Abstract
Objectives
The rise in prevalence of diabetes is alarming and research ascribes most of the increase to lifestyle. However, little knowledge exists about the influence of occupational factors on the risk for developing diabetes. This study estimates the importance of work and lifestyle as risk factors for developing diabetes mellitus among healthcare workers and explores the association of work factors and obesity, which is a risk factor for diabetes.
Methods
Questionnaire-based prospective cohort study among 7,305 health care workers followed for seven years in the Danish National Diabetes Register. We used bivariate comparisons to give an unadjusted estimate of associations, followed by adjusted survival analysis and logistic regression models to estimate the influences of potential risk factors related to job, health and lifestyle on diabetes and obesity.
Results
During seven years of follow up, 3.5% of participants developed diabetes, associated with obesity (HR = 6.53; 95% CI 4.68–9.10), overweight (HR = 2.89; CI 2.11–3.96) age 50–69 y (HR = 2.27; 95% CI 1.57–3.43) and high quality of leadership (HR = 1.60; CI 1.19–2.16). Obesity at baseline was most common among the youngest employees, and was mainly associated with developing diabetes (OR = 3.84; CI 2.85–5.17), impaired physical capacity and physical inactivity. In the occupational setting, obesity was associated with shift work, severe musculoskeletal pain, low influence, but also by good management, fewer role conflicts and a positive work-life balance. Looking only at non-smokers, removed the influence of age and pain. However, non-smokers also had higher depression scores and more role conflicts.
Conclusions
Confirming obesity as the strongest risk factor for developing diabetes, the present study identified few occupational risk factors. However, obesity, the key risk factor for diabetes, had a more variable relation with work than did diabetes.
Introduction
The rising retirement age in many Western societies means that the workplace will undergo new challenges from increasing numbers of employees with age- and lifestyle-related diseases. However, it is no longer adequate or productive to reduce lifestyle to something only relevant to the private life of individuals because the proliferation of sedentary work in modern employment contributes significantly to the increasing prevalence of lifestyle diseases. One of these is type 2 diabetes mellitus (T2DM), a condition currently reaching epidemic [1], [2] or pandemic [3] proportions, that is, in turn, closely related to the obesity epidemic [3], [4] and the sedentary work and life of many people. Although it is expected that T2DM will influence ability to work [5], most employers are yet not fully aware of, or prepared to meet, this challenge. Furthermore, little knowledge exists about the consequences of T2DM for society, workplaces and employees [6]. It is, however, likely to influence productivity, efficiency, quality and safety [7]–[10], not just because of absenteeism due to sickness, but also because it drains people of both physical and mental energy [11], [12]. In addition, the consequences are greater among the least educated and the socially most vulnerable groups [13]. This is the same category of employees already at higher risk of long term absenteeism, early retirement, disability pension and unemployment [14].
It is estimated that types 1 and 2 diabetes collectively cause the loss of an average of 9 years of life at age 30 years and 3 years at age 70: the relative risk for cardiovascular disease among those with diabetes, compared to those without it, is 3.5 at age 50 [15]. We are unable to distinguish between type 1 and type 2 diabetes in terms of these effects. However, since T2DM accounts for more than 90% of diagnosed diabetes and is the only form of the disease influenced by external factors like lifestyle and work, we refer to T2DM hereafter, unless otherwise specified. Due to the combination of increased prevalence and rising age at retirement, T2DM might soon become one of the most important factors related to the health of the senior workforce. It is surprising, therefore, that so little is known about relationships between T2DM and work.
Since health care workers experience high psychosocial strain and are at increased risk of sickness absenteeism, early labour market exit, musculoskeletal problems and unhealthy lifestyle [16]–[20], they may also be at increased risk of developing diabetes. The prevalence of overweight and physical inactivity is high among health care workers, and the frequent occurrence of physical pain and physical and mental exhaustion from work could reduce the capacity to remain fit and active during leisure. There are also some suggestions that psychosocial strain—especially low control—increases the risk of T2DM [21]–[23], metabolic syndrome [24] and dyslipidemia [25] among women.
The aim of this study is to investigate the potential influence of occupational factors on developing diabetes among healthcare workers. Furthermore, because obesity is the single most important risk factor for T2DM, a second aim was to investigate associations between work and lifestyle factors related to obesity.
Materials and Methods
Our prospective observational design combined data on lifestyle and working conditions with the risk of developing diabetes by linking a large cohort of female health care workers with the Danish National Diabetes Register (DNDR) [26]. We used 2005 as the baseline year and excluded patients with diagnosed diabetes in 2005 to examine incidence after baseline.
The health care worker cohort
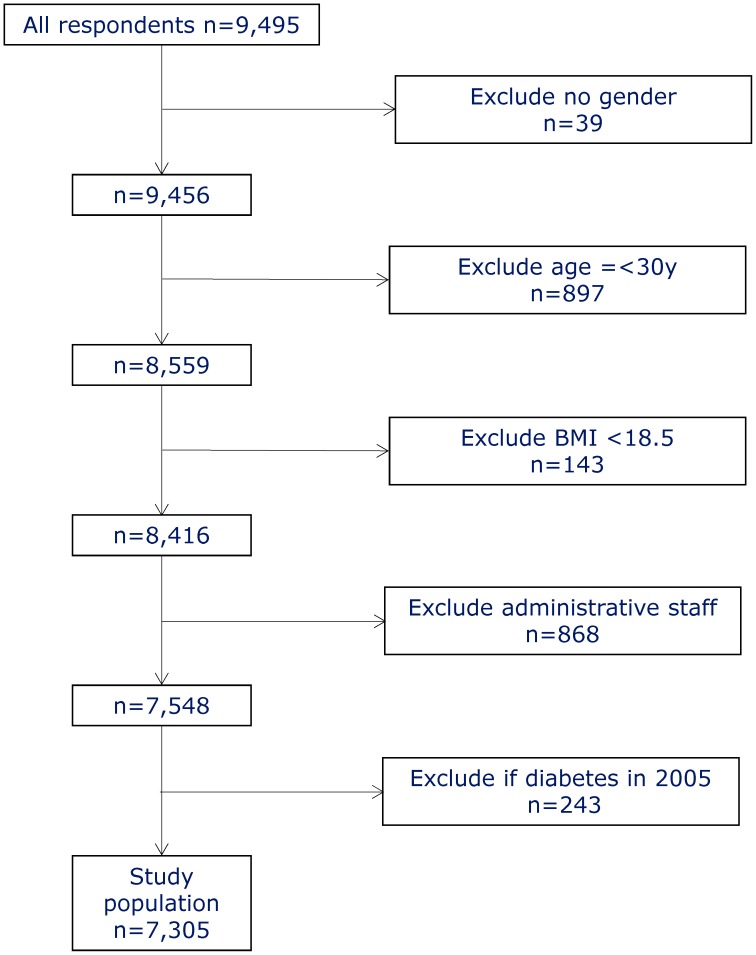
The cohort is based on a survey of eldercare service employees conducted in 2004–5 in 35 Danish municipalities. All employees (12,744) received a written questionnaire that was administered by a local contact person in each municipality; 9,495 responded, a response rate of 75%. We excluded respondents who didn't report their gender, underweight workers, and administrative staff. We also excluded workers aged 30 years or younger because of the greater risk of type 1 diabetes (Figure 1). The remaining 7,305 health care workers were linked to disease and population registers via a unique personal identification number and followed for seven years. Detailed information on most of the measures has been reported elsewhere [18]–[20].
Figure 1. Participant Flow Chart.
The National Diabetes Register
In 2006 Denmark established a National Diabetes Register (DNDR) that includes all incidences of diabetes since 1995 [26]. DNDR combines data from three different national registries: the National Patient Register (NPR) [27], the National Health Insurance Service Registry (NHISR) [28] and the Register of Medicinal Product Statistics (RMPS) [29]. Individuals must meet at least one of six criteria to be registered in DNDR: 1) receive a diagnosis of diabetes (data source, NPR); 2) receive diabetes-related chiropody care (NHISR); 3) have blood glucose measured five times in a calendar year (NHISR); 4) have at least two annual blood glucose measurements over a period of five consecutive years (NHISR); 5) purchase prescribed oral anti-diabetic medication (registered at second purchase, RMPS); 6) purchase prescribed insulin (RMPS). In addition to the unique personal identification number of each individual, DNDR contains data on sex, date of birth, date of death, and date of inclusion according to the entry criteria. However, the register does not distinguish between type 1 and type 2 diabetes. DNDR has been validated and found to be reliable as a source for linkable information on diabetes at a national level [15], [30].
Demographic variables
Age, information about ethnicity and household type was drawn from Statistics Denmark [31] through linking with the Danish Civil Registration System [32].
Measures of health
All measures of health originated from the baseline questionnaires, with the exception of diabetes data from DNDR. General health was self-assessed on a five-point scale ranging from ‘poor’ to ‘outstanding’ and dichotomised as poor if respondents selected one of the two lowest scores and good otherwise. Sleep problems were identified if at least one of five questions was scored higher than three on a six-point scale. Participants separately rated pain in the low back, neck/shoulders and knees as average pain during the last three months on a numerical rating scale from 0–9, where 0 represented ‘no pain’ and 9 represents ‘worst imaginable pain’. Based on the distribution of the rating, pain was categorised in four groups to make it easier to interpret than if using the continuous scale [33]. Depression was evaluated using the Danish version of the Major Depression Inventory (MDI), and the WHO-5 well-being scale was used to assess the risk for developing depression and stress [20], [34].
Measures of job-related factors
Working hours were self-reported in a single item. Ergonomic strain was assessed with the Hollmann index, a compound measure of body postures and weight lifted during the work day [20]. Strain was stratified in four categories based on the distribution of the continuous compound measure scale. Work-life balance was defined as poor if respondents reported that work was draining both time and energy from their private lives. Assessment of psychosocial working conditions used the same model as in a long-term sickness absenteeism survey [19], in which four scales—emotional demands, influence, role conflict and quality of leadership—were based on four items from the Copenhagen Psychosocial Questionnaire (COPSOQ) [35].
Measures of lifestyle
All lifestyle variables were self-assessed in the questionnaire. Leisure time physical activity was classified as good if respondents reported they were very active or fairly active. Physical capacity was rated across the domains of physical fitness, strength, endurance and body movement as the average score on a nine-point scale from worst (1) to best (9). On the basis of the distribution of the scores, the authors decided to stratify into four categories. Smokers were those reporting daily smoking. Finally Body Mass Index (BMI) was categorised as normal weight (18.5≤BMI<25), overweight (25≤BMI<30) and obese (BMI≥30).
The study was approved by the Danish Data Protection Agency. In Denmark, however, approval from Ethics Committees is not required for survey research. Furthermore, participation in the study was voluntary which implies that written informed consent is not necessary as this consent is implied in individual respondents' voluntary participation.
Statistical analyses
Initially, unadjusted bivariate (2×n) analyses compared each variable with the incidence of diabetes using Chi square analysis for trend. All variables were then included in a saturated Cox regression model with diabetes as the dependent variable using SAS Proc Genmod; this was used as the basis for a subsequent manual backward elimination based on log likelihood ratio tests to correct for multiple testing. A similar analytic approach followed, in which obesity at baseline was the dependent variable. However, since this was a cross-sectional design, the Logistic procedure in SAS 9.3 was used for a multiple logistic regression analysis. Manual backwards elimination using the log likelihood ratio test was used to fit the model. The Hosmer and Lemeshow goodness-of-fit test was used to evaluate the logistic analyses [36].
Results
Health care workers who did not respond to the questionnaire were significantly younger than those who did (OR = 2.52; 95% CI 2.29–2.75) and more likely to belong to an ethnic minority (OR = 2.02; 95% CI 1.66–2.43). Non-respondents had a lower incidence of diabetes (OR 0.64 95% CI: 0.48–0.86) though as the fact that they were, on average, younger than respondents provides a potential explanation for this.
Table 1 presents descriptive statistics and the distribution of diabetes incidence. BMI is the single most important risk factor for the development of diabetes, followed by age and lack of physical exercise. Poor general health, musculoskeletal pain and sleep problems predict an increasing diabetes risk, but none of the psychological variables showed significance. From the occupational arena, only shift work (evening/night) and quality of leadership were associated with an increased risk of diabetes.
Table 1. Incidence of diabetes among health care workers over seven years.
| N | Developed diabetes | |||
| Demography | Female | 7,119 | 245 | (3.6%) |
| Male | 186 | 8 | (4.3%) p = 0.560 | |
| Age in 2005: 30–39 y | 1,475 | 34 | (2.3%) | |
| Age in 2005: 40–49 y | 2,721 | 68 | (2.5%) | |
| Age in 2005: 50–69 y | 3,109 | 160 | (5.2%) p<0.0001 | |
| Danish origin | 6,977 | 250 | (3.6%) | |
| Ethnic minority | 293 | 10 | (3.4%) p = 0.878 | |
| Live with a partner | 6,022 | 215 | (3.6%) | |
| Live alone | 1,283 | 47 | (3.7%) p = 0.871 | |
| Health | Good self-rated health | 6,398 | 213 | (3.3%) |
| Poor self-rated health | 862 | 45 | (5.2%) p = 0.005 | |
| No musculoskeletal pain | 1,115 | 37 | (3.3%) | |
| Low musculoskeletal pain | 2,644 | 79 | (3.0%) | |
| Moderate musculoskeletal pain | 2,821 | 106 | (3.8%) | |
| Severe musculoskeletal pain | 435 | 28 | (6.6%) p = 0.004 | |
| No depression | 7,161 | 255 | (3.6%) | |
| Depression | 144 | 7 | (4.9%) p = 0.406 | |
| Not at risk for stress or depression | 5,962 | 203 | (3.4%) | |
| At risk for stress or depression | 1,343 | 59 | (4.4%) p = 0.079 | |
| No problems with sleep | 6,026 | 202 | (3.4%) | |
| At least one problem with sleep | 1,279 | 60 | (4.7%) p = 0.019 | |
| Work | Work entirely/partly during daytime | 5,480 | 176 | (3.2%) |
| Work only evening/nights | 1,812 | 86 | (4.8%) p = 0.002 | |
| Work does not drain time and energy | 5,954 | 210 | (3.5%) | |
| Work drains time and energy | 1,264 | 45 | (3.6%) p = 0.946 | |
| Lowest ergonomic strain | 2,071 | 81 | (3.9%) | |
| Low ergonomic strain | 1,703 | 52 | (3.1%) | |
| High ergonomic strain | 1,745 | 54 | (3.1%) | |
| Highest ergonomic strain | 1,786 | 75 | (4.2%) p = 0.158 | |
| Low emotional demands | 1,319 | 54 | (4.1%) | |
| Medium emotional demands | 4,670 | 157 | (3.4%) | |
| High emotional demands | 1,316 | 51 | (3.9%) p = 0.352 | |
| Low influence | 1,588 | 68 | (4.3%) | |
| Medium influence | 3,846 | 129 | (3.4%) | |
| High influence | 1,871 | 65 | (3.5%) p = 0.236 | |
| Low role conflicts | 1,449 | 50 | (3.5%) | |
| Medium role conflicts | 4,346 | 148 | (3.4%) | |
| High role conflicts | 1,510 | 64 | (4.2%) p = 0.301 | |
| Low quality of leadership | 1,780 | 73 | (4.1%) | |
| Medium quality of leadership | 3,668 | 100 | (2.7%) | |
| High quality of leadership | 1,857 | 89 | (4.8%) p = 0.0002 | |
| Lifestyle | Exercise | 3,898 | 117 | (3.0%) |
| No exercise | 3,327 | 138 | (4.2%) p<0.012 | |
| Lowest self-reported physical capacity | 2,633 | 107 | (4.1%) | |
| Low self-reported physical capacity | 1,374 | 62 | (4.5%) | |
| High self-reported physical capacity | 1,493 | 50 | (3.4%) | |
| Highest self-reported physical capacity | 1,805 | 43 | (2.4%) p = 0.005 | |
| Non-smoker | 4,590 | 161 | (3.5%) | |
| Smoker | 2,672 | 100 | (3.7%) p = 0.604 | |
| Normal BMI | 4,308 | 67 | (1.6%) | |
| Overweight | 2,181 | 107 | (4.9%) | |
| Obese | 809 | 86 | (10.6%) p<0.0001 | |
Controlling for covariates in the saturated Cox regression model removed most occupational and all health-related variables (Table 2). The risk of developing diabetes was associated with obesity, being overweight, increased age and quality of leadership. These four variables remained significant in the fitted model.
Table 2. Survival analysis for 7-year diabetes incidence among health care workers (n = 6,784).
| Full Model | Fitted modela | ||||
| Demography | Gender (female v male) | 0.87 | (0.41–1.87) | - | - |
| Age in 2005: (40–49 y v 30–39 y) | 1.11 | (0.72–1.72) | - | - | |
| Age in 2005: (50–69 y v 30–39 y) | 2.37 | (1.53–3.39) | 2.27 | (1.57–3.43) | |
| Ethnicity (minority v original Danish) | 0.94 | (0.46–1.92) | - | - | |
| Family (living alone v living with partner) | 0.99 | (0.70–1.39) | - | - | |
| Work | Shift work (evening/night v day) | 1.27 | (0.95–1.70) | - | - |
| Ergonomic strain (low v lowest) | 0.81 | (0.56–1.17) | - | - | |
| Ergonomic strain (high v lowest) | 0.82 | (0.57–1.19) | - | - | |
| Ergonomic strain (highest v lowest) | 0.92 | (0.63–1.33) | - | - | |
| Work-life balance (poor v good) | 0.95 | (0.66–1.38) | - | - | |
| Emotional demands (low v medium) | 1.22 | (0.86–1.71) | - | - | |
| Emotional demands (high v medium) | 1.07 | (0.76–1.51) | - | - | |
| Influence (low v medium) | 1.05 | (0.75–1.45) | - | - | |
| Influence (high v medium) | 1.04 | (0.76–1.44) | - | - | |
| Role conflicts (low v medium) | 0.82 | (0.57–1.16) | - | - | |
| Role conflicts (high v medium) | 1.04 | (0.75–1.46) | - | - | |
| Quality of leadership (low v medium) | 1.15 | (0.82–1.61) | - | - | |
| Quality of leadership (high v medium) | 1.71 | (1.25–2.32) | 1.60 | (1.19–2.16) | |
| Health | General health (poor v good) | 1.11 | (0.75–1.64) | - | - |
| Musculoskeletal pain (low v none) | 1.05 | (0.69–1.60) | - | - | |
| Musculoskeletal pain (moderate v none) | 1.21 | (0.80–1.84) | - | - | |
| Musculoskeletal pain (severe v none) | 1.49 | (0.84–2.65) | - | - | |
| Sleep (problems v no problems) | 1.14 | (0.80–1.62) | - | - | |
| MDI score (depression v no depression) | 0.94 | (0.40–2.23) | - | - | |
| WHO well-being score (at risk v not at risk) | 1.11 | (0.78–1.60) | - | - | |
| Lifestyle | BMI (overweight v normal weight) | 2.84 | (2.06–3.90) | 2.89 | (2.11–3.96) |
| BMI (obese v normal weight) | 6.30 | (4.27–8.49) | 6.53 | (4.68–9.10) | |
| Physical exercise (no exercise v exercise) | 1.10 | (0.83–1.44) | - | - | |
| Physical capacity (high v highest) | 1.25 | (0.82–1.91) | - | - | |
| Physical capacity (low v highest) | 1.42 | (0.94–2.16) | - | - | |
| Physical capacity (lowest v highest) | 1.11 | (0.75–1.67) | - | - | |
| Smoking (smoker v non-smoker) | 1.21 | (0.93–1.59) | - | - | |
Backwards elimination of class variables using log likelihood ratio tests.
Looking at body weight, the youngest employees and those who were ethnically Danish had the highest prevalence of obesity (Table 3). Both physical and mental health problems were associated with obesity. The risk of developing diabetes had the highest odds ratio of all variables in terms of obesity. Shift work and having low influence and scoring high on role conflicts were associated with obesity. Leisure time physical inactivity was associated with obesity, and it is notable that a significantly lower proportion of obese employees were smokers.
Table 3. Obesity among health care workers.
| N | BMI≥30 | |||
| Demography | Female | 7,119 | 792 | (11.1%) |
| Male | 186 | 17 | (9.4%) p = 0.394 | |
| Age in 2005: 30–39 y | 1,475 | 193 | (13.1%) | |
| Age in 2005: 40–49 y | 2,721 | 289 | (10.6%) | |
| Age in 2005: 50–69 y | 3,109 | 327 | (10.5%) p<0.022 | |
| Danish origin | 6,977 | 784 | (11.2%) | |
| Ethnic minority | 293 | 22 | (7.5%) p = 0.046 | |
| Live with a partner | 6,022 | 679 | (11.3%) | |
| Live alone | 1,283 | 130 | (10.1%) p = 0.236 | |
| Health | Good self-rated health | 6,398 | 668 | (10.4%) |
| Poor self-rated health | 862 | 140 | (16.2%) p<0.0001 | |
| No musculoskeletal pain | 1,115 | 106 | (9.5%) | |
| Low musculoskeletal pain | 2,644 | 248 | (9.4%) | |
| Moderate musculoskeletal pain | 2,821 | 347 | (12.3%) | |
| Severe musculoskeletal pain | 435 | 66 | (15.2%) p = 0.0001 | |
| No depression | 7,161 | 784 | (11.0%) | |
| Depression | 144 | 25 | (17.4%) p = 0.015 | |
| Not at risk for stress or depression | 5,962 | 641 | (10.8%) | |
| At risk for stress or depression | 1,343 | 168 | (12.5%) p = 0.064 | |
| No problems with sleep | 6,026 | 626 | (10.4%) | |
| At least one problem with sleep | 1,279 | 183 | (14.3%) p<0.0001 | |
| Did not develop diabetes | 7,043 | 723 | (10.3%) | |
| Developed diabetes | 262 | 86 | (32.8%) p<0.0001 | |
| Work | Work entirely/partly during daytime | 5,480 | 566 | (10.3%) |
| Work only evening/nights | 1,812 | 242 | (13.4%) p = 0.0004 | |
| Work does not drain time and energy | 5,964 | 673 | (11.3%) | |
| Work drains time and energy | 1,264 | 125 | (9.9%) p = 0.151 | |
| Lowest ergonomic strain | 2,071 | 215 | (10.4%) | |
| Low ergonomic strain | 1,703 | 189 | (11.1%) | |
| High ergonomic strain | 1,745 | 181 | (10.4%) | |
| Highest ergonomic strain | 1,786 | 224 | (12.5%) p = 0.122 | |
| Low emotional demands | 1,319 | 145 | (11.0%) | |
| Medium emotional demands | 4,670 | 511 | (10.9%) | |
| High emotional demands | 1,316 | 153 | (11.6%) p = 0.779 | |
| Low influence | 1,588 | 216 | (13.6%) | |
| Medium influence | 3,643 | 401 | (10.4%) | |
| High influence | 1,871 | 192 | (10.3%) p = 0.001 | |
| Low role conflicts | 1,449 | 135 | (9.3%) | |
| Medium role conflicts | 4,346 | 485 | (11.2%) | |
| High role conflicts | 1,510 | 189 | (12.5%) p = 0.021 | |
| Low quality of leadership | 1,780 | 200 | (11.2%) | |
| Medium quality of leadership | 3,668 | 381 | (10.4%) | |
| High quality of leadership | 1,857 | 228 | (12.3%) p = 0.103 | |
| Lifestyle | Exercise | 3,898 | 320 | (8.2%) |
| No exercise | 3,327 | 477 | (14.3%) p<0.0001 | |
| Lowest self-reported physical capacity | 2,633 | 388 | (14.7%) | |
| Low self-reported physical capacity | 1,374 | 178 | (13.0%) | |
| High self-reported physical capacity | 1,493 | 144 | (9.6%) | |
| Highest self-reported physical capacity | 1,805 | 99 | (5.5%) p<0.0001 | |
| Non-smoker | 4,590 | 570 | (12.4%) | |
| Smoker | 2,672 | 236 | (8.8%) p<0.0001 | |
Table 4 shows that controlling for confounding removed the association with general and mental health status and role conflicts and added influence from quality of leadership and work-life balance. Apart from introducing the importance of musculoskeletal pain, the fitted regression showed the same pattern as the full adjusted logistic regression model. As smoking is known to reduce obesity, reanalysing the obesity data for non-smokers, we found that smoking could explain the effects of age and musculoskeletal pain. On the other hand, statistical associations of high depression scores and role conflicts with obesity are seen for non-smokers.
Table 4. Logistic regression models for obesity among all health care workers (n = 6,784) and only the non-smokers (n = 4.282).
| All health care workers | Only non-smoking health care workers | ||||||||
| Full Modela | Fitted modelb | Full modelc | Fitted modeld | ||||||
| Demography | Gender (female v male) | 1.27 | (0.72–2.23) | - | - | 1.27 | (0.65–2.49) | - | - |
| Age (40–49 y v 30–39 y) | 0.76 | (0.61–0.93) | 0.76 | (0.62–0.94) | 0.85 | (0.66–1.09) | - | - | |
| Age (50–69 y v 30–39 y) | 0.67 | (0.54–0.82) | 0.68 | (0.55–0.84) | 0.76 | (0.59–0.98) | - | - | |
| Ethnicity (minority v original Danish) | 0.54 | (0.33–0.90) | 0.54 | (0.33–0.88) | 0.45 | (0.24–0.84) | 0.45 | (0.25–0.87) | |
| Family (living alone v living with partner) | 0.95 | (0.77–1.18) | - | - | 1.00 | (0.77–1.31) | - | - | |
| Work | Shift work (evening/night v day) | 1.50 | (1.25–1.80) | 1.51 | (1.26–1.81) | 1.52 | (1.21–1.92) | 1.50 | (1.25–1.92) |
| Ergonomic strain(low v lowest) | 1.05 | (0.83–1.31) | - | - | 0.99 | (0.76–1.30) | - | - | |
| Ergonomic strain (high v lowest) | 0.94 | (0.75–1.18) | - | - | 1.05 | (0.80–1.37) | - | - | |
| Ergonomic strain (highest v lowest) | 1.11 | (0.88–1.39) | - | - | 1.11 | (0.84–1.47) | - | - | |
| Work-life balance (poor v good) | 0.73 | (0.58–0.92) | 0.75 | (0.60–0.94) | 0.66 | (0.50–0.88) | 0.68 | (0.51–0.89) | |
| Emotional demands (low v medium) | 1.04 | (0.83–1.30) | - | - | 1.19 | (0.91–1.55) | - | - | |
| Emotional demands (high v medium) | 1.02 | (0.82–1.27) | - | - | 1.10 | (0.85–1.42) | - | - | |
| Influence (low v medium) | 1.31 | (1.08–1.60) | 1.33 | (1.10–1.62) | 1.32 | (1.04–1.67) | 1.35 | (1.07–1.71) | |
| Influence (high v medium) | 1.04 | (0.85–1.27) | - | - | 1.05 | (0.82–1.34) | - | - | |
| Role conflicts (low v medium) | 0.81 | (0.65–1.02) | 0.82 | (0.65–1.01) | 0.85 | (0.65–1.11) | - | - | |
| Role conflicts (high v medium) | 1.12 | (0.91–1.37) | - | - | 1.33 | (1.04–1.69) | 1.40 | (1.12–1.77) | |
| Quality of leadership (low v medium) | 0.96 | (0.78–1.17) | - | - | 0.95 | (0.74–1.22) | - | - | |
| Quality of leadership (high v medium) | 1.28 | (1.05–1.55) | 1.29 | (1.06–1.56) | 1.35 | (1.07–1.70) | 1.32 | (1.03–1.57) | |
| Health | General health (poor v good) | 1.19 | (0.93–1.52) | - | - | 1.26 | (0.94–1.69) | - | - |
| Musculoskeletal pain (low v none) | 0.94 | (0.73–1.21) | - | - | 0.99 | (0.73–1.35) | - | - | |
| Musculoskeletal pain (moderate v none) | 1.17 | (0.91–1.50) | - | - | 1.17 | (0.86–1.60) | - | - | |
| Musculoskeletal pain (severe v none) | 1.42 | (0.97–2.06) | 1.60 | (1.12–2.28) | 1.33 | (0.83–2.12) | - | - | |
| Sleep (problems v no problems) | 1.22 | (0.97–1.52) | - | - | 1.10 | (0.84–1.45) | - | - | |
| MDI score (depression v no depression) | 1.14 | (0.67–1.93) | - | - | 1.73 | (0.95–3.15) | 2.02 | (1.11–3.35) | |
| WHO well-being score (at risk v not at risk) | 0.90 | (0.71–1.12) | - | - | 0.87 | (0.66–1.16) | - | - | |
| Developed diabetes (yes v no) | 3.80 | (2.82–5.13) | 3.84 | (2.85–5.17) | 3.30 | (2.27–4.81) | 3.32 | (2.30–484) | |
| Lifestyle | Physical exercise (no exercise v exercise) | 1.61 | (1.36–1.91) | 1.62 | (1.37–1.91) | 1.69 | (1.38–2.07) | 1.70 | (1.37–2.05) |
| Physical capacity (high v highest) | 1.68 | (1.27–2.24) | 1.69 | (1.27–2.25) | 1.78 | (1.25–2.53) | 1.81 | (2.01–3.79) | |
| Physical capacity (low v highest) | 2.25 | (1.70–2.97) | 2.26 | (1.71–2.98) | 2.28 | (1.61–3.22) | 2.34 | (1.68–3.32) | |
| Physical capacity (lowest v highest) | 2.31 | (1.79–3.00) | 2.37 | (1.83–3.06) | 2.66 | (1.93–3.67) | 2.81 | (1.28–2.57) | |
| Smoking (smoker v non-smoker) | 0.61 | (0.51–0.72) | 0.61 | (0.51–0.73) | - | - | - | - | |
Hosmer and Lemeshow Goodness-of-fit test: p = 0.9407.
Log likelihood ratio test used for manual backward elimination. Hosmer and Lemeshow Goodness-of-fit test: p = 0.4955.
Hosmer and Lemeshow Goodness-of-fit test: p = 0.7268.
Log likelihood ratio test used for manual backward elimination. Hosmer and Lemeshow Goodness-of-fit test: p = 0.7577.
Discussion
The present study showed both lifestyle and occupational risk factors among healthcare workers for developing diabetes over a period of seven years. The most important risk factor was a BMI above the normal category. At baseline, obesity was associated with low level of exercise, poor self-rated physical fitness, shift work and problems with health and sleep.
Diabetes and work
Pain was significantly associated with an increased diabetes risk in the bivariate analysis. In the same cohort, it has been shown that the more pain health care workers have, the higher the long-term sickness absenteeism [33], [37]. After controlling for lifestyle, however, we found little impact from occupational risk factors for developing diabetes. Therefore, if health care workers have so much musculoskeletal pain or are so drained of energy by their work that they cannot stay fit, it will have significant indirect effects on diabetes. The same factors are also expected to cause selection out of work.
Shift work was another factor that increased the risk of developing diabetes in our study. Potential explanations for this finding include the difficulty of maintaining a healthy lifestyle, e.g., a tendency to eat unhealthy foods and exercise less, and effects on the endocrine circadian rhythm [38]–[40]. Although a review of the epidemiological evidence found only moderate support for an association between shift work and metabolic syndrome and limited evidence for a relationship to diabetes [41], those with shift work who already had diabetes experienced more problems maintaining glycaemic control [42].
Interestingly, we found that quality of leadership influenced diabetes risk, but only high-quality leadership carried this effect, referencing those with medium-quality leadership; this did not hold true for low-quality leadership. A potential explanation is that high-quality leadership is important if people with diabetes have experienced support for increased sickness absence or health problems before they were diagnosed with diabetes, i.e. the opposite of the healthy worker effect [43]. More research is needed in this area because it is important to know how management could help employees with diabetes remain productive workers [9]. Alternatively, high-quality leadership may lead to over-commitment [44], which may again entail adverse health outcomes, such as diabetes.
There is scientific support that chronic stress—or, especially, lack of control—might cause diabetes among females. We thought that this cohort would provide insight into the strength of the stress-diabetes link [21]–[23], not least because this cohort has elsewhere identified that psychosocial demands and depression played a role in long-term sickness absenteeism [19]. However, our findings did not support this theory.
Obesity and work
Our results suggest that the occupational setting affects diabetes indirectly through the influence of obesity and physical inactivity. Referring to diabetes as a ‘lifestyle disease’ is misleading, implying that there is something wrong with the character of the employee, when the truth is that what we call ‘lifestyle’ is a combination of structural conditions for health and capacities for coping with both living and working conditions. Based on the present study, the occupational setting may be more important for the prevention of diabetes than previously thought. Our survey confirms that occupational risk factors were associated with obesity to a much higher extent than was seen for diabetes.
Another challenge is that the causes of obesity are tightly interwoven with parallel factors from both working and non-working life. Traditionally, obesity has not been regarded as an occupational health and safety (OHS) issue, but as a matter for workplace health promotion (WHP). However, more than thirty years of WHP have not been able to reverse the rising prevalence of obesity, and initiatives addressing nutrition and physical activities have only showed modest effect [45]–[47]. Lifestyle is not simply a confounder to occupational risk factors; it is both a causal factor and mediator because work has become so much more sedentary [48]. One would have expected health care workers to be in relatively good physical shape because they walk, lift, move a lot and generally have physically demanding work [18], [20]. However, new research shows that the majority of people who are considered to have strenuous physical work may still not reach activity intensity levels that could improve physical capacity [49].
T2DM has hitherto been considered as a condition only affecting the elderly and caused by factors related to individuals' private lives; it has, therefore, viewed as largely irrelevant to OHS. This view will need to be revised as both obesity and diabetes become more prevalent within the working population. Even a small increase in diabetes prevalence will have considerable impact on the labour market. The gradually increasing pension age means that diabetes will occur in many more people while they are still active in the labour market [50]. Instead of continuing with WHP alone, the challenge will be to investigate if it is possible to organise work itself to support and foster health promotion. If so, the occupational arena may be able to contribute much more to the improvement of public health than is the case today.
Strengths and limitations
A study limitation is that all baseline measures, including BMI, were based on self-report. However, self-report is expected to provide a reasonably reliable, albeit conservative, categorisation of obesity vs. non obesity [51]. A second limitation is that the DNDR does not distinguish between type 1 and type 2 diabetes; however, we estimate this had a minimal effect on our findings. Due to the low number of males in the survey, the results might not be generalizable to similar jobs with a different gender distribution. The dichotomous measure of ethnicity is probably too simple, since we know that Non-western populations have a higher diabetes risk than people of Western or Danish origin. However, the relatively low number of ethnic minority health workers hindered further stratification. One of the strengths of the study is the large sample size and high response rate. In addition, our ability to link high quality registers covering the entire Danish population with individually based information on work and lifestyle is unique. The homogenous population is also a strength of the study because it reduces the potential for confounding from the social gradient of health.
Conclusions
In conclusion, diabetes is notably prevalent among health care workers. However, the risk of developing diabetes was mediated through obesity and physical inactivity, which play a causal role whether they are influenced by work or non-work lifestyle factors. Factors from the occupational setting were also associated with obesity. The importance of the occupational setting should therefore be reconsidered in the fight against diabetes. Obesity could be the target for interventions and diabetes would be a suitable disease model for surveillance of long-term effects. Finally, DNDR is a new and promising tool that needs to be explored further to elucidate its future value for monitoring large scale trends in the development of diabetes in the working population.
Funding Statement
This paper is financed by internal funding from Steno Diabetes Center and National Research Centre for the Working Environment. Steno Diabetes Center receives part of its core funding from unrestricted grants from the Novo Foundation and Novo Nordisk A/S. The funder, Steno Diabetes Center, provided support in the form of salaries for authors KP and BC, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Danaei G, Finuance MM, Lu Y, Singh GM, Cowan MJ, et al. (2011) National, regional, and global trends in fasting plasma glucose and diabetes prevalance since 1980: Systematic analysis of health examination survey and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 378: 31–40 10.1016/S0140-6736(11)60679-X [DOI] [PubMed] [Google Scholar]
- 2. Wild S, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes. Estimates for the year 2000 and projections for 2030. Diabetes Care 27: 1047–1053 10.2337/diacare.27.5.1047 [DOI] [PubMed] [Google Scholar]
- 3. Tobias M (2011) Global control of diabetes: information for action. Lancet 378: 3–4 10.1016/S0140-6736(11)60604-1 [DOI] [PubMed] [Google Scholar]
- 4. Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, et al. (2011) National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination survey and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 377: 557–567 10.1016/S0140-6736(10)62037-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Breton M-C, Guénette L, Amiche MA, Kayibanda J-F, Grégoire J-P, et al. (2013) Burden of diabetes on the ability to work: A systematic review. Diabetes Care 36: 740–749 10.2337/dc12-0354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Herquelot E, Gueguen A, Bonenfant S, Dray-Spira R (2011) Impact of diabetes on work cessation: Data from the GAZEL cohort study. Diabetes Care 34: 1344–1349 10.2337/dc10-2225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Seeger R, Lehmann R (2011) [Driving ability and fitness to drive in people with diabetes mellitus]. Ther Umsch 68: 249–252 10.1024/0040-5930/a000159 [DOI] [PubMed] [Google Scholar]
- 8. Tunceli K, Bradley CJ, Nerenz D, Williams LK, Pladevall M, et al. (2005) The impact of diabetes on employment and work productivity. Diabetes Care 28: 2662–2667 10.2337/diacare.28.11.2662 [DOI] [PubMed] [Google Scholar]
- 9. Lavigne JE, Phelps CE, Mushlin A, Lednar WM (2003) Reductions in individual work productivity associated with type 2 diabetes mellitus. Pharmacoeconomics 21: 1123–1134 PubMed: 14596631. [DOI] [PubMed] [Google Scholar]
- 10. Ramsey S, Summers SK, Leong SA, Birnbaum HG, Kemner JE, et al. (2002) Productivity and medical costs of diabetes in a large employer population. Diabetes Care 25: 23–29 10.2337/diacare.25.1.23 [DOI] [PubMed] [Google Scholar]
- 11. Harris SB, Khunti K, Landin-Olsson M, Galbo-Jørgensen CB, Bøgelund M, et al. (2013) Descriptions of health states associated with increasing severity and frequency of hypoglycemia: a patient-level perspective. Patient Prefer Adherence 7: 925–936 10.2147/PPA.S46805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hempler NF, Ekholm O, Willaing I (2013) Differences in social relations between persons with type 2 diabetes and the general population. Scand J of Public Health 41: 340–343 10.1177/1403494813482535 [DOI] [PubMed] [Google Scholar]
- 13. Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuck A (2011) Type 2 diabetes incidence and socio-economic position: A systematic review and meta-analysis. Int J Epidemiol 40: 804–818 10.1093/ije/dyr029 [DOI] [PubMed] [Google Scholar]
- 14. Robroek SJ, Reeuwijk KG, Hillier FC, Bambra CL, van Rijn RM, et al. (2013) The contribution of overweight, obesity, and lack of physical activity to exit from paid employment: A meta-analysis. Scand J Work Environ Health 39: 233–240 10.5271/sjweh.3354 [DOI] [PubMed] [Google Scholar]
- 15. Hansen MB, Jensen ML, Carstensen B (2012) Causes of death among diabetes patients in Denmark. Diabetologia 55: 294–302 10.1007/s00125-011-2383-2 [DOI] [PubMed] [Google Scholar]
- 16. Jensen JN, Holtermann A, Clausen T, Mortensen OS, Carneiro IG, et al. (2012) The greatest risk for low-back pain among newly educated female health care workers: Body weight or physical work load? BMC Musculoskelet Disord 13: 1–6 10.1186/1471-2474-13-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hannerz H, Tüchsen F, Spangenberg S, Albertsen K (2004) Industrial differences in disability retirement rates in Denmark, 1996–2000. Int J Occup Med Environ Health 17: 465–471 PubMed: 15852761 [PubMed] [Google Scholar]
- 18. Andersen LL, Burdorf A, Fallentin N, Persson R, Jakobsen MD, et al. (2013) Patient transfers and assistive devices: Prospective cohort study on the risk for occupational back injury among healthcare workers. Scand J Work Environ Health 10.5271/sjweh.3382 [DOI] [PubMed] [Google Scholar]
- 19. Clausen T, Nielsen K, Carneiro IG, Borg V (2011) Job demands, job resources and long-term sickness absence in the Danish eldercare service: A prospective analysis of register-based outcomes. J Adv Nurs 68: 127–136 10.1111/j.1365-2648.2011.05724.x [DOI] [PubMed] [Google Scholar]
- 20. Clausen T, Andersen LL, Holtermann A, Jorgensen AF, Aust B (2013) Do self-reported psychosocial working conditions predict low back pain after adjustment for both physical work load and depressive symptoms? A prospective study among female eldercare workers. Occup Environ Med 70: 538–544 10.1136/oemed-2012-101281 [DOI] [PubMed] [Google Scholar]
- 21. Heraclides A, Chandola T, Witte DR, Brunner EJ (2009) Psychosocial stress at work doubles the risk of type 2 diabetes in middle-aged women: Evidence from the Whitehall II study. Diabetes Care 32: 2230–2235 10.2337/dc09-0132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Norberg M, Stenlund H, Lindahl B, Andersson C, Eriksson JW, et al. (2007) Work stress and low emotional support is associated with increased risk of future type 2 diabetes in women. Diab Res Clin Pract 76: 368–377 10.1016/j.diabres.2006.09.002 [DOI] [PubMed] [Google Scholar]
- 23. Agardh E, Ahlbom A, Andersson T, Effendic S, Grill V, et al. (2003) Work stress and low sense of coherence is associated with type 2 diabetes in middle-aged Swedish women. Diabetes Care 26: 719–724 PubMed: 12610028. [DOI] [PubMed] [Google Scholar]
- 24. Chandola T, Brunner E, Marmot M (2006) Chronic stress at work and the metabolic syndrome: Prospective study. BMJ 332: 521–526 10.1136/bmj.38693.435301.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Catalina-Romero C, Calvo E, Sánchez-Chaparro MA, Valdivielso P, Sainz JC, et al. (2013) The relationship between job stress and dyslipidemia. Scand J Public Health 41: 142–149 10.1177/1403494812470400 [DOI] [PubMed] [Google Scholar]
- 26. Carstensen B, Kristensen JK, Marcussen MM, Borch-Johnsen K (2011) The National Diabetes Register. Scand J Public Health 39: 58–61 10.1177/1403494811404278 [DOI] [PubMed] [Google Scholar]
- 27. Lynge E, Sandegaard JL, Reboli M (2011) The Danish National Patient Register. Scand J Public Health 39: 30–33 10.1177/1403494811401482 [DOI] [PubMed] [Google Scholar]
- 28. Andersen JS, Olivarius NDF, Krasnik A (2011) The Danish National Health Service Register. Scand J Public Health 39: 34–37 10.1177/1403494810394718 [DOI] [PubMed] [Google Scholar]
- 29. Kildemoes HW, Sørensen HT, Hallas J (2011) The Danish National Prescription Registry. Scand J Public Health 39: 38–41 10.1177/1403494810394717 [DOI] [PubMed] [Google Scholar]
- 30. Carstensen B, Kristensen JK, Ottosen P, Borch-Johnsen K (2008) The Danish National Diabetes Register: trends in incidence, prevalence and mortality. Diabetologia 51: 2187–2196 10.1007/s00125-008-1156-z [DOI] [PubMed] [Google Scholar]
- 31. Thygesen LC, Ersbøll AK (2011) Danish population-based registers for public health and health-related welfare research: Introduction to the supplement. Scand J Public Health 39: 8–10 10.1177/1403494811409654 [DOI] [PubMed] [Google Scholar]
- 32. Pedersen CB (2011) The Danish Civil Registration System. Scand J Public Health 39: 22–25 10.1177/1403494810387965 [DOI] [PubMed] [Google Scholar]
- 33. Andersen LL, Clausen T, Burr H, Holtermann A (2012) Threshold of musculoskeletal pain intensity for increased risk of long-term sickness absence among female healthcare workers in eldercare. PLoS One 7: 1–6 10.1371/journal.pone.0041287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sundhedsstyrelsen (2007) [Referenceprogram for unipolar depression hos voksne]. 1–137 Available:. Accessed 13 December 2013. [Google Scholar]
- 35. Pejtersen JH, Kristensen TS, Borg V, Bjorner JB (2010 February) http://www.sst.dk/publ/publ2007/plan/sfr/sst_dep.rapport.pdf The second version of the Copenhagen Psychosocial Questionnaire. Scand J Public Health 38: 8–24 10.1177/1403494809349858 [DOI] [PubMed] [Google Scholar]
- 36.Hosmer DW, Lemeshow S (1989) Applied logistic regression. New York: John Wiley & Sons Inc. 300 p. [Google Scholar]
- 37. Andersen LL, Clausen T, Mortensen OS, Burr H, Holtermann A (2011) A prospective cohort study on musculoskeletal risk factors for long-term sickness absence among healthcare workers in eldercare. Int Arch Occup Environ Health 85: 615–622 10.1007/s00420-011-0709-5 [DOI] [PubMed] [Google Scholar]
- 38. Karlson B, Carlsson F, Hansen ÅM, Garde AH, Österberg K, et al. (2006) Diurnal cortisol pattern of shift workers on a workday and a day off. Scand J Work Environ Health Suppl 2: 27–34 Available: http://www.sjweh.fi/show_abstract.php?abstract_id=1041. Accessed 13 December 2013. [Google Scholar]
- 39. Karlsson B, Alfredsson L, Knutsson A, Andersson E, Torén K (2005) Total mortality and cause-specific mortality of Swedish shift- and dayworkers in the pulp and paper industry in 1952–2001. Scand J Work Environ Health 31: 30–35 PubMed: 15751616. [DOI] [PubMed] [Google Scholar]
- 40. Morikawa Y, Nakagawa H, Miura K, Soyama Y, Isizaki M, et al. (2005) Shift work and the risk of diabetes mellitus among Japanese male factory workers. Scand J Work Environ Health 31: 179–183 10.5271/sjweh.867 [DOI] [PubMed] [Google Scholar]
- 41. Wang XS, Armstrong ME, Cairns BJ, Key TJ, Travis RC (2011) Shift work and chronic disease: The epidemiological evidence. Occup Med 61: 78–89 10.1093/occmed/kqr001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Knutsson A, Kempe A (2013) [Systematiska kundskabsöversikter; 4. Diabetes och arbete]. Arbete och Hälsa 47: 1–56 Available: https://gupea.ub.gu.se/bitstream/2077/32883/4/gupea_2077_32883_4.pdf. Accessed 13 December 2013. [Google Scholar]
- 43. Li CY, Sung FC (1999) A review of healthy worker effect in occupational epidemiology. Occup Med 49: 225–229 PubMed: 10474913. [DOI] [PubMed] [Google Scholar]
- 44. Tsutsumi A, Kawakami N (2004) A review of empirical studies on the model of effort-reward imbalance at work: Reducing occupational stress by implementing a new theory. Soc Sci Med 59: 2335–2359 PubMed: 15450708. [DOI] [PubMed] [Google Scholar]
- 45. Kahn-Marshall JL, Gallant MP (2012) Making healthy behaviors the easy choice for employees: A review of the literature on environmental and policy changes in worksite health promotion. Health Educ Behav 39: 752–776 10.1177/1090198111434153 [DOI] [PubMed] [Google Scholar]
- 46. Anderson LM, Quinn TA, Glanz K, Ramirez G, Kahwati LC, et al. (2009) The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: A systematic review. Am J Prev Med 37: 340–357 10.1016/j.amepre.2009.07.003 [DOI] [PubMed] [Google Scholar]
- 47. Rongen A, Robroek SJ, van Lenthe FJ, Burdorf A (2013) Workplace health promotion. A meta-analysis of effectiveness. Am J Prev Med 44: 406–415 10.1016/j.amepre.2012.12.007 [DOI] [PubMed] [Google Scholar]
- 48. Adler NE, Newman K (2002) Socioeconomic disparities in health: pathways and policies. Health Affairs 21: 60–76 10.1377/hlthaff.21.2.60 [DOI] [PubMed] [Google Scholar]
- 49. Jakobsen MD, Sundstrup E, Persson R, Andersen CH, Andersen LL (2013) Is Borg's perceived exertion scale a useful indicator of muscular and cardiovascular load in blue-collar workers with lifting tasks? A cross-sectional workplace study. Eur J Appl Physiol 1–10 10.1007/s00421-013-2782-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Marmot MG (2010) Fair society, healthy lives. The Marmot review 1–242 Available: http://www.ucl.ac.uk/whitehallII/pdf/FairSocietyHealthyLives.pdf. Accessed 13 December 2013. [Google Scholar]
- 51. Grosschädl F, Haditsch B, Stronegger WJ (2011) Validity of self-reported weight and height in Austrian adults: sociodemographic determinants and consequences for the classification of BMI categories. Public Health Nutr 15: 20–27 10.1017/S1368980011001911 [DOI] [PubMed] [Google Scholar]