Abstract
Background:
Breast cancer is the most prevalent type of cancer among Iranian females; it is noteworthy that the condition of this type of cancer among Iranian women does not significantly differ from what has been reported from other countries. Considering the importance of this issue, identification of the backgrounds factors and risk factors of the breast cancer risk are highly needed. Therefore, the present study is aimed to compare the risk factors of resident patients of Isfahan province, Iran, with accredited risk factors by other countries and also identify the importance of each factor in the incidence of cancer.
Materials and Methods:
The present work is a case-control study, which was conducted in 2011. In order to conduct the study, 216 women who had been clinically identified with breast cancer were selected from Seiedo-Shohada Hospital, Isfahan, Iran, as the case group. Moreover, 41 healthy women who were the relatives of the selected patients (i.e., sisters and aunts) were selected as the control group. The data and information of the patients from 1999 to 2010 were collected from either assessing the database system of the center for breast cancer research or interviewing the patients through phone. To analyze the data, multiple logistic regression method was applied.
Results:
The range of age among selected individuals in this study was from 20-75 years old. The determinant factors for odds of breast cancer included in the applied multiple logistic regression model were the use of oral contraceptive pills (OCPs) (odds ratio [OR] =0.18, 95% confidence interval [CI] = 0.04-0.75) as the protective factor, hormone replacement therapy (OR = 10.2, 95% CI = 1.18-88.89) and menopause at old age (OR = 1.26, 95% CI = 1.11-2.12) as the risk factors. Furthermore, there was not seen any significant relationship between age, vocation, and marital status with odds of breast cancer in multiple model.
Conclusion:
Based on the results, use of OCPs as protective factor, hormone replacement therapy, and menopause at old age are identified as the risk factors in developing breast cancer among women. Influencing and modifiable factors should be considered very important in society based interventions and preventive interventions planning.
Keywords: Breast cancer, case-control, hormone, Isfahan, reproductive, risk factors
INTRODUCTION
Diseases and problems of breast is a common issue in clinical medicine. In fact, physicians and health personnel are confronted with these problems every day Breast cancer is the most prevalent type of cancer among Iranian women, which its condition is almost the same with recognized cases of this cancer in other countries. Based on the statistical reports, dying from breast cancer is the fifth cause of death among Iranian women. The age specific mortality rate of breast cancer in Iran is around 25 individuals per 100,000 with 7500 annually incidence of new cases.[1,2]
According to the achieved data from a study on 18 provinces in 2001, the average age of women identified with breast cancer was 53.4 years old. Based on the released reports of study, 2.5 women per 100,000 women died from the cancer which it stands on the 4th rank of the causes of death after gastric, lungs, and hepatocellular carcinoma in females.[3]
Considering the high prevalence of this cancer among women, the factors triggering this cancer have not been well-recognized yet. In fact, there is a highly needed theory upon which such factors can be identified and applied in order to prevent the developing of this disease among women.[4] Regarding the importance of this issue, there has been a wide range of cross-sectional, case control, and cohort studies to identify the role of specific reproductive and hormonal factors, which are as the follows: Oral contraceptive pills (OCPs), age of the initiation of menses, initial age of menopause, abortion (spontaneously or induced), age of the first pregnancy, duration of breast feeding, multi parity, regular menses, diet, obesity, inheritance factors, etc., However, the scientists and researchers are not in agreement about the relationship between these factors and breast cancer.[5]
Although many epidemiological studies have been conducted on the risk factors of breast cancer, different results have been reported. Most of these conducted studies reported that there is a relationship between the incidence of breast cancer and the reproductive condition among women and its related issues, including early menses, delayed menopause, no parity, giving birth at old age, diet, physical activity and using hormone.[6,7,8] In a conducted study in Switzerland, it was observed that each parity or delivery of live birth reduces the risk of developing breast cancer by 10%.[9] Furthermore, in a cohort study in France, a relationship between no parity and the incidence of breast cancer was reported.[10] In a systematic review of 30 case-control studies, the protective effect of breast feeding against breast cancer incidence was shown. Furthermore, it was found that both pregnancy and parity through life time are in fact protective factors against breast cancer.[11]
Based on the results of systematic review and meta-analysis study of 13 cohort studies, significant relationship between the use of OCPs and the risk of breast cancer incidence was not observed.[12] However, in another systematic review and meta-analysis study on the risk factors of breast cancer, it was derived that hormone therapy, diabetics, and use of OCPs increase the risk of breast cancer incidence, whereas breast feeding decreases the breast cancer incidence.[13]
Considering the fact that the prevalence of the risk factors of breast cancer in societies can be changed through conducting intervention activities, knowing these factors and their prevalence in different regions of Iran provides specific information by which appropriate planning for each region can be expected. Therefore, the present case-control study is aimed to compare the risk factors of resident patients of Isfahan, Iran, with accredited risk factors by other countries and also identify the importance of each factor in the incidence of cancer.
MATERIALS AND METHODS
Study design and sample
The present work is a case-control study which was conducted in 2011. In order to conduct the study, 216 women who had been clinically identified with breast cancer were selected from Seiedo-Shohada Hospital, Isfahan, Iran, as the case group. And, 41 healthy women who were the relatives of the selected patients (i.e., sisters and aunts) were selected as the control group. It is noteworthy that the time period of this study was from 1999-2010. The included individuals in control group were selected from the close relatives of the patients so as to have matching in terms of socio-economic status and related genetic to inheritance. Due mostly to this reason that the patients who were diagnosed with cancer were all from different regions of Isfahan, the results of this study can be accounted for the whole population of this province.
The selected patients had been diagnosed with cancer by the oncology group of the hospital via histopathology diagnosis method. The control group was included with women who were the relatives of the patients; they were healthy and not diagnosed with breast cancer back then. The required data from the intervention group, including initial age of menses, age of the first pregnancy, menopause status, breastfeeding status, the history of abortion, the number of parity, and the age of the individuals were collected from either assessing the database of the center for breast cancer research or interviewing the patients via phone. As for the control group, the needed data was achieved via either person-to-person interview or phone. The sampling method applied in this study for both groups was non probability and convenience sampling method.
Data analyzes
The collected data was analyzed by applying SPSS version 16.0 (SPSS Inc, Chicago, Illinois) software. To compare the quantitative and qualitative variables in both groups, Chi-square and independent samples t-tests were applied. Furthermore, multiple logistic regression method was used to control the confounding factors as well as estimating the risk of breast cancer, by which it means the odds ratio (OR) and 95% confidence interval (CI). Variables which their significance level was less than 0.2 in univariate analysis, were entered to the model. Then, the variables which their significance level was less than 0.05 were kept in the final multiple logistic regression model.
RESUTLS
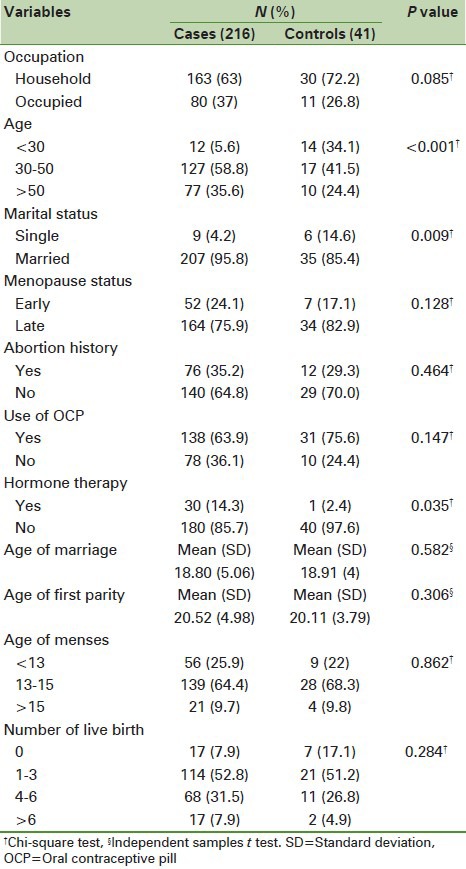
Based on the results, the range of age among selected individuals in this study was from 20-75. Descriptive, demographic and reproductive characteristics of the included individuals in both case and control groups are shown in Table 1. As it has shown in Table 1, the variables, which their significance level were lower than 0.2, were allowed to enter to the model. Based on the results of the comparative tests, specific variables, including vocation, age, marital status, menopause status, use of OCPs, and hormone therapy have significant relationship (P < 0.2) with developing of breast cancer. These variables were entered to the multiple logistic regression model to assess the determining factors of developing breast cancer.
Table 1.
Demographic and reproductive characteristics of cases and controls groups of Isfahan patients included in study
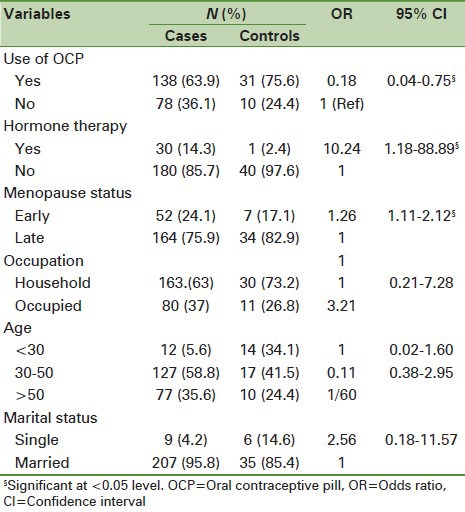
The independent risk factors of breast cancer under the control of confounding factors in the applied multiple logistic regression model are shown in Table 2. As it can be seen from the table, vocation, age and marital status were found to be the confounding factors; in other words, multiple analyses showed that these factors were not statistically significant in association with the odds of breast cancer. Based on the results, OCPs as a protective factor, hormone therapy, and late menopause should be considered as the risk factors of breast cancer incidence. The use of OCPs significantly decreases the odds of developing breast cancer by 80% (OR = 0.18, 95% CI = 0.04-0.75). The women who had been under hormone therapy were 10.2 times higher at the odds of developing breast cancer, in comparison with women who have had no history of hormone therapy (95% CI = 1.18-88.89). Furthermore, the odds of breast cancer in women with late menopause was significantly higher than women who have had early menopause (OR = 1.26, 95% CI = 1.11-2.12). According to the final results of the model, there was not seen any significant relationship between the risk of breast cancer with age, vocation, and marital status.
Table 2.
Risk factors for odds of breast cancer in Isfahan patients in multiple logistic regression model
DISCUSSION
In the present study, it was concluded that the use of OCPs could be regarded as a protective factor in developing of breast cancer. On the other hand, hormone therapy and late menopause were found to be the risk factors of this cancer. Breast cancer is known as a disease with high socio-economical level. However, this trend differs in both developing and under developed countries with what has been reported from developed ones. In other words, the main factors are affected by the traditional ways of living and higher birth rate, in comparison with developed countries.
Although the effects of OCPs in the incidence of breast cancer have been widely studied, the reported results from these studies are not in line with each other. For example, a significant relationship between the use of the pills and the risk of breast cancer incidence was not found in previously conducted study,[14] whereas in another one this relationship was approved to be an affecting factor.[15] In the present study, the multiple analyses showed that the use of the pills does not increase the odds of breast cancer incidence, but it in fact decreases the odds. Experienced based studies strongly suggest that estrogen plays an important role in not only the incidence of the cancer but also its development stages.[16] Considering the benefits of the OCPs, further studies on specific groups of cancer patients should be conducted in order to identify the true role of this factor in the incidence of breast cancer.
In addition, the results showed that hormone therapy increases the odds of breast cancer. Epidemiological observational studies and randomized controlled trials showed that the hormone therapy along with receiving a combination of estrogen and progesterone increase the risk of breast cancer incidence.[24] Considering the above mentioned results, hormone therapy not only plays a risk factor role in breast cancer incidence, but also increases the odds of stroke and blood clots.[25] Furthermore, some of the studies have shown that the decrease in hormone therapy prescription could result in the decrease of the risk of the breast cancer.[26]
Abortion, whether it is spontaneous or induced, causes both increase and decrease of the risk of breast cancer. It is also considered that this factor may do not have any relationship with the incidence of the cancer.[17,18,19] Based on the results of the European Prospective Investigation into Cancer (EPIC) study, the relative risk of the cancer incidence was significantly higher in women who had no record of abortion, in comparison with women with one or more experience of abortion through their life time.[20] It seems that separately studying the spontaneous and induced abortions would be a better way to understand the ways that abortion affects the development or incidence of the breast cancer.
According to the results of multiple analyses in the present study, late menopause could be considered as a risk factor in the developing of the breast cancer. This result is in line with the findings of previously conducted research in which the status of menopause as well as age of menopause were in relationship with the increase of breast cancer risk.[21] Based on the results of that study, the risk of breast cancer in women whose menopause started before they were 45 years old is a third of those who had delayed menopause. However, the outputs of the final applied model in the present study did not show any significant relationship between the initial age of menopause and breast cancer incidence. These findings are also consistent with another case-control study.[21] There are also reports that show the protective role of late menopause in women with family history of breast cancer.[22] The differences which can be noticed in the results of the conducted studies could be due mostly to the regional difference in women age distribution and also difficulty in remembering the initial age of menopause. It should also be noted that there are probably a lot of factors which could interfere with the studies. From the theoretical point of view, breast's tissue exposes to more sexual hormone, including estrogen, if menopause starts prematurely.[23] Hence, this can demonstrate why this factor should be considered as a risk factor of breast cancer.
In addition, the results showed that marital status was not an independent risk factor in the multiple analyses. It seems that marital status does not have any significant effect in the increase of the risk of the cancer. Furthermore, the protective role of this factor which has been reported by some of the previously conducted studies is in fact rooted from the effect of age in the first parity; in other words, it approves the confounding role of this variable in the studies of this field.
In conclusion, the use of OCPs is considered to be a protective factor against the odds of breast cancer. On the other hand, hormone therapy and late menopause are found to be the risk factors of breast cancer occurrence. Distinguishing and differentiating the risk factors and their possible related mechanisms in different societies are very important in determining the breast cancer etiology. Based on the results, both hormone and reproductive status of women should be taken into account. Also, it should be considered that the influencing and modifiable factors could be applied by those who perform society based intervention and preventive intervention planning.
Limitation
Although case-control studies can be conducted more often with acceptable costs, there are some drawbacks and biases in the field of cancers researches which need to be mentioned, including response bias, information bias and recall bias; it is noteworthy that the authors were full aware of the mentioned problems. Specific limitations, including unavailability of the individuals and the number of individuals in control group, which was lower than case group, were also confronted in this study.
ACKNOWLEDGMENT
The authors would like to thank Deputy for Research of Isfahan University of Medical Sciences for funding this study. The authors would like to thank all of participants who helped to conduct this study.
Footnotes
Source of Support: Deputy for Research, Isfahan University of Medical Sciences
Conflict of Interest: None declared
References
- 1.Akbari ME. Tehran: Cancer Research Center, Shahid Beheshti University of Medical Sciences, Qom, Dar-olfekr; 2008. Iran Cancer Report. [Google Scholar]
- 2.Naghavi M. Tehran: Deputy of Health, Ministry of Health and Medical Education; 2004. Profile of death in 23 provenances of Iran. [Google Scholar]
- 3.Naghavi M. Tehran: Deputy of Health, Ministry of Health and Medical Education, Tandis; 1382. Profile of death in 18 provenances of Iran; p. 75. [Google Scholar]
- 4.Byers T, Graham S, Rzepka T, Marshall J. Lactation and breast cancer. Evidence for a negative association in premenopausal women. Am J Epidemiol. 1985;121:664–74. doi: 10.1093/aje/121.5.664. [DOI] [PubMed] [Google Scholar]
- 5.Nojomi M, Mirfakhraee R, Hosseini N. Relationship between hormonal factors and breast cancer. J Hakim. 1383;7:19–25. [Google Scholar]
- 6.Ozmen V. Brest cancer in the world and Turkey. J Breast Health. 2008;4:6–12. [Google Scholar]
- 7.Fidaner C, Eser SY, Parkin DM. Incidence in Izmir in 1993-1994: First results from Izmir Cancer Registry. Eur J Cancer. 2001;37:83–92. doi: 10.1016/s0959-8049(00)00355-5. [DOI] [PubMed] [Google Scholar]
- 8.Kuru B, Ozaslan C, Ozdemir P, Dinç S, Camlibel M, Alagöl H. Risk factors for breast cancer in Turkish women with early pregnancies and long-lasting lactation – A case-control study. Acta Oncol. 2002;41:556–61. doi: 10.1080/02841860214964. [DOI] [PubMed] [Google Scholar]
- 9.Lambe M, Hsieh CC, Chan HW, Ekbom A, Trichopoulos D, Adami HO. Parity, age at first and last birth, and risk of breast cancer: A population-based study in Sweden. Breast Cancer Res Treat. 1996;38:305–11. doi: 10.1007/BF01806150. [DOI] [PubMed] [Google Scholar]
- 10.Clavel-Chapelon F, E3N-EPIC Group. Differential effects of reproductive factors on the risk of pre- and postmenopausal breast cancer. Results from a large cohort of French women. Br J Cancer. 2002;86:723–7. doi: 10.1038/sj.bjc.6600124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang L, Jacobsen KH. A systematic review of the association between breastfeeding and breast cancer. J Womens Health (Larchmt) 2008;17:1635–45. doi: 10.1089/jwh.2008.0917. [DOI] [PubMed] [Google Scholar]
- 12.Ozmen V, Ozcinar B, Karanlik H, Cabioglu N, Tukenmez M, Disci R, et al. Breast cancer risk factors in Turkish women – A University Hospital based nested case control study. World J Surg Oncol. 2009;7:37. doi: 10.1186/1477-7819-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beji NK, Reis N. Risk factors for breast cancer in Turkish women: A hospital-based case-control study. Eur J Cancer Care (Engl) 2007;16:178–84. doi: 10.1111/j.1365-2354.2006.00711.x. [DOI] [PubMed] [Google Scholar]
- 14.Lupulescu A. Estrogen use and cancer incidence: A review. Cancer Invest. 1995;13:287–95. doi: 10.3109/07357909509094464. [DOI] [PubMed] [Google Scholar]
- 15.Rosenblatt KA, Gao DL, Ray RM, Rowland MR, Nelson ZC, Wernli KJ, et al. Induced abortions and the risk of all cancers combined and site-specific cancers in Shanghai. Cancer Causes Control. 2006;17:1275–80. doi: 10.1007/s10552-006-0067-x. [DOI] [PubMed] [Google Scholar]
- 16.Michels KB, Xue F, Colditz GA, Willett WC. Induced and spontaneous abortion and incidence of breast cancer among young women: A prospective cohort study. Arch Intern Med. 2007;167:814–20. doi: 10.1001/archinte.167.8.814. [DOI] [PubMed] [Google Scholar]
- 17.Brewster DH, Stockton DL, Dobbie R, Bull D, Beral V. Risk of breast cancer after miscarriage or induced abortion: A Scottish record linkage case-control study. J Epidemiol Community Health. 2005;59:283–7. doi: 10.1136/jech.2004.026393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reeves GK, Kan SW, Key T, Tjønneland A, Olsen A, Overvad K, et al. Breast cancer risk in relation to abortion: Results from the EPIC study. Int J Cancer. 2006;119:1741–5. doi: 10.1002/ijc.22001. [DOI] [PubMed] [Google Scholar]
- 19.Oran B, Celik I, Erman M, Baltali E, Zengin N, Demirkazik F, et al. Analysis of menstrual, reproductive, and life-style factors for breast cancer risk in Turkish women: A case-control study. Med Oncol. 2004;21:31–40. doi: 10.1385/MO:21:1:31. [DOI] [PubMed] [Google Scholar]
- 20.Becher H, Schmidt S, Chang-Claude J. Reproductive factors and familial predisposition for breast cancer by age 50 years. A case-control-family study for assessing main effects and possible gene-environment interaction. Int J Epidemiol. 2003;32:38–48. doi: 10.1093/ije/dyg003. [DOI] [PubMed] [Google Scholar]
- 21.Travis RC, Key TJ. Oestrogen exposure and breast cancer risk. Breast Cancer Res. 2003;5:239–47. doi: 10.1186/bcr628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ross RK, Paganini-Hill A, Wan PC, Pike MC. Effect of hormone replacement therapy on breast cancer risk: Estrogen versus estrogen plus progestin. J Natl Cancer Inst. 2000;92:328–32. doi: 10.1093/jnci/92.4.328. [DOI] [PubMed] [Google Scholar]
- 23.Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results From the Women's Health Initiative randomized controlled trial. JAMA. 2002;288:321–33. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 24.von Euler-Chelpin M. Breast cancer incidence and use of hormone therapy in Denmark 1978-2007. Cancer Causes Control. 2011;22:181–7. doi: 10.1007/s10552-010-9685-4. [DOI] [PubMed] [Google Scholar]
- 25.Zhu H, Lei X, Feng J, Wang Y. Oral contraceptive use and risk of breast cancer: A meta-analysis of prospective cohort studies. Eur J Contracept Reprod Health Care. 2012;17:402–14. doi: 10.3109/13625187.2012.715357. [DOI] [PubMed] [Google Scholar]
- 26.Anothaisintawee T, Wiratkapun C, Lerdsitthichai P, Kasamesup V, Wongwaisayawan S, Srinakarin J, et al. Risk factors of breast cancer: A systematic review and meta-analysis. Asia Pac J Public Health. 2013;25:368–87. doi: 10.1177/1010539513488795. [DOI] [PubMed] [Google Scholar]


