Abstract
Background
Implant malposition can produce unsatisfactory aesthetic results after breast augmentation. The goal of this article is to identify aspects of the preoperative surgical planning and intraoperative flap fixation that can prevent implant malposition.
Methods
This study examined 36 patients who underwent primary dual plane breast augmentation through an inframammary incision between September 1, 2012 and January 31, 2013. Before the surgery, preoperative evaluation and design using the Randquist formula were performed. Each patient was evaluated retrospectively for nipple position relative to the breast implant and breast contour, using standardized preoperative and postoperative photographs. The average follow-up period was 10 months.
Results
Seven of 72 breasts were identified as having implant malposition. These malpositions were divided into two groups. In relation to the new breast mound, six breasts had an inferiorly positioned and one breast had a superiorly positioned nipple-areolar complex. Two of these seven breasts were accompanied with an unsatisfactory breast contour.
Conclusions
We identified two main causes of implant malposition after inframammary augmentation mammaplasty. One cause was an incorrect preoperatively designed nipple to inframammary fold (N-IMF) distance. The breast skin and parenchyma quality, such as an extremely tight envelope, should be considered. If an extremely tight envelope is found, the preoperatively designed new N-IMF distance should be increased. The other main cause of malposition is failure of the fascial suture from Scarpa's fascia to the perichondrium through an inframammary incision. As well, when this fixation is performed, it should be performed directly downward to the perichondrium, rather than slanted in a cranial or caudal direction.
Keywords: Mammaplasty, Breast implant, Nipples
INTRODUCTION
Breast augmentation is currently the most popular cosmetic surgery procedure performed worldwide [1]. Statistics from the American Society of Plastic Surgeons indicate that the number of breast augmentation procedures increased by 44.5% from 212,500 in 2000 to 307,180 in 2011 [2]. As the number of patients undergoing breast augmentation has increased, the number of complications has also increased. Infection, bleeding or hematoma, sensory changes to the nipple and/or breast, breast asymmetry, and capsular contracture are all potential complications of the procedure. Reoperation may be required to address these complications [1]. Nevertheless, the occurrence of complications after breast augmentation is likely underestimated. When the surgeon and patient evaluate the results of breast augmentation, their degree of satisfaction is affected by the postoperative breast size and contour, and the location of the implant on the breast mound. Many techniques have been advocated in an attempt to achieve the best cosmetic result, and the postoperative position of the nipple-areolar complex is one of the most important factors influencing the degree of satisfaction with the procedure. If the breast implant is located in suboptimal position, then the nipple-areolar complex will also be displaced. Because of the relationship of the nipple-areolar complex to the inserted implant, a malpositioned nipple-areola complex produces the most obvious abnormality [3]. Thus, breast implant malposition produces an unsatisfactory nipple position and the surgeon should avoid this malposition to obtain the best cosmetic results.
To increase the likelihood of obtaining a satisfying result and to minimize the risk of complications, the plastic surgeon performing breast augmentation attempts to obtain all relevant information about the patients' breasts before the procedure [3]. To achieve a successful outcome, accurate preoperative evaluation and design are essential. In this study, we attempted to identify aspects of the preoperative planning and surgical procedure that led to implant malposition in inframammary augmentation mammaplasty.
METHODS
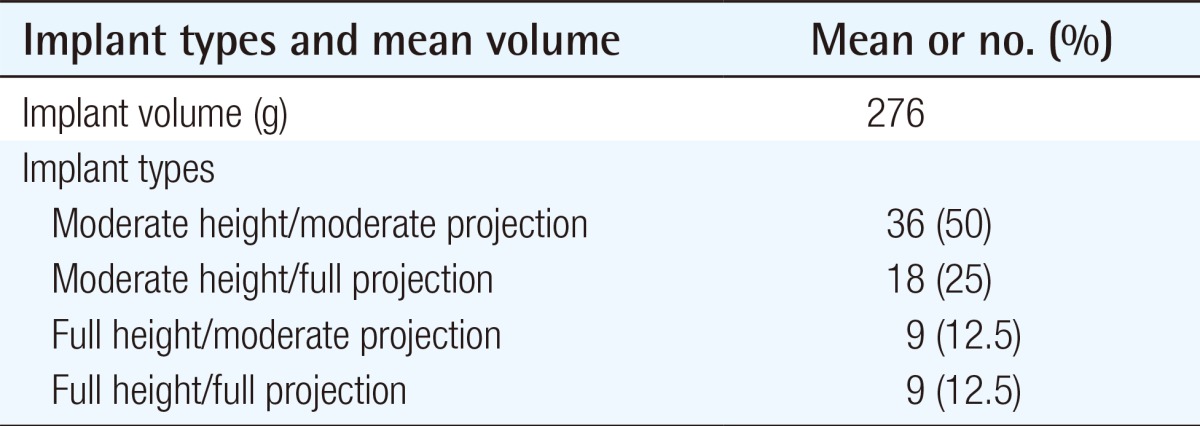
This study examined 36 patients who underwent primary dual plane breast augmentation through an inframammary incision with an anatomical implant, between September 1, 2012 and January 31, 2013. Anatomic implants containing cohesive silicone with a textured surface (Style 410 series, Allergan, California, USA) were used. The minimal follow-up period was 8 months and maximal period was 13 months. The average follow-up period was 10 months. Before the surgery, preoperative evaluation and design using the Randquist formula were performed. All patients underwent several baseline measurements, which were performed by a single surgeon using a standard protocol. The mean volume of the implant selected for augmentation mammaplasty was 276 g (Table 1). The most commonly used implant type was moderate height/moderate projection (50% of implants). Using of extra-full projection implant can cause uncorrectable tissue deformity by pressure on skin, subcutaneous tissue, breast parenchyma, muscle and bone, therefore the extra-full projection implant type was not used for long-term breast volume maintenance [4]. For each patient, data regarding the position of the nipple and breast contour were obtained retrospectively from standardized preoperative and postoperative photographs, as well as intraoperative findings.
Table 1.
Analysis of 72 breast implants
Preoperative planning
Implants were selected carefully, in accordance with a thorough understanding the patient's expectation [5]. The surgeon measured the patient's chest wall circumference at inframammary fold level and breasts circumference at nipple level. The following measurements were obtained from each breast: base width, sternal notch to nipple distance, intermammary distance, nipple to inframammary fold (N-IMF) distance during maximum-stretched and non-stretched conditions, and soft tissue pinch thickness of the upper pole.
The new N-IMF distance and IMF position were determined, based on the implant width (IW). Prior to the surgery, design using the Randquist formula was performed. According to designs using this formula, the adequate new IMF position could be located. The algorithm developed for implant positioning is shown in Table 2 [6]. In the current study, the surgeon evaluated the breast skin and parenchyma quality by determining the N-IMF distance during maximum-stretched and non-stretched conditions. For example, an 11.0 cm IW requires lowering the fold to 7.5±0.5 cm. If the patient has a tight or firm envelope that does not stretch, 0.5 cm should be added. If the patient has loose or overstretched skin, 0.5 cm should be subtracted [6]. Therefore, the quality of the breast skin and parenchyma was an important element of the preoperative design.
Table 2.
Algorithm used to determine implant positioning
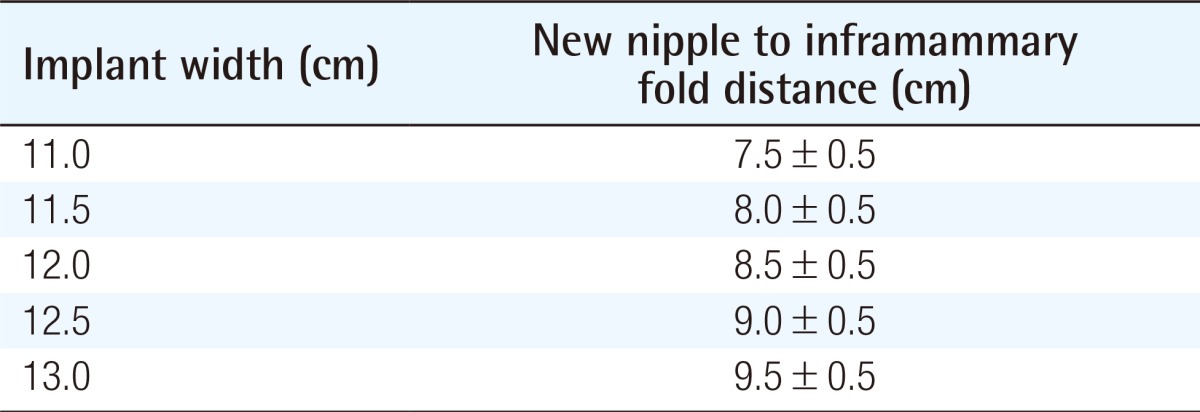
Randquist Formula: If the patient has a tight or firm envelope that does not stretch, 0.5 cm should be added. If the patient has loose or overstretched skin, 0.5 cm should be substracted.
Surgical technique
The following describes our surgical technique and includes suggestions and precautions to help optimize the surgical outcome. After induction of general anesthesia, the patient is placed in the supine position. A 4.0 cm incision is made according to the preoperative marking of the new IMF. After dissecting through the deep dermis and subcutaneous fat, the lateral border of pectoralis major muscle is identified. It is important to avoid dissecting the soft tissue below the incision line. Subgrandular dissection is performed at the lateral side of the pectoralis major muscle, as designed preoperatively. Entrance into the subpectoral space is begun by dividing the inferior margin of the pectoralis major muscle. When the surgeon divides the inferior border of pectoralis major muscle, it is important to avoid dividing the medial aspect of this muscle. The medial pinnate origin should be removed accurately. In other words, to create a dual plane pocket, the surgeon should divide the inferior origins of the pectoralis major muscle across the IMF 1 cm superior to the fold and stop dividing where the IMF joins the sternum. The inferior edge of pectoralis muscle does not be separated from overlying breast parenchyma [5]. The lateral and medial borders of the pectoralis major muscle must be dissected according to the preoperative design; however, the superior border can be dissected more than specified in the design, if necessary.
The implant is inserted by the bimanual technique. With the surgeon standing at the lateral side of the patient, the implant is inserted into the subpectoral pocket at the 3 o'clock position, by performing a 90° counterclockwise rotation. After the implant has been inserted, its axis is verified using the palpable linear line or spot. This palpable line or spot is located on the surface of the anatomic implant, along its long axis. If the implant has been inserted along the wrong axis, the implant is held over the surgeon's palm and rotated until the preoperatively designed axis is achieved.
The wound is closed in three layers. The first layer is the deep Scarpa's fascia and perichondrium. Fascial suturing is performed at the level of the preoperatively designed IMF. This layer is closed using figure-of-eight anchoring sutures. It is a very important aspect of constructing the new IMF. The second layer is the subcutaneous layer. The last layer is the superficial dermis and epidermis, which is closed with a continuous subcuticular or simple interrupted sutures. This last layer of sutures is removed one week after the operation.
RESULTS
During the 10 months of follow-up after surgery, seven of the 72 breasts undergoing augmentation were identified as having an unsatisfactory nipple-areolar complex position. Even though 10 months was short follow-up period to evaluate the other complications, there was not identified complication like capsular contracture, serosanguinous fluid collection, infection, capsular contracture and so on. An unsatisfactory nipple-areolar complex position was defined as a nipple position that strayed beyond the preoperatively designed nipple position. Deviations from the design position tend to reduce the breast's attractiveness [7]. For the seven breasts with nipple-areolar complex malposition, the mean implant volume was 230 g, and the most commonly used implant type was moderate height/moderate projection (72%) (Table 3).
Table 3.
Analysis of 7 malpositioned breast implants
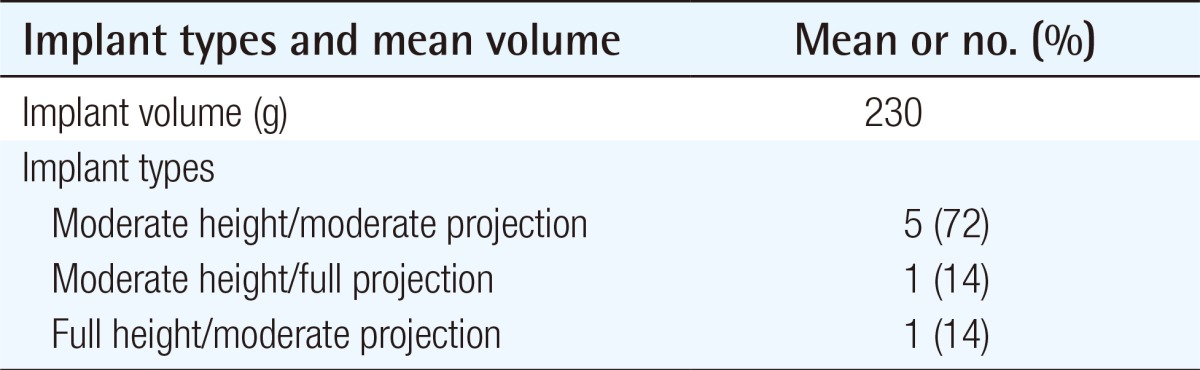
These seven cases of unsatisfactory nipple-areolar complex position were divided into two groups, based on the position of the nipple-areolar complex in relation to the new breast mound. Six complexes were positioned inferior to, and one complex was positioned superior to, the preoperatively predicted nipple-areolar complex position on the new breast mound. No laterally or medially malpositioned nipple-areolar complexes were observed. Two of these seven breasts were accompanied by an unsatisfactory breast contour. However, no patient required nipple repositioning or another reoperation.
For the group of breasts with the nipple-areolar complex positioned inferiorly in the new breast mound, the implant was located on the subpectoral pocket higher than the preoperatively designed position. This may have been caused by an incorrect design. The new N-IMF distance should be increased, especially in young Asian women who have extremely tight skin and parenchyma. Inferiorly positioned nipple-areolar complexes may have also been caused by the fascial suture from the Scarpa's fascia to the perichondrium not being fixed directly downward to the perichondrium, rather than slanted in a cranial or caudal direction.
For the single breast in the second group, in which the nipple-areolar complex was positioned superior in the new breast mound, the unsatisfactory nipple position was caused by loosening of the fascial suture. To prevent this, the fascial suture should be placed onto the perichondrium, not the muscle or other soft tissues.
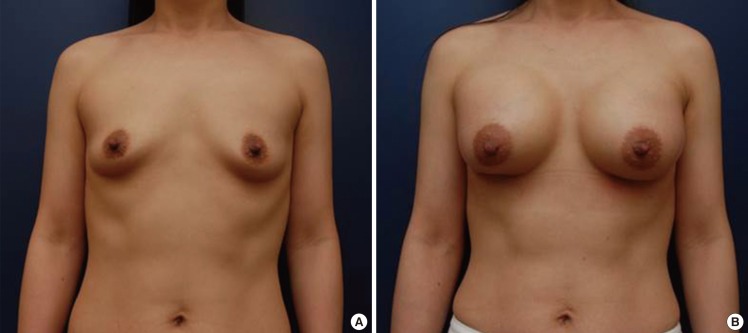
Case 1: inferiorly malpositioned nipple-areolar complex
A 42-year-old woman underwent primary dual plane breast augmentation through an inframammary incision, with an anatomical implant. Before the surgery, detailed preoperative evaluation and design were performed. (Fig. 1A). This woman had tight envelopes (the N-IMF fold distance under maximum-stretched and non-stretched conditions was 1.0 cm) and constricted breasts with ptosis. The N-IMF distance was extremely short. The selected implants had a 280 g volume and 12.0 cm IW, and were of moderate height and moderate projection. The new N-IMF distance was calculated to be 9.0 cm. However, during the 10-month follow-up period after breast augmentation, both nipple-areolar complexes deviated slightly inferiorly in relation to the new breast mound (Fig. 1B).
Fig. 1.
Preoperative and postoperative photographs of case 1
(A) Preoperative view. (B) Postoperative view at 10 months after dual plane breast augmentation with cohesive gel implant (Allergan, anatomic shape, MM, 280 g) through an inframammary incision. The both nipple.areolar complexes were positioned inferiorly in relation to the new breast mound because the implants were displaced superiorly. MM, moderate height/moderate projection.
As this patient's skin and parenchyma were extremely tight, a 12.0 cm IW required lowering of the fold to 9.0 cm. Although 0.5 cm was added to the value by the Ranquist formula, this did not provide sufficient lowering of new IMF line to prevent an inferiorly malpositioned nipple-areolar complex. Intraoperatively, inferiorly positioned nipple-areolar complex was noted after implant insertion on sitting position. Even though the surgeon considered this finding and performed perichondrial fixation, both nipple-areolar complexes deviated slightly inferiorly in relation to the new breast mound.
Case 2: superiorly malpositioned nipple-areolar complex
A 32-year-old woman underwent primary dual plane breast augmentation with an anatomical implant, through an inframammary incision. She had moderate envelopes (the N-IMF distance under maximum-stretched and non-stretched conditions was 1.5 cm) (Fig. 2A). The implant selected for the right side was 245 g and of moderate height and moderate profile, and the implant selected for the left implant was 225 g and of moderate height and high profile.
Fig. 2.
Preoperative and postoperative photographs of case 2
(A) Preoperative view. (B) Postoperative view at 3 months after dual plane breast augmentation with cohesive gel implant (Allergan, anatomic shape; left: MF, 225 g; right: MM, 245 g) through an inframammary incision. The left nipple-areolar complex was positioned superiorly in relation to the new breast mound, and a bottom-out deformity was apparent on the medial side of the new IMF. No proper perichondrium has been detected intraoperatively on the medial side of new IMF, therefore, it was not performed to suture the Scapa's fascia to the perichondrium. The Scapa's fascia was fixed to the muscle layer instead. MF, moderate height/full projection; MM, moderate height/moderate projection; IMF, inframammary.
Three months after breast augmentation, the left nipple-areolar complex was positioned superior in relation to the new breast mound (Fig. 2B). The left lower pole contour was not convex and a bottom-out deformity was apparent on the medial side of new IMF of the left breast. No proper perichondrium had been detected intraoperatively on the medial side of new IMF. The new IMF runs just along the intercostal space in the medial aspect. It was therefore not possible to suture the Scarpa's fascia to the perichondrium, and the Scarpa's fascia was fixed to the muscle layer instead.
Since the fascial suture of the left breast did not involve the perichondrium, the fascial suture loosened, thereby producing the bottom-out deformity on medial side. If no proper perichondrium exists on the new IMF, then the fascial suture point can be moved lateral or medial to find a proper rib to allow the perichondrium to be included in this suture.
DISCUSSION
In this study, the surgeon performed dual plane implant placement though an inframammary incision in all cases. All patients had limited amount of subcutaneous fat and breast tissue coverage, which led to our use of the dual plane implant placement and high-level pocket dissection. This was easily accomplished through the inframammary incision in all patients.
The choices of incision for breast augmentation surgery include inframammary, periareolar, transaxillary and transumbrical incisions [8]. The inframammary incision is the most widely used approach in breast augmentation. It provides more direct vision and better surgical control than other types of incisions [9]. Furthermore, the inframammary approach causes the least amount of adjacent tissue trauma intraoperatively, particularly during pocket dissection and implant insertion [5]. For these reasons, many inexperienced surgeons prefer this type of incision. Using this approach, they can minimize operation times and optimize patient recovery [5]. However, these advantages like better surgical control can cause more malposition of breast implant when the surgeon makes a mistake in surgical techniques. Therefore, we evaluated implant malposition in primary dual plane breast augmentation through an especially inframammary incision.
Capsular attenuation and contracture remain the most important factors contributing to breast implant malposition [10,11]. Capsular contracture (Baker grades III and IV) is one of the most frequent complications and the most common cause for reoperation after breast augmentation surgery [10]. The cause of capsular contracture is multifactorial; therefore, it is challenging to prevent and manage implant-associated breast asymmetry and deformities.
In 1996, Brink [12] suggested possible mechanisms for implant malposition. He noted that serosanguinous fluid can persist at the inferior pole of the periprosthetic space for weeks after subpectoral breast augmentation. This sequestered fluid may allow the implant to become displaced. In addition, the blunt dissection used to make the pocket stretches and partially tears the pectoralis muscle at its inferomedial origin. This can induce postoperative pain and muscle spasm. Spasm of the pectoralis muscle compresses the prosthetic space and thereby squeezes the implant, resulting in a high-riding implant [12].
Mallucci and Branford [13] identified 100 consecutive women chosen because of their aesthetically appealing breasts. These breasts were characterized by a nipple position with a 45:55 upper to lower pole distance ratio, a 20-degrees upward angulation of the nipple at the meridian, lower pole convexity, and upper pole linear or concave slope [7]. Based on these criteria, we evaluated the breasts of our study patients for position and asymmetry of the nipple using standardized preoperative and postoperative photographs. Seven of 72 breasts were identified as having an unsatisfactory nipple-areolar complex position.
In our study, we identified two main causes of anatomic implant malposition in breast augmentation: inappropriately designed new N-IMF distance and failure to suture the Scarpa's fascia to the perichondrium. In contrast to the factors contributing to implant malposition mentioned in the previous paragraphs, these two causes are potentially preventable. To calculate the new N-IMF distance, it is important to thoroughly evaluate the quality of the breast skin and parenchyma. We performed this evaluation by determining the N-IMF distance under maximum-stretched and non-stretched conditions. However, the anterior pull skin stretch, in which the skin of the areola is grasped and pulled maximally anteriorly is a more suitable method to estimate the quality of the parenchyma for breast augmentation [14]. The anterior pull skin stretch causes pain and discomfort to the patients, but this method can provide more valuable informations for surgeons. Furthermore, the Randquist formula was originated for Caucasians. As young and small Asian women such as slender twenties who have tight or firm envelope that does not stretch, this difference should be considered when a surgeon uses the Randquist formula in Asians. For example, if the patient has an extremely tight envelope that does not stretch, then 1.0 cm or more should be added to the calculated new N-IMF distance.
Failure to suture the Scarpa's fascia to the perichondrium through an inframammary incision was the other main cause of nipple-alreolar complex malposition that we identified in our study. In case 2, no proper perichondrium was detected intraoperatively on the medial side of the new IMF. Therefore, a fascial suture from the Scarpa's fascia to the perichondrium was not performed. We suggest some surgical tips for perichondrial fixation in here. If no proper perichondrium exists on the new IMF, then the fascial suture point can be moved lateral or medial to find a proper rib to allow the perichondrium to be included in this suture. As well, when this fixation is performed, it should be performed directly downward to the perichondrium, rather than slanted in a cranial or caudal direction.
However, if there is no appropriate perichondrium on any designed new IMF line, in other words, the new IMF runs just along the intercostal space, then the fascial suture should be placed through the perichondrium inferior to the line, rather than the perichondrium superior to it.
Although the inframammary incision could cause a visible scar, the inframammary incision has several advantages such as good surgical vision and easily manipulation of the implant, compared to the other approaches, for inexperienced surgeons. If the inexperienced surgeon pays particular attention to the two main causes of implant malposition accompanying this approach, the occurrence of an unsatisfactory nipple-areolar complex position due to implant displacement should be decreased.
There are limitations to this study. The relatively short follow-up period may have underestimated the number of unsatisfactory results or other complications. In addition, the study was small, involving only 36 patients, which limits our ability to discuss the general applicability of our results. Another limitation was that all baseline measurements and assessments of the nipple-areolar complex position and breast contour were performed by a single surgeon. If these were performed by the patients or other surgeons, this may have provided us with more objective data. However, this was not possible because the retrospective nature of the study limited the amount and type of data that were available. Furthermore, each patient was evaluated retrospectively for nipple position relative to the breast mound. If the distance of sternal notch to new nipple-areolar complex was measured, this result gives us more objective evaluation.
We have noted that the anterior pull skin stretch may be a more suitable method to estimate the breast parenchyma quality than the maximum-stretched N-IMF distance in breast augmentation; however, we are aware of no study that has directly compared the accuracy of the two methods. Reducing or eliminating the above limitations should be considered in future studies.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Adams WP, Jr, Mallucci P. Breast augmentation. Plast Reconstr Surg. 2012;130:597e–611e. doi: 10.1097/PRS.0b013e318262f607. [DOI] [PubMed] [Google Scholar]
- 2.Alpert BS, Lalonde DH. MOC-PS(SM) CME article: breast augmentation. Plast Reconstr Surg. 2008;121:1–7. doi: 10.1097/01.prs.0000305933.31540.5d. [DOI] [PubMed] [Google Scholar]
- 3.Youn ES. Importance of the new position of the nipple-areola complex in breast augmentation surgery. Plast Reconstr Surg. 2006;118:18S–31S. doi: 10.1097/01.prs.0000246235.00439.3d. [DOI] [PubMed] [Google Scholar]
- 4.Tebbetts JB, Teitelbaum S. High- and extra-high-projection breast implants: potential consequences for patients. Plast Reconstr Surg. 2010;126:2150–2159. doi: 10.1097/PRS.0b013e3181f44564. [DOI] [PubMed] [Google Scholar]
- 5.Tebbetts JB. Augmentation mammaplasty: redefining the surgeon and patient experience. London: Elsevier; 2010. [Google Scholar]
- 6.Hall-Findlay EJ, Evans G. Aesthetic and reconstructive surgery of the breast. Philadelphia: Saunders; 2012. [Google Scholar]
- 7.Spear SL, Albino FP, Al-Attar A. Classification and management of the postoperative, high-riding nipple. Plast Reconstr Surg. 2013;131:1413–1421. doi: 10.1097/PRS.0b013e31828bd3e0. [DOI] [PubMed] [Google Scholar]
- 8.Hidalgo DA. Breast augmentation: choosing the optimal incision, implant, and pocket plane. Plast Reconstr Surg. 2000;105:2202–2216. doi: 10.1097/00006534-200005000-00047. [DOI] [PubMed] [Google Scholar]
- 9.Cardenas-Camarena L, Ramirez-Macias R, et al. International Confederation for Plastic Reconstructive and Aesthetic Surgery. Augmentation/mastopexy: how to select and perform the proper technique. Aesthetic Plast Surg. 2006;30:21–33. doi: 10.1007/s00266-005-0133-x. [DOI] [PubMed] [Google Scholar]
- 10.Spear SL, Seruya M, Clemens MW, et al. Acellular dermal matrix for the treatment and prevention of implant-associated breast deformities. Plast Reconstr Surg. 2011;127:1047–1058. doi: 10.1097/PRS.0b013e31820436af. [DOI] [PubMed] [Google Scholar]
- 11.Poeppl N, Schreml S, Lichtenegger F, et al. Does the surface structure of implants have an impact on the formation of a capsular contracture? Aesthetic Plast Surg. 2007;31:133–139. doi: 10.1007/s00266-006-0091-y. [DOI] [PubMed] [Google Scholar]
- 12.Brink RR. Sequestered fluid and breast implant malposition. Plast Reconstr Surg. 1996;98:679–684. doi: 10.1097/00006534-199609001-00012. [DOI] [PubMed] [Google Scholar]
- 13.Mallucci P, Branford OA. Concepts in aesthetic breast dimensions: analysis of the ideal breast. J Plast Reconstr Aesthet Surg. 2012;65:8–16. doi: 10.1016/j.bjps.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Tebbetts JB, Adams WP. Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process. Plast Reconstr Surg. 2006;118:35S–45S. doi: 10.1097/01.prs.0000191163.19379.63. [DOI] [PubMed] [Google Scholar]