Abstract
Background
Autism prevalence in California, based on persons eligible for state-funded services, rose throughout the 1990s. The extent to which this trend is explained by changes in age at diagnosis or inclusion of milder cases has not been previously evaluated.
Methods
Autism cases were identified from 1990 through 2006 in databases of the California Department of Developmental Services, which coordinates services for persons with specified developmental disorders. The main outcomes were population incident cases younger than age 10 for each quarter, cumulative incidence by age and birth year, age-specific incidence rates stratified by birth year, and proportions of diagnoses by age across birth years.
Results
Autism incidence in children rose throughout the period. Cumulative incidence to 5 years of age per 10,000 births rose consistently from 6.2 for 1990 births to 42.5 for 2001 births. Age-specific incidence rates increased most steeply for 2- and 3-year olds. The proportion diagnosed by age 5 increased only slightly, from 54% for 1990 births to 61% for 1996 births. Changing age at diagnosis can explain a 12% increase, and inclusion of milder cases, a 56% increase.
Conclusions
Autism incidence in California shows no sign yet of plateauing. Younger ages at diagnosis, differential migration, changes in diagnostic criteria and inclusion of milder cases do not fully explain the observed increases. Other artifacts have yet to be quantified, and as a result, the extent to which the continued rise represents a true increase in the occurrence of autism remains unclear.
Autism is a pervasive developmental disorder involving deficits in 3 domains: social skills, communication, and repetitive behaviors or restricted interests, all before 36 months of age.1,2 Current estimates of prevalence for all pervasive developmental disorders are in the range of 20 to 80 per 10,000 persons.3–5 Numbers of diagnoses have been rising in recent decades, but the relative contributions from heightened awareness, changes in definitions, more complete ascertainment, improved diagnosis, greater funding for services, and an increased desire of parents to seek services for affected children are difficult to determine.
In California, the Lanterman Developmental Disabilities Services Act, passed in 1969 and amended numerous times over the subsequent 6 years, guarantees that all persons with developmental disabilities can receive age-appropriate services for specified conditions (autism, mental retardation, cerebral palsy and epilepsy).6 During that period, the paradigm for services to persons with disabilities was shifting from the medical model to the developmental model, a change implemented by state and national policies. By 1976, 21 Regional Centers were established in California to administer and coordinate those services in a community rather than institutional setting. Administrative databases from these Regional Centers are now compiled centrally by the Department of Developmental Services (DDS) and have been analyzed to track trends in developmental disabilities.7–10
Croen and colleagues7 demonstrated an increasing prevalence of autism among births in 1987 through 1994; the trend was independent of maternal age, education, race, ethnicity, and parity. Similar patterns were reported for cumulative incidence of autism to 48 months of age.11 Although the authors initially concluded that the increase was due to a shift of diagnoses from the category of mental retardation, a reanalysis demonstrated that diagnostic substitution could not explain the increase. The state caseload data were recently used to argue that autism incidence in California began to decline in 2002.12 However, caseload statistics do not provide valid information about persons newly diagnosed. A recent study analyzing DDS data reported consistent increases in prevalence of autism from birth years 1989–2003 for each estimated age older than 2 years.13 However, an error-prone method was used to assign age at diagnosis, leading to serious underestimates for young ages.
To clarify the most recent trends in autism incidence in California and to evaluate the contribution of declines in age at diagnosis, we analyzed DDS data from 1990 through 2006, as well as Census and birth data. We conducted 2 sets of analyses evaluating 1) quarterly incidence rates by using Census population estimates, and 2) cumulative incidence proportions by year of birth, and age-specific incidence rates and proportions based on California births. The protocol for this study was approved by Institutional Review Boards for the Protection of Human Subjects of the State of California and of the University of California, Davis. Unlike Schecter & Grether,13 our goal was not to conduct an ecologic correlation analysis with any particular exposure but to quantify the trends in autism by using rigorous methodology – focusing on cumulative incidence to an age beyond which few cases are diagnosed. We also identify faulty assumptions (especially regarding age at diagnosis) in a simulation study that attempted to assess the contributions to time trends in autism from artifacts such as changes in definition, age at diagnosis, and ascertainment.
Methods
Identification of Autism Cases in California
Clients of the DDS Regional Centers aged 3 years and older undergo periodic evaluations that are recorded on a Client Development Evaluation Report. These electronic files were obtained from DDS for the period 1990 through 2006. Records for the Early Start Report, used for children younger than 3 years of age, were obtained from the program’s startup phase in 1993–1995 through the end of 2006. Clients who met any of the following criteria were included as cases of autism 1) an autism level of 1 (full syndrome autism) on any Client Development Evaluation Report, 2) an International Classification of Diseases (ICD) code of 299.0 (autistic disorder) in any field in which ICD codes could be noted on either a Client Development Evaluation Report, or an Early Start Report, or 3) a checkmark for “autism” under developmental disabilities in an Early Start Report. For each child, we used the earliest date on which 1 of the criteria was met. A total of 31,307 cases up to age 10 had a first report of autism during the period 1990 through 2006. Of these, 30,832 (98.5%) had an autism designation on the Client Developmental Evaluation Reports, whereas 475 (1.5%) had an autism designation on an Early Start Report only. Among children 4 years of age or older at the end of 2006, 87% of those who ever had an autism designation on an Early Start Report also had it on a Client Development Evaluation Report, that is, after their third birthday.
Calculation of Population Incidence Rates
Dates of onset of autism were not known. Month and year of diagnosis was recorded on 87% of the Client Development Evaluation Reports; 74% of these records were within 3 months of the diagnosis whereas 93% were within 12 months. Because of missing diagnosis dates, we used the earliest date of a DDS record with autism noted. Population incidence rates were determined for children ages 0–4 years and 5–9 years by using Census data to derive denominators. For the numerator, we multiplied the number of newly reported cases of autism in the age group during each quarter by 4 to give an equivalent annual rate for the quarter. Annual California population estimates were obtained from the U.S. Census Bureau, including intercensal estimates. Given that we used full population data (i.e., no sampling), random error would not be present; hence standard errors were not calculated. We applied the SAS14 LOESS nonparametric method for estimating regression curves to both age ranges. The averaging period for each data point is chosen so that the neighborhood contains a specified percentage of the data points.
Matching Cases to Birth Records
For the California birth cohort analyses, it was necessary to exclude children with autism in the DDS database who were born outside California. Confidential birth records were obtained from the California Department of Health Services for the years 1990 through 200315 as well as the Client Master File from DDS. For each autism case born in those years, we conducted a computerized search for a match based on child’s first and last name, and date and place of birth; mother’s first name and maiden name, date of birth, and social security number; and father’s first name, date of birth, and social security number. Father’s first name and parents’ social security numbers were not available from 1990 through 1995. Questionable matches were reviewed by hand. Match rates (excluding children known to be born outside California) for birth years 1990 to 1995 were 88%, 89%, 90%, 89%, 90%, and 90%. Match rates for years 1996–2003 were 92%, 94%, 94%, 95%, 95%, 95%, 95%, and 95%. The overall match rate was 93%. Of the cases not matched, the DDS record indicated that 15% were born in California, 55% outside California, and the remainder not recorded. We excluded unmatched cases from the cohort analysis rates, but inclusion had a negligible impact (differences for each year were <1.1 per 10,000) on results. A total of 26,761 children with autism born 1990 through 2003 were matched to their California birth record.
Birth Cohort Analyses
Cumulative incidence by age and birth cohort for years 1990 through 2003 was determined for the first ten years of life, that is, through age 9, or up to the age achieved on their birthday in 2006 for birth years 1997 or later. We subtracted infant deaths from the number of live births to calculate denominators.15,16 Age at diagnosis was defined as age at first appearance in the DDS Regional Center system with an autism diagnosis. For each birth year, the number of children with autism diagnosed before each age (2–10 years) was divided by the total number of children at risk (births minus infant deaths) in that birth cohort.
Trends in age-specific incidence rates for birth cohorts for 1990–2003 were examined for children ages 2 through 9. For each birth year, the number of children in whom autism was diagnosed at each age was divided by the total number of children at risk in the birth cohort. We assessed the trends in the proportion of diagnoses at each age as a fraction of all diagnoses by age 10.
We excluded from the case group, children with their first autism designation in the DDS system at age 10 years or older. Births to mothers living outside California at the time of delivery were excluded from both the numerator and denominator.
Results
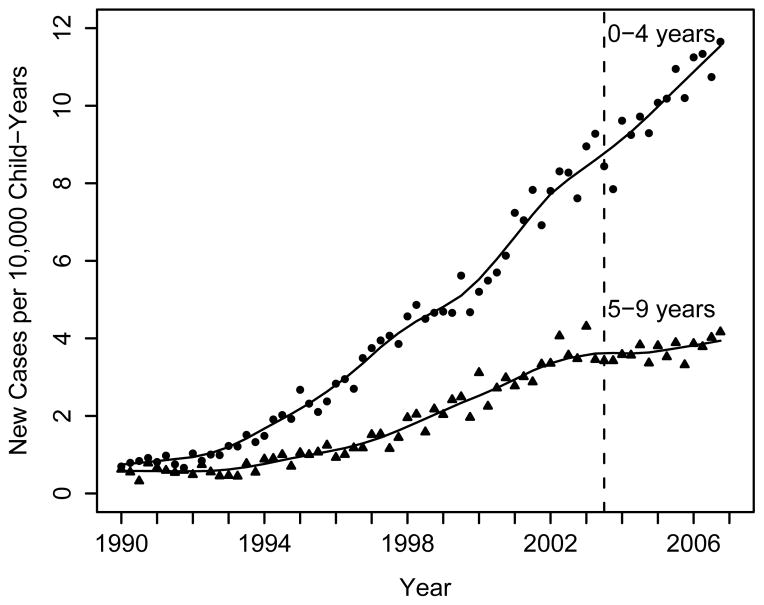
Table 1 shows numbers of new autism cases at ages 0–4, the size of the population, and annual incidence rates for each quarter from 1990 to 2006. These and corresponding data for 5–9 year olds demonstrate a slow rise in new cases of autism in children younger than 10 years of age during the early 1990s, followed by a steeper rise in the late 1990s and early 2000s (Fig. 1). The rates for 0–4 year olds continued to rise through 2006 whereas rates for 5–9 year olds were leveling off by 2003.
Table 1.
Numbers and Rates of New Cases of Autism in the California DDS System, 1990–2006, for Children Under 5 Years of Age. Rates are Per 10,000 Person Years.
| Year | No. | Rate | Population Estimate 0–4 Y |
|---|---|---|---|
| 1990 | 205 | 0.8 | 2,534,451 |
| 1991 | 213 | 0.8 | 2,664,214 |
| 1992 | 266 | 1.0 | 2,752,513 |
| 1993 | 370 | 1.3 | 2,807,471 |
| 1994 | 519 | 1.8 | 2,829,617 |
| 1995 | 662 | 2.4 | 2,797,903 |
| 1996 | 816 | 3.0 | 2,726,617 |
| 1997 | 1,029 | 3.9 | 2,635,231 |
| 1998 | 1,189 | 4.7 | 2,557,813 |
| 1999 | 1,227 | 4.9 | 2,499,258 |
| 2000 | 1,403 | 5.6 | 2,491,907 |
| 2001 | 1,817 | 7.3 | 2,503,706 |
| 2002 | 2,022 | 8.0 | 2,527,918 |
| 2003 | 2,221 | 8.6 | 2,574,005 |
| 2004 | 2,482 | 9.5 | 2,621,554 |
| 2005 | 2,757 | 10.4 | 2,663,441 |
| 2006 | 3,011 | 11.2 | 2,678,019 |
Figure 1.
Annual incidence rates of autism based on the administrative database of the California Department of Developmental Services, 1990 through 2006, by quarter. Each point represents the number of new cases in each quarter divided by the population of children in the respective age group at the midpoint of the year (an estimate of the number of child-quarter-years), and then multiplied by 4 to obtain an annualized rate. The fitted lines represent smoothed loess curves and the vertical line at year 2003 quarter 3 is the time at which access to state services became more restrictive (see Discussion).
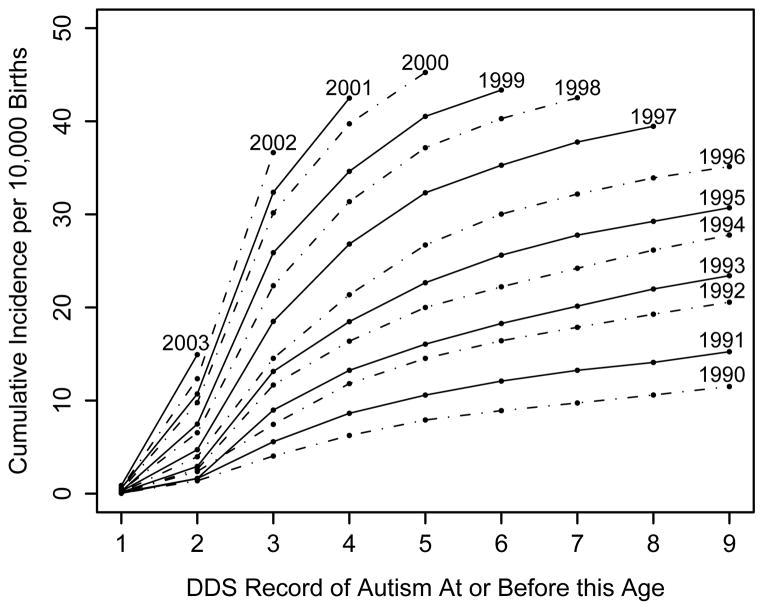
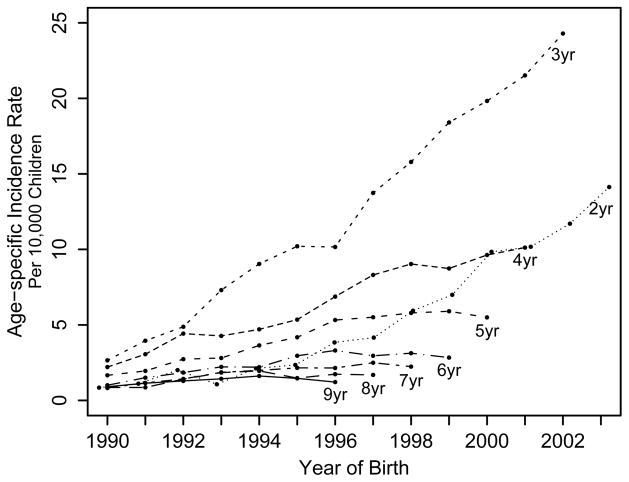
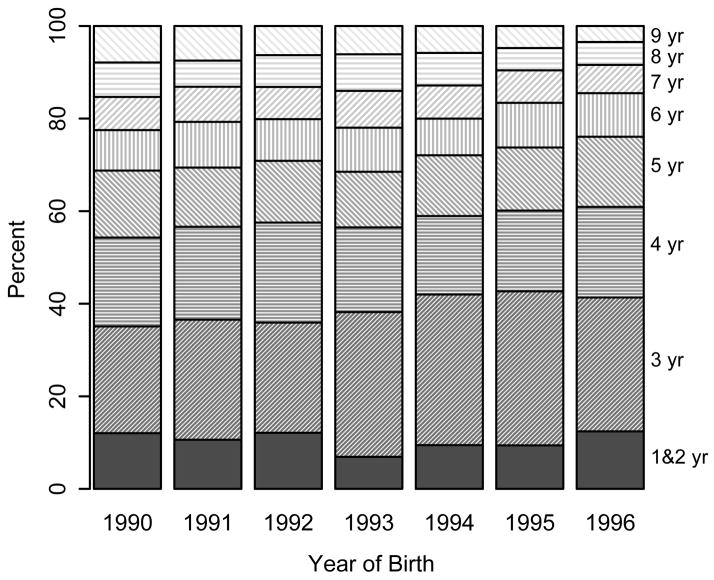
Cumulative incidence proportions are shown for each birth cohort, 1990 to 2003, as it ages from 1 to 9 years (Fig. 2). With each successive year of births, cumulative incidence increased, and this was true at every age above 2 years. For instance, at age 6, the cumulative incidence of autism was 8.9 in the 1990 birth cohort, 22.2 in the 1994 birth cohort, and 40.3 in the 1998 birth cohort. Increasing trends were observed for all races, all categories of mother’s or father’s age, both sexes, all education levels of parents, and any payment method for delivery of child (data not shown). Age-specific incidence rates (Fig 3) indicate the steepest rise over time in children 3 years of age, followed by 2-year olds, 4-year olds, and successively older ages. The proportional shift in age at DDS report of autism is shown explicitly in Figure 4: Children are appearing at California’s Regional Centers at younger ages, even as total diagnoses have been increasing. The proportion diagnosed by age 5 rose from 54% for 1990 births to 61% for 1996 births.
Figure 2.
Cumulative incidence of autism by birth cohort from 1990 to 2003, at ages 1 through 9 years, California Departmental of Developmental Services database.
Figure 3.
Age-specific incidence rates of autism, births 1990 through 2003, California Departmental of Developmental Services database.
Figure 4.
Proportion of cases with first record of autism in the California Departmental of Developmental Services database at each age. Ages 1 through 9, by year of birth.
Discussion
Based on administrative data from the California DDS Regional Center system, the annual number of new cases of autism has continued to rise in California, especially among preschool aged children. These trends are generally consistent with a recent analysis of the state’s Client Developmental Evaluation Record data.13 However, because we used data from the Early Start Reports for younger children in addition to the data on children aged 3 and older, and because we used the true age of the child rather than a crude estimate based on date of record archival, our rates for 2- and 3-year olds are more accurate. Our analysis shows substantially higher rates of autism among 3-year olds than those previously published.
Changes in Definitions and Ascertainment
The rise in autism incidence has occurred during a time of diagnostic and legislative changes affecting the definition of autism and the availability of services for developmental disabilities. In the late 1980s a revision of DSM-III (DSM-III-R) expanded the definition of autism. However, this expansion was considered “overly broad,”17 and the 1994 implementation of the ICD-101 was more restrictive and considered appropriately reflective of clinician practices.17 The DSM-IV criteria matched closely the ICD-10, but used a more compact set of qualifying behaviors.2,17. A study in northern Finland compared the prevalence proportions obtained using a Kanner definition to those obtained from ICD-10 and DSM-IV criteria in close to 1000 children and adolescents with autism or other developmental or psychiatric conditions.18 The application of two sets of criteria to the entire sample indicated a 2.2-fold higher prevalence using the more recent diagnostic criteria (12.2 vs. 5.6 per 10,000). A meta-analysis of 37 studies of autism prevalence found a 3.6-fold higher risk from DSM-IV or ICD-10 criteria vs. other criteria, but this figure would have been confounded by year of study.19 Thus, an expanded definition potentially increased the numbers in California who met criteria for autism and may have been partially responsible for changes from the early 1990s to 2006, as it can take years for practitioners to adopt new diagnostic standards.
In the third quarter of 2003, the state eligibility criteria changed from having a condition that results in “a major impairment of cognitive and/or social functioning” to additionally having “significant functional limitations, as determined by the regional center, in 3 or more of the following areas of major life activity, as appropriate to the person’s age: receptive and expressive language, learning, self-care, mobility, self-direction, capacity for independent living, and economic self-sufficiency.” Despite these additional qualifying criteria, the autism incidence continued to rise in preschool aged children. It has, however, leveled off above age 4, possibly reflecting fewer severe functional limitations20 in those diagnosed at a later age.
The inclusion of milder cases has been suggested as an explanation for the increase in autism. Neither Asperger’s syndrome nor “pervasive developmental disorders not otherwise specified” qualify under the category of autism in the DDS system. In the CHARGE study (Childhood Autism Risks from Genetics and the Environment), which enrolls children from 20 California counties, 64% of the cases of autism recorded in the state system for 2–5 year olds were confirmed by 2 standardized, research-reliable instruments (Autism Diagnostic Observation Schedule21 and Autism Diagnostic Inventory22), 87% were confirmed by at least 1 of the instruments, and 98% met criteria for autism spectrum disorders based on at least 1 of the instruments.23 Some children not meeting the criteria for full syndrome autism may have met the criteria previously but improved through treatment prior to the CHARGE study evaluation. These confirmation proportions are only from recent years; in the most extreme scenario, if all cases in the early years met criteria on both instruments, these data might suggest a 56% rise (100%/64%) due to a trend towards providing services to milder cases.
Age at Diagnosis
A shift toward younger age at diagnosis was clear but not huge: 12% more children were diagnosed before age 5 in the 1996 birth cohort (the most recent with ten years of follow-up) compared with the 1990 cohort. No corresponding decline in diagnoses occurred in school-aged children, and only in the last few years has the rate of diagnosis at ages 5–9 begun to level off. Calculating cumulative incidence to an older age (such as age 10) minimizes the affect of decreasing age of diagnosis because diagnoses above this cutpoint are infrequent. Shifts from above to below this cutpoint would tend to be minimal and affect primarily mild cases, thus likely playing a minor role in our analysis.
Inappropriate use of prevalence and other measures of occurrence can engender the problem of noncomparability. Prevalence data or incidence data in earlier years in the younger ages will miss cases who have not yet been diagnosed. Also, if increasing awareness is a major factor in time trends, an unknown number of undiagnosed cases in the oldest age groups will disproportionately affect rates or proportions in the earlier years. Jick and Kaye,24 calculated annual incidence rates in children 24–59 months old in the large General Practice Research Database from the United Kingdom within a defined 7-year birth cohort, but as noted elsewhere,25 the earliest year of the analysis included only 2-year olds, and the most recent births were only 3 years old in the later years used for the trend analysis. This meant different opportunities for a diagnosis across time. A later analysis of this database reported a peak in 1999 with a leveling off after 2000,26 a pattern quite different from our population incidence findings of a continued rise throughout the same period and well beyond. In any case, because of the relatively young cut-off (59 months), their estimates could also have been influenced by a change in age at diagnosis. However, the common practice of calculating prevalence over a broad age range can also produce biased comparisons across time. In general, cumulative incidence is a more valid measure than prevalence for assessment of time trends; it avoids the problem of noncomparability across years due to changing age at diagnosis when calculated to an age beyond which diagnoses are rare.
A simulation study by Wazana and colleagues27 suggests that an apparent increase of as much as 28-fold could be explained by the combination of 3 artifacts: a change in case definition, a decline in age at diagnosis, and better ascertainment. Several problems with this analysis detract from its validity and applicability. First, the data they use for the decline in mean age at diagnosis are based on noncomparable cohorts. Specifically, they rely on a report by Croen et al,7 who used follow-up to a specific calendar date rather than to a specific age. This inflates the decline in age at diagnosis because calculations for recent birth cohorts cannot include those diagnosed at older ages. Using longer follow-up and equivalent follow-up periods, we recalculated the mean age at diagnosis for birth cohorts from 1990 to 1996 to be 5.23, 5.16, 5.12, 5.18, 5.02, 4.90, 4.83, a ten-fold smaller shift (0.14 years between 1991 and 1994) than what was assumed in the simulation study (1.6 years), but consistent with our Figure 4. Secondly, the extremely large increases found in the simulation are observed only in the analysis of cumulative incidence to age 4 (labeled “prevalence” by the authors).27 When the simulation is carried out to age 12, the magnitude of the explained increase is much less. By this age, the impact of age at diagnosis is largely eliminated, and the magnitude of artifactual increases that result from the other 2 assumptions (change in definition and more efficient ascertainment) combine to a 2.4-fold increase. This prediction is much smaller than the actual increases in autism rates in the California DDS data, even if we assume, as Wazana et al did, that all clinicians were using DSM-III in the early period (unlikely, given that DSM-III-R had already been adopted) and all clinicians were using DSM-IV at the end of our study period.
Migration
Our birth cohort analysis assumed that out-migration was independent of whether a child developed autism. If out-migration were differential, the population incidence rates or cumulative incidence proportions could be slightly under- or overestimated. In either case, out-migration would not have affected overall trends unless the differential also varied substantially over time. Domestic out-migration from California is low—about 1.4% per year among children 0–10 years of age.
Access
Programmatic and financial changes implemented in this time period could have affected access to state-funded services. In the 1980s, services for persons with developmental disabilities became Medicaid reimbursable. From the early 1990s to 2002, State of California funding for family services for persons with developmental disabilities rose from about $60 million to over $300 million, and total spending for individual, family, and community services increased from $2.2 billion to $3.7 billion.28 Although these figures include funds for cerebral palsy, epilepsy, and mental retardation, the population prevalence proportions of these other conditions have remained stable.10 In 1986, state legislation in California mandated preschool programs for 3–5 year olds who have disabilities or who are at risk. Implementation of the Early Start program was initiated in 1993, reaching statewide coverage by about 1995. The federal Education of the Handicapped Act was amended in 1990 to include children with autism.29
Comparison of DDS Rates with Rates From Other Populations
A review of studies completed between 1998 and 2001 from several countries concluded that the prevalence of autism is about 13 per 10,000 persons and for pervasive developmental disorders more generally, 37 per 10,000 persons.4 Data from educational systems or administrative databases alone tend to indicate lower proportions, whereas recent investigations using intensive screening or multiple ascertainment sources obtain higher figures: a range of 58–67 cases of pervasive developmental disorder per 10,000. 3,30–32 The CDC’s Autism and Developmental Disabilities Monitoring network found prevalence of autism spectrum disorders (ASD), defined as autistic disorder, Asperger’s syndrome, and pervasive developmental disorder not otherwise specified, at age 8 years ranged from 45 to 99 per 10,000 across 6 sites.33 The CDC use of a single age likely produced data more comparable with our cumulative incidence measure, and by age 8, also avoided much of the bias associated with changing age at diagnosis. By comparison, the cumulative incidence of autism (not the broader category of ASDs) through 9 years of age, based on the California State data, was about 30 per 10,000 for the 1995 California birth cohort, and will certainly exceed 40 per 10,000 for the 2000 and 2001 birth cohorts. These figures are higher than most published estimates for autism alone but may be inflated by inclusion of some ASD cases.
However, because the State of California does not perform active autism surveillance, these figures underestimate the true autism incidence. Whereas many children with autism enter the state system well beyond the age of 3 years (when symptoms are by definition already present) some may never enter. These include those who receive services through the educational system, those whose families can afford private providers, those whose parents are undocumented immigrants (who are eligible for services but may fear contact with state agencies), or whose parents are mentally or physically ill, and others. Underrepresentation of this type, however, is unlikely to have changed so as to explain the observed long-term trends: an 8-fold rise in annual new cases in 16 years, and a 7-fold increase in cumulative incidence over 11 birth cohorts.
One strength of this study relative to many other analyses of time trends is the reliance on a single administrative database with consistent study methodology over a 12–15 year period covering a well-defined geographic region. Another is our use of cumulative incidence to a fixed follow-up age, beyond which few diagnoses occur, to compare birth cohorts. The data presented here would not be subject to varying study methods, but would be affected by community awareness—which has grown in the general public as well as among health providers. Also, the availability of early treatment programs has sparked hope for improvement of those affected, which could also contribute to the increased numbers seeking services. The increased funding of services may have attracted more families to the Regional Centers. However, the demand for services for persons with autism has tended to outstrip supply, suggesting the rise is not simply artifact fueled by federal and state funding. Similarly, although state funding for Regional Centers increased during 1992–1997 as the federal government raised the ceiling on Medicaid eligibility numbers, increases in autism incidence continued well beyond this period.
In summary, the incidence of autism rose 7- to 8-fold in California from the early 1990s through the present. Quantitative analysis of changes in diagnostic criteria, inclusion of milder cases, and an earlier age at diagnosis suggests that these factors probably contribute 2.2-fold, 1.56-fold, and 1.12-fold increases in autism, and hence cannot fully explain the magnitude of the rise in autism. Differential migration also likely played a minor role, if any. Wider awareness, greater motivation of parents to seek services as a result of expanding treatment options, and increased funding may each have contributed, but documentation or quantification of these effects is lacking. With no evidence of a leveling off, the possibility of a true increase in incidence deserves serious consideration. One approach to this question would be a rigorous investigation to determine incidence or prevalence in 20–30-year olds. If there has been no true increase and no individuals who were cured or outgrew their diagnosis, then application to adults of criteria equivalent to those being used today in children should find, for each previously identified autism case, 4 to 8 undiagnosed cases. Whatever the final determination with regard to overlooked cases of autism in the past, the current occurrence of autism, a seriously disabling disorder in young children, at rates of greater than 30 per 10,000 – and still rising in California– is a major public health and educational concern.
Acknowledgments
We thank the Data Extraction Unit of the California Department of Developmental Services for providing data files.
Funding: Supported by grants from the National Institute of Environmental Health Sciences 1P01-ES11269, 2P01-ES11269, 1R01-ES015359 and by the Medical Investigations of Neurodevelopmental Disorders (M.I.N.D.) Institute.
References
- 1.International Classification of Diseases, Tenth Revision (ICD-10) Geneva: World Health Organization; 1994. [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: APA; 1994. (DSM-IV) [Google Scholar]
- 3.Chakrabarti S, Fombonne E. Pervasive developmental disorders in preschool children: confirmation of high prevalence. Am J Psychiatry. 2005;162(6):1133–41. doi: 10.1176/appi.ajp.162.6.1133. [DOI] [PubMed] [Google Scholar]
- 4.Fombonne E. Epidemiology of autistic disorder and other pervasive developmental disorders. J Clin Psychiatry. 2005;66 (Suppl 10):3–8. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Mental Health in the United States: Parental Report of Diagnosed Autism in Children Aged 4–17 Years --- United States, 2003–2004. Morbidity and Mortality Weekly Report. 2006;55:481–486. [PubMed] [Google Scholar]
- 6.Lanterman Developmental Disabilities Services Act. California Welfare and Institutions Code, Division. 1969. pp. 4.1–4.7. [Google Scholar]
- 7.Croen LA, Grether JK, Hoogstrate J, Selvin S. The changing prevalence of autism in California. J Autism Dev Disord. 2002;32(3):207–15. doi: 10.1023/a:1015453830880. [DOI] [PubMed] [Google Scholar]
- 8.Byrd R. The Epidemiology of Autism in California: A Comprehensive Pilot Study, Report to the Legislature on the Principal Findings. 2002. [Google Scholar]
- 9.California Department of Developmental Services. A Report to the Legislature. Sacramento, CA: California Health and Human Services Agency; 1999. Changes in the Population of Persons with Autism and Pervasive Developmental Disorders in California’s Developmental Services System: 1987–1998. [Google Scholar]
- 10.California Department of Developmental Services. An Update 1999 Through 2002. Sacramento, CA: State of California; 2003. Autism Spectrum Disorders. Changes in the California Caseload. [Google Scholar]
- 11.Blaxill MF, Baskin DS, Spitzer WO. Commentary: Blaxill, Baskin, and Spitzer on Croen et al (2002), the changing prevalence of autism in California. J Autism Dev Disord. 2003;33(2):223–6. doi: 10.1023/a:1022912115365. discussion 227–9. [DOI] [PubMed] [Google Scholar]
- 12.Geier D, Geier M. Early downward trends in neurodevelopmental disorders following removal of thimerosal-containing vaccines. J American Physicians and Surgeons. 2006;11(1):8–13. [Google Scholar]
- 13.Schechter R, Grether JK. Continuing increases in autism reported to California’s developmental services system: mercury in retrograde. Arch Gen Psychiatry. 2008;65(1):19–24. doi: 10.1001/archgenpsychiatry.2007.1. [DOI] [PubMed] [Google Scholar]
- 14.SAS (Statistical Analysis Software) 9.1.3. Cary, NC: SAS Institute; 2002. [Google Scholar]
- 15.State of California Center for Health Statistics; Department of Health Services, editor. Confidential Birth 980-Byte File, 1990–2003. State of California; [Google Scholar]
- 16.California Department of Health Services. Sacramento. 2003. [Google Scholar]
- 17.Volkmar FR, Klin A, Siegel B, Szatmari P, Lord C, Campbell M, Freeman BJ, Cicchetti DV, Rutter M, Kline W, et al. Field trial for autistic disorder in DSM-IV. Am J Psychiatry. 1994;151(9):1361–7. doi: 10.1176/ajp.151.9.1361. [DOI] [PubMed] [Google Scholar]
- 18.Kielinen M, Linna SL, Moilanen I. Autism in Northern Finland. Eur Child Adolesc Psychiatry. 2000;9(3):162–7. doi: 10.1007/s007870070039. [DOI] [PubMed] [Google Scholar]
- 19.Williams JG, Higgins JP, Brayne CE. Systematic review of prevalence studies of autism spectrum disorders. Arch Dis Child. 2006;91(1):8–15. doi: 10.1136/adc.2004.062083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.State of California, editor. California Code of Regulations, Chapter 3, Community Services, Subchapter 1: General, Article 1: Definitions, Section 54001 - Substantial Disability. 2003. Vol. Title 17, Division 2. [Google Scholar]
- 21.Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule Manual. Los Angeles: Western Psychological Services; 2003. [Google Scholar]
- 22.Le Couteur A, Lord C, Rutter M. Autism Diagnostic Interview - Revised (ADI-R) Western Psychological Services; 2003. [Google Scholar]
- 23.Hertz-Picciotto I, Croen LA, Hansen R, Jones CR, van de Water J, Pessah IN. The CHARGE study: an epidemiologic investigation of genetic and environmental factors contributing to autism. Environ Health Perspect. 2006;114(7):1119–25. doi: 10.1289/ehp.8483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jick H, Kaye JA. Epidemiology and possible causes of autism. Pharmacotherapy. 2003;23(12):1524–30. doi: 10.1592/phco.23.15.1524.31955. [DOI] [PubMed] [Google Scholar]
- 25.Blaxill MF. Study fails to establish diagnostic substitution as a factor in increased rate of autism. Pharmacotherapy. 2004;24(6):812–3. doi: 10.1592/phco.24.8.812.36060. author reply 813–5. [DOI] [PubMed] [Google Scholar]
- 26.Jick H, Beach KJ, Kaye JA. Incidence of autism over time. Epidemiology. 2006;17(1):120–1. doi: 10.1097/01.ede.0000190553.72757.15. [DOI] [PubMed] [Google Scholar]
- 27.Wazana A, Bresnahan M, Kline J. The autism epidemic: fact or artifact? J Am Acad Child Adolesc Psychiatry. 2007;46(6):721–30. doi: 10.1097/chi.0b013e31804a7f3b. [DOI] [PubMed] [Google Scholar]
- 28.Coleman Institute; Coleman Institute, editor. State of the States. [Google Scholar]
- 29.A bill to reauthorize the Education of the Handicapped Act, and for other purposes. S.1824, 1990.
- 30.Baird G, Charman T, Baron-Cohen S, Cox A, Swettenham J, Wheelwright S, Drew A. A screening instrument for autism at 18 months of age: a 6-year follow-up study. J Am Acad Child Adolesc Psychiatry. 2000;39(6):694–702. doi: 10.1097/00004583-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Bertrand J, Mars A, Boyle C, Bove F, Yeargin-Allsopp M, Decoufle P. Prevalence of autism in a United States population: the Brick Township, New Jersey, investigation. Pediatrics. 2001;108(5):1155–61. doi: 10.1542/peds.108.5.1155. [DOI] [PubMed] [Google Scholar]
- 32.Chakrabarti S, Fombonne E. Pervasive developmental disorders in preschool children. Jama. 2001;285(24):3093–9. doi: 10.1001/jama.285.24.3093. [DOI] [PubMed] [Google Scholar]
- 33.Rice C. Prevalence of Autism Spectrum Disorders - Autism and Developmental Disabilities Monitoring Network, 14 Sites, United States, 2002. Morbidity and Mortality Weekly Report. 2007;56(SS01):12–28. [PubMed] [Google Scholar]