Abstract
Background
Recurrent pyogenic cholangitis (RPC) is common in Asia. Its management differs from centre to centre.
Methods
A retrospective review of 80 patients undergoing surgery for RPC was performed. Immediate and longterm outcomes were analysed.
Results
All patients underwent hepaticocutaneousjejunostomy (HCJ) for biliary drainage and stone removal. Additional hepatectomy was performed in 38 patients with intrahepatic ductal stricture or liver segmental atrophy. Twenty-three patients had residual stones and 25 had recurrent stones. All patients with residual stones underwent repeated choledochoscopy (median: four sessions) for stone removal and obtained confirmation of ductal clearance. Four patients developed cholangiocarcinoma, of which two died. The complication rate was 17.5%. Most of the complications were wound infections. No mortality related to surgery occurred. Multivariate analysis found that gender, disease extent (unilobar versus bilobar) and surgery type (HCJ alone versus HCJ with hepatectomy) were not associated with increased risk for residual or recurrent stones. A raised preoperative bilirubin level was the only risk factor identified as associated with an increased risk for recurrent stones (P < 0.001); it was not associated with an increased risk for residual stones.
Conclusions
Recurrent pyogenic cholangitis is a distinct disease, the management of which requires a high level of surgical expertise. Hepaticojejunostomy is recommended as the primary drainage procedure, but hepatectomy should be reserved for complicated RPC.
Introduction
Recurrent pyogenic cholangitis (RPC) is a disease characterized by the formation of intrabiliary pigmented stones, which results in the stricturing of the biliary tree followed by biliary obstruction and recurrent bouts of cholangitis. It is a peculiar disease entity usually found in Southeast Asia and was first described by Digby in 1930.1
In the 1950s, Queen Mary Hospital in Hong Kong received up to 50 new patients with RPC every year (Unpublished data from Queen Mary Hospital, Department of Surgery database, 1960). Improvements in the socioeconomic environment resulted in a fall in incidence over subsequent years to an average of 16.5 new patients per year in the 1990s.2 Patients classically present with repeated episodes of cholangitis. The recurrence of cholangitis after cholecystectomy also raises suspicions of this diagnosis. Typical imaging features on computed tomography (CT) or cholangiography [e.g. endoscopic retrograde cholangiopancreatography (ERCP)] are arrowhead signs, indicating the presence of intrahepatic ductal stones or strictures (Fig. 1). Both CT and ERCP are important tools in the management of patients with RPC. They allow the sites of strictures and intrahepatic stones to be located and also provide a road map for future surgery.3,4
Figure 1.
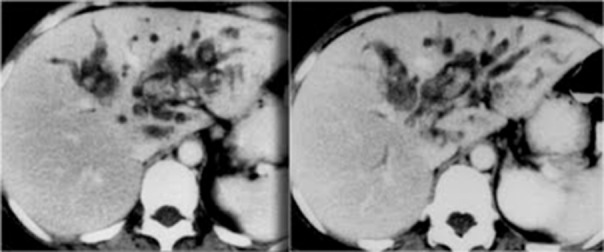
Classical computed tomography images showing dilated intrahepatic ducts with intrahepatic ductal stones and arrowhead signs involving the left lobe of the liver
The management of RPC includes the control of sepsis during an episode of cholangitis, a delayed definitive procedure in the form of hepatectomy or hepaticocutaneousjejunostomy (HCJ), and subsequent surveillance for malignancy. Hepaticocutaneousjejunostomy (Fig. 2) is the mainstay of treatment of RPC. It offers a platform from which to explore the intrahepatic ducts with choledochoscopy. The cutaneous stoma (Fig. 3) created can be closed once ductal clearance is confirmed. In a case of recurrent cholangitis, the cutaneous limb of the HCJ can be reopened readily for further choledochoscopy.
Figure 2.
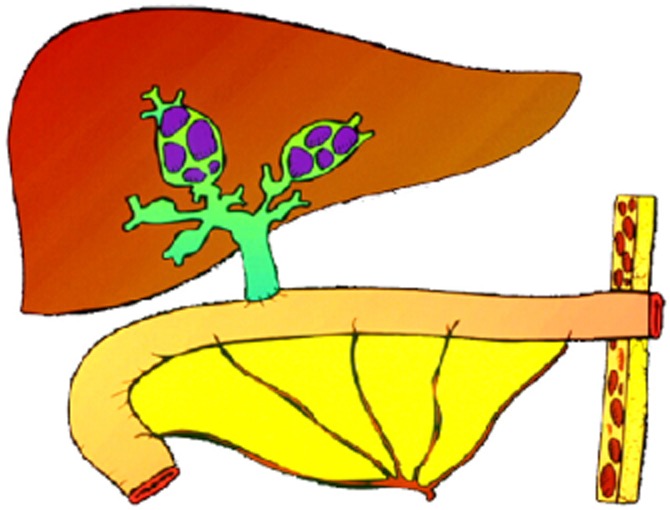
Diagram showing hepaticocutaneousjejunostomy
Figure 3.

Clinical photograph showing the stoma in hepaticocutaneousjejunostomy
The management strategy depends largely on the location of the stone or stricture. For example, if the main culprit of the disease is in the left lateral segment of the liver, especially when parenchymal atrophy or ductal stricture is also present, segmental liver resection should be the treatment of choice. Hepatectomy has been shown to achieve a high rate of immediate stone clearance and to result in a low rate of recurrent stone formation.5,6
Surgical techniques for HCJ for RPC have been modified over the last decade. No longer is a cutaneous stoma routinely created; instead, a latex drainage T-tube is inserted through the Roux loop of the jejunal limb to splint the biliary system at the hepaticojejunostomy, which is usually fashioned with a single layer of 5–0 polydioxanone suture (either interrupted or continuous) (Fig. 4). This procedure (referred to as ‘modified HCJ’ herein) avoids the need to create a stoma, but offers a similar and readily available access route to the biliary system.
Figure 4.
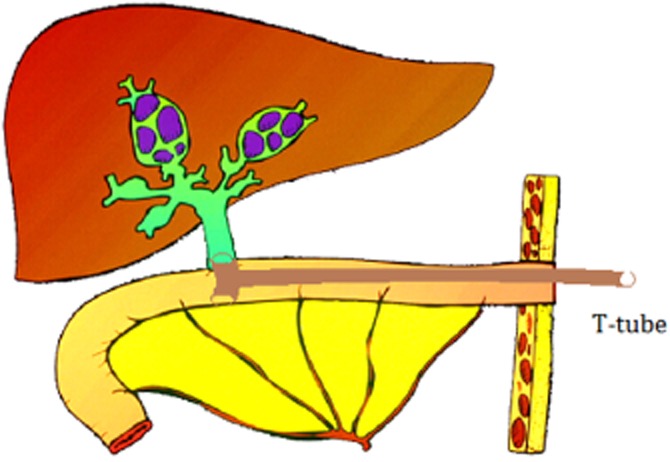
Diagram illustrating the modified technique for hepaticocutaneousjejunostomy with splintage using a T-tube
A few weeks after the procedure, T-tube cholangiography is performed. The T-tube can be removed when ductal clearance is confirmed. The tract will close spontaneously within a few days. The Roux loop of the jejunal limb can be reopened at any time for further stone removal by choledochoscopy if required.
The management of RPC is made difficult by the presence of multiple deeply seated intrahepatic ductal stones and strictures. The rarity of the disease also limits experience in developing a management strategy. This study looked into recent experiences in the surgical management of RPC at a tertiary referral centre in Hong Kong. Immediate outcomes, such as the rate of stone clearance, and longterm outcomes, such as rates of recurrent stone formation, recurrent cholangitis and development of cholangiocarcinoma, were analysed.
Materials and methods
A retrospective review was performed of data for the 80 patients with RPC who underwent surgical treatment between January 2001 and December 2010 at the Department of Surgery, Tung Wah Hospital, University of Hong Kong. Of these 80 patients, 35 were male and 45 were female. The median follow-up time was 5.3 years and the median patient age was 60 years (range: 29–80 years). Data investigated included details of the types of operation, rates of residual and recurrent stones, number of episodes of cholangitis after primary surgery and complication rates after surgery, as well as the number of patients in the cohort who developed cholangiocarcinoma.
Diagnoses of RPC were based on clinical and radiological findings of intrahepatic ductal stones or strictures. A residual stone was defined as incomplete stone clearance revealed during surgery or by imaging at <3 months after surgery.3 A recurrent stone was defined as a stone identified >3 months after surgery. Complications were graded according to the Clavien system of classification and postoperative mortality was defined as death within 30 days after the operation. Independent risk factors for the formation of residual and recurrent stones were identified using chi-squared tests. Statistically significant risk factors were further analysed by multivariate analysis. A P-value of <0.05 was considered to indicate statistical significance.
Results
All of the 80 patients underwent HCJ (or modified HCJ) for biliary drainage and stone removal. Thirty-eight patients (47.5%) also submitted to hepatectomy; these were the only patients to have pathological confirmation of the disease, which was acquired after hepatectomy. Table 1 shows the types of hepatectomy performed. Twenty-three (28.8%) patients had residual stones that required re-intervention, and 25 (31.3%) patients had recurrent stones after the primary operation. All of the latter group required biliary clearance with choledochoscopy via T-tube.
Table 1.
Types of hepatectomy performed
| Type of operation | n |
|---|---|
| Left lateral sectionectomy | 19 |
| Left hepatectomy | 11 |
| Right hepatectomy | 5 |
| Right posterior hepatectomy | 2 |
| Segment VIII resection | 1 |
| Total | 38 |
The chi-squared test identified four statistically significant risk factors for recurrent or residual biliary stones: gender (P = 0.047); type of surgery (HCJ alone versus HCJ with hepatectomy) (P = 0.039); extent of disease (unilobar versus bilobar) (P = 0.042), and preoperative serum bilirubin level [normal versus raised (defined as >20 μmol/l)] (P < 0.001).
Multivariate analysis found that none of gender [odds ratio (OR) = 0.72; P = 0.622], type of surgery (OR = 0.58; P = 0.332) and extent of disease (OR = 0.69; P = 0.611) were associated with an increased risk for the formation of residual or recurrent stones. A raised preoperative serum bilirubin level was also not associated with increased risk for residual stones (P = 0.294), but was found to be an independent risk factor for the formation of recurrent stones (OR = 13.8; P < 0.001).
Sixteen patients developed recurrent cholangitis after primary surgery; six of them had a single recurrent attack. The median number of episodes of cholangitis was 0.5 (range: 0–10 episodes). All patients with cholangitis required antibiotics and biliary drainage with choledochoscopy via HCJ. The median number of choledochoscopy sessions required for biliary clearance was four (range: 1–51 sessions).
Fourteen (17.5%) patients developed complications, mainly wound infections, as a result of the surgical management of RPC. Table 2 shows the different types of complication that occurred. There was no postoperative mortality.
Table 2.
Complications occurring after surgery for recurrent pyogenic cholangitis
| Complication grade | Complications, n | Details |
|---|---|---|
| I | 10 | Wound infection, n = 9 |
| Postoperative ileus, n = 1 | ||
| II | 0 | |
| IIIa | 1 | Intra-abdominal collection, n = 1 (requiring percutaneous drainage) |
| IIIb | 3 | Bile leak, n = 1 (requiring open repair) Incisional hernia, n = 2 (requiring elective hernia repair) |
| IVa | 0 | |
| IVb | 0 | |
| V | 0 | |
Four (5.0%) patients developed cholangiocarcinoma and two of these died of the malignancy during a median follow-up of 36 months (range: 17–54 months). Overall survival in the cohort was 97.5% after a median follow-up of 63.3 months (range: 20–121 months).
Discussion
Recurrent pyogenic cholangitis is an oriental disease; it is rarely seen in the West. In 1930, Digby documented its occurrence in Hong Kong and described eight cases he had encountered.1 The Queen Mary Hospital, Department of Surgery at the University of Hong Kong managed up to 50 new patients per year in the 1950s. The incidence of the disease gradually declined to an average of 16.5 new patients per year in the 1990s as a result of general improvements in the socioeconomic environment, in which better social and environmental hygiene reduced the incidence of liver fluke (Clonorchis sinensis) infestation and thus RPC. However, a growing incidence of RPC has been observed in the West as a result of increased immigration. In Japan, 4.1% of patients who undergo surgery for biliary stones are eventually diagnosed with RPC.7
Patients with RPC have been considered as ‘stone-forming’. These patients develop biliary stones even after cholecystectomy. One study comparing hepatectomy with percutaneous biliary drainage with choledochoscopy for RPC found that both treatment modalities achieved satisfactory stone clearance, but the rate of stone recurrence in the percutaneous drainage group was much higher (31.5% versus 5.6%).8 In 1962, Ong pioneered the use of HCJ at the University of Hong Kong for biliary drainage and stone removal.9 This technique has long been adopted as the primary surgical treatment for RPC. Patients with RPC may require several sessions of choledochoscopy in order to ensure all biliary stones are removed. When ductal clearance is confirmed by choledochoscopy or plain CT, the stoma created can be closed. With modified HCJ, a cutaneous stoma is no longer routinely created, but, instead, a T-tube is inserted to splint the hepaticojejunostomy and is brought out to the abdominal wall through the Roux loop of the jejunum. Choledochoscopy is performed via the T-tube, which can be removed once ductal clearance is confirmed. If recurrent biliary stone formation occurs, the jejunal limb is reopened for operation. Observations throughout the past few decades indicate that most patients are free of residual or recurrent stones after HCJ. In an instance of recurrence, the stoma can be reopened readily to facilitate the removal of further stones.
In the current study, the only identifiable risk factor for recurrent stone formation was a deranged preoperative serum bilirubin level. Patients with a raised serum bilirubin level on presentation have a higher risk for stone recurrence. Whether a more radical approach using surgical treatments such as hepatectomy will translate into a significant clinical benefit requires further evaluation.
In the present study, some patients underwent HCJ only and others underwent both HCJ and hepatectomy. When these two groups of patients were compared, no statistically significant difference in the rate of residual or recurrent stone formation emerged. This probably reflects the effect of a strict patient selection protocol on surgical outcome. Chronic or recurrent cholangitis renders the liver atrophic and the affected segment of liver is usually non-functional. Many authorities therefore advocate hepatectomy in the treatment of RPC. In fact, the study hospital also performs hepatectomy, but in a more selective manner. Undoubtedly, the present study includes an element of selection bias because patients with complicated RPC were treated with both HCJ and hepatectomy, whereas those with uncomplicated disease underwent HCJ only. However, the results have demonstrated the importance of careful patient selection for operation; hepatectomy should be reserved for patients with liver atrophy, segmental intrahepatic biliary stricture or malignancy.
In the current study, 17.5% (n = 14/80) of patients developed surgical complications, most of which were wound infections. Biliary stasis, biliary obstruction and in situ biliary catheterization were all contributing factors. Bile spillage is often unavoidable in biliary surgery, whether the surgery involves a drainage procedure or hepatectomy. Therefore, the present authors routinely administer i.v. antibiotics. Additional doses of antibiotics are given in prolonged operations.
Four (5.0%) patients in the study cohort developed cholangiocarcinoma and two of them died of it. Surveillance for malignancy using tumour markers such as carbohydrate antigen 19-9 (CA 19-9) and carcinoembryonic antigen (CEA), as well as annual imaging using CT, is therefore essential.
Although the rates of residual and recurrent stones were higher in the current study than in an earlier study conducted in 2004,6 the complication rate was lower. This probably reflects the impact of an improved surgical technique, meticulous control of contamination of the surgical field, and the use of antibiotics. None of the 80 patients died after surgery (i.e. of surgery-related causes), which probably also reflects the use of a refined surgical technique for hepatectomy, improved postoperative care and the nutritional support of patients.
In conclusion, HCJ with or without hepatectomy provides reasonably good results in the treatment of RPC. It is safe and feasible and offers additional benefits in terms of facilitating salvage surgery (the reopening of a stoma and repeat choledochoscopy) for the treatment of recurring stones.
Conflicts of interest
None declared.
References
- 1.Digby KH. Common-duct stones of liver origin. Br J Surg. 1930;17:578–591. [Google Scholar]
- 2.Lo CM, Fan ST, Wong J. The changing epidemiology of recurrent pyogenic cholangitis. Hong Kong Med J. 1997;3:302–304. [PubMed] [Google Scholar]
- 3.Fan ST, Choi TK, Chan FL, Lai EC, Wong J. Role of computed tomography in the management of recurrent pyogenic cholangitis. Aust N Z J Surg. 1990;60:599–605. doi: 10.1111/j.1445-2197.1990.tb07439.x. [DOI] [PubMed] [Google Scholar]
- 4.Lam SK, Wong KP, Chan PK, Ngan H, Ong GB. Recurrent pyogenic cholangitis: a study by endoscopic retrograde cholangiography. Gastroenterology. 1978;74:1196–1203. [PubMed] [Google Scholar]
- 5.Lee TY, Chan YL, Chang HC, Chan CP, Kuo ST. Outcomes of hepatectomy for hepatolithiasis. World J Surg. 2007;31:479–482. doi: 10.1007/s00268-006-0441-6. [DOI] [PubMed] [Google Scholar]
- 6.Chen DW, Poon RT, Liu CL, Fan ST, Wong J. Immediate and longterm outcomes of hepatectomy for hepatolithiasis. Surgery. 2004;135:386–393. doi: 10.1016/j.surg.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Nakayama F, Furusawa T, Nakama T. Hepatolithiasis in Japan: present status. Am J Surg. 1980;139:216–220. doi: 10.1016/0002-9610(80)90257-3. [DOI] [PubMed] [Google Scholar]
- 8.Otani K, Shimizu S, Chijiiwa K, Ogawa T, Morisaki T, Sugitani A, et al. Comparison of treatments for hepatolithiasis: hepatic resection versus cholangioscopic lithotomy. J Am Coll Surg. 1999;189:177–182. doi: 10.1016/s1072-7515(99)00109-x. [DOI] [PubMed] [Google Scholar]
- 9.Ong GB. A study of recurrent pyogenic cholangitis. Arch Surg. 1962;84:199. doi: 10.1001/archsurg.1962.01300200047004. [DOI] [PubMed] [Google Scholar]


