Abstract
Parastomal hernia is the most common late stomal complication. Its appearance is usually asymptomatic. We report a parastomal hernia containing stomach. A 69-year-old patient with end colostomy arrived at the emergency room presenting with abdominal pain associated with vomiting and functioning stoma. She had a distended and painful abdomen without signs of peritoneal irritation and pericolostomic eventration in the left iliac fossa. X-ray visualized gastric fornix dilatation without dilated intestine bowels, and computed tomography showed parastomal incarcerated gastric herniation. Gastrografin (Bayer Australia Limited, New South Wales, Australia) was administered, showing no passage to duodenum. She underwent surgery, with stomal transposition and placement of onlay polypropylene mesh around the new stoma. Parastomal hernias are a frequent late complication of colostomy. Only four gastric parastomal hernia cases are reported in the literature. Three of these four cases required surgery. The placement of prosthetic mesh in the moment of stoma elaboration should be considered as a potential preventive measure.
Key words: Colostomy, Gastric hernia, Parastomal hernia, Stomach disease, Postoperative complications
Parastomal hernia is the most common late stoma complication.1 Its appearance is usually asymptomatic, however, it may be associated with abdominal discomfort, pain, nausea, vomiting, obstruction, and strangulation.2
We report a parastomal hernia containing stomach, a very rare case with only four precedents in literature.2–5
Clinic Case
A 69-year-old patient with end colostomy (Hartmann's procedure) due to perforated sigmoid adenocarcinoma (pT4N0M0) in 2005, arrived at the emergency room presenting with abdominal pain associated with vomiting and functioning stoma. Physical examination revealed a distended and painful abdomen without signs of peritoneal irritation and pericolostomic eventration in the left iliac fossa, which was partially reduced.
Additional tests were performed, including a blood test that showed 11.7 × 109 / L (leukocytes) with 88% neutrophils (other parameters were not noteworthy). and an X-ray that visualized gastric fornix dilatation without dilated intestine bowels. Afterwards the patient underwent a computed tomography, which showed parastomal incarcerated gastric herniation and absence of tumor recurrence. (Fig. 1)
Fig. 1.
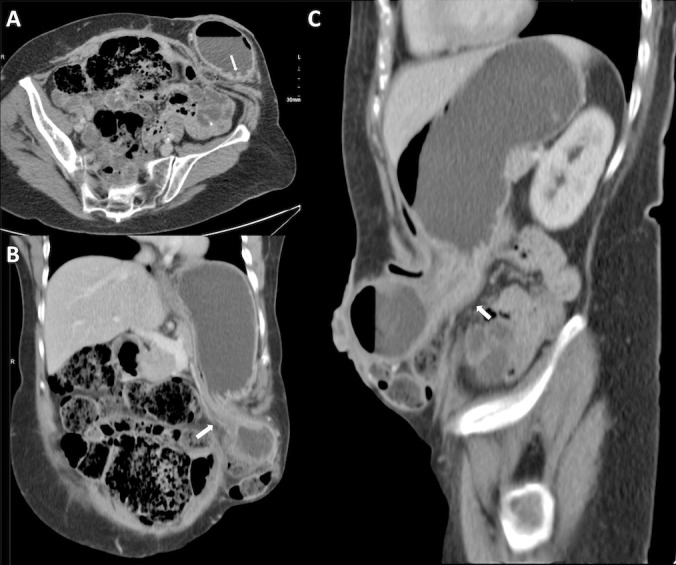
Oblique abdominal CT reconstruction with intravenous contrast on axial (A), coronal (B) and sagittal (C). It shows the pericolostomic hernia of a portion of the gastric antrum with constriction at the orifice of the hernia (white arrows in B and C). The yellow arrow in the axial reconstruction (A) shows the gastric folds in herniated portion.
Gastrografin (Bayer Australia Limited, New South Wales, Australia) contrast solution was administered, showing no passage to duodenum (Fig. 2). Given the lack of clinical response, surgery was decided. Laparotomy and hernia content reduction were performed along with previous verification of its feasibility, stomal transposition and placement of onlay polypropylene mesh around the new stoma, and herniorrhaphy of the old hernia orifice. After 10 days of hospitalization without further complications, the patient was discharged from the hospital.
Fig. 2.

Abdominal X-ray after administration of Gastrografin, supine (A) and standing (B). Passage of contrast to herniated portion of stomach (B) and delimitation of gastric folds (A) are objectivized. No progress to duodenum.
Discussion
Gastric parastomal hernia is very unusual. Only four cases are reported in the literature. All cases had similar symptoms, and only one was manually reduced; the remaining three cases required surgery.
However, a parastomal hernia is one of the most frequent colostomies with long-term complications and, although they usually have no clinical impact, there is an incidence between 0 and 48.1%.2 The location of the enterostomy drives the subsequent formation of hernias, being much larger when performing laterally to rectus abdominis muscle than transrectal.3
Risk factors for the development of parastomal herniation can be differentiated between patient-dependent (abdominal circumference greater than 100 cm, age over 60 years, increased intra-abdominal pressure, corticosteroid medication, malnutrition, cancer, lung disease, etc.), of surgical technique (preparation of stoma and stoma type), and postoperative (surgical wound infection and long-term survival).6
There are reports in the literature that reflect the difficulty of parastomal hernia defect correction and high rates of recurrence later.6
There are many surgical techniques for hernia repair: open surgery with or without stomal transposition, with or without prosthesis placement, which, in turn, may be subdivided into supra-aponeurotic placement (onlay), deep in the wall or between two aponeurotic planes (sublay), and intra-abdominal; and laparoscopic techniques. According to the literature, more studies are still required to learn the techniques with better results in terms of recurrence, infection, etc.6,7
Some randomized studies lean towards the use of prophylactic prosthetics to reinforce the fascia during the initial elaboration of the stoma.8 Similarly Tam et al,7 after a systematic review of the literature, talk about a recurrence rate of 15.4% in patients who underwent prophylactic stent placement, compared with 55.2% who underwent conventional stoma elaboration.
Conclusion
Parastomal hernias are a frequent late complication of colostomy. They do rarely present gastric content; in fact only four cases have been historically recorded in the literature.
Surgical repair is not normally required. However, three of four gastric hernia cases have needed surgery. Therefore the placement of prosthetic mesh in the moment of stoma elaboration should be considered as a potential preventive measure.6–8
References
- 1.Sohn YJ, Moon SM, Shin US, Jee SH. Incidence and risk factors of parastomal hernia. J Korean Soc Coloproctol. 2012;28(5):241–246. doi: 10.3393/jksc.2012.28.5.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ilyas C, Young AL, Lewis M, Suppia A, Gerotfeke R, Perry EP. Parastomal hernia causing gastric emphysema. Ann R Coll Surg Engl. 2012;94(2):e72–73. doi: 10.1308/003588412X13171221588613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McAllister JD, D'Altorio RA. A rare cause of parastomal hernia: stomach herniation. South Med J. 1991;84(7):911–912. doi: 10.1097/00007611-199107000-00023. [DOI] [PubMed] [Google Scholar]
- 4.Bota E, Shaikh I, Fernandes R, Doughan S. Stomach in a parastomal hernia: uncommon presentation. BMJ Case Rep. doi: 10.1136/bcr.01.2012.5508. 2012 Mar 8;2012, pii: bcr0120125508, doi: 10.1136/bcr.01.2012.5508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ramia-Ángel JM, De la Plaza R, Quiñones-Sampedro J, Veguillas P, García-Parreño J. Education and imaging. Gastrointestinal: gastric incarceration in parastomal hernia. J Gastroenterol Hepatol. 2012;27(8):1405. doi: 10.1111/j.1440-1746.2012.07181.x. [DOI] [PubMed] [Google Scholar]
- 6.Tadeo-Ruiz G, Picazo-Yeste JS, Moreno-Sanz C, Herrero-Bogajo ML. Parastomal hernias: background, current status and future prospects. Cir Esp. 2010;87(6):339–349. doi: 10.1016/j.ciresp.2009.11.018. [DOI] [PubMed] [Google Scholar]
- 7.Tam KW, Wei PL, Kuo LJ, Wu CH. Systematic review of the use of a mesh to prevent parastomal hernia. World J Surg. 2010;34(11):2723–2729. doi: 10.1007/s00268-010-0739-2. [DOI] [PubMed] [Google Scholar]
- 8.Serra-Aracil X, Bombardo-Junca J, Moreno-Matias J, Darnell A, Mora-Lopez L, Alcantara-Moral M, et al. Randomized, controlled, prospective trial of the use of a mesh to prevent parastomal hernia. Ann Surg. 2009;249(4):583–587. doi: 10.1097/SLA.0b013e31819ec809. [DOI] [PubMed] [Google Scholar]


