Abstract
Objectives
Determine whether self-efficacy independently predicted weight loss in a behavioral intervention and explore factors that influence the path between self-efficacy and weight change.
Design
Secondary analysis of the PREMIER trial, a randomized controlled trial testing effects of lifestyle interventions on blood pressure.
Setting
Four academic medical centers.
Participants
PREMIER recruited adults (n = 810) with pre-hypertension/stage 1 hypertension, not currently receiving medication. This analysis excluded participants in the control arm, resulting in n = 537.
Interventions
Participants were randomly assigned to 1 of 3 groups: advice only, established lifestyle recommendations, or established lifestyle recommendations plus Dietary Approaches to Stop Hypertension dietary pattern.
Main Outcome Measures
Self-efficacy (dietary self-efficacy [DSE], exercise self-efficacy [ESE]), dietary intake, fitness.
Analysis
Pearson correlations, 1-way analysis of variance, mediation analyses.
Results
Despite an overall decrease in DSE/ESE, change in DSE/ESE significantly predicted weight change at 6 (β = −.21, P < .01; β = −.19, P < .01, respectively) and 18 months (β = −.19, P < .01; β = −.35, P <.01). Change in percent calories from fat partially mediated the DSE/weight change relationship at 6 months. Change in fitness partially mediated the ESE/weight change relationship at 18 months.
Conclusions and Implications
Changes in DSE/ESE were not associated with behavior change as hypothesized. Additional research is needed to identify mediators between self-efficacy and adoption of behaviors that influence weight loss.
Keywords: obesity, behavior change, self-efficacy, dietary intake, physical activity
INTRODUCTION
Self-efficacy refers to an individual’s confidence in his or her ability to carry out a specific behavior.1 Originally developed by Bandura,1 self-efficacy now makes up a key construct of many health behavior change theories, including the Transtheoretical Model and the Health Belief Model.2–5 These theories propose that higher self-efficacy is associated with better adoption of behavior change, and that increasing self-efficacy is a key strategy to increasing uptake of a specific health behavior. Multiple studies have shown evidence of a significant correlation between change in self-efficacy and change in weight over time, however, literature related to the predictive ability of self-efficacy on weight loss and weight loss maintenance is inconsistent.
Strecher et al6 concluded that self-efficacy had similar predictive qualities for weight loss as those seen in other health behaviors, including smoking and alcohol cessation, noting that self-efficacy showed significant predictive ability of short- and long-term weight loss. Bernier and Avard7 found that baseline self-efficacy was a significant predictor of weight loss at 6-week and 6-month time points in a sample of 62 overweight women. Palmeira et al8 examined differences in weight loss based on 4 predominant health behavior change theories and found that the theories that included self-efficacy were better able to predict weight change than those that did not.
Other studies found that whereas there was a significant correlation between increase in self-efficacy and change in weight, there was no predictive ability of self-efficacy for long-term weight loss. Fontaine and Cheskin9 found no correlation between baseline self-efficacy and weight loss over a 14-week intervention. Martin et al10 found an inverse predictive relationship between self-efficacy and weight loss, such that individuals with higher baseline self-efficacy scores lost less weight than those who started with lower self-efficacy scores.
This inconsistency may result from the lack of research related to the mechanism by which self-efficacy relates to weight loss. Because weight loss is a complex health issue influenced by many biological and psychosocial factors, the relationship between self-efficacy and weight loss may be affected by a number of factors. Specifically, a substantial evidence base exists to support a significant correlation between self-efficacy and physical activity and dietary intake.11–14 Many lifestyle interventions include recommendations for specific dietary changes such as increased fruit and vegetable intake, reduced caloric intake or percentage of calories from fat, and increased physical activity.15,16 Because self-efficacy is associated with these behaviors, it may be that the path from self-efficacy to weight loss is directly influenced by the adoption of these behaviors.
Mediation analysis allows for the assessment of the impact of a third, mediating variable, on the direct relationship between 2 variables. Mediation analyses have traditionally focused on 2 objectives.17 The first objective is to aid in developing a more clear understanding of a known relationship. Once a relationship has been established between a predictor variable and outcome variable, a mediation analysis can show the impact of other variables that are believed to contribute to the effect. The second objective is intervention development and evaluation. Interventions that directly impact the mediating variable will in turn directly impact the outcome variable. Exploring the potential impact of behavior change as a mediator in the relationship between self-efficacy and weight loss may lead to a greater understanding of how interventions can target self-efficacy and behavior change to lead to more consistent weight loss results.
Two studies have examined the mediation effects of diet and exercise on the relationship between self-efficacy and weight loss. In a secondary data analysis including 170 adults, Warziski et al18 found no mediating effects of calorie intake or fat gram intake at baseline or 6, 12, or 18 months. Conversely, Linde et al19 reported full mediation effect of behaviors on the relationship between self-efficacy and weight loss during an 8-week intervention, although the behaviors included in this mediation analysis consisted primarily of self-monitoring behaviors and perceived effort, and not dietary intake or exercise patterns.
The purpose of this report was to examine the mediation effects of diet and exercise behaviors on the relationship between self-efficacy and weight loss in the PREMIER trial. The PREMIER trial, a multicenter, randomized clinical trial, tested the effects of lifestyle modification interventions on blood pressure, weight, dietary intake, and physical fitness. The objectives of this analysis were to use data from the PREMIER trial to: (1) assess changes in dietary self-efficacy (DSE) and exercise self-efficacy (ESE) over time, (2) explore the relationship of these changes with behavior change and weight change, and (3) conduct mediation analyses to explore the impact of change in behavior on the relationship between self-efficacy and weight change at 6 and 18 months.
METHODS
The design and methods of the PREMIER trial have been described in detail elsewhere.20 Briefly, this 4-site clinical trial recruited adult participants with either pre-hypertension or stage 1 hypertension, who were not currently receiving antihypertensive medication. Participants were randomly assigned to 1 of 3 groups: an advice-only group consisting of a single 30-minute informational session; an intervention group based on established, traditional lifestyle recommendations (established group); or an intervention group based on established lifestyle recommendations plus adherence to the Dietary Approaches to Stop Hypertension (DASH) dietary pattern (established plus DASH group).21 This analysis included only individuals randomized to the established or established plus DASH groups, because these were the only groups that received behavioral interventions.
The “established lifestyle recommendations” included are commended minimum weight loss of at least 6.8 kg, 180 min/wk of moderate physical activity (defined as activity at a level of 3–6 metabolic equivalents of task), a daily maximum intake of 100 mmol dietary sodium, and a daily maximum alcohol consumption of 2 drinks for men and 1 drink for women. The DASH dietary pattern required a daily intake of 9–12 servings of fruits and vegetables with 2–3 servings of low-fat dairy products, and daily fat intake limited to < 25% of total calories.
The established and established plus DASH interventions were provided in parallel series of group sessions, with 14 sessions during the initial 6 months supplemented with 4 individual intervention sessions. The intervention in the next 12 months included 9 monthly group sessions along with 3 individual sessions. Participants were instructed to record food intake and physical activity minutes daily using a Food and Fitness Diary, which intervention facilitators collected and reviewed at each behavioral session. The PREMIER interventions are described in detail in Funk et al.22
An external protocol review committee and the National Institutes of Health–National Heart, Blood, and Lung Institute reviewed this study, which the institutional review board approved at each site. Each participant provided written informed consent.
Measures
Body mass index
Study staff who were blinded to the protocol weighed participants, who wore light clothing and no shoes, on a calibrated scale at baseline and 6 and 18 months. Staff used a calibrated wall-mounted stadiometer to measure participants’ height. Body mass index was calculated as kilograms per meter squared.15,23
Self-efficacy
Participants completed DSE and ESE measures at baseline and 6 and 18 months. Dietary self-efficacy was measured using the Eating Habits Confidence Questionnaire. This 27-item scale asks participants to rate confidence in their ability to adhere to specific dietary behaviors. The response set consisted of a 5-point Likert-type scale ranging from 1, “I know I cannot,” to 5, “I know I can.” Possible scores on the Eating Habits Confidence Questionnaire range from 27 to 135, with higher scores indicating higher self-efficacy. This scale was adapted from an existing dietary self-efficacy scale.24 Seven items were added to the original questionnaire to reflect goals specific to the dietary patterns prescribed in this study. These questions related to confidence in increasing fruit and vegetable intake and low-fat dairy. The Eating Habits Confidence Questionnaire showed good internal consistency in this sample (Cronbach α = .89).
Exercise self-efficacy was measured using the Exercise Confidence Questionnaire.24 This 12-item scale asks participants to rate confidence in their ability to maintain an exercise routine when facing various barriers. Possible scores on the Exercise Confidence Questionnaire range from 12 to 60, with higher scores indicating higher self-efficacy. Changes in scale scores were calculated to determine the change in DSE and ESE from baseline to6 months and baseline to 18 months. The Exercise Confidence Questionnaire showed good internal consistency in this sample (Cronbach α = .89).
Dietary behaviors
Intake of nutrients and food groups was assessed from unannounced 24-hour dietary recalls conducted by telephone interviewers. Two recalls (1 obtained on a weekday and the other on a weekend day) were obtained at baseline and 6 and 18 months. The Diet Assessment Center of Pennsylvania State University administered recalls with the use of Nutrition Data System software (NDS-R; version NDS-R 1998, University of Minnesota, Minnesota, MN, 1998). Dietary data for each day were collected using a multiple-pass technique and portion size estimation aids to improve the quality of the data collected.25 Daily caloric intake, percentage of calories from fat, and daily servings of fruit and vegetables were used as the 3 dietary behavior variables for this analysis.
Physical activity
Participants completed a 7-day physical activity recall at baseline and 6 and 18 months.26 Weekly minutes of physical activity were calculated using the number of minutes of activity reported at a moderate or harder level. A modified Bruce submaximal treadmill test was used to determine participants’ cardiorespiratory fitness at baseline and 6 and 18 months. The measure used to estimate cardiorespiratory fitness was the maximum heart rate achieved during the treadmill test.
Statistical Analysis
Data distributions were tested for normality using q-q plots. Pearson correlation coefficients were calculated to determine the correlations between DSE, ESE, weight, and lifestyle behaviors at baseline.27 Change scores of each of these variables were used to calculate Pearson correlation coefficients for 6- and 18-month follow-up. Relationships that showed significant correlation at 6 or 18 months were included in the mediation analysis. To further explore the differences in self-efficacy scores, tertiles of high, medium, and low scores were created. One-way analysis of variance tests were used to assess the differences in self-efficacy change and weight change based on these groups.
Mediation effects of dietary behavior and physical activity outcomes were analyzed using the test of Barron and Kenny.28 This methodology includes conducting 4 regression equations. The first equation tests that the predictor variable (DSE/ESE change scores) is associated with the outcome (weight loss). The second equation tests the association of the predictor variable to the putative mediator (dietary and physical activity variables). The third equation tests whether the mediator is associated with the outcome. The final equation includes both the predictor variable and the mediator, and tests the association of these as covariates with the outcome. For mediation to be present, each of the first 3 regression equations must produce a significant association. In addition, the beta coefficient of the predictor variable must be reduced to 0 when the mediator is added as a covariate in the fourth equation. Data from the 2 treatment groups were pooled for the mediation analyses, but group assignment was controlled for in all analyses. Age and race were also controlled for in all equations. In the case that the beta coefficient was reduced but not reduced to 0, a Sobel test was conducted, which measures the indirect effect, or the amount of mediation effect present.29,30
RESULTS
Study Population
Participants included 537 adults with a mean ± SD age of 50 ± 8.9 years. A total of 61% of participants were female and 66% were non-Hispanic white. The mean change in weight was −11.4 ± 12.2 lb at 6 months and −8.8 ± 14.5 lb at 18 months (Table 1). Mean self-efficacy scores decreased significantly at each time point for all groups (P < .001). There were no significant differences in self-efficacy scores among treatment groups at any time point.
Table 1.
Change in Weight, Self-efficacy, and Behavior Measures at Baseline and 6 and 12 Months of Participants (n = 537) in Established and Established Plus DASH Groups of PREMIER Trial, Mean (SD)
| Baseline | 6 Months | 18 Months | |
|---|---|---|---|
| Body mass index (kg/m2) | 33.2 (5.9) | 31.2 (5.9) | 31.7 (6.2) |
|
| |||
| Weight (lb) | 210.9 (42.7) | 199.1 (42.5) | 201.2 (44.0) |
|
| |||
| Daily caloric intake (kcal) | 1,957.0 (638.0) | 1,687.4 (526.2) | 1,679.9 (522.5) |
|
| |||
| Daily servings of fruit and vegetable | 4.6 (2.4) | 6.5 (3.2) | 6.1 (3.3) |
|
| |||
| Percent of calories from fat (%) | 33.4 (7.8) | 26.6 (9.0) | 28.2 (8.7) |
|
| |||
| Weekly minutes of moderate to vigorous physical activity | 220.3 (333.5) | 274.9 (272.8) | 260.7 (284.5) |
|
| |||
| Cardiorespiratory fitness (beats/min) | 131.1 (14.6) | 121.8 (15.9) | 121.3 (16.4) |
|
| |||
| Dietary self-efficacy | |||
| Total sample | 119.7 (12.5) | 115.2 (15.0) | 114.6 (15.1) |
| Tertiles (based on baseline scores) | |||
| High | 132.1 (2.5) | 123.2 (13.2) | 122.0 (13.7) |
| Medium | 122.5 (3.3) | 115.2 (14.8) | 115.3 (12.9) |
| Low | 106.0 (9.3) | 108.3 (13.3) | 107.1 (14.6) |
|
| |||
| Exercise self-efficacy | |||
| Total sample | 49.6 (8.2) | 43.7 (10.6) | 43.3 (10.8) |
| Tertiles (based on baseline scores) | |||
| High | 57.8 (2.0) | 48.7 (9.3) | 47.5 (11.1) |
| Medium | 51.0 (2.1) | 44.6 (9.8) | 44.7 (9.6) |
| Low | 40.5 (6.8) | 38.6 (10.3) | 37.9 (9.6) |
DASH indicates Dietary Approaches to Stop Hypertension.
Changes in Self-efficacy
When divided into groups of low, medium, and high self-efficacy scores based on baseline scores, the group with the highest DSE baseline scores had a mean decrease in DSE of 8.9 ± 12.5 points at 6 months. This was significantly different from the group with the lowest baseline scores, which had a mean increase of 2.1 ± 13.6 points at 6 months (P < .001) (Table 1). At 18 months, these differences persisted. The group with the highest baseline scores had a mean decrease of 10.1 ± 13.3 points at 18 months, which was significantly different from the mean increase of 0.7 ± 15.9 (P < .001) seen in the group with the lowest baseline DSE scores.
The group with the highest ESE baseline scores had a mean decrease in ESE of 9.0 ± 9.1 points at 6 months. This was significantly different from the mean decrease of 6.4 ± 9.8 (P < .001) points in the medium group and 1.7 ± 11.2 (P < .001) in the group with the lowest baseline ESE scores. At 18 months, these differences persisted. The group with the highest baseline scores had a mean decrease of 10.4 ± 10.7 (P < .001) points at 18 months, which was significantly different from the mean decrease of 6.4 ± 9.8 (P < .001) points in the medium group and 2.7 ± 10.1 (P < .001) in the group with the lowest baseline ESE scores.
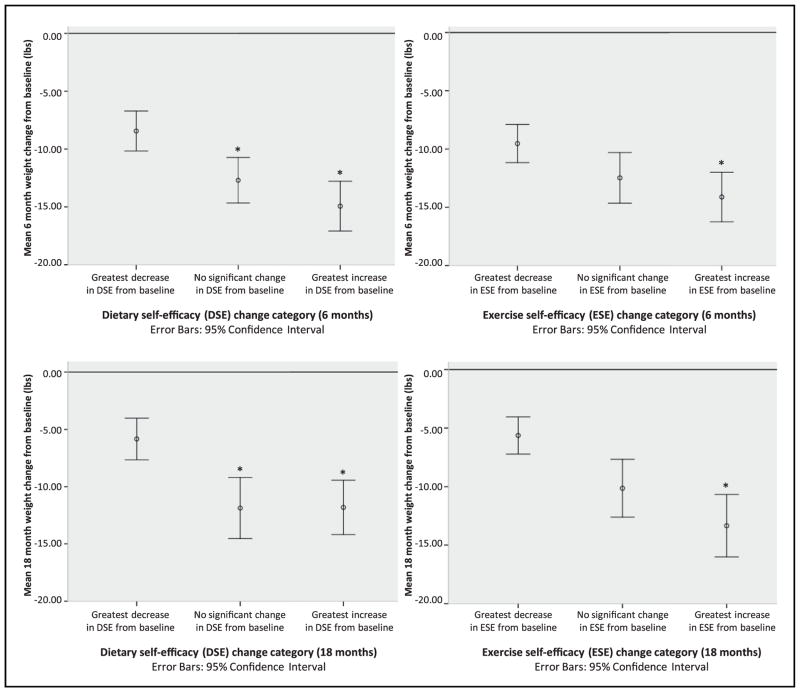
The group with the lowest baseline DSE scores lost significantly more weight at 6 months than the group with the highest baseline DSE scores (P = .01). There was no significant difference in weight loss at 18 months based on baseline DSE scores. There were significant differences based on DSE change scores (Figure 1). At 6 months, the group with the greatest decrease in DSE scores lost 4.3 ± 1.4 lb less than the group with no significant change in DSE and 6.5 ± 1.4 lb less than the group with greatest increase in DSE scores (P = .002). These differences remained significant at 18 months, when the group with the largest decrease in DSE lost 6.0 ± 1.6 lb less than the group with no significant change in DSE and 6.0 ± 1.5 lb less than the group with the greatest increase in DSE (P < .001).
Figure 1.
Differences in weight loss between self-efficacy (SE) tertiles at 6 and 18 months. Groups formed by creating tertiles of change in self-efficacy scores from baseline to follow-up. Tertiles represent greatest increase in SE, no significant change in SE, and greatest decrease in SE. *Significantly different from greatest decrease group at P < .01 level.
There was no significant difference in weight loss at 6 or 18 months based on baseline ESE scores, but there were significant differences at 6 and 18 months based on ESE change scores (Figure 1). At 6 months, the group with the greatest increase in ESE scores lost 4.6 ± 1.4 lb more than the group with the greatest decrease in ESE scores (P = .001). The difference between the groups with the greatest increase and greatest decrease remained significant at 18 months (7.7 ± 1.5 lb) (P < .001).
Relationship Between Self-efficacy and Behavior Change
Correlation coefficients were computed to determine which dietary and exercise variables were significantly associated with DSE/ESE at baseline, as well as correlations between the change scores of these variables and changes in DSE/ESE at 6 and 18 months (Table 2). There was a significant inverse correlation between DSE and daily caloric intake at baseline (r = −0.23; P < .001). There was no significant correlation between change in DSE scores and change in caloric intake at 6 or 18 months. There was a significant inverse correlation between DSE and percent of calories from fat at baseline (r = −0.14; P = .002). Change in percent fat was significantly associated with changes in DSE scores at 6 months (r = −0.11; P = .02), but not at 18 months. Baseline DSE was not significantly correlated with daily servings of fruit and vegetables, but change in daily servings of fruit and vegetables was significantly associated with change in DSE at 6 and 18 months (r = 0.17, P = .001; r = 0.13, P = .007).
Table 2.
Correlationsa Between Change in Self-efficacy, Weight Change, and Behavior Change Measures of Participants in Established and Established Plus DASH Groups in PREMIER Trial (n = 537)
| Independent Variable | Correlation With Change in DSE | Correlation With Change in ESE | ||
|---|---|---|---|---|
| 6 Months | 18 Months | 6 Months | 18 Months | |
| Self-efficacy | ||||
| Change in dietary self-efficacy | .47** | .49** | ||
| Change in exercise self-efficacy | .47** | .49** | ||
|
| ||||
| Change in weight | −.24** | −.16** | −.20** | −.25** |
|
| ||||
| Dietary behaviors | ||||
| Change in daily caloric intake | −.02 | .04 | .06 | .02 |
| Change in daily servings of fruit and vegetables | −.17* | .13* | .09 | .07 |
| Change in % fat | −.11* | −.05 | −.06 | −.03 |
|
| ||||
| Exercise behaviors/fitness measures | ||||
| Change in weekly min of physical activity | .11* | .06 | .05 | .14** |
| Change in cardiorespiratory fitness | −.10* | −.12* | −.09 | −.11* |
DASH indicates Dietary Approaches to Stop Hypertension.
P < .05;
P < .01;
Pearson correlation coefficient.
Baseline ESE was significantly correlated with weekly minutes of physical activity (r = 0.09; P = .04). Change in weekly minutes of physical activity was not significantly correlated with ESE change score at 6 months, but there was a significant correlation at 18 months (r = 0.14; P = .003). Baseline cardiorespiratory fitness was not significantly correlated with baseline ESE. Change in cardiorespiratory fitness was not significantly associated with change in ESE at 6 months, but there was a significant correlation at 18 months (r = −0.11; P = .02).
Mediation Analysis
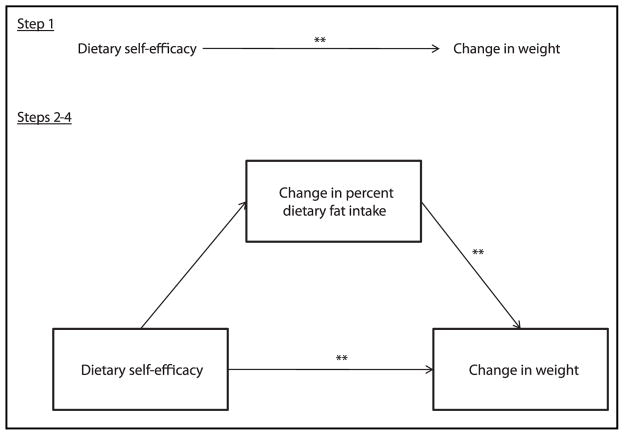
Because change in daily caloric intake did not have a significant association with DSE change, a mediation analysis was not conducted on this variable. Figure 2 shows the results of the dietary mediation analyses. Step 1 established the relationship of DSE as a significant predictor of weight change. The figure shows the beta coefficients and P for the indicated variable in each of the models in steps 2–4 of the analyses. Figures are presented only for those analyses in which steps 1–4 all met significance.
Figure 2.
Mediation analysis for change in percent dietary fat intake at 6 months. *P < .05; **P < .001. Statistical test: Baron and Kenny mediation analysis.28 Step 1 β = −.21; Step 2 β = −.07; Step 3 β = .31; Step 4 β = −.18.
Mediation analyses revealed that change in fruit and vegetable intake did not mediate the relationship between DSE change and weight change at 6 or 18 months. This was because change in DSE did not significantly predict change in fruit and vegetable intake at either time point (β = .02, P = .05 at both time points). Change in percent fat partially mediated the relationship between DSE change and weight change at 6 months. There was a significant initial relationship between DSE change and weight change (β = −.21, P < .001). After controlling for change in percent fat, the magnitude of this association decreased but remained significant (β = −.18, P < .001). The Sobel test confirmed that the decrease was significant (z = −2.13; P = .03).
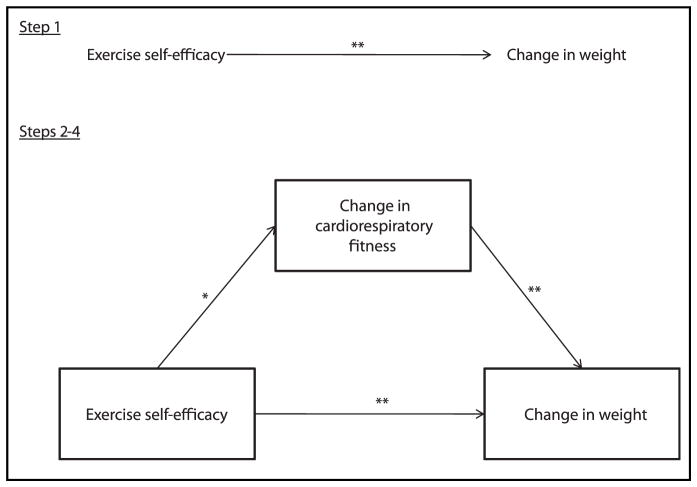
The mediation analyses for minutes of physical activity and cardiorespiratory fitness (Figure 3) indicated that only cardiorespiratory fitness had a partial mediation effect on the relationship between change in ESE and change in weight at 18 months. Change in minutes of physical activity was not significantly associated with change in weight, indicating no mediation effect of this variable. The significant initial relationship between ESE change and weight change decreased but remained significant after controlling for change in cardiorespiratory fitness (β1 = −.35, P < .001; β4 = −.31, P < .001). The Sobel test indicated that this was a significant indirect effect (z = −2.14, P = .03).
Figure 3.
Mediation analysis for change in cardiorespiratory fitness at 18 months. *P < .05; **P < .001. Statistical test: Baron and Kenny mediation analysis.28 Step 1 β = −.35; Step 2 β = −.17; Step 3 β = −.59; Step 4 β = −.31.
DISCUSSION
This study assessed the predictive qualities of DSE and ESE on weight loss at 2 time points. Furthermore, a potential mechanism through which self-efficacy could lead to weight loss was explored. Specifically, this study explored the mediation effects of dietary and exercise behavior changes on this relationship.
Results indicated that baseline weight was correlated with DSE but not ESE. In line with existing literature, participants in this study who had the greatest increase in self-efficacy over the course of the intervention had the greatest weight loss. However, the mean self-efficacy scores of the study sample decreased significantly over time. One reason for the decrease in self-efficacy over time may be related to the magnitude of baseline self-efficacy scores. A small number of studies have discussed the idea of barrier underestimation and the effect of this on change in self-efficacy over the course of an intervention.10,31 Barrier underestimation refers to underestimating the difficulty of changing behavior. An individual may report high self-efficacy beliefs at baseline because of high motivation or lack of experience with a particular behavior. However, when the individual begins to incorporate new behaviors into the daily lifestyle, initiation or maintenance of this particular behavior is not as easy as originally believed. Barrier underestimation has been found to be associated with poor behavior change and weight change outcomes. If those who had the highest self-efficacy at baseline were more likely to underestimate barriers to behavior change, it would potentially explain why this group showed the greatest decline in self-efficacy over time—a decline associated with a 5- to 6-lb difference in weight compared with those with an increase in self-efficacy.
Despite the overall decrease in self-efficacy seen in this study, there was a significant weight loss seen at both 6 and 18 month follow-up points. This indicates that although self-efficacy significantly predict weight loss, weight loss can be achieved in the absence of an increase in self-efficacy. This supports the hypothesis that the path from self-efficacy to weight loss is not direct, and that there is a need for exploration into other factors that mediate the path from self-efficacy to weight loss. Mediation analysis indicated that there was a partial mediation effect of some dietary behavior changes at 6 months, but not at 18 months. The DSE scores were not a significant predictor of fruit and vegetable intake at either time point, and did not predict percent calories from fat at 18 months, which indicates that there is no mediation of these variables on the path from self-efficacy to weight loss. This was an unexpected finding because it indicates that the association between self-efficacy and specific behavior change may differ for various dietary behaviors, and relationships that were significant at 6 months decreased over time. Therefore, it may be that the mechanisms by which self-efficacy leads to initial weight loss may differ from those that lead to long-term weight maintenance.
Because weight loss and weight maintenance are complex health issues composed of a multitude of behavioral, medical, and psychosocial components, other factors may serve a more significant role in the path between self-efficacy and weight loss. For example, Linde et al19 reported full mediating effects of self-monitoring behaviors on the relationship between self-efficacy and weight loss. It may be that these behaviors more fully explain the relationship than adoption of specific dietary and exercise patterns. In addition, there may be multiple factors that mediate the relationship between self-efficacy and behavior change, independent of those that influence weight loss.32–34 Bruening et al33 found that perceived barriers mediated the relationship between self-efficacy and fruit and vegetable intake among a sample of adolescents. Similarly, Nothwehr34 reported that whereas self-efficacy was significantly associated with changes in coping strategies related to dietary behaviors, it was not associated with change in dietary behaviors. In this analysis, there no significant correlation was found between DSE and caloric intake at 6 or 18 months, or between ESE and weekly minutes of physical activity and cardiorespiratory fitness at 6 months. Other correlations between dietary behaviors and self-efficacy, although significant, were lower than expected. Future research will benefit from exploring the impact of other mediators on the relationship between self-efficacy and weight loss, as well as further exploring the mechanisms by which self-efficacy influences behavior change.
The primary limitation of this study is that it was conducted using secondary data analysis. The measures were not specifically designed for this study, and as such may not provide the best possible measures for this study. However, the self-efficacy and behavior change data were collected using direct measures that were intended to measure these constructs, and no proxy measures were used, which increased the quality of the analysis. In addition, the self-efficacy measures used have shown sound criterion validity for measuring dietary and exercise behaviors measured in this study.24 There may be additional variables that are unaccounted for in these mediation models that potentially diminished the effect of self-efficacy on the outcomes observed in this study. These variables could be better accounted for in a future study specifically designed to measure the effect of self-efficacy on behavior change. Second, the PREMIER study intervention was designed as a lifestyle intervention, and therefore, behavioral constructs including self-efficacy were considered when designing the intervention. However, the intervention was not designed with the primary goal of increasing self-efficacy. Using an intervention that directly targets self-efficacy as an outcome, or that tailors the intervention based on baseline self-efficacy scores, may show results different from those found in this study.
IMPLICATIONS FOR RESEARCH AND PRACTICE
This analysis indicated that the lifestyle intervention employed by the PREMIER trial led to significant weight loss, despite a significant mean decrease in self-efficacy scores at both 6 and 18 months. Change in self-efficacy scores were predictive of weight loss outcomes, however, in that participants with the greatest increases in self-efficacy scores had significantly greater weight loss than those whose self-efficacy decreased over time. The results of the mediation analysis indicate that the path from self-efficacy to weight loss may be indirectly affected by adoption of the dietary and physical activity patterns prescribed in this intervention. Nevertheless, the fact that many of the models did not show a significant relationship between self-efficacy and adoption of the specific behavior may indicate that the relationship between self-efficacy and weight loss is too distal to be adequately explained with any given mediator. Rather, future research that explores the mediating factors between self-efficacy and adoption of specific behaviors may lead to a better understanding of how to tailor lifestyle interventions to lead to successful long-term weight loss.
Acknowledgments
At the time of this work, Dr. Wingo was supported, in part, by grant 1 T32 HS019463 from the Agency for Healthcare Research and Quality, Rockville, MD.
References
- 1.Bandura A. Self-efficacy: toward a unifying theory of behavior change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 2.Prochaska JO, Diclemente CC. Stages and process of self-change in smoking: towards an integrative model of change. J Consult Clin Psychol. 1983;51:390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 3.Prochaska JO, Reddind CA, Ever KE. The transtheoretical model and stage of change. In: Glanz K, editor. Health Behavior and Health Education, Theory, Research and Practice. 3. San Francisco, CA: Josey-Bass Publishers; 2002. pp. 99–120. [Google Scholar]
- 4.Rosenstock IM. Why people use health services. Milbank Mem Fund Q. 1966;44:94–127. [PubMed] [Google Scholar]
- 5.Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15:175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 6.Strecher VJ, DeVillis BM, Becker MH, Rosenstock IM. The role of self-efficacy in achieving health behavior change. Health Educ Q. 1986;13:73–91. doi: 10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- 7.Bernier M, Avard J. Self-efficacy, outcome, and attrition in a weight-reduction program. Cognit Ther Res. 1986;10:319–338. [Google Scholar]
- 8.Palmeira AL, Teixeira PJ, Branco TL, et al. Predicting short-term weight-loss using 4 leading health behavior change theories. [Accessed February 6, 2013];Int J Behav Nutr Phys Act. 2007 4:14. doi: 10.1186/1479-5868-4-14. http://www.ijbnpa.org/content/4/1/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fontaine KR, Cheskin LJ. Self-efficacy, attendance, and weight loss in obesity treatment. Addict Behav. 1997;22:567–570. doi: 10.1016/s0306-4603(96)00068-8. [DOI] [PubMed] [Google Scholar]
- 10.Martin PD, Dutton GR, Brantley PJ. Self-efficacy as a predictor of weight change in African-American women. Obes Res. 2004;12:646–651. doi: 10.1038/oby.2004.74. [DOI] [PubMed] [Google Scholar]
- 11.Gallagher KI, Jakicic JM, Napolitano MA, Marcus BH. Psychosocial factors related to physical activity and weight loss in overweight women. Med Sci Sports Exerc. 2006;38:971–980. doi: 10.1249/01.mss.0000218137.25970.c6. [DOI] [PubMed] [Google Scholar]
- 12.Nies MA, Kershaw TC. Psychosocial and environmental influences on physical activity and health outcomes in sedentary women. J Nurs Scholars. 2002;34:243–249. doi: 10.1111/j.1547-5069.2002.00243.x. [DOI] [PubMed] [Google Scholar]
- 13.Nishida Y, Suzuki H, Wang D, Kira S. Psychosocial determinants of physical activity in Japanese female employees. J Occup Health. 2003;45:15–22. doi: 10.1539/joh.45.15. [DOI] [PubMed] [Google Scholar]
- 14.Steptoe A, Rink E, Kerry S. Psychosocial predictors of changes in physical activity in overweight sedentary adults following counseling in primary care. Prev Med. 2000;31:183–194. doi: 10.1006/pmed.2000.0688. [DOI] [PubMed] [Google Scholar]
- 15.National Heart Lung and Blood Institute. Clinical Guidelines on the Identification, Evaluation and Treatment of Overweight and Obesity in Adults: the Evidence Report. Bethesda, MD: National Institutes of Health; 1998. Publication number 98–4083. [PubMed] [Google Scholar]
- 16.National Heart Lung and Blood Institute. The Practical Guide: Identification, Evaluation and Treatment of Overweight and Obesity in Adult. Bethesda, MD: National Institutes of Health; 2000. Publication number 00–4084. [Google Scholar]
- 17.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Warziski MT, Sereika SM, Styn MA, Music E, Burke LE. Changes in self-efficacy and dietary adherence: the impact on weight loss in the PREFER study. J Behav Med. 2008;31:81–92. doi: 10.1007/s10865-007-9135-2. [DOI] [PubMed] [Google Scholar]
- 19.Linde JA, Rothman AJ, Baldwin AS, Jeffery RW. The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Health Psychol. 2006;25:282–291. doi: 10.1037/0278-6133.25.3.282. [DOI] [PubMed] [Google Scholar]
- 20.Svetkey L, Harsha D, Vollmer W, et al. PREMIER: a clinical trial of comprehensive lifestyle modification for blood pressure control: rationale, design and baseline characteristics. Ann Epidemiol. 2003;13:462–471. doi: 10.1016/s1047-2797(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 21.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 22.Funk KL, Elmer PJ, Stevens VJ, et al. PREMIER—A trial of lifestyle interventions for blood pressure control: design and rationale. Health Promot Pract. 2008;9:271–280. doi: 10.1177/1524839906289035. [DOI] [PubMed] [Google Scholar]
- 23.Garrow JS, Webster J. Quetelet’s index (W/H2) as a measure of fatness. Int J Obes. 1985;9:147–153. [PubMed] [Google Scholar]
- 24.Sallis JF, Pinski RB, Grossman RM, Patterson TL, Nader PR. The development of self-efficacy scales for health-related diet and exercise behaviors. Health Educ Res. 1988;3:283–292. [Google Scholar]
- 25.Conway JM, Ingwersen LA, Moshfegh AJ. Accuracy of dietary recall using the USDA five-step multiple-pass method in men: an observational validation study. J Am Diet Assoc. 2004;104:595–603. doi: 10.1016/j.jada.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 26.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 27.Rodgers JL, Nicewander WA. Thirteen ways to look at the correlation coefficient. Am Stat. 1988;42:59–66. [Google Scholar]
- 28.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 29.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 30.Kenny DA. [Accessed January 24, 2013];Mediation. http://davidakenny.net/cm/mediate.htm. Updated April 3, 2012.
- 31.Dibonaventura MD, Chapman GB. The effects of barrier underestimation on weight management and exercise change. Psychol Health Med. 2008;13:111–122. doi: 10.1080/13548500701426711. [DOI] [PubMed] [Google Scholar]
- 32.Dishman RK, Motl RW, Sallis JF, et al. Self-management strategies mediate self-efficacy and physical activity. Am J Prev Med. 2005;29:10–18. doi: 10.1016/j.amepre.2005.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bruening M, Kunik MY, Kenyon D, Davey C, Story M. Perceived barriers mediate the association between self-efficacy and fruit and vegetable consumption among students attending alternative high schools. J Am Diet Assoc. 2010;110:1542–1546. doi: 10.1016/j.jada.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nothwehr F. Self-efficacy and its association with use of diet-related behavioral strategies and reported dietary intake. Health Educ Behav. 2008;35:698–706. doi: 10.1177/1090198106296771. [DOI] [PubMed] [Google Scholar]