Abstract
Background:
Although psychological factors are now recognized as playing a significant and independent role in the development of coronary heart disease (CHD) and its complications, many of these factors are correlated with each other. The present study is aimed at examining the association between alexithymia and anxiety depression, stress, quality of life, and social support in CHD patients.
Materials and Methods:
In this research 398 patients with coronary heart disease (166 females and 232 males) from the city of Isfahan were selected using random sampling. The tools used included depression, anxiety, and stress scale (DASS-21), Health-related to Quality Of Life (HRQOL-26), Multiple Scale Perceived Social Support (MSPSS-12), and the Toronto Alexithymia Scale (TAS-20). The data were analyzed using structural equation modeling by using the Statistical Package for Social Science (SPSS21) (IBM Corp: Armonk, New York.U.S.) and Asset Management Operating System (AMOS21) SPSS, an IBM Company: Chicago, U.S. Software.
Results:
Results of the structural equation model showed an acceptable goodness of fit, for the explanation alexithymia that was significantly associated with lower HRQOL and social support and increasing anxiety, depression, and stress.
Conclusions:
Alexithymia may increase anxiety, depression, and stress and can be a predisposing factor to poorer HRQOL and social support.
Keywords: Alexithymia, anxiety, coronary heart disease, depression, quality of life, social support, stress
INTRODUCTION
During the recent decade, a number of researchers have described the growing psychosocial risk factors for coronary heart disease (CHD), which include depression, anxiety, stress,[1,2,3] and alexithymia[4,5,6] that decrease the health-related quality of life[7,8,9,10,11] and protective factors such as social support.[12,13,14,15]
Substantial evidence shows a strong association between the psychological factors and risk of CHD. The role of depression, anxiety, and stress was confirmed through global research.[2,16,17,18] Studies carried out internationally highlight that besides negative psychological factors like depression, anxiety, and stress, positive factors such as social support play a protective role in the onset and progress of CHD.[19,20]
In 1973, Sifnoes proposed the term ‘alexithymia’ to imply a cognitive–affective disturbance, characteristic of persons who cannot describe their feelings or elaborate their fantasies. The term ‘alexithymia’ was originally defined as an inability to recognize and verbalize emotions. It has been characterized more generally as an emptiness of feeling,[21] a poverty of imagination or a life of fantasy,[22] difficulty in communicating with others,[21] and a lack of positive emotions with a high prevalence of negative emotions.[23] Alexithymia may influence somatic disease via physiological, behavioral, cognitive or social pathways.[24] Alexithymia is associated with states of negative affect.[25] which increase the possibility of somatic complaints.[24,26] The assumption is that these characteristics would lead to a deficiency in cognitive processing and regulation and adjustment of emotions, and are associated with starting and/or continuing some of the psychiatric and medical disorders.[27] Some researchers believe that dysfunction in the limbic system, brain abnormal lateralization, and/or difficulty in the efficiency of hemispheric communication are the causes of its emergence.[28]
The prevalence of alexithymia in working age populations has been shown to be about 9-17% for men and 5-10% for women.[29,30] At the population level, alexithymia is associated with older age, lower socioeconomic status, fewer years of education, single marital status, and poorer perceived health.[31,32] Alexithymia has been shown to be associated with several medical conditions and mental health problems.[33,34] An association between alexithymia and dissatisfaction with life has been found in some studies of coronary heart disease patients.[35]
One study investigated factors associated with alexithymia in patients (n = 153) with coronary heart disease verified by coronary angiography. In CHD patients, alexithymia was unrelated to cardiovascular diseases, but was related to depression and decreased life satisfaction.[36]
In the Kuopio Ischemic Heart Disease Risk-Factor Study, 2682 middle-aged men were studied using the 26-item Toronto Alexithymia Scale (TAS). High TAS scores were associated with a previous diagnosis of CHD. Alexithymia was associated with greater self-reporting of symptoms during exercise-tolerance testing and it was found that the extent of carotid atherosclerosis was inversely related to the degree of alexithymia, suggesting a biological connection to atherosclerosis.[37] In this study, the same group was followed for 5.5 years. Men in the highest alexithymia quintile were at a two-fold greater risk of death from any cause, while no association was found between behavioral or physiological risk factors and mortality.[38]
Kauhanen et al.[37] and Lumley et al.,[39] observed that the degree of alexithymia (TAS-20) was associated with the presence or absence of chest pain during exercise testing, but not with CHD (n = 180). They concluded that alexithymia was associated with an increased risk of illness-related behavior, but not necessarily with the presence or severity of CHD.
One study to testing the validity of existing conceptualizations of the alexithymia concept in the general adult population described that older adults engaged in less introspective thoughts, traditionally thought to denote increased alexithymia. Difficulty in identifying and describing emotions did not differentiate older and younger adults, but they were both associated with heightened depression, anxiety, and poor perceived quality of life.[40]
Alexithymia in somatoform and depressive disorders (2003) was investigated in one study (two groups of 30 subjects each, bearing diagnoses of somatoform disorder and depressive disorder, respectively, and one group of 30 normal controls) and the results showed that the mean of alexithymia scores in the somatoform (60.4) and depressive disorder groups (62.5) were higher than in normal subjects (54.2). Even as the total alexithymia scores did not differentiate somatoform from depressive disorders, the depressed subjects had greater difficulty in expressing their feelings.[41]
Bagby et al.,[42] reported a positive correlation between depression and alexithymia scores. Kauhanen et al.,[43] noted more physical symptom-reporting with high alexithymia, and Myers[44] observed alexithymia-elevated anxiety scores.
Linden et al., noted that high alexithymia showed smaller heart rate responses to the stress task and more anger in behavior.[45]
Mattila.et al. (2009) investigated the relationship between alexithymia and the health-related quality of life (HRQOL) in a nationally representative population sample of 5,418 subjects, of age 30 to 97 years, and concluded that alexithymia could be a predisposing factor to a poorer HRQOL.[5]
A study investigated the relationship between alexithymia and the health-related quality of life (HRQoL) and concluded that the alexithymic group had significantly (P < 0.001) lower mean scores on every dimension of HRQOL, even after controlling for confounding demographic variables, somatic diagnoses, and depressive and anxiety disorders. The differences were the greatest in the psychosocial domains.[46]
Several studies have also shown an association between alexithymia and sociocultural factors.[47] Alexithymia is also associated with poor social support or impaired relationships.[48]
MATERIALS AND METHODS
This research was a cross-sectional study that examined the causal relationship between alexithymia and DASS (depression, anxiety, stress), quality of life, and social support. The sample consisted of 398 CHD patients (166 females and 232 males and age: 40-70 years), who were randomly selected from the Isfahan Chamran Heart Center and Isfahan Cardiovascular Research Center (ICRC) (2013) and the Other Heart Clinical Center. The patients filled in five questionnaires assessing depression, anxiety, stress (DASS-21), alexithymia (TAS-20), health-related to quality of life (WHOQOL-26), multiple scale of perceived social support (MSPSS-12), and another questionnaire, which obtained demographic information. Before attending the study, each patient had been examined by a cardiologist, who had confirmed the diagnosis as coronary heart disease.
The questionnaires used were as follows:
1. Alexithymia-TAS-20 Scale: The TAS is a 20-item instrument[49] that is one of the most commonly used measures for alexithymia. The TAS-20 has three subscales:
1.1. - Difficulty Describing Feelings subscale (DDF) is used to measure the difficulty in describing emotions., which has five items: 2, 4, 7, 12, 17.
1.2. - Difficulty Identifying Feelings subscale (DIF) is used to measure the difficulty in identifying emotions., which has seven items: 1, 3, 6, 11, 9, 13, 14.
1.3. - Externally-Oriented Thinking subscale (EOT) is used to measure the tendency of individuals to focus their attention externally, which has eight items: 5, 8, 10, 15, 16, 18, 19, 20.
The items are rated using a five-point Likert scale whereby 1 = strongly disagree and 5 = strongly agree.
The total alexithymia score is the sum of responses to all the 20 items, while the score for each subscale factor is the sum of the responses to that subscale. The TAS-20 uses cutoff scoring: Equal to or less than 51 = non-alexithymia, equal to or greater than 61 = alexithymia. It demonstrates good internal consistency in the normal Iranian sample (Cronbach's alpha = 0.81) and test–retest reliability (0.77, P <0.01). The internal consistency reported in a clinical sample from Iran, using Cronbach's alpha for the total TAS-20 scale and subscales of DIF, DDF, and EOT, were. 79.,75.,71, and. 66, respectively, and the total validity using test–retesting for TAS-20 and its subscales DIF, DDF, and EOT were. 77.,73.,69., and 65, respectively.[50]
2-DASS scale-21: The DASS scale is a set of three self-report scales designed to measure the negative emotional states of depression, anxiety, and stress. The DASS should meet the requirements of both researchers and scientist-professional clinicians. Each of the three DASS scales contains seven items, divided into subscales of two to five items with a similar content.[51]
2.1. The Depression scale assesses dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest/involvement, anhedonia, and inertia.
2.2. The Anxiety scale assesses autonomic arousal, skeletal muscle effects, situational anxiety, and subjective experience of anxious affect.
2.3. The Stress scale is sensitive to levels of chronic non-specific arousal. It assesses difficulty in relaxing, nervous arousal, and being easily upset/agitated, irritable/over-reactive and impatient.
Subjects are asked to use the four-point severity/frequency scales to rate the extent to which they have experienced each state over the past week. Scores for Depression, Anxiety, and Stress are calculated by summing the scores for the relevant items. The assumption on which the DASS development has been based (and which has been confirmed by the research data) is that the differences between depression, anxiety, and stress experienced by normal subjects and the clinically disturbed, are essentially differences of degrees. The validity and reliability of this scale was reviewed by Samani and joker[52] (2007), who reported that reliabilities for depression, anxiety, and stress scale were. 80.,76.,77 and the Cronbach's alpha was. 81.,74.,78 for each, respectively.
3. Multiple Scale Perceived social support: The 12-question Multidimensional Scale of Perceived Social Support (MSPSS)[53] was used to measure the degree of social support each participant felt he or she had. High levels of perceived social support are generally associated with low levels of depression and anxiety. This self-report scale has three subscales (1. Family; 2. Friends; 3. Significant others) based on the seven-point Likert measures, which measures the respondents’ perceptions of the availability of various types of social support such as family, friends, and significant others. The reliability of this measure was high (a =0.92).
4. WHOQOL-26 questionnaire: The WHOQOL is a self-reporting questionnaire. The study participants could answer the questions on their own. The instrument consisted of 26 broad and comprehensive questions.
The remaining 24 items comprise four dimensions of health including, physical, psychological, social, and environmental. All scores are transformed to reflect 4-20 for each domain, with the higher scores corresponding to a better QOL. The individual's perception of quality of life is measured by summing the total scores for each particular domain. All domain scores are scaled in a positive direction (higher score indicates a higher QOL). This questionnaire was standardized on a sample of 2,956 healthy and 2,936 unhealthy rural and urban inhabitants (age 30 years and above) from Isfahan, Najaf-Abad, and Arak, who participated in the ‘Isfahan Healthy Heart Program’ (IHHP) from two dissimilar Iranian provinces, during 2006.[9]
5. Demographic questionnaire: This questionnaire consists of questions about age, sex, marital status, education, and so on.
RESULTS
Table 1 shows the patients’ sociodemographic characteristics based on age, sex, marital status, and education.
Table 1.
Patients’ sociodemographic characteristics (n = 398)
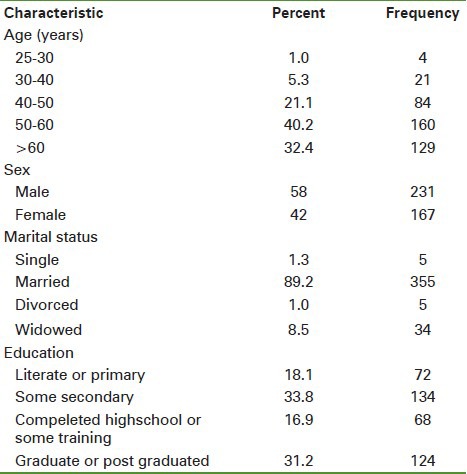
Table 2 shows Patients’ Descriptive characteristics such as Mean and Standard deviation.
Table 2.
Patients’ descriptive characteristics
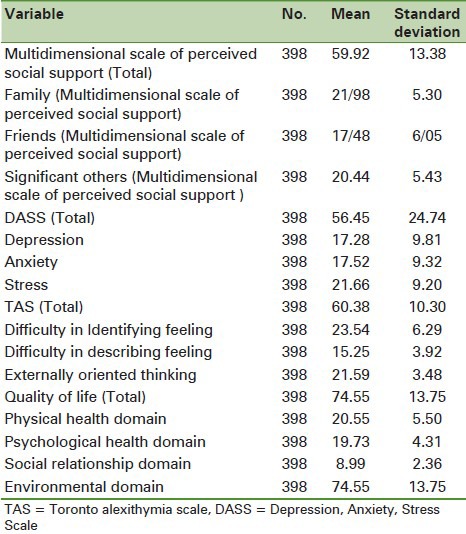
Cronbach's alpha was calculated as 0.74 for the Toronto Alexithymia Scale (TAS), 0.89 for the Depression, Anxiety, and Stress Scale (DASS), 0.87 for the Multidimensional Scale of Perceived Social Support (MSPSS), and 0.90 for the World Health Organization Quality of Life Questionnaire (WHOQOL).
Structural model to explain Alexithymia
Based on the conceptual model [Figure 1] of the study, the structural model of variables (i.e., TAS, DASS, MSPSS, and WHOQOL scores) was presented using the outputs of AMOS. Although in traditional statistical methods, the researcher uses a single measure to verify the null hypothesis, the complexity of the structural equation modeling eliminates this single measure. Therefore, three main groups of indices (Absolute fit, comparative fit, and parsimonious fit indices) are used to fit a model.[54]
Figure 1.
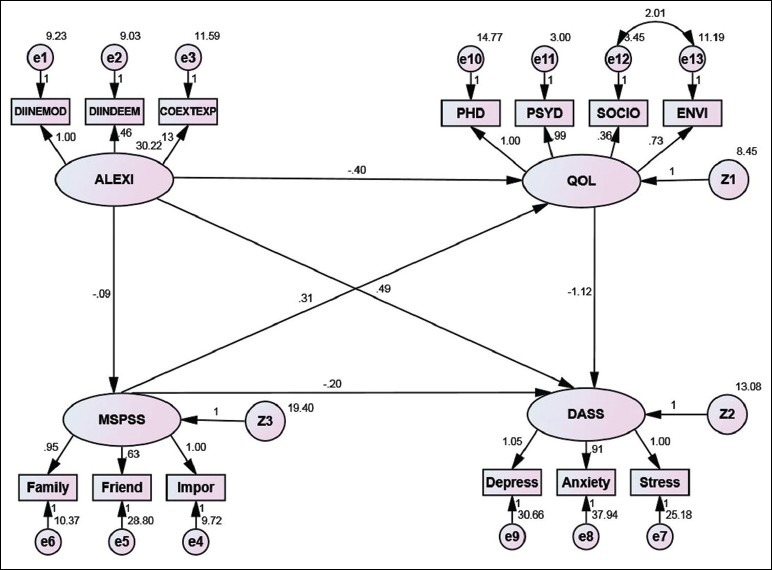
The conceptual model of Alexithymia
According to Table 3 [relative Chi-square (CMIN/df) =2.580 and df = 58 for default model], the model fitted well. Even as most experts consider relative Chi-square values of 2-3 to show a good fitting model, Schumacher and Lomax expanded the range to 1-5.[54]
Table 3.
Chi-square (CMIN) values and number of parameters
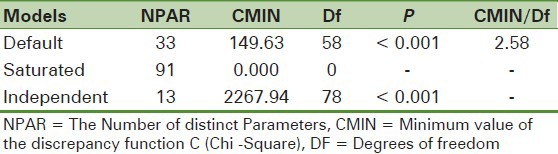
Table 4 shows the absolute fit indices. Goodness of fit index (GFI = 0.94) and adjusted goodness of fit index (AGFI = 0.91) suggested good fitting of the default model (values between 0 and 1 for these two indices indicate good fitting). However, evaluation of other indices seemed necessary.
Table 4.
Absolute fit indices
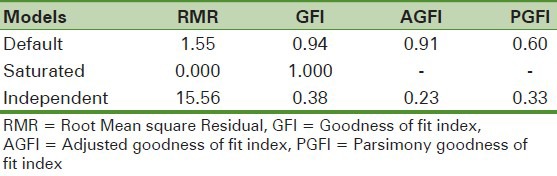
Table 5 shows the comparative fit index (CFI), parsimony comparative fit index (PCFI), and root mean square error of approximation (RMSEA). As is seen, the calculated values (CFI = 0.96 and PCFI = 0.71) suggest a good fit for the default model (CFI > 0.90 and PCFI > 0.50 are favorable). RMSEA can be calculated for confidence intervals, to determine the significance of the difference between the obtained value for the model and zero. As RMSEA < 0.08 is acceptable, our default model fitted well (RMSEA = 0.06). In addition, the Holter index of 204 was again indicative of a well-fitting model.[54]
Table 5.
Comparative and parsimonious fit indices
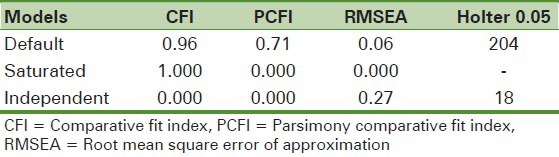
According to all the mentioned indicators, the default model presented a good fit for the relationship between alexithymia and depression, anxiety, stress, quality of life, and social support.
DISCUSSION
Alexithymia, a condition of inability to use words to understand the emotional states of oneself or others, prevents individuals from adjusting to their emotions. The present study has examined the predictive value of alexithymia in changes in depression, anxiety, stress, social support, and quality of life among patients with coronary heart disease. After fitting all the data, alexithymia shows significant positive relationships with depression, anxiety, and stress, as previous research has described.[40,41,42]
In other words, increasing levels of alexithymia and its two dimensions would worsen depression and anxiety in patients. The results of this study are consistent with previous studies on depression and anxiety. Sarrijarri[55] has shown that exacerbation of depressive symptoms will cause difficulty in identifying, describing, and sharing their feelings with others. Similarly, research has shown that alexithymia is more common in people with anxiety disorders and that anxiety is related to the two mentioned aspects of alexithymia.[56]
Alexithymia is a cognitive-emotional disorder that impairs the adjustment of emotions, concentration, processing, and evaluation of cognitive-emotional information. Therefore, individuals with alexithymia fail to manage their cognitive-emotional system and properly deal with stressful situations, particularly diseases. This strengthens the feelings of inadequacy and insufficiency in this group and intensifies negative emotions such as anxiety and depression.[57] Moreover, since emotional arousal is associated with physiological arousal, negative emotions (e.g. anxiety and depression) will bring about physical symptoms including pain, fatigue, and dizziness. Physical symptoms will in turn increase the negative emotions. Finally, disruption of psychological defenses in subjects with alexithymia leads them to deny their emotions and makes them incapable of describing them.
We also found difficulty in identifying feelings and difficulty in describing feelings to be related to depression and anxiety. Previous studies have reported comparable results. Matn and Jenakar[57] suggested difficulty in identifying feelings as the only aspect of alexithymia that predicts depressive symptoms. Furthermore, they reported difficulty in both identifying and describing feelings as predictors of anxiety symptoms.
Our findings confirmed a relationship between alexithymia and stress. Previous studies have indicated consistent results in terms of the relationship between alexithymia and stress and inadequacy of coping styles with stress.[58] This finding can be justified by considering the poor emotional intelligence of people with alexithymia, which combines with difficulties in identifying and describing feelings and reduces the ability of dealing with stressful situations. As the inability to cope with difficult situations imposes a lot of stress on the individual, a positive relationship exists between alexithymia and stress.[58]
Another finding of this study was the negative relationship between alexithymia and social support and its aspects, that is, increasing alexithymia decreases social support. In fact, patients with alexithymia cannot receive adequate social support from their family, friends, and/or significant others. Seemingly, impaired emotional intelligence in these individuals results in their poor interpersonal skills and inability to receive social support.[59]
The relationship between alexithymia and quality of life was also investigated in this study. The results indicated that there is a negative relationship between alexithymia and quality of life. The strongest relationships were identified between difficulty in identifying feelings and psychological aspect of the quality of life (r = - 0.48; P < 0.01), physical aspect of quality of life (r = - 0.43; P < 0.01), social aspect of quality of life (r = - 0.34; P < 0.01), and environmental aspect of quality of life (r = -0.24; P < 0.01). Similar relationships were suggested by a previous research.[60,61,62] Available evidence about the association between the difficulty in identifying feelings and somatoform disorder can explain the negative effects of alexithymia on the quality of life. It also seems that difficulty in identifying feelings results in a false interpretation of physical feelings and decreases the health-related quality of life. In other words, alexithymia is not only an inner state, but is also associated with health outcomes. Research has shown that people with alexithymia do not use normal coping styles, and may hence, have a higher tendency toward unhealthy behaviors such as suppression of emotions and drinking.[63]
Alexithymia can also increase the risk of death. Patients might experience problems in different aspects of life, that is, negative emotions may cause psychological problems, wrong interpretation of physical health may lead to physical problems, social relations may be affected by difficulty in establishing good social relations, and environmental quality of life can be decreased due to inappropriate interactions with the environment.
According to the results of the present study it is important to pay attention to alexithymia as an important variable associated with (depression, anxiety, stress), social support, and quality of life of patients with coronary heart disease. It can be concluded that alexithymia is connected with the pathological indicators of cardiac disease (depression, anxiety, and stress) and its protective parameters (social support and quality of life). Most patients with heart disease are elderly and alexithymia is also more common among older people. Therefore, conducting a longitudinal study to determine the precise role of alexithymia in the psychiatric pathology of cardiac diseases is essential.
This research showed the relation between alexithymia and (depression, anxiety, stress), social support, and quality of life, as a psychological structural model in CHD. Most of the relationships were associated with alexithymia, depression, anxiety, and stress (DASS: 49%) and the lowest relationship was between alexithymia and social support (MSPSS: 09%). Of particular interest in the findings, was the inverse relationship alexithymia had with the quality of life. If alexithymia is considered to be a personality trait or state-dependent trait, alexithymic individuals are at risk for medical or psychiatric disorders and negative emotions. Increasing our knowledge regarding the role of a negative affect may have a major implication on how future interventions are targeted, for example, if evidence supports the lack of emotional awareness (e.g. depression, anxiety, and stress) as an underlying factor for a subset of patients seeking interdisciplinary treatment, then intervention can be modified to focus on processes related to increasing emotional awareness and identification, with a hope to improve the quality of life in patients with coronary heart diseases.
The limitations of the study were: Inability to control the behaviors that were associated with alexithymia and could thus affect the relationship between alexithymia and depression, anxiety, stress, social support, and quality of life. As the study population was limited, generalization of the results to other patients had to be made with caution.
CONCLUSIONS
The present study showed the structural relations between the psychological factors associated with alexithymia in coronary heart disease. The results highlight the importance of alexithymia as a risk factor associated with neuroticism (anxiety, depression, and stress) and social support which reduces the quality of life among coronary heart disease patients.
In this regard, psychological interventions are recommended to reduce the consequences of this disorder, especially among coronary heart disease patients. Conducting longitudinal studies in this area may lead to more interesting and favorable results, which is recommended to the researchers interested in this field.
ACKNOWLEDGMENT
The authors’ deepest gratitude goes to all the patients who participated in the study and the authorities of the Isfahan Cardiovascular Research Institute, Chamran Heart Hospital, Noor and Ali Asghar Hospitals, and other medical centers that helped in the process of this research.
Footnotes
Source of Support: This article was extracted from dissertation of PhD and the research supported by Isfahan Cardiovascular Research Institute
Conflict of Interest: None declared
References
- 1.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Ann Rev Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 2.Suls J, Bunde J. Anger, anxiety, and depression as risk factors for cardiovascular disease: The problems and implications of overlapping affective dispositions. Psychol Bull. 2005;131:260–300. doi: 10.1037/0033-2909.131.2.260. [DOI] [PubMed] [Google Scholar]
- 3.Khayyam Nekouei Z, Yousefy A. Application of cognitive-behavioral therapy for reducing anxiety in cardiac patients. ARYA Atheroscler J. 2007;3:69–71. [Google Scholar]
- 4.Mikolajczak M, Luminet O, Menil C. Predicting resistance to stress: Incremental validity of trait emotional intelligence over alexithymia and optimism. Psicothema. 2006;18:79–88. [PubMed] [Google Scholar]
- 5.Mattila AK, Saarnei SI, Salminen JK, Htala H, Sintonen H, Joukamaa M. Alexithymia and Health-Related Quality of Life in a General Population. Psychosomatics. 2009;50:59–68. doi: 10.1176/appi.psy.50.1.59. [DOI] [PubMed] [Google Scholar]
- 6.Nehra1 DK, Sharma NR, Ali G, Margoob MA, Mushtaq H, Kumar P, et al. Alexithymia and Type “A” Behavior Pattern (TABP) in Coronary Heart Diseases: A preliminary study. Dali Psychiatry J. 2012;15(2):320–326. [Google Scholar]
- 7.Khayyam Nekouei Z, Neshat Doost H, Yousefy A, Sadeghei M, Manshaee GH. Psychological factors and coronary heart disease. ARYA Atheroscler J. 2013;9(1):1–10. [PMC free article] [PubMed] [Google Scholar]
- 8.Khayam Nekouei Z, Yousefy AR, Khayyam Nekouei AR, Sadeqhi M. The relation between anxiety and quality of life in heart patients. Health Inf Manage. 2009;5:19–24. [Google Scholar]
- 9.Yousefy AR, Ghassemi GR, Sarrafzadegan N, Mallik S, Baghaei AM, Rabiei K. Psychometric properties of the WHOQOL-BREF in an Iranian adult sample. Community Ment Health J. 2010;46:139–47. doi: 10.1007/s10597-009-9282-8. [DOI] [PubMed] [Google Scholar]
- 10.Yousefy A, Nekouei ZK. Basis of Cognitive-Behavioral Trainings and its Applications in Recovery of Chronic Diseases. Iran J Med Educ. 2011;10:792–800. [Google Scholar]
- 11.Nekouei ZK, Yousefy AR, Manshaee G. Cognitive-behavioral therapy and quality of life: An experience among cardiac patients. J Edu Health Promot. 2012;1:2. doi: 10.4103/2277-9531.94410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uchino BN. Social Support and Health: A Review of Physiological Processes Potentially Underlying Links to Disease Outcomes. J of Behavioral Medicine. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 13.Lofvenmark C, Mittiasson AC, Billing E, Edne M. Perceived loneliness and social support in Patients with chronic heart failure. Eur J Cardiovasc Nurs. 2009;8:251–8. doi: 10.1016/j.ejcnurse.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 14.Barth J, Schneider S, Von Känel R. Lack of social support in the etiology and the prognosis of coronary heart disease: A systematic review and meta-analysis. Psychosom Med. 2010;72:229–38. doi: 10.1097/PSY.0b013e3181d01611. [DOI] [PubMed] [Google Scholar]
- 15.Williams ED, Nazroo JY, Kooner JS, Steptoe A. Subgroup difference in psychological factors relating to coronary heart disease in the UK South Asian population. J Psychosom Res. 2010;69:379–87. doi: 10.1016/j.jpsychores.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krantz DS, McCeney KT. Effects of psychological and social factors on organic disease: A critical assessment of research on coronary heart disease. Annu Rev Psychol. 2002;53:341–69. doi: 10.1146/annurev.psych.53.100901.135208. [DOI] [PubMed] [Google Scholar]
- 17.Brotman DJ, Golden SH, Wittstein IS. The cardiovascular toll of stress. Lancet. 2007;370:1089–100. doi: 10.1016/S0140-6736(07)61305-1. [DOI] [PubMed] [Google Scholar]
- 18.Rozanski A, Blumenthal AJ, Davidson WK, Saab PG, Kubzansky L. The epidemiology pathophysiology, and management of psychosocial risk factors in cardiac practice: The emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637–51. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 19.Uchino BN. New Haven, CT: Yale University Press; 2004. Social support and physical health: Understanding the health consequences of our relationships. [Google Scholar]
- 20.Wang HX, Mittleman MA, Orth-Gomer K. Influence of social support on progression coronary artery disease in women. Soc Sci Med. 2005;60:599–607. doi: 10.1016/j.socscimed.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 21.Sifneos PE. Affect, emotional conflict, and deficit: An overview. Psychother Psychosom. 1991;56:116–22. doi: 10.1159/000288543. [DOI] [PubMed] [Google Scholar]
- 22.Haviland MG, Reise SP A. California Q-set alexithymia prototype and its relationship to ego-control and ego-resiliency. J Psychosom Res. 1996;41:597–608. doi: 10.1016/s0022-3999(96)00223-1. [DOI] [PubMed] [Google Scholar]
- 23.Taylor GJ. The alexithymia construct: Conceptualization, validation, and relationships with basic dimensions of personality. New Trends Exp Clin Psychiatry. 1994;10:61–74. [Google Scholar]
- 24.Lumley MA, Stettner L, Wehmer F. How are alexithymia and physical illness linked? A review and critique of pathways. J Psychosom Res. 1996;41:505–18. doi: 10.1016/s0022-3999(96)00222-x. [DOI] [PubMed] [Google Scholar]
- 25.Taylor GJ, Bagby RM, Parker JD. The revised Toronto Alexithymia Scale: Some reliability, validity and normative data. Psychother Psychosom. 1992;57:34–41. doi: 10.1159/000288571. [DOI] [PubMed] [Google Scholar]
- 26.Wise TN, Mann LS. The attribution of somatic symptoms in psychiatric Outpatients. Compr Psychiatry. 1995;36:407–10. doi: 10.1016/s0010-440x(95)90247-3. [DOI] [PubMed] [Google Scholar]
- 27.Lumley MA, Neely LC, Burger AJ. The assessment of alexithymia in medical settings: Implications for understanding and treating health problems. J Pers Assess. 2007;89:230–46. doi: 10.1080/00223890701629698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shahgolian M, Moradi AR, Kafi M. Alexithymia expressed excitement about the styles and general health in students. Iran Psychiatry Clin Psychol. 2007;13:238–48. [Google Scholar]
- 29.Lane RD, Sechrest L, Riedel R. Socio demographic correlates of alexithymia. Compr Psychiatry. 1998;39:377–85. doi: 10.1016/s0010-440x(98)90051-7. [DOI] [PubMed] [Google Scholar]
- 30.Salminen JK, Saarijärvi S, Aärelä E, Toikka T, Kauhanen J. Prevalence of alexithymia and its association with sociodemographic variables in the general population of Finland. J Psychosom Res. 1999;46:75–82. doi: 10.1016/s0022-3999(98)00053-1. [DOI] [PubMed] [Google Scholar]
- 31.Honkalampi K, Hintikka J, Tanskanen A, Lehtonen J, Viinamäki H. Depression is strongly associated with alexithymia in the general population. J Psychosom Res. 2000;48:99–104. doi: 10.1016/s0022-3999(99)00083-5. [DOI] [PubMed] [Google Scholar]
- 32.Kokkonen P, Karvonen JT, Veijola J, Läksy K, Jokelainen J, Järvelin MR, et al. Prevalence and sociodemographic correlates of alexithymia in a population sample of young adults. Compr Psychiatry. 2001;42:471–6. doi: 10.1053/comp.2001.27892. [DOI] [PubMed] [Google Scholar]
- 33.Nehra DK, Sharma V, Mushtaq H, Sharma NR, Sharma M, Nehra S. Emotional Intelligence and Alexithymia in Alcoholics. Behav Sci. 2011;12:101–8. [Google Scholar]
- 34.Nekouei ZK, Mazaheri M, Manshaee GH. Shiraz, Fars, Iran: Fars Science and Research branch; 2011. Alexithymia and autism spectrum disorders. The first international congress child and adolescent psychology. 1st to 6th May 2011. [Google Scholar]
- 35.Valkamo M, Hintikka J, Niskanen L. Depression and associated factors in coronary heart disease. Scand Cardiovasc J. 2001;35:259–63. doi: 10.1080/14017430152581378. [DOI] [PubMed] [Google Scholar]
- 36.Valkamoa M, Hintikkaa J, Honkalampia K, Niskanenb L, Koivumaa-Honkanena H, ViinamaÈkia H. Alexithymia in patients with coronary heart diseas. J Psychosomatic Res. 2001;50:125–30. doi: 10.1016/s0022-3999(00)00209-9. [DOI] [PubMed] [Google Scholar]
- 37.Khauhanen J, Kaplan JA, Cohen RD, Salonen R, Salonen JT. Alexithymia may influence the diagnosis of coronary heart disease. Psychosom Med. 1994;56:237–44. doi: 10.1097/00006842-199405000-00010. [DOI] [PubMed] [Google Scholar]
- 38.Kauhanen J, Kaplan G, Cohen R, Julkunen J, Salonen JT. Alexithymia and risk of death in middle-aged men. J Psychosom Res. 1996;41:541–9. doi: 10.1016/s0022-3999(96)00226-7. [DOI] [PubMed] [Google Scholar]
- 39.Lumley MA, Tomakowsky J, Torosian T. The relationship of alexithymia to subjective and biomedical measures of disease. Psychosomatics. 1997;38:497–502. doi: 10.1016/S0033-3182(97)71427-0. [DOI] [PubMed] [Google Scholar]
- 40.Henrya JD, Phillip LH, Maylorc EA, Hosieb J, Milneb AB, Meyerc C. A new conceptualization of alexithymia in the general adult population: Implications for research involving older adults. J Psychosomatic Res. 2006;60:535–43. doi: 10.1016/j.jpsychores.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 41.Duddu V, Isaac MK, Chaturvedi SK. Alexithymia in somatoform and depressive disorders. J Psychosomatic Res. 2003;54:435–8. doi: 10.1016/s0022-3999(02)00440-3. [DOI] [PubMed] [Google Scholar]
- 42.Bagby RM, Taylor GJ, Parker JD. Construct validity of the Toronto alexithymia scale. Psychother Psychosom. 1988;50:29–34. doi: 10.1159/000288097. [DOI] [PubMed] [Google Scholar]
- 43.Kauhanen J, Julkunen J, Salonen JT. Alexithymia and perceived symptoms: Criterion validity of the Toronto Alexithymia Scale. Psychother Psychosom. 1991;56:247–52. doi: 10.1159/000288563. [DOI] [PubMed] [Google Scholar]
- 44.Myers LB. Alexithymia and repression: The role of defensiveness and trait anxiety. Pers lndivid Dif. 1995;19:489–92. [Google Scholar]
- 45.Linden W, Lenz JW, Stossel C. Alexithymia, defensiveness and cardiovascular to stress. J Psychosomatic Res. 1999;41:575–83. doi: 10.1016/s0022-3999(96)00229-2. [DOI] [PubMed] [Google Scholar]
- 46.Mattila AK, Alanen E, Salminen JK, Kronholm JA, Sintonen H, Joukamaa M. Health-related quality-of-life profiles in nonalexithymic and alexithymic subjects from general population. J Psychosomatic Res. 2010;68:279–83. doi: 10.1016/j.jpsychores.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 47.Dion KL. Ethnolinguistic correlates of alexithymia: Toward a cultural Perspective. J Psychosom Res. 1996;41:531–9. doi: 10.1016/s0022-3999(96)00295-4. [DOI] [PubMed] [Google Scholar]
- 48.Fukunishi I, Kaji N, Hosaka T, Berger D, Rahe RH. The relationship of Alexithymia and poor social support to ulcerative changes on gastrofiberscopy. Psychosomatics. 1997;38:20–6. doi: 10.1016/S0033-3182(97)71499-3. [DOI] [PubMed] [Google Scholar]
- 49.Bagby RM, Pa rker JD, Taylor GJ. The twenty-item TorontoAlexithymia Scale-I. Item selection and cross-validation of the factor structure. J Psychosomatic Res. 1994;38:23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 50.Shahgholian M, Moradi A, Kafi SM. Relation of alexithymia with emotional expression styles and general health in students. Iran J Psychiatry Clinl Psychological. 2007;13:238–48. [Google Scholar]
- 51.Lovibond SH, Lovibond PF. 2nd ed. Sydney: Psychology Foundation; 1995. Manual for the Depression anxiety Stress Scales. [Google Scholar]
- 52.Samani S, Jokar B. Study the validity and reliability of the Iranian version of the Depression, Anxiety, Stress Scale. J Soc Humanities Shiraz University 263. 2007 [Google Scholar]
- 53.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess. 1990;55:610–7. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 54.Ghasemi V. Tehran: Jameeshenasan Publication; 2010. Structural equation modeling in social researches using amos graphics. [Google Scholar]
- 55.Saarijarvi S, Salminen JK, Toikka TB. Alexithymia and depression: A 1-year follow-up study in outpatients with major depression. J Psychosom Res. 2001;51:729–33. doi: 10.1016/s0022-3999(01)00257-4. [DOI] [PubMed] [Google Scholar]
- 56.Beshart MA. Relation of Alexithymia with depression, anxiety, psychological helplessness and well being. J Psychol Tabriz Univ. 2008;10:17–40. [Google Scholar]
- 57.Morton I, Gencoz T. The Relationship Between the Dimensions of Alexithymia and the Intensity of Depression and Anxiety. Turk Psikiyatri Derg. 2007;18:333–43. [PubMed] [Google Scholar]
- 58.Hisli Sahin N, Güler M, Basim HN. The relationship between cognitive intelligence, emotional intelligence, coping and stress symptoms in the context of type A personality pattern. Turk Psikiyatri Derg. 2009;20:243–54. [PubMed] [Google Scholar]
- 59.Lumley MA, Ovies T, Stettner L, Wehmer F, Lakey B. Alexithymia, social support and health problems. J Psychosomatic Res. 1996;41:519–30. doi: 10.1016/s0022-3999(96)00227-9. [DOI] [PubMed] [Google Scholar]
- 60.Verissimo R, Mota-Cardoso R, Taylor G. Relationships between alexithymia, emotional control, and quality of life in patients with inflammatory bowel disease. Psychother Psychosom. 1998;67:75–80. doi: 10.1159/000012263. [DOI] [PubMed] [Google Scholar]
- 61.Mattila AK, Saarni SI, Salminen JK, Huhtala H, Sintonen H, Joukamaa M. Alexithymia and health-related quality of life in general population. Psychosomatic. 2009;50:59–68. doi: 10.1176/appi.psy.50.1.59. [DOI] [PubMed] [Google Scholar]
- 62.Salminen JK, Saarijärvi S, Toikka T. Alexithymia and health-related quality of life. J Psychosom Res. 2002;52:324. [Google Scholar]
- 63.Fortune DG, Richards HL, Griffiths CE, Main CJ. Psychological stress, distress and disability in patients with psoriasis: Consensus and variation in the contribution of illness perceptions, coping and alexithymia. Br J Clin Psychol. 2002;41:157–74. doi: 10.1348/014466502163949. [DOI] [PubMed] [Google Scholar]


