Abstract
Lung cancer is the leading cause of mortality among malignant diseases in humans worldwide. During the last decade, molecular targeted therapies for non-small cell lung cancer using first-generation, reversible epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs), including gefitinib, have been shown to be a promising approach for patients harboring activating mutations in EGFR. The current study reports a 77-year-old patient diagnosed with adenocarcinoma harboring L858R and T790M point mutations in the EGFR gene. The patient was treated with gefitinib as the second-line therapy, but no clinical benefit was observed. As the majority of patients with lung cancer receiving EGFR-TKI therapy acquire resistance, repeated biopsies and detection of the EGFR mutation state are beneficial for selecting appropriate treatments.
Keywords: adenocarcinoma, biopsy, non-small cell lung cancer, epidermal growth factor receptor, mutation
Introduction
Lung cancer is the leading cause of cancer-related mortality worldwide (1). Recent studies on personalized treatment, conducted by selecting patients who are likely to respond to a particular therapeutic agent, may allow improved treatment efficacy. Activated mutations of the EGFR gene are normally located in exons 18 to 21, >90% of which consist of deletions in exon 19 and L858R substitution in exon 21 (2). Patients with non-small cell lung cancer (NSCLC) harboring mutations in the epidermal growth factor receptor (EGFR) gene exhibit a significant response to EGFR-tyrosine kinase inhibitors (TKIs) (3,4). Clinical trials have demonstrated that gefitinib improves progression-free and overall survival in the treatment of NSCLC (5). Gefitinib is now approved for these indications (6). Gefitinib has also been proposed for the treatment of patients with locally advanced or metastatic NSCLC with EGFR-activating mutations (7), which targets the tyrosine kinase (TK) domain of EGFR, inhibiting the downstream signaling processes for growth and proliferation. Mutations in the EGFR gene may also affect the behavior of the receptor and its response to inhibitors.
The majority of NSCLC patients with EGFR mutations initially benefit favorably from treatment with gefitinib, suggesting that these mutations promote tumorigenesis. However, among tumors that initially respond to EGFR-TKIs, the majority of patients eventually acquire resistance, often due to the emergence of a secondary mutation, such as T790M, in the kinase domain of EGFR (8). Patients with both L858R and T790M EGFR mutations are extremely rare (9). Written informed consent was obtained from the patient’s family.
Case report
A 77-year-old male with a history of smoking was admitted to the Department of Interventional Radiology, The First Affiliated Hospital of Sun Yat-sen University (Guangzhou, China) in November 2011 due to an abnormal shadow in the right upper field following a chest X-ray. Physical examination revealed no significant abnormalities; however, computed tomography (CT) of the chest revealed a tumor measuring 66×74×80 mm in size in the right S1+2 with multiple lung and bone metastases (cT3N3M1; stage IV), according to the TNM classification (10). A transbronchial lung biopsy (TBLB) was conducted and the pathological diagnosis of the TBLB specimen was acinar adenocarcinoma (Fig. 1A). Immunohistochemical staining was positive for transcription factor-1 protein (Fig. 1B). Laboratory findings were within the normal range, with the exception of the carcinoembryonic antigen (CEA) level of 12.65 ng/ml (normal range, 0–3.4 ng/ml) in the serum. A diagnosis of lung adenocarcinoma was determined and the patient was treated with first-line chemotherapy consisting of cisplatin (80 mg/m2) and docetaxel (60 mg/m2), every three weeks for up to three cycles. However, no marked response was observed.
Figure 1.
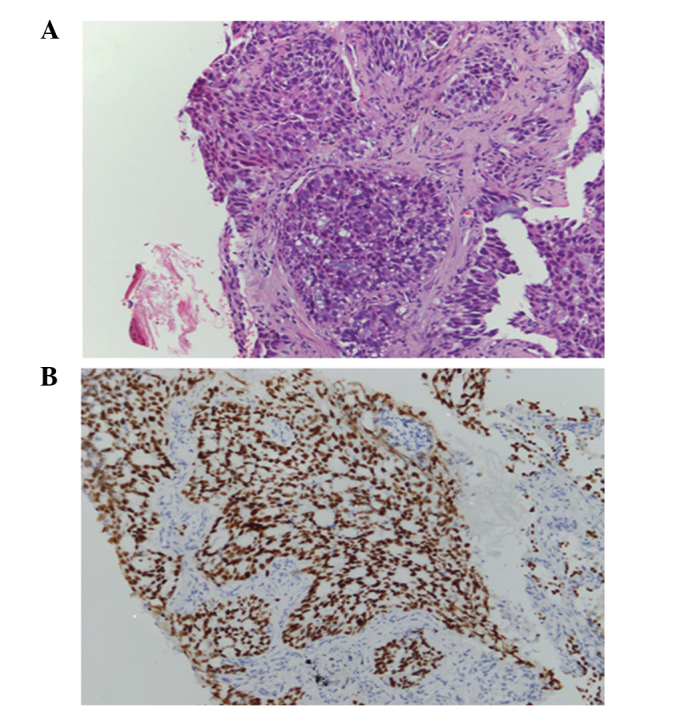
Histological morphology of the primary lung adenocarcinoma with a predominantly solid growth pattern. (A) Hematoxylin-eosin staining and (B) immunohistochemical staining for transcription factor-1 (magnification, ×10).
Following the initial treatment, a mutation in the EGFR gene was identified (exon 21; L858R, in which the leucine at amino acid position 858 is replaced by arginine; Fig. 2A). The second-line chemotherapy was gefitinib (250 mg) once a day, administered between March and July 2012. The gefitinib therapy was effective, and no adverse events were reported. A CT scan of the thorax was performed in May 2012, which revealed residual disease in the right lung (51×72×51 cm in diameter) and few metastatic bone lesions (Fig. 3).
Figure 2.
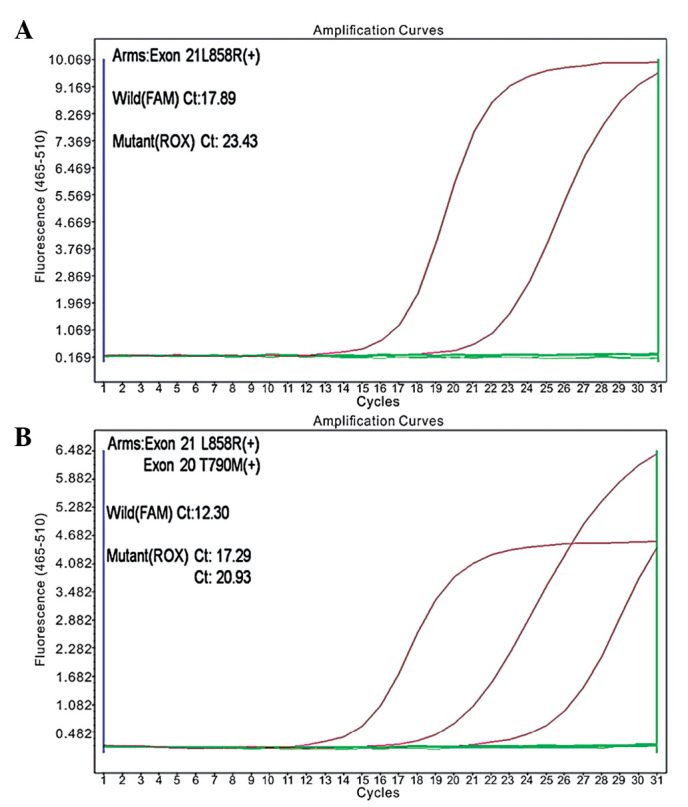
Epidermal growth factor receptor gene mutation was positive according to the amplification-refractory mutation system method. (A) L858R point mutation prior to the use of gefitinib, and (B) L858R and T790M point mutations following treatment with gefitinib.
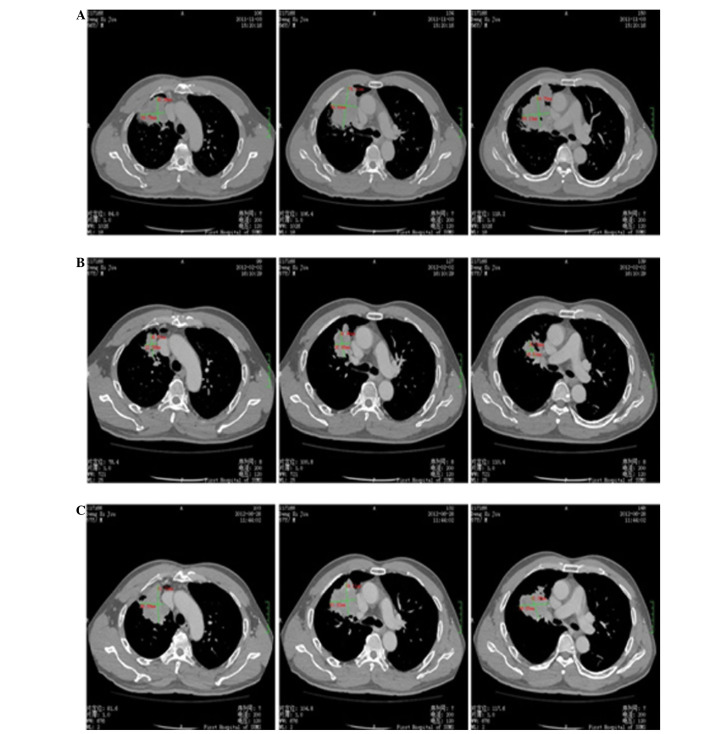
Figure 3.
Computed tomography scans of the present non-small cell lung cancer patient. (A) Prior to treatment with gefitinib, (B) stable disease and (C) disease progression following long-term treatment with gefitinib.
In November 2012, a further CT scan revealed a number of new lesions (one in the right lung, and several in the bone and brain), indicating disease progression. The patient was subjected to a rebiopsy to detect EGFR mutations, with analysis by the amplification refractory mutation system. L858R and T790M point mutations were detected in the tumor cells (Fig. 2B). Subsequently, the patient underwent three cycles of third-line chemotherapy (150 mg erlotinib per day for three months); however, further metastases emerged in the brain and, therefore, palliative care was administered in May 2013. The gefitinib therapy was discontinued to introduce the third-line chemotherapy, which induced an infusion reaction, and no remarkable response was observed. Following discontinuation of the third-line chemotherapy, the tumor growth induced empyema and the patient’s general condition gradually deteriorated and the patient succumbed to the disease in August, 2013.
Discussion
It has been demonstrated that the majority of patients with lung cancer that are responsive to EGFR-TKIs harbor activating mutations in the TK domain of EGFR (11–13). This further supports the hypothesis that the identification of genetic signatures associated with oncogenic alterations may serve as predictive biomarkers for corresponding molecular target inhibitors. In comparison with smokers, EGFR mutations have consistently been found to be more common in non-smokers (14). In the present study, the patient did not have a history of smoking. Histopathologically, mutation rates among adenocarcinoma are predominantly higher than those in squamous cell lung carcinomas (15). The diagnosis of squamous cell carcinoma or adenocarcinoma is based on histomorphological grounds in cases where the appearances are characteristic; additionally, immunohistochemical staining is performed using antibodies against TTF-1, p63, M-CEA and CK. Immunohistochemical nuclear expression of TTF-1 also confirms a primary pulmonary origin. Furthermore, M-CEA-positive and p63-negative tumor cells indicate a glandular epithelium origin (16).
According to the Food and Drug Administration regulations, EGFR inhibitors have been approved as the first-line treatment for advanced NSCLC patients positive for EGFR-activating mutations (17). However, EGFR inhibitors are not used to treat patients with wild-type EGFR and, by contrast, a poor outcome has been observed in response to the treatment (18,19). Activating mutations of the EGFR gene are predominantly located in exons 18–21 and >90% are deletions in exon 19 or the L858R substitution in exon 21. These activating mutations are eligible for treatment with modern TKIs, for example gefitinib (20–22). Therefore, the accurate detection of EGFR mutations is critical for determining the efficacy in the adoption of gefitinib for advanced NSCLC in any given population. In the current study, the L858R point mutation of exon 21 was detected in the tumor cells, and an effective and curative outcome was observed following treatment with gefitinib. However, after several months, a CT scan revealed new lesions in the brain, indicating disease progression. The L858R point mutation of exon 21 and a compound T790M EGFR substitution mutation were detected in the tumor cells, which was consistent with the study by Pao et al (23), indicating that the efficacy of EGFR-TKIs in lung cancer is severely compromised by the rapid emergence of targeted therapy-resistant clones within one year.
In conclusion, the current study reports a rare case of lung cancer harboring an L858R point mutation of exon 21 and a compound T790M EGFR substitution mutation following treatment with gefitinib. However, following the detection of the T790M EGFR substitution mutation in the tumor cells, the patient exhibited poor curative effect when treatment with gefitinib was continued. Therefore, to improve the selection of optimal treatment regimens in individual patients, further investigation into determining the genetic causes of drug resistance at various points during the clinical course is required.
Acknowledgments
This study was funded by the National Natural Science Foundation of China (grant nos. 30900650/H1615, 81372501/H1615, 81172232/H1615 and 81172564/H1625), Guangdong Natural Science Foundation (grant nos. S2012010008378 and S2013010015327), the Research Fund for the Doctoral Program of Higher Education of China (grant no. 20120171120086) and the Science and Technology Planning Project of Guangdong Province (grant no. 2012B061700078).
References
- 1.Langevin SM, Kratzke RA, Kelsey KT. Epigenetics of lung cancer. Transl Res. 2014 Mar 12; doi: 10.1016/j.trsl.2014.03.001. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shigematsu H, Gazdar AF. Somatic mutations of epidermal growth factor receptor signaling pathway in lung cancers. Int J Cancer. 2006;118:257–262. doi: 10.1002/ijc.21496. [DOI] [PubMed] [Google Scholar]
- 3.Xu L, Kikuchi E, Xu C, et al. Combined EGFR/MET or EGFR/HSP90 inhibition is effective in the treatment of lung cancers codriven by mutant EGFR containing T790M and MET. Cancer Res. 2012;72:3302–3311. doi: 10.1158/0008-5472.CAN-11-3720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Witta SE, Jotte RM, Konduri K, et al. Randomized phase II trial of erlotinib with and without entinostat in patients with advanced non-small-cell lung cancer who progressed on prior chemotherapy. J Clin Oncol. 2012;30:2248–2255. doi: 10.1200/JCO.2011.38.9411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.D’Incecco A, Cappuzzo F. Gefitinib for non-small-cell lung cancer treatment. Expert Opin Drug Saf. 2011;10:987–996. doi: 10.1517/14740338.2011.617738. [DOI] [PubMed] [Google Scholar]
- 6.Costanzo R, Piccirillo MC, Sandomenico C, et al. Gefitinib in non small cell lung cancer. J Biomed Biotechnol. 2011;2011:815269. doi: 10.1155/2011/815269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kobayashi T, Takeda M, Marumo S, Koshimo Y, Teranishi T, Higami Y, Kato M. Long-term gefitinib treatment of occult lung carcinoma with multiple brain metastases. Lung Cancer. 2013;80:109–111. doi: 10.1016/j.lungcan.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 8.Pao W, Chmielecki J. Rational, biologically based treatment of EGFR-mutant non-small-cell lung cancer. Nat Rev Cancer. 2010;10:760–774. doi: 10.1038/nrc2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tokumo M, Toyooka S, Ichihara S, et al. Double mutation and gene copy number of EGFR in gefitinib refractory non-small-cell lung cancer. Lung Cancer. 2006;53:117–121. doi: 10.1016/j.lungcan.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 10.Wrona A, Jassem J. The new TNM classification in lung cancer. Pneumonol Alergol Pol. 2010;78:407–417. (In Polish) [PubMed] [Google Scholar]
- 11.Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–2139. doi: 10.1056/NEJMoa040938. [DOI] [PubMed] [Google Scholar]
- 12.Sequist LV, Martins RG, Spigel D, et al. First-line gefitinib in patients with advanced non-small-cell lung cancer harboring somatic EGFR mutations. J Clin Oncol. 2008;26:2442–2449. doi: 10.1200/JCO.2007.14.8494. [DOI] [PubMed] [Google Scholar]
- 13.Paez JG, Jänne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–1500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- 14.Cortes-Funes H, Gomez C, Rosell R, et al. Epidermal growth factor receptor activating mutations in Spanish gefitinib-treated non-small-cell lung cancer patients. Ann Oncol. 2005;16:1081–1086. doi: 10.1093/annonc/mdi221. [DOI] [PubMed] [Google Scholar]
- 15.Weiss GJ, Liman AK, Allen J, et al. Squamous cell carcinoma of the lung with metastasis to the GI tract associated with EGFR exon 19 deletion. Case Rep Med. 2013;2013:874836. doi: 10.1155/2013/874836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fang W, Zhang J, Liang W, et al. Efficacy of epidermal growth facor receptor-tyrosine kinase inhibitors for Chinese patients with squamous carcinoma of lung harboring EGFR mutation. J Thorac Dis. 2013;5:585–592. doi: 10.3978/j.issn.2072-1439.2013.09.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khozin S, Blumenthal GM, Jiang X, et al. U.S. Food and Drug Administration Approval Summary: Erlotinib for the first-line treatment of metastatic non-small cell lung cancer with epidermal growth factor receptor exon 19 deletions or exon 21 (L858R) substitution mutations. Oncologist. 2014 May 27; doi: 10.1634/theoncologist.2014-0089. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947–957. doi: 10.1056/NEJMoa0810699. [DOI] [PubMed] [Google Scholar]
- 19.Rosell R, Moran T, Queralt C, et al. Spanish Lung Cancer Group: Screening for epidermal growth factor receptor mutations in lung cancer. N Engl J Med. 2009;361:958–967. doi: 10.1056/NEJMoa0904554. [DOI] [PubMed] [Google Scholar]
- 20.Gazdar AF. Activating and resistance mutations of EGFR in non-small-cell lung cancer: role in clinical response to EGFR tyrosine kinase inhibitors. Oncogene. 2009;28(Suppl 1):S24–S31. doi: 10.1038/onc.2009.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shigematsu H, Gazdar AF. Mutations of EGFR in lung cancers and their implications for targeted therapy. Discov Med. 2004;4:444–447. [PubMed] [Google Scholar]
- 22.Shigematsu H, Gazdar AF. Somatic mutations of epidermal growth factor receptor signaling pathway in lung cancers. Int J Cancer. 2006;118:257–262. doi: 10.1002/ijc.21496. [DOI] [PubMed] [Google Scholar]
- 23.Bean J, Riely GJ, Balak M, Marks JL, Ladanyi M, Miller VA, Pao W. Acquired resistance to epidermal growth factor receptor kinase inhibitors associated with a novel T854A mutation in a patient with EGFR-mutant lung adenocarcinoma. Clin Cancer Res. 2008;14:7519–7525. doi: 10.1158/1078-0432.CCR-08-0151. [DOI] [PMC free article] [PubMed] [Google Scholar]