Abstract
This study was conducted to introduce a simple modification that can facilitate microsurgical subinguinal varicocelectomy (MSV) especially for surgeons inexperienced in microsurgical technique. A single surgeon performed microsurgical intermediate subinguinal varicocelectomy (MISV) on 52 patients with 61 cases between September 2010 and August 2012. Patient age, varicocele grade, operation time, intraoperative findings, postoperative complications, and 3-month follow-up results were analyzed. Patient mean age was 28 years (range, 15–69 years), and there were 9 bilateral cases. The mean operative time was 51 minutes (range, 34–109 minutes). We compared the first 31 cases to the second 30 cases, to assess investigator experience on operating times. The mean number of ligated veins was 5 (range, 3–10) in internal spermatic vein, 1 (range, 0–4) in external spermatic vein, and 1 (range, 0–3) in gubernacular vein. In 28 patients, the average postoperative sperm concentration at the 3-month follow-up was significantly higher than the preoperative sperm concentration (28.5 ± 18.2 × 106/mL versus 10.5 ± 23.0 × 106/mL; P = 0.003). Mean motility improved after MSIV (65.7% ± 18.2% versus 47.2% ± 21.7%; P = 0.004). In conclusion, MISV appears comparable with MSV in terms of the high success rate, low complication rate, and low postoperative pain; and it can be easily accomplished by inexperienced surgeons.
Key words: Varicocele, Male infertility, Treatment outcome
The most common cause of male infertility is varicocele, which can be detected in at least 35% of infertile men and is correctable or at least improvable.1,2 The pregnancy rate was estimated to be 38.4% after varicocele repair through the pooled analysis.3 There have been a variety of approaches used including retroperitoneal, inguinal, subinguinal, and scrotal approaches. In terms of surgical technique, conventional open surgery, microsurgical technique, laparoscopic surgery including laparoendoscopic single-site surgery, radiographic embolization, and sclerotherapy have been introduced over several decades.4−9
Microsurgical subinguinal varicocelectomy (MSV) was introduced by Marmar et al in 1985 and then was modified by Goldstein et al in 1992.10,11 In a recent review, MSV showed the highest pregnancy rate, as well as the lowest recurrence and hydrocele formation rates.12–14 In addition, MSV resulted in significant increases in sperm concentration, total sperm count, and testosterone in all age groups studied, including men in the fifth and sixth decades of life.15 MSV is also associated with less operative and postoperative pain than inguinal approaches.16 Therefore, MSV can be regarded as the gold standard of varicocele repair; however, it requires a longer operation time and remains technically challenging for surgeons without microsurgical expertise.17 MSV is also more challenging owing to the greater number of vessels encountered at this level, compared with the inguinal canal.18 Thus, we introduce a simple modification that can facilitate MSV, which we call microsurgical intermediate subinguinal varicocelectomy (MISV); it may be especially useful for surgeons inexperienced in microsurgical technique.
Patients and Methods
Patient cohorts
In this study, MISV was conducted on 52 patients in our institution from September 2010 to August 2012. All procedures were performed by a single surgeon (KSC), who had performed fewer than 10 cases of microsurgical varicocelectomy prior to this case series. Preoperative evaluation consisted of physical examination for varicocele grade and testis volume, color Doppler ultrasonography, and semen analysis. Indications for surgical treatment included varicocele with infertility, abnormal semen parameter, scrotal pain, or testicular atrophy. Patient age, varicocele grade, operation time, intraoperative findings (number of internal spermatic arteries and veins), postoperative complication, and 3-month follow-up results were recorded. We compared surgical operating times between the first half and the second half of the cases.
Good clinical practice protocols
The study was performed in agreement with applicable laws and regulations, good clinical practices, and ethical principles as described in the Declaration of Helsinki (as revised in Seoul 2008). The Institutional Review Board of the hospital approved this study protocol (Approval number: 4-2012-0628).
Microsurgical intermediate subinguinal varicocelectomy
First, a 2- to 3-cm transverse skin incision was made over the external inguinal ring. The Camper's and Scarpa's fascia were divided using electrocautery, and the spermatic cord was identified, grasped with a Babcock clamp, and then a small silastic drain was placed beneath the spermatic cord. The testicle was then delivered, and the gubernacular veins and external spermatic perforators were isolated and divided; then the testicle was returned to the scrotum.
Next, we applied a technical modification to facilitate microdissection of the spermatic cord. The spermatic cord under the external oblique aponeurosis was dissected carefully using peanut dissector. A short, 1-cm incision on the external inguinal ring incision was made along the right angle clamp, and subsequently further dissection around the upper part of the spermatic cord was completed. Another large silastic drain was introduced between the internal spermatic vessels and the external spermatic fascia and its associated structures, as previously described.19 While retracting the small silastic drain caudally, the spermatic cord was elevated on a large silastic drain, and the microscope was brought into the operating field and the cord was examined. Eventually, we could explore the spermatic cord at approximately the 2-cm upper level compared with the conventional level without external inguinal ring incision, and the spermatic cord was more redundant without arterial choking by external spermatic ring.
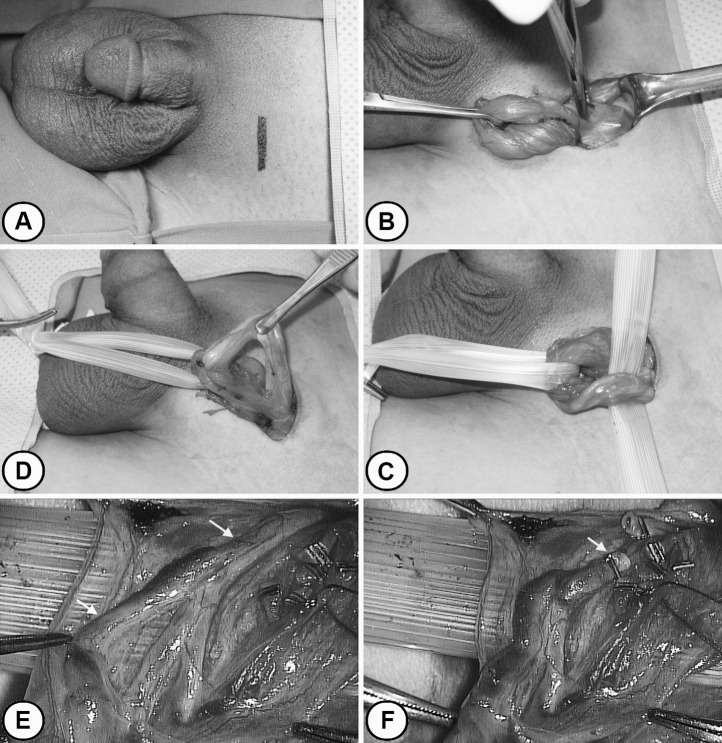
We could identify arteries by detecting arterial pulsation carefully; all identified arteries were saved (Fig. 1). Lymphatic channels were also preserved, but all veins except the vasal veins were clipped or ligated with 4-0 silk ties and divided. At the completion of the procedure, the spermatic cord was returned to the subinguinal level. A figure-eight stitch using 2-0 absorbable suture was placed to repair the external inguinal ring. Scarpa's fascia was closed with an interrupted 3-0 absorbable suture, and the skin was closed.
Fig. 1.
Microsurgical intermediate subinguinal varicocelectomy. (A) A 2- to 3-cm transverse skin incision was made over the external inguinal ring. (B) A short, 1-cm incision on the external inguinal ring incision was made along the right angle clamp, and subsequently further dissection around the upper part of spermatic cord was completed. (C) and (D) As retracting the small silastic drain caudally, the spermatic cord was elevated on a large silastic drain. (E) and (F) We could explore the spermatic cord at approximately the 2-cm upper level compared with the conventional subinguinal level (arrowhead) without an external inguinal ring incision; the venous plexus was less complex with fewer veins at our intermediate subinguinal level (arrow), and the spermatic cord would be more redundant without arterial choking by external spermatic ring. The structure encircled by black silk tie is the preserved internal spermatic artery.
Statistical analysis
Assessments included postoperative complications including hydrocele, recurrence, operation time, hospitalization length of stay, and postoperative pain. The severity of pain was rated using a scale of 0 to 10, with zero indicating pain-free status and 10 representing the worst pain imaginable using visual analogue scale (VAS).20 Mann-Whitney U test, Student t test, and the Wilcoxon test were used for comparison of each variable. Statistical calculations were carried out with MedCalc (version 11.2.1.0, MedCalc Software, Mariakerke, Belgium). A P value <0.05 was considered significant.
Results
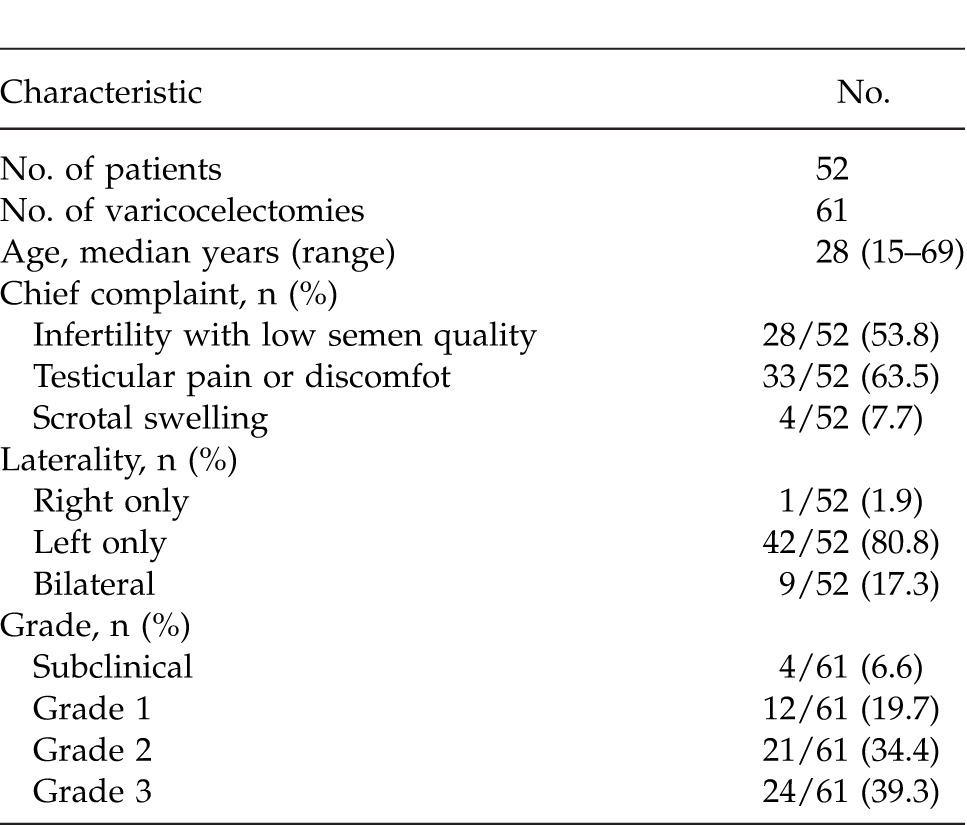
The median age was 28 years (range, 15–69 years), and bilateral cases were 9 of 52 patients. Chief complaints of patients included (1) infertility with low semen quality in 28 patients (53.8%), (2) testicular pain or discomfort in 33 (63.5%), and (3) scrotal swelling in 4 (7.7%). The number of cases with subclinical varicocele was 4 (6.6%); 12 cases (19.7%) were grade 1; 21 cases (34.4%) were grade 2, and 24 cases (39.3%) were grade 3 (Table 1).
Table 1.
Patient characteristics
The mean operation time was 51 minutes (range, 34–109 minutes). The mean operation time was 55 minutes (range, 37–109 minutes) in the first half (31 cases), and 50 minutes (range, 34–88 minutes) in the second half (30 cases). There were no statistical differences between first and second half of the cases (P = 0.086) (Table 2). The mean number of ligated veins was 5 (range, 3–10) in internal spermatic vein, 1 (range, 0–4) in external spermatic vein, and 1 (range, 0–3) in gubernacular vein. The number of internal spermatic arteries saved was 1 of 46 cases (75.4%) and 2 of 15 cases (24.6%). No intraoperative or early postoperative complications were worse than a grade-II Clavien-Dindo Classification.21 All patients were discharged at postoperative day 1; their mean VAS scores were 1.7 ± 1.1 (range, 0–3) and 1.1 ± 0.8 (range, 0–2) on the operative day and the first postoperative day, respectively (P = 0.003). No patients used opioid pain killer or patient-controlled anesthesia postoperatively. Postoperative hydrocele was not observed, and recurrent varicocele was observed in 1 patient (1.6%). None of the patients experienced hematoma, wound infection, or testicular atrophy.
Table 2.
Operative and postoperative outcomes
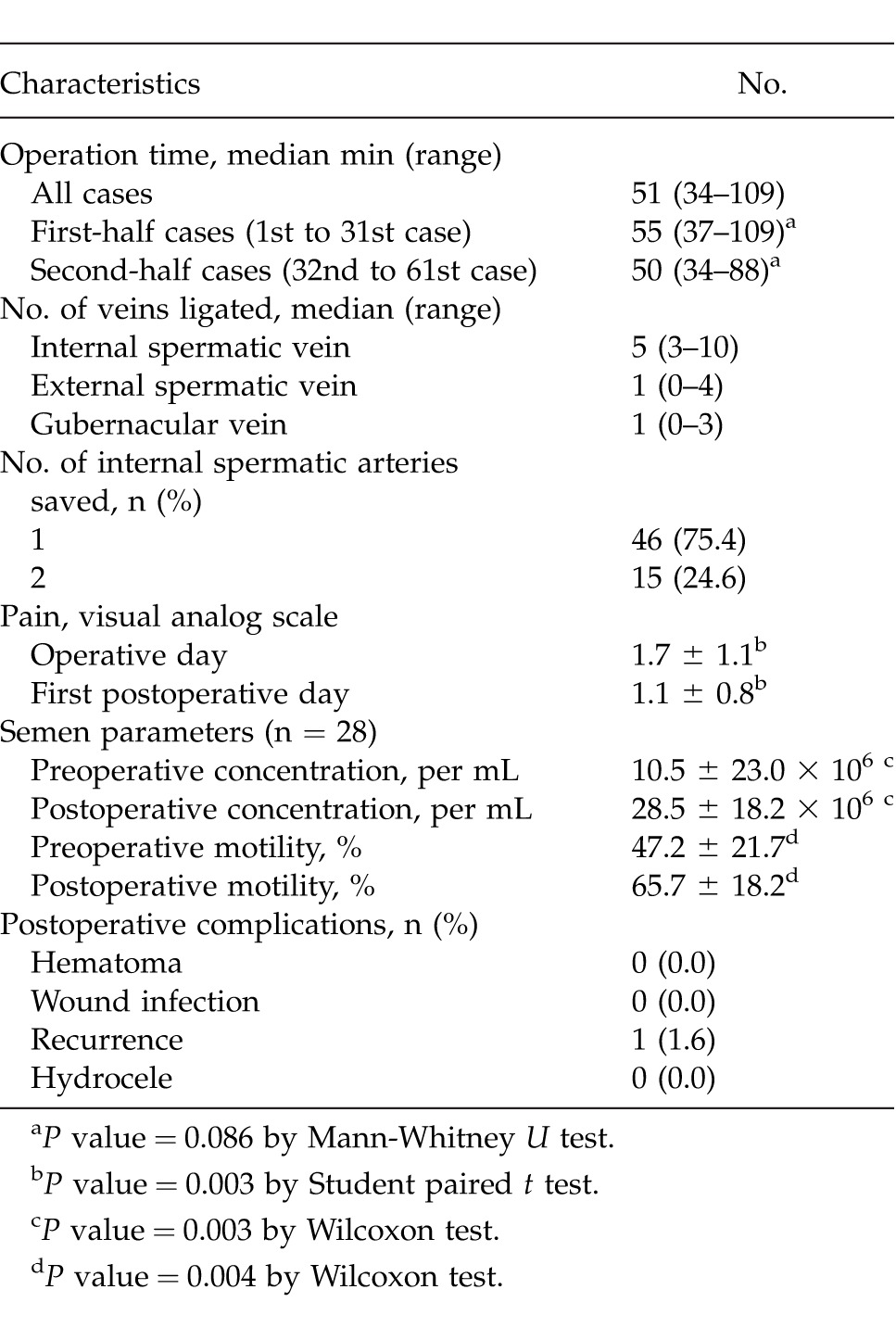
In 28 patients who showed abnormal semen values preoperatively, the average postoperative sperm concentration at the 3-month follow-up was significantly higher than the preoperative sperm concentration (28.5 ± 18.2 × 106/mL versus 10.5 ± 23.0 × 106/mL; P = 0.003). Mean motility also showed improvement after MSIV (65.7% ± 18.2% versus 47.2% ± 21.7%; P = 0.004) (Table 2).
Discussion
A variety of approaches have been advocated for management of varicoceles, but recent evidence supports the premise that the MSV is the “gold standard.”22,23 A possible cause of varicoceles is reflux in the collateral veins, including the cremasteric and external pudendal veins or gubernacular veins, all of which drain into the iliac vein.24 Thus, MSV with delivery of the testis provides direct visual access to all avenues of testicular venous drainage and is reported to result in a significant decrease in the incidence of varicocele recurrence.25 In a number of studies, it has been shown that microsurgical varicocelectomy (inguinal or subinguinal) is superior to non-microsurgical procedures with respect to the development of postoperative complications such as hydrocele or recurrence.11,26 In a meta-analysis, MSV has higher spontaneous pregnancy rates and lower postoperative recurrence and hydrocele formation than conventional varicocelectomy techniques in infertile men.27
However, the greater number of vessels (arteries and veins) encountered at this level and their complexity make this a technically challenging procedure that requires microsurgical expertise.28 MSV may be somewhat difficult to perform for beginners who have little experience with microscopic surgery, which has a steep learning curve. Thus, various modification methods of MSV have been reported to overcome procedural difficulty.19,29 Hopps et al reported that multiple spermatic arteries were identified in 75% of subinguinal dissections and in only 31% of inguinal dissections.18 They also showed that internal spermatic arteries were surrounded by a dense complex of adherent veins in 95% of cases using the subinguinal approach, whereas this finding was true in only 30% of cases with the inguinal approach. Preservation of the artery could also be performed more easily with an MSV, because only 1 to 2 arteries were exposed and ligated. In our MISV, the venous plexus was less complex and fewer veins were encountered than with conventional MSV because the internal spermatic vasculature was controlled in the upward level of the external inguinal ring.
In addition, incision on the external inguinal ring and upward dissection can provide the additional benefit for arterial preservation, because this procedure could make the spermatic cord more redundant when it was placed on the large silastic drain, and then artery choking could be avoided by the external spermatic ring. Actually, the pulsatile artery was identified without difficulty; there was no need to use papaverine or lidocaine in any of the cases. For these reasons, MISV might have an acceptable operation time when considering that the surgeon was not a microsurgical expert, and there seemed to be no learning curve during this early experience. It is known that the inguinal approach is easier than subinguinal but might result in more postoperative pain. However, in our study, using only a 1-cm incision on the external inguinal ring did not show severe postoperative pain in patients. Therefore, MISV may be a feasible procedure, which seems to be easier than conventional MSV, and results in less pain compared with the inguinal approach.
Several studies on fertility issues in children have recommended the microscopic inguinal approach in prepubertal boys because the artery is so small and suggested the subinguinal approach in postpubertal adolescents.14 Richter et al report the results of questionnaire study designed to assess the practice patterns among urologists with regard to prepubertal varicocele management.30 In their study, only 30% of pediatric urologists opted to use a microscope or use the subinguinal approach in the repair of pediatric varicocele. The expectation of greater difficulty in the performance of surgery in pediatric patients owing to the complex entangling of the smaller vasculature has been suggested as a possible reason.31 Our MISV may also be applied to pediatric patients with varicocele.
Our study is the first report to introduce MISV in patients with varicocele. However, we note that our study has some limitations. A major limitation is that it is not a comparative study to microsurgical subinguinal or inguinal procedures, and another is that all the procedures were performed by single surgeon. Therefore, a randomized clinical trial by various surgeons is needed to confirm our favorable initial experiences for MISV.
Conclusions
This initial experience suggests that MISV would be a better alternative to MSV especially for surgeons inexperienced in microsurgical technique. MISV is expected to be comparable to MSV in terms of high success rate, low complication rate, and low postoperative pain as it can be easily accomplished even by inexperienced surgeons. However, a larger comparative study is necessary to secure solid evidence for the potential benefits of MISV.
References
- 1.Kass EJ, Reitelman C. Adolescent varicocele. Urol Clin North Am. 1995;22(1):151–159. [PubMed] [Google Scholar]
- 2.Schlesinger MH, Wilets IF, Nagler HM. Treatment outcome after varicocelectomy: a critical analysis. Urol Clin North Am. 1994;21(3):517–529. [PubMed] [Google Scholar]
- 3.Diegidio P, Jhaveri JK, Ghannam S, Pinkhasov R, Shabsigh R, Fisch H. Review of current varicocelectomy techniques and their outcomes. BJU Int. 2011;108(7):1157–1172. doi: 10.1111/j.1464-410X.2010.09959.x. [DOI] [PubMed] [Google Scholar]
- 4.Lee SW, Lee JY, Kim KH, Ha US. Laparoendoscopic single-site surgery versus conventional laparoscopic varicocele ligation in men with palpable varicocele: a randomized, clinical study. Surg Endosc. 2012;26(4):1056–1062. doi: 10.1007/s00464-011-1997-2. [DOI] [PubMed] [Google Scholar]
- 5.Lee JY, Kang DH, Chung JH, Jo JK, Lee SW. Laparoendoscopic single-site surgery for benign urologic disease with a homemade single port device: design and tips for beginners. Korean J Urol. 2012;53(3):165–170. doi: 10.4111/kju.2012.53.3.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee HS, Seo JT. Advances in surgical treatment of male infertility. World J Mens Health. 2012;30(2):108–113. doi: 10.5534/wjmh.2012.30.2.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee MJ, Cho SH, Choi JY, Kim SB, Lee ST, Min SK. Significance of laparoscopic varicocelectomy. Korean J Androl. 2010;28(3):209–216. [Google Scholar]
- 8.Kang DH, Lee JY, Chung JH, Jo JK, Lee SH, Ham WS, et al. Laparoendoscopic single site varicocele ligation: comparison of testicular artery and lymphatic preservation versus complete testicular vessel ligation. J Urol. 2013;189(1):243–249. doi: 10.1016/j.juro.2012.09.024. [DOI] [PubMed] [Google Scholar]
- 9.Chen C. Varicocele in male factor infertility: role of laparoscopic varicocelectomy. Int Surg. 2006;91(suppl 5):S90–S94. [PubMed] [Google Scholar]
- 10.Marmar JL, DeBenedictis TJ, Praiss D. The management of varicoceles by microdissection of the spermatic cord at the external inguinal ring. Fertil Steril. 1985;43(4):583–588. doi: 10.1016/s0015-0282(16)48501-8. [DOI] [PubMed] [Google Scholar]
- 11.Goldstein M, Gilbert BR, Dicker AP, Dwosh J, Gnecco C. Microsurgical inguinal varicocelectomy with delivery of the testis: an artery and lymphatic sparing technique. J Urol. 1992;148(6):1808–1811. doi: 10.1016/s0022-5347(17)37035-0. [DOI] [PubMed] [Google Scholar]
- 12.Minevich E, Wacksman J, Lewis AG, Sheldon CA. Inguinal microsurgical varicocelectomy in the adolescent: technique and preliminary results. J Urol. 1998;159(3):1022–1024. [PubMed] [Google Scholar]
- 13.Greenfield SP, Seville P, Wan J. Experience with varicoceles in children and young adults. J Urol. 2002;168(4 pt 2):1684–1688. doi: 10.1097/01.ju.0000027120.88391.91. discussion 1688. [DOI] [PubMed] [Google Scholar]
- 14.Yaman O, Soygur T, Zumrutbas AE, Resorlu B. Results of microsurgical subinguinal varicocelectomy in children and adolescents. Urology. 2006;68(2):410–412. doi: 10.1016/j.urology.2006.02.022. [DOI] [PubMed] [Google Scholar]
- 15.Hsiao W, Rosoff JS, Pale JR, Greenwood EA, Goldstein M. Older age is associated with similar improvements in semen parameters and testosterone after subinguinal microsurgical varicocelectomy. J Urol. 2011;185(2):620–625. doi: 10.1016/j.juro.2010.09.114. [DOI] [PubMed] [Google Scholar]
- 16.Al-Kandari AM, Shabaan H, Ibrahim HM, Elshebiny YH, Shokeir AA. Comparison of outcomes of different varicocelectomy techniques: open inguinal, laparoscopic, and subinguinal microscopic varicocelectomy: a randomized clinical trial. Urology. 2007;69(3):417–420. doi: 10.1016/j.urology.2007.01.057. [DOI] [PubMed] [Google Scholar]
- 17.Mirilas P, Mentessidou A. Microsurgical subinguinal varicocelectomy in children, adolescents and adults: surgical anatomy and anatomically justified technique. J Androl. 2011;33(3):338–349. doi: 10.2164/jandrol.111.013052. [DOI] [PubMed] [Google Scholar]
- 18.Hopps CV, Lemer ML, Schlegel PN, Goldstein M. Intraoperative varicocele anatomy: a microscopic study of the inguinal versus subinguinal approach. J Urol. 2003;170(6 pt 1):2366–2370. doi: 10.1097/01.ju.0000097400.67715.f8. [DOI] [PubMed] [Google Scholar]
- 19.Zini A, Fischer A, Bellack D, Noss M, Kamal K, Chow V, et al. Technical modification of microsurgical varicocelectomy can reduce operating time. Urology. 2006;67(4):803–806. doi: 10.1016/j.urology.2005.10.044. [DOI] [PubMed] [Google Scholar]
- 20.Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17(1):45–56. doi: 10.1016/0304-3959(83)90126-4. [DOI] [PubMed] [Google Scholar]
- 21.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 22.Cayan S, Kadioglu TC, Tefekli A, Kadioglu A, Tellaloglu S. Comparison of results and complications of high ligation surgery and microsurgical high inguinal varicocelectomy in the treatment of varicocele. Urology. 2000;55(5):750–754. doi: 10.1016/s0090-4295(99)00603-2. [DOI] [PubMed] [Google Scholar]
- 23.Ghanem H, Anis T, El-Nashar A, Shamloul R. Subinguinal microvaricocelectomy versus retroperitoneal varicocelectomy: comparative study of complications and surgical outcome. Urology. 2004;64(5):1005–1009. doi: 10.1016/j.urology.2004.06.060. [DOI] [PubMed] [Google Scholar]
- 24.Moon KH, Cho SJ, Kim KS, Park S, Park S. Recurrent varicoceles: causes and treatment using angiography and magnification assisted subinguinal varicocelectomy. Yonsei Med J. 2012;53(4):723–728. doi: 10.3349/ymj.2012.53.4.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beck EM, Schlegel PN, Goldstein M. Intraoperative varicocele anatomy: a macroscopic and microscopic study. J Urol. 1992;148(4):1190–1194. doi: 10.1016/s0022-5347(17)36857-x. [DOI] [PubMed] [Google Scholar]
- 26.Grober ED, O'Brien J, Jarvi KA, Zini A. Preservation of testicular arteries during subinguinal microsurgical varicocelectomy: clinical considerations. J Androl. 2004;25(5):740–743. doi: 10.1002/j.1939-4640.2004.tb02849.x. [DOI] [PubMed] [Google Scholar]
- 27.Cayan S, Shavakhabov S, Kadioglu A. Treatment of palpable varicocele in infertile men: a meta-analysis to define the best technique. J Androl. 2009;30(1):33–40. doi: 10.2164/jandrol.108.005967. [DOI] [PubMed] [Google Scholar]
- 28.Zini A. Varicocelectomy: microsurgical subinguinal technique is the treatment of choice. Can Urol Assoc J. 2007;1(3):273–276. [PMC free article] [PubMed] [Google Scholar]
- 29.Tung MC, Huang WJ, Chen KK. Modified subinguinal varicocelectomy for painful varicocele and varicocele-associated infertility. J Chin Med Assoc. 2004;67(6):296–300. [PubMed] [Google Scholar]
- 30.Richter F, Stock JA, LaSalle M, Sadeghi-Nejad H, Hanna MK. Management of prepubertal varicoceles-results of a questionnaire study among pediatric urologists and urologists with infertility training. Urology. 2001;58(1):98–102. doi: 10.1016/s0090-4295(01)01118-9. [DOI] [PubMed] [Google Scholar]
- 31.Park K, Cho SY, Kim SW. The surgical difficulty of microsurgical subinguinal varicocelectomy is similar regardless of age. J Urol. 2011;186(6):2397–2401. doi: 10.1016/j.juro.2011.07.110. [DOI] [PubMed] [Google Scholar]