of specific Hispanic/Latino backgrounds, allowing the study to estimate prevalence of diseases and risk factors for each background. In order to obtain diabetes prevalence estimates taking into account age, sex, and Hispanic background distribution, nonresponse adjusted, trimmed, and calibrated weights were used to approximate the census 2010 target population (2). The age, sex, and Hispanic background distributions based on the sampling weighted estimates are very similar to the census 2010 target population, with the differences less than 1.6% and in most cases less than 0.45%.
Population-based sampling was used to identify and recruit HCHS/SOL participants (4). Rosters of eligible participants were generated for each household sampled, and eligibility screening took place through telephone calls or in-person visits. Eligible participants were community-dwelling adults who self-identified as Hispanic or Latino, were able to travel to a local field center for examination, were not on active military duty or pregnant, and did not plan to move from the study area within 3 years. Census tracts were selected to provide an adequate number of Hispanics/Latinos that included diversity in socioeconomic status and study-wide diversity in Hispanic/Latino background. The rostered, eligible individuals were further sampled within age strata so that there were 9,714 participants aged 45–74 years (59%) and 6,701 participants aged 18–44 years (41%). Of screened individuals who were eligible, 42% were enrolled. All participants provided informed consent, and the study had institutional review board approval from each institution participating in the study.
Study Procedures
Each participant had a clinical examination that included completion of clinical assessments and questionnaires and measurement of height and weight (6). The study used standardized instruments to determine information about health behaviors, medical history, and demographics. Study procedures included a 2-h oral glucose tolerance test (OGTT) except for those who had fasting plasma glucose (FPG) >150 mg/dL and those reporting being previously diagnosed with diabetes. Participants were required to fast for at least 8 h prior to the visit, consuming only water and necessary medications. Venous blood specimens were collected, processed, and frozen on site toward the beginning of the visit and also 2 h after a 75 g glucose load. Plasma glucose was assessed using a hexokinase enzymatic method (Roche Diagnostics Corporation, Indianapolis, IN). Glycosylated hemoglobin (A1C) was measured in EDTA whole blood using a Tosoh G7 automated high-performance liquid chromatography analyzer (Tosoh Bioscience Inc., San Francisco, CA). Throughout the 3-year exam period, collection of blinded repeat blood samples and repeated random measurements of clinical procedures were used as quality control procedures.
Self-report obtained by interview with certified assessors was used to define personal and family history of medical diagnoses such as diabetes; being aware of diabetes; and demographic variables, including age, sex, Hispanic/Latino background, income, education, and length of residence in the U.S. (but not territories). Height and weight were measured to the nearest 1.0 cm and 0.1 kg, respectively, with participants wearing light clothing. BMI was calculated as kg/m2. Inventory methods were used to list all currently used medications. Diabetes was defined as either FPG ≥126 mg/dL (7 mmol/L), a 2-h postload glucose level (2-h OGTT) ≥200 mg/dL (11.2 mmol/L), A1C level ≥6.5% (48 mmol/mol), or documented use of hypoglycemic agents (scanned medications). The American Diabetes Association goal for A1C level of <7.0% (53 mmol/mol) was used to define glycemic control.
Statistical Analyses
Statistical analyses were conducted upon 16,385 participants with nonmissing diabetes data. Descriptive characteristics, age standardized to the 2010 U.S. population, were computed by sex and for all participants by Hispanic/Latino background. All reported prevalence values were weighted to adjust for sampling probability and nonresponse, trimming to handle extreme values of the weights, and calibration to the known population distribution (4). Statistical analyses examined the prevalence of diabetes by sex, age, Hispanic background, field center, BMI, education, household income, and years living in the U.S. and determined rates of diabetes awareness, glycemic control, and health insurance status as well. Logistic regression models were analyzed and included the variables of interest adjusted for selected covariates. Statistical tests were two-sided at a significance level of 0.05, but adjustments were not made for multiple comparisons. All analyses were performed using SAS version 9.2 (SAS Institute) and SUDAAN release 10.0.0 (RTI).
Results
The prevalence of diabetes by Hispanic/Latino background, sex, age, and BMI assessed at the baseline exam by objective measures (FPG, 2-h OGTT, A1C, or scanned medications) are shown in Table 1. Because some epidemiological studies, including the National Health and Nutrition’s Examination Survey (NHANES), used self-report to estimate diabetes prevalence, we provide diabetes prevalence data in part derived from self-report in Supplementary Table 1. Total prevalence of diabetes in persons aged 18–74 years (Table 1) was 16.9%. The unweighted prevalence of diabetes in the HCHS/SOL was 19.6%, including 3,211 of 16,385 participants having diabetes. Weighted prevalence for diabetes was similar for men and women after controlling for age, BMI, Hispanic background, field center, and years lived in the U.S. (men = 15.3%; women = 14.2%; P = 0.0941).
Table 1.
Prevalence of diabetes by sex, Hispanic/Latino background, age, and BMI
| Men and women |
Women |
Men |
||||
|---|---|---|---|---|---|---|
| Sample size | Prevalence (95% CI) | Sample size | Prevalence (95% CI) | Sample size | Prevalence (95% CI) | |
| Overall | 16,385 | 16.9 (16.11–17.69) | 9,820 | 17.1 (16.16–18.19) | 6,565 | 16.5 (15.41–17.71) |
| Hispanic background | ||||||
| Dominican | 1,470 | 18.1 (16.21–20.13) | 961 | 18.2 (15.60–21.08) | 509 | 18.0 (14.83–21.71) |
| Central American | 1,730 | 17.7 (15.36–20.22) | 1,047 | 18.5 (15.59–21.82) | 683 | 16.9 (13.75–20.57) |
| Cuban | 2,347 | 13.4 (12.03–14.91) | 1,249 | 13.5 (11.64–15.55) | 1,098 | 13.2 (11.45–15.14) |
| Mexican | 6,466 | 18.3 (16.84–19.86) | 4,018 | 17.9 (16.18–19.74) | 2,448 | 18.7 (16.32–21.33) |
| Puerto Rican | 2,719 | 18.1 (16.30–19.98) | 1,586 | 19.5 (16.98–22.23) | 1,133 | 16.6 (14.31–19.27) |
| South American | 1,070 | 10.2 (8.36–12.29) | 634 | 9.8 (7.73–12.36) | 436 | 10.6 (7.85–14.09) |
| Mixed/other | 502 | 21.2 (15.74–27.88) | 276 | 22.1 (14.92–31.49) | 226 | 19.6 (13.64–27.29) |
| Missing | 81 | 57.4 (46.58–67.57) | 49 | 64.3 (51.10–75.62) | 32 | 43.1 (30.36–56.92) |
| Age group, years | ||||||
| 18–29 | 2,675 | 2.6 (1.93–3.36) | 1,427 | 2.9 (1.98–4.11) | 1,248 | 2.2 (1.49–3.38) |
| 30–39 | 2,389 | 6.7 (5.49–8.15) | 1,384 | 6.4 (4.94–8.31) | 1,005 | 7.0 (5.23–9.28) |
| 40–49 | 4,204 | 14.1 (12.64–15.69) | 2,573 | 14.5 (12.68–16.59) | 1,631 | 13.6 (11.50–16.07) |
| 50–59 | 4,330 | 25.0 (23.06–27.09) | 2,727 | 26.2 (23.47–29.08) | 1,603 | 23.6 (21.03–26.32) |
| 60–69 | 2,287 | 38.7 (35.64–41.79) | 1,396 | 37.3 (33.44–41.28) | 891 | 40.3 (36.00–44.73) |
| 70–74 | 500 | 48.6 (41.57–55.64) | 313 | 51.3 (42.17–60.36) | 187 | 44.3 (34.67–54.34) |
| BMI, kg/m2 | ||||||
| <25 | 3,317 | 9.8 (8.56–11.24) | 1,942 | 9.5 (7.90–11.42) | 1,375 | 10.2 (8.33–12.52) |
| ≥25 < 30 | 6,108 | 14.2 (13.10–15.35) | 3,375 | 13.5 (11.98–15.12) | 2,733 | 15.0 (13.39–16.67) |
| ≥30 | 6,897 | 22.4 (21.08–23.69) | 4,470 | 23.1 (21.39–24.89) | 2,427 | 21.4 (19.49–23.41) |
| Missing | 63 | 31.3 (20.36–44.88) | 33 | 31.9 (18.27–49.49) | 30 | 33.6 (21.79–47.83) |
Diabetes is based on FPG, 2-h OGTT, A1C, or scanned medications. Values except sample size are weighted for study design and nonresponse, and age is standardized to Census 2010 U.S. population.
In Table 1, the lowest prevalence estimates based on objective measurements of HCHS/SOL participants were for South Americans (10.2%) and Cubans (13.4%). Central Americans (17.7%), Dominicans (18.0%), Puerto Ricans (18.0%), and Mexicans (18.3%) had notably higher rates of diabetes. Differences in diabetes prevalence as a function of Hispanic/Latino background remained significant after adjusting for age, sex, BMI, field center, and years lived in the U.S. (P < 0.0001). Diabetes prevalence increased with age from 2.6% for those aged 18–29 years to 48.4% in those 70–74 years. Differences in diabetes as a function of age were significant after adjusting for sex, BMI, Hispanic/Latino background, field center, and years lived in the U.S. (P < 0.0001). Diabetes prevalence similarly increased as a function of BMI from 9.8% in those with BMI <25 kg/m2 to 22.3% in those with BMI ≥30 kg/m2. The difference in diabetes prevalence as a function of BMI remained significant after adjusting for age, sex, Hispanic/Latino background, field center, and years lived in the U.S. (P < 0.0001).
At the baseline exam, 11.9% of women and men reported having previously been diagnosed with diabetes, whereas 6.2% of participants were newly classified as having diabetes on the basis of FPG, 2-h OGTT, A1C, or scanned hypoglycemic medications.
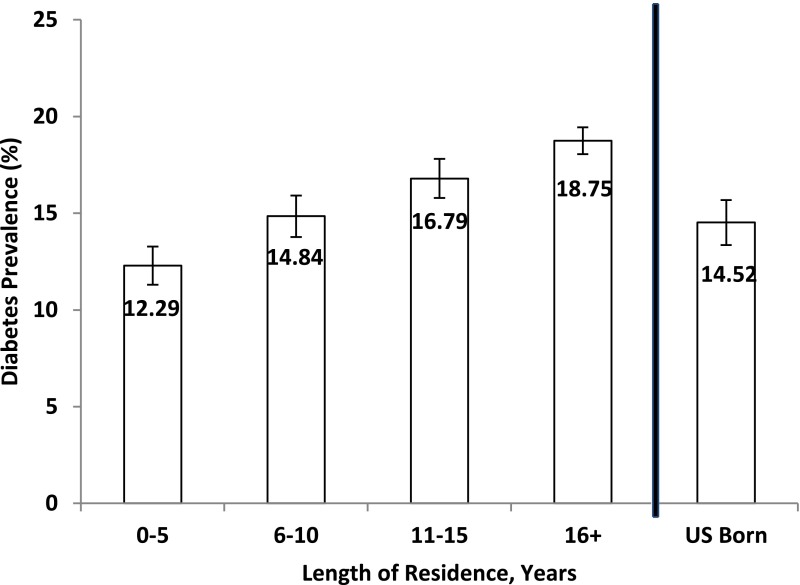
The prevalence of diabetes was significantly related to length of residence in the U.S. (Fig. 1) after adjustment for age and sex (P = 0.0010); 11.8% of those with diabetes were born in the U.S. After adjustment for age, sex, BMI, Hispanic background, and field center, those living in the U.S. for 5 years or less did not differ significantly from those born in the U.S. (P = 0.8551), whereas those living 10 or more years in the U.S. did differ significantly from those born in the U.S. (P = 0.0162) or who lived in the U.S. for 10 years or less (P = 0.0232).
Figure 1.
Prevalence (and SE) of diabetes related to length of residence in the U.S. or being born in the U.S. Data are weighted and age standardized using the 2010 U.S. population census.
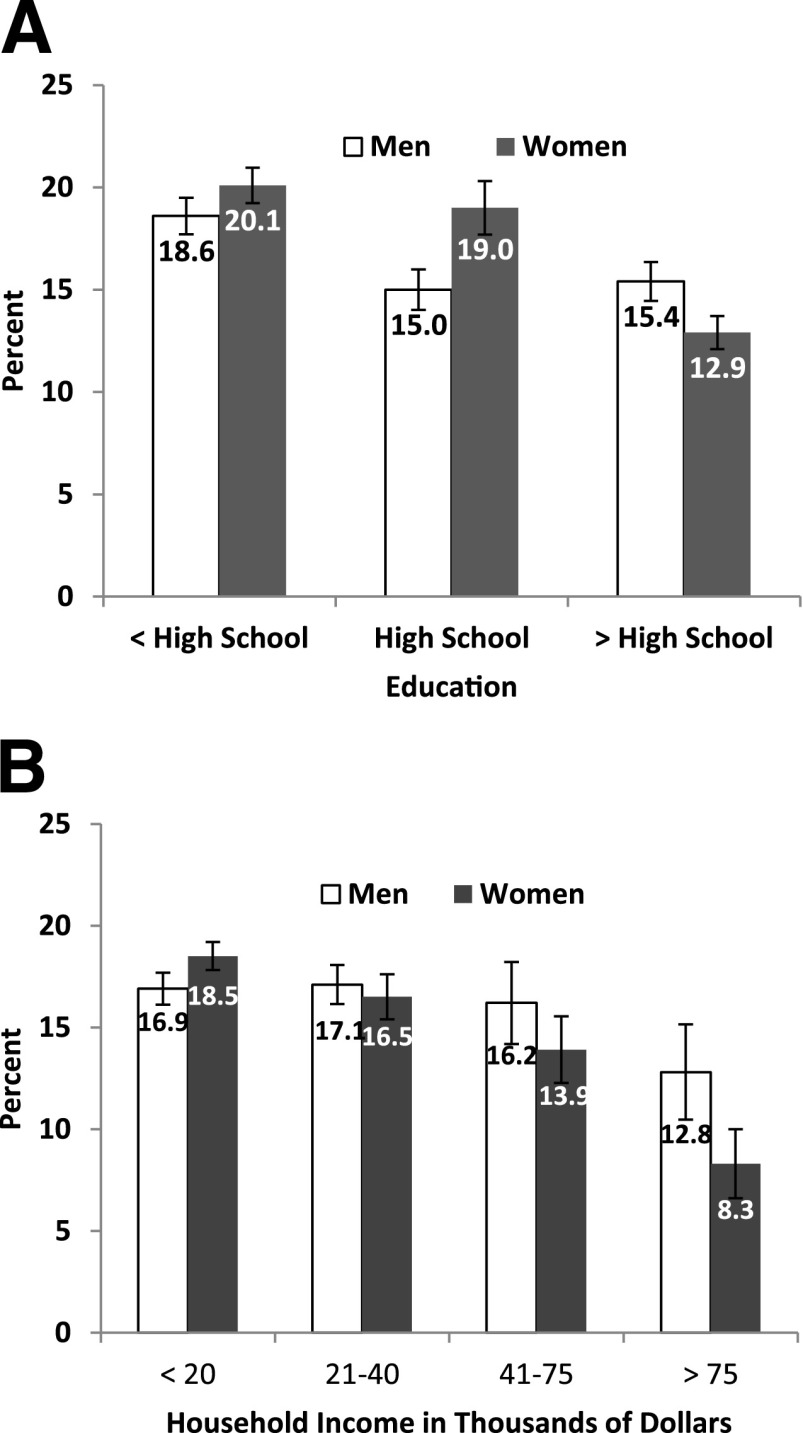
Women with more than a high school education had a lower prevalence of diabetes than those having a high school education or less; men who had at least a high school education had a lower prevalence of diabetes than men with less than a high school education (Fig. 2A). The negative association of diabetes prevalence with education remained statistically significant after adjusting for age, sex, BMI, Hispanic/Latino background, field center, and length of residence in the U.S. (P = 0.0005). Similarly, women from higher-income households had a lower prevalence of diabetes than women from lower-income households, but the gradient relating prevalence of diabetes to household income was less steep for men (Fig. 2B). After adjustments for age, sex, BMI, Hispanic/Latino background, field center, and length of time living in the U.S., the negative association of diabetes prevalence with household income was statistically significant (P = 0.0043); the interaction for household income and sex was not (P = 0.4411).
Figure 2.
Prevalence (and SE) of diabetes related to (A) education and (B) household income. Data are weighted and age standardized using 2010 U.S. population census.
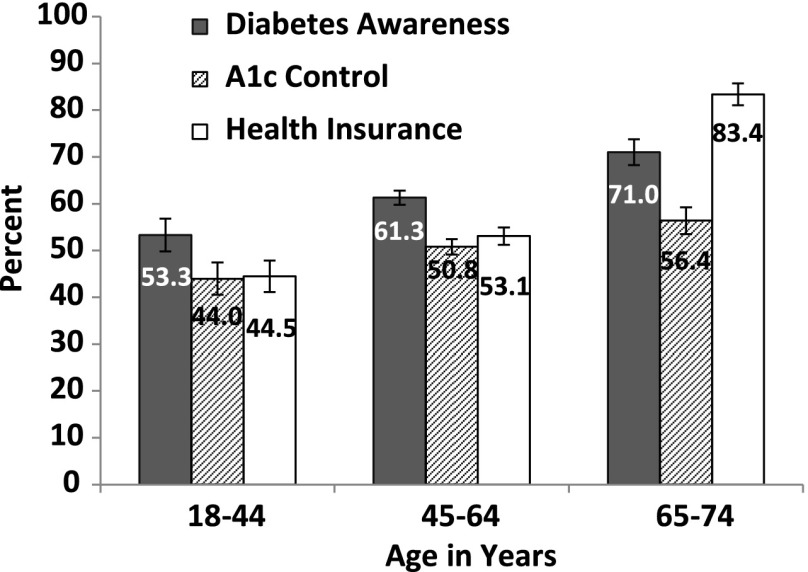
Among HCHS/SOL participants with objectively defined diabetes, 58.7% indicated awareness of their condition, 48% displayed adequate diabetes control (A1C <7%; 53 mmol/mol), and 52.4% reported having health insurance. The rate of diabetes awareness, glycemic control, and having health insurance among participants in three age groups is shown in Fig. 3. After controlling for sex, Hispanic/Latino background, BMI, field center, education, and years living in the U.S., the percentage of participants with health insurance (P = 0.0001), diabetes awareness (P = 0.0011), and glycemic control (P = 0.0299) increased significantly with age.
Figure 3.
Rate (and SE) of health insurance, diabetes awareness, and A1C control among diabetic participants with diabetes in three age groups. Data are weighted and age standardized using 2010 U.S. population census.
After controlling for the same variables, those 65 years and older revealed greater rates of diabetes awareness (P = 0.0001), control (P = 0.0106), and insurance coverage (P = 0.0001) than those who were younger. Following adjustment for the same variables, individuals who were aware of their diabetes showed greater diabetes control than those who were unaware (P = 0.0001), and those who had health insurance were more likely to be aware than those who did not (P = 0.0001). Individuals with health insurance were less likely among all participants (5 vs. 6.5%) to present at the clinic exam with unrecognized diabetes (P = 0.0030).
Conclusions
The total prevalence of diabetes for persons aged 18–74 years was 16.9% and was similar in men and women. Significant differences in diabetes prevalence were related to Hispanic/Latino background. Based upon analyses of HCHS/SOL data, prevalence ranged from 10.2% in South Americans to 18.3% in Mexicans. Although using a somewhat different metric in persons 20 years or older from 2007–2009 and sex and age standardized to the 2000 U.S. population (our data are from 2008–2011 and age standardized to the 2010 U.S. population), the CDC has reported a prevalence estimate of 10.2% in non-Hispanic whites and 18.7% for non-Hispanic blacks (1). Thus the range of diabetes prevalence among Hispanics/Latinos appears to approximate the prevalence range between non-Hispanic whites and non-Hispanic blacks. Moreover, the diversity in diabetes prevalence across Hispanic/Latino heritage groups is consistent with there being other variations in cardiovascular disease risk factors observed among Hispanic/Latino-background groups in the HCHS/SOL (8).
The prevalence of diabetes self-reported at the HCHS/SOL baseline visit was 11.9%, and the prevalence recognized at baseline was 6.2%. Thus 34.3% of HCHS/SOL participants with diabetes were first detected at the baseline visit. This percentage of HCHS/SOL participants with diabetes first detected consequent to the clinic exam is comparable to the 37.5% of non-Hispanic whites first identified consequent to the NHANES clinic exam in 2005–2006, but age and sex standardized to the 2000 U.S. census (9), with the NHANES exam data based solely on FPG.
By merging the results of two earlier surveys, it was possible to compare estimates in the total prevalence of self-reported and undiagnosed diabetes among 20–74-year-old blacks, whites, Cuban Americans, Mexican Americans, and Puerto Ricans living in the U.S. (10). This was achieved by combining data analysis of the 1976–1980 NHANES study of blacks and whites and the Hispanic Health and Nutrition Examination Survey of 1982–1984 that examined Mexican Americans in the Southwest, Cuban Americans in Miami, and Puerto Ricans in New York City and surroundings. The combined study reported an age-standardized prevalence of diabetes of 6.2% in whites, 9.3% in Cubans, 10.2% in blacks, 13.0% in Mexican Americans, and 13.4% in Puerto Ricans. Although the prevalence of diabetes observed from 1976–1984 was far lower than that observed after 2007, the diversity of diabetes prevalence across racial/ethnic groups has continued and occurs in approximately the same rank order.
Prevalence of diabetes significantly increased in relation to length of residence in the U.S., both in the HCHS/SOL and in the 1997–2005 study by the NHIS (11). The HCHS/SOL, however, found that participants born in the U.S. did not differ significantly from those living in the U.S. for 5 years or less but did differ reliably from those living in the U.S. for more than 10 years. The present findings therefore are not consistent with the report that immigrants to the U.S. are healthier than U.S.-born people of similar ethnic background (12) but is consistent with the finding that migrant health tends to become worse with increased duration living in the U.S. (13,14). A recent study conducted on NHANES data from 1988–1994 and 1999–2008 suggested that with regard to diabetes in Mexican Americans, the “healthy migrant effect” exists, although it is diminished when the differential in unrecognized diabetes between migrants and nonmigrants is taken into account (15). Thus people first coming to the U.S. were reported to have more undiagnosed diabetes than people born in the U.S. The HCHS/SOL did not observe this migrant advantage, and the diabetes prevalence related to length of residence in migrants was based solely on objective criteria.
The current study also found that prevalence of diabetes is negatively related to education and household income, and this association remains significant after adjustments for age, sex, BMI, Hispanic background, field center, and time living in the U.S. This is consistent with a large-scale meta-analysis of type 2 diabetes incidence and socioeconomic status carried out worldwide (16). The investigators found that risk of getting type 2 diabetes was associated with low socioeconomic status including education and income in high-, middle-, and low-income countries, but the relationship was strongest in high-income countries such as the U.S. In a study conducted using NHANES data from 2001–2006, which combined education and income to obtain an index of socioeconomic status, a strong inverse socioeconomic gradient of cardiovascular disease risk was found in all race/ethnicity groups except foreign-born Mexican American men (17). The study did not account for length of time participants lived in the U.S., however, and the analysis of Hispanics/Latinos was limited to Mexican Americans. In any event, findings from the HCHS/SOL confirm that negative associations exist between diabetes prevalence and both income and education.
Many people with diabetes in the current study were unaware of their diabetes (41.3%), had poor glycemic control (52.0% had A1C ≥7.0% [53 mmol/mol]), and/or lacked health insurance (47.9%). The rate of diabetes awareness, however, appears to be the same as those reported for non-Hispanic whites (9) and increased significantly with age. In contrast, the rate of adequate glycemic control (A1C < 7.0; <53 mmol/mol) for Hispanics/Latinos in the HCHS/SOL (48.0%) appears to be somewhat lower than those for non-Hispanic whites (52.9%) and non-Hispanic blacks (52.6%) observed in the NHANES for 2007–2010 (18). The rate of glycemic control for Hispanics/Latinos in the NHANES was 47.3%, which, together with the HCHS/SOL findings, suggests that fewer Hispanics/Latinos with diabetes have adequate glycemic control. Differences in health insurance and glycemic control increased with age and particularly for health insurance; these differences may have been due to Medicare enrollment. Although the HCHS/SOL enrolled a relatively small number of individuals between the ages of 65 and 74 years, participants 65 years and older were more likely to have health insurance and revealed better glycemic control than those who were younger. Interestingly, the percentage of Hispanic/Latino adults aged 18–64 years lacking health insurance in the NHIS for 2008 was 41.6% compared with 14.6% in non-Hispanic whites and 22.1% in non-Hispanic blacks (19). A meta-analysis comparing A1C levels between Hispanic/Latinos and non-Hispanic white adults with diabetes has reported that A1C was 0.5% (5.5 mmol/mol) higher in the Hispanic/Latino patients (20). Although the reasons for the disparity in glycemic control between whites and Hispanics/Latinos have not been investigated, the apparent similarity of diabetes awareness between non-Hispanic whites and Hispanics/Latinos in conjunction with a large disparity in health insurance between the groups suggests that the differences in health insurance and/or other aspects of access to health care (e.g., ability to meet copayments) may well account for the differences in glycemic control. This appears to be particularly important in terms of public health and clinical medicine, because a decrease of 0.5% (5.5 mmol/mol) in A1C is associated with a 10.5% decrease in risk of vascular complications (21).
Although a major strength of the HCHS/SOL was the use of population-based sampling strategies, it should be noted that of those eligible for the study, 42% chose to enroll. Because the study entailed a 6.5 h clinical exam and participants could not really be compensated for lost wages and child care, it was essential that the study design include statistical adjustment for nonresponse so that data estimates are representative of the communities from which participants were drawn. A further limitation of the study is that it did not differentiate type 1 from type 2 diabetes. However, study participants ranged in age from 18–74 years, with only 2.6% of those 18–29 years of age having diabetes. Consequently, one can surmise that the overwhelming percentage of participants with diabetes in the HCHS/SOL have type 2 diabetes.
The design of the HCHS/SOL has been conducive to the examination of variations in diabetes prevalence among specific Hispanic/Latino heritage groups living in the U.S., including Central Americans, Cubans, Dominicans, Mexicans, Puerto Ricans, and South Americans. This design is facilitating detailed, comprehensive examination in four large urban centers concerning the risk factors, health habits, and prevalence of several chronic diseases. Thus, for example, we have observed a differential prevalence in diabetes ranging from 10.2 to 18.3% among different Hispanic/Latino-background groups. However, a limitation of the HCHS/SOL is that its design does not provide for a representative sample of all Hispanic/Latino heritage groups in terms of their demography (e.g., rural versus urban background; Mexican Americans in Texas) and proportion of the total Hispanic/Latino and total U.S. population. According to the U.S. census, the U.S. Hispanic/Latino population in 2010 made up 16% of the total U.S. population and among Hispanics/Latinos included 63.0% Mexicans, 9.2% Puerto Ricans, 7.9% Central Americans, 5.5% South Americans, 3.5% Cubans, and 2.8% Dominicans (2). In order to make inferences about disparities in diabetes prevalence among Hispanics/Latinos living in the U.S. one must take two observations into account. The first finding is that diabetes prevalence ranged from 10.2 to 18.3% among heritage groups in the HCHS/SOL. The second observation is that four of these groups (Mexicans, Puerto Ricans, Central Americans, and Dominicans) all had prevalence rates above 18% and that these four groups make up 82.9% of the Hispanic/Latino population in the U.S. Thus the HCHS/SOL data document a large variation in diabetes prevalence among Hispanic/Latino heritage groups but are also consistent with previous findings that Hispanic/Latinos have a greater prevalence of diabetes than non-Hispanic whites (10,19).
The HCHS/SOL findings document a low rate of enrollment in health insurance plans among Hispanics/Latinos with diabetes together with a need for increasing awareness and glycemic control in Hispanics/Latinos with diabetes. Potential implications for public health policy, including need for increased access to health care, appear to be particularly important when one examines the present findings indicating a significant negative relationship between diabetes prevalence and household income. Interestingly, participants in the HCHS/SOL with diabetes who were 65 years or older were more likely to have health insurance and showed better glycemic control than younger participants with diabetes. Since those persons 65 years and older typically had modest household incomes, our results suggest that increasing access to health insurance and medical care for those under 65 years would likely improve both diagnosis of diabetes and glycemic control.
Supplementary Material
Article Information
Acknowledgments. The authors thank the more than 16,000 participants who generously gave of their time and provided the study data. The authors also thank the more than 250 staff members of the HCHS/SOL for their dedication and expertise. The study website is http://www.cscc.unc.edu/hchs/.
Funding. The HCHS/SOL was carried out as a collaborative study supported by contracts from the NHLBI to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following institutes/centers/offices contributed to the baseline HCHS/SOL funding period through a transfer of funds to the NHLBI: National Institute on Minority Health and Health Disparities, National Institute on Deafness and Other Communication Disorders, National Institute of Dental and Craniofacial Research, National Institute of Diabetes and Digestive and Kidney Diseases, National Institute of Neurological Disorders and Stroke, and National Institutes of Health Office of Dietary Supplements.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. N.S. researched the literature, interpreted data, and organized and wrote the manuscript. M.L., C.C.C., J.B., M.C., L.C.G., A.L.G., G.H., R.C.K., L.M.L., L.V.-C., and M.L.A.-S. contributed to the interpretation of data, were involved in manuscript preparation, and critically reviewed and edited the manuscript. Y.T. analyzed the data and was involved in manuscript preparation. N.S. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Preliminary data from this study were presented in a symposium at the 71st Scientific Sessions of the American Diabetes Association, San Diego, CA, 24–28 June 2011.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc13-2939/-/DC1.
A slide set summarizing this article is available online.
L.M.L. is currently affiliated with the Office of Biostatistics, Center for Drug Evaluations and Research, Food and Drug Administration, Silver Spring, MD.
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official position of the National Institutes of Health, the U.S. Department of Health and Human Services, or the federal government.
References
- 1.Centers for Disease Control and Prevention National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States. Atlanta, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2011 [Google Scholar]
- 2.U.S. Census Bureau Briefs The Hispanic Population. Washington, DC, U.S. Census Bureau, 2010 [Google Scholar]
- 3.Centers for Disease Control and Prevention. Age-adjusted percentage of civilian, noninstitutionalized population with diagnosed diabetes, Hispanics, United States, 1997–2011 [article online], 2013. Available from http://www.cdc.gov/diabetes/statistics/prev/national/figbyhispanic.htm Accessed 5 December 2013
- 4.Lavange LM, Kalsbeek WD, Sorlie PD, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol 2010;20:642–649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pew Research Hispanic Trends Project. Hispanic population in select U.S. metropolitan areas [article online], 2011. Available from http://www.pewhispanic.org/2013/08/29hispanic-population-in-select-U-S-metropolitan-areas-2011/ Accessed 29 August 2013
- 6.Sorlie PD, Avilés-Santa LM, Wassertheil-Smoller S, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol 2010;20:629–641 [DOI] [PMC free article] [PubMed]
- 7.Bays HE, Chapman RH, Grandy S, SHIELD Investigators’ Group The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: comparison of data from two national surveys. Int J Clin Pract 2007;61:737–747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daviglus ML, Talavera GA, Avilés-Santa ML, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA 2012;308:1775–1784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cowie CC, Rust KF, Ford ES, et al. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988-1994 and 2005-2006. Diabetes Care 2009;32:287–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris MI. Epidemiological correlates of NIDDM in Hispanics, whites, and blacks in the U.S. population. Diabetes Care 1991;14(Suppl. 3):639–648 [DOI] [PubMed] [Google Scholar]
- 11.Oza-Frank R, Stephenson R, Narayan KMV. Diabetes prevalence by length of residence among US immigrants. J Immigr Minor Health 2011;13:1–8 [DOI] [PubMed] [Google Scholar]
- 12.Singh GK, Siahpush M. All-cause and cause-specific mortality of immigrants and native born in the United States. Am J Public Health 2001;91:392–399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fuentes-Afflick E, Hessol NA, Pérez-Stable EJ. Testing the epidemiologic paradox of low birth weight in Latinos. Arch Pediatr Adolesc Med 1999;153:147–153 [DOI] [PubMed] [Google Scholar]
- 14.Rumbaut RG. Paradoxes (and orthodoxies) of assimilation. Sociol Perspect 1997;40:483–511 [Google Scholar]
- 15.Barcellos SH, Goldman DP, Smith JP. Undiagnosed disease, especially diabetes, casts doubt on some of reported health ‘advantage’ of recent Mexican immigrants. Health Aff (Millwood) 2012;31:2727–2737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol 2011;40:804–818 [DOI] [PubMed] [Google Scholar]
- 17.Karlamangla AS, Merkin SS, Crimmins EM, Seeman TE. Socioeconomic and ethnic disparities in cardiovascular risk in the United States, 2001-2006. Ann Epidemiol 2010;20:617–628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stark Casagrande S, Fradkin JE, Saydah SH, Rust KF, Cowie CC. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988-2010. Diabetes Care 2013;36:2271–2279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moonesinghe R, Zhu J, Truman BI; Centers for Disease Control and Prevention. Health insurance coverage - United States, 2004 and 2008. MMWR Surveill Summ 2011;60(Suppl.):35–37 [PubMed] [Google Scholar]
- 20.Kirk JK, Passmore LV, Bell RA, et al. Disparities in A1C levels between Hispanic and non-Hispanic white adults with diabetes: a meta-analysis. Diabetes Care 2008;31:240–246 [DOI] [PubMed] [Google Scholar]
- 21.Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000;321:405–412 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.