Dr. Tuveson and colleagues provide a comprehensive review on the fundamental role of cancer-associated fibroblasts in shaping the tumor microenvironment and promoting tumor initiation and progression.
Abstract
Fibroblasts regulate the structure and function of healthy tissues, participate transiently in tissue repair after acute inflammation, and assume an aberrant stimulatory role during chronic inflammatory states including cancer. Such cancer-associated fibroblasts (CAFs) modulate the tumor microenvironment and influence the behavior of neoplastic cells in either a tumor-promoting or tumor-inhibiting manner. These pleiotropic functions highlight the inherent plasticity of fibroblasts and may provide new avenues to understand and therapeutically intervene in malignancies. We discuss the emerging themes of CAF biology in the context of tumorigenesis and therapy.
Although the concept of “seed and soil” was proposed over 100 years ago (Paget, 1889), investigators have only recently revealed the fundamental importance of the tumor-associated stoma in cancer development. Fibroblasts are essential in tissue homeostasis and wound healing, and consistent with the hypothesis that “a tumor is a wound that never heals” (Dvorak, 1986), an emerging body of evidence demonstrates that the fibroblasts in tumors, often referred to as cancer-associated fibroblasts (CAFs), are key players in the process of tumorigenesis (Hanahan and Weinberg, 2011). Indeed, recent studies have shown that many of the cancer-promoting and therapy-resisting properties of the stroma can be attributed to the activity of fibroblasts. It is necessary to acknowledge that CAFs can derive from multiple origins and make up a heterogeneous population of cells but nevertheless are united by their capacity to alter the tumor microenvironment and to change the fate of neoplastic cells.
To be able to fully understand the role of fibroblasts in cancer, it is important to consider the function of this cell type in normal tissues. Fibroblasts are elongated cells of mesodermal origin, showing a fusiform or spindle-like shape, and express fibroblast-specific protein 1 (FSP-1; Strutz et al., 1995). Beyond FSP-1, they show a complex expression pattern of protein markers, reflecting an inherent diversity within a population of fibroblasts (Anderberg and Pietras, 2009).
Fibroblasts are found embedded within the extracellular matrix (ECM) and are the most abundant cell type in connective tissue. The ECM is composed of fibrillar collagens, fibronectins, hyaluronic acid, and proteoglycans, providing a structural framework for all tissues. The ECM also acts as a reservoir for cytokines and growth factors, and as a scaffold for cell migration. In fact, fibroblasts are the major producers of the ECM and thereby participate in tissue homeostasis, and the regulation of interstitial fluid volume and pressure. Fibroblasts are also highly involved in regulating tissue remodeling and repair. Upon tissue damage, fibroblasts proliferate and differentiate into myofibroblasts, a process characterized by de novo expression of α–smooth muscle actin (α-SMA), contractile stress fibers, and splice variants of fibronectin (Serini et al., 1998; Tomasek et al., 2002). The synthesis of ECM and ECM remodeling proteases is up-regulated, resulting in deposition of a reactive stroma, often referred to as a desmoplastic reaction or desmoplastic stroma. The induced expression of α–SMA alters cytoskeletal organization, which increases the contractile ability of myofibroblasts (Rønnov-Jessen and Petersen, 1996; Hinz et al., 2001). Myofibroblasts contract the ECM to bring the borders of the wound together, and secrete matrix proteins that repair the remaining tissue defects and attract epithelial cells to complete the healing process. Upon completion of wound healing, activated fibroblasts undergo apoptosis (Desmoulière et al., 1995) or a particular type of programmed cell death termed nemosis (programmed necrosis; Bizik et al., 2004).
Definition and markers of CAFs
CAFs are found in almost all solid tumors; however, their abundance varies between different types of cancers. For example, breast, prostate, and pancreatic cancers contain high numbers of CAFs, whereas brain, renal, and ovarian cancers demonstrate fewer (Neesse et al., 2011; Smith et al., 2013). They are defined as all the fibroblastic, nonneoplastic, nonvascular, nonepithelial, and noninflammatory cells found in a tumor (Fig. 1). However, there is no consensus on their molecular definition (Kalluri and Zeisberg, 2006; Orimo and Weinberg, 2007; Pietras and Ostman, 2010; Xing et al., 2010). CAFs can be distinguished from neoplastic cells that have undergone epithelial-mesenchymal transition and show a fibroblast-like morphology by their stable karyotype and the lack of genetic alterations. Although p53 mutations in CAFs have been reported (Kurose et al., 2002; Hill et al., 2005; Patocs et al., 2007), these studies have been criticized for using methods highly prone to generating experimental artifacts (Campbell et al., 2009). Moreover, recent studies have confirmed the lack of frequent mutations in CAFs (Qiu et al., 2008; Walter et al., 2008; Hosein et al., 2010).
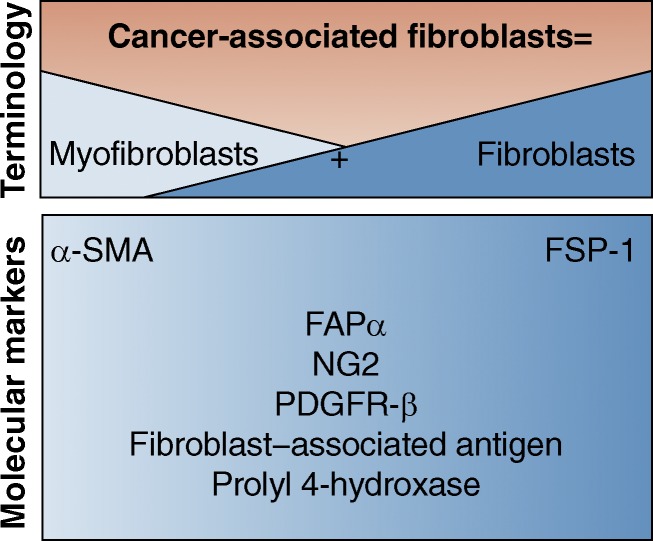
Figure 1.
Molecular definition of cancer-associated fibroblasts. CAFs are composed of two morphologically distinctive populations: fibroblasts and myofibroblasts. Indicated are common molecular markers that define CAFs.
The molecular definition of CAFs is still a debated issue, and emerging data demonstrate that CAFs make up a complex and heterogeneous population of cells. Several markers have been suggested in the past to define CAFs, but it is now being appreciated that these markers do not mark all CAFs and that most of them are not even unique to CAFs or to the fibroblasts lineage. α–SMA is a robust CAF marker, which usually identifies CAFs with myofibroblast morphology (Desmoulière et al., 2004). Nonetheless, α–SMA is also expressed by normal fibroblasts (Hawinkels et al., 2014), and in some cases, normal fibroblasts show comparable or even more α–SMA expression compared with CAFs (Madar et al., 2009; Berdiel-Acer et al., 2014). α–SMA expression is detected in other cell types as well, such as pericytes and smooth muscle cells surrounding vasculature, visceral smooth muscle cells, and cardiomyocytes (Wendling et al., 2009). The cell-surface serine protease fibroblast-activation protein α (FAPα) is another common marker for CAFs in many carcinomas including breast, lung, ovarian, and pancreatic (Garin-Chesa et al., 1990). However, FAPα is also not specific to CAFs, as it is highly expressed in quiescent mesodermal cells in multiple tissue types (Roberts et al., 2013), and activated fibroblasts during wound healing and collagen vascular disease (Wang et al., 2005). Another well-studied marker is FSP-1 (also known as S100A4), which seems to play a distinctive and somewhat dual role in cancer, as evident by a protective role of FSP-1–positive cells against carcinogen-mediated malignancy (Zhang et al., 2013a). Yet FSP-1 is also not restricted to CAFs and is also expressed by epithelial cells undergoing EMT (Okada et al., 1997) and bone marrow–derived cells, including macrophages, that respond to tissue injury (Österreicher et al., 2011; Cheng et al., 2012). Additional proteins expressed in some CAFs include NG2 (Neuron-glial Antigen-2, also known as Chondroitin sulfate proteoglycan), platelet-derived growth factor receptor–β (PDGFR-β), fibroblast-associated antigen, and Prolyl 4-hydroxylase (Orimo and Weinberg, 2007). However, these markers are also not unique to CAFs. For example, NG2 is a neural marker that is expressed in the nervous system (Polito and Reynolds, 2005), and PDGFR-β expression is also common to vascular smooth muscles, skeletal muscles, and myocardium (Cuttler et al., 2011). PDGFR-β was recently reported to be expressed by invasive pancreatic cancer cells (Weissmueller et al., 2014) and thus may also represent a new EMT marker.
It is therefore important to keep in mind that there is currently no marker that completely and exclusively defines CAFs, and this should be taken into account when interpreting results from different models. Moreover, apart from FSP-1, which identifies a unique CAF population, these proteins are often expressed or coexpressed heterogeneously among CAFs, possibly reflecting different stages of activation and sources of CAFs (Fig. 1; Sugimoto et al., 2006).
The origin of CAFs
Several tissues contribute to the population of CAFs found in an individual tumor (Fig. 2; Xing et al., 2010; Cirri and Chiarugi, 2011). Indeed, numerous cell types have been reported to transdifferentiate to CAFs. The most direct source of CAFs derives from resident tissue fibroblasts and mesenchymal stem cells (MSCs; Rønnov-Jessen and Petersen, 1993; Kojima et al., 2010; Paunescu et al., 2011; Quante et al., 2011; Vicent et al., 2012). The stellate cell is a distinct cell type that shares many of the same functions as fibroblasts. In its quiescent state it is a vitamin A–storing and lipid droplet–containing cell that can be found in the liver, pancreas, kidney, intestine, lung, spleen, uterus, and skin (Kordes et al., 2009). Similar to fibroblasts, stellate cells activate α-SMA expression upon stimulation and acquire a myofibroblast-like phenotype. Stellate cells are responsible for the majority of the desmoplastic reaction seen in chronic pancreatitis and pancreatic cancer (Bachem et al., 1998), as well as in liver fibrosis (Yin et al., 2013), and are categorized as CAFs when seen in cancer tissue. In addition to these local sources of CAFs, bone marrow–derived cells termed fibrocytes can be recruited to the tumor and differentiate into myofibroblasts and fibroblasts (Ishii et al., 2003; Direkze et al., 2004; Mishra et al., 2008; Kidd et al., 2012). α–SMA–expressing myofibroblasts have also been shown to originate from neighboring adipose tissue (Kidd et al., 2012). Endothelial-mesenchymal transition (EndMT), a process where endothelial cells down-regulate their CD31 expression and induce expression of FSP-1, is another potential source of CAFs (Zeisberg et al., 2007). FSP-1–positive fibroblasts can also be derived from local epithelial-mesenchymal transition (EMT), indicating that nontransformed epithelial cells may be an additional source of CAFs by undergoing EMT in response to stimuli from surrounding cells (Iwano et al., 2002). Therefore, CAFs may be derived from multiple tissue types, reflecting local and distant cues that are sensed during tumorigenesis, and thus cannot be referred to as one population of cells. The relative contribution of each source of CAFs is highly dependent on the experimental conditions used and less certain in actual human cancers.
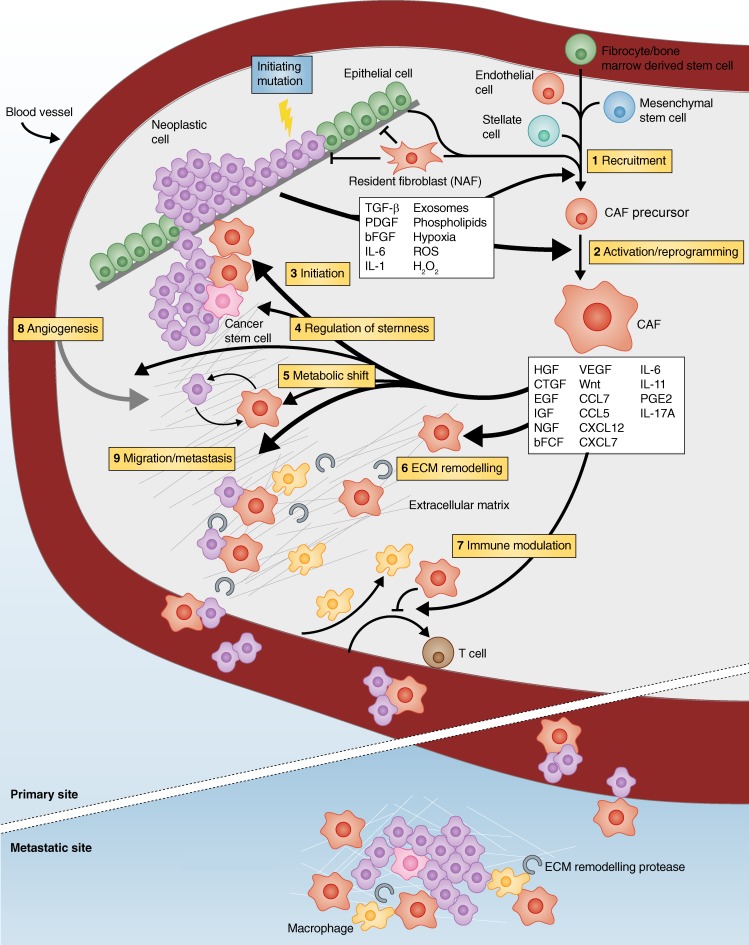
Figure 2.
CAFs promote tumorigenesis: a schematic illustration representing all the fronts in which CAFs boost cancer. By secreting soluble factors and lipid-based particles, transformed epithelium drives recruitment (1) and reprogramming (2) of several types of cells into CAFs, including resident fibroblasts (NAFs) that are naturally tumor-suppressive. CAFs are then activated to promote tumor initiation (3), cancer cell stemness (4), and to change tumor metabolism (5) by intensive cross talk of ligands/receptors, cell–cell contact, and remodeling the ECM (6). Concomitantly, CAFs prevent immune surveillance of tumor cells (7) while balancing inflammation and angiogenesis (8). Finally, CAFs stimulate invasion and metastasis by facilitating tumor cell dissemination, intra- and extravasation, and metastatic colonization (9).
Neoplastic cells recruit and activate CAFs
Early work of Stoker et al. (1966) demonstrated that normal quiescent fibroblasts inhibit the growth of polyoma-transformed cells by direct contact between the two cell types. It has later been shown that normal tissue-associated fibroblasts (NAFs) isolated from different organs can inhibit the growth of neoplastic cells (Flaberg et al., 2011), presumably due to the ability of fibroblasts to maintain epithelial homeostasis and proliferative quiescence (Trimboli et al., 2009). Indeed, this has been proposed as one reason why certain tumors found in autopsy studies appear dormant and nonprogressing (Bissell and Hines, 2011). Given these properties of NAFs, neoplastic cells must evolve to both recruit fibroblasts (from the different potential sources mentioned above) and to reprogram them into CAFs, thereby converting the fibroblast from being tumor suppressive to tumor supportive. Interestingly, once reprogrammed, the CAF phenotype can persist in cell culture even in the absence of continued exposure to intratumoral stimuli (Orimo et al., 2005). Several studies have shown that NAFs are functionally distinct from CAFs. Prostate CAFs are more proliferative and less prone to contact inhibition than their NAF counterparts (Madar et al., 2009). Furthermore, colonic CAFs more potently induce the proliferation and migration of neoplastic cells compared with NAFs (Berdiel-Acer et al., 2014).
Oncogenic signaling within neoplastic cells frequently drives the recruitment and activation of fibroblasts by secreting fibroblast-activating factors (Yang et al., 2006), thereby mimicking the normal wound healing process where these factors are normally secreted from injured epithelial cells and macrophages (Fig. 2). TGF-β is a major regulator of fibrosis and is one of the most important and well-studied cancer cell–derived factors affecting CAF activation (Lieubeau et al., 1994; Löhr et al., 2001). TGF-β binds to the type-2 TGF-β receptor (TGFBR2) on the cell surface of fibroblasts, inducing recruitment and phosphorylation of TGFBR1 and expression of factors involved in paracrine signaling and ECM production and remodeling (Pickup et al., 2013a). Platelet-derived growth factor (PDGF) is also highly expressed in most neoplastic cells, which rarely express PDGF receptors (PDGFRs) themselves. Instead, other cell types, such as CAFs and endothelial cells, express PDGFR (Bronzert et al., 1987; Forsberg et al., 1993), and PDGF has been shown to stimulate proliferation of CAFs and to be an important initiator of the desmoplastic reaction in tumors (Shao et al., 2000). Basic fibroblast growth factor (bFGF) is another mitogen secreted by neoplastic cells that stimulates the proliferation and differentiation of fibroblasts to CAFs (Armelin, 1973; Strutz et al., 2000; Kwabi-Addo et al., 2004). Cytokines produced by neoplastic cells, including IL-6, also stimulate the production of CAFs (Giannoni et al., 2010). In addition, phospholipid derivates, such as lysophosphatidic acid (LPA), can be secreted from neoplastic cells to stimulate differentiation of human MSCs into myofibroblast-like CAFs (Jeon et al., 2008).
Besides growth factors and cytokines, other mechanisms of CAF activation have been reported. For example, exosomes can transfer protein, RNA, and microRNA (miR) from one cell to another, and cancer-derived exosomes have been shown to contribute to the recruitment and activation of fibroblasts and MSCs within tumors (Webber et al., 2010; Cho et al., 2012; Gu et al., 2012; Kahlert and Kalluri, 2013). In addition, hypoxia and reactive oxygen species (ROS) promote activation of CAFs. ROS have been shown to support conversion of fibroblasts into myofibroblasts through the accumulation of the hypoxia-inducible factor (HIF)-1α, whereas antioxidants have been found to reduce HIF-1α levels, inhibiting numerous myofibroblast features (Toullec et al., 2010).
CAFs modulate the tumor microenvironment
Upon reprogramming, many transcriptional changes occur that distinguish CAFs from their normal counterparts (Allinen et al., 2004; Nakagawa et al., 2004; Hu et al., 2005). Reprogramming cells into CAFs also involves changes in miR expression, affecting target genes posttranscriptionally (Aprelikova et al., 2010, 2013; Musumeci et al., 2011; Bronisz et al., 2012; Mitra et al., 2012; Masamune et al., 2014). Furthermore, epigenetic changes, such as global DNA hypomethylation frequently seen in neoplastic cells, have also been observed in CAFs (Jiang et al., 2008). Together, all these gene regulatory changes induce a shift in the metabolome and secretome, which maintain the differentiated state of myofibroblasts in an autocrine manner (Kojima et al., 2010) but also stimulate neoplastic cells in a paracrine manner (Fig. 2). In the following sections, we will discuss principle strategies used by activated CAFs to communicate these protumorigenic effects.
CAFs secrete soluble factors.
CAFs orchestrate key pathophysiological processes in cancer development through paracrine interactions involving the secretion of multiple soluble factors. Growth factors such as hepatocyte growth factor (HGF), connective tissue growth factor (CTGF), epidermal growth factor (EGF), insulin-like growth factor (IGF), nerve growth factor (NGF), basic fibroblast growth factor (bFGF), and members of the Wnt family (Orimo et al., 2001, 2005; Allinen et al., 2004; Bhowmick et al., 2004; Kalluri and Zeisberg, 2006; Erez et al., 2010; Räsänen and Vaheri, 2010; Chaffer and Weinberg, 2011; Cirri and Chiarugi, 2011), as well as many cytokines, such as CCL7 and CXCL12 (Orimo et al., 2005; Jung et al., 2010), have all been reported to be involved in this paracrine cross talk. The CAF secretome also regulates angiogenesis. Vascular endothelial growth factor A (VEGF-A) is induced in CAFs by neoplastic cells (Guo et al., 2008), as well as CXCL12, CXCL14, and CTGF (Orimo et al., 2005; Yang et al., 2005; Augsten et al., 2009). The three most studied CAF-secreted factors will hereafter be discussed in detail.
CXCL12 is highly overexpressed in CAFs (Allinen et al., 2004) and several in vitro and in vivo models have revealed a key role of CXCL12 and its receptor CXCR4 in tumor–stroma interactions. CXCL12 provides stimulatory input to CXCR4-expressing neoplastic cells, resulting in proliferation and migration (Domanska et al., 2012). In pancreatic cancer cells, CXCL12/CXCR4 signaling triggers invasion and EMT through noncanonical Hedgehog pathway (Li et al., 2012c) and further contributes to cancer progression by activation of the canonical Wnt pathway (Wang et al., 2008). CTGF has a key role in fibrosis (Gao and Brigstock, 2005) and is also highly up-regulated in numerous cancers (Jacobson and Cunningham, 2012), including pancreatic ductal adenocarcinoma (Charrier and Brigstock, 2013). CTGF expression is induced by TGF-β (Pickup et al., 2013a) and hypoxia (Eguchi et al., 2013) in both activated pancreatic stellate cells and neoplastic cells (Hartel et al., 2004) and causes increased invasiveness of neoplastic cells, which can be inhibited through CTGF depletion (Eguchi et al., 2013). In head and neck squamous cancer cells, CTGF enhanced stem-like properties and increased expression of multiple pluripotency genes (Chang et al., 2013). HGF was originally identified as a mitogen for hepatocytes but also plays an important role in wound healing and tissue repair. Normally, HGF is sequestered in the ECM in a latent form. Proteolysis of the latent form of HGF enables binding to and signaling by the c-Met tyrosine kinase (Benvenuti and Comoglio, 2007). The c-Met signaling pathway is often affected in cancer, either by mutations in neoplastic cells leading to constant oncogenic c-Met signaling (Peruzzi and Bottaro, 2006) or by overexpression of HGF in CAFs, leading to increased proliferation of neoplastic cells. Furthermore, in a three-dimensional model of ductal carcinoma in situ, co-cultures with HGF-secreting fibroblasts were found to increase the invasive outgrowth by enhancing the ability of these preneoplastic cells to degrade the ECM (Jedeszko et al., 2009).
CAFs modify tumor metabolism.
Metabolic alterations are not only restricted to cancer cells; CAFs also show important metabolic changes that promote tumorigenesis. Fibroblasts are metabolically active already in their quiescent state (Lemons et al., 2010), but when transformed into CAFs they change their metabolic profile and show increased autophagy (Chaudhri et al., 2013). As an example, phosphoglycerate kinase-1 (PGK1), a part of the glycolytic pathway, is highly up-regulated in CAFs compared with normal fibroblasts. Upon overexpression of PGK1, normal fibroblasts gain a myofibroblastic phenotype, which promotes tumor cell growth when coimplanted with neoplastic cells in vivo (Wang et al., 2010).
Interestingly, CAFs have been reported to use aerobic glycolysis as a source of energy. In some tumors, CAFs express glycolytic enzymes related to the Warburg effect, such as the M2 isoform of pyruvate kinase and lactate dehydrogenase, whereas adjacent neoplastic cells do not (Pavlides et al., 2009). A switch to aerobic glycolysis in CAFs is hypothesized to generate lactate and ketones, which are secreted into the intracellular space and act as paracrine onco-metabolites that fuel oxidative mitochondrial metabolism in neoplastic cells. This phenomenon is referred to as the “reverse Warburg effect” (Pavlides et al., 2009). To further support the significance of this phenomenon, high stromal MTC4 expression (a functional marker of hypoxia, oxidative stress, aerobic glycolysis, and lactate efflux) was shown to be correlated with decreased overall survival in triple-negative breast cancer, whereas expression of MTC4 in neoplastic cells had no prognostic value (Witkiewicz et al., 2012). In ex vivo co-culture systems containing breast cancer cells and fibroblasts, glucose uptake was increased and mitochondria activity was decreased in fibroblasts and the opposite effect was observed in neoplastic cells (Martinez-Outschoorn et al., 2011). Mechanistically, neoplastic cells have been shown to secrete H2O2, which initiates an oxidative stress in the tumor stroma, switching CAFs to aerobic glycolysis (Martinez-Outschoorn et al., 2011). Furthermore, the TGF-β pathway in CAFs induces a metabolic reprogramming that promotes mitochondrial activity in adjacent neoplastic cells (Guido et al., 2012). In contrast, other tumors are characterized by the conventional Warburg phenotype in which the neoplastic cells are driven by anaerobic metabolism, and CAFs have been reported to express lactate transporters (MCT1/MCT2) while reducing the expression of glucose transporters (GLUT1; Koukourakis et al., 2006), suggesting a role of CAFs in buffering and recycling the products derived from anaerobic metabolism in neoplastic cell.
There is a great diversity in metabolic phenotype among different tumors. In an attempt to map the metabolic heterogeneity in breast cancer, tumors were classified as having Warburg type (glycolysis in neoplastic cells, nonglycolysis in stroma), reverse Warburg type (nonglycolysis in neoplastic cells, glycolysis in stroma), mixed type (glycolysis in both stroma and neoplastic cells), and null type (nonglycolysis in both stroma and neoplastic cells; Choi et al., 2013). The results indicate a correlation between different metabolic phenotypes and different tumor subtypes (Luminal A, B, triple-negative, etc.).
Collectively, CAFs participate in a dynamic metabolic interplay with the neoplastic cells and can adapt to the metabolic needs of the tumor. This is important to keep in mind when targeting metabolic pathways, and it also indicates that PET imaging may be specifically detecting glucose uptake in the tumor stroma rather than in the neoplastic cells in certain tumors.
CAFs remodel the ECM.
One characteristic feature of activated CAFs is their ability to synthesize and remodel the ECM in the desmoplastic stroma. Severe desmoplasia is correlated with poor prognosis in lung, pancreas, breast, and colorectal tumors (Cardone et al., 1997; Maeshima et al., 2002; Tsujino et al., 2007; Erkan et al., 2008; Kawase et al., 2008). Changes in the composition and cross-linking of the ECM influence the stiffness of the tissue, which has a pivotal role in tumorigenesis (Erler and Weaver, 2009; Cukierman and Bassi, 2010). By regulating the remodeling of the ECM, CAFs drive the recruitment of other cells into the tumor, promote migration, and facilitate a metastatic phenotype of neoplastic cells.
Hyaluronic acid is a major component of the ECM and CAFs contribute to its production. Apart from serving as a structural component, hyaluronic acid possesses biological functions, such as macrophage recruitment (Kobayashi et al., 2010). Furthermore, CAFs express Lysyl oxidase (LOX), an enzyme responsible for cross-linking collagen I (Pickup et al., 2013b). In breast cancer, tumorigenesis is accompanied by changes in collagen cross-linking, and reduced LOX-mediated collagen cross-linking diminished tumor tissue stiffness and decreased tumor incidence in a xenograft mouse model (Levental et al., 2009).
In contrast, CAFs also regulate the degradation of the ECM. By expressing members of the matrix metalloproteinase (MMP) family, CAFs can facilitate tumor growth, invasion, and metastasis (Poulsom et al., 1992; Stetler-Stevenson et al., 1993; Sternlicht et al., 1999; Vosseler et al., 2009; Zigrino et al., 2009). MMP-mediated ECM remodeling is essential for cancer angiogenesis, and MMP13 expressed from CAFs plays a key role in promoting angiogenesis by releasing VEGF that is bound and sequestered in the ECM (Lederle et al., 2010). In addition, MMPs stimulate protease-activated receptors (PARs) on the surface of neoplastic cells, thereby promoting growth and invasion (Boire et al., 2005). Other proteases are also involved in ECM degradation. For instance, urokinase-type plasminogen activator (uPA) activates the serine protease Plasmin and has thereby been shown to increase proliferation, migration, and invasion (Danø et al., 2005; Noskova et al., 2009). Finally, the CAF marker FAPα is a membrane-bound glycoprotein with both collagenase and dipeptidyl peptidase (DPP) activities that are important for degrading the ECM (Scanlan et al., 1994) and stimulating tumor growth (Cheng et al., 2005).
CAFs trigger tumor initiation and progression
Many studies have highlighted the importance of CAFs in initiation and progression of cancer mediated by the ability of the CAFs to alter important functions in neoplastic cells, such as cell cycle regulation, migration, and death (Shimoda et al., 2010). Interestingly, neoplastic cells of different origins differ in their responses upon stimulation from CAFs (Kadaba et al., 2013), illustrating a unique relationship with CAFs across tumor types.
By using in vitro co-culture and in vivo transplantation experiments, Olumi et al. (1999) showed that human prostatic CAFs induced the proliferation and the ability to initiate tumors from immortalized nontumorigenic human prostatic epithelial cells. This effect was not manifested by normal fibroblasts and CAFs did not affect growth of normal human prostatic epithelial cells under identical conditions (Olumi et al., 1999). In a similar study, senescent human fibroblasts were shown to stimulate premalignant and malignant, but not normal, epithelial cells to proliferate in culture and develop tumors when engrafted in mice (Krtolica et al., 2001). This elegantly demonstrates how fibroblasts can initiate tumor formation in premalignant cells that have not acquired sufficient genetic alterations for complete transformation. Interestingly, when regrafted into secondary mice in the absence of CAFs, the epithelial cells sustain their tumorigenic potential, showing that the CAF-mediated transformation of epithelial cells is long-lasting (Hayward et al., 2001).
Secreted factors from CAFs are believed to be responsible for this tumor-initiating potential. Although TGF-β signaling helps maintain the CAF phenotype, ablating TGFBR in fibroblasts resulted in spontaneous neoplasia in the prostate, illustrating a tumor-suppressive function of TGF-β signaling in early tumor development (Bhowmick et al., 2004). Notably, HGF can compensate for TGF-β loss, making HGF a candidate for mediating the tumor-initiating effect of CAFs. Indeed, overexpression of HGF in fibroblasts induced hyperproliferation of normal epithelium in a xenograft model (Kuperwasser et al., 2004), which further supports an initiating role of HGF. In addition to tumor initiation, CAFs also participate in tumor maintenance and progression. For example, co-implantation of breast cancer cells with CAFs was shown to increase xenograft tumor growth (Orimo et al., 2005).
Further evidence for the role of CAFs in tumor progression comes from studies in which activated CAFs were inactivated or in which key proteins were reduced in CAFs through genetic ablation. Activated stellate cells in pancreatic cancer could be driven back into a quiescent state by retinoic acid, resulting in reduced paracrine cross talk, such as Wnt/β-catenin signaling. In a three-dimensional co-culture system, these quiescent stellate cells slowed tumor progression by reducing neoplastic cell proliferation and migration (Froeling et al., 2011). Mice deficient for the CAF marker FSP-1 also showed reduced engraftment of neoplastic cells and delayed tumor growth (Grum-Schwensen et al., 2005).
CAFs regulate cancer stemness
There is accumulating evidence for the acquisition of stem-like plasticity in a subset of the cancer cells, usually referred to as cancer stem cells (CSCs). Inflammatory mediators and cytokines are the most common cues reported to induce stemness of neoplastic cells. Many factors secreted by CAFs, such as IL-6, IL-17A, CXCL7, PGE2, and HGF, were shown to trigger the Wnt–β-catenin pathway in neoplastic cells and augment the CSC population (Giannoni et al., 2010, 2011; Vermeulen et al., 2010; Liu et al., 2011; Li et al., 2012a; Malanchi et al., 2012; Lotti et al., 2013). CD44, a prominent CSC marker and receptor for hyaluronic acid, is up-regulated in breast, prostate, and colorectal cancers by different cytokines produced by CAFs and contributes to maintaining CSC self-renewal features and general stemness capacity (Giannoni et al., 2010; Liu et al., 2011; Lotti et al., 2013). Interestingly, CD44 is also expressed on CAFs, where it is indispensable for the existence of the neighboring CSC population. In response to hypoxia or reduced nutrient conditions, CAFs elevate CD44 and maintain stem cell properties of neoplastic cells (Kinugasa et al., 2014).
CAFs also induce expression of other CSC markers, such as ALDH1 and Nestin, in many tumor types (Liu et al., 2011; Hamada et al., 2012; Matsuda et al., 2012). Expression of these stem cell markers and the elevation of the CSC population are correlated with aggressive tumors, which exhibit enhanced invasiveness and metastatic capacities (Giannoni et al., 2011; Li et al., 2012a; Malanchi et al., 2012). Together, these data show that CAFs maintain stemness in neoplastic cells to support further tumor progression.
CAFs modulate the immune response
An inflammatory environment is known to promote error-prone, high-rate proliferation, thereby facilitating tumorigenesis (Grivennikov et al., 2010). Indeed, chronic inflammation is a prominent risk factor for many cancers, including hepatocellular carcinoma, gastric cancer, and pancreatic ductal adenocarcinoma (Pikarsky et al., 2004; Peek and Crabtree, 2006; Guerra et al., 2007). CAFs mediate tumor-enhancing inflammation by expressing a proinflammatory gene signature, which creates a microenvironment that attracts myeloid cells and supports tumor growth and angiogenesis (Erez et al., 2010; Torres et al., 2013). This signature, identified early in dysplastic lesions and maintained throughout tumorigenesis, is mediated via NF-κB-dependent signaling and initiated by IL-1β in skin cancer. Most importantly, normal fibroblasts can be induced by carcinoma cells to turn on this proinflammatory gene signature (Erez et al., 2010). A similar NF-κB–dependent inflammatory signature was activated by CAFs to support prostate cancer stemness and invasion (Giannoni et al., 2011).
Cyclooxygenase 2 (COX2), an NF-κB target involved in mediating inflammation and a part of the proinflammatory gene signature, is expressed by CAFs and neoplastic cells (Nakagawa et al., 2004; Erez et al., 2010), and has been shown to function as a mediator of tumor progression. Indeed, the implantation of lung carcinoma cells in COX2-deficient mice or treatment with COX2 inhibitors reduced tumor growth and vascular density (Williams et al., 2000). In a xenograft model of ductal carcinoma in situ, fibroblasts were shown to induce the expression of COX2 in neoplastic cells, affecting tumor growth and progression. As a consequence of increased COX2, MMP14 and VEGF expression were increased, causing a more invasive phenotype. Administration of a selective COX2 inhibitor, Celecoxib, impeded this invasion (Hu et al., 2009). Likewise, in vitro coculturing of pancreatic cancer cells with CAFs increased expression of COX2, and a selective COX2 inhibitor abrogated migration of these cells (Sato et al., 2004).
Genetically altered neoplastic cells often generate neoantigens that can potentially be recognized and destroyed by the immune system. However, most tumors evade immune surveillance despite the abundance of an inflammatory milieu. Accumulating evidence shows that the tumor stroma and CAFs actively participate in modulating the immune response to help neoplastic cells escape detection, thereby supporting tumor progression (Singh et al., 1992; Liao et al., 2009; Iijima et al., 2011). CAFs have been shown to protect pancreatic tumors and lung carcinoma cells from the cytotoxic effect of T cells via different mechanisms. FAPα-positive CAFs were shown to produce CXCL12, which mediated the exclusion of T cells from neoplastic cells (Feig et al., 2013). CAFs also opposed the TNF- and IFN-γ–mediated necrosis of neoplastic cells by T cells (Kraman et al., 2010). Depletion of FAPα-positive cells restored immunological detection and destruction of the tumor, indicating that FAPα-positive cells are immune-suppressive cells in the tumor microenvironment (Kraman et al., 2010; Feig et al., 2013). Additionally, pancreatic stellate cells induce the differentiation of peripheral blood mononuclear cells into immune-suppressive myeloid-derived suppressor cells, contributing to T cell inhibition (Mace et al., 2013). Finally, CAFs derived from hepatocellular carcinoma impair NK cell cytotoxic activity by reducing cytotoxic receptors on their cell surface and interfering with their cytokine production (Li et al., 2012b). This was mediated through the secretion of prostaglandin E2 (PGE2) from CAFs, which also interfered with NK cell functions in melanoma (Balsamo et al., 2009). In summary, CAFs possess the ability to manipulate the immune system, both by excluding and opposing T and NK cell functions and by maintaining an aberrant inflammatory pro-tumorigenic environment.
CAFs promote cancer cell migration and metastasis
Neoplastic cell metastasis leads to the demise of most patients, and CAFs participate in this process. Neoplastic cells undergo epigenetic and genetic changes resulting in a metastatic phenotype, and CAFs coevolve with the neoplastic cells during tumor progression by acquiring a proinflammatory gene expression pattern (Saadi et al., 2010). Furthermore, gene signatures characterizing active CAFs are often correlated with poor clinical outcomes (Herrera et al., 2013).
The close proximity between neoplastic cells and CAFs yields an effective cross talk, which ultimately supports invasion and metastasis. TGF-β response in CAFs led to secretion of IL-11, which in turn can induce GP130/STAT3 signaling in neoplastic cells to support tumor initiation and accelerate metastasis (Calon et al., 2012). Breast cancer cells also create a paracrine loop by reprogramming their surrounding MSCs into CAFs that secrete CCL5. The cancer cells then responded to CCL5 through the CCR5 receptor, resulting in augmented metastatic capacity (Karnoub et al., 2007). The noncanonical Wnt–planar cell polarity (PCP) pathway also promotes the dissemination of breast cancer to distant sites in the body. The PCP pathway controls convergent-extension movements during embryogenesis and regulates cell motility by changing cell morphology and inducing protrusions. Interestingly, exosomes secreted from CAFs triggered Wnt-11 autocrine induction of the PCP pathway in neoplastic cells, enhancing breast cancer metastatic potential (Luga et al., 2012).
Another important consequence of CAF-mediated signaling on neoplastic cells is EMT, which is considered a critical process in the extravasation of tumors (Guarino et al., 2007). For example, pancreatic stellate cells in pancreatic tumors were shown to trigger EMT in co-cultured neoplastic cells, correlating with increased metastasis (Kikuta et al., 2010). Notch and COX2/NF-κB signaling have also been shown to be involved in acquiring and maintaining the EMT phenotype (Wang et al., 2009b; Li et al., 2012a). Indeed, CAF-secreted MMPs triggered the COX2–NF-κB cascade in prostate cancer cells to promote ROS accumulation and prostate cancer invasion (Giannoni et al., 2011).
Interestingly, CAFs can promote metastasis in the absence of EMT. CAFs use Rho-dependent signaling pathways to create force-dependent movements by which they migrate and form tracks in the matrix for the neighboring neoplastic cells to follow (Gaggioli et al., 2007; Goetz et al., 2011; Sanz-Moreno et al., 2011). Rho-dependent cytoskeletal remodeling in CAFs was shown to be activated by Palladin, Cav-1, or JAK signaling cascades, and led to Actomyosin contractility and enhanced invasion (Hooper et al., 2010; Goetz et al., 2011; Sanz-Moreno et al., 2011; Brentnall et al., 2012). Mesenchymal-derived Cav-1 also conferred microenvironment remodeling to favor the migration of neoplastic cells. CAFs further facilitated intra- and extravasation and were shown to accompany neoplastic cells to their metastatic site (Duda et al., 2010; Xu et al., 2010). Clusters of cells composed of neoplastic cells and fibroblasts have been shown to be more viable than single neoplastic cells in the blood stream and have a survival advantage when seeding in metastatic sites (Duda et al., 2010). By these means, neoplastic cells can sustain their epithelial features while relying on CAFs for invasion.
CAFs have also been reported to increase the rate of successful colonization by selecting for neoplastic clones bearing a specific metastatic advantage while still residing in the primary lesion. This effect is mediated through the secretion of CXCL12 and IGF (Zhang et al., 2013b). Successful colonization has also been shown to be dependent on proangiogenic factors secreted from FSP-1–positive cells (O’Connell et al., 2011).
CAFs alter therapeutic responses
The protumorigenic effects of CAFs can also promote therapeutic resistance. Evidence for the clinical relevance of CAFs came from a study by Farmer et al. (2009), who found that breast cancer patients responded poorly to neoadjuvant chemotherapy if their tumors had increased expression of stromal genes. The stroma can interfere with therapeutic agents by two major mechanisms. First, it can simply function as an interstitial barrier that prevents efficient drug delivery (Jain, 1990). The second mechanism involves the activation of signaling pathways that change the therapeutic outcome, driving the neoplastic cell to a more drug-resistant phenotype.
Conversely, a limited number of studies report that CAFs can also increase the anti-neoplastic potency of certain drugs. The mechanism for this unexpected sensitization may include the alteration of signaling pathways in neoplastic cells that are induced by CAFs (McMillin et al., 2013). Although we will not discuss this topic further, it highlights the need to consider the tumor microenvironment during therapeutic development.
Environment-mediated drug resistance.
Although acquired drug resistance of neoplastic cells is considered to be a cell autonomous process that leads to adaptive biochemical, epigenetic, or genetic changes, the microenvironment can also participate in this process by providing extrinsic cues that promote cell survival and thereby impede drug toxicity. The impact of the tumor microenvironment on drug resistance was shown previously when mammary cancer cells that were refractory in vivo to cytotoxic drugs became sensitive upon transfer to an in vitro setting where the microenvironment was excluded (Teicher et al., 1990). The importance of the “soil” was further demonstrated in an experiment where colon carcinoma cells were injected at different sites, and showed varying responses to chemotherapy merely based on their location (Fidler et al., 1994). Compared with cell autonomous drug resistance, which develops over a long period of time, environment-mediated resistance can develop rapidly. Thus, environment-mediated resistance may protect neoplastic cells from apoptosis while they acquire the mutations needed for cell-intrinsic protection of chemotherapy (Meads et al., 2009).
Environment-mediated drug resistance can be further categorized into two major groups: soluble factor–mediated drug resistance and cell adhesion–mediated drug resistance (Meads et al., 2009). Soluble factor-mediated drug resistance is induced by cytokines and growth factors secreted from CAFs and other cell types in the stroma. By binding to neoplastic cell receptors, these factors cause transcriptional changes and also activate nontranscriptional mechanisms including degradation or redistribution of activators of apoptosis, and increased stability of suppressors of apoptosis and cell cycle regulators. Resistance due to secreted factors from stromal cells is common, particularly to targeted agents (Straussman et al., 2012). Many cancers have been shown to harbor driving mutations in receptor tyrosine kinase (RTK) pathways, constitutively activating these pathways and making the neoplastic cell “kinase-addicted.” Inhibiting these pathways has shown promising results in vitro but many times failed in vivo, where neoplastic cells soon develop resistance to such drugs. Wilson et al. (2012) made it clear that because of redundancy and overlap in many RTK signaling pathways, otherwise kinase-addicted neoplastic cells that respond to certain RTK inhibitors can be rescued from drug sensitivity simply by adding one or more RTK ligands. As CAFs are a major source of secreted RTK ligands, this gives a mechanistic explanation to how CAFs mediate resistance toward targeted therapy. Additional evidence was provided by Wang et al. (2009a), who showed that CAFs recruited to lung tumors induced resistance to tyrosine kinase inhibitors against the EGF receptor (EGFR-TKIs). Interestingly, if HGF was inhibited, the resistance to EGFR-TKIs was eliminated, both in vivo and in vitro. This shows the striking impact that a single CAF-secreted growth factor can have on drug resistance.
Moreover, CAFs also play a role in targeted anti-angiogenesis treatments. Crawford et al. (2009) found that the expression of PDGF is up-regulated in CAFs from tumors that are resistant to anti-VEGF therapy and that a PDGF-neutralizing antibody impaired the observed anti-VEGF resistance, suggesting a crucial role for CAFs in mediating resistance to anti-angiogenesis therapy.
Soluble factor-mediated drug resistance is also directed against conventional chemotherapies. The CXCL12–CXCR4 signaling axis has been shown to mediate chemotherapy resistance (Singh et al., 2010; Domanska et al., 2012), and furthermore, pancreatic stellate cells drive resistance to chemotherapy-induced apoptosis and radiation-induced apoptosis via a mechanism involving activation of the AKT pathway (Hwang et al., 2008). As mentioned earlier, CAFs also secrete factors that stimulate neoplastic cells to undergo EMT and this process has also been shown to augment resistance to chemotherapy (Wang et al., 2009b).
Cell adhesion–mediated drug resistance occurs when neoplastic cells either adhere to the ECM or make direct cell-to-cell contact with stromal cells. Early observations revealed enhanced tumorigenicity and drug resistance when small cell lung cancer (SCLC) cells were grown on a basement membrane (Fridman et al., 1990). Furthermore, if the integrin-mediated contact with the ECM was blocked, the tumor load decreased in vivo (Fridman et al., 1990). Adhesion of SCLC cells to the ECM was later shown to enhance tumorigenicity and confer resistance to chemotherapeutic agents as a result of β1 integrin–stimulated tyrosine kinase activation, suppressing chemotherapy-induced apoptosis (Sethi et al., 1999). These results provide a mechanistic explanation behind cell adhesion–mediated drug resistance. Similar effects have been reported in ovarian cancer (Sherman-Baust et al., 2003) and pancreatic ductal adenocarcinoma cells (Miyamoto et al., 2004). Furthermore, resistance to radiotherapy can also be induced by cell adhesion, and β1-integrin–mediated adhesion to fibronectin and collagens has been shown to be essential for cell survival after radiation-induced injury (Cordes et al., 2006).
Finally, cell adhesion can mediate resistance to targeted therapies using the same principles as described for soluble factor–mediated resistance. For example, PI3K/mTOR inhibitors caused cell death in matrix-deprived ovarian cancer spheroids, whereas matrix-attached cells were resistant (Muranen et al., 2012).
Therapy-induced responses in CAFs.
Cancer therapies target all cells in vivo, including CAFs, which have been shown to undergo a DNA damage response that paradoxically results in the secretion of proteins that drive tumorigenesis. For example, after exposure to therapeutic agents, CAFs activate canonical Wnt signaling in prostate cancer cells, promoting cancer cell survival and disease progression (Sun et al., 2012). Moreover, when breast cancer cells were injected into the irradiated fat pads of mice, increased neoplastic potential was observed compared with the same cells injected into nonirradiated fat pads (Barcellos-Hoff and Ravani, 2000). Along these lines, irradiated fibroblasts increased invasiveness in pancreatic cancer cells, an effect which could be inhibited with an HGF antagonist (Ohuchida et al., 2004). In addition, Lotti et al. (2013) compared colorectal tumors before and after cytotoxic treatment and found more CAFs in the posttreated tissue. These chemotherapy-treated CAFs, when isolated and co-cultured with CSCs, increased self-renewal, chemoresistance, and tumor growth of CSCs via IL-17A secretion. Collectively, these data illustrate how CAFs can gain new features upon exposure to chemo- or radiotherapy, which not only enables them to reverse or attenuate the effect of anti-cancer drugs but also contributes to a more aggressive cancer phenotype (Barcellos-Hoff et al., 2005).
Targeting the CAF-induced protumorigenic effects
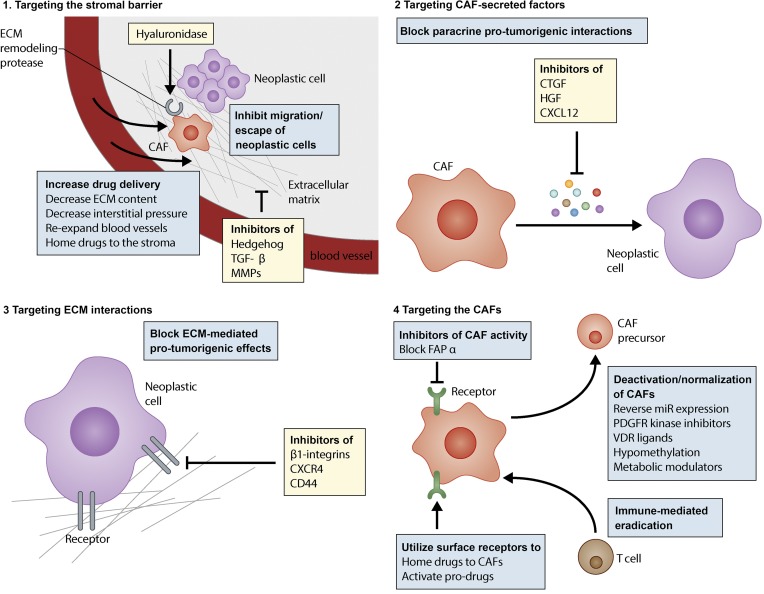
The broad range of mechanisms used by CAFs to stimulate tumorigenesis and drug resistance (Fig. 2) provides multiple avenues to pursue therapeutic development. Indeed, four general strategies have been suggested to target CAFs and thereby achieve therapeutic benefits: (1) targeting the biophysical stromal barrier to increase drug delivery; (2) sequestering or inhibiting CAF-secreted factors that stimulate neoplastic cell behavior and drug resistance; (3) depleting or blocking the ECM components to reduce adhesion-mediated signaling; and (4) targeting the CAFs themselves to disable their downstream effects (Fig. 3).
Figure 3.
Principle strategies for targeting CAF-induced pro-tumorigenic effects. Presented are four general approaches to control and diminish CAFs and their activity toward tumorigenesis and drug resistance. Examples of targets that have been hypothesized and/or empirically tested are indicated.
Many informative experiments testing these strategies have been performed in combination with conventional chemotherapeutic or targeted drugs. The following section will briefly summarize some of the experiments that have provided additional insights to CAF/ECM targeting.
1. Targeting the stromal barrier.
The tumor stroma can be considered a barrier that needs to be lowered so that drugs can be optimally delivered. A variety of strategies have been tested to increase drug delivery by overcoming the stromal barrier. Targeting the production of the ECM or degrading the ECM are both feasible strategies to loosen the stroma, resulting in a change in the interstitial pressure of the tumor and the consequent reexpansion of blood vessels. Hyaluronic acid, TGF-β, and the Hedgehog pathway have all been tested as targets in this context.
High interstitial fluid pressure is evident in solid tumors, especially those rich in ECM, resulting in vascular collapse and effectively limiting perfusion and diffusion (Provenzano et al., 2012). Hyaluronic acid compresses vessels in collagen-rich tumors, and both collagen and hyaluronic acid are critical targets for decompressing tumor vessels. Enzymatic degradation of hyaluronic acid using hyaluronidase normalized the interstitial fluid pressure and expanded the microvasculature, leading to increased intratumoral delivery of chemotherapeutic agents (Provenzano et al., 2012; Jacobetz et al., 2013). Accordingly, the combination of hyaluronidase and conventional chemotherapy inhibited tumor growth and prolonged survival relative to monotherapy in mouse models of pancreatic cancer (Provenzano et al., 2012; Jacobetz et al., 2013). This concept is now being tested in clinical trials.
Inhibitors of TGF-β were shown to decrease collagen I content and increase the fraction of perfused vessels in a mouse breast cancer orthotopic model, leading to preclinical benefit. Furthermore, the normalization of the tumor stroma improved intratumoral delivery of conventional chemotherapeutic drugs, leading to better drug response (Liu et al., 2012). TGF-β inhibitors are also capable of inhibiting cancer progression in animal models (Akhurst and Hata, 2012), but this pathway is highly context-dependent and complicated to target. Indeed, TGF-β signaling exhibits a seemingly biphasic action during tumorigenesis, being tumor-suppressive early in tumorigenesis and becoming tumor-promoting in later stages. Indirectly targeting MMPs by inhibiting the TGF-β pathway is an alternative mechanism by which the stromal barrier may be attenuated. Low doses of the TGF-type I receptor inhibitor have been shown to increase the delivery of anti-cancer nanocarriers, thereby potentiating their tumor-inhibitory effect without altering either TGF signaling in neoplastic cells or the amount of fibrosis (Kano et al., 2007). Given that TGF-β and MMP14 are both involved in a pathway that regulates vessel stability, inhibiting this pathway may increase delivery efficacy by increasing perfusion of the tumor (Sounni et al., 2010).
Angiotensin receptor blockers (ARBs) were originally developed for the treatment of hypertension but also inhibit TGF-β signaling (Diop-Frimpong et al., 2011), although the exact mechanism for this is unclear. Nevertheless, the Angiotensin signaling pathway is activated in stellate cells and contributes to the desmoplastic reaction (Sakurai et al., 2011). ARBs have been shown to inhibit the production of collagen I by CAFs (Diop-Frimpong et al., 2011), and in a subcutaneous xenograft mouse model, ARB reduced expression of α-SMA in the tumor, resulting in reduced ECM and tumor inhibition (Masamune et al., 2013). By reducing collagen and hyaluronic acid production, ARBs can increase vascular perfusion and drug delivery (Chauhan et al., 2013). A retrospective study further suggested the role of the Angiotensin pathway in cancer by showing that pancreatic cancer patients that underwent gemcitabine monotherapy and at the same time received hypertension treatment with ARB had a significantly better survival than patients without ARB treatment (Nakai et al., 2010).
Hedgehog (Hh) signaling mediates tumorigenesis in many types of cancer (Thayer et al., 2003; Bailey et al., 2009). Interestingly, despite ligand production in neoplastic cells, Hh signaling is not activated in these cells. Instead, CAFs have been demonstrated to respond to Hh stimulation by increasing the production of ECM (Yauch et al., 2008), indirectly supporting tumor growth. An inhibitor of Hh signaling, IPI-926, resulted in stromal depletion in a mouse model of pancreatic cancer. In combination with gemcitabine, IPI-926 increased the intratumoral vascular density, perfusion, and intratumoral concentration of chemotherapy, correlating with transient growth inhibition (Olive et al., 2009). Importantly, this study and the aforementioned studies targeting hyaluronan showed that by depleting the stroma barrier, drug delivery is increased, resulting in transiently improved survival. Although the combination of IPI-926 and chemotherapy was promising in a Phase I trial, this approach failed in a randomized phase II clinical trial. To address these conflicting data, a follow-up study was recently conducted, where Hh was genetically ablated in the epithelial compartment of a pancreatic cancer mouse model. Interestingly, despite a decreased number of stromal cells and an increased vascularization, these tumors were more aggressive and tended to be much less differentiated, subsequently leading to reduced survival of these mice (Rhim et al., 2014). Similar results were obtained in another study, where depletion of cancer-associated myofibroblasts in a pancreatic cancer model led to more aggressive and less differentiated tumors (Özdemir et al., 2014). Thus, the protective role of certain stromal elements should be kept in mind, although further interrogation of this phenomenon in other settings is required to evaluate the physiological role of the stroma in restraining cancer.
MMP inhibitors are another example that illustrates the complexity of the tumor stroma. These inhibitors were developed to block the degradation of the ECM, a process which was predicted to facilitate tumor progression. Early preclinical studies with MMP inhibitors were promising; however, randomized clinical trials were not positive (Dufour and Overall, 2013). An explanation for this may lie in the fact that MMPs have many different substrates, and besides ECM structures, they also affect chemokines and cell surface receptors that might have tumor suppressive effects (Dufour and Overall, 2013). Unfortunately, side effects limited the dosing of the MMP inhibitor, and therefore the results of this trial may be misleading.
It is also possible to use the tumor ECM as a homing signal for drugs, limiting reactivity to normal tissues. By conjugating drugs to antibodies or small molecules that recognize stromal epitopes, drugs can be accumulated in the tumor, limiting the area of cytotoxicity. For instance, the plasminogen activator inhibitor type 2 (PAI2) has high affinity to plasminogen activator (uPA), which is highly expressed in the stroma of pancreatic cancer. By conjugating a radioisotope onto PAI2, radioactivity was concentrated in the tumor and caused complete inhibition of tumor growth in a xenograft model (Qu et al., 2005). Additionally, nAb-Paclitaxel, an albumin-formulated Paclitaxel, was hypothesized to bind to the matricellular protein Osteonectin/SPARC that is present in many tumor types and thereby cause stromal depletion. This hypothesis was supported by data from patient-derived pancreatic cancer xenografts that demonstrated stromal loss after treatment (Von Hoff et al., 2011), and from resected specimens of patients who were treated with nAb-Paclitaxel and gemcitabine that demonstrated loss of neoplastic cells and a deficient stroma (Alvarez et al., 2013). However, direct experiments in genetic mouse models did not corroborate stromal loss as the primary mode of action for nAb-paclitaxel but rather implicated drug–drug interactions leading to increased neoplastic cell death as an important aspect of its activity (Frese et al., 2012). Furthermore, mice harboring pancreatic tumors and lacking SPARC responded to nAb-Paclitaxel in an indistinguishable manner compared with mice that expressed SPARC (Neesse et al., 2014). To reconcile these seemingly contradictory findings, it is logical that the loss of neoplastic cells will lead to secondary decreases in stromal abundance.
2. Targeting CAF-secreted factors.
CAFs secrete a variety of mitogens, chemokines, and matricellular proteins that promote tumor progression and drug resistance. Neesse et al. (2013) showed that targeting the stroma in a mouse pancreatic cancer model with a CTGF antibody yielded a synergistic effect with gemcitabine without increasing the intratumoral gemcitabine concentration. Mechanistic analysis revealed that CTGF deregulates the expression of the apoptosis modulating protein XIAP, highlighting the impact that secreted factors from CAFs have on neoplastic cells in terms of response to therapy. This modality is currently undergoing clinical investigation.
The HGF–Met pathway has been interrogated in many preclinical studies, either as monotherapy or in combination with other drugs. For example, a competitive antagonist of c-Met (NK4) has been shown to reduce liver metastasis and prolong survival in a mouse model of colon cancer (Wen et al., 2004). Furthermore, stromal fibroblast-secreted HGF is involved in mediating therapy resistance in melanoma. BRAF mutant melanomas are highly dependent on constitutive BRAF kinase activity, and inhibition of BRAF improves survival in patients (Bollag et al., 2010; Flaherty et al., 2010; Chapman et al., 2011; Sosman et al., 2012). However, CAF-derived HGF and subsequent activation of the HGF receptor c-Met have been shown to mediate resistance to targeted RAF inhibition. Interestingly, targeting both RAF and c-Met reversed the observed resistance (Straussman et al., 2012), illustrating how microenvironment-derived mediators of drug resistance can serve as promising targets to overcome the resistance problem with targeted therapies seen in the clinic.
The CXCR4 antagonist AMD3100 was shown to chemosensitize prostate cancer cells to the chemotherapeutic agent docetaxel in a synergistic manner (Domanska et al., 2012). As discussed previously, CXCL12 secreted from FAPα-positive cells was shown to be important for immune suppression in pancreatic cancer, providing a conceivable explanation as to why immunological checkpoint antagonists, such as anti-PDL1, have failed in pancreatic cancer (Royal et al., 2010). Notably, in a mouse model of pancreas cancer, CXCR4 inhibition promoted T cell accumulation in the tumor site and synergized potently with anti-PDL1 (Feig et al., 2013).
3. Targeting ECM interactions.
Neoplastic cells interact with the ECM using a variety of cell surface receptors, of which integrins are the most studied. In a three-dimensional culture system of breast cancer, a β1-integrin inhibitor induced apoptosis and inhibited growth of breast cancer cells, highlighting the therapeutic potential of blocking integrin interactions with the ECM (Park et al., 2006). Furthermore, β1-integrin inhibitors synergized with radiation therapy to increase apoptosis and inhibit tumor growth in a mouse xenograft model (Park et al., 2008). Integrin antagonists have therefore been tested in clinical trials (Mullamitha et al., 2007; Reardon et al., 2008), and although they were well tolerated, clinical benefits have not yet been demonstrated. CD44 expressed by neoplastic cells allows an additional interacting point with the ECM. It binds to collagen and hyaluronic acid, and certain isoforms of CD44 provide survival signals in neoplastic cells (Bourguignon et al., 2003; Götte and Yip, 2006). Abrogating CD44–ECM interactions has been shown to inhibit tumor growth in xenograft models (Ahrens et al., 2001); however, this awaits clinical confirmation.
Soluble factors secreted from CAFs can also indirectly regulate adhesion of neoplastic cells. For example, CXCL12-induced integrin activation was found to increase adhesion of SCLC cells to fibronectin and collagen and thereby protects SCLC cells from chemotherapy-induced apoptosis (Hartmann et al., 2005).
4. Targeting the CAFs.
Normalization of CAF behavior to change their properties to a more “non-myofibroblastic” phenotype can be achieved by multiple mechanisms. One way is by targeting epigenetic changes unique for CAFs. Many groups have recently shown that therapies aimed at reconstituting miR expression might be a successful strategy to deactivate CAFs (Musumeci et al., 2011; Bronisz et al., 2012; Mitra et al., 2012; Aprelikova et al., 2013). Inhibition of PDGF signaling, an important pathway in the activation of CAFs, can reverse CAFs to normal fibroblasts (Haubeiss et al., 2010). Using a clinically approved PDGFR kinase inhibitor (Imatinib) in a mouse model of cervical carcinogenesis, tumor proliferation was reduced and angiogenesis was inhibited. Furthermore, the progression of premalignant cervical lesions was attenuated and the growth of preexisting invasive carcinomas was impaired (Pietras et al., 2008). Because CAFs undergo changes in their metabolic activity, normalization of the metabolic phenotype and inhibition of metabolic pathways have also been suggested as a plausible way to target tumors (Witkiewicz et al., 2012; Doherty and Cleveland, 2013).
Another approach to target the CAFs would be to dedifferentiate them into a quiescent state. Hepatic stellate cells play a crucial role in liver fibrosis and in the desmoplastic reaction in liver cancer and are known to express several nuclear hormone receptors including the vitamin D receptor (VDR). Ding et al. (2013) demonstrated that VDR ligands promoted the dedifferentiation of stellate cells and abrogated fibrosis, stressing the potential use of VDR ligands to target CAFs. Taking advantage of existing epigenetic changes has also been suggested as a means to induce CAF arrest. Treatment of CAFs with hypomethylating drugs is hypothesized to result in a “hypomethylation crisis” by causing further demethylation in the already hypomethylated CAF genomes (Gonda et al., 2010), resulting in growth arrest.
Finally, FAPα has been proposed as a potential therapeutic target (Brennen et al., 2012). This serine protease is expressed on most CAFs. Blocking FAPα was found to inhibit tumor growth, and to decrease myofibroblast content and blood vessel density in lung and colon tumors (Santos et al., 2009). Furthermore, a phase I trial showed that FAPα can be targeted without apparent side effects (Scott et al., 2003). However, no significant efficacy was shown for the treatment of metastatic colorectal cancer (Hofheinz et al., 2003).
FAPα can also be used to deliver cytotoxic drugs to the CAFs. An anti-FAPα antibody conjugated to an anti-mitotic agent induced long-lasting inhibition of tumor growth in xenograft models (Ostermann et al., 2008). Investigators have also used the proteolytic activity of FAPα to target CAFs. By delivering an inert pro-drug that contains the FAPα cleavage site, FAPα-positive cells in the tumor stroma can cleave and activate the drug, a method which has been tested both in vitro (Huang et al., 2011) and in xenograft models (LeBeau et al., 2009), resulting in a significant growth inhibition.
In addition, FAPα is a target selected for immunotherapy experiments. Cancer mouse models have been immunized against FAPα-positive cells, resulting in tumor growth inhibition (Lee et al., 2005). Also, an oral DNA vaccine directed against FAPα-positive cells caused CD8+ T cell–mediated killing of CAFs and suppression of primary tumor growth and metastasis, accompanied by a greater intratumoral uptake of chemotherapeutic drugs and improved drug response (Loeffler et al., 2006). In spite of the successful preclinical results, no FAPα-directed agents are currently in clinical practice (Brennen et al., 2012).
Concluding remarks
Based on the body of evidence now available, it is clear that the tumor microenvironment is involved in all stages of tumorigenesis, shaping how neoplastic cells respond to targeted therapies, chemotherapies, or radiotherapy. Thus, the tumor microenvironment has significant impact on clinical outcome. Unfortunately, preclinical drug testing has been largely restricted to two dimensional cell culture systems or subcutaneous xenograft murine models, without fully incorporating a relevant tumor microenvironment. This lack of tumor stroma in cancer models may reflect the lack of efficacy seen in later clinical trials of many drugs. Therefore, it is of high priority to transfer preclinical drug development to platforms that take stromal interactions into account.
CAFs are tempting drug targets for many reasons. They are genetically more stable then neoplastic cells, making them less prone to develop resistance phenotypes as a result of high mutation rates and clonal selection. Additionally, CAFs show epigenetic changes that distinguish them from normal stromal cells, and furthermore, the composition of the cancer-associated stroma is distinct from normal stroma. This presents opportunities to find unique drug targets that do not affect normal physiology. In addition, CAFs in some cases cause sensitization to certain drugs, giving a rationale for the use of inhibitors against pathways that are activated by CAFs in neoplastic cells. Moreover, CAFs have the potential to activate pathways that mediate resistance to targeted anti-neoplastic agents, and resistance may be avoided if CAF-derived stimuli are neutralized. Finally, CAFs accompany and support neoplastic cells during the whole spectrum of the disease, from preinvasive lesions all the way to the metastatic site. By targeting CAFs, different stages of the disease and also many different pathophysiological processes may become treatable, including angiogenesis, EMT, and immune evasion.
Developing combinatorial therapies that target both the CAFs and the neoplastic cells holds promise for synergistic effects. If neoplastic cells are dependent on a certain input from the CAFs, it is reasonable to assume that depleting this input would make the neoplastic cells more vulnerable and less resistant to a second line of treatment with conventional therapies. Rationale supporting this hypothesis was provided by a study where pretreatment with drugs targeting oncogenic signaling pathways sensitized breast carcinoma cells to conventional chemotherapy (Lee et al., 2012). In addition, some conventional therapies potentiate the pro-tumorigenic effects of CAFs, conferring an even more aggressive cancer phenotype. This effect may be avoided if the CAFs were targeted first. Finally, drug delivery in a second round of therapy would be improved in the absence of CAFs, the major constituent of the stroma barrier.
CAFs represent a very heterogeneous population of cells, and each subpopulation might have different pathophysiological functions. Some CAFs might also have tumor-suppressive roles by preventing neoplastic cell proliferation or migration. It is in no way excluded that certain CAFs, and also other components within the tumor-associated stroma, are induced as a result of a host-driven response to the neoplastic cells. In fact, cancer progression in vivo is a relatively slow process compared with what is observed in vitro. Autopsy studies show that many preneoplastic lesions, despite harboring dominant genetic alterations sufficient to promote tumorigenesis, remain dormant. Emerging data further reinforce this idea of CAFs as a double-edged sword in tumorigenesis by demonstrating that ablation of a single cue from epithelial cells to stromal cells (Rhim et al., 2014), or depletion of the entire myofibroblastic population (Özdemir et al., 2014), accelerates pancreatic cancer. These studies question the general dogma of the field and illustrate how components in the microenvironment actually inhibit cancer progression. These findings further enlighten the complex nature of the tumor stroma; however, the implications of these findings are yet to be determined in a broader perspective. Also, it is important to keep in mind that rapidly developing tumors in murine cancer models driven by one or a few defined mutations might not fully recapitulate the complexity of the tumor microenvironment seen in human tumors. This provides a probable explanation as to why some approaches resulting in a global depletion of the tumor-associated stroma can show promising results in mouse models but cause increased tumor growth when applied to patients. It also raises the idea that the targets within the stroma must be specific and cannot cause a general and unselective depletion of the stroma or the CAFs. Another pitfall is that researchers often study a specific subpopulation of CAFs, based on one or a few expressed markers, but interpret the data as true for all populations of CAFs. The term “cancer-associated fibroblast” is therefore somewhat misleading, as it groups cells of different origin merely based on their location despite their heterogeneity and diverse roles in tumorigenesis. It is important to keep in mind that the only feature that unites the CAFs are their ability to alter the microenvironment and the behavior of neoplastic cells, but this can result in either a pro- or anti-tumorigenic effect. Efforts must therefore be put into resolving the complexity of the tumor stroma and understanding the unique roles of the different subpopulations of CAFs.
Traditionally, cancer is viewed as a result of clonal expansion, where neoplastic cells constantly undergo selection and the clones that constitute late-stage tumors are the ones most fit to avoid the host response and given therapies. However, when an initiating preneoplastic cell emerges, it does so in the context of its microenvironment, which then coevolves during the whole process of tumorigenesis such that both entities develop a symbiotic relationship that promotes tumor growth. Thus, what is seen in patients is a selected population of CAFs and neoplastic cells that collectively survives and thrives. It is vital for a neoplastic cell to achieve the ability to reprogram normal stromal cells into CAFs and by this influence to modulate the microenvironment. This process represents a fundamental and crucial hallmark of cancer. Neoplastic cells that fail to develop this capacity will not pass critical barriers in tumorigenesis and will remain dormant. Therefore, understanding the interplay between neoplastic cells and their microenvironment is critical, especially in the initiation of cancer. Further insights in this process have the potential to reveal relevant discoveries with subsequent clinical implications.
Acknowledgments
We thank Lindsey A. Baker, Vincenzo Corbo, Christine Chio, Mariano Ponz-Sarvise, Dannielle Engle, Abram Handly-Santana, and Tobiloba Oni for critical feedback on the manuscript.
Daniel Öhlund is supported by the Swedish Research Council (537-2013-7277), The Kempe Foundations (JCK-1301), and The Swedish Society of Medicine (SLS-326921, SLS-250831). Ela Elyada is supported by the Human Frontiers Science Program (LT000403/2014) and by the Weizmann Institute of Science Women in Science award. David Tuveson is supported by the Lustgarten Foundation for Pancreatic Cancer Research, the Cold Spring Harbor Laboratory Association, the Carcinoid Foundation, the STARR foundation (I7-A718), PCUK, DOD (W81XWH-13-PRCRP-IA), and the National Institutes of Health (5P30CA45508-26, 5P50CA101955-07, 1U10CA180944-01, and 5U01CA168409-3).
The authors declare no competing financial interests.
References
- Ahrens, T., Sleeman J.P., Schempp C.M., Howells N., Hofmann M., Ponta H., Herrlich P., and Simon J.C.. 2001. Soluble CD44 inhibits melanoma tumor growth by blocking cell surface CD44 binding to hyaluronic acid. Oncogene. 20:3399–3408 10.1038/sj.onc.1204435 [DOI] [PubMed] [Google Scholar]
- Akhurst, R.J., and Hata A.. 2012. Targeting the TGFβ signalling pathway in disease. Nat. Rev. Drug Discov. 11:790–811 10.1038/nrd3810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allinen, M., Beroukhim R., Cai L., Brennan C., Lahti-Domenici J., Huang H., Porter D., Hu M., Chin L., Richardson A., et al. 2004. Molecular characterization of the tumor microenvironment in breast cancer. Cancer Cell. 6:17–32 10.1016/j.ccr.2004.06.010 [DOI] [PubMed] [Google Scholar]
- Alvarez, R., Musteanu M., Garcia-Garcia E., Lopez-Casas P.P., Megias D., Guerra C., Muñoz M., Quijano Y., Cubillo A., Rodriguez-Pascual J., et al. 2013. Stromal disrupting effects of nab-paclitaxel in pancreatic cancer. Br. J. Cancer. 109:926–933 10.1038/bjc.2013.415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderberg, C., and Pietras K.. 2009. On the origin of cancer-associated fibroblasts. Cell Cycle. 8:1461–1465 10.4161/cc.8.10.8557 [DOI] [PubMed] [Google Scholar]
- Aprelikova, O., Yu X., Palla J., Wei B.-R., John S., Yi M., Stephens R., Simpson R.M., Risinger J.I., Jazaeri A., and Niederhuber J.. 2010. The role of miR-31 and its target gene SATB2 in cancer-associated fibroblasts. Cell Cycle. 9:4387–4398 10.4161/cc.9.21.13674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aprelikova, O., Palla J., Hibler B., Yu X., Greer Y.E., Yi M., Stephens R., Maxwell G.L., Jazaeri A., Risinger J.I., et al. 2013. Silencing of miR-148a in cancer-associated fibroblasts results in WNT10B-mediated stimulation of tumor cell motility. Oncogene. 32:3246–3253 10.1038/onc.2012.351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armelin, H.A.1973. Pituitary extracts and steroid hormones in the control of 3T3 cell growth. Proc. Natl. Acad. Sci. USA. 70:2702–2706 10.1073/pnas.70.9.2702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augsten, M., Hägglöf C., Olsson E., Stolz C., Tsagozis P., Levchenko T., Frederick M.J., Borg A., Micke P., Egevad L., and Ostman A.. 2009. CXCL14 is an autocrine growth factor for fibroblasts and acts as a multi-modal stimulator of prostate tumor growth. Proc. Natl. Acad. Sci. USA. 106:3414–3419 10.1073/pnas.0813144106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachem, M.G., Schneider E., Gross H., Weidenbach H., Schmid R.M., Menke A., Siech M., Beger H., Grünert A., and Adler G.. 1998. Identification, culture, and characterization of pancreatic stellate cells in rats and humans. Gastroenterology. 115:421–432 10.1016/S0016-5085(98)70209-4 [DOI] [PubMed] [Google Scholar]
- Bailey, J.M., Mohr A.M., and Hollingsworth M.A.. 2009. Sonic hedgehog paracrine signaling regulates metastasis and lymphangiogenesis in pancreatic cancer. Oncogene. 28:3513–3525 10.1038/onc.2009.220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balsamo, M., Scordamaglia F., Pietra G., Manzini C., Cantoni C., Boitano M., Queirolo P., Vermi W., Facchetti F., Moretta A., et al. 2009. Melanoma-associated fibroblasts modulate NK cell phenotype and antitumor cytotoxicity. Proc. Natl. Acad. Sci. USA. 106:20847–20852 10.1073/pnas.0906481106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barcellos-Hoff, M.H., and Ravani S.A.. 2000. Irradiated mammary gland stroma promotes the expression of tumorigenic potential by unirradiated epithelial cells. Cancer Res. 60:1254–1260 [PubMed] [Google Scholar]
- Barcellos-Hoff, M.H., Park C., and Wright E.G.. 2005. Radiation and the microenvironment - tumorigenesis and therapy. Nat. Rev. Cancer. 5:867–875 10.1038/nrc1735 [DOI] [PubMed] [Google Scholar]
- Benvenuti, S., and Comoglio P.M.. 2007. The MET receptor tyrosine kinase in invasion and metastasis. J. Cell. Physiol. 213:316–325 10.1002/jcp.21183 [DOI] [PubMed] [Google Scholar]
- Berdiel-Acer, M., Sanz-Pamplona R., Calon A., Cuadras D., Berenguer A., Sanjuan X., Paules M.J., Salazar R., Moreno V., Batlle E., et al. 2014. Differences between CAFs and their paired NCF from adjacent colonic mucosa reveal functional heterogeneity of CAFs, providing prognostic information. Mol. Oncol. 10.1016/j.molonc.2014.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhowmick, N.A., Chytil A., Plieth D., Gorska A.E., Dumont N., Shappell S., Washington M.K., Neilson E.G., and Moses H.L.. 2004. TGF-β signaling in fibroblasts modulates the oncogenic potential of adjacent epithelia. Science. 303:848–851 10.1126/science.1090922 [DOI] [PubMed] [Google Scholar]
- Bissell, M.J., and Hines W.C.. 2011. Why don’t we get more cancer? A proposed role of the microenvironment in restraining cancer progression. Nat. Med. 17:320–329 10.1038/nm.2328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bizik, J., Kankuri E., Ristimäki A., Taïeb A., Vapaatalo H., Lubitz W., and Vaheri A.. 2004. Cell-cell contacts trigger programmed necrosis and induce cyclooxygenase-2 expression. Cell Death Differ. 11:183–195 10.1038/sj.cdd.4401317 [DOI] [PubMed] [Google Scholar]
- Boire, A., Covic L., Agarwal A., Jacques S., Sherifi S., and Kuliopulos A.. 2005. PAR1 is a matrix metalloprotease-1 receptor that promotes invasion and tumorigenesis of breast cancer cells. Cell. 120:303–313 10.1016/j.cell.2004.12.018 [DOI] [PubMed] [Google Scholar]
- Bollag, G., Hirth P., Tsai J., Zhang J., Ibrahim P.N., Cho H., Spevak W., Zhang C., Zhang Y., Habets G., et al. 2010. Clinical efficacy of a RAF inhibitor needs broad target blockade in BRAF-mutant melanoma. Nature. 467:596–599 10.1038/nature09454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourguignon, L.Y., Singleton P.A., Zhu H., and Diedrich F.. 2003. Hyaluronan-mediated CD44 interaction with RhoGEF and Rho kinase promotes Grb2-associated binder-1 phosphorylation and phosphatidylinositol 3-kinase signaling leading to cytokine (macrophage-colony stimulating factor) production and breast tumor progression. J. Biol. Chem. 278:29420–29434 10.1074/jbc.M301885200 [DOI] [PubMed] [Google Scholar]
- Brennen, W.N., Isaacs J.T., and Denmeade S.R.. 2012. Rationale behind targeting fibroblast activation protein-expressing carcinoma-associated fibroblasts as a novel chemotherapeutic strategy. Mol. Cancer Ther. 11:257–266 10.1158/1535-7163.MCT-11-0340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brentnall, T.A., Lai L.A., Coleman J., Bronner M.P., Pan S., and Chen R.. 2012. Arousal of cancer-associated stroma: overexpression of palladin activates fibroblasts to promote tumor invasion. PLoS ONE. 7:e30219 10.1371/journal.pone.0030219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronisz, A., Godlewski J., Wallace J.A., Merchant A.S., Nowicki M.O., Mathsyaraja H., Srinivasan R., Trimboli A.J., Martin C.K., Li F., et al. 2012. Reprogramming of the tumour microenvironment by stromal PTEN-regulated miR-320. Nat. Cell Biol. 14:159–167 10.1038/ncb2396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronzert, D.A., Pantazis P., Antoniades H.N., Kasid A., Davidson N., Dickson R.B., and Lippman M.E.. 1987. Synthesis and secretion of platelet-derived growth factor by human breast cancer cell lines. Proc. Natl. Acad. Sci. USA. 84:5763–5767 10.1073/pnas.84.16.5763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calon, A., Espinet E., Palomo-Ponce S., Tauriello D.V., Iglesias M., Céspedes M.V., Sevillano M., Nadal C., Jung P., Zhang X.H., et al. 2012. Dependency of colorectal cancer on a TGF-β-driven program in stromal cells for metastasis initiation. Cancer Cell. 22:571–584 10.1016/j.ccr.2012.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, I., Polyak K., and Haviv I.. 2009. Clonal mutations in the cancer-associated fibroblasts: the case against genetic coevolution. Cancer Res. 69:6765–6768 10.1158/0008-5472.CAN-08-4253 [DOI] [PubMed] [Google Scholar]
- Cardone, A., Tolino A., Zarcone R., Borruto Caracciolo G., and Tartaglia E.. 1997. Prognostic value of desmoplastic reaction and lymphocytic infiltration in the management of breast cancer. Panminerva Med. 39:174–177 [PubMed] [Google Scholar]
- Chaffer, C.L., and Weinberg R.A.. 2011. A perspective on cancer cell metastasis. Science. 331:1559–1564 10.1126/science.1203543 [DOI] [PubMed] [Google Scholar]
- Chang, C.C., Hsu W.H., Wang C.C., Chou C.H., Kuo M.Y., Lin B.R., Chen S.T., Tai S.K., Kuo M.L., and Yang M.H.. 2013. Connective tissue growth factor activates pluripotency genes and mesenchymal-epithelial transition in head and neck cancer cells. Cancer Res. 73:4147–4157 10.1158/0008-5472.CAN-12-4085 [DOI] [PubMed] [Google Scholar]
- Chapman, P.B., Hauschild A., Robert C., Haanen J.B., Ascierto P., Larkin J., Dummer R., Garbe C., Testori A., Maio M., et al. BRIM-3 Study Group. 2011. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N. Engl. J. Med. 364:2507–2516 10.1056/NEJMoa1103782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charrier, A., and Brigstock D.R.. 2013. Regulation of pancreatic function by connective tissue growth factor (CTGF, CCN2). Cytokine Growth Factor Rev. 24:59–68 10.1016/j.cytogfr.2012.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhri, V.K., Salzler G.G., Dick S.A., Buckman M.S., Sordella R., Karoly E.D., Mohney R., Stiles B.M., Elemento O., Altorki N.K., and McGraw T.E.. 2013. Metabolic alterations in lung cancer-associated fibroblasts correlated with increased glycolytic metabolism of the tumor. Mol. Cancer Res. 11:579–592 10.1158/1541-7786.MCR-12-0437-T [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan, V.P., Martin J.D., Liu H., Lacorre D.A., Jain S.R., Kozin S.V., Stylianopoulos T., Mousa A.S., Han X., Adstamongkonkul P., et al. 2013. Angiotensin inhibition enhances drug delivery and potentiates chemotherapy by decompressing tumour blood vessels. Nat. Commun. 4:2516 10.1038/ncomms3516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng, J., Wang Y., Liang A., Jia L., and Du J.. 2012. FSP-1 silencing in bone marrow cells suppresses neointima formation in vein graft. Circ. Res. 110:230–240 10.1161/CIRCRESAHA.111.246025 [DOI] [PubMed] [Google Scholar]
- Cheng, J.D., Valianou M., Canutescu A.A., Jaffe E.K., Lee H.O., Wang H., Lai J.H., Bachovchin W.W., and Weiner L.M.. 2005. Abrogation of fibroblast activation protein enzymatic activity attenuates tumor growth. Mol. Cancer Ther. 4:351–360 [DOI] [PubMed] [Google Scholar]
- Cho, J.A., Park H., Lim E.H., and Lee K.W.. 2012. Exosomes from breast cancer cells can convert adipose tissue-derived mesenchymal stem cells into myofibroblast-like cells. Int. J. Oncol. 40:130–138 [DOI] [PubMed] [Google Scholar]
- Choi, J., Kim H., Jung W.H., and Koo J.S.. 2013. Metabolic interaction between cancer cells and stromal cells according to breast cancer molecular subtype. Breast Cancer Res. 15:R78 10.1186/bcr3472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cirri, P., and Chiarugi P.. 2011. Cancer associated fibroblasts: the dark side of the coin. Am J Cancer Res. 1:482–497 [PMC free article] [PubMed] [Google Scholar]
- Cordes, N., Seidler J., Durzok R., Geinitz H., and Brakebusch C.. 2006. β1-integrin-mediated signaling essentially contributes to cell survival after radiation-induced genotoxic injury. Oncogene. 25:1378–1390 10.1038/sj.onc.1209164 [DOI] [PubMed] [Google Scholar]
- Crawford, Y., Kasman I., Yu L., Zhong C., Wu X., Modrusan Z., Kaminker J., and Ferrara N.. 2009. PDGF-C mediates the angiogenic and tumorigenic properties of fibroblasts associated with tumors refractory to anti-VEGF treatment. Cancer Cell. 15:21–34 10.1016/j.ccr.2008.12.004 [DOI] [PubMed] [Google Scholar]
- Cukierman, E., and Bassi D.E.. 2010. Physico-mechanical aspects of extracellular matrix influences on tumorigenic behaviors. Semin. Cancer Biol. 20:139–145 10.1016/j.semcancer.2010.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuttler, A.S., LeClair R.J., Stohn J.P., Wang Q., Sorenson C.M., Liaw L., and Lindner V.. 2011. Characterization of Pdgfrb-Cre transgenic mice reveals reduction of ROSA26 reporter activity in remodeling arteries. Genesis. 49:673–680 10.1002/dvg.20769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danø, K., Behrendt N., Høyer-Hansen G., Johnsen M., Lund L.R., Ploug M., and Rømer J.. 2005. Plasminogen activation and cancer. Thromb. Haemost. 93:676–681 [DOI] [PubMed] [Google Scholar]
- Desmoulière, A., Redard M., Darby I., and Gabbiani G.. 1995. Apoptosis mediates the decrease in cellularity during the transition between granulation tissue and scar. Am. J. Pathol. 146:56–66 [PMC free article] [PubMed] [Google Scholar]
- Desmoulière, A., Guyot C., and Gabbiani G.. 2004. The stroma reaction myofibroblast: a key player in the control of tumor cell behavior. Int. J. Dev. Biol. 48:509–517 10.1387/ijdb.041802ad [DOI] [PubMed] [Google Scholar]
- Ding, N., Yu R.T., Subramaniam N., Sherman M.H., Wilson C., Rao R., Leblanc M., Coulter S., He M., Scott C., et al. 2013. A vitamin D receptor/SMAD genomic circuit gates hepatic fibrotic response. Cell. 153:601–613 10.1016/j.cell.2013.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diop-Frimpong, B., Chauhan V.P., Krane S., Boucher Y., and Jain R.K.. 2011. Losartan inhibits collagen I synthesis and improves the distribution and efficacy of nanotherapeutics in tumors. Proc. Natl. Acad. Sci. USA. 108:2909–2914 10.1073/pnas.1018892108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Direkze, N.C., Hodivala-Dilke K., Jeffery R., Hunt T., Poulsom R., Oukrif D., Alison M.R., and Wright N.A.. 2004. Bone marrow contribution to tumor-associated myofibroblasts and fibroblasts. Cancer Res. 64:8492–8495 10.1158/0008-5472.CAN-04-1708 [DOI] [PubMed] [Google Scholar]
- Doherty, J.R., and Cleveland J.L.. 2013. Targeting lactate metabolism for cancer therapeutics. J. Clin. Invest. 123:3685–3692 10.1172/JCI69741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domanska, U.M., Timmer-Bosscha H., Nagengast W.B., Oude Munnink T.H., Kruizinga R.C., Ananias H.J., Kliphuis N.M., Huls G., De Vries E.G., de Jong I.J., and Walenkamp A.M.. 2012. CXCR4 inhibition with AMD3100 sensitizes prostate cancer to docetaxel chemotherapy. Neoplasia. 14:709–718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duda, D.G., Duyverman A.M., Kohno M., Snuderl M., Steller E.J., Fukumura D., and Jain R.K.. 2010. Malignant cells facilitate lung metastasis by bringing their own soil. Proc. Natl. Acad. Sci. USA. 107:21677–21682 10.1073/pnas.1016234107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dufour, A., and Overall C.M.. 2013. Missing the target: matrix metalloproteinase antitargets in inflammation and cancer. Trends Pharmacol. Sci. 34:233–242 10.1016/j.tips.2013.02.004 [DOI] [PubMed] [Google Scholar]
- Dvorak, H.F.1986. Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N. Engl. J. Med. 315:1650–1659 10.1056/NEJM198612253152606 [DOI] [PubMed] [Google Scholar]
- Eguchi, D., Ikenaga N., Ohuchida K., Kozono S., Cui L., Fujiwara K., Fujino M., Ohtsuka T., Mizumoto K., and Tanaka M.. 2013. Hypoxia enhances the interaction between pancreatic stellate cells and cancer cells via increased secretion of connective tissue growth factor. J. Surg. Res. 181:225–233 10.1016/j.jss.2012.06.051 [DOI] [PubMed] [Google Scholar]
- Erez, N., Truitt M., Olson P., Arron S.T., and Hanahan D.. 2010. Cancer-Associated Fibroblasts Are Activated in Incipient Neoplasia to Orchestrate Tumor-Promoting Inflammation in an NF-κB-Dependent Manner. Cancer Cell. 17:135–147 10.1016/j.ccr.2009.12.041 [DOI] [PubMed] [Google Scholar]
- Erkan, M., Michalski C.W., Rieder S., Reiser-Erkan C., Abiatari I., Kolb A., Giese N.A., Esposito I., Friess H., and Kleeff J.. 2008. The activated stroma index is a novel and independent prognostic marker in pancreatic ductal adenocarcinoma. Clin. Gastroenterol. Hepatol. 6:1155–1161 10.1016/j.cgh.2008.05.006 [DOI] [PubMed] [Google Scholar]
- Erler, J.T., and Weaver V.M.. 2009. Three-dimensional context regulation of metastasis. Clin. Exp. Metastasis. 26:35–49 10.1007/s10585-008-9209-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer, P., Bonnefoi H., Anderle P., Cameron D., Wirapati P., Becette V., André S., Piccart M., Campone M., Brain E., et al. 2009. A stroma-related gene signature predicts resistance to neoadjuvant chemotherapy in breast cancer. Nat. Med. 15:68–74 10.1038/nm.1908 [DOI] [PubMed] [Google Scholar]
- Feig, C., Jones J.O., Kraman M., Wells R.J., Deonarine A., Chan D.S., Connell C.M., Roberts E.W., Zhao Q., Caballero O.L., et al. 2013. Targeting CXCL12 from FAP-expressing carcinoma-associated fibroblasts synergizes with anti-PD-L1 immunotherapy in pancreatic cancer. Proc. Natl. Acad. Sci. USA. 110:20212–20217 10.1073/pnas.1320318110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fidler, I.J., Wilmanns C., Staroselsky A., Radinsky R., Dong Z., and Fan D.. 1994. Modulation of tumor cell response to chemotherapy by the organ environment. Cancer Metastasis Rev. 13:209–222 10.1007/BF00689637 [DOI] [PubMed] [Google Scholar]
- Flaberg, E., Markasz L., Petranyi G., Stuber G., Dicso F., Alchihabi N., Oláh È., Csízy I., Józsa T., Andrén O., et al. 2011. High-throughput live-cell imaging reveals differential inhibition of tumor cell proliferation by human fibroblasts. Int. J. Cancer. 128:2793–2802 10.1002/ijc.25612 [DOI] [PubMed] [Google Scholar]
- Flaherty, K.T., Puzanov I., Kim K.B., Ribas A., McArthur G.A., Sosman J.A., O’Dwyer P.J., Lee R.J., Grippo J.F., Nolop K., and Chapman P.B.. 2010. Inhibition of mutated, activated BRAF in metastatic melanoma. N. Engl. J. Med. 363:809–819 10.1056/NEJMoa1002011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsberg, K., Valyi-Nagy I., Heldin C.H., Herlyn M., and Westermark B.. 1993. Platelet-derived growth factor (PDGF) in oncogenesis: development of a vascular connective tissue stroma in xenotransplanted human melanoma producing PDGF-BB. Proc. Natl. Acad. Sci. USA. 90:393–397 10.1073/pnas.90.2.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frese, K.K., Neesse A., Cook N., Bapiro T.E., Lolkema M.P., Jodrell D.I., and Tuveson D.A.. 2012. nab-Paclitaxel potentiates gemcitabine activity by reducing cytidine deaminase levels in a mouse model of pancreatic cancer. Cancer Discov. 2:260–269 10.1158/2159-8290.CD-11-0242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridman, R., Giaccone G., Kanemoto T., Martin G.R., Gazdar A.F., and Mulshine J.L.. 1990. Reconstituted basement membrane (matrigel) and laminin can enhance the tumorigenicity and the drug resistance of small cell lung cancer cell lines. Proc. Natl. Acad. Sci. USA. 87:6698–6702 10.1073/pnas.87.17.6698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Froeling, F.E., Feig C., Chelala C., Dobson R., Mein C.E., Tuveson D.A., Clevers H., Hart I.R., and Kocher H.M.. 2011. Retinoic acid-induced pancreatic stellate cell quiescence reduces paracrine Wnt-β-catenin signaling to slow tumor progression. Gastroenterology. 141:1486–1497: 1497.e14 10.1053/j.gastro.2011.06.047 [DOI] [PubMed] [Google Scholar]
- Gaggioli, C., Hooper S., Hidalgo-Carcedo C., Grosse R., Marshall J.F., Harrington K., and Sahai E.. 2007. Fibroblast-led collective invasion of carcinoma cells with differing roles for RhoGTPases in leading and following cells. Nat. Cell Biol. 9:1392–1400 10.1038/ncb1658 [DOI] [PubMed] [Google Scholar]
- Gao, R., and Brigstock D.R.. 2005. Connective tissue growth factor (CCN2) in rat pancreatic stellate cell function: integrin α5β1 as a novel CCN2 receptor. Gastroenterology. 129:1019–1030 10.1053/j.gastro.2005.06.067 [DOI] [PubMed] [Google Scholar]
- Garin-Chesa, P., Old L.J., and Rettig W.J.. 1990. Cell surface glycoprotein of reactive stromal fibroblasts as a potential antibody target in human epithelial cancers. Proc. Natl. Acad. Sci. USA. 87:7235–7239 10.1073/pnas.87.18.7235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannoni, E., Bianchini F., Masieri L., Serni S., Torre E., Calorini L., and Chiarugi P.. 2010. Reciprocal activation of prostate cancer cells and cancer-associated fibroblasts stimulates epithelial-mesenchymal transition and cancer stemness. Cancer Res. 70:6945–6956 10.1158/0008-5472.CAN-10-0785 [DOI] [PubMed] [Google Scholar]
- Giannoni, E., Bianchini F., Calorini L., and Chiarugi P.. 2011. Cancer associated fibroblasts exploit reactive oxygen species through a proinflammatory signature leading to epithelial mesenchymal transition and stemness. Antioxid. Redox Signal. 14:2361–2371 10.1089/ars.2010.3727 [DOI] [PubMed] [Google Scholar]
- Goetz, J.G., Minguet S., Navarro-Lérida I., Lazcano J.J., Samaniego R., Calvo E., Tello M., Osteso-Ibáñez T., Pellinen T., Echarri A., et al. 2011. Biomechanical remodeling of the microenvironment by stromal caveolin-1 favors tumor invasion and metastasis. Cell. 146:148–163 10.1016/j.cell.2011.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonda, T.A., Varro A., Wang T.C., and Tycko B.. 2010. Molecular biology of cancer-associated fibroblasts: can these cells be targeted in anti-cancer therapy? Semin. Cell Dev. Biol. 21:2–10 10.1016/j.semcdb.2009.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Götte, M., and Yip G.W.. 2006. Heparanase, hyaluronan, and CD44 in cancers: a breast carcinoma perspective. Cancer Res. 66:10233–10237 10.1158/0008-5472.CAN-06-1464 [DOI] [PubMed] [Google Scholar]
- Grivennikov, S.I., Greten F.R., and Karin M.. 2010. Immunity, inflammation, and cancer. Cell. 140:883–899 10.1016/j.cell.2010.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grum-Schwensen, B., Klingelhofer J., Berg C.H., El-Naaman C., Grigorian M., Lukanidin E., and Ambartsumian N.. 2005. Suppression of tumor development and metastasis formation in mice lacking the S100A4(mts1) gene. Cancer Res. 65:3772–3780 10.1158/0008-5472.CAN-04-4510 [DOI] [PubMed] [Google Scholar]
- Gu, J., Qian H., Shen L., Zhang X., Zhu W., Huang L., Yan Y., Mao F., Zhao C., Shi Y., and Xu W.. 2012. Gastric cancer exosomes trigger differentiation of umbilical cord derived mesenchymal stem cells to carcinoma-associated fibroblasts through TGF-β/Smad pathway. PLoS ONE. 7:e52465 10.1371/journal.pone.0052465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guarino, M., Rubino B., and Ballabio G.. 2007. The role of epithelial-mesenchymal transition in cancer pathology. Pathology. 39:305–318 10.1080/00313020701329914 [DOI] [PubMed] [Google Scholar]
- Guerra, C., Schuhmacher A.J., Cañamero M., Grippo P.J., Verdaguer L., Pérez-Gallego L., Dubus P., Sandgren E.P., and Barbacid M.. 2007. Chronic pancreatitis is essential for induction of pancreatic ductal adenocarcinoma by K-Ras oncogenes in adult mice. Cancer Cell. 11:291–302 10.1016/j.ccr.2007.01.012 [DOI] [PubMed] [Google Scholar]
- Guido, C., Whitaker-Menezes D., Capparelli C., Balliet R., Lin Z., Pestell R.G., Howell A., Aquila S., Andò S., Martinez-Outschoorn U., et al. 2012. Metabolic reprogramming of cancer-associated fibroblasts by TGF-β drives tumor growth: connecting TGF-β signaling with “Warburg-like” cancer metabolism and L-lactate production. Cell Cycle. 11:3019–3035 10.4161/cc.21384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo, X., Oshima H., Kitmura T., Taketo M.M., and Oshima M.. 2008. Stromal fibroblasts activated by tumor cells promote angiogenesis in mouse gastric cancer. J. Biol. Chem. 283:19864–19871 10.1074/jbc.M800798200 [DOI] [PubMed] [Google Scholar]
- Hamada, S., Masamune A., Takikawa T., Suzuki N., Kikuta K., Hirota M., Hamada H., Kobune M., Satoh K., and Shimosegawa T.. 2012. Pancreatic stellate cells enhance stem cell-like phenotypes in pancreatic cancer cells. Biochem. Biophys. Res. Commun. 421:349–354 10.1016/j.bbrc.2012.04.014 [DOI] [PubMed] [Google Scholar]
- Hanahan, D., and Weinberg R.A.. 2011. Hallmarks of cancer: the next generation. Cell. 144:646–674 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- Hartel, M., Di Mola F.F., Gardini A., Zimmermann A., Di Sebastiano P., Guweidhi A., Innocenti P., Giese T., Giese N., Büchler M.W., and Friess H.. 2004. Desmoplastic reaction influences pancreatic cancer growth behavior. World J. Surg. 28:818–825 10.1007/s00268-004-7147-4 [DOI] [PubMed] [Google Scholar]
- Hartmann, T.N., Burger J.A., Glodek A., Fujii N., and Burger M.. 2005. CXCR4 chemokine receptor and integrin signaling co-operate in mediating adhesion and chemoresistance in small cell lung cancer (SCLC) cells. Oncogene. 24:4462–4471 10.1038/sj.onc.1208621 [DOI] [PubMed] [Google Scholar]
- Haubeiss, S., Schmid J.O., Mürdter T.E., Sonnenberg M., Friedel G., van der Kuip H., and Aulitzky W.E.. 2010. Dasatinib reverses cancer-associated fibroblasts (CAFs) from primary lung carcinomas to a phenotype comparable to that of normal fibroblasts. Mol. Cancer. 9:168 10.1186/1476-4598-9-168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawinkels, L.J., Paauwe M., Verspaget H.W., Wiercinska E., van der Zon J.M., van der Ploeg K., Koelink P.J., Lindeman J.H., Mesker W., ten Dijke P., and Sier C.F.. 2014. Interaction with colon cancer cells hyperactivates TGF-β signaling in cancer-associated fibroblasts. Oncogene. 33:97–107 10.1038/onc.2012.536 [DOI] [PubMed] [Google Scholar]
- Hayward, S.W., Wang Y., Cao M., Hom Y.K., Zhang B., Grossfeld G.D., Sudilovsky D., and Cunha G.R.. 2001. Malignant transformation in a nontumorigenic human prostatic epithelial cell line. Cancer Res. 61:8135–8142 [PubMed] [Google Scholar]
- Herrera, M., Islam A.B., Herrera A., Martín P., García V., Silva J., Garcia J.M., Salas C., Casal I., de Herreros A.G., et al. 2013. Functional heterogeneity of cancer-associated fibroblasts from human colon tumors shows specific prognostic gene expression signature. Clin. Cancer Res. 19:5914–5926 10.1158/1078-0432.CCR-13-0694 [DOI] [PubMed] [Google Scholar]
- Hill, R., Song Y., Cardiff R.D., and Van Dyke T.. 2005. Selective evolution of stromal mesenchyme with p53 loss in response to epithelial tumorigenesis. Cell. 123:1001–1011 10.1016/j.cell.2005.09.030 [DOI] [PubMed] [Google Scholar]
- Hinz, B., Celetta G., Tomasek J.J., Gabbiani G., and Chaponnier C.. 2001. Alpha-smooth muscle actin expression upregulates fibroblast contractile activity. Mol. Biol. Cell. 12:2730–2741 10.1091/mbc.12.9.2730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofheinz, R.D., al-Batran S.E., Hartmann F., Hartung G., Jäger D., Renner C., Tanswell P., Kunz U., Amelsberg A., Kuthan H., and Stehle G.. 2003. Stromal antigen targeting by a humanised monoclonal antibody: an early phase II trial of sibrotuzumab in patients with metastatic colorectal cancer. Onkologie. 26:44–48 10.1159/000069863 [DOI] [PubMed] [Google Scholar]
- Hooper, S., Gaggioli C., and Sahai E.. 2010. A chemical biology screen reveals a role for Rab21-mediated control of actomyosin contractility in fibroblast-driven cancer invasion. Br. J. Cancer. 102:392–402 10.1038/sj.bjc.6605469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosein, A.N., Wu M., Arcand S.L., Lavallée S., Hébert J., Tonin P.N., and Basik M.. 2010. Breast carcinoma-associated fibroblasts rarely contain p53 mutations or chromosomal aberrations. Cancer Res. 70:5770–5777 10.1158/0008-5472.CAN-10-0673 [DOI] [PubMed] [Google Scholar]
- Hu, M., Yao J., Cai L., Bachman K.E., van den Brûle F., Velculescu V., and Polyak K.. 2005. Distinct epigenetic changes in the stromal cells of breast cancers. Nat. Genet. 37:899–905 10.1038/ng1596 [DOI] [PubMed] [Google Scholar]
- Hu, M., Peluffo G., Chen H., Gelman R., Schnitt S., and Polyak K.. 2009. Role of COX-2 in epithelial-stromal cell interactions and progression of ductal carcinoma in situ of the breast. Proc. Natl. Acad. Sci. USA. 106:3372–3377 10.1073/pnas.0813306106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, S., Fang R., Xu J., Qiu S., Zhang H., Du J., and Cai S.. 2011. Evaluation of the tumor targeting of a FAPα-based doxorubicin prodrug. J. Drug Target. 19:487–496 10.3109/1061186X.2010.511225 [DOI] [PubMed] [Google Scholar]
- Hwang, R.F., Moore T., Arumugam T., Ramachandran V., Amos K.D., Rivera A., Ji B., Evans D.B., and Logsdon C.D.. 2008. Cancer-associated stromal fibroblasts promote pancreatic tumor progression. Cancer Res. 68:918–926 10.1158/0008-5472.CAN-07-5714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iijima, J., Konno K., and Itano N.. 2011. Inflammatory alterations of the extracellular matrix in the tumor microenvironment. Cancers (Basel). 3:3189–3205 10.3390/cancers3033189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishii, G., Sangai T., Oda T., Aoyagi Y., Hasebe T., Kanomata N., Endoh Y., Okumura C., Okuhara Y., Magae J., et al. 2003. Bone-marrow-derived myofibroblasts contribute to the cancer-induced stromal reaction. Biochem. Biophys. Res. Commun. 309:232–240 10.1016/S0006-291X(03)01544-4 [DOI] [PubMed] [Google Scholar]
- Iwano, M., Plieth D., Danoff T.M., Xue C., Okada H., and Neilson E.G.. 2002. Evidence that fibroblasts derive from epithelium during tissue fibrosis. J. Clin. Invest. 110:341–350 10.1172/JCI0215518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobetz, M.A., Chan D.S., Neesse A., Bapiro T.E., Cook N., Frese K.K., Feig C., Nakagawa T., Caldwell M.E., Zecchini H.I., et al. 2013. Hyaluronan impairs vascular function and drug delivery in a mouse model of pancreatic cancer. Gut. 62:112–120 10.1136/gutjnl-2012-302529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson, A., and Cunningham J.L.. 2012. Connective tissue growth factor in tumor pathogenesis. Fibrogenesis Tissue Repair. 5:S8 10.1186/1755-1536-5-S1-S8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain, R.K.1990. Vascular and interstitial barriers to delivery of therapeutic agents in tumors. Cancer Metastasis Rev. 9:253–266 10.1007/BF00046364 [DOI] [PubMed] [Google Scholar]
- Jedeszko, C., Victor B.C., Podgorski I., and Sloane B.F.. 2009. Fibroblast hepatocyte growth factor promotes invasion of human mammary ductal carcinoma in situ. Cancer Res. 69:9148–9155 10.1158/0008-5472.CAN-09-1043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeon, E.S., Moon H.J., Lee M.J., Song H.Y., Kim Y.M., Cho M., Suh D.S., Yoon M.S., Chang C.L., Jung J.S., and Kim J.H.. 2008. Cancer-derived lysophosphatidic acid stimulates differentiation of human mesenchymal stem cells to myofibroblast-like cells. Stem Cells. 26:789–797 10.1634/stemcells.2007-0742 [DOI] [PubMed] [Google Scholar]
- Jiang, L., Gonda T.A., Gamble M.V., Salas M., Seshan V., Tu S., Twaddell W.S., Hegyi P., Lazar G., Steele I., et al. 2008. Global hypomethylation of genomic DNA in cancer-associated myofibroblasts. Cancer Res. 68:9900–9908 10.1158/0008-5472.CAN-08-1319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung, D.W., Che Z.M., Kim J., Kim K., Kim K.Y., Williams D., and Kim J.. 2010. Tumor-stromal crosstalk in invasion of oral squamous cell carcinoma: a pivotal role of CCL7. Int. J. Cancer. 127:332–344 [DOI] [PubMed] [Google Scholar]
- Kadaba, R., Birke H., Wang J., Hooper S., Andl C.D., Di Maggio F., Soylu E., Ghallab M., Bor D., Froeling F.E., et al. 2013. Imbalance of desmoplastic stromal cell numbers drives aggressive cancer processes. J. Pathol. 230:107–117 10.1002/path.4172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahlert, C., and Kalluri R.. 2013. Exosomes in tumor microenvironment influence cancer progression and metastasis. J. Mol. Med. 91:431–437 10.1007/s00109-013-1020-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalluri, R., and Zeisberg M.. 2006. Fibroblasts in cancer. Nat. Rev. Cancer. 6:392–401 10.1038/nrc1877 [DOI] [PubMed] [Google Scholar]
- Kano, M.R., Bae Y., Iwata C., Morishita Y., Yashiro M., Oka M., Fujii T., Komuro A., Kiyono K., Kaminishi M., et al. 2007. Improvement of cancer-targeting therapy, using nanocarriers for intractable solid tumors by inhibition of TGF-β signaling. Proc. Natl. Acad. Sci. USA. 104:3460–3465 10.1073/pnas.0611660104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karnoub, A.E., Dash A.B., Vo A.P., Sullivan A., Brooks M.W., Bell G.W., Richardson A.L., Polyak K., Tubo R., and Weinberg R.A.. 2007. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature. 449:557–563 10.1038/nature06188 [DOI] [PubMed] [Google Scholar]
- Kawase, A., Ishii G., Nagai K., Ito T., Nagano T., Murata Y., Hishida T., Nishimura M., Yoshida J., Suzuki K., and Ochiai A.. 2008. Podoplanin expression by cancer associated fibroblasts predicts poor prognosis of lung adenocarcinoma. Int. J. Cancer. 123:1053–1059 10.1002/ijc.23611 [DOI] [PubMed] [Google Scholar]
- Kidd, S., Spaeth E., Watson K., Burks J., Lu H., Klopp A., Andreeff M., and Marini F.C.. 2012. Origins of the tumor microenvironment: quantitative assessment of adipose-derived and bone marrow-derived stroma. PLoS ONE. 7:e30563 10.1371/journal.pone.0030563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kikuta, K., Masamune A., Watanabe T., Ariga H., Itoh H., Hamada S., Satoh K., Egawa S., Unno M., and Shimosegawa T.. 2010. Pancreatic stellate cells promote epithelial-mesenchymal transition in pancreatic cancer cells. Biochem. Biophys. Res. Commun. 403:380–384 10.1016/j.bbrc.2010.11.040 [DOI] [PubMed] [Google Scholar]
- Kinugasa, Y., Matsui T., and Takakura N.. 2014. CD44 expressed on cancer-associated fibroblasts is a functional molecule supporting the stemness and drug resistance of malignant cancer cells in the tumor microenvironment. Stem Cells. 32:145–156 10.1002/stem.1556 [DOI] [PubMed] [Google Scholar]
- Kobayashi, N., Miyoshi S., Mikami T., Koyama H., Kitazawa M., Takeoka M., Sano K., Amano J., Isogai Z., Niida S., et al. 2010. Hyaluronan deficiency in tumor stroma impairs macrophage trafficking and tumor neovascularization. Cancer Res. 70:7073–7083 10.1158/0008-5472.CAN-09-4687 [DOI] [PubMed] [Google Scholar]
- Kojima, Y., Acar A., Eaton E.N., Mellody K.T., Scheel C., Ben-Porath I., Onder T.T., Wang Z.C., Richardson A.L., Weinberg R.A., and Orimo A.. 2010. Autocrine TGF-β and stromal cell-derived factor-1 (SDF-1) signaling drives the evolution of tumor-promoting mammary stromal myofibroblasts. Proc. Natl. Acad. Sci. USA. 107:20009–20014 10.1073/pnas.1013805107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kordes, C., Sawitza I., and Häussinger D.. 2009. Hepatic and pancreatic stellate cells in focus. Biol. Chem. 390:1003–1012 10.1515/BC.2009.121 [DOI] [PubMed] [Google Scholar]
- Koukourakis, M.I., Giatromanolaki A., Harris A.L., and Sivridis E.. 2006. Comparison of metabolic pathways between cancer cells and stromal cells in colorectal carcinomas: a metabolic survival role for tumor-associated stroma. Cancer Res. 66:632–637 10.1158/0008-5472.CAN-05-3260 [DOI] [PubMed] [Google Scholar]
- Kraman, M., Bambrough P.J., Arnold J.N., Roberts E.W., Magiera L., Jones J.O., Gopinathan A., Tuveson D.A., and Fearon D.T.. 2010. Suppression of antitumor immunity by stromal cells expressing fibroblast activation protein-α. Science. 330:827–830 10.1126/science.1195300 [DOI] [PubMed] [Google Scholar]
- Krtolica, A., Parrinello S., Lockett S., Desprez P.Y., and Campisi J.. 2001. Senescent fibroblasts promote epithelial cell growth and tumorigenesis: a link between cancer and aging. Proc. Natl. Acad. Sci. USA. 98:12072–12077 10.1073/pnas.211053698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuperwasser, C., Chavarria T., Wu M., Magrane G., Gray J.W., Carey L., Richardson A., and Weinberg R.A.. 2004. Reconstruction of functionally normal and malignant human breast tissues in mice. Proc. Natl. Acad. Sci. USA. 101:4966–4971 10.1073/pnas.0401064101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurose, K., Gilley K., Matsumoto S., Watson P.H., Zhou X.P., and Eng C.. 2002. Frequent somatic mutations in PTEN and TP53 are mutually exclusive in the stroma of breast carcinomas. Nat. Genet. 32:355–357 10.1038/ng1013 [DOI] [PubMed] [Google Scholar]
- Kwabi-Addo, B., Ozen M., and Ittmann M.. 2004. The role of fibroblast growth factors and their receptors in prostate cancer. Endocr. Relat. Cancer. 11:709–724 10.1677/erc.1.00535 [DOI] [PubMed] [Google Scholar]
- LeBeau, A.M., Brennen W.N., Aggarwal S., and Denmeade S.R.. 2009. Targeting the cancer stroma with a fibroblast activation protein-activated promelittin protoxin. Mol. Cancer Ther. 8:1378–1386 10.1158/1535-7163.MCT-08-1170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lederle, W., Hartenstein B., Meides A., Kunzelmann H., Werb Z., Angel P., and Mueller M.M.. 2010. MMP13 as a stromal mediator in controlling persistent angiogenesis in skin carcinoma. Carcinogenesis. 31:1175–1184 10.1093/carcin/bgp248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, J., Fassnacht M., Nair S., Boczkowski D., and Gilboa E.. 2005. Tumor immunotherapy targeting fibroblast activation protein, a product expressed in tumor-associated fibroblasts. Cancer Res. 65:11156–11163 10.1158/0008-5472.CAN-05-2805 [DOI] [PubMed] [Google Scholar]
- Lee, M.J., Ye A.S., Gardino A.K., Heijink A.M., Sorger P.K., MacBeath G., and Yaffe M.B.. 2012. Sequential application of anticancer drugs enhances cell death by rewiring apoptotic signaling networks. Cell. 149:780–794 10.1016/j.cell.2012.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemons, J.M., Feng X.J., Bennett B.D., Legesse-Miller A., Johnson E.L., Raitman I., Pollina E.A., Rabitz H.A., Rabinowitz J.D., and Coller H.A.. 2010. Quiescent fibroblasts exhibit high metabolic activity. PLoS Biol. 8:e1000514 10.1371/journal.pbio.1000514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levental, K.R., Yu H., Kass L., Lakins J.N., Egeblad M., Erler J.T., Fong S.F., Csiszar K., Giaccia A., Weninger W., et al. 2009. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell. 139:891–906 10.1016/j.cell.2009.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, H.J., Reinhardt F., Herschman H.R., and Weinberg R.A.. 2012a. Cancer-stimulated mesenchymal stem cells create a carcinoma stem cell niche via prostaglandin E2 signaling. Cancer Discov. 2:840–855 10.1158/2159-8290.CD-12-0101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, T., Yang Y., Hua X., Wang G., Liu W., Jia C., Tai Y., Zhang Q., and Chen G.. 2012b. Hepatocellular carcinoma-associated fibroblasts trigger NK cell dysfunction via PGE2 and IDO. Cancer Lett. 318:154–161 10.1016/j.canlet.2011.12.020 [DOI] [PubMed] [Google Scholar]
- Li, X., Ma Q., Xu Q., Liu H., Lei J., Duan W., Bhat K., Wang F., Wu E., and Wang Z.. 2012c. SDF-1/CXCR4 signaling induces pancreatic cancer cell invasion and epithelial-mesenchymal transition in vitro through non-canonical activation of Hedgehog pathway. Cancer Lett. 322:169–176 10.1016/j.canlet.2012.02.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao, D., Luo Y., Markowitz D., Xiang R., and Reisfeld R.A.. 2009. Cancer associated fibroblasts promote tumor growth and metastasis by modulating the tumor immune microenvironment in a 4T1 murine breast cancer model. PLoS ONE. 4:e7965 10.1371/journal.pone.0007965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieubeau, B., Garrigue L., Barbieux I., Meflah K., and Gregoire M.. 1994. The role of transforming growth factor beta 1 in the fibroblastic reaction associated with rat colorectal tumor development. Cancer Res. 54:6526–6532 [PubMed] [Google Scholar]
- Liu, J., Liao S., Diop-Frimpong B., Chen W., Goel S., Naxerova K., Ancukiewicz M., Boucher Y., Jain R.K., and Xu L.. 2012. TGF-β blockade improves the distribution and efficacy of therapeutics in breast carcinoma by normalizing the tumor stroma. Proc. Natl. Acad. Sci. USA. 109:16618–16623 10.1073/pnas.1117610109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, S., Ginestier C., Ou S.J., Clouthier S.G., Patel S.H., Monville F., Korkaya H., Heath A., Dutcher J., Kleer C.G., et al. 2011. Breast cancer stem cells are regulated by mesenchymal stem cells through cytokine networks. Cancer Res. 71:614–624 10.1158/0008-5472.CAN-10-0538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeffler, M., Krüger J.A., Niethammer A.G., and Reisfeld R.A.. 2006. Targeting tumor-associated fibroblasts improves cancer chemotherapy by increasing intratumoral drug uptake. J. Clin. Invest. 116:1955–1962 10.1172/JCI26532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löhr, M., Schmidt C., Ringel J., Kluth M., Müller P., Nizze H., and Jesnowski R.. 2001. Transforming growth factor-beta1 induces desmoplasia in an experimental model of human pancreatic carcinoma. Cancer Res. 61:550–555 [PubMed] [Google Scholar]
- Lotti, F., Jarrar A.M., Pai R.K., Hitomi M., Lathia J., Mace A., Gantt G.A. Jr, Sukhdeo K., DeVecchio J., Vasanji A., et al. 2013. Chemotherapy activates cancer-associated fibroblasts to maintain colorectal cancer-initiating cells by IL-17A. J. Exp. Med. 210:2851–2872 10.1084/jem.20131195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luga, V., Zhang L., Viloria-Petit A.M., Ogunjimi A.A., Inanlou M.R., Chiu E., Buchanan M., Hosein A.N., Basik M., and Wrana J.L.. 2012. Exosomes mediate stromal mobilization of autocrine Wnt-PCP signaling in breast cancer cell migration. Cell. 151:1542–1556 10.1016/j.cell.2012.11.024 [DOI] [PubMed] [Google Scholar]
- Mace, T.A., Ameen Z., Collins A., Wojcik S., Mair M., Young G.S., Fuchs J.R., Eubank T.D., Frankel W.L., Bekaii-Saab T., et al. 2013. Pancreatic cancer-associated stellate cells promote differentiation of myeloid-derived suppressor cells in a STAT3-dependent manner. Cancer Res. 73:3007–3018 10.1158/0008-5472.CAN-12-4601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madar, S., Brosh R., Buganim Y., Ezra O., Goldstein I., Solomon H., Kogan I., Goldfinger N., Klocker H., and Rotter V.. 2009. Modulated expression of WFDC1 during carcinogenesis and cellular senescence. Carcinogenesis. 30:20–27 10.1093/carcin/bgn232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeshima, A.M., Niki T., Maeshima A., Yamada T., Kondo H., and Matsuno Y.. 2002. Modified scar grade: a prognostic indicator in small peripheral lung adenocarcinoma. Cancer. 95:2546–2554 10.1002/cncr.11006 [DOI] [PubMed] [Google Scholar]
- Malanchi, I., Santamaria-Martínez A., Susanto E., Peng H., Lehr H.A., Delaloye J.F., and Huelsken J.. 2012. Interactions between cancer stem cells and their niche govern metastatic colonization. Nature. 481:85–89 10.1038/nature10694 [DOI] [PubMed] [Google Scholar]
- Martinez-Outschoorn, U.E., Lin Z., Trimmer C., Flomenberg N., Wang C., Pavlides S., Pestell R.G., Howell A., Sotgia F., and Lisanti M.P.. 2011. Cancer cells metabolically “fertilize” the tumor microenvironment with hydrogen peroxide, driving the Warburg effect: implications for PET imaging of human tumors. Cell Cycle. 10:2504–2520 10.4161/cc.10.15.16585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masamune, A., Hamada S., Kikuta K., Takikawa T., Miura S., Nakano E., and Shimosegawa T.. 2013. The angiotensin II type I receptor blocker olmesartan inhibits the growth of pancreatic cancer by targeting stellate cell activities in mice. Scand. J. Gastroenterol. 48:602–609 10.3109/00365521.2013.777776 [DOI] [PubMed] [Google Scholar]
- Masamune, A., Nakano E., Hamada S., Takikawa T., Yoshida N., and Shimosegawa T.. 2014. Alteration of the microRNA expression profile during the activation of pancreatic stellate cells. Scand. J. Gastroenterol. 49:323–331 10.3109/00365521.2013.876447 [DOI] [PubMed] [Google Scholar]
- Matsuda, Y., Kure S., and Ishiwata T.. 2012. Nestin and other putative cancer stem cell markers in pancreatic cancer. Med. Mol. Morphol. 45:59–65 10.1007/s00795-012-0571-x [DOI] [PubMed] [Google Scholar]
- McMillin, D.W., Negri J.M., and Mitsiades C.S.. 2013. The role of tumour-stromal interactions in modifying drug response: challenges and opportunities. Nat. Rev. Drug Discov. 12:217–228 10.1038/nrd3870 [DOI] [PubMed] [Google Scholar]
- Meads, M.B., Gatenby R.A., and Dalton W.S.. 2009. Environment-mediated drug resistance: a major contributor to minimal residual disease. Nat. Rev. Cancer. 9:665–674 10.1038/nrc2714 [DOI] [PubMed] [Google Scholar]
- Mishra, P.J., Mishra P.J., Humeniuk R., Medina D.J., Alexe G., Mesirov J.P., Ganesan S., Glod J.W., and Banerjee D.. 2008. Carcinoma-associated fibroblast-like differentiation of human mesenchymal stem cells. Cancer Res. 68:4331–4339 10.1158/0008-5472.CAN-08-0943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitra, A.K., Zillhardt M., Hua Y., Tiwari P., Murmann A.E., Peter M.E., and Lengyel E.. 2012. MicroRNAs reprogram normal fibroblasts into cancer-associated fibroblasts in ovarian cancer. Cancer Discov. 2:1100–1108 10.1158/2159-8290.CD-12-0206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyamoto, H., Murakami T., Tsuchida K., Sugino H., Miyake H., and Tashiro S.. 2004. Tumor-stroma interaction of human pancreatic cancer: acquired resistance to anticancer drugs and proliferation regulation is dependent on extracellular matrix proteins. Pancreas. 28:38–44 10.1097/00006676-200401000-00006 [DOI] [PubMed] [Google Scholar]
- Mullamitha, S.A., Ton N.C., Parker G.J., Jackson A., Julyan P.J., Roberts C., Buonaccorsi G.A., Watson Y., Davies K., Cheung S., et al. 2007. Phase I evaluation of a fully human anti-alphav integrin monoclonal antibody (CNTO 95) in patients with advanced solid tumors. Clin. Cancer Res. 13:2128–2135 10.1158/1078-0432.CCR-06-2779 [DOI] [PubMed] [Google Scholar]
- Muranen, T., Selfors L.M., Worster D.T., Iwanicki M.P., Song L., Morales F.C., Gao S., Mills G.B., and Brugge J.S.. 2012. Inhibition of PI3K/mTOR leads to adaptive resistance in matrix-attached cancer cells. Cancer Cell. 21:227–239 10.1016/j.ccr.2011.12.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musumeci, M., Coppola V., Addario A., Patrizii M., Maugeri-Saccà M., Memeo L., Colarossi C., Francescangeli F., Biffoni M., Collura D., et al. 2011. Control of tumor and microenvironment cross-talk by miR-15a and miR-16 in prostate cancer. Oncogene. 30:4231–4242 10.1038/onc.2011.140 [DOI] [PubMed] [Google Scholar]
- Nakagawa, H., Liyanarachchi S., Davuluri R.V., Auer H., Martin E.W. Jr, de la Chapelle A., and Frankel W.L.. 2004. Role of cancer-associated stromal fibroblasts in metastatic colon cancer to the liver and their expression profiles. Oncogene. 23:7366–7377 10.1038/sj.onc.1208013 [DOI] [PubMed] [Google Scholar]
- Nakai, Y., Isayama H., Ijichi H., Sasaki T., Sasahira N., Hirano K., Kogure H., Kawakubo K., Yagioka H., Yashima Y., et al. 2010. Inhibition of renin-angiotensin system affects prognosis of advanced pancreatic cancer receiving gemcitabine. Br. J. Cancer. 103:1644–1648 10.1038/sj.bjc.6605955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neesse, A., Michl P., Frese K.K., Feig C., Cook N., Jacobetz M.A., Lolkema M.P., Buchholz M., Olive K.P., Gress T.M., and Tuveson D.A.. 2011. Stromal biology and therapy in pancreatic cancer. Gut. 60:861–868 10.1136/gut.2010.226092 [DOI] [PubMed] [Google Scholar]
- Neesse, A., Frese K.K., Bapiro T.E., Nakagawa T., Sternlicht M.D., Seeley T.W., Pilarsky C., Jodrell D.I., Spong S.M., and Tuveson D.A.. 2013. CTGF antagonism with mAb FG-3019 enhances chemotherapy response without increasing drug delivery in murine ductal pancreas cancer. Proc. Natl. Acad. Sci. USA. 110:12325–12330 10.1073/pnas.1300415110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neesse, A., Frese K.K., Chan D.S., Bapiro T.E., Howat W.J., Richards F.M., Ellenrieder V., Jodrell D.I., and Tuveson D.A.. 2014. SPARC independent drug delivery and antitumour effects of nab-paclitaxel in genetically engineered mice. Gut. 63:974–983 10.1136/gutjnl-2013-305559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noskova, V., Ahmadi S., Asander E., and Casslén B.. 2009. Ovarian cancer cells stimulate uPA gene expression in fibroblastic stromal cells via multiple paracrine and autocrine mechanisms. Gynecol. Oncol. 115:121–126 10.1016/j.ygyno.2009.06.026 [DOI] [PubMed] [Google Scholar]
- O’Connell, J.T., Sugimoto H., Cooke V.G., MacDonald B.A., Mehta A.I., LeBleu V.S., Dewar R., Rocha R.M., Brentani R.R., Resnick M.B., et al. 2011. VEGF-A and Tenascin-C produced by S100A4+ stromal cells are important for metastatic colonization. Proc. Natl. Acad. Sci. USA. 108:16002–16007 10.1073/pnas.1109493108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohuchida, K., Mizumoto K., Murakami M., Qian L.W., Sato N., Nagai E., Matsumoto K., Nakamura T., and Tanaka M.. 2004. Radiation to stromal fibroblasts increases invasiveness of pancreatic cancer cells through tumor-stromal interactions. Cancer Res. 64:3215–3222 10.1158/0008-5472.CAN-03-2464 [DOI] [PubMed] [Google Scholar]
- Okada, H., Danoff T.M., Kalluri R., and Neilson E.G.. 1997. Early role of Fsp1 in epithelial-mesenchymal transformation. Am. J. Physiol. 273:F563–F574 [DOI] [PubMed] [Google Scholar]
- Olive, K.P., Jacobetz M.A., Davidson C.J., Gopinathan A., McIntyre D., Honess D., Madhu B., Goldgraben M.A., Caldwell M.E., Allard D., et al. 2009. Inhibition of Hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science. 324:1457–1461 10.1126/science.1171362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olumi, A.F., Grossfeld G.D., Hayward S.W., Carroll P.R., Tlsty T.D., and Cunha G.R.. 1999. Carcinoma-associated fibroblasts direct tumor progression of initiated human prostatic epithelium. Cancer Res. 59:5002–5011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orimo, A., and Weinberg R.A.. 2007. Heterogeneity of stromal fibroblasts in tumors. Cancer Biol. Ther. 6:618–619 10.4161/cbt.6.4.4255 [DOI] [PubMed] [Google Scholar]
- Orimo, A., Tomioka Y., Shimizu Y., Sato M., Oigawa S., Kamata K., Nogi Y., Inoue S., Takahashi M., Hata T., and Muramatsu M.. 2001. Cancer-associated myofibroblasts possess various factors to promote endometrial tumor progression. Clin. Cancer Res. 7:3097–3105 [PubMed] [Google Scholar]
- Orimo, A., Gupta P.B., Sgroi D.C., Arenzana-Seisdedos F., Delaunay T., Naeem R., Carey V.J., Richardson A.L., and Weinberg R.A.. 2005. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell. 121:335–348 10.1016/j.cell.2005.02.034 [DOI] [PubMed] [Google Scholar]
- Ostermann, E., Garin-Chesa P., Heider K.H., Kalat M., Lamche H., Puri C., Kerjaschki D., Rettig W.J., and Adolf G.R.. 2008. Effective immunoconjugate therapy in cancer models targeting a serine protease of tumor fibroblasts. Clin. Cancer Res. 14:4584–4592 10.1158/1078-0432.CCR-07-5211 [DOI] [PubMed] [Google Scholar]
- Österreicher, C.H., Penz-Österreicher M., Grivennikov S.I., Guma M., Koltsova E.K., Datz C., Sasik R., Hardiman G., Karin M., and Brenner D.A.. 2011. Fibroblast-specific protein 1 identifies an inflammatory subpopulation of macrophages in the liver. Proc. Natl. Acad. Sci. USA. 108:308–313 10.1073/pnas.1017547108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özdemir, B.C., Pentcheva-Hoang T., Carstens J.L., Zheng X., Wu C.C., Simpson T.R., Laklai H., Sugimoto H., Kahlert C., Novitskiy S.V., et al. 2014. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell. 25:719–734 10.1016/j.ccr.2014.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paget, S.1889. The distribution of secondary growths in cancer of the breast. Lancet. 133:571–573 10.1016/S0140-6736(00)49915-0 [DOI] [PubMed] [Google Scholar]
- Park, C.C., Zhang H., Pallavicini M., Gray J.W., Baehner F., Park C.J., and Bissell M.J.. 2006. β1 integrin inhibitory antibody induces apoptosis of breast cancer cells, inhibits growth, and distinguishes malignant from normal phenotype in three dimensional cultures and in vivo. Cancer Res. 66:1526–1535 10.1158/0008-5472.CAN-05-3071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, C.C., Zhang H.J., Yao E.S., Park C.J., and Bissell M.J.. 2008. β1 integrin inhibition dramatically enhances radiotherapy efficacy in human breast cancer xenografts. Cancer Res. 68:4398–4405 10.1158/0008-5472.CAN-07-6390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patocs, A., Zhang L., Xu Y., Weber F., Caldes T., Mutter G.L., Platzer P., and Eng C.. 2007. Breast-cancer stromal cells with TP53 mutations and nodal metastases. N. Engl. J. Med. 357:2543–2551 10.1056/NEJMoa071825 [DOI] [PubMed] [Google Scholar]
- Paunescu, V., Bojin F.M., Tatu C.A., Gavriliuc O.I., Rosca A., Gruia A.T., Tanasie G., Bunu C., Crisnic D., Gherghiceanu M., et al. 2011. Tumour-associated fibroblasts and mesenchymal stem cells: more similarities than differences. J. Cell. Mol. Med. 15:635–646 10.1111/j.1582-4934.2010.01044.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavlides, S., Whitaker-Menezes D., Castello-Cros R., Flomenberg N., Witkiewicz A.K., Frank P.G., Casimiro M.C., Wang C., Fortina P., Addya S., et al. 2009. The reverse Warburg effect: aerobic glycolysis in cancer associated fibroblasts and the tumor stroma. Cell Cycle. 8:3984–4001 10.4161/cc.8.23.10238 [DOI] [PubMed] [Google Scholar]
- Peek, R.M. Jr, and Crabtree J.E.. 2006. Helicobacter infection and gastric neoplasia. J. Pathol. 208:233–248 10.1002/path.1868 [DOI] [PubMed] [Google Scholar]
- Peruzzi, B., and Bottaro D.P.. 2006. Targeting the c-Met signaling pathway in cancer. Clin. Cancer Res. 12:3657–3660 10.1158/1078-0432.CCR-06-0818 [DOI] [PubMed] [Google Scholar]
- Pickup, M., Novitskiy S., and Moses H.L.. 2013a. The roles of TGFβ in the tumour microenvironment. Nat. Rev. Cancer. 13:788–799 10.1038/nrc3603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickup, M.W., Laklai H., Acerbi I., Owens P., Gorska A.E., Chytil A., Aakre M., Weaver V.M., and Moses H.L.. 2013b. Stromally derived lysyl oxidase promotes metastasis of transforming growth factor-β-deficient mouse mammary carcinomas. Cancer Res. 73:5336–5346 10.1158/0008-5472.CAN-13-0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietras, K., and Ostman A.. 2010. Hallmarks of cancer: interactions with the tumor stroma. Exp. Cell Res. 316:1324–1331 10.1016/j.yexcr.2010.02.045 [DOI] [PubMed] [Google Scholar]
- Pietras, K., Pahler J., Bergers G., and Hanahan D.. 2008. Functions of paracrine PDGF signaling in the proangiogenic tumor stroma revealed by pharmacological targeting. PLoS Med. 5:e19 10.1371/journal.pmed.0050019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pikarsky, E., Porat R.M., Stein I., Abramovitch R., Amit S., Kasem S., Gutkovich-Pyest E., Urieli-Shoval S., Galun E., and Ben-Neriah Y.. 2004. NF-κB functions as a tumour promoter in inflammation-associated cancer. Nature. 431:461–466 10.1038/nature02924 [DOI] [PubMed] [Google Scholar]
- Polito, A., and Reynolds R.. 2005. NG2-expressing cells as oligodendrocyte progenitors in the normal and demyelinated adult central nervous system. J. Anat. 207:707–716 10.1111/j.1469-7580.2005.00454.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulsom, R., Pignatelli M., Stetler-Stevenson W.G., Liotta L.A., Wright P.A., Jeffery R.E., Longcroft J.M., Rogers L., and Stamp G.W.. 1992. Stromal expression of 72 kda type IV collagenase (MMP-2) and TIMP-2 mRNAs in colorectal neoplasia. Am. J. Pathol. 141:389–396 [PMC free article] [PubMed] [Google Scholar]
- Provenzano, P.P., Cuevas C., Chang A.E., Goel V.K., Von Hoff D.D., and Hingorani S.R.. 2012. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell. 21:418–429 10.1016/j.ccr.2012.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu, W., Hu M., Sridhar A., Opeskin K., Fox S., Shipitsin M., Trivett M., Thompson E.R., Ramakrishna M., Gorringe K.L., et al. 2008. No evidence of clonal somatic genetic alterations in cancer-associated fibroblasts from human breast and ovarian carcinomas. Nat. Genet. 40:650–655 10.1038/ng.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu, C.F., Song E.Y., Li Y., Rizvi S.M., Raja C., Smith R., Morgenstern A., Apostolidis C., and Allen B.J.. 2005. Pre-clinical study of 213Bi labeled PAI2 for the control of micrometastatic pancreatic cancer. Clin. Exp. Metastasis. 22:575–586 10.1007/s10585-005-5788-9 [DOI] [PubMed] [Google Scholar]
- Quante, M., Tu S.P., Tomita H., Gonda T., Wang S.S., Takashi S., Baik G.H., Shibata W., Diprete B., Betz K.S., et al. 2011. Bone marrow-derived myofibroblasts contribute to the mesenchymal stem cell niche and promote tumor growth. Cancer Cell. 19:257–272 10.1016/j.ccr.2011.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Räsänen, K., and Vaheri A.. 2010. Activation of fibroblasts in cancer stroma. Exp. Cell Res. 316:2713–2722 10.1016/j.yexcr.2010.04.032 [DOI] [PubMed] [Google Scholar]
- Reardon, D.A., Fink K.L., Mikkelsen T., Cloughesy T.F., O’Neill A., Plotkin S., Glantz M., Ravin P., Raizer J.J., Rich K.M., et al. 2008. Randomized phase II study of cilengitide, an integrin-targeting arginine-glycine-aspartic acid peptide, in recurrent glioblastoma multiforme. J. Clin. Oncol. 26:5610–5617 10.1200/JCO.2008.16.7510 [DOI] [PubMed] [Google Scholar]
- Rhim, A.D., Oberstein P.E., Thomas D.H., Mirek E.T., Palermo C.F., Sastra S.A., Dekleva E.N., Saunders T., Becerra C.P., Tattersall I.W., et al. 2014. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell. 25:735–747 10.1016/j.ccr.2014.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts, E.W., Deonarine A., Jones J.O., Denton A.E., Feig C., Lyons S.K., Espeli M., Kraman M., McKenna B., Wells R.J., et al. 2013. Depletion of stromal cells expressing fibroblast activation protein-α from skeletal muscle and bone marrow results in cachexia and anemia. J. Exp. Med. 210:1137–1151 10.1084/jem.20122344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rønnov-Jessen, L., and Petersen O.W.. 1993. Induction of α-smooth muscle actin by transforming growth factor-β1 in quiescent human breast gland fibroblasts. Implications for myofibroblast generation in breast neoplasia. Lab. Invest. 68:696–707 [PubMed] [Google Scholar]
- Rønnov-Jessen, L., and Petersen O.W.. 1996. A function for filamentous α-smooth muscle actin: retardation of motility in fibroblasts. J. Cell Biol. 134:67–80 10.1083/jcb.134.1.67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royal, R.E., Levy C., Turner K., Mathur A., Hughes M., Kammula U.S., Sherry R.M., Topalian S.L., Yang J.C., Lowy I., and Rosenberg S.A.. 2010. Phase 2 trial of single agent Ipilimumab (anti-CTLA-4) for locally advanced or metastatic pancreatic adenocarcinoma. J. Immunother. 33:828–833 10.1097/CJI.0b013e3181eec14c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saadi, A., Shannon N.B., Lao-Sirieix P., O’Donovan M., Walker E., Clemons N.J., Hardwick J.S., Zhang C., Das M., Save V., et al. 2010. Stromal genes discriminate preinvasive from invasive disease, predict outcome, and highlight inflammatory pathways in digestive cancers. Proc. Natl. Acad. Sci. USA. 107:2177–2182 10.1073/pnas.0909797107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakurai, T., Kudo M., Fukuta N., Nakatani T., Kimura M., Park A.M., and Munakata H.. 2011. Involvement of angiotensin II and reactive oxygen species in pancreatic fibrosis. Pancreatology. 11:7–13 10.1159/000323478 [DOI] [PubMed] [Google Scholar]
- Santos, A.M., Jung J., Aziz N., Kissil J.L., and Puré E.. 2009. Targeting fibroblast activation protein inhibits tumor stromagenesis and growth in mice. J. Clin. Invest. 119:3613–3625 10.1172/JCI38988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanz-Moreno, V., Gaggioli C., Yeo M., Albrengues J., Wallberg F., Viros A., Hooper S., Mitter R., Féral C.C., Cook M., et al. 2011. ROCK and JAK1 signaling cooperate to control actomyosin contractility in tumor cells and stroma. Cancer Cell. 20:229–245 10.1016/j.ccr.2011.06.018 [DOI] [PubMed] [Google Scholar]
- Sato, N., Maehara N., and Goggins M.. 2004. Gene expression profiling of tumor-stromal interactions between pancreatic cancer cells and stromal fibroblasts. Cancer Res. 64:6950–6956 10.1158/0008-5472.CAN-04-0677 [DOI] [PubMed] [Google Scholar]
- Scanlan, M.J., Raj B.K., Calvo B., Garin-Chesa P., Sanz-Moncasi M.P., Healey J.H., Old L.J., and Rettig W.J.. 1994. Molecular cloning of fibroblast activation protein alpha, a member of the serine protease family selectively expressed in stromal fibroblasts of epithelial cancers. Proc. Natl. Acad. Sci. USA. 91:5657–5661 10.1073/pnas.91.12.5657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott, A.M., Wiseman G., Welt S., Adjei A., Lee F.T., Hopkins W., Divgi C.R., Hanson L.H., Mitchell P., Gansen D.N., et al. 2003. A Phase I dose-escalation study of sibrotuzumab in patients with advanced or metastatic fibroblast activation protein-positive cancer. Clin. Cancer Res. 9:1639–1647 [PubMed] [Google Scholar]
- Serini, G., Bochaton-Piallat M.L., Ropraz P., Geinoz A., Borsi L., Zardi L., and Gabbiani G.. 1998. The fibronectin domain ED-A is crucial for myofibroblastic phenotype induction by transforming growth factor-β1. J. Cell Biol. 142:873–881 10.1083/jcb.142.3.873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sethi, T., Rintoul R.C., Moore S.M., MacKinnon A.C., Salter D., Choo C., Chilvers E.R., Dransfield I., Donnelly S.C., Strieter R., and Haslett C.. 1999. Extracellular matrix proteins protect small cell lung cancer cells against apoptosis: a mechanism for small cell lung cancer growth and drug resistance in vivo. Nat. Med. 5:662–668 10.1038/9511 [DOI] [PubMed] [Google Scholar]
- Shao, Z.M., Nguyen M., and Barsky S.H.. 2000. Human breast carcinoma desmoplasia is PDGF initiated. Oncogene. 19:4337–4345 10.1038/sj.onc.1203785 [DOI] [PubMed] [Google Scholar]
- Sherman-Baust, C.A., Weeraratna A.T., Rangel L.B., Pizer E.S., Cho K.R., Schwartz D.R., Shock T., and Morin P.J.. 2003. Remodeling of the extracellular matrix through overexpression of collagen VI contributes to cisplatin resistance in ovarian cancer cells. Cancer Cell. 3:377–386 10.1016/S1535-6108(03)00058-8 [DOI] [PubMed] [Google Scholar]
- Shimoda, M., Mellody K.T., and Orimo A.. 2010. Carcinoma-associated fibroblasts are a rate-limiting determinant for tumour progression. Semin. Cell Dev. Biol. 21:19–25 10.1016/j.semcdb.2009.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, S., Ross S.R., Acena M., Rowley D.A., and Schreiber H.. 1992. Stroma is critical for preventing or permitting immunological destruction of antigenic cancer cells. J. Exp. Med. 175:139–146 10.1084/jem.175.1.139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, S., Srivastava S.K., Bhardwaj A., Owen L.B., and Singh A.P.. 2010. CXCL12-CXCR4 signalling axis confers gemcitabine resistance to pancreatic cancer cells: a novel target for therapy. Br. J. Cancer. 103:1671–1679 10.1038/sj.bjc.6605968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, N.R., Baker D., Farren M., Pommier A., Swann R., Wang X., Mistry S., McDaid K., Kendrew J., Womack C., et al. 2013. Tumor stromal architecture can define the intrinsic tumor response to VEGF-targeted therapy. Clin. Cancer Res. 19:6943–6956 10.1158/1078-0432.CCR-13-1637 [DOI] [PubMed] [Google Scholar]
- Sosman, J.A., Kim K.B., Schuchter L., Gonzalez R., Pavlick A.C., Weber J.S., McArthur G.A., Hutson T.E., Moschos S.J., Flaherty K.T., et al. 2012. Survival in BRAF V600-mutant advanced melanoma treated with vemurafenib. N. Engl. J. Med. 366:707–714 10.1056/NEJMoa1112302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sounni, N.E., Dehne K., van Kempen L., Egeblad M., Affara N.I., Cuevas I., Wiesen J., Junankar S., Korets L., Lee J., et al. 2010. Stromal regulation of vessel stability by MMP14 and TGFβ. Dis. Model. Mech. 3:317–332 10.1242/dmm.003863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sternlicht, M.D., Lochter A., Sympson C.J., Huey B., Rougier J.P., Gray J.W., Pinkel D., Bissell M.J., and Werb Z.. 1999. The stromal proteinase MMP3/stromelysin-1 promotes mammary carcinogenesis. Cell. 98:137–146 10.1016/S0092-8674(00)81009-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stetler-Stevenson, W.G., Aznavoorian S., and Liotta L.A.. 1993. Tumor cell interactions with the extracellular matrix during invasion and metastasis. Annu. Rev. Cell Biol. 9:541–573 10.1146/annurev.cb.09.110193.002545 [DOI] [PubMed] [Google Scholar]
- Stoker, M.G., Shearer M., and O’Neill C.. 1966. Growth inhibition of polyoma-transformed cells by contact with static normal fibroblasts. J. Cell Sci. 1:297–310 [DOI] [PubMed] [Google Scholar]
- Straussman, R., Morikawa T., Shee K., Barzily-Rokni M., Qian Z.R., Du J., Davis A., Mongare M.M., Gould J., Frederick D.T., et al. 2012. Tumour micro-environment elicits innate resistance to RAF inhibitors through HGF secretion. Nature. 487:500–504 10.1038/nature11183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strutz, F., Okada H., Lo C.W., Danoff T., Carone R.L., Tomaszewski J.E., and Neilson E.G.. 1995. Identification and characterization of a fibroblast marker: FSP1. J. Cell Biol. 130:393–405 10.1083/jcb.130.2.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strutz, F., Zeisberg M., Hemmerlein B., Sattler B., Hummel K., Becker V., and Müller G.A.. 2000. Basic fibroblast growth factor expression is increased in human renal fibrogenesis and may mediate autocrine fibroblast proliferation. Kidney Int. 57:1521–1538 10.1046/j.1523-1755.2000.00997.x [DOI] [PubMed] [Google Scholar]
- Sugimoto, H., Mundel T.M., Kieran M.W., and Kalluri R.. 2006. Identification of fibroblast heterogeneity in the tumor microenvironment. Cancer Biol. Ther. 5:1640–1646 10.4161/cbt.5.12.3354 [DOI] [PubMed] [Google Scholar]
- Sun, Y., Campisi J., Higano C., Beer T.M., Porter P., Coleman I., True L., and Nelson P.S.. 2012. Treatment-induced damage to the tumor microenvironment promotes prostate cancer therapy resistance through WNT16B. Nat. Med. 18:1359–1368 10.1038/nm.2890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher, B.A., Herman T.S., Holden S.A., Wang Y.Y., Pfeffer M.R., Crawford J.W., and Frei E. III. 1990. Tumor resistance to alkylating agents conferred by mechanisms operative only in vivo. Science. 247:1457–1461 10.1126/science.2108497 [DOI] [PubMed] [Google Scholar]
- Thayer, S.P., di Magliano M.P., Heiser P.W., Nielsen C.M., Roberts D.J., Lauwers G.Y., Qi Y.P., Gysin S., Fernández-del Castillo C., Yajnik V., et al. 2003. Hedgehog is an early and late mediator of pancreatic cancer tumorigenesis. Nature. 425:851–856 10.1038/nature02009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomasek, J.J., Gabbiani G., Hinz B., Chaponnier C., and Brown R.A.. 2002. Myofibroblasts and mechano-regulation of connective tissue remodelling. Nat. Rev. Mol. Cell Biol. 3:349–363 10.1038/nrm809 [DOI] [PubMed] [Google Scholar]
- Torres, S., Bartolomé R.A., Mendes M., Barderas R., Fernandez-Aceñero M.J., Peláez-García A., Peña C., Lopez-Lucendo M., Villar-Vázquez R., de Herreros A.G., et al. 2013. Proteome profiling of cancer-associated fibroblasts identifies novel proinflammatory signatures and prognostic markers for colorectal cancer. Clin. Cancer Res. 19:6006–6019 10.1158/1078-0432.CCR-13-1130 [DOI] [PubMed] [Google Scholar]
- Toullec, A., Gerald D., Despouy G., Bourachot B., Cardon M., Lefort S., Richardson M., Rigaill G., Parrini M.C., Lucchesi C., et al. 2010. Oxidative stress promotes myofibroblast differentiation and tumour spreading. EMBO Mol. Med. 2:211–230 10.1002/emmm.201000073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trimboli, A.J., Cantemir-Stone C.Z., Li F., Wallace J.A., Merchant A., Creasap N., Thompson J.C., Caserta E., Wang H., Chong J.L., et al. 2009. Pten in stromal fibroblasts suppresses mammary epithelial tumours. Nature. 461:1084–1091 10.1038/nature08486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsujino, T., Seshimo I., Yamamoto H., Ngan C.Y., Ezumi K., Takemasa I., Ikeda M., Sekimoto M., Matsuura N., and Monden M.. 2007. Stromal myofibroblasts predict disease recurrence for colorectal cancer. Clin. Cancer Res. 13:2082–2090 10.1158/1078-0432.CCR-06-2191 [DOI] [PubMed] [Google Scholar]
- Vermeulen, L., De Sousa E Melo F., van der Heijden M., Cameron K., de Jong J.H., Borovski T., Tuynman J.B., Todaro M., Merz C., Rodermond H., et al. 2010. Wnt activity defines colon cancer stem cells and is regulated by the microenvironment. Nat. Cell Biol. 12:468–476 10.1038/ncb2048 [DOI] [PubMed] [Google Scholar]
- Vicent, S., Sayles L.C., Vaka D., Khatri P., Gevaert O., Chen R., Zheng Y., Gillespie A.K., Clarke N., Xu Y., et al. 2012. Cross-species functional analysis of cancer-associated fibroblasts identifies a critical role for CLCF1 and IL-6 in non-small cell lung cancer in vivo. Cancer Res. 72:5744–5756 10.1158/0008-5472.CAN-12-1097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Hoff, D.D., Ramanathan R.K., Borad M.J., Laheru D.A., Smith L.S., Wood T.E., Korn R.L., Desai N., Trieu V., Iglesias J.L., et al. 2011. Gemcitabine plus nab-paclitaxel is an active regimen in patients with advanced pancreatic cancer: a phase I/II trial. J. Clin. Oncol. 29:4548–4554 10.1200/JCO.2011.36.5742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vosseler, S., Lederle W., Airola K., Obermueller E., Fusenig N.E., and Mueller M.M.. 2009. Distinct progression-associated expression of tumor and stromal MMPs in HaCaT skin SCCs correlates with onset of invasion. Int. J. Cancer. 125:2296–2306 10.1002/ijc.24589 [DOI] [PubMed] [Google Scholar]
- Walter, K., Omura N., Hong S.M., Griffith M., and Goggins M.. 2008. Pancreatic cancer associated fibroblasts display normal allelotypes. Cancer Biol. Ther. 7:882–888 10.4161/cbt.7.6.5869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, X.M., Yu D.M., McCaughan G.W., and Gorrell M.D.. 2005. Fibroblast activation protein increases apoptosis, cell adhesion, and migration by the LX-2 human stellate cell line. Hepatology. 42:935–945 10.1002/hep.20853 [DOI] [PubMed] [Google Scholar]
- Wang, Z., Ma Q., Liu Q., Yu H., Zhao L., Shen S., and Yao J.. 2008. Blockade of SDF-1/CXCR4 signalling inhibits pancreatic cancer progression in vitro via inactivation of canonical Wnt pathway. Br. J. Cancer. 99:1695–1703 10.1038/sj.bjc.6604745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, W., Li Q., Yamada T., Matsumoto K., Matsumoto I., Oda M., Watanabe G., Kayano Y., Nishioka Y., Sone S., and Yano S.. 2009a. Crosstalk to stromal fibroblasts induces resistance of lung cancer to epidermal growth factor receptor tyrosine kinase inhibitors. Clin. Cancer Res. 15:6630–6638 10.1158/1078-0432.CCR-09-1001 [DOI] [PubMed] [Google Scholar]
- Wang, Z., Li Y., Kong D., Banerjee S., Ahmad A., Azmi A.S., Ali S., Abbruzzese J.L., Gallick G.E., and Sarkar F.H.. 2009b. Acquisition of epithelial-mesenchymal transition phenotype of gemcitabine-resistant pancreatic cancer cells is linked with activation of the notch signaling pathway. Cancer Res. 69:2400–2407 10.1158/0008-5472.CAN-08-4312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, J., Ying G., Wang J., Jung Y., Lu J., Zhu J., Pienta K.J., and Taichman R.S.. 2010. Characterization of phosphoglycerate kinase-1 expression of stromal cells derived from tumor microenvironment in prostate cancer progression. Cancer Res. 70:471–480 10.1158/0008-5472.CAN-09-2863 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Webber, J., Steadman R., Mason M.D., Tabi Z., and Clayton A.. 2010. Cancer exosomes trigger fibroblast to myofibroblast differentiation. Cancer Res. 70:9621–9630 10.1158/0008-5472.CAN-10-1722 [DOI] [PubMed] [Google Scholar]
- Weissmueller, S., Manchado E., Saborowski M., Morris J.P. IV, Wagenblast E., Davis C.A., Moon S.H., Pfister N.T., Tschaharganeh D.F., Kitzing T., et al. 2014. Mutant p53 drives pancreatic cancer metastasis through cell-autonomous PDGF receptor β signaling. Cell. 157:382–394 10.1016/j.cell.2014.01.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen, J., Matsumoto K., Taniura N., Tomioka D., and Nakamura T.. 2004. Hepatic gene expression of NK4, an HGF-antagonist/angiogenesis inhibitor, suppresses liver metastasis and invasive growth of colon cancer in mice. Cancer Gene Ther. 11:419–430 10.1038/sj.cgt.7700705 [DOI] [PubMed] [Google Scholar]
- Wendling, O., Bornert J.M., Chambon P., and Metzger D.. 2009. Efficient temporally-controlled targeted mutagenesis in smooth muscle cells of the adult mouse. Genesis. 47:14–18 10.1002/dvg.20448 [DOI] [PubMed] [Google Scholar]
- Williams, C.S., Tsujii M., Reese J., Dey S.K., and DuBois R.N.. 2000. Host cyclooxygenase-2 modulates carcinoma growth. J. Clin. Invest. 105:1589–1594 10.1172/JCI9621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson, T.R., Fridlyand J., Yan Y., Penuel E., Burton L., Chan E., Peng J., Lin E., Wang Y., Sosman J., et al. 2012. Widespread potential for growth-factor-driven resistance to anticancer kinase inhibitors. Nature. 487:505–509 10.1038/nature11249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewicz, A.K., Whitaker-Menezes D., Dasgupta A., Philp N.J., Lin Z., Gandara R., Sneddon S., Martinez-Outschoorn U.E., Sotgia F., and Lisanti M.P.. 2012. Using the “reverse Warburg effect” to identify high-risk breast cancer patients: stromal MCT4 predicts poor clinical outcome in triple-negative breast cancers. Cell Cycle. 11:1108–1117 10.4161/cc.11.6.19530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xing, F., Saidou J., and Watabe K.. 2010. Cancer associated fibroblasts (CAFs) in tumor microenvironment. Front Biosci (Landmark Ed). 15:166–179 10.2741/3613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, Z., Vonlaufen A., Phillips P.A., Fiala-Beer E., Zhang X., Yang L., Biankin A.V., Goldstein D., Pirola R.C., Wilson J.S., and Apte M.V.. 2010. Role of pancreatic stellate cells in pancreatic cancer metastasis. Am. J. Pathol. 177:2585–2596 10.2353/ajpath.2010.090899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, F., Tuxhorn J.A., Ressler S.J., McAlhany S.J., Dang T.D., and Rowley D.R.. 2005. Stromal expression of connective tissue growth factor promotes angiogenesis and prostate cancer tumorigenesis. Cancer Res. 65:8887–8895 10.1158/0008-5472.CAN-05-1702 [DOI] [PubMed] [Google Scholar]
- Yang, G., Rosen D.G., Zhang Z., Bast R.C. Jr, Mills G.B., Colacino J.A., Mercado-Uribe I., and Liu J.. 2006. The chemokine growth-regulated oncogene 1 (Gro-1) links RAS signaling to the senescence of stromal fibroblasts and ovarian tumorigenesis. Proc. Natl. Acad. Sci. USA. 103:16472–16477 10.1073/pnas.0605752103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yauch, R.L., Gould S.E., Scales S.J., Tang T., Tian H., Ahn C.P., Marshall D., Fu L., Januario T., Kallop D., et al. 2008. A paracrine requirement for hedgehog signalling in cancer. Nature. 455:406–410 10.1038/nature07275 [DOI] [PubMed] [Google Scholar]
- Yin, C., Evason K.J., Asahina K., and Stainier D.Y.. 2013. Hepatic stellate cells in liver development, regeneration, and cancer. J. Clin. Invest. 123:1902–1910 10.1172/JCI66369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeisberg, E.M., Potenta S., Xie L., Zeisberg M., and Kalluri R.. 2007. Discovery of endothelial to mesenchymal transition as a source for carcinoma-associated fibroblasts. Cancer Res. 67:10123–10128 10.1158/0008-5472.CAN-07-3127 [DOI] [PubMed] [Google Scholar]
- Zhang, J., Chen L., Liu X., Kammertoens T., Blankenstein T., and Qin Z.. 2013a. Fibroblast-specific protein 1/S100A4-positive cells prevent carcinoma through collagen production and encapsulation of carcinogens. Cancer Res. 73:2770–2781 10.1158/0008-5472.CAN-12-3022 [DOI] [PubMed] [Google Scholar]
- Zhang, X.H., Jin X., Malladi S., Zou Y., Wen Y.H., Brogi E., Smid M., Foekens J.A., and Massagué J.. 2013b. Selection of bone metastasis seeds by mesenchymal signals in the primary tumor stroma. Cell. 154:1060–1073 10.1016/j.cell.2013.07.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigrino, P., Kuhn I., Bäuerle T., Zamek J., Fox J.W., Neumann S., Licht A., Schorpp-Kistner M., Angel P., and Mauch C.. 2009. Stromal expression of MMP-13 is required for melanoma invasion and metastasis. J. Invest. Dermatol. 129:2686–2693 10.1038/jid.2009.130 [DOI] [PubMed] [Google Scholar]