Eosinophil degranulation of peroxidase promotes DC activation and mobilization from the intestine to LNs to induce Th2 immunity and food allergy.
Abstract
Eosinophils natively inhabit the small intestine, but a functional role for them there has remained elusive. Here, we show that eosinophil-deficient mice were protected from induction of Th2-mediated peanut food allergy and anaphylaxis, and Th2 priming was restored by reconstitution with il4+/+ or il4−/− eosinophils. Eosinophils controlled CD103+ dendritic cell (DC) activation and migration from the intestine to draining lymph nodes, events necessary for Th2 priming. Eosinophil activation in vitro and in vivo led to degranulation of eosinophil peroxidase, a granule protein whose enzymatic activity promoted DC activation in mice and humans in vitro, and intestinal and extraintestinal mouse DC activation and mobilization to lymph nodes in vivo. Further, eosinophil peroxidase enhanced responses to ovalbumin seen after immunization. Thus, eosinophils can be critical contributors to the intestinal immune system, and granule-mediated shaping of DC responses can promote both intestinal and extraintestinal adaptive immunity.
Ehrlich described the presence of rich magenta eosin-staining granules that characterize eosinophils over 130 yr ago (Erlich, 1879). Yet, the precise roles of eosinophils in health and disease remain to be fully defined (Rosenberg et al., 2013). Eosinophils have been identified in tissues of lower vertebrates and eosinophil-like cells in some invertebrates. Thus, eosinophils evolved before adaptive T and B cell immunity emerged (McGarry, 2013). Eosinophils may have evolved from phagocytic cells in primitive invertebrates when digestion and immunity became specialized functions (Lenzi et al., 1997). In this regard, the intestine is one of few immune sites that natively houses an abundance of eosinophils. The presence of eosinophils in the healthy gut has long been overlooked (Mowat and Bain, 2010) and most research on intestinal myeloid cells has rather focused on DCs and macrophages. Thus, the function of eosinophils in the healthy gut is unclear.
Most work on eosinophils has concentrated on their role during Th2 responses, in particular helminth infections and allergic responses. In this regard, eosinophil granulocytes are classically thought of as specialized effector cells recruited from the blood and bone marrow to tissues during adaptive Th2 responses. Thus, consistently other than the intestine, most healthy tissues are devoid of eosinophils (Barnes, 2004; Rosenberg et al., 2013). Once in the tissue, recruited eosinophils are activated, produce several cytokines, and release characteristic cationic granules such as eosinophil peroxidase (EPO) in a process termed degranulation. Eosinophils have been ascribed both beneficial and harmful functions. For example, there is evidence of eosinophil attachment to helminths and subsequent degranulation, and cytotoxicity toward helminths. However, an indispensable role for eosinophils in host defense against helminths remains controversial (Cadman and Lawrence, 2010; Rosenberg et al., 2013). With respect to allergic disease, eosinophils are thought to play a pathogenic inflammatory role in diseases such as allergic asthma, atopic dermatitis, or food allergy. In response to helminths or allergens, Th2 responses in the gastrointestinal (GI) tract, and elsewhere, are characterized by the late influx of eosinophils into the tissue to mediate inflammation. However, a role for the abundant native GI eosinophil population has remained enigmatic (Drury, 1915; Duran-Jorda, 1947; Mowat and Bain, 2010).
The small intestine (SI) plays a vital role in the digestion and absorption of macronutrients. The immune system must recognize food antigens as innocuous and, hence, develop tolerance. Extensive work has shown this process to be mediated by oral antigen uptake by CD103+ DCs, which migrate to the draining mesenteric LN (MLN) in a CCR7-dependent manner to prime antigen-specific naive T cells to differentiate into T regulatory cells (Pabst and Mowat, 2012). However, a subversion of oral tolerance leads to aberrant immune responses that result in the development of diseases such as food allergies. These are characterized by an adaptive Th2 immune response that results in IgE-mediated allergic reactions, including a life-threatening systemic reaction termed anaphylaxis (Burks, 2008; Berin and Sampson, 2013). Compared with other known classes of adaptive immune responses, the innate mechanisms that drive Th2 induction are much less clear (Paul and Zhu, 2010; Pulendran et al., 2010). Indeed, the APCs involved, their activation conditions, and T cell polarization factors such as the source of the initial IL-4 for Th2 cell priming remain unclear.
In stark contrast with the classical notion that eosinophils participate in immune responses as terminal effector leukocytes whose production, migration and activation is under the control of adaptive Th2 immunity, we report just the opposite process. Here, we found a crucial role for indigenous SI eosinophils in the initiation of Th2 immunity, with critical importance to the development of peanut food allergy. Eosinophil activation during intestinal Th2 priming results in the release of EPO that controls CD103+ DC activation and CCR7-dependent migration to the MLN, where DCs then promote Th2 responses. We further show that EPO-mediated DC activation is functional in both mice and humans, is mediated by EPO’s peroxidase enzymatic activity, and that EPO is also sufficient as an adjuvant to promote extraintestinal adaptive immunity. Collectively, these data identify a critical in vivo role for indigenous eosinophils in intestinal immunity, and reveals the potential for eosinophil granule-mediated shaping of DC responses in promoting adaptive immunity.
RESULTS
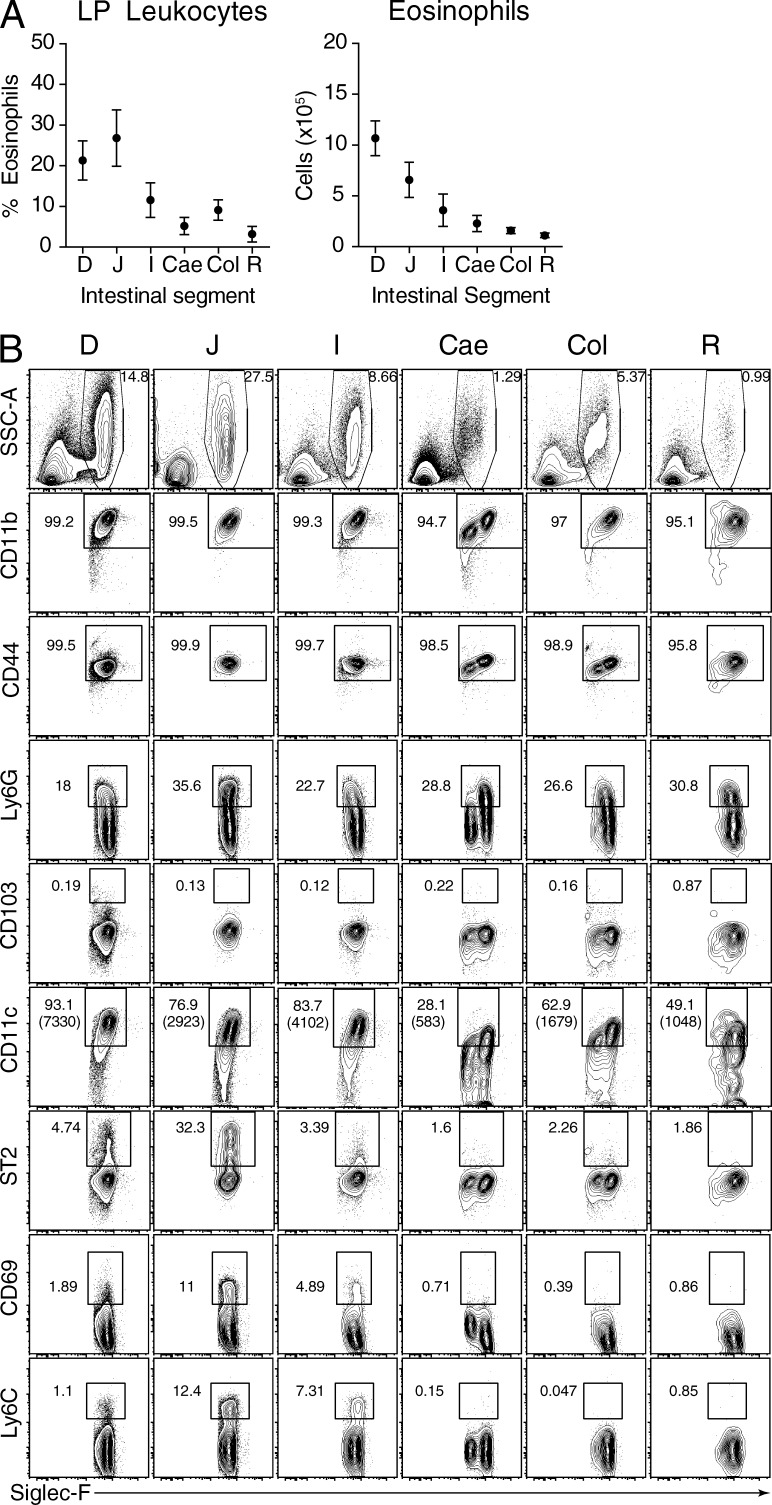
Definition of indigenous eosinophils along the intestinal tract
Eosinophils along the intestinal tract were histologically quantified in 1999 (Mishra et al., 1999), and Carlens et al. (2009) recently established a sensitive flow cytometric method to evaluate intestinal eosinophils. Here, we took advantage of flow cytometry’s capability for precise quantitation and multiparameter analysis to better define eosinophils along the intestinal tract. Eosinophils were most prevalent within the SI, ranging from ∼15–25% of all lamina propria (LP) leukocytes in the duodenum, ∼15–35% in the jejunum, and ∼5–15% in the ileum (Fig. 1 A). The frequency of eosinophils was lower in the large intestine (LI), ∼3–5% eosinophils in the cecum, ∼7% in the colon, and <1% in the rectum (Fig. 1 A). Quantifying eosinophil numbers revealed that they decreased along the length of the intestinal tract (Fig. 1 A), potentially suggesting negative regulation by the microbiota. Phenotypically, although both SI and LI eosinophils were Siglec-F+, CD11b+, CD44+, CD103−, and ∼30% Ly6G+, SI and LI eosinophils also displayed distinct cell surface phenotypes (Fig. 1 B). More SI eosinophils expressed CD11c, and at higher levels, than LI eosinophils. As well, a greater proportion of SI eosinophils expressed ST2 (IL-33 receptor), CD69, and Ly6C, compared with LI eosinophils. Therefore, different compartments of the intestine harbor different proportions, numbers and phenotypes of eosinophils at baseline. Given the prominence of eosinophils in the SI, we next sought to evaluate the impact of eosinophil ablation on SI function and immunity.
Figure 1.
Characterization of eosinophils along the intestinal tract. (A, left) Proportion of eosinophils of total LP leukocytes or (right) absolute cell number. (B) Phenotypic characterization of eosinophils along the intestinal tract. Mean ± SD, n = 6–8, with each sample being pooled from 3–4 mice from 4 experiments. D, duodenum; J, jejunum; I, ileum; Ce, cecum; Col, colon; R, rectum.
Indigenous enteric eosinophils promote induction of Th2 immunity in vivo independently of their ability to produce IL-4
ΔdblGATA1 mice (Yu et al., 2002; Humbles et al., 2004; Fattouh et al., 2011), lack a high-affinity GATA-binding site in the GATA-1 promoter, resulting in strong, but submaximal GATA-1 promoter activity and, ultimately, complete ablation of the eosinophil lineage (Yu et al., 2002). Other GATA-1–dependent lineages, namely erythrocytes, megakaryocytes and mast cells, are not affected as their lineages do not require maximal GATA-1 promoter activity. A recent publication suggested that ΔdblGATA1 mice may have slightly reduced basophils (Nei et al., 2013).
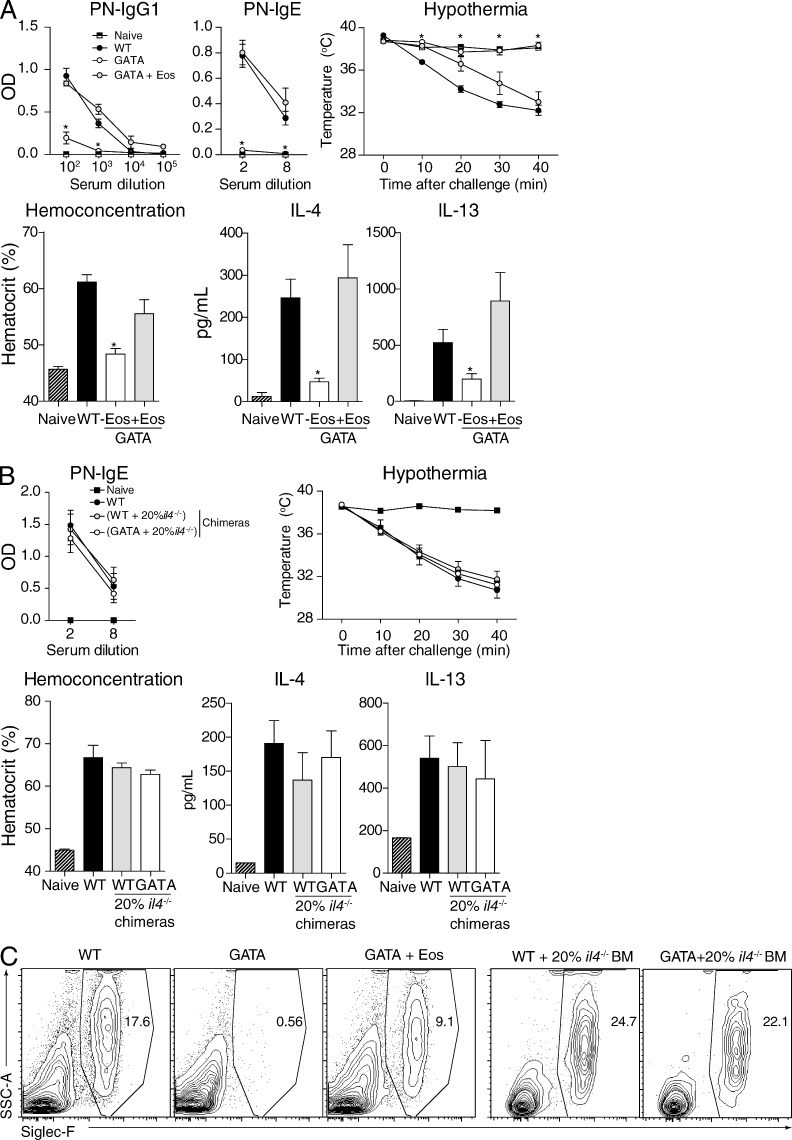
Intragastric (i.g.) immunization to the common food allergen peanut (PN) with the classical oral Th2-inducing adjuvant cholera toxin (CT) induces basophil-independent, OX40L- and IL-4–dependent SI Th2 priming, such that subsequent allergen challenge elicits systemic anaphylaxis (Chu et al., 2013) similar to human peanut allergy (Li et al., 2000; Leung et al., 2003; Vadas et al., 2008; Arias et al., 2009, 2011). Whereas WT mice mounted robust antigen-specific IgE, IgG1, and Th2 cytokine responses and, clinically, anaphylactic hypothermia and hemoconcentration, ΔdblGATA1 mice did not (Fig. 2 A). This defect was corrected by adoptive transfer of eosinophils into ΔdblGATA1 mice (Fig. 2, A and C). Thus, eosinophils were required for SI Th2 priming.
Figure 2.
Eosinophils are required for induction of Th2 immunity to oral antigen. WT, ΔdblGATA1 (GATA), ΔdblGATA1 mice that received eosinophils weekly (GATA+Eos), or mixed BM chimeras were kept naive or administered PN+CT i.g. weekly for 4 wk. BM chimeras were generated by mixing 80% WT or ΔdblGATA1 BM with 20% il4−/− BM, resulting in mice with il4+/+ or il4−/− eosinophil compartments, respectively. (A and B, top left) Serum PN-specific (PN-) IgG1 and PN-IgE at week 5. (A and B, top right) Clinical anaphylaxis assessment of hypothermia and vascular leakage after i.p. challenge at week 5. (A and B, bottom) Th2 cytokine production from PN-stimulated splenocytes. (C) SI LP eosinophils in WT, eosinophil-deficient, and eosinophil-reconstituted mice. Mean ± SEM, n = 3–12 from 3–5 experiments. *, P < 0.05 versus WT.
Eosinophils are known to be IL-4 competent, including in the SI-draining MLN, (Svensson et al., 2011), raising the possibility that eosinophils were required during SI priming to provide IL-4 to promote Th2 differentiation. However, mixed bone marrow chimeras showed that reconstitution of the eosinophil compartment (Fig. 2 C) with IL-4–deficient eosinophils fully restored Th2 priming to i.g. PN+CT. This was borne out by full restoration of antigen-specific IgE production, clinical anaphylaxis, and cytokine production (Fig. 2 B). Thus, normally resident enteric eosinophils are critical to initiate SI Th2 immunity in vivo, independent of their ability to produce IL-4.
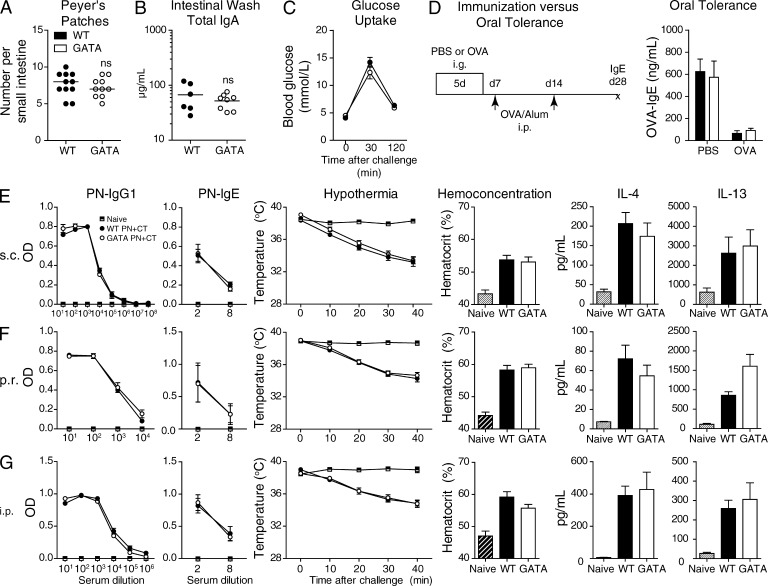
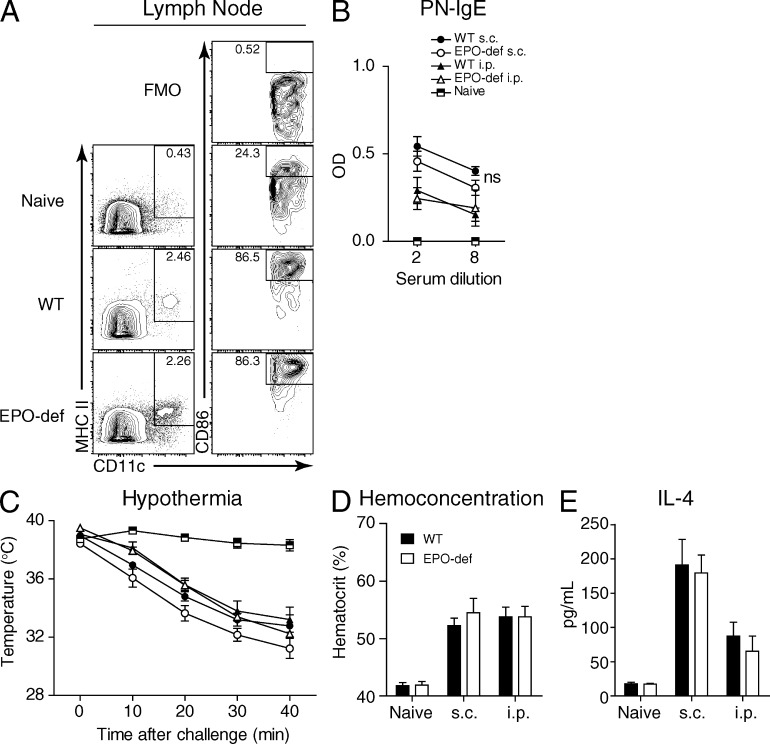
Conventional parameters of intestinal and adaptive immunity are intact in eosinophil-deficient mice
A series of control experiments revealed that eosinophil deficiency did not impair conventional parameters of intestinal and adaptive immunity, including Peyer’s patch organogenesis (Fig. 3 A), intestinal IgA levels (Fig. 3 B), macronutrient uptake (Fig. 3 C), antigen-specific IgE production in response to intraperitoneal immunization, or oral tolerance induction (Fig. 3 D). These data show that eosinophil-deficient mice are not inherently defective in basal intestinal immunity and macronutrient absorption, nor are they defective in their capability to elicit parenteral adaptive Th2 immunity and IgE responses, as well as, under basal conditions, to induce CD103+ DC, CCR7, and T regulatory cell–dependent oral tolerogenic immunity (Pabst and Mowat, 2012). Consistent with reports of intact Th2 priming to parenteral immunization in eosinophil-deficient mice (Humbles et al., 2004; Swartz et al., 2006; Knott et al., 2007; Fattouh et al., 2011; Svensson et al., 2011), we also found that the requirement for eosinophils in initiating Th2 adaptive immunity was site-dependent as immunization via the peritoneum, skin, or rectum, tissues with little to no eosinophils at baseline, resulted in robust Th2 priming (Fig. 3, E–G). These data comprehensively show that the immunological machinery to initiate Th2 responses is intact in eosinophil-deficient mice. They also show that eosinophils are not required to induce anaphylaxis, per se. Thus, eosinophils are required for SI Th2 priming, but not baseline intestinal immunity or parenteral Th2 priming.
Figure 3.
Conventional features of intestinal and adaptive immunity are intact in the absence of eosinophils. (A) Median number of Peyer’s patches with individual data shown. (B) Mean intestinal wash IgA with individual data shown. (C) i.g. glucose challenge and blood glucose over time. (D) Serum OVA-specific IgE at day 28 from mice i.g. fed OVA or PBS daily from day 0 to 5 before i.p. immunization on day 7 and 14 with OVA adsorbed to aluminum hydroxide. (E–G) WT or ΔdblGATA1 (GATA) mice were kept naive or administered PN+CT (E) s.c., (F) p.r., or (G) i.p. weekly for 4 wk. (E–G, left) Serum PN-specific (PN-) IgG1 and PN-IgE at week 5. (E–G, middle) Clinical anaphylaxis assessment of hypothermia and vascular leakage after i.p. challenge at week 5. (E–G, right) Th2 cytokine production from PN-stimulated splenocytes. Mean ± SEM, n = 3–12 from 2–3 experiments. All WT versus GATA comparisons in this figure were not statistically different (ns).
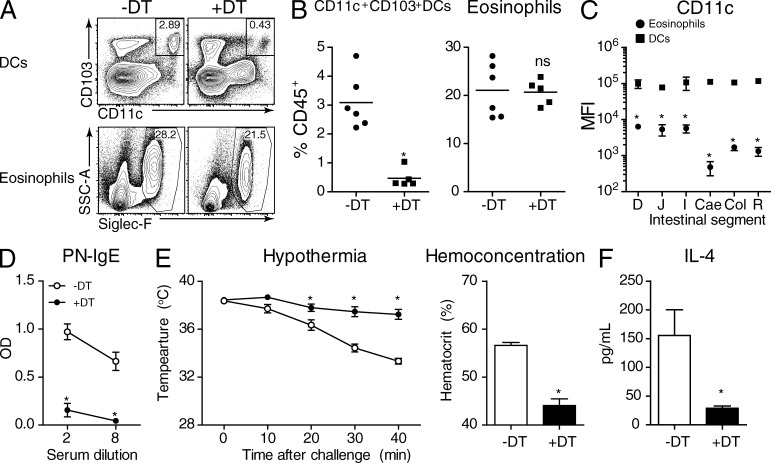
CD11c+ cells are required for intestinal Th2 priming
Aside from being a potential source of IL-4, there is also evidence that granulocytes such as basophils may supplant DCs in their requirement as APCs to launch Th2 immune responses (Perrigoue et al., 2009; Sokol et al., 2009; Akuthota et al., 2010) and eosinophils have been recognized as potential APCs under certain conditions (Shi et al., 2000; Akuthota et al., 2010). CD11c-diphtheria toxin receptor (DTR) transgenic mice are commonly used to probe the function of DCs in a given process through selective depletion of CD11c+ cells. However, the use of CD11c-targeted strategies (e.g., DTR, GFP/YFP-reporters, or MACS) to analyze the intestinal immune system is potentially complicated by non-DC CD11c+ populations such as GI eosinophils (Carlens et al., 2009; Fig. 1 B). Thus, to clarify whether the CD11c-DTR transgenic system depleted SI eosinophils, DCs, or both, we generated CD11c-DTR transgenic → WT BM chimeras, which allow for the depletion of CD11c+ cells with repeated injection of DT. Importantly, such chimeras treated with DT lacked SI DCs but not CD11c+ eosinophils (Fig. 4, A and B), and this was associated with ∼10–100-fold higher expression of CD11c (and therefore likely the DTR transgene) by DCs (Fig. 4 C). Depletion of DCs throughout sensitization protected CD11c-DTR → WT chimeras from i.g. PN+CT sensitization and anaphylaxis (Fig. 4, D–F) as indicated by a lack of antigen-specific IgG1 and IgE, IL-4 production, and clinical anaphylactic hypothermia and hemoconcentration. Altogether, these data show that this CD11c-DTR system can be used to selectively deplete intestinal DCs and not CD11c+ SI eosinophils. These also show a differential critical contribution of CD11c+ DCs and eosinophils to initiating intestinal Th2 priming.
Figure 4.
CD11c-DTR → WT chimeras show that DCs are required for induction of Th2 immunity to oral antigen. CD11c-DTR → WT chimeras received i.p. PBS or DT 24h before each i.g. PN+CT, weekly, for four weeks. (A and B) Depletion of SI DCs but not eosinophils. (C) Comparison of CD11c MFI ± SD between SI eosinophils and CD103+ DCs. (D) Serum PN-specific PN-IgE at week 5. (E) Clinical anaphylaxis assessment of hypothermia and hemoconcentration after i.p. challenge at week 5. (F) Th2 cytokine production from PN-stimulated splenocytes. Mean ± SEM unless otherwise stated; n = 5–10 from 2 experiments. *, P < 0.05 versus (B and F) -DT or (C) DCs. ns, not statistically different.
MLN CD103+ DCs, not eosinophils, act as APCs during Th2 priming to oral antigen
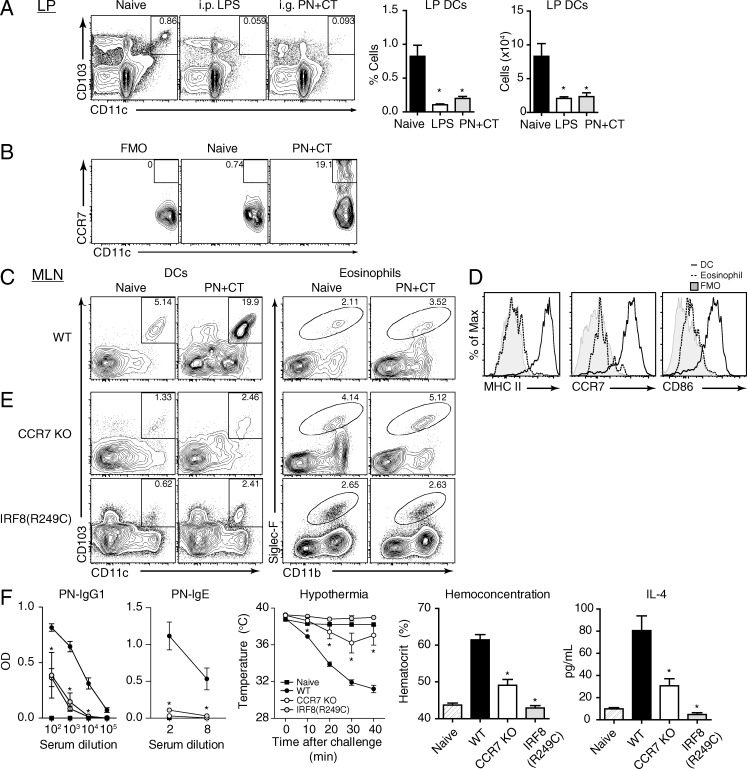
Adaptive immunity is primed in the draining LNs, where naive T cells interact with APCs that have migrated from peripheral sites carrying antigen and are equipped with a particular package of immunological instructions (Ritz et al., 2002). Thus, we further evaluated whether eosinophils or DCs acted as APCs by migrating from the SI to the MLN to activate CD4+ T cells. CD103+ intestinal migratory DCs are elicited from the SI LP after parenteral LPS i.p. administration (Turnbull et al., 2005; Schulz et al., 2009), and we used this as a positive control in our experiments. In response to PN+CT, CD103+ DCs decreased in the SI LP (Fig. 5 A), up-regulated CCR7 (Fig. 5 B), and accumulated within the MLN (Fig. 5 C), suggesting DC migration. Although CD103+ DCs increased within the MLN, eosinophils did not (Fig. 5 C). Similarly, MLN DCs, but not eosinophils, expressed MHC II, CCR7, and the co-stimulatory molecule CD86 (Fig. 5 D). These data suggest that DCs, not eosinophils, are the primary migratory APCs in this system.
Figure 5.
CD103+ DCs are required for induction of Th2 immunity to oral antigen. WT, CCR7 KO, or IRF8(R249C) mice were administered PN+CT i.g. for three consecutive days, or weekly for 4 wk. (A) SI DC percentage and number after three consecutive days of PN+CT i.g., or 16 h after LPS i.p. (B) SI DC expression of CCR7. (C) DC and eosinophil percentages in MLN in response to PN+CT (D) Expression of MHC II, CCR7, and CD86 on DCs but not eosinophils. (E) Migratory DCs and eosinophils in CCR7 KO and IRF8(R249C) mice. (F) Immunological and clinical responses in the absence of CD103+ DCs. Mean ± SEM, n = 3–10 from 2 experiments. *, P < 0.05 versus (A) Naive or (F) WT.
Under basal conditions, SI CD103+ DCs preferentially capture ingested food antigens and then home to the draining MLN in a CCR7-dependent fashion to induce oral tolerance and T regulatory cells (Worbs et al., 2006; Schulz et al., 2009). Whether similar mechanisms take place during Th2 priming to oral antigen is unclear, especially given reports that mice deficient in CCR7 signaling mount augmented Th2, IgE, and inflammatory responses in various systems (Grinnan et al., 2006; Kawakami et al., 2012; Moschovakis et al., 2012). We found that CCR7 controlled homing of CD103+ DCs, but not eosinophils, to the MLN and that this was required to drive Th2 responses to i.g. PN+CT (Fig. 5, E and F). Likewise, IRF8(R249C) mutant mice, which are deficient in the SI CD103+ DC subset because of a block in differentiation (Edelson et al., 2010), were sufficient in eosinophils (Fig. 5 E) and protected from allergic sensitization (Fig. 5 F). These data illustrate a differential contribution of eosinophils and DCs to i.g. priming, whereby antigen-carrying CD103+ DCs are elicited from the SI to the MLN in a CCR7-dependent manner and these migratory DCs act as a critically required APC to initiate adaptive Th2 immunity.
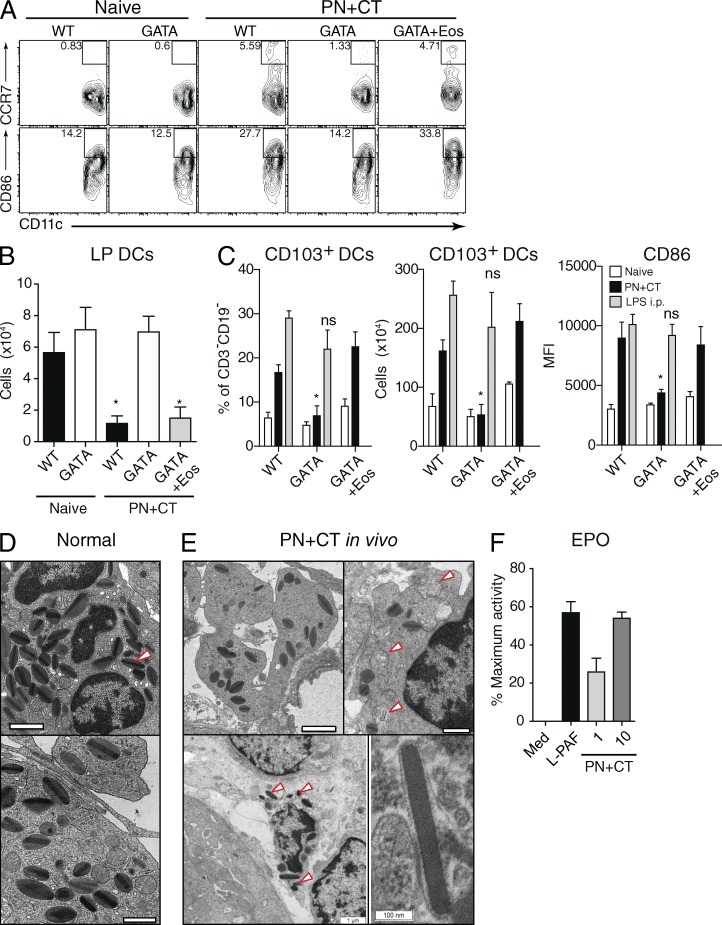
Eosinophil control of DC activation and migration is associated with degranulation in vitro and in vivo
That ablation of either eosinophils or CD103+ DCs prevented the induction of Th2 responses suggested that these two cell types acted in series rather than in parallel. The capability to induce adaptive immunity by nonoral immunization routes (Fig. 3) suggested that the defect in immunizing ΔdblGATA1 mice i.g. was upstream of T or B cell activation and differentiation. Consistent with this reasoning, we found that eosinophils were required for CD103+ DC mobilization to the MLN in response to i.g. PN+CT (Fig. 6 A). Although CD103+ DCs were comparable in their baseline activation and expression of CCR7 and CD86, only CD103+ DCs from WT or eosinophil-reconstituted ΔdblGATA1 mice up-regulated CCR7 and CD86 (Fig. 6 A) and emigrated from the LP in response to intestinal priming with PN+CT (Fig. 6 B). Likewise, activated CD103+ DCs accumulated in the MLN of WT, but not eosinophil-deficient mice, and this was corrected with eosinophil reconstitution (Fig. 6 C). The ability to mobilize SI DCs was not inherently disabled in eosinophil-deficient mice because CD103+ DCs migrated to the MLN in response to i.p. LPS (Fig. 6 C).
Figure 6.
Eosinophil control of CD103+ DC migration and activation is associated with degranulation in vitro and in vivo. WT, δdblGATA1 (GATA), or eosinophil-reconstituted (GATA+Eos) mice were kept naive or received PN+CT i.g. daily for three consecutive days, or i.p. LPS 16 h before analysis. (A) Expression of CCR7 and CD86 on SI DCs. (B) LP DC cell number. (C) Proportion, number, and activation status of CD103+ DCs in MLN. (D, top and bottom) Normal SI eosinophil transmission electron microscopy ultrastructure, showing bi-lobed nuclei and a high density of granules composed of an electron-dense core surrounded by an electron-lucent matrix rich in EPO (arrowhead). (E, top left) PN+CT-stimulated intact eosinophil with marked membrane protrusions and ruffling with loss of granule density. (E, top right) Formation of degranulation chambers (arrowheads). (E, bottom left) Extracellular free granules amid apoptotic/necrotic eosinophil debris (arrowheads). (E, bottom right) Dissolution of eosinophil granule matrix. (F) Purified eosinophils were incubated for 24 h with L-PAF or increasing amounts of PN+CT and assayed for EPO activity. Mean ± SEM, n = 3–8 from 2–4 experiments. *, P < 0.05 versus WT. ns, not statistically different versus WT.
To better understand how eosinophils control DC activation and migration, we undertook ultrastructural analysis of intestinal eosinophils within 24 h after i.g. PN+CT priming. Electron microscopy revealed that compared with normal SI eosinophils (Fig. 6 D) i.g. PN+CT caused marked morphological changes in LP eosinophils in vivo, including the development of cytoplasmic protrusions and cell membrane ruffling (Fig. 6 E, top row), marked decreases in granule density (Fig. 6 E, top row) and the development of degranulation chambers, a sign of exocytosis (Fig. 6 E, top right). We also observed membrane-bound granules and semidissolved granules amid extracellular cell debris (Fig. 6 E, bottom left). Together, these data illustrate that Th2 priming with PN+CT induces eosinophil degranulation by means of both active granule release and eosinophil cytolysis (Fig. 6 E). Notably, several granules lost their electron-lucent matrix (Fig. 6 E, bottom right), which contains the eosinophil-specific granule protein, EPO. To test if degranulation could result from direct encounter with allergen, eosinophils were activated in vitro with lyso-platelet–activating factor (L-PAF) as a positive control (Dyer et al., 2010), or PN+CT. Similar to L-PAF, PN+CT induced release of EPO (Fig. 6 F). Thus, eosinophils control CD103+ DC migration to the MLN in response to i.g. PN+CT, and this is associated with degranulation of EPO in vitro and in vivo.
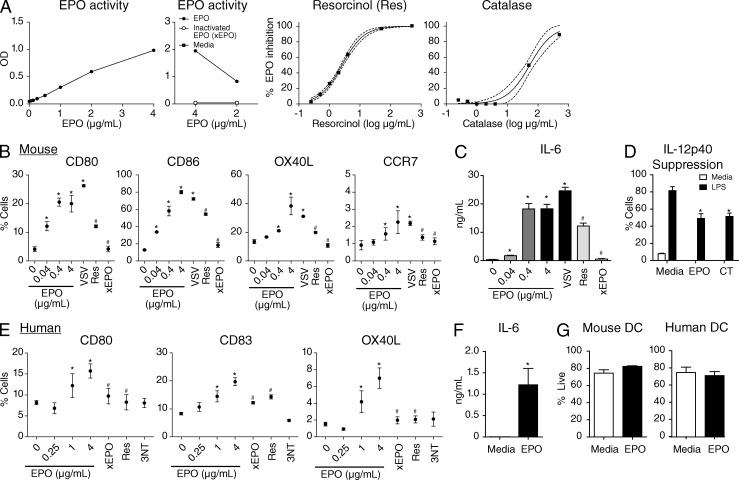
EPO activates mouse and human DCs
EPO is a peroxidase enzyme that oxidizes substrates through catalysis of hydrogen peroxide (H2O2). EPO-mediated oxidation of proteins generates 3-nitrotyrosine (3-NT; Duguet et al., 2001). As expected (Ain et al., 2002), recombinant EPO oxidative activity is abolished upon heat-induced denaturation, direct enzyme inhibition by resorcinol, or if H2O2 substrate is depleted with exogenous catalase (Fig. 7 A).
Figure 7.
EPO activates mouse and human DCs. (A) Characterization of recombinant EPO activity and conditions for enzyme inactivation. (B) Mouse BMDC activation status and (C) cytokine production was analyzed after incubation with increasing concentrations of EPO with or without resorcinol (Res), heat-inactivated EPO (xEPO), or a positive control replication-deficient vesicular stomatitis virus. (D) BMDCs were conditioned for 16 h with media, EPO, or CT as a positive control before stimulation with media or LPS and analysis for IL-12p40 by intracellular cytokine staining. (E) Human monocyte-derived DC activation status and (F) cytokine production was analyzed after incubation with increasing concentrations of EPO with or without resorcinol, xEPO, or 3-nitrotyrosine (3NT). (G) Viability of mouse and human DCs by PI exclusion and flow cytometry. Mean ± SEM, n = 3–8 from 2–4 experiments for mouse DCs; n = 16 from 2–4 experiments for human DCs. *, P < 0.05 vs. media. #, P < 0.05 versus 4 µg/ml EPO.
To test if EPO could directly activate mouse DCs, we generated BMDCs and incubated them with media, increasing concentrations of EPO, or a replication-deficient vesicular stomatitis virus (VSV) as a positive control (Boudreau et al., 2009). Compared with media controls, mouse DCs stimulated with EPO expressed higher levels of CD80, CD86, CCR7, and OX40L (Fig. 7 B), a co-stimulatory molecule that we have previously shown to be critical for driving intestinal Th2 immunization (Chu et al., 2013; Chu et al., 2014a). This effect was inhibited by heat-inactivation of EPO or co-incubation of EPO with resorcinol (Fig. 7, A and B). Consistent with this, DCs activated with EPO secreted high levels of IL-6 (Fig. 7 C) and TNF (not depicted), and this was inhibited by resorcinol or heat inactivation. We also tested if EPO selectively promoted Th2 responses through modulation of DC IL-12 production. To accomplish this, mouse DCs were conditioned with media, EPO, or CT as a positive control (Braun et al., 1999; Chu et al., 2013) before activation with LPS. Compared with mock conditioning, EPO significantly inhibited DC IL-12p40 production (Fig. 7 D). Thus, EPO directly activates mouse DC co-stimulatory molecule expression and proinflammatory cytokine production through its enzymatic activity, while also suppressing IL-12p40 production.
We next tested if this pathway was conserved in humans by incubating EPO with monocyte-derived DCs from healthy adult donors. EPO consistently activated human DCs in a dose-dependent manner, and this was inhibited by heat inactivation or resorcinol inhibition (Fig. 7 E). An end-product of EPO activity is the nitration of proteins, most readily detected as 3-NT (Duguet et al., 2001; Ulrich et al., 2008), and we questioned if 3-NT mediated the activation of DCs by EPO. However, 3-NT failed to stimulate human DCs over media controls (Fig. 7 E), suggesting that EPO activates DCs independently of 3-NT generation. Similar to mouse DCs, human DCs activated with EPO also secreted high levels of IL-6 (Fig. 7 F) and TNF (not depicted). Lastly, we evaluated potential toxicity of EPO-mediated activation of DCs. Notably, cell viability was not impaired after incubation of mouse and human DCs with EPO (Fig. 7 G). Thus, EPO can be a nontoxic direct activator of multiple DCs parameters through its oxidant enzyme activity in both mice and humans.
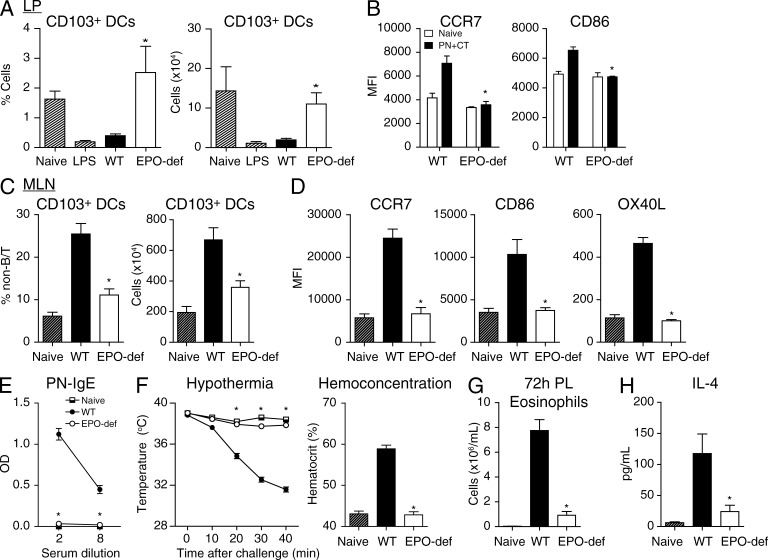
EPO-mediated mobilization and activation of DCs is required for intestinal Th2 priming
We next tested if this EPO–DC pathway was important for intestinal priming in vivo. In response to i.g. PN+CT, EPO-deficient mice phenocopied ΔdblGATA1 mice. Indeed, a lack of EPO resulted in the inability of DCs to be mobilized from the SI LP (Fig. 8, A and B) to the MLN (Fig. 8 C) and become activated, including up-regulation of CCR7, CD86, and OX40L (Fig. 8 D). As it would then be expected, EPO deficiency resulted in a lack of induction of antigen-specific IgE (Fig. 8 E) and full protection from anaphylaxis (Fig. 8 F), peritoneal delayed-type hypersensitivity eosinophilic inflammation (Fig. 8 G), and Th2 cytokine production (Fig. 8 H).
Figure 8.
EPO controls CD103+ DC migration, activation, and induction of Th2 immunity in vivo. WT or EPO-deficient mice were kept naive or (A) administered LPS i.p. 16 h before analysis, or (A–D) PN+CT i.g. daily for 3 d or (E–H) weekly for 4 wk. (A) Proportion and number of CD103+ DCs in SI LP. (B) Activation status of SI DCs. (C) Proportion and number of CD103+ DCs in the MLN. (D) CCR7, CD86, and OX40L expression. (E) Serum PN-IgE at week 5. (F) Clinical anaphylactic hypothermia and hemoconcentration. (G) Peritoneal eosinophilic inflammation 72 h after i.p. challenge. (H) Th2 cytokine production. Mean ± SEM, n = 3–8 from 2–3 experiments. *, P < 0.05 versus WT.
Similar to eosinophil-deficient mice, parenteral immunization did not rely on EPO for DC mobilization and activation, IgE or cytokine production, or induction of allergy and anaphylaxis (Fig. 9). Thus, DCs rely on eosinophil cues, at least in the form of EPO, to become activated and migrate to the MLN to initiate intestinal adaptive immunity in vivo.
Figure 9.
Parenteral immunization bypasses the requirement for EPO in DC activation and Th2 immunity. (A) WT or EPO-deficient mice received s.c. PN+CT or were kept naive, and draining inguinal LNs were analyzed 16–18 h later. Mice were immunized s.c. or i.p. weekly for 4 wk, or kept naive. (B) PN-IgE at wk 5. (C and D) Clinical responses after allergen challenge. (E) IL-4 production. Mean ± SEM, n = 3–8 from 2 experiments. ns, not significantly different.
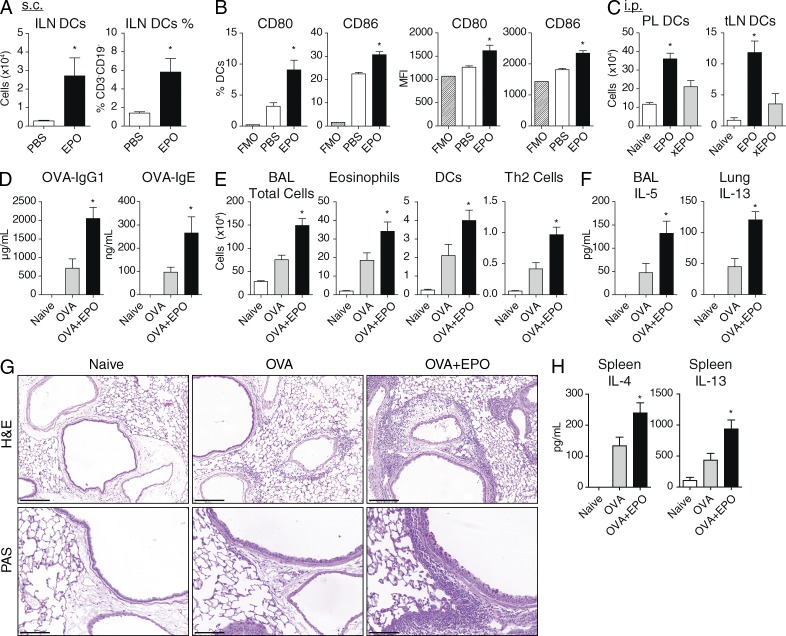
EPO promotes extraintestinal DC activation and adaptive immunity
Lastly, we evaluated whether EPO-mediated DC activation could be functional outside of the intestine in vivo. In response to the administration of EPO s.c. or i.p., DCs became activated and migrated to draining LNs (Fig. 10, A–C), suggesting that EPO could promote extraintestinal innate-to-adaptive immune activation.
Figure 10.
EPO promotes extraintestinal DC and adaptive immune activation in vivo. (A–C) WT mice received PBS, EPO, or heat-inactivated EPO (xEPO) s.c. or i.p. and 24 h later, respective draining inguinal (ILN) or thoracic (tLN) LNs were analyzed. (D–H) WT mice were immunized with OVA alone (OVA) or combination OVA with EPO (OVA+EPO) i.p. on d0 and 14, challenged i.n with OVA on d28-30 and analyzed 24 h later. (D) Serum OVA-specific IgG1 and IgE. (E) BAL inflammatory cells identified by total cell count and flow cytometry. (F) IL-5 in BAL and IL-13 in lung homogenates. (G) H&E staining of lung sections and PAS staining to identify goblet cells. (H) IL-4 and IL-13 cytokine production from OVA-stimulated splenocytes. Mean ± SEM, n = 3–7 from 2 experiments. *, P < 0.05 versus (A and B) PBS, (C) xEPO, or (D–H) OVA alone.
To test if EPO could act as an adjuvant in vivo, we used a standard model involving i.p. immunization, followed by recall i.n. challenge to induce airway inflammation. Compared with i.p. OVA alone, i.p. combination OVA with EPO (OVA+EPO) induced enhanced levels of OVA-specific IgG1 and IgE (Fig. 10 D). Further, when these mice were challenged with OVA i.n., OVA+EPO-immunized mice mounted greater inflammatory cellular responses, including total cells, eosinophils, DCs, and Th2 cells (Fig. 10 E). Both IL-5 and IL-13 were elevated in the lungs of mice immunized with OVA+EPO compared with those immunized with OVA alone (Fig. 10 F). Consistent with this, histological analysis of lungs revealed greater cellular inflammation and goblet cell hypertrophy and hyperplasia (Fig. 10 G). These enhanced responses were maintained during recall cytokine production, suggesting enhanced priming in the OVA+EPO group over those immunized with OVA alone. Thus, although EPO is necessary for enteral, but not parenteral, immune priming, these data show that EPO is sufficient for extraintestinal DC activation and promotion of adaptive immunity in vivo.
DISCUSSION
Recruited eosinophil granulocytes are a hallmark of Th2-mediated immune responses. However, in some tissue, particularly in the SI, eosinophils are constitutively present. In contrast to the conventional view of eosinophils as effector cells during Th2 responses, here we show that intestinal eosinophils play a critical role in the initiation of Th2 immunity with direct relevance to the development of food allergy. Eosinophil activation during intestinal immunization results in the release of EPO that triggers CD103+ DC activation and CCR7-dependent migration to the MLN, where DC CD86 and OX40L then control induction of Th2 responses. In support of these data, human intestinal eosinophils also degranulate during infection with CT-producing Vibrio cholera (Qadri et al., 2004), patients with food allergy exhibit increased intestinal eosinophil activation and degranulation compared to non-allergic controls (Vandezande et al., 1999; Schwab et al., 2003), and in vitro co-cultures of human DCs and eosinophils result in enhanced DC activation to CpG-ODN stimulation (Lotfi and Lotze, 2008). Indeed, here, we also show that EPO activates mouse and human DCs through its enzymatic activity, and this pathway is sufficient for EPO to act as an adjuvant in vivo. Thus, eosinophil-granule-DC shaping of adaptive immune responses may represent a therapeutic target in food allergy, and may also be a useful adjuvant or immunomodulator for other diseases.
The healthy intestinal tract has long been recognized as the most abundant site of normally resident eosinophils. Histological analyses of genetically deficient mice have shown that this baseline eosinophilia is partially dependent on eotaxin (Mishra et al., 1999) and independent of β7-integrin (Artis et al., 2000). More recently, Carlens et al. (2009) developed an eosinophil-sensitive intestinal isolation and flow cytometry method. They showed that SI eosinophils have a markedly longer lifespan compared with circulating eosinophils, and that regulation of cell survival rather than constant influx of newly generated eosinophils likely determines baseline SI eosinophilia (Carlens et al., 2009). Although additional factors that regulate homeostatic intestinal eosinophilia remain to be determined, herein we sought to better define the number of phenotype along the intestinal tract. We found that the SI, particularly the duodenum and jejunum, is enriched in eosinophils compared with the LI. Further, SI and LI eosinophils differed in expression of ST2, CD69, Ly6C, and CD11c. That CD11c is correlated with eosinophil longevity (Carlens et al., 2009) suggests that LI eosinophils may have shorter lives and hence, rely more on influx from the blood to maintain homeostatic tissue levels. This further supports the notion that SI and LI eosinophils may differ phenotypically and functionally. Indeed, priming through tissues with little to no baseline eosinophilia, such as the skin, peritoneum, or rectum, resulted in unimpaired Th2 priming in eosinophil deficient mice, which is consistent with reports of largely intact Th2 responses to the helminths Schistosoma mansoni (Swartz et al., 2006), Nippostrongylus brasiliensis (Knott et al., 2007), or Trichuris muris (Svensson et al., 2011) in the absence of eosinophils. Nevertheless, it remains to be tested whether the eosinophil–DC activation pathway identified here might also be operative in other tissues with abundant indigenous eosinophil populations, such as the uterus or thymus, or those in a pathological (hyper)eosinophilic state.
Aside from their classical cytotoxic/destructive inflammatory functions, eosinophils have more recently been ascribed various immunomodulatory and tissue remodeling activities (Rosenberg et al., 2013; Wong et al., 2014). Notably, several of these reports stem from in vitro work or data on eosinophils infiltrating helminth infected or allergen exposed tissues such as the lung, skin, or peritoneum. First, direct APC activity for T cell priming has been shown for eosinophils after they were Ag-pulsed in vitro, and then placed in co-culture or transferred to otherwise naive mice (Shi et al., 2000; Akuthota et al., 2010). Second, eosinophils have been shown to express IL-4 (Lacy and Moqbel, 2000; Shinkai et al., 2002; Voehringer et al., 2004; Svensson et al., 2011), and as the initial source of IL-4 required for naive CD4+ T to Th2 differentiation remains contentious, eosinophils have been speculated to be a potential candidate for this. In support of these data, eosinophils have long been recognized to localize to the T cell zone of LNs (Litt, 1964). Here, we found that intestinal LN eosinophils did not express MHC II, CCR7, or CD86 or increase in number under naive or immunized conditions in vivo and, further, that selective deletion of IL-4 in eosinophils did not impair the induction of Th2-cytokine mediated immunity. The defect in intestinal immunization of eosinophil-deficient mice was instead more proximal to the level of T or B cell activation as these mice could fully mount cellular and humoral Th2 responses to priming through the lung (Fattouh et al., 2011), skin, or peritoneum. These data highlight novel and essential contributions of indigenous eosinophils to shaping adaptive immunity. During the review of our article, a study was published that suggests a role for eosinophils in regulating B cells, particularly intestinal IgA (Chu et al., 2014b). These and our data also raise questions as to how eosinophils might regulate commensal microbes and vice versa.
Tolerance and immunity are viewed as opposing outcomes after intestinal antigen encounter with the immune system (Pabst and Mowat, 2012). DCs are also thought to be central to this process, with antigen-bearing CD103+ DCs migrating in a CCR7-dependent manner to the MLN to induce T regulatory cells. It is less clear how Th2 responses are induced. Indeed, Th2 responses to the intestinal helminth T. muris require basophils to act as APCs instead of DCs (Perrigoue et al., 2009). Although we have previously shown that basophils are not required for Th2 priming to oral antigen (Chu et al., 2013), we questioned the importance of DCs in this system. Indeed, although Fahlén-Yrlid et al. (2009) showed that CD11c-DTR–mediated depletion of CD11c+ cells prevented OVA+CT-induced IgG and IgA titers, it remained unclear to what extent this was due to depletion of DCs or eosinophils and whether or not this truly impacted Th2 immunity. Here, we clarify that at least this CD11c-DTR system can selectively deplete DCs over eosinophils, likely due to the 10–100-fold higher expression of CD11c on DCs and transgenic system setup. We further show that ablation of oral tolerance-associated CD103+ DCs or CCR7 prevented Th2 immunization. Thus, these data identify DCs as being critical for Th2 immunity in this system and further illustrate the potential Janus nature of intestinal CD103+ DCs as inducers of either tolerance or immunity to oral antigen (Laffont et al., 2010).
Granulocyte-DC cooperation has been reported in papain-induced Th2 responses, with antigen-presenting DCs cooperating with IL-4+ basophils during T cell priming (Tang et al., 2010). Herein, we identify a different level of granulocyte-DC cooperation: eosinophils and EPO mediate activation of DCs, and these activated DCs then migrate to the LN to prime T cells. We found that EPO oxidant enzymatic activity induced mouse and human DCs to up-regulate multiple co-stimulatory molecules, produce cytokines such as IL-6, and suppress IL-12p40 expression, without inducing toxicity. Although a hallmark end-product of EPO activity is production of 3-NT, stimulation of DCs with this failed to mimic the effects of EPO. Nonetheless, these data fortify the notion that DCs may heavily rely upon signals from the microenvironment, now including eosinophil cues, to initiate specific classes of adaptive immunity. Consistent with this, we found that eosinophil deficiency prevented Th2 induction, but did not impact T regulatory cell-mediated oral tolerance. Thus, the initiation and articulation of adaptive immunity is not only determined by direct DC sensing of antigen, but also by the demographics and activity of the cells neighboring those DCs.
We have analyzed the contribution of eosinophils to multiple parameters of intestinal innate and adaptive immunity and have found that normally resident SI eosinophils initiate primary adaptive immune responses through a pathway conserved in mice and humans that is dependent on EPO oxidant enzymatic activity. These data identify a role for indigenous eosinophil populations in influencing the initiation of adaptive immunity, as well as a Th2 induction pathway whereby the hallmark effector cell type also acts as an incipient early inducer of the very same immune cascade. That we identify a molecular link between food, eosinophils, DCs and T cell priming, suggests that eosinophil activation in the intestine may represent a primitive digestive-immune mechanism that has been coopted during evolution to aid in the initiation of adaptive immunity. Indeed, DC activation required degranulation of the microbicidal peroxidase EPO, consistent with an innate defense role for intestinal eosinophils (Yousefi et al., 2008). While this pathway is necessary to promote adaptive immunity in the SI, it is can be fully instigated extraintestinally. Therefore, the identification of a mechanism that shapes adaptive immunity through cooperative eosinophil-DC interaction should broadly encourage investigation into the role of eosinophils, EPO, or other eosinophil products in the (patho)genesis or treatment of immune mediated processes such as chronic inflammation, allergy, autoimmunity, cancer, vaccines and infectious disease.
MATERIALS AND METHODS
Mice.
Age-, sex-, vendor-, and strain-matched controls were used in all experiments. ΔdblGATA1 (C.Cg-Gata1tm6Sho) and CD11c-DTR (B6.FVB-Tg(Itgax-DTR/EGFP)57Lan/J; Jung et al., 2002) mice were bred in-house. IL-4 KO (BALB/c-Il4tm2Nnt/J), CCR7 KO (B6.129P2(C)-Ccr7tm1Rfor/J), IRF8(R249C; BXH2/TyJ), and EPO-deficient (Duguet et al., 2001; NZW/LacJ) mice were purchased from The Jackson Laboratory. IL-5 transgenic (IL-5Tg) mice were obtained from Charles River. All procedures were approved by the McMaster University Research Ethics Board.
Intestinal cell isolation.
Intestines were opened longitudinally, cut into 2–3 mm pieces and incubated in 1mM DTT (Sigma-Aldrich) in PBS for 15 min, and then 3 rounds of 15 min in 10% FBS in PBS and 2 mM EDTA before digestion in 0.239 mg/ml Collagenase A (Roche) with DNase (Roche) for 50–60 min and 40/70% Percoll (GE Healthcare) separation (Carlens et al., 2009).
Flow cytometry.
In all assays, cells were incubated with anti-FcγRII/IIIb before incubation with fluorochrome-conjugated antibodies. Dead cells were excluded by propidium iodide (PI) uptake or fixable viability dye eFluor780 (eBioscience), and gated on singlets. Whole blood was anticoagulated with EDTA and lysed with ACK lysis buffer before staining. Antibodies were obtained from eBioscience, BD, or BioLegend: CD3-FITC or Pacific Blue; CD4-APC, eFluor605, or eFluor650; CD19-PE-Cy5; MHC II-eFluor 650 or Alexa Fluor 700; F4/80-eFluor 450 or Pacific Blue; Siglec-F-PE; CD44-V500 or Alexa 700; B220-eFluor650 or V500; Ly6G-Alexa 700 or APC-Cy7; Ly6C-Alexa Fluor 700 or APC-Cy7; ST2-FITC or biotin; CD11b-PerCP-Cy5.5, Alexa Fluor 488, PE-Cy7, or Alexa Fluor 700; CD11c-APC, PerCP-Cy5.5, or PE-Cy7; CD69-PE-Cy7; CD45-eFluor605 or APC-eFluor780; CD103-APC, Brilliant Violet 421, or biotin; CD80-FITC; CD86-PE-Cy7, PerCP-Cy5.5, or eFluor605; OX40L-biotin; CCR7-biotin or APC; Streptavidin-APC, Qdot-800 (Invitrogen), or PE; IL-12p40-PE or APC; and TNF-PE or APC. Fluorescence minus one (FMO) controls were used for gating. Data were acquired on an LSR II (BD) and analyzed using FlowJo (Tree Star).
Intestinal Ig measurements.
Intestines were flushed with 5 ml ice cold soybean trypsin inhibitor (Sigma-Aldrich) in PBS-EDTA-PMSF, centrifuged at 2,000 rpm for 10 min, and supernatants analyzed for total IgA (Hapfelmeier et al., 2010).
Glucose uptake.
After an overnight fast, 2 g/kg d-glucose was administered by oral gavage. Blood glucose was measured at various time points using a hand-held glucometer (Accu-CheckActive; Roche).
Oral tolerance.
Mice were fed with PBS or 1 mg OVA (Grade V; Sigma-Aldrich) i.g. daily for days 0–5, and then injected with 200 µg OVA adsorbed to 1 mg aluminum hydroxide i.p. on days 7 and 14. Serum was collected on day 28 and analyzed for OVA-IgE (Cayman).
Peanut allergy model.
3.75 mg PN (Kraft) with 5 µg CT (List Biologicals) was administered i.g. (Delvo), i.p., p.r., or s.c. weekly for 4 wk, with challenge by crude PN extract (CPE; Greer) 1 wk later. Serum was collected 24 h before challenge and analyzed for PN-specific Igs (Chu et al., 2013). Temperature was assessed by rectal probe, and hematocrit by centrifuging anticoagulated blood at 40 min after challenge. Peritoneal lavage (PL) was performed with PBS-EDTA. Total cells were counted using Turks and hemocytometer. Peritoneal eosinophils were quantified using flow cytometry as F4/80lo, Siglec-F+ cells.
Adoptive transfer.
Spleen and PL from IL-5Tg mice were labeled with biotin-labeled antibodies against CD3, CD19, Thy1.2, B220, CD11c, MHC II, F4/80, c-Kit, TER-119, and >90% pure eosinophils isolated using antibiotin microbeads and LS MACS columns (Miltenyi Biotec) before 5 × 107 eosinophils were transferred i.v. to ΔdblGATA1 mice 16–24 h before each gavage.
Cytokine production.
800,000 live splenocytes were cultured for 120 h in complete RPMI alone or supplemented with 250 µg/ml CPE and cytokines in cell-free supernatants were quantified using Luminex (Millipore) or ELISA (R&D Systems).
Bone marrow chimeras.
Mice irradiated twice with 5.5 Gy (Cs137 source) received 5 × 106 T cell depleted BM cells i.v., rested for 8 wk, and then were used in experiments. 100 ng DT was injected i.p. 24 h before each gavage for CD11c-DTR experiments. For mixed BM chimeras, i.v. injections were composed of 80% WT or ΔdblGATA1 BM mixed with 20% IL-4 KO BM.
LN processing.
LNs were triturated between frosted slides in HBSS, washed and filtered (40 µm).
Transmission electron microscopy.
Immediately after excision, tissues were immersed in fixative consisting of 3% formaldehyde and 1% glutaraldehyde in 0.1-M phosphate buffer (pH 7.2). After the initial fixation, samples were post-fixed in 1% osmium tetroxide for 1 h, dehydrated in graded acetone solutions, and embedded in Polybed 812 (Polysciences, Inc.). Ultrathin sections (60–80 nm) were cut on an LKB MK III ultratome and routinely contrasted with uranyl acetate and lead citrate. The sections were examined using a FEI Tecnai Spirit BioTWIN transmission electron microscope (Fei).
EPO assay.
With minor modifications from previously described EPO assays (Humbles et al., 2002; Dyer et al., 2010), eosinophils were isolated as described above, and incubated for 24 h with media, L-PAF (Sigma-Aldrich), and 1 or 10 µg/ml PN+CT and assayed for EPO activity by oxidation of o-phenylenediamine (Sigma-Aldrich), stopped with sulphuric acid and absorbance measured at 492 nm. Results were normalized to maximal activity from Triton-X 100 lysed eosinophils. EPO was heat denatured by incubation at 90°C x 15–60 min and inhibited with resorcinol or catalase (both Sigma-Aldrich).
Mouse BM-derived DCs (BMDCs) generation, stimulation, and conditioning.
As previously reported (Chu et al., 2013), GM-CSF–derived BMDCs were generated and then incubated for 24 h with media, increasing concentrations of EPO with or without resorcinol, heat-inactivated EPO, or 25 multiplicity of infection VSV-ΔM51, which transduces DCs without significant progeny virus production or effect on viability. Some DCs were conditioned for 16 h with media, EPO, or 10 µg/ml CT before stimulation for 12 h with or without 10 ng/ml Escherichia coli 0111:B4 LPS (Cell culture tested; Sigma-Aldrich). For intracellular cytokine staining, DCs were incubated with 10 µg/ml brefeldin A (eBioscience) for the last 6 h. Supernatants were analyzed for IL-6 and TNF by duoset ELISA (R&D).
Generation of human monocyte-derived DCs (MoDCs) and immunophenotyping.
Peripheral blood was obtained from adult healthy human donors after informed consent and approval by the McMaster Research Ethics Board. PBMCs were isolated by Ficoll-Hypaque density gradient centrifugation using standard techniques and monocytes were enriched by adherence. Monocytes were differentiated for 8 d in X-VIVO 10 media (Lonza), supplemented with 5% pooled human AB serum (Corning) and 50 ng/ml IL-4 and GM-CSF (BioLegend), replacing with fresh media on day 4.
For immunophenotyping, the following conjugated antibodies were used: CD303-FITC, OX40L-PE (BD); CD1c-Brilliant Violet 421, CD14-Pacific Blue or -Brilliant Violet 605, CD3-Alexa Fluor 700, CD19-Alexa Fluor 700, CD56-Alexa Fluor 700, CD40-APC Cy7, CD80-PE Cy7, CD83-APC, CD86-Brilliant Violet 510, HLA-DR-PerCp Cy5.5, CCR7-PerCp eFluor710 (BioLegend); CD209-FITC (ABD Serotec). Blood DCs were defined as: lineage negative (CD3, CD19, CD56), HLA-DR positive, CD14 negative, and CD1c (myeloid DCs) or CD303 positive (plasmacytoid DCs). MoDCs were defined as CD14 low or negative and CD209 positive.
All stimulations were performed in X-VIVO 10 media with 5% human AB serum for 48 h. Some MoDCs were stimulated with 100 µM 3-NT (Eiserich et al., 1999; Sigma-Aldrich). MoDCs were stimulated at 5.0–7.5 × 105 cells/ml, whereas PBMCs were stimulated at 4.0 × 106 cells/ml. Cytokine secretion was measured using Ready-Set Go ELISAs (eBioscience) according to manufacturer’s instructions.
Airway inflammation model.
Mice were immunized i.p. with 100 µg OVA with or without 5 µg EPO on day 0 and 14, before i.n. challenge on days 28–30 and tissue collection on day 31. Lungs were homogenized in 500 µl PBS, incubated with 1% Triton-X 100 for 1 h under constant agitation, centrifuged at 13,000 rpm for 10 min and stored at −20°C. Bronchoalveolar lavage (BAL) was performed with sequential instillation and recovery of 300 and 400 µl PBS, respectively, before being spun at 2,000 rpm for 10 min, supernatants stored at −20°C and cell pellets resuspended in 150 µl PBS and counted with Turks. Spleens were stimulated with 40 µg/ml OVA for 5d (Fattouh et al., 2005). Cytokines were analyzed by Luminex.
Histology.
Formalin fixed lungs were dehydrated in graded ethanols, embedded in paraffin and cut to 4-µm sections before being stained with H&E or periodic acid-Schiff (PAS).
Statistics.
Comparisons were made using unpaired Student’s t tests or one- or two-way ANOVA. Repeated measures were used for temperature data. P < 0.05 was considered statistically significant.
Acknowledgments
We thank Cassie Colbert, Janis Macdonald, Juliana L. Xie, Waleed Ahmed, Talveer Mandur, Britt-Marie Nilsson, and Xueya Feng for technical assistance. We thank Dr. Jonathan Bramson for providing CD11c-DTR mice and Jane-Ann Smith for assistance with genotyping. We thank Dr. Elizabeth Walsh (National Institutes of Health) for assistance with adoptive transfer. We are grateful to all the volunteers who donated blood, and to the International Eosinophil Society and MIRC faculty for their support and insightful comments.
This work was supported by grants from Anaphylaxis Canada and MedImmune LLC. D.K. Chu is a CIHR Vanier scholar. MJ holds a senior Canada Research Chair. ALG was supported by a Fundación Caja Madrid doctoral scholarship (Spain). R. Kolbeck and AAH are employees of MedImmune LLC. All other authors declare no conflicts of interest.
D.K. Chu designed and performed experiments, analyzed data and wrote the manuscript. T.D. Walker, S. Goncharova, A. Llop-Guevara, N.G. Barra, J.D. Bassett, J. Kong, M.E. Gordon, R. Jimenez-Saiz, R. Fattouh, and P. Shen performed experiments. C.P. Verschoor performed and analyzed human DC experiments. J.S. Erjefält performed TEM experiments and analysis. R. Fattouh, R. Kolbeck, A.A. Humbles, K.D. McCoy, D.M. Bowdish and O. Pabst provided reagents and input. S. Waserman and M. Jordana obtained funding. M. Jordana oversaw the project and edited the manuscript.
Footnotes
Abbreviations used:
- 3-NT
- 3-nitrotyrosine
- BAL
- bronchoalveolar lavage
- BMDC
- BM-derived DC
- CT
- cholera toxin
- DT
- diphtheria toxin
- DTR
- DT receptor
- EPO
- eosinophil peroxidase
- GI
- gastrointestinal
- H&E
- hematoxylin and eosin
- i.g.
- intragastric
- LI
- large intestine
- LP
- lamina propria
- L-PAF
- lyso-platelet activating factor
- MLN
- mesenteric LN
- MoDC
- monocyte-derived DC
- PAS
- periodic-acid Schiff
- PL
- peritoneal lavage
- PN
- peanut
- Res
- Resorcinol
- SI
- small intestine
- VSV
- vesicular stomatitis virus
- xEPO
- heat-inactivated EPO
References
- Ain, R., Tash J.S., and Soares M.J.. 2002. A simple method for the in situ detection of eosinophils. J. Immunol. Methods. 260:273–278 10.1016/S0022-1759(01)00526-9 [DOI] [PubMed] [Google Scholar]
- Akuthota, P., Wang H., and Weller P.F.. 2010. Eosinophils as antigen-presenting cells in allergic upper airway disease. Curr. Opin. Allergy Clin. Immunol. 10:14–19 10.1097/ACI.0b013e328334f693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arias, K., Baig M., Colangelo M., Chu D., Walker T., Goncharova S., Coyle A., Vadas P., Waserman S., and Jordana M.. 2009. Concurrent blockade of platelet-activating factor and histamine prevents life-threatening peanut-induced anaphylactic reactions. J. Allergy Clin. Immunol. 124:307–314: e1–e2 10.1016/j.jaci.2009.03.012 [DOI] [PubMed] [Google Scholar]
- Arias, K., Chu D.K., Flader K., Botelho F., Walker T., Arias N., Humbles A.A., Coyle A.J., Oettgen H.C., Chang H.D., et al. 2011. Distinct immune effector pathways contribute to the full expression of peanut-induced anaphylactic reactions in mice. J. Allergy Clin. Immunol. 127:1552–1561: e1 10.1016/j.jaci.2011.03.044 [DOI] [PubMed] [Google Scholar]
- Artis, D., Humphreys N.E., Potten C.S., Wagner N., Müller W., McDermott J.R., Grencis R.K., and Else K.J.. 2000. Beta7 integrin-deficient mice: delayed leukocyte recruitment and attenuated protective immunity in the small intestine during enteric helminth infection. Eur. J. Immunol. 30:1656–1664 [DOI] [PubMed] [Google Scholar]
- Barnes, P.J.2004. New drugs for asthma. Nat. Rev. Drug Discov. 3:831–844 10.1038/nrd1524 [DOI] [PubMed] [Google Scholar]
- Berin, M.C., and Sampson H.A.. 2013. Food allergy: an enigmatic epidemic. Trends Immunol. 34:390–397 10.1016/j.it.2013.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boudreau, J.E., Bridle B.W., Stephenson K.B., Jenkins K.M., Brunellière J., Bramson J.L., Lichty B.D., and Wan Y.. 2009. Recombinant vesicular stomatitis virus transduction of dendritic cells enhances their ability to prime innate and adaptive antitumor immunity. Mol. Ther. 17:1465–1472 10.1038/mt.2009.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun, M.C., He J., Wu C.Y., and Kelsall B.L.. 1999. Cholera toxin suppresses interleukin (IL)-12 production and IL-12 receptor beta1 and beta2 chain expression. J. Exp. Med. 189:541–552 10.1084/jem.189.3.541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burks, A.W.2008. Peanut allergy. Lancet. 371:1538–1546 10.1016/S0140-6736(08)60659-5 [DOI] [PubMed] [Google Scholar]
- Cadman, E.T., and Lawrence R.A.. 2010. Granulocytes: effector cells or immunomodulators in the immune response to helminth infection? Parasite Immunol. 32:1–19 10.1111/j.1365-3024.2009.01147.x [DOI] [PubMed] [Google Scholar]
- Carlens, J., Wahl B., Ballmaier M., Bulfone-Paus S., Förster R., and Pabst O.. 2009. Common gamma-chain-dependent signals confer selective survival of eosinophils in the murine small intestine. J. Immunol. 183:5600–5607 10.4049/jimmunol.0801581 [DOI] [PubMed] [Google Scholar]
- Chu, D.K., Llop-Guevara A., Walker T.D., Flader K., Goncharova S., Boudreau J.E., Moore C.L., Seunghyun In T., Waserman S., Coyle A.J., et al. 2013. IL-33, but not thymic stromal lymphopoietin or IL-25, is central to mite and peanut allergic sensitization. J. Allergy Clin. Immunol. 131:187–200: e1–e8 10.1016/j.jaci.2012.08.002 [DOI] [PubMed] [Google Scholar]
- Chu, D.K., Mohammed-Ali Z., Jiménez-Saiz R., Walker T.D., Goncharova S., Llop-Guevara A., Kong J., Gordon M.E., Barra N.G., Gillgrass A.E., et al. 2014a. T helper cell IL-4 drives intestinal Th2 priming to oral peanut antigen, under the control of OX40L and independent of innate-like lymphocytes. Mucosal Immunol. 10.1038/mi.2014.29 [DOI] [PubMed] [Google Scholar]
- Chu, V.T., Beller A., Rausch S., Strandmark J., Zänker M., Arbach O., Kruglov A., and Berek C.. 2014b. Eosinophils promote generation and maintenance of immunoglobulin-A-expressing plasma cells and contribute to gut immune homeostasis. Immunity. 40:582–593 10.1016/j.immuni.2014.02.014 [DOI] [PubMed] [Google Scholar]
- Drury, A.N.1915. The eosinophil cell of teleostean fish. J. Physiol. 49:349–440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duguet, A., Iijima H., Eum S.Y., Hamid Q., and Eidelman D.H.. 2001. Eosinophil peroxidase mediates protein nitration in allergic airway inflammation in mice. Am. J. Respir. Crit. Care Med. 164:1119–1126 10.1164/ajrccm.164.7.2010085 [DOI] [PubMed] [Google Scholar]
- Duran-Jorda, F.1947. Secretion of red blood corpuscles. Nature. 159:293–294 10.1038/159293a0 [DOI] [PubMed] [Google Scholar]
- Dyer, K.D., Percopo C.M., Xie Z., Yang Z., Kim J.D., Davoine F., Lacy P., Druey K.M., Moqbel R., and Rosenberg H.F.. 2010. Mouse and human eosinophils degranulate in response to platelet-activating factor (PAF) and lysoPAF via a PAF-receptor-independent mechanism: evidence for a novel receptor. J. Immunol. 184:6327–6334 10.4049/jimmunol.0904043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelson, B.T., Kc W., Juang R., Kohyama M., Benoit L.A., Klekotka P.A., Moon C., Albring J.C., Ise W., Michael D.G., et al. 2010. Peripheral CD103+ dendritic cells form a unified subset developmentally related to CD8alpha+ conventional dendritic cells. J. Exp. Med. 207:823–836 10.1084/jem.20091627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eiserich, J.P., Estévez A.G., Bamberg T.V., Ye Y.Z., Chumley P.H., Beckman J.S., and Freeman B.A.. 1999. Microtubule dysfunction by posttranslational nitrotyrosination of alpha-tubulin: a nitric oxide-dependent mechanism of cellular injury. Proc. Natl. Acad. Sci. USA. 96:6365–6370 10.1073/pnas.96.11.6365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erlich, P.1879. Beitrage zur Kenntnis der granulierten Bindegewebszellen und der eosinophilen Leukocyten. Arch Anat Physiol. 3:166–169 [Google Scholar]
- Fahlén-Yrlid, L., Gustafsson T., Westlund J., Holmberg A., Strömbeck A., Blomquist M., MacPherson G.G., Holmgren J., and Yrlid U.. 2009. CD11c(high) dendritic cells are essential for activation of CD4+ T cells and generation of specific antibodies following mucosal immunization. J. Immunol. 183:5032–5041 10.4049/jimmunol.0803992 [DOI] [PubMed] [Google Scholar]
- Fattouh, R., Pouladi M.A., Alvarez D., Johnson J.R., Walker T.D., Goncharova S., Inman M.D., and Jordana M.. 2005. House dust mite facilitates ovalbumin-specific allergic sensitization and airway inflammation. Am. J. Respir. Crit. Care Med. 172:314–321 10.1164/rccm.200502-198OC [DOI] [PubMed] [Google Scholar]
- Fattouh, R., Al-Garawi A., Fattouh M., Arias K., Walker T.D., Goncharova S., Coyle A.J., Humbles A.A., and Jordana M.. 2011. Eosinophils are dispensable for allergic remodeling and immunity in a model of house dust mite-induced airway disease. Am. J. Respir. Crit. Care Med. 183:179–188 10.1164/rccm.200905-0736OC [DOI] [PubMed] [Google Scholar]
- Grinnan, D., Sung S.S., Dougherty J.A., Knowles A.R., Allen M.B., Rose C.E. III, Nakano H., Gunn M.D., Fu S.M., and Rose C.E. Jr. 2006. Enhanced allergen-induced airway inflammation in paucity of lymph node T cell (plt) mutant mice. J. Allergy Clin. Immunol. 118:1234–1241 10.1016/j.jaci.2006.07.036 [DOI] [PubMed] [Google Scholar]
- Hapfelmeier, S., Lawson M.A., Slack E., Kirundi J.K., Stoel M., Heikenwalder M., Cahenzli J., Velykoredko Y., Balmer M.L., Endt K., et al. 2010. Reversible microbial colonization of germ-free mice reveals the dynamics of IgA immune responses. Science. 328:1705–1709 10.1126/science.1188454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humbles, A.A., Lu B., Friend D.S., Okinaga S., Lora J., Al-Garawi A., Martin T.R., Gerard N.P., and Gerard C.. 2002. The murine CCR3 receptor regulates both the role of eosinophils and mast cells in allergen-induced airway inflammation and hyperresponsiveness. Proc. Natl. Acad. Sci. USA. 99:1479–1484 10.1073/pnas.261462598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humbles, A.A., Lloyd C.M., McMillan S.J., Friend D.S., Xanthou G., McKenna E.E., Ghiran S., Gerard N.P., Yu C., Orkin S.H., and Gerard C.. 2004. A critical role for eosinophils in allergic airways remodeling. Science. 305:1776–1779 10.1126/science.1100283 [DOI] [PubMed] [Google Scholar]
- Jung, S., Unutmaz D., Wong P., Sano G., De los Santos K., Sparwasser T., Wu S., Vuthoori S., Ko K., Zavala F., et al. 2002. In vivo depletion of CD11c+ dendritic cells abrogates priming of CD8+ T cells by exogenous cell-associated antigens. Immunity. 17:211–220 10.1016/S1074-7613(02)00365-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawakami, M., Narumoto O., Matsuo Y., Horiguchi K., Horiguchi S., Yamashita N., Sakaguchi M., Lipp M., Nagase T., and Yamashita N.. 2012. The role of CCR7 in allergic airway inflammation induced by house dust mite exposure. Cell. Immunol. 275:24–32 10.1016/j.cellimm.2012.03.009 [DOI] [PubMed] [Google Scholar]
- Knott, M.L., Matthaei K.I., Giacomin P.R., Wang H., Foster P.S., and Dent L.A.. 2007. Impaired resistance in early secondary Nippostrongylus brasiliensis infections in mice with defective eosinophilopoeisis. Int. J. Parasitol. 37:1367–1378 10.1016/j.ijpara.2007.04.006 [DOI] [PubMed] [Google Scholar]
- Lacy, P., and Moqbel R.. 2000. Eosinophil cytokines. Chem. Immunol. 76:134–155 10.1159/000058782 [DOI] [PubMed] [Google Scholar]
- Laffont, S., Siddiqui K.R., and Powrie F.. 2010. Intestinal inflammation abrogates the tolerogenic properties of MLN CD103+ dendritic cells. Eur. J. Immunol. 40:1877–1883 10.1002/eji.200939957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenzi, H.L., Pacheco R.G., Pelajo-Machado M., Panasco M.S., Romanha W.S., and Lenzi J.A.. 1997. Immunological system and Schistosoma mansoni: co-evolutionary immunobiology. What is the eosinophil role in parasite-host relationship? Mem. Inst. Oswaldo Cruz. 92(Suppl 2):19–32 10.1590/S0074-02761997000800005 [DOI] [PubMed] [Google Scholar]
- Leung, D.Y., Sampson H.A., Yunginger J.W., Burks A.W. Jr, Schneider L.C., Wortel C.H., Davis F.M., Hyun J.D., and Shanahan W.R. Jr. Avon Longitudinal Study of Parents and Children Study Team. 2003. Effect of anti-IgE therapy in patients with peanut allergy. N. Engl. J. Med. 348:986–993 10.1056/NEJMoa022613 [DOI] [PubMed] [Google Scholar]
- Li, X.M., Serebrisky D., Lee S.Y., Huang C.K., Bardina L., Schofield B.H., Stanley J.S., Burks A.W., Bannon G.A., and Sampson H.A.. 2000. A murine model of peanut anaphylaxis: T- and B-cell responses to a major peanut allergen mimic human responses. J. Allergy Clin. Immunol. 106:150–158 10.1067/mai.2000.107395 [DOI] [PubMed] [Google Scholar]
- Litt, M.1964. Eosinophils and Antigen-Antibody Reactions. Ann. N. Y. Acad. Sci. 116:964–985 10.1111/j.1749-6632.1964.tb52562.x [DOI] [PubMed] [Google Scholar]
- Lotfi, R., and Lotze M.T.. 2008. Eosinophils induce DC maturation, regulating immunity. J. Leukoc. Biol. 83:456–460 10.1189/jlb.0607366 [DOI] [PubMed] [Google Scholar]
- McGarry, M.2013. The Evolutionary Origins and Presence of Eosinophils in Extant Species. Eosinophils in Health and Disease. Lee J., and Rosenberg H., Elsevier Inc, Waltham, MA: pp. 13–17 10.1016/B978-0-12-394385-9.00002-X [DOI] [Google Scholar]
- Mishra, A., Hogan S.P., Lee J.J., Foster P.S., and Rothenberg M.E.. 1999. Fundamental signals that regulate eosinophil homing to the gastrointestinal tract. J. Clin. Invest. 103:1719–1727 10.1172/JCI6560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moschovakis, G.L., Bubke A., Dittrich-Breiholz O., Braun A., Prinz I., Kremmer E., and Förster R.. 2012. Deficient CCR7 signaling promotes TH2 polarization and B-cell activation in vivo. Eur. J. Immunol. 42:48–57 10.1002/eji.201141753 [DOI] [PubMed] [Google Scholar]
- Mowat, A., and Bain C.. 2010. The curious case of the intestinal eosinophil. Mucosal Immunol. 3:420–421 10.1038/mi.2010.24 [DOI] [Google Scholar]
- Nei, Y., Obata-Ninomiya K., Tsutsui H., Ishiwata K., Miyasaka M., Matsumoto K., Nakae S., Kanuka H., Inase N., and Karasuyama H.. 2013. GATA-1 regulates the generation and function of basophils. Proc. Natl. Acad. Sci. USA. 110:18620–18625 10.1073/pnas.1311668110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pabst, O., and Mowat A.M.. 2012. Oral tolerance to food protein. Mucosal Immunol. 5:232–239 10.1038/mi.2012.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul, W.E., and Zhu J.. 2010. How are T(H)2-type immune responses initiated and amplified? Nat. Rev. Immunol. 10:225–235 10.1038/nri2735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrigoue, J.G., Saenz S.A., Siracusa M.C., Allenspach E.J., Taylor B.C., Giacomin P.R., Nair M.G., Du Y., Zaph C., van Rooijen N., et al. 2009. MHC class II-dependent basophil-CD4+ T cell interactions promote T(H)2 cytokine-dependent immunity. Nat. Immunol. 10:697–705 10.1038/ni.1740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulendran, B., Tang H., and Manicassamy S.. 2010. Programming dendritic cells to induce T(H)2 and tolerogenic responses. Nat. Immunol. 11:647–655 10.1038/ni.1894 [DOI] [PubMed] [Google Scholar]
- Qadri, F., Bhuiyan T.R., Dutta K.K., Raqib R., Alam M.S., Alam N.H., Svennerholm A.M., and Mathan M.M.. 2004. Acute dehydrating disease caused by Vibrio cholerae serogroups O1 and O139 induce increases in innate cells and inflammatory mediators at the mucosal surface of the gut. Gut. 53:62–69 10.1136/gut.53.1.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritz, S.A., Stämpfli M.R., Davies D.E., Holgate S.T., and Jordana M.. 2002. On the generation of allergic airway diseases: from GM-CSF to Kyoto. Trends Immunol. 23:396–402 10.1016/S1471-4906(02)02278-0 [DOI] [PubMed] [Google Scholar]
- Rosenberg, H.F., Dyer K.D., and Foster P.S.. 2013. Eosinophils: changing perspectives in health and disease. Nat. Rev. Immunol. 13:9–22 10.1038/nri3341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz, O., Jaensson E., Persson E.K., Liu X., Worbs T., Agace W.W., and Pabst O.. 2009. Intestinal CD103+, but not CX3CR1+, antigen sampling cells migrate in lymph and serve classical dendritic cell functions. J. Exp. Med. 206:3101–3114 10.1084/jem.20091925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwab, D., Müller S., Aigner T., Neureiter D., Kirchner T., Hahn E.G., and Raithel M.. 2003. Functional and morphologic characterization of eosinophils in the lower intestinal mucosa of patients with food allergy. Am. J. Gastroenterol. 98:1525–1534 10.1111/j.1572-0241.2003.07484.x [DOI] [PubMed] [Google Scholar]
- Shi, H.Z., Humbles A., Gerard C., Jin Z., and Weller P.F.. 2000. Lymph node trafficking and antigen presentation by endobronchial eosinophils. J. Clin. Invest. 105:945–953 10.1172/JCI8945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinkai, K., Mohrs M., and Locksley R.M.. 2002. Helper T cells regulate type-2 innate immunity in vivo. Nature. 420:825–829 10.1038/nature01202 [DOI] [PubMed] [Google Scholar]
- Sokol, C.L., Chu N.Q., Yu S., Nish S.A., Laufer T.M., and Medzhitov R.. 2009. Basophils function as antigen-presenting cells for an allergen-induced T helper type 2 response. Nat. Immunol. 10:713–720 10.1038/ni.1738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svensson, M., Bell L., Little M.C., DeSchoolmeester M., Locksley R.M., and Else K.J.. 2011. Accumulation of eosinophils in intestine-draining mesenteric lymph nodes occurs after Trichuris muris infection. Parasite Immunol. 33:1–11 10.1111/j.1365-3024.2010.01246.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz, J.M., Dyer K.D., Cheever A.W., Ramalingam T., Pesnicak L., Domachowske J.B., Lee J.J., Lee N.A., Foster P.S., Wynn T.A., and Rosenberg H.F.. 2006. Schistosoma mansoni infection in eosinophil lineage-ablated mice. Blood. 108:2420–2427 10.1182/blood-2006-04-015933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang, H., Cao W., Kasturi S.P., Ravindran R., Nakaya H.I., Kundu K., Murthy N., Kepler T.B., Malissen B., and Pulendran B.. 2010. The T helper type 2 response to cysteine proteases requires dendritic cell-basophil cooperation via ROS-mediated signaling. Nat. Immunol. 11:608–617 10.1038/ni.1883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbull, E.L., Yrlid U., Jenkins C.D., and Macpherson G.G.. 2005. Intestinal dendritic cell subsets: differential effects of systemic TLR4 stimulation on migratory fate and activation in vivo. J. Immunol. 174:1374–1384 10.4049/jimmunol.174.3.1374 [DOI] [PubMed] [Google Scholar]
- Ulrich, M., Petre A., Youhnovski N., Prömm F., Schirle M., Schumm M., Pero R.S., Doyle A., Checkel J., Kita H., et al. 2008. Post-translational tyrosine nitration of eosinophil granule toxins mediated by eosinophil peroxidase. J. Biol. Chem. 283:28629–28640 10.1074/jbc.M801196200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vadas, P., Gold M., Perelman B., Liss G.M., Lack G., Blyth T., Simons F.E., Simons K.J., Cass D., and Yeung J.. 2008. Platelet-activating factor, PAF acetylhydrolase, and severe anaphylaxis. N. Engl. J. Med. 358:28–35 10.1056/NEJMoa070030 [DOI] [PubMed] [Google Scholar]
- Vandezande, L.M., Wallaert B., Desreumaux P., Tsicopoulos A., Lamblin C., Tonnel A.B., and Janin A.. 1999. Interleukin-5 immunoreactivity and mRNA expression in gut mucosa from patients with food allergy. Clin. Exp. Allergy. 29:652–659 10.1046/j.1365-2222.1999.00511.x [DOI] [PubMed] [Google Scholar]
- Voehringer, D., Shinkai K., and Locksley R.M.. 2004. Type 2 immunity reflects orchestrated recruitment of cells committed to IL-4 production. Immunity. 20:267–277 10.1016/S1074-7613(04)00026-3 [DOI] [PubMed] [Google Scholar]
- Wong, T.W., Doyle A.D., Lee J.J., and Jelinek D.F.. 2014. Eosinophils regulate peripheral B cell numbers in both mice and humans. J. Immunol. 192:3548–3558 10.4049/jimmunol.1302241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worbs, T., Bode U., Yan S., Hoffmann M.W., Hintzen G., Bernhardt G., Förster R., and Pabst O.. 2006. Oral tolerance originates in the intestinal immune system and relies on antigen carriage by dendritic cells. J. Exp. Med. 203:519–527 10.1084/jem.20052016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yousefi, S., Gold J.A., Andina N., Lee J.J., Kelly A.M., Kozlowski E., Schmid I., Straumann A., Reichenbach J., Gleich G.J., and Simon H.U.. 2008. Catapult-like release of mitochondrial DNA by eosinophils contributes to antibacterial defense. Nat. Med. 14:949–953 10.1038/nm.1855 [DOI] [PubMed] [Google Scholar]
- Yu, C., Cantor A.B., Yang H., Browne C., Wells R.A., Fujiwara Y., and Orkin S.H.. 2002. Targeted deletion of a high-affinity GATA-binding site in the GATA-1 promoter leads to selective loss of the eosinophil lineage in vivo. J. Exp. Med. 195:1387–1395 10.1084/jem.20020656 [DOI] [PMC free article] [PubMed] [Google Scholar]