Abstract
Objectives
To describe rates of Medicaid-funded services provided by orthodontists in Iowa to children and adolescents, identify factors associated with utilization, and describe geographic barriers to care.
Methods
We analyzed enrollment and claims data from the Iowa Medicaid program for a 3-year period, January 2008 through December 2010. Descriptive, bivariate, and multivariable logistic regression analyses were performed with utilization of orthodontic services as the main outcome variable. Service areas were identified by small area analysis in order to examine regional variability in utilization.
Results
The overall rate of orthodontic utilization was 3.1 percent. Medicaid enrollees living in small towns and rural areas were more likely to utilize orthodontic services than those living in urban areas. Children who had an oral evaluation by a primary care provider in the year prior to the study period were more likely to receive orthodontic services. Service areas with lower population density and greater mean travel distance to participating orthodontists had higher utilization rates than smaller, more densely populated areas.
Conclusions
Rural residency and increased travel distances do not appear to act as barriers to orthodontic care for this population. The wide variability of utilization rates seen across service areas may be related to workforce supply in the form of orthodontists who accept Medicaid-insured patients. Referrals to orthodontists from primary care dentists may improve access to specialty care for Medicaid enrollees.
INTRODUCTION
Access to orthodontic treatment for low-income children in the United States has been mandated by the Early and Periodic Screening, Diagnosis and Treatment Program since 1967 (1). Despite federally required coverage, minority and low-income children are consistently found to utilize orthodontic services at lower rates than white, affluent children while demonstrating higher levels of treatment need (2-5). Limited research has examined the effects of geographic barriers on the receipt of specialty dental care.
In 2004, approximately 6 percent of US children and adolescents insured through Medicaid received orthodontic care, compared with 17 percent of privately insured youth (3). Rates of orthodontic utilization by publicly insured children and adolescents vary considerably by state. Less than 1 percent of Medicaid eligible children in Washington State received orthodontic treatment in 1999 (6) and less than .5 percent of Medicaid eligible children in North Carolina received orthodontic treatment from 2002 to 2003 (7). These rates are especially low given estimates that approximately 14 percent of all children and 29 percent of adolescents have severe or very severe handicapping malocclusions (7).
Among all income groups, utilization rates vary substantially with race and ethnicity. Even after adjusting for income and insurance status, black and Hispanic children are less likely to have a history of orthodontic treatment than whites (2,3,8). Despite these differences in the receipt of orthodontic treatment, professionally defined need for treatment has been found to be similar among all racial and ethnic groups, with black youth demonstrating a greater proportion of individuals categorized as having severe need for treatment (9).
Patient gender and age also demonstrate associations with orthodontic service utilization rates. Females consistently receive treatment at higher rates than males, even though clinical data suggest that need may be greater among males (3,5,8). Nationally, active receipt of orthodontic services peaks at age 14 and is highest for the age group including 12- to 18-year-olds (3,10).
A component of orthodontic need depends heavily on the subjective perceptions of patients, parents, and providers. A child and his or her family must consider a malocclusion aesthetically or functionally severe enough to seek treatment, a dentist must concur, and then accept or refer the case for treatment. This relationship is further complicated for those with public insurance. Child, family, orthodontist, and the state agent for case review must agree on treatment need. Approval for treatment in Iowa requires case review based on the process described by Salzmann (11) and is approved for the “most handicapping malocclusions only” (12). Conditions are considered to be handicapping if they are potentially detrimental to oral health or an individual’s well-being through temporomandibular joint dysfunction, mastication impairment, increased risk of periodontal disease or caries, or speech impairment.
Recent changes in Iowa Medicaid have increased the case complexity required for approval of orthodontic treatment. These changes may limit the orthodontic care that can be provided by a general or pediatric dentist for Medicaid children. The Iowa Medicaid program covers orthodontic services for individuals through age 20. In addition to strict guidelines for approval of orthodontic services, access to care is also limited through low Medicaid participation of dentists, especially specialists. One study found that fewer than 10 percent of North Carolina orthodontists submitted claims for at least 10 Medicaid patients during a 3-month period during 2005 (7). It is unknown how Medicaid participation by orthodontists varies with urban or rural practice location. While previous research has found utilization to be higher among children living in urban areas than those living in rural areas (8,13), it is unclear whether this is due to variation in patient demand or variation in the supply of services offered by providers.
Variation in utilization of health services can be examined using small area analysis, which defines local health market areas by examining the population’s use of common resources such as hospitals and physicians (14). This approach to identifying market areas has been employed in medical research since the 1950s in the United States and is the foundation for research that examines regional variation in medical expenditures and utilization (14,15). Despite its longstanding use in medicine, the application of small area analysis to examine variation in oral health services is nearly nonexistent.
We hypothesize that variation in utilization of orthodontic services among Medicaid children and adolescents is a function of individual need, demand, and access to care. The goal of this study is to describe rates of Medicaid-funded services provided by orthodontists in Iowa to children and adolescents, identify patient and family characteristics associated with utilization, and describe geographic variation in utilization. We will identify dental service area (DSA) boundaries at the zip code level in order to account for regional variation in orthodontic access and demand. Incorporating information about local market areas will allow us to control for regional characteristics that may affect perceived need and ability to access care. Our primary interests are the associations between urbanicity, travel distance, and the receipt of orthodontic services.
METHODS
This study used a retrospective cohort design to examine access to orthodontic services among Medicaid-enrolled children and adolescents in the Iowa Medicaid program during 2008-2010.
Data
We analyzed data from Iowa Medicaid enrollment and claims files from calendar years (CYs) 2008-2010 to examine rates of orthodontic utilization. The claims files included all claims submitted to Iowa Medicaid by orthodontists for services rendered to Medicaid-enrolled children. Dental services were coded using Current Dental Terminology (CDT). Medicaid enrollment files were obtained for all individuals who met the inclusion criteria described below. After claims data and enrollment data were linked, personal identifiers were removed in order to protect confidentiality. This study was approved by the University of Iowa Institutional Review Board.
Study population
This study focused on Medicaid-enrolled children and adolescents who were ages 6 to 18 years (hereafter referred to as “children”) during CY 2008-2010. Because the utilization rate for 3- to 5-year-olds was so low (<0.01 percent), this age group was not included in our analyses. The study population was limited to individuals eligible for Medicaid through Supplemental Security Income or based on income eligibility requirements. Rates of orthodontic utilization were examined among individuals who were continuously enrolled in the Iowa Medicaid program for at least 11 months during the study period. Age was calculated at the beginning of this qualifying enrollment period. The period of continuous enrollment is designed to correspond to the Healthcare Effectiveness Data and Information Set (HEDIS) requirement for children to be continuously insured for at least 11 months during the study period, as specified in HEDIS protocols (16).
DSAs
DSAs were identified using claims data submitted by orthodontists for care provided to all eligible Medicaid-enrolled children. Zip code level data provided on the first claim per individual were used to identify the Medicaid enrollees’ residential and orthodontists’ practice locations. DSA boundaries were generated using the methods of small area analysis described by Wennberg and Gittelsohn (17). A minimum of 10 Medicaid enrollees who utilized orthodontic services was set as a service area threshold in order to protect confidentiality and to produce reliable statistics. Zip codes containing no enrollees who utilized orthodontic services were assigned to the nearest provider destination as identified by road network analysis. The initial DSA assignments were adjusted to improve contiguity of service area boundaries. Zip code tabulation area (ZCTA) shapefiles from the US Census Bureau were used to approximate zip code geographic boundaries.
Study variables
The dependent variable of interest was whether a child utilized orthodontic services during the study period. Utilization was identified as submission of a claim by an orthodontist to Iowa Medicaid on behalf of a continuously enrolled individual for CDT codes D8010 through D8693. We examined individual and family demographic and socioeconomic characteristics as predictors of orthodontic utilization including age, sex, race/ethnicity, Medicaid eligibility program, and family poverty level. Race/ethnicity is optionally reported by parents to Iowa Medicaid in the enrollment files. This was categorized as white, black, Hispanic, other, and unknown or missing. Other individual predictors included length of enrollment during the study period (36 months versus 11-35 months) and whether a child received an oral evaluation by a primary care dentist during 2007.
Primary care dental visits were identified by the submission of a Medicaid claim by a general or pediatric dentist for a routine or comprehensive oral exam in 2007 (D0120, D0145, or D0150). Receipt of a primary care oral evaluation was hypothesized to be positively associated with the likelihood of utilizing orthodontic services. Previous research has indicated that orthodontists are more likely to accept Medicaid patients if they are referred by another dentist (18).
The urbanicity of each Medicaid enrollee’s place of residence was measured using rural-urban commuting area (RUCA) codes. RUCA codes identify census tracts or zip codes as metropolitan (urbanized area), micropolitan (nonmetro, urban cluster of at least 10,000 people), small town (urban cluster of 2,500-10,000), and rural (no urban cluster, or urban cluster <2,500) (19). Zip code approximations of census tract-based RUCA codes were obtained from the University of Washington (20) and linked with residential zip codes.
Service area level variables were created, including rates of orthodontic utilization, mean travel distance between patient zip codes of origin and provider zip code destination (weighted by the total Medicaid-enrolled population per zip code), primary care dentist-to-population ratios, and population density. Population density was used as a measure of service area urbanicity.
Statistical analysis
We generated descriptive statistics of the study population and the comparison groups (utilizers versus non-utilizers). Chi-square tests and analyses of variance were used to evaluate bivariate relationships between demographic and socioeconomic variables and orthodontic utilization. Multivariable logistic regression was used to examine the relationship between residential urbanicity and orthodontic utilization while adjusting for known predictors of utilization.
Maps were generated to examine geographic variation in orthodontic utilization rates across service areas. DSAs were linked with ZCTA population data from the 2010 US Census and workforce data from the 2010 Iowa Dentist Tracking System (IDTS). IDTS maintains current information about licensed dentists actively practicing in the state (21). Service areas were grouped into quartiles of increasing orthodontic utilization rates. Characteristics were summarized for each quartile using counts, means, and proportions of service area-level characteristics.
Statistical analyses were performed using IBM SPSS Statistics 20 (IBM Corporation, Armonk, NY, USA). Road network analysis and the generation of service area boundaries were conducted using ArcGIS 10.0 (Esri, Redlands, CA, USA). A significance level of.05 was used in all hypothesis tests.
RESULTS
During 2008-2010, there were 116,330 children and adolescents who were continuously enrolled for at least 11 months in the Iowa Medicaid program. The overall rate of orthodontic utilization among the study population was 3.1 percent. The most commonly billed procedures, excluding radiographs, were for comprehensive orthodontic treatment (CDT D8070 and D8080). Fewer than 4 percent of the utilizers received interceptive treatment (n = 137), and there were no claims submitted during 2008-2010 for limited orthodontic treatment.
The majority of children in the study population were white (57.4 percent), although approximately 22 percent had missing data for race/ethnicity (Table 1). Mean length of enrollment for children who met the 11-month minimum enrollment requirement was 28 months [standard deviation (SD) 8.9]; 40 percent of children were enrolled for the entire 36-month period. Orthodontic utilizers differed significantly from non-utilizers by age, sex, race/ethnicity, length of enrollment, aid category, and poverty level. Utilizers were also significantly more likely to have had an oral evaluation by a primary care provider during the year before the study period. A significantly greater proportion of females received orthodontic services than males. White children accounted for 67.6 percent of the population with a visit, even though they comprised 57.4 percent of the study population. Individuals who received orthodontic services were significantly more likely to have been enrolled for the entire year preceding the study period and more likely to have been enrolled for the duration of 2008 through 2010 (36 months). Children living in small towns and rural areas were significantly more likely to have received orthodontic services than those living in metropolitan and micropolitan areas.
Table 1.
Description of continuously enrolled Iowa Medicaid children ages 6 through 18 years (2008-2010) and significance testing results between orthodontic utilizers and non-utilizers by Chi-square analysis
|
Total population N=116,330 |
Ortho non- utilizers N=112,749 |
Ortho utilizers N=3,581 |
Significance | |
|---|---|---|---|---|
| Variable | N(%) | |||
|
Age Mean ± SD 6-9 years 10-13 14-18 |
11.4 ± 3.7 43,315 (37.2) 35,355 (30.4) 37,660 (32.4) |
11.7 ± 3.7 42,593 (37.8) 33,223 (29.5) 36,933 (32.8) |
11.5 ± 2.4 722 (20.2) 2,132 (59.5) 727 (20.3) |
0.053 |
|
Sex Female Male |
59172 (50.9) 57158 (49.1) |
57059 (50.6) 55690 (49.4) |
2113 (59.0) 1468 (41.1) |
<0.0001 |
|
Race/ethnicity White Black Hispanic Other Unknown/missing |
66780 (57.4) 9904 (8.5) 10078 (8.7) 3797 (3.3) 25771 (22.2) |
64360 (57.1) 9760 (8.7) 9798 (8.7) 3699 (3.3) 25132 (22.3) |
2420 (67.6) 144 (4.0) 280 (7.8) 98 (2.7) 639 (17.8) |
<0.0001 |
|
Length of enrollment (2008-2010) Mean ± SD (months) 11-35 months 36 months |
28.0 ± 8.9 69839 (60.0) 46491 (40) |
27.9 ± 9.0 68123 (60.4) 44626 (39.6) |
30.7 ± 7.7 1716 (47.9) 1865 (52.1) |
<0.0001 |
|
Previous enrollment (2007) 0 months 1-11 months 12 months |
32531 (28.0) 27320 (23.5) 56479 (48.6) |
31769 (28.2) 26510 (23.5) 54470 (48.3) |
762 (21.3) 810 (22.6) 2009 (56.1) |
<0.0001 |
|
Medicaid aid category Income eligible SSI |
111072 (95.5) 5258 (4.5) |
107590 (95.4) 5159 (4.6) |
3482 (97.2) 99 (2.8) |
<0.0001 |
|
Federal Poverty Level (FPL) 0% 1-133% > 133% |
31261 (26.9) 81179 (69.8) 3,866 (3.3) |
30568 (27.1) 78403 (69.6) 3,754 (3.3) |
693 (19.4) 2776 (77.5) 112 (3.1) |
<0.0001 |
|
Primary care oral evaluation (2007) Yes No |
37190 (32.0) 79140 (68.0) |
35550 (31.5) 77199 (68.5) |
1640 (45.8) 1941 (54.2) |
<0.0001 |
|
Urbanicity of residential zip code Metropolitan Micropolitan Small town Rural |
58255 (50.1) 20630 (17.7) 20826 (17.9) 16619 (14.3) |
56730 (50.3) 20090 (17.8) 20023 (17.8) 15906 (14.1) |
1525 (42.6) 540 (15.1) 803 (22.4) 713 (19.9) |
<0.0001 |
After adjusting for covariates in the logistic regression model, children living in small towns and rural areas of Iowa were significantly more likely to have received orthodontic services than those living in metropolitan or micropolitan areas (Table 2). Children with a primary care visit in 2007 were significantly more likely to have received orthodontic services during the study period than those with no visit (odds ratio = 1.60). Children between the ages of 10 and 13 were the most likely age group to receive orthodontic services.
Table 2.
Multivariable logistic regression model for orthodontic utilization by Medicaid-enrolled children and adolescents, ages 6-18, during CY 2008-2010
| Odds Ratio | 95% Confidence Interval |
Significance | |
|---|---|---|---|
|
Age 6-9 years 10-13 14-18 |
1 3.86 1.31 |
- 3.54 – 4.21 1.18 – 1.46 |
- <0.0001 <0.0001 |
|
Sex Female Male |
1.46 1 |
1.36 – 1.56 - |
<0.0001 - |
|
Race/ethnicity White Black Hispanic Other Unknown/missing |
1 .46 .84 .81 .86 |
- .39 - .55 .74 - .95 .66 - .99 .79 - .94 |
- <0.0001 0.007 0.042 0.001 |
|
Length of enrollment (2008-2010) 11-35 months 36 months |
1 1.37 |
- 1.28 – 1.47 |
- <0.0001 |
|
FPL 0% 1-133% > 133% |
1 1.27 1.22 |
- 1.17 – 1.39 1.00 – 1.50 |
- <0.0001 .056 |
|
Primary care oral evaluation (2007) Yes No |
1.58 1 |
1.47 – 1.69 - |
<0.0001 - |
|
Urbanicity of residential zip code Metropolitan Micropolitan Small town Rural |
1 0.94 1.36 1.46 |
- 0.85 – 1.04 1.23 – 1.47 1.33 – 1.61 |
- 0.227 <0.0001 <0.0001 |
In order to facilitate comparisons, the 2010 Medicaid claims data were compared with the IDTS for that year. The IDTS maintains information about all licensed dentists actively practicing in the state. Forty-two of the 85 licensed orthodontists (49.4 percent) practicing in Iowa during 2010 submitted a claim to Medicaid during that year. Mean number of Medicaid-enrolled children treated by these providers in 2010 was 40.2 (SD 41.8) and ranged from 1 to 185. Thirty-two orthodontists submitted claims to Medicaid for the treatment of 10 or more individuals.
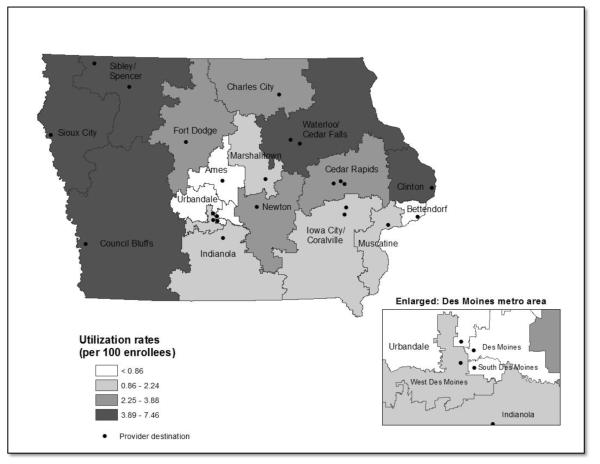
After aggregating zip codes based on where a plurality of Medicaid-enrolled children received orthodontic treatment, 19 DSAs were created (Figure 1). Descriptive characteristics of orthodontic DSAs are provided in Table 3. Service areas are named for the provider location within each DSA. Mean number of zip codes per DSA was 49.2 (SD 36.2). The Council Bluffs DSA included 145 zip codes – the most of any service area. Council Bluffs also had the greatest total population (n = 284,501). The smallest service area in terms of number of zip codes (n = 3) and total population (n = 63,726) was South Des Moines. Mean travel distance per DSA ranged from 5.1 miles to 49.2 miles. Three service areas in the Des Moines metro area had the shortest mean travel distances (5.12-5.83 miles). The greatest mean travel distances were found in the Council Bluffs DSA (41.9 miles) and the Iowa City/Coralville DSA (49.2 miles).
Figure 1.
Orthodontic dental service areas (DSAs) in Iowa (n=19)
Table 3.
Descriptive characteristics of orthodontic DSAs
| DSA | Recipient zip codes (n) |
Medicaid enrollees (n) |
Ortho utilizers (% of enrollees) |
Weighted‡ travel distance (miles) |
Total population (2010) |
Population density |
Land area (square miles) |
Medicaid orthodontists (2010) |
|---|---|---|---|---|---|---|---|---|
| Ames | 27 | 2687 | .60 | 10.85 | 116450 | 89.9 | 1295 | 1 |
| Bettendorf | 15 | 7465 | .86 | 8.47 | 156980 | 458.2 | 343 | 1 |
| Cedar Rapids | 65 | 9538 | 3.23 | 13.93 | 292061 | 97.6 | 2992 | 7 |
| Charles City | 54 | 4123 | 3.52 | 30.33 | 115511 | 32.2 | 3586 | 2 |
| Clinton | 26 | 2971 | 5.25 | 13.17 | 70695 | 48.5 | 1459 | 1 |
| Council Bluffs | 145 | 12659 | 6.26 | 41.87 | 284501 | 27.6 | 10305 | 4 |
| Des Moines | 16 | 10232 | .50 | 5.36 | 210574 | 875.2 | 241 | 2 |
| Fort Dodge | 65 | 4382 | 3.63 | 22.07 | 104631 | 26.4 | 3970 | 1 |
| Indianola | 63 | 4296 | 1.79 | 36.62 | 102593 | 24.4 | 4214 | 1 |
| Iowa City/Coralville | 88 | 11211 | 1.26 | 49.18 | 306321 | 57.0 | 5376 | 5 |
| Marshalltown | 31 | 3542 | 1.07 | 16.22 | 70825 | 39.3 | 1800 | 1 |
| Muscatine | 28 | 5312 | 2.24 | 26.20 | 101417 | 71.4 | 1420 | 2 |
| Newton | 44 | 4573 | 3.21 | 27.07 | 125219 | 44.3 | 2829 | 1 |
| Sibley/Spencer | 63 | 3700 | 7.46 | 30.28 | 97522 | 22.8 | 4284 | 2 |
| Sioux City | 68 | 8188 | 6.19 | 17.25 | 190191 | 42.4 | 4488 | 3 |
| South Des Moines | 3 | 3862 | .85 | 5.12 | 63726 | 1543.0 | 41 | 1 |
| Urbandale | 19 | 2664 | .49 | 14.03 | 132549 | 145.6 | 910 | 2 |
| Waterloo/Cedar Falls | 104 | 13143 | 3.89 | 40.35 | 377504 | 59.5 | 6350 | 6 |
| West Des Moines | 11 | 1782 | 1.52 | 5.83 | 109432 | 331.9 | 330 | 2 |
Weighted by the number of Medicaid enrollees ages 6-18 years per zip code.
Grouping orthodontic DSAs into quartiles of increasing utilization rates allowed us to compare findings from the individual-level analysis with the geographic variation seen across the state (Table 4). The service area analysis supported the results of the logistic regression model that demonstrated increased utilization rates among children living in small towns and rural areas. Service areas with the lowest utilization rates had the greatest mean population density (566 people per square mile), whereas the DSAs with the highest utilization rates were the least densely populated. Additionally, areas with the lowest utilization rates had the largest minority populations.
Table 4.
Descriptive characteristics of orthodontic DSAs grouped by quartiles of utilization rates
| Low utilization rates |
Medium low utilization rates |
Medium high utilization rates |
High utilization rates |
|
|---|---|---|---|---|
| Mean utilization rate per 100 Medicaid enrollees | 0.66 | 1.58 | 3.40 | 5.81 |
| Number of service areas in quartile | 5 | 5 | 4 | 5 |
| Mean population density (per square mile) | 622.4 | 104.8 | 50.1 | 40.1 |
| Mean geographic area (square miles) | 566.0 | 2628.0 | 3344.1 | 5376.9 |
| Mean total population, 2010 (n) | 136,056 | 138,118 | 159,356 | 204,083 |
| White population (%) | 46.2 | 55.7 | 68.9 | 63.1 |
| Black population (%) | 13.3 | 4.6 | 4.9 | 5.7 |
| Hispanic population (%) | 10.2 | 11.5 | 4.4 | 10.1 |
| Mean travel distance to orthodontist (miles) | 8.8 | 26.8 | 23.4 | 28.6 |
A sensitivity analysis was conducted to examine the effects of combining the three smallest Des Moines metro service areas: West Des Moines, Des Moines, and South Des Moines (see enlarged area, Figure 1). A combined Des Moines DSA would have the largest total service area population (n = 383,732) and the fourth lowest utilization rate (0.70 percent). Substantial variation in utilization rates would be obscured by combining these three metro DSAs, which displayed utilization rates of 0.50 to 1.52 percent. While geographically large DSAs (e.g., Council Bluffs) have the potential to obscure local variation in utilization rates, it should be noted that providers serving this population were located in only one zip code within the DSA. The high utilization rate found in Council Bluffs was due to several orthodontists located in close geographic proximity providing services to a large number of Medicaid-enrolled children during the study period.
DISCUSSION
Overall, approximately 3 percent of our study population received care from orthodontists during the study period. This figure is less than the national average of 6 percent reported for Medicaid-enrolled children and 17 percent for privately insured children.
The Medicaid program in Iowa offers coverage to children from low-income families for specialty dental care including orthodontics. Evidence of increased orthodontic utilization among females and among white children enrolled in Medicaid compared with males and other racial and ethnic groups are congruent with previous studies (2-5,8). Our findings that an oral examination by a primary care dentist prior to the study period was associated with orthodontic utilization offers potential support for the importance of an established dental home. Previous research has found that adolescents in Northern Ireland with a history of regular dental visits were approximately three times as likely to receive orthodontic treatment than those with irregular use (22). Similar factors that motivate patients to seek primary dental care may also motivate them to seek specialty services. Additionally, primary care dentists may facilitate access to these services through recommendations or direct referrals for care.
The discovery that children living in rural areas of Iowa were more likely to receive services from an orthodontist than those living in metropolitan or micropolitan areas was contrary to our working hypothesis that geographic accessibility would be an important factor limiting access to care. This relationship between urbanicity and utilization differs from the conclusions of previous research, both in the United States and internationally (8,13,23). Differences in care-seeking behavior among urban and rural dwellers may arise from different priorities in time budgeting; low-income families in rural communities may have learned to accommodate the increased time commitment related to routine travel patterns associated with activities such as work, school, and health-care services.
The high degree of variability in rates of orthodontic treatment across service areas indicates that variation in provider availability may pose a more significant barrier to care for publicly insured children and adolescents than travel distance. Studies of orthodontic utilization in France and Northern Ireland have found that increased local supplies of orthodontists were positively associated with the likelihood of utilization (13,22). Future studies that investigate characteristics of orthodontists who provide high volumes of care to this population, including how their offices come to accept Medicaid patients, are needed. For example, these providers may only accept referrals from preferred primary care colleagues. This information could be used to design effective policy aimed at improving access to specialty dental care.
Our use of service areas is supported by findings from the individual-level evaluation of access to orthodontic treatment among Medicaid-enrolled children. The similarities seen at both levels of analysis validate the use of DSAs generated through small area analysis of patient origins as a research tool. Workforce evaluation at the service area level can investigate differences in Medicaid participation among orthodontists and explore the relationship between provider availability and the receipt of orthodontic treatment.
This study has several limitations. First, the data are cross-sectional and limited to a single state, which may limit generalizability of this research. The use of administrative data for analysis did not provide any information about patient-perceived need and demand for orthodontic care. Our findings that service areas with the highest proportions of minority populations were also the areas with the lowest utilization rates suggests potential cultural barriers to orthodontic treatment. These barriers could be the result of patient preferences for care, patient acceptability of available providers, or barriers imposed by orthodontists that limit their availability (either implicitly or explicitly) to potential patients based on social class or ethnicity.
As an additional limitation, we were unable to incorporate information about normative need or provider-evaluated need for orthodontic treatment. Variability in the prevalence of malocclusions could affect the regional variability of utilization demonstrated in this study. However, previous research has demonstrated repeatedly that normative need is not a requisite for patient demand for or for the receipt of orthodontic treatment (8,22,24). Administrative data from Iowa Medicaid do not contain information about orthodontic case complexity, although approval for treatment requires evidence of need based on Salzmann’s system of assessing malocclusions (11). In state fiscal year 2010, approximately 88 percent of 3,003 cases submitted to Iowa Medicaid were approved for orthodontic benefits (Iowa Medicaid Enterprise, written communication). Adjusting for case complexity in the Medicaid population could produce different results than those from the current study.
The relationship between rural residency and increased utilization may not apply to other types of dental care or other populations. Medicaid patients may have more severe malocclusions than privately insured patients who seek care. This treatment severity may confound the relationship between urbanicity and utilization. Finally, due to the small number of orthodontic service areas in Iowa, we were unable to conduct multivariable analyses to examine associations between regional characteristics and utilization rates. Future research is planned that will examine regional variation of access to other dental services including preventive and emergency services. Incorporating information about market areas for those services will allow us to examine how utilization is affected by workforce supply.
References
- 1.U.S. Health Resources and Service Administration [cited 9 Mar 2012];EPSDT Program Background. Available at: http://mchb.hrsa.gov/epsdt/overview.html.
- 2.Proffit WR, Fields HW, Jr, Moray LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult Orthodon Orthognath Surg. 1998;13(2):97–106. [PubMed] [Google Scholar]
- 3.Okunseri C, Pajewski NM, McGinley EL, Hoffmann RG. Racial/ethnic disparities in self-reported pediatric orthodontic visits in the United States. J Public Health Dent. 2007;67(4):217–223. doi: 10.1111/j.1752-7325.2007.00032.x. Fall. [DOI] [PubMed] [Google Scholar]
- 4.Nelson S, Armogan V, Abel Y, Broadbent BH, Hans M. Disparity in orthodontic utilization and treatment need among high school students. J Public Health Dent. 2004;64(1):26–30. doi: 10.1111/j.1752-7325.2004.tb02722.x. Winter. [DOI] [PubMed] [Google Scholar]
- 5.Anderson AB. PhD thesis. The University of Tennessee Health Science Center; May, 2010. A survey of treatment characteristics in a university-based graduate orthodontic program. [Google Scholar]
- 6.King GJ, Hall CV, Milgrom P, Grembowski DE. Early orthodontic treatment as a means to increase access for children enrolled in Medicaid in Washington state. J Am Dent Assoc. 2006 Jan;137(1):86–94. doi: 10.14219/jada.archive.2006.0026. [DOI] [PubMed] [Google Scholar]
- 7.Murdock JE, Phillips C, Beane R, Quinonez R. Break-even analysis of Medicaid vs. fee for service in orthodontic practice: North Carolina as a case study. Am J Orthod Dentofacial Orthop. 2010 Mar;137(3):334–339. doi: 10.1016/j.ajodo.2008.08.024. [DOI] [PubMed] [Google Scholar]
- 8.Wheeler TT, McGorray SP, Yurkiewicz L, Keeling SD, King GJ. Orthodontic treatment demand and need in third and fourth grade schoolchildren. Am J Orthod Dentofacial Orthop. 1994 Jul;106(1):22–33. doi: 10.1016/S0889-5406(94)70017-6. [DOI] [PubMed] [Google Scholar]
- 9.Shi L, Stevens GD, Lebrun LA, Faed P, Tsai J. Enhancing the measurement of health disparities for vulnerable populations. J Public Health Management Practice. 2008 Nov;(Suppl):S45–S52. doi: 10.1097/01.PHH.0000338386.59565.dc. [DOI] [PubMed] [Google Scholar]
- 10.Guay AH, Brown LJ, Wall T. Orthodontic dental patients and expenditures--2004. Am J Orthod Dentofacial Orthop. 2008 Sep;134(3):337–343. doi: 10.1016/j.ajodo.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 11.Salzmann JA. Handicapping malocclusion assessment to establish treatment priority. Am J Orthod. 1968 Oct;54(10):749–765. doi: 10.1016/0002-9416(68)90065-1. [DOI] [PubMed] [Google Scholar]
- 12.State of Iowa Department of Human Services [cited 9 Mar 2012];Medicaid Provider Manual - Dental Services. 2002 Jul 1; Available at: http://www.dhs.state.ia.us/policyanalysis/PolicyManualPages/Manual_Documents/Provman/dental.pdf.
- 13.Germa A, Kaminski M, Nabet C. Impact of social and economic characteristics on orthodontic treatment among children and teenagers in France. Community Dent Oral Epidemiol. 2010 Apr;38(2):171–179. doi: 10.1111/j.1600-0528.2009.00515.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paul-Shaheen P, Clark JD, Williams D. Small area analysis: a review and analysis of the North American literature. J Health Polit Policy Law. 1987;12(4):741–809. doi: 10.1215/03616878-12-4-741. [DOI] [PubMed] [Google Scholar]
- 15.The Dartmouth Institute for Health Policy and Clinical Practice [cited 9 Mar 2012];Defining Primary Care Service Areas. Available at: http://pcsa.dartmouth.edu/technical_information.html.
- 16.Agency for Healthcare Research and Quality [cited 9 Mar 2012];Child Health Care Quality Toolbox: Established Child Health Care Quality Measures - HEDIS: Health Plan Employer Data and Information Set. Available at: http://www.ahrq.gov/chtoolbx/measure4.htm.
- 17.Wennberg JE, Gittelsohn A. Variations in medical care among small areas. Sci Am. 1982;246(4):120–134. doi: 10.1038/scientificamerican0482-120. [DOI] [PubMed] [Google Scholar]
- 18.Im JL, Phillips C, Lee J, Beane R. The North Carolina Medicaid program: participation and perceptions among practicing orthodontists. Am J Orthod Dentofacial Orthop. 2007 Aug;132(2):144.e15–144.e21. doi: 10.1016/j.ajodo.2006.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.USDA Economic Research Service [cited 20 Jan 2012];2000 Rural-Urban Commuting Area Codes. 2005 Available at: http://www.ers.usda.gov/briefing/Rurality/RuralUrbanCommutingAreas/
- 20.WWAMI Rural Health Research Center [cited 20 Jan 2012];RUCA Data Version 2.0. 2005 Available at: http://depts.washington.edu/uwruca/ruca-data.php.
- 21.Kuthy RA, McKernan SC, Hand JS, Johnsen DC. Dentist workforce trends in a primarily rural state: Iowa: 1997-2007. J Am Dent Assoc. 2009 Dec;140(12):1527–1534. doi: 10.14219/jada.archive.2009.0105. [DOI] [PubMed] [Google Scholar]
- 22.Breistein B, Burden DJ. Equity and orthodontic treatment: A study among adolescents in Northern Ireland. Am J Orthod Dentofacial Orthop. 1998;113:408–13. doi: 10.1016/s0889-5406(98)80012-7. [DOI] [PubMed] [Google Scholar]
- 23.Borders SB. PhD thesis. Texas A&M University; 2006. Transportation barriers to health care: Assessing the Texas Medicaid program. [Google Scholar]
- 24.Tickle M, Kay EJ, Bearn D. Socio-economic status and orthodontic treatment need. Community Dent Oral Epidemiol. 1999 Dec;27(6):413–418. doi: 10.1111/j.1600-0528.1999.tb02040.x. [DOI] [PubMed] [Google Scholar]