Abstract
Throughout the world, cereals have always been recognized as a fundamental food. Human evolution, through the development of cooking, led to the production of food rich in gluten, in order to take full advantage of the nutritional properties of this food. The result has been that gluten intolerance has arisen only in those populations that developed the art of cooking wheat. It is also recognized that wheat, one of the central elements of the Mediterranean diet, cannot be tolerated in some individuals. Among the wheat-related pathologies, coeliac disease is the best known: it is a chronic inflammatory condition affecting the gastrointestinal tract, which develops in genetically predisposed individuals. The most common manifestation is the malabsorption of nutrients. Recently, another wheat-related disease has appeared: non-coeliac gluten sensitivity, defined as the onset of a variety of manifestations related to wheat, rye and barley ingestion, in patients in whom coeliac disease and wheat allergy have been excluded. In this paper we will explore the damaging power of wheat, analysing the harmful process by which it realizes the onset of clinical manifestations associated with wheat-related disorders.
Keywords: Broad spectrum, evolving diseases, coeliac disease, Mediterranean diet, gluten
Introduction
Throughout the world, the foods that have been recognized for centuries as fundamental are cereals, and bread in particular. In fact, a famous proverb says ‘bread and water’, originating from the minimum food that had to be ensured in prisons. There is no doubt that wheat is an important food, and has always been part of the Mediterranean diet, but it is also true that it cannot be tolerated in some individuals. The best known disease related to gluten consumption is coeliac disease.
Coeliac disease is a chronic inflammatory condition affecting the gastrointestinal tract, in particular the small intestine and jejunum; the result of this pathology is an atrophy of the absorbent apparatus (Figure 1) and consequent malabsorption of nutrients.
Figure 1.
(a) normal cytoarchitectonic villus-crypt and absorbent epithelium of the small intestine scanning electron microscopy (left) and histology (right. Emat.cos.80x) (b) subtotal villous atrophy in scanning electron microscopy (left) associated with hyperplasia of the crypts (right. Emat.cos.x80).
Coeliac disease develops in genetically predisposed individuals (10–40% of the general population), and is induced by the ingestion of gluten and triggered by environmental factors.1,2 It occurs in children and adults, with rates close to 1% of the general population even though, in many patients (9/10), the disease remains undiagnosed.3,4 Currently, the diagnosis of coeliac disease is made by three major steps:5 blood tests for gluten autoantibodies (anti-endomysial (EMA), anti-tissue transglutaminase (TTG)), small bowel biopsy to assess gut damage, and implementation of a gluten-free diet.
Currently there is no doubt that gluten, the water-soluble wheat flour, gliadin, its alcohol-soluble subfraction, or the fraction of Frazer III, derived from its peptic-tryptic digestion, are causative agents in coeliac disease (Figure 2(a)).
Figure 2.
Wheat, barley and ‘oats's metabolism Lead to rlie toxic product Gliadine.
In fact, we know that contact of the substance with the intestinal mucosa generates, in some individuals, anatomical damage which variably affects the absorption of the active ingredients introduced by the diet; at the same time, the mechanisms by which this damage is generated are not yet fully understood. Experiments have demonstrated that the chemical hydrolysis of toxic peptides produces solutions that are not toxic, even for carriers of coeliac disease. This has led to the hypothesis that the biochemical defect consists of a genetically determined deficiency of a peptidasic enzyme, normally able to convert the gluten in the non-toxic form.
Gluten as damage factor
Therefore, the hypothesis of intolerance by intestinal mucosa to a particular substance introduced with the food is valid. Biochemical research has identified gliadin as responsible for the harmful action on the absorbent epithelium,6 for an allergic mechanism or specific enzyme deficiencies. Gee, in 1888, was the first to attribute the cause of the disease to a dietary problem. Following this first observation, many years passed until repeated observations and experimental research could specify the problem, supporting the hypothesis. In 1950, Dicke concluded that the disappearance of most of the symptoms in children with coeliac disease occurred after the suppression of maize flour (wheat factor).6 These observations were the starting point for a series of experimental studies7–12 to discover the toxic factor in wheat, barley and in oats (Figure 2(b)).
Numerous studies have shown that not all forms of gliadin, from alpha to omega, have the same toxicity in genetically determined individuals.13 Thus, it was possible to ascertain that the toxic substance was contained and localized in the protein fraction, and in particular, in gluten; this substance contains a water-soluble part, glutenin, and an alcohol-soluble fraction, gliadin. This fraction, coupled to proteins, is the most toxic: it is rich in glutamine (43%), non-toxic in its free part, proline (13%) and small amounts of lysine, methionine, threonine and other amino acids.
Biochemical and experimental studies have shown that the same gliadin loses its toxic power if deaminated by boiling for 45 minutes in a normal solution of hydrochloric acid. In this process, the transformation of 90% of glutamine to glutamic acid and ammonia occurs, by reductive cleavage of the peptide bonds.7,14 The toxicity of gliadin may therefore be due to the presence of the glutamine peptide, while the lipid fraction of the wheat may be harmless.15
Frazer et al.16–18 and Krainick and colleagues19,20 conducted more extensive research. Their studies demonstrated that gluten is a proteic compound, hardly characterizable. In particular, it was difficult to characterize components of the water-soluble fraction (in the presence of salts for peptic and tryptic digestion of gliadin).
Ultrafiltration, however, indicates that 66% of the fraction is composed of peptides of a molecular weight less than 15,000, and that 8% is represented by free amino acids. It is worth considering that chromatography, electrophoresis, dialysis searches and precipitation with trichloroacetic acid indicated that fraction III is not identical to the original gluten. The next step of elimination of residual protein with heat forms a toxicity-unchanged fraction, named IIIS.
It seems that the toxic peptides have a molecular weight between 820 and 928, being composed of 6–7 amino acids, as ultrafiltration of the product of peptic and tryptic digestion of gliadin has demonstrated.19 The incubation of the ultrafiltrate with pork intestinal mucosa leads to the disappearance of its toxicity, through the production of a significant amount of glutamine and proline. There is, therefore, only a fraction composed of unbranched chains of peptides in which the toxic properties of gluten remains unchanged; this fraction was identified after tryptic and peptic digestion of gliadin.21
In conclusion, we can say with Crabbe22 that the chemical characteristics of the toxic substance, extracted from wheat flour, are those that do not contain carbon, lipids, proteins, being composed of short-chain peptides, having a molecular weight less than 15,000, and perhaps 1000, and rich in glutamine and proline. The toxic substances, produced by the different stages of degradation of gluten, lose their toxicity after complete hydrolysis into free amino acids, after deamination by the action of a normal solution of hydrochloric acid or papain, and after incubation with an extract of pork intestinal mucosa; treatments that essentially produce the liberation of substantial quantities of glutamine and proline. These assumptions confirmed, by clinical and laboratory methods, the success obtained by a complete and prolonged gluten-free diet in patients with sprue.23–30
Among the problematic disorders related to gluten, about 6% may be non-coeliac gluten sensitivity, 10% may be wheat allergy, and only 1% is coeliac disease.
Coeliac disease
History
Arateus of Cappadocia in 250 AD reported the first case in history relatable to coeliac disease, describing cases of diarrhoea, weight loss and general decline in children and young adults. Summarizing the most important events about human habits and nutrition, we can identify about 10,000 years ago the start of the domestication of animals, such as dogs and horses, the breeding of livestock (sheep and cattle), and at the same time the cultivation of seeds, representing the first agriculture. Then, in a few thousand years, agriculture arose independently in many areas in the word.
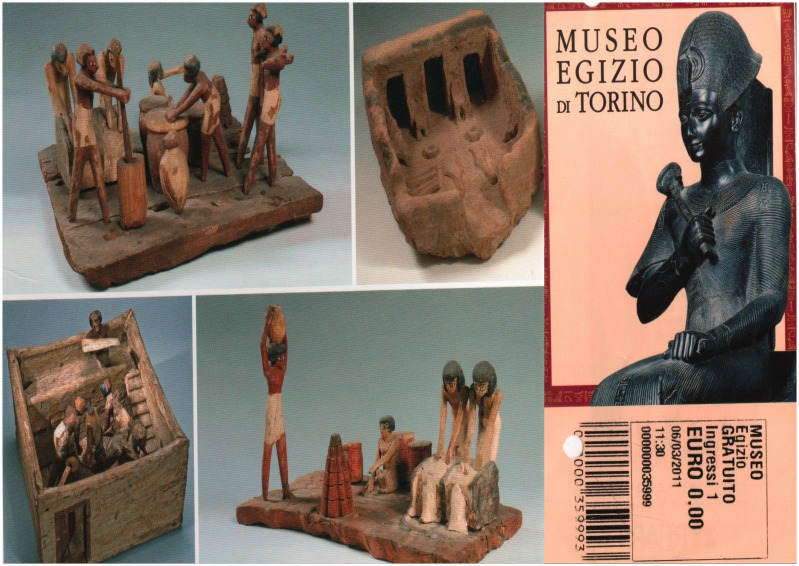
Following the oldest proof, dated about 11,500 years ago in Abu Hureyra (today between Iraq and Syria), in the following millennia the cultivation expanded from the Fertile Crescent to Mesopotamia, in the valley between the Tigris and the Euphrates (Figure 3). In this area, which represents the ideal theatre for Neolithic revolutions and in which were located the great nations of antiquity, such as ancient Egypt, the Levant and Mesopotamia, agricultural civilizations were first developed.
Figure 3.
the ancient use of cereal in Egyptians.
The climate of Fertile Crescent allowed the growth of the ‘eight fundamental Neolithic crops’: emmer, einkorn (progenitor of the modern wheat), barley, flax, chickpeas, peas, lentils and Vicia ervilia (a legume similar to red lentils); it also led to the development of breeding of cows, goats, sheep and pigs, representing four of the five most important species of farm animals (the fifth species, the horse, spread to neighbouring regions but not to the Fertile Crescent).
Homo sapiens expanded his knowledge and his domains to Africa, but also to Europe and the East, reaching Australia and North and maybe South America. In the east of the world, especially in China, the appearance of agriculture was slow for a few thousand years: millet was grown in the north about 9000 years ago and, at the same time, the cultivation of rice began in the south of the region. In Central and South America, agriculture began about 8000 years ago, from the cultivation of corn, squash and beans, and then growing potatoes, tomatoes, cacao and cassava.
About 8000–9000 years ago, agriculture and livestock arrived in North America, before reaching Africa. The spread to the rest of the continent occurred about 4000 years ago, at the same time as the desertification of the Sahara. In Central America, there would have been no cases in that period due to coeliac disease: the fundamental food was maize, considered divine because it arises from the claws of the god Centeol.
Among the prehistoric archaeological sites of Tuscany, there is a particularly interesting area located in Grosseto, especially on the coasts, where crops such as Triticum aestivum / Durum / Durcidum, monococcum / dicoccum / Spelt Horleum Vulgaris, Triticum Spelt, Panicum namely cereals and barley have developed. This occurred in the city of Cosa, located above the Bay of Ansedonia, which includes one of the most interesting sites of the ancient Roman Civilization.
Here, there is the so-called tomb of the interred, a grave, designed to carefully preserve the skeletons from weather and animals, built according to the customs of the time. The grave contains the skeleton of a young woman, adorned with gold and bronze rings on her left hand. The skeleton also has two gold earrings and a small gold button (probably a hatpin for a cape) positioned at the upper chest.31 An anthropological study was made, revealing a very frail physique, and short stature (140–145 cm) in relation to age.32,33 In addition, the research showed some pathological manifestations, such as the presence of orbital cribra, suggesting anaemia, and hypoplasia of the tooth enamel, a non-specific sign of nutritional stress or infection. On this basis, and in the absence of other important information, archaeologists have hypothesized a ‘state of chronic deficiency’ linked to an infectious or parasitic disease, a metabolic imbalance and a malformation, causing stunted growth and organic impairment. A specific diagnosis of coxa valga, characterized by sub-dislocation from congenital hip dysplasia, can be made by detecting the angle between the femoral neck shape axis with the axis of the shaft (inclination angle), which appears wider (135°) than the average found in the adult (125°). To confirm this, there is the flattening of the posterior portion of the posterior acetabular cavity. Analysing the femur’s content, the material derived from the bone marrow is particularly abundant, perhaps expressing a functional hyperplasia, perhaps likely traceable to a protracted state of deficiency (Iron? Calcium? Other nutrients?).
Genetics
The association between the disease and HLA genes, in particular HLA-DQ2 and DQ8, is very strong, especially in comparison with other diseases associated with HLA genes. This has been confirmed by studies showing familial aggregation34 and concordance among monozygotic twins, estimated at around 85%.35 It is necessary to consider, however, that about a third of the general population carries HLA-DQ2, noting that other factors are necessary beyond this gene (Figure 4).36
Figure 4.
Etiopathogenisis of gluten damage.
These include not only environmental factors; it is possible that genes other than HLA may influence the development of coeliac disease. In support of this hypothesis, there is evidence that the association between identical twins is much stronger than that between family members carrying an identical HLA structure. Recent experimental studies have revealed new possible genes involved in the pathogenesis of coeliac disease, including COELIAC337 and COELIAC438, at position 2q33 and 19p13.1. More detailed studies are needed to assess the relationship between these genes and coeliac disease.
There are many pathologies associated with coeliac disease; among these, autoimmune diseases have an important role. One of the first studies that supported this feature was conducted by Cooper and colleagues.39 They found that autoimmune diseases were present in 19% of patients in a group of 57 subjects suffering from coeliac disease. Today, the particular association among coeliac disease and thyroiditis, type I diabetes, inflammatory bowel disease (IBD), Systemic lupus erythematosus (SLE) and Addison’s disease is recognized throughout the world.31
Non-coeliac gluten sensitivity
Non-coeliac gluten sensitivity is a recently identified pathology, defined as the onset of a variety of manifestations related to wheat, rye and barley ingestion, in patients in whom coeliac disease and wheat allergy have been excluded.40 The diagnosis of non-coeliac gluten sensitivity is made in the presence of a symptomatic reaction to gluten with a negative serology, negative immuno-allergy test, normal duodenal biopsy and the resolution of symptoms with a gluten-free diet.41 Volta and De Giorgio proposed the final diagnostic step to diagnose non-coeliac gluten sensitivity, identifying the upswing of symptoms with the reintroduction of wheat in the diet as the final fundamental feature.42
In 1978 Ellis and Linaker described one of the first cases, writing about the history of a patient suffering from abdominal pain and diarrhoea with a normal duodenal histology and a dramatic improvement through a gluten-free diet.43 From that first case, several studies have been developed to assess the phenotypic, genotypic and immune markers of this new entity.
Wahnshaffe and colleagues identified a sub-population of patients with irritable bowel syndrome associated with diarrhoea (IBS-D) carrying the HLA-DQ2 allele, with normal biopsy, who had improvement of symptoms after undergoing a gluten-free diet;44,45 those patients presented immunological alterations (IgA anti-gliadin or anti-TTG), whereas they have been shown normal in an older study carried out by Jones and colleagues.46
A recent comparative study by Sapone et al. has evaluated the differences in gut permeability between coeliac disease and non-coeliac gluten sensitivity.47 The results did not show alterations in gut permeability in patients with non-coeliac gluten sensitivity, unlike those with coeliac disease. Contextually they studied the innate and adaptive immunity expression in coeliac disease and non-coeliac gluten sensitivity, demonstrating a higher presence of IL-6 and IL-21 (adaptive immunity markers) only in coeliac disease while the expression of the innate immunity marker TLR-2 was increased in non-coeliac gluten sensitivity but not in coeliac disease.47
Comment
It has not yet been shown with certainty that the extent of intestinal lesions correlates with the importance of clinical symptoms. This concept applies not only to structural cellular alterations of the villo–crypt axis, but also to those of the intestinal epithelium (even the smallest), of tight junctions (with implications for the gut mucosal barrier), of the lymphatic, endocrine and vascular system, and the bowel lamina propria.
Furthermore, there is still no certainty about the correlation between the extent of the clinical presentation and characteristics of gut microbiota. This is increasingly becoming a factor of crucial importance in bowel disease, both in so-called functional (IBS) and purely inflammatory (IBD); many studies are being undertaken to explore this new aspect.
Finally, we would like to give some practical advice to the clinician, in order to identify and better treat patients suffering from gluten-related diseases (Figure 5):
Perform a thorough medical history, with particular attention to the native gut microbiota (type of birth, breastfeeding);
Extensively explore the symptoms, understanding the psychology of the subject;48
Assess the presence of any history of allergies, anaphylactic shock; assess mediators such as C3 and C4, and the status of the intestinal loops;
Marsh type 1 should not be considered decisive for diagnosis because it can be present in many other diseases;36 Marsh classifications 2, 3, 4 are fundamental for diagnosis, although in our opinion these should be revised;49
The genetic background must be evaluated with great care because it is often important to target or confirm the diagnosis, and in some cases make it unlikely;
It is always necessary to consider the possible presence of an allergy to gluten and, on a practical level, that there may be reactions to non-gluten-tolerant foods when eaten in large amounts, remembering that a gluten-free diet leads to an excessive introduction of carbohydrates and nickel that cannot be well tolerated in those same subjects.
Figure 5.
diagnostic algorithm of celiac Disease.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
None declared.
References
- 1.Corazza GR, Gasbarrini G. Coeliac disease in adults. Baillieres Clin Gastroenterol 1995; 9: 329–350. [DOI] [PubMed] [Google Scholar]
- 2.Gasbarrini G, Malandrino N, Giorgio V, et al. Celiac disease: What's new about it? Digest Dis 2008; 26: 121–127. [DOI] [PubMed] [Google Scholar]
- 3.Bianchi PI, Biagi F, Corazza GR. Histologic evidence for mild lesions in coeliac disease: The challenge is open. Intern Emerg Med 2012; 7: 295–296. [DOI] [PubMed] [Google Scholar]
- 4.Corazza GR, Andreani ML, Biagi F, et al. The smaller size of the ‘coeliac iceberg' in adults. Scand J Gastroenterol 1997; 32: 917–919. [DOI] [PubMed] [Google Scholar]
- 5.Bai JC, Fried M, Corazza GR, et al. World Gastroenterology Organisation global guidelines on celiac disease. J Clin Gastroenterol 2013; 47: 121–126. [DOI] [PubMed] [Google Scholar]
- 6.Dicke WK, Weijers HA, Van De Kamer JH. Coeliac disease. II. The presence in wheat of a factor having a deleterious effect in cases of coeliac disease. Acta Paediatr 1953; 42: 34–42. [DOI] [PubMed] [Google Scholar]
- 7.Van De Kamer JH, Weijers HA, Dicke WK. Coeliac disease. IV. An investigation into the injurious constituents of wheat in connection with their action on patients with coeliac disease. Acta paediatr 1953; 42: 223–231. [DOI] [PubMed] [Google Scholar]
- 8.Weijers HA, Van De Kamer JH. Coeliac disease. III. Excretion of unsaturated and saturated fatty acids by patients with coeliac disease. Acta Paediatr 1953; 42: 97–112. [DOI] [PubMed] [Google Scholar]
- 9.Weijers HA, Van De Kamer JH. Coeliac disease. I. Criticism of the various methods of investigation. Acta Paediatr 1953; 42: 24–33. [DOI] [PubMed] [Google Scholar]
- 10.Weijers HA, Van De Kamer JH. Coeliac disease. VI. A rapid method to test wheat sensitivity. Acta Paediatr 1955; 44: 536–540. [DOI] [PubMed] [Google Scholar]
- 11.Weijers HA, Van De Kamer JH. Coeliac disease. VII. Application and interpretation of the gliadine tolerance curve. Acta Paediatr 1959; 48: 17–24. [PubMed] [Google Scholar]
- 12.Weijers HA, Van De Kamer JH. Some biochemical investigations into the cause of wheat sensitivity in celiac disease. Gastroenterology 1960; 38: 587–591. [PubMed] [Google Scholar]
- 13.Corazza GR, Rawcliffe PM, Frisoni M, et al. Specificity of leucocyte migration inhibition test in coeliac disease. A reassessment using different gluten subfractions. Clin Exp Immunol 1985; 60: 117–122. [PMC free article] [PubMed] [Google Scholar]
- 14.Crabbe P. [Nontropical Sprue: Etiology and Pathogenesis]. Acta Gastroenterol Belg 1964; 27: 7–18. [PubMed] [Google Scholar]
- 15.Alvey C, Anderson CM, Freeman M. Wheat gluten and coeliac disease. Arch Dis Child 1957; 32: 434–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frazer AC. Mechanism of intestinal absorption of fat. Nature 1955; 175: 491–493. [DOI] [PubMed] [Google Scholar]
- 17.Frazer AC. Fat absorption and its disorders. Br Med Bull 1958; 14: 212–220. [DOI] [PubMed] [Google Scholar]
- 18.Frazer AC, Fletcher RF, Ross CA, et al. Gluten-induced enteropathy: The effect of partially digested gluten. Lancet 1959; 2: 252–255. [DOI] [PubMed] [Google Scholar]
- 19.Krainick HG, Debatin F, Gautier E, et al. [Additional research on the injurious effect of wheat flour in celiac disease.I. Acute gliadin reaction (gliadin shock)]. Helv Paediatr Acta 1958; 13: 432–454. [PubMed] [Google Scholar]
- 20.Krainick HG, Mohn G. [Further investigations on the toxic effect of wheat flour in celiac disease. 2. Effect of enzymatic by-products of gliadin]. Helv Paediatr Acta 1959; 14: 124–140. [PubMed] [Google Scholar]
- 21.van Roon J, Haex AJ, Seeder WA, et al. Clinical and biochemical analysis of gluten toxicity. I. Experientia 1960; 16: 209–209. [DOI] [PubMed] [Google Scholar]
- 22.Crabbe P. [Non-Tropical Sprue: Diagnostic Criteria]. Rev Med Chir Mal Foie 1964; 39: 307–318. [PubMed] [Google Scholar]
- 23.Gruttner R, Mellin R, Bramstedt F. [Studies on appearance of serum peptides in celiac disease]. Klin Wochenschr 1959; 37: 237–240. [DOI] [PubMed] [Google Scholar]
- 24.Anderson CM. Histological changes in the duodenal mucosa in coeliac disease. Reversibility during treatment with a wheat gluten free diet. Arch Dis Child 1960; 35: 419–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.French DL, Coller BS, Usher S, et al. Prenatal diagnosis of Glanzmann thrombasthenia using the polymorphic markers BRCA1 and THRA1 on chromosome 17. Br J Haematol 1998; 102: 582–587. [DOI] [PubMed] [Google Scholar]
- 26.Gerrard JW, Marko AM, Buchan D. Glutamic acid derivatives in juvenile and adult celiac disease. I. Plasma glutamic acid levels after a gliadin tolerance test. CMAJ 1960; 83: 1321–1323. [PMC free article] [PubMed] [Google Scholar]
- 27.Buchan DJ, Gerrard JW. Celiac disease. Problems in diagnosis and effects of a gluten free diet. Ann Intern Med 1962; 57: 85–95. [DOI] [PubMed] [Google Scholar]
- 28.Buchan DJ, Gerrard JW. Peroral jejunal biopsy. CMAJ 1961; 85: 1301–1303. [PMC free article] [PubMed] [Google Scholar]
- 29.Lederer J, Delcourt A, Duret R. [Dietetics and sprue]. Acta Gastroenterol Belg 1962; 25: 253–264. [PubMed] [Google Scholar]
- 30.Bayless TM, Yardley JH, Hendrix TR. Adult celiac disease: Treatment with a gluten-free diet. Serial metabolic and pathologic studies in six patients. Arch Intern Med 1963; 111: 83–92. [DOI] [PubMed] [Google Scholar]
- 31.Gasbarrini GB, Mangiola F, Gerardi V, et al. Coeliac disease: an old or a new disease? History of a pathology. Intern Emerg Med 2014; doi:10.1007/s11739-013-1044-5. [DOI] [PubMed]
- 32.Gasbarrini G, Rickards O, Martinez-Labarga C, et al. Origin of celiac disease: How old are predisposing haplotypes? World J Gastroenterol 2012; 18: 5300–5304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Frezza D, Giambra V, Cianci R, et al. Increased frequency of the immunoglobulin enhancer HS1,2 allele 2 in coeliac disease. Scand J Gastroenterol 2004; 39: 1083–1087. [DOI] [PubMed] [Google Scholar]
- 34.Corazza G, Valentini RA, Frisoni M, et al. Gliadin immune reactivity is associated with overt and latent enteropathy in relatives of celiac patients. Gastroenterology 1992; 103: 1517–1522. [DOI] [PubMed] [Google Scholar]
- 35.Nistico L, Fagnani C, Coto I, et al. Concordance, disease progression, and heritability of coeliac disease in Italian twins. Gut 2006; 55: 803–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Di Sabatino A, Corazza GR. Coeliac disease. Lancet 2009; 373: 1480–1493. [DOI] [PubMed] [Google Scholar]
- 37.Holopainen P, Naluai AT, Moodie S, et al. Candidate gene region 2q33 in European families with coeliac disease. Tissue Antigens 2004; 63: 212–222. [DOI] [PubMed] [Google Scholar]
- 38.Monsuur AJ, de Bakker PI, Alizadeh BZ, et al. Myosin IXB variant increases the risk of celiac disease and points toward a primary intestinal barrier defect. Nat Genet 2005; 37: 1341–1344. [DOI] [PubMed] [Google Scholar]
- 39.Cooper BT, Holmes GK, Cooke WT. Coeliac disease and immunological disorders. BMJ 1978; 1: 537–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ludvigsson JF, Leffler DA, Bai JC, et al. The Oslo definitions for coeliac disease and related terms. Gut 2013; 62: 43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sapone A, Bai JC, Ciacci C, et al. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Med 2012; 10: 13–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Volta U, De Giorgio R. New understanding of gluten sensitivity. Nat Rev Gastroenterol Hepatol 2012; 9: 295–299. [DOI] [PubMed] [Google Scholar]
- 43.Ellis A, Linaker BD. Non-coeliac gluten sensitivity? Lancet 1978; 1: 1358–1359. [DOI] [PubMed] [Google Scholar]
- 44.Wahnschaffe U, Ullrich R, Riecken EO, et al. Celiac disease-like abnormalities in a subgroup of patients with irritable bowel syndrome. Gastroenterology 2001; 121: 1329–1338. [DOI] [PubMed] [Google Scholar]
- 45.Wahnschaffe U, Schulzke JD, Zeitz M, et al. Predictors of clinical response to gluten-free diet in patients diagnosed with diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol 2007; 5: 844–850; quiz 769. [DOI] [PubMed] [Google Scholar]
- 46.Jones VA, McLaughlan P, Shorthouse M, et al. Food intolerance: a major factor in the pathogenesis of irritable bowel syndrome. Lancet 1982; 2: 1115–1117. [DOI] [PubMed] [Google Scholar]
- 47.Sapone A, Lammers KM, Casolaro V, et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: Celiac disease and gluten sensitivity. BMC Med 2011; 9: 23–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Addolorato G, Leggio L, D'Angelo C, et al. Affective and psychiatric disorders in celiac disease. Digest Dis 2008; 26: 140–148. [DOI] [PubMed] [Google Scholar]
- 49.Corazza GR, Villanacci V. Coeliac disease. J Clin Pathol 2005; 58: 573–574. [DOI] [PMC free article] [PubMed] [Google Scholar]