Abstract
In recent years, medical guidelines for communicating bad news to patients have been published. Training for this task was included in the curricula of undergraduate medical courses, specialization, and continuing medical education. The objective of this review is to evaluate the existing evidence in the literature on the effectiveness of such training. Only seven controlled trials were found, four of which were randomized, and these four indicate an improvement in the trainees. These findings suggest that training undergraduate and postgraduate doctors in skills for communicating bad news may be beneficial but there are important limitations to reach a definitive conclusion. These limitations are discussed in this article.
Keywords: Bad news, communication skills, medical education, physician-patient relations
INTRODUCTION
Even though delivering bad news is something that occurs daily in most medical practice, the majority of clinicians has not received formal training for this essential and important communication, and would consider this as an extremely difficult task.[1] The term ‘bad news’ refers to any information transmitted to patients or their families that directly or indirectly involves a negative change in their lives. As breaking bad news is a stressful task, many physicians either avoid it or perform it inadequately because it “results in a cognitive, behavioral, or emotional deficit in the person receiving the news that persists for some time after the news is received.”[2]
Physicians used to believe that disclosure of bad news would cause anguish, threatening to cripple the preservation of any hope for patients, justifying thus the concealment of bad news.[3] However, since the second half of the last century, patients, physicians, and the general public started to communicate the diagnostic and prognostic aspects with a more open and clearer approach.[4]
Interactions in which bad news is discussed are admittedly distressing for doctors, patients, and their families. The way the diagnosis of serious diseases, like cancer, is communicated can have a significant impact not only on the perceptions of patients about their disease, but also on the long-term relationship with their physician.[5]
When medical residents were evaluated using an instrument regarding the skills considered necessary for giving bad news in a caring and informative manner, they showed a general lack of competence in its delivery, representing barriers to interactions with patients. Part of this problem is associated with self-fears, lack of support from supervisors, and time constraint.[6] Another thing to note is that many fail because they do not consider the perspectives and expectations of the patient.[7,8]
Although the length of professional experience enhances medical fitness to communicate bad news,[9] a considerable proportion of experienced doctors still feel insufficiently instructed on how to perform this task.[10] Surveys show that most medical experts believe that training programs are useful in this practice.[1,11]
To address this problem, researchers investigated the experiences and wishes of health professionals, patients, and their families,[12] and developed guidelines for interactions in the oncology setting.[13,14] These guidelines divide the interaction basically into three steps: (a) Preparation for communication of the news, establishing personal contact, and the degree of knowledge of the patients regarding the diagnosis and extent of the information they want to receive (b) the information itself, with appropriate language and rhythm, and (c) an empathic response to the reaction of the patient. Besides guiding the verbal content that should be expressed, the guidelines take into account the nonverbal impact of the quality of communication.[15]
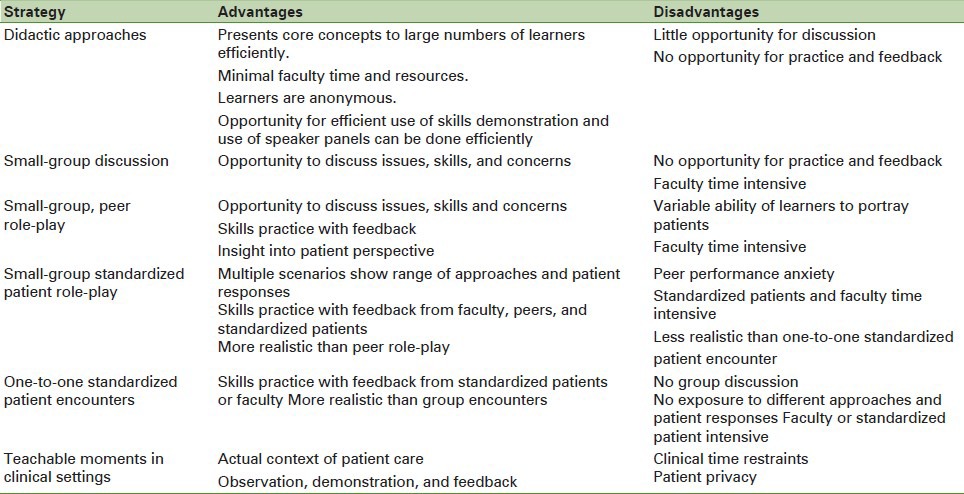
Based on the premise that communication skills can be taught,[16] different educational strategies for medical students and physicians were developed.[17] These strategies include didactic lectures, small-group discussions, practical individual or group performance with simulated patients, and teaching moments during clinical care. Each of these modalities has potential advantages and disadvantages, as shown in Table 1.
Table 1.
Advantages and disadvantages of strategies for teaching communication of bad news for students and residents
A survey with hematology/oncology fellowship program directors in the United States showed that 63% of the program directors felt that extensive, formal training is important for skill development in delivering bad news, and 23% received moderate to extensive training.[18] Although this training will become a consistent part of medical education, there are few data to demonstrate the effectiveness of such training programs.[19]
The objective of this review was to determine the existing evidence in the literature on the effectiveness of the training of doctors and medical students to communicate bad news.
MATERIALS AND METHODS
We reviewed the databases PubMed, LILACS, and SciELO with the following: ’ Medical education ’ or ‘medical oncology/education’ and ‘physician-patient relations’ or ‘communication’ and ‘truth disclosure’ or ‘bad news’ or ‘diagnosis’ or ‘prognosis’ or ‘reveal’ or ‘revelation’ or ‘fatal’ or ‘death’ or ‘end of life’ or ‘unfavorable’, using the limiter ‘clinical trials’. The publication period was extended until August 30, 2011, with unlimited start date and no language restriction.
Based on this search, we selected for analysis only controlled trials on the training of medical students or doctors, specific to the communication of bad news, for the diagnoses of life-threatening diseases such as cancer or severely debilitating diseases like neurodegenerative diseases, or changing the prognosis from therapeutic to palliative care. Clinical trials evaluating the efficacy of medical training in communication in general were not considered for this analysis.
RESULTS
Of the 85 trials identified, only seven matched the inclusion criteria defined for this review, all of which were published in the last 10 years. Their characteristics are shown in Table 2.[20,21,22,23,24,25,26]
Table 2.
Characteristics of trails
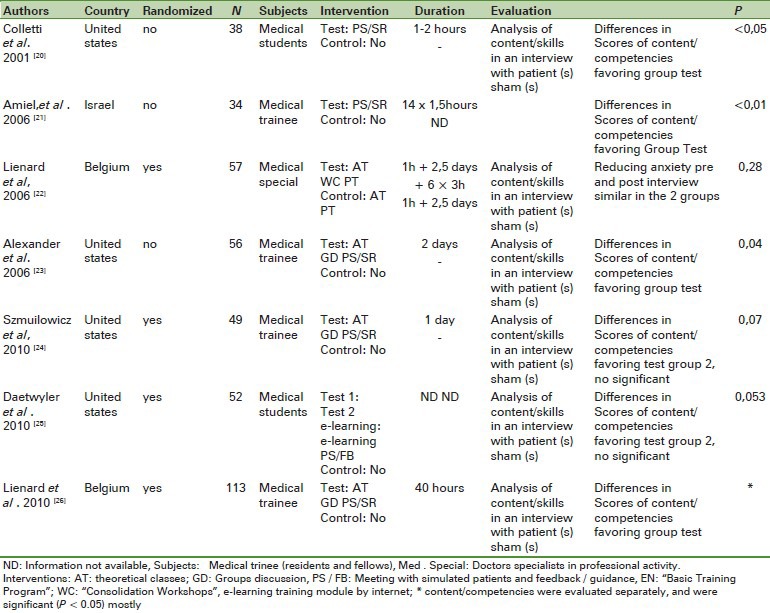
The methods of training conducted and the content, duration, and extension were considerably different in each study. Furthermore, in two studies,[21,22] the control groups were also interventional. One study[25] used Internet communication for training and assessment from a distance.
The questionnaires or scoring systems used to evaluate the performance of each research subject were unique to each study, constructed on different guidelines for reporting bad news based on existing and/or previous experience in each research group. Only in one study, used Internet communication for training and assessment from a distance.
The questionnaires or scoring systems used to evaluate the performance of each research subject were unique to each study, constructed on different guidelines for reporting bad news based on existing and/or previous experience in each research group. Only in one study,[22] the outcome assessed was related to patient interviews (State Trait Anxiety Inventory before and after a consultation.
Concerning the aspect of evaluation, different strategies were used. In three studies,[20,21,25] simulated patients were responsible for filling out questionnaires evaluating content and skills of the interviewer. In two studies,[23,24] this task fell upon two external evaluators, and in another,[26] a software content analysis of the transcripts was used, powered by dictionaries built specifically for this purpose. In all studies, the assessors were blinded as to the group each subject belonged to.
Four of the seven studies showed significant differences favoring groups that conducted the training (or had more extensive training in cases of interventional studies with controls). When only the randomized studies are considered, only one of four studies[26] revealed outcomes that favored the trained group. However, in two of them,[24,25] it was found that the test group showed a better performance close to statistical significance.
DISCUSSION
From the formulation and publication of guidelines for the communicating of bad news, various forms of training for this task became part of the curricula of various undergraduate courses in medicine, residency training, and continuing medical education. The training strategies are varied and often resource- and time-intensive for educators;[17] there are many models for teaching skills for delivering bad news, and the choice depends on resources available in terms of faculty, Standerdized patients, and curricular time. The availability of new technologies based on the Internet can reduce cost and increase the applicability of these training programs.[25]
Although previous studies have shown that such training programs provided satisfaction to students and participating physicians and enhanced their confidence to communicate bad news,[27,28,29] this review shows that few studies were adequately designed to evaluate the effectiveness of these training programs.
Of the seven controlled trials, four groups showed willingness to undergo training. In two randomized trials, there was a nonsignificant trend in favor of the intervention group. As in the previous studies there was no formal calculation of sample size, it is possible that they did not have sufficient power to detect differences. variation in training methods and evaluation groups between studies also limits the analysis of data. Another limitation of existing studies is that analyzing the outcomes after the completion of training does not permit evaluation of the ability of physicians to retain the learning of long-term skills. Similar limitations occur when investigating the evidence on the effectiveness of general medical training in communication, as evidenced by systematic reviews.[30]
Although the focus of the guidelines for communicating bad news is ultimately to reduce anxiety and improve understanding and patient adherence,[24] all trials assessed here, with one exception-and most trials were not controlled-had as the main outcome, changes in behavior of medical students. The only randomized controlled trial that evaluated the reduction in anxiety score of the patients failed to show benefits of training.[21] The scarcity of trials evaluating outcomes related to patients is most likely related to the difficulties in planning and executing such trials.
CONCLUSION
This review shows that there is concern about the quality of communication of bad news to the patient, but could not conclude unequivocally that training of medical students and resident physicians can be beneficial for them to acquire the skills deemed necessary.
Finally, one must consider that there are differences in the forms of verbal and nonverbal communication between different cultures and, therefore, conducting controlled studies at local, national, and international levels is highly encouraged.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Barnett MM, Fisher JD, Cooke H, James PR, Dale J. Breaking bad news: Consultants’ experien ce, previous education and views on educational format and timing. Med Educ. 2007;41:947–56. doi: 10.1111/j.1365-2923.2007.02832.x. [DOI] [PubMed] [Google Scholar]
- 2.Lino AC, Augusto KL, Oliveira RA, Feitosa LB, Caprara A. Using the Spikes protocol to teach skills in breaking bad news. Rev Bras Med Educ. 2011;35:52–7. [Google Scholar]
- 3.Reiser SJ. Words those Scalpels: Words as scalpels: Transmitting evidence in the clinical dialogue. Ann Intern Med. 1980;92:837–42. doi: 10.7326/0003-4819-92-6-837. [DOI] [PubMed] [Google Scholar]
- 4.Charlton RC. Breaking bad news. Med J Aust. 1992;157:615–21. doi: 10.5694/j.1326-5377.1992.tb137405.x. [DOI] [PubMed] [Google Scholar]
- 5.Maguire P. Breaking bad news. Eur J Surg Oncol. 1998;24:188–91. doi: 10.1016/s0748-7983(98)92929-8. [DOI] [PubMed] [Google Scholar]
- 6.Eggly S, Afonso N, Rojas G, Baker M, Cardozo L, Robertson RS. An assessment of residents’ competence in the delivery of bad news to patients. Acad Med. 1997;72:397–9. doi: 10.1097/00001888-199705000-00023. [DOI] [PubMed] [Google Scholar]
- 7.Maguire P, Fairbairn S, Fletcher C. Consultation skills of young doctors: II-Most young doctors are bad at giving information. Br Med J (Clin Res Ed) 1986;292:1576–8. doi: 10.1136/bmj.292.6535.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dosanjh S, Barnes J, Bhandari M. Barriers to breaking bad news among medical and surgical residents. Med Educ. 2001;35:197–205. doi: 10.1046/j.1365-2923.2001.00766.x. [DOI] [PubMed] [Google Scholar]
- 9.Dickinson GE, Tournier RE. A decade beyond medical school: A longitudinal study of physicians’ attitudes Toward death and terminally-ill patients. Soc Med Sci. 1994;38:1397–400. doi: 10.1016/0277-9536(94)90277-1. [DOI] [PubMed] [Google Scholar]
- 10.Orgel E, McCarter R, Jacobs S. A failing medical educational model: A self-assessment by physicians at all levels of training of ability and comfort to deliver bad news. Palliat Med J. 2010;13:677–83. doi: 10.1089/jpm.2009.0338. [DOI] [PubMed] [Google Scholar]
- 11.Costantini A, Baile WF, Lenzi R, Costantini M, Ziparo V, Marchetti P, et al. Overcoming cultural barriers to giving bad news: Feasibility of training to promote truth-telling to cancer patients. J Cancer Educ. 2009;24:180–5. doi: 10.1080/08858190902876262. [DOI] [PubMed] [Google Scholar]
- 12.Fallowfield L, Jenkins V. Communicating sad, bad, and difficult news in medicine. Lancet. 2004;363:312–9. doi: 10.1016/S0140-6736(03)15392-5. [DOI] [PubMed] [Google Scholar]
- 13.Girgis A, Sanson-Fisher RW. Breaking bad news: Consensus guidelines for medical practitioners. J Clin Oncol. 1995;13:2449–56. doi: 10.1200/JCO.1995.13.9.2449. [DOI] [PubMed] [Google Scholar]
- 14.Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES: A six-step protocol for delivering bad news-Application to the patient with cancer. Oncologist. 2000;5:302–11. doi: 10.1634/theoncologist.5-4-302. [DOI] [PubMed] [Google Scholar]
- 15.Rossi L, Lima CC, Queiroz IN, Froes SS, Caldeira AP. The perception of patients about non-verbal communication in healthcare. Rev Bras Med Ed. 2010;34:363–70. [Google Scholar]
- 16.Turini B, Martins ND, Tavares MS, Nunes SO, Silva VL, Thomson Z. Communication in medical education: Experience, structuring and new challenges in medical curricula. R Rev Bras Med Ed. 2008;32:264–70. [Google Scholar]
- 17.Rosenbaum ME, Ferguson KJ, Wolves JG. Teaching medical students and residents skills for delivering bad news: A review of strategies. Acad Med. 2004;79:107–17. doi: 10.1097/00001888-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Hebert HD, Butera JN, Castillo J, Mega AE. Are we training our fellows adequately in delivering bad news to patients? A survey of hematology/oncology program directors. Palliat Med J. 2009;12:1119–24. doi: 10.1089/jpm.2009.0074. [DOI] [PubMed] [Google Scholar]
- 19.Wittenberg-Lyles EM, Goldsmith J, Sanchez-Reilly S, Ragan SL. Communicating a terminal prognosis in a palliative care setting: Deficiencies in current communication training protocols. Soc Sci Med. 2008;66:2356–65. doi: 10.1016/j.socscimed.2008.01.042. [DOI] [PubMed] [Google Scholar]
- 20.Colletti L, Gruppen L, Barclay M, Stern D. Teaching students to break bad news. Am J Surg. 2001;182:20–3. doi: 10.1016/s0002-9610(01)00651-1. [DOI] [PubMed] [Google Scholar]
- 21.Amiel GE, Ungar L, Alperin M, Baharier Z, Cohen R, Reis S. Ability of primary care physician's to break bad news: A performance based assessment of an educational intervention. Patient Educ Couns. 2006;60:10–5. doi: 10.1016/j.pec.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 22.Lienard A, Merckaert I, Libert Y, Delvaux N, Marchal S, Boniver J, et al. Factors That Influence cancer patients’ anxiety Following the medical consultation: Impact of a communication skills training program for physicians. Ann Oncol. 2006;17:1450–8. doi: 10.1093/annonc/mdl142. [DOI] [PubMed] [Google Scholar]
- 23.Alexander SC, Keitz SA, Sloane R, Tulsky JA. A controlled trial of a short course to Improve residents’ communication with pacientes at the end of life. Acad Med. 2006;81:1008–12. doi: 10.1097/01.ACM.0000242580.83851.ad. [DOI] [PubMed] [Google Scholar]
- 24.Szmuilowicz E, el-Jawahri A, Chiappetta L, Kamdar M, Block S. Improving residents’ end-of-life communication skills with a short retreat: A randomized controlled trial. Palliat Med J. 2010;13:439–52. doi: 10.1089/jpm.2009.0262. [DOI] [PubMed] [Google Scholar]
- 25.Daetwyler CJ, Cohen DG, Gracely E, Novack DH. eLearning to Enhance physician patient communication: A pilot test of “doc.com” and “WebEncounter” in teaching bad news delivery. Med Teach. 2010;32:e381–90. doi: 10.3109/0142159X.2010.495759. [DOI] [PubMed] [Google Scholar]
- 26.Liénard A, Merckaert I, Libert Y, Bragard I, Delvaux N, Etienne AM, et al. Is it Possible to Improve residents breaking bad news skills? A randomized study Assessing the efficacy of a communication skills training program. Br J Cancer. 2010;103:171–7. doi: 10.1038/sj.bjc.6605749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cushing AM, Jones A. Evaluation of a breaking bad news course for medical students. Educ Med. 1995;29:430–5. doi: 10.1111/j.1365-2923.1995.tb02867.x. [DOI] [PubMed] [Google Scholar]
- 28.Garg A, Buckman R, Kason Y. Teaching medical students to break bad news. CMAJ. 1997;156:1159–64. [PMC free article] [PubMed] [Google Scholar]
- 29.Baile WF, Kudelka AP, Beale EA, Glober GA, Myers EG, Greisinger AJ, et al. Communication skills training in oncology. Description and preliminary outcomes of work-shops on breaking bad news and managing patient reactions to illness. Cancer. 1999;86:887–97. [PubMed] [Google Scholar]
- 30.Moore PM, Wilkinson SS, Rivera Mercado S. The Cochrane Library. 10. Communication skills training for health care professionals working with cancer patients, Their families and/or carers. Cochrane Database of Systematic Reviews. Article No. CD003751. [Google Scholar]


