Abstract
♦ Introduction: International professional groups are supporting the training of physicians in developing countries in nephrology, including peritoneal dialysis (PD). This report documents the impact of such efforts in the provision of manual PD for children with acute kidney injury (AKI) in a public hospital in Lagos, Nigeria.
♦ Methods: Medical records of all children with AKI managed with PD between July 2010 and March 2013 were reviewed.
♦ Results: Seventeen children with a mean (SEM) age of 3.8 (0.8) years received PD for 0 - 18 days; about half were infants. PD was provided manually, frequently with intercostal drains as catheters. Blockage of catheters and peritonitis occurred in 4 (23.5%) and 2 (11.8%) children, respectively. Eight (47.1%) of the 17 children had resolution of AKI and were discharged from hospital. In 4 (57.1%) of the 7 children who died, PD was performed for ≤ 2 days.
♦ Conclusion: PD for childhood AKI is feasible in resource-constrained regions with fairly good outcome. Blockage of catheter was the most common complication encountered.
Keywords: Acute kidney injury, catheters, catheter blockage, peritoneal dialysis, peritonitis, sepsis
Dialysis provides relief of complications of acute kidney injury (AKI) arising from fluid and electrolyte derangements while creating opportunity for treatment of the underlying cause of the AKI. In the absence of dialysis, the short-term outcome of AKI is frequently poor in severe cases of AKI (1-3). For most cases of AKI, peritoneal dialysis (PD) is comparable in effectiveness to other renal replacement therapy (RRT) in managing the complications of AKI (4,5); since less expertise and less expensive equipment is needed, the use of PD in developing regions of the world is recommended (6-8). However, dialysis services are still unavailable in most developing regions of the world and when present, access by children is significantly lower than for adults (9). In recent years, fellowship grants from organizations such as the International Society for Peritoneal Dialysis (ISPD), the International Pediatric Nephrology Association (IPNA) and International Society of Nephrology (ISN) have allowed physicians working in resource-constrained regions of the world to gain competencies in the provision of dialysis service.
This report documents the initiation of PD for children with AKI, hospital outcomes of these children and common complications encountered in the use of PD in the Lagos University Teaching Hospital. Between 2010 and 2012, two of the authors completed pediatric nephrology training after receiving fellowship support from the IPNA and ISPD.
Method
Hospital records of all children who received PD for AKI between July 2010 and March 2013 in Lagos University Teaching Hospital were reviewed. The hospital, located in southwest Nigeria, is a 760-bed tertiary hospital and one of two government-funded tertiary hospitals providing renal care to children in Lagos and neighboring states. It has about 65 beds in the general wards for children older than one month. The majority of critically ill children are managed in the general wards rather than in the intensive care unit (ICU) of the hospital; mostly due to lack of money and unavailability of ventilator support for young children. The hospital operates a fee-for-service policy. Prior to the start of the PD program, PD for AKI was performed for three children over a 7-year period; all three children died. Also, during this period the only paediatric nephrologist in the employ of the hospital resigned from service.
Information regarding age, sex, cause of AKI, and indications for dialysis were obtained from each child’s record. Year and month of PD, catheter type used for PD, type of PD fluid, duration of PD and complications associated with PD were also obtained. Outcome of hospitalization, either discharge, death or discharge against medical advice was also documented. Prior to the start of the study, approval was received from the Health Research and Ethics Committee of the hospital.
In all children, a PD catheter was inserted at the bedside by one of the authors. All the catheters were inserted in the midline 2 - 3 cm below the umbilicus after local skin disinfection and instillation of local anaesthetics. In children with intact sensorium, sedation with midazolam was also needed before the procedure. Catheter insertion was done using the Seldinger technique. When intercostal drains were used as PD catheters, additional fenestrations were made at the distal end of the drain to facilitate filling and drainage (Figure 1). Since 2011, the catheters were secured with a purse string after insertion to reduce the risk of leakage. A 3-way tap was used to connect the bag of PD fluid and the drainage bag (Figure 1). Drainage of effluent PD fluid was achieved via a drip-giving set attached to a urine bag using a 2-mL syringe as a connector (Figure 1,2), while filling was performed using a calibrated burrete attached to the bag of PD fluid. The PD set-up was usually checked for leakage, adequate filling and draining using 10 - 15mL/kg of normal saline before commencement of dialysis.
FIGURE 1 —

Intercostal drain, dilator, guide wire and a 3-way tap.
FIGURE 2 —

Intercostal drain inserted for peritoneal dialysis.
Dialysis was usually started with a fill volume of 20 mL/kg and an initial dwell time of 45 - 60 minutes for each cycle. In the first few days, 10 - 12 cycles of PD were performed per day. When needed, the fill volume was increased to a maximum of 30 - 40 mL/kg by day two or three. Depending on the degree of ultrafiltration needed, the strength of PD fluid used varied between 1.3% and 4.0%. Increase in the strength of PD fluid was achieved by adding the required volume of 50% dextrose water to each bag of PD fluid. Heparin dose of 250 - 500 u/L was also added to each bag of PD fluid. When serum potassium was less than 4.5mmol/L, potassium was added to each bag to achieve a concentration of 4 mmol/L.
PD was performed manually with filling and draining of the peritoneal cavity done by the resident doctors. For each child undergoing PD, a daily chart was opened in which the time and volume of fluid in and out of the peritoneal cavity during each cycle was recorded.
When peritonitis was suspected on clinical grounds, PD effluent was examined under the microscope. PD-related peritonitis was defined as > 100 white cells/mm3 with at least 50% being polymorphonuclear leucocytes (10). PD was usually discontinued when urine output exceeded 0.5 mL/kg/day and resolution of complications of AKI that warranted starting PD was achieved.
Results
During the period of 33 months, 17 children aged 4 months - 9.9 years, mean age of 3.8 (0.8) years, received PD for AKI. The number of females and infants were nine (52.9%) each. Primary kidney diseases (50%) and sepsis (40%) were the most common causes of AKI requiring dialysis. Encephalopathy (10; 34.5%), severe metabolic acidosis (5; 17.2%) and symptomatic fluid overload (8; 27.6%) such as pulmonary oedema and severe hypertension were the most common reasons for initiating PD. Only one (5.9%) child had severe hyperkalemia (Table 1). In 14 (82.4%) of the 17 children, intercostal chest drains were used as the PD catheters (Table 2). For the majority (14; 82.4%) of the children, standard PD fluids were used; in 2 (11.8%) children, ringer’s lactate with added glucose was employed. The duration of PD ranged between one cycle to 18 days with mean duration of 5.9 (1.2) days. Catheter blockage (4; 23.5%) was the most common complication of PD observed. Catheter blockage did not occur in any of the three children who had standard PD catheters. In two children (11.8%) who developed peritonitis, there were also exit site infection and leakage of fluid from the PD site. Both children received PD at the same period and for a duration of two to three weeks.
TABLE 1.
Demographics, Causes of AKI and Indications for Dialysis in the Children Studied
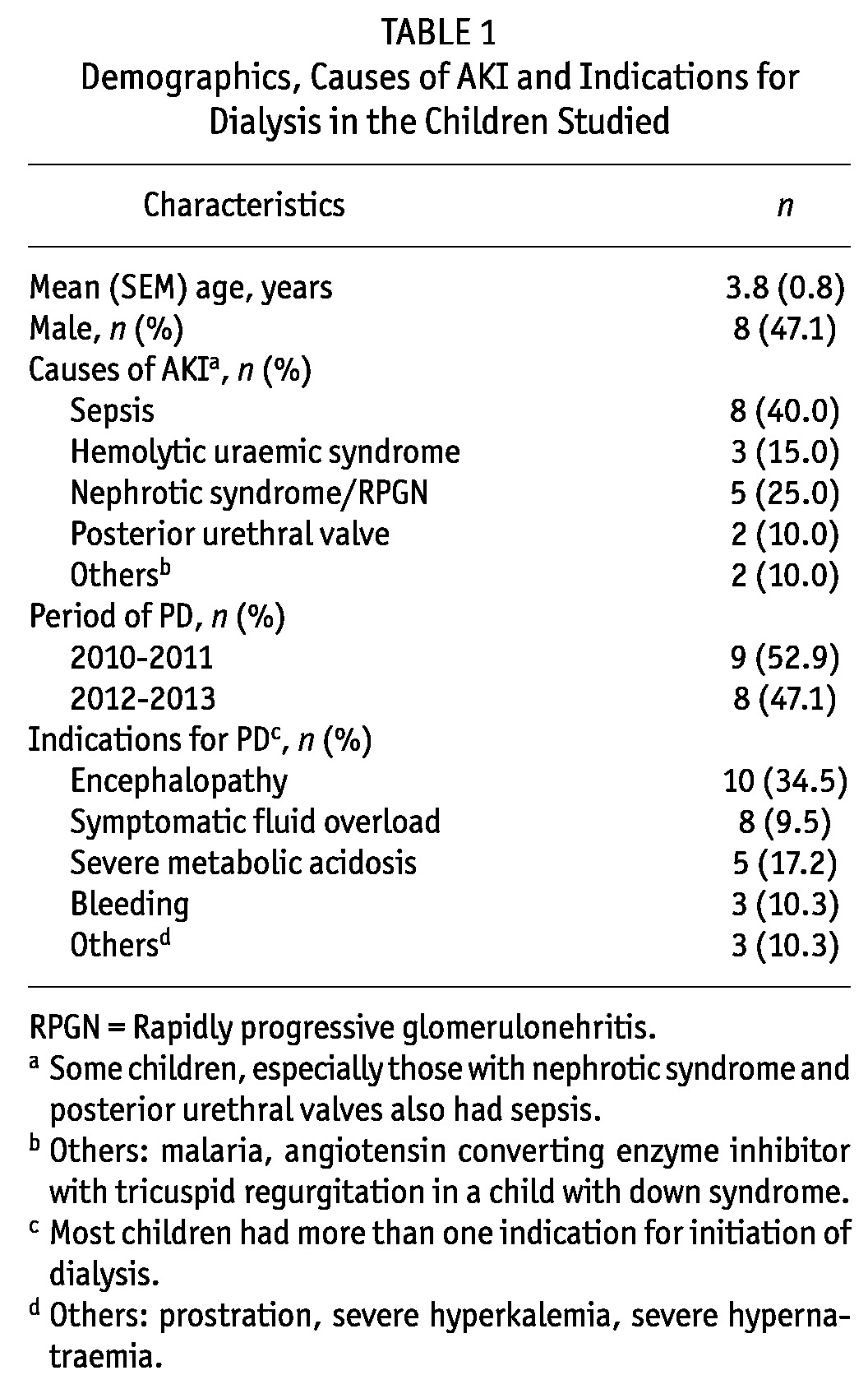
TABLE 2.
Nature of Peritoneal Dialysis Services for Acute Kidney Injury
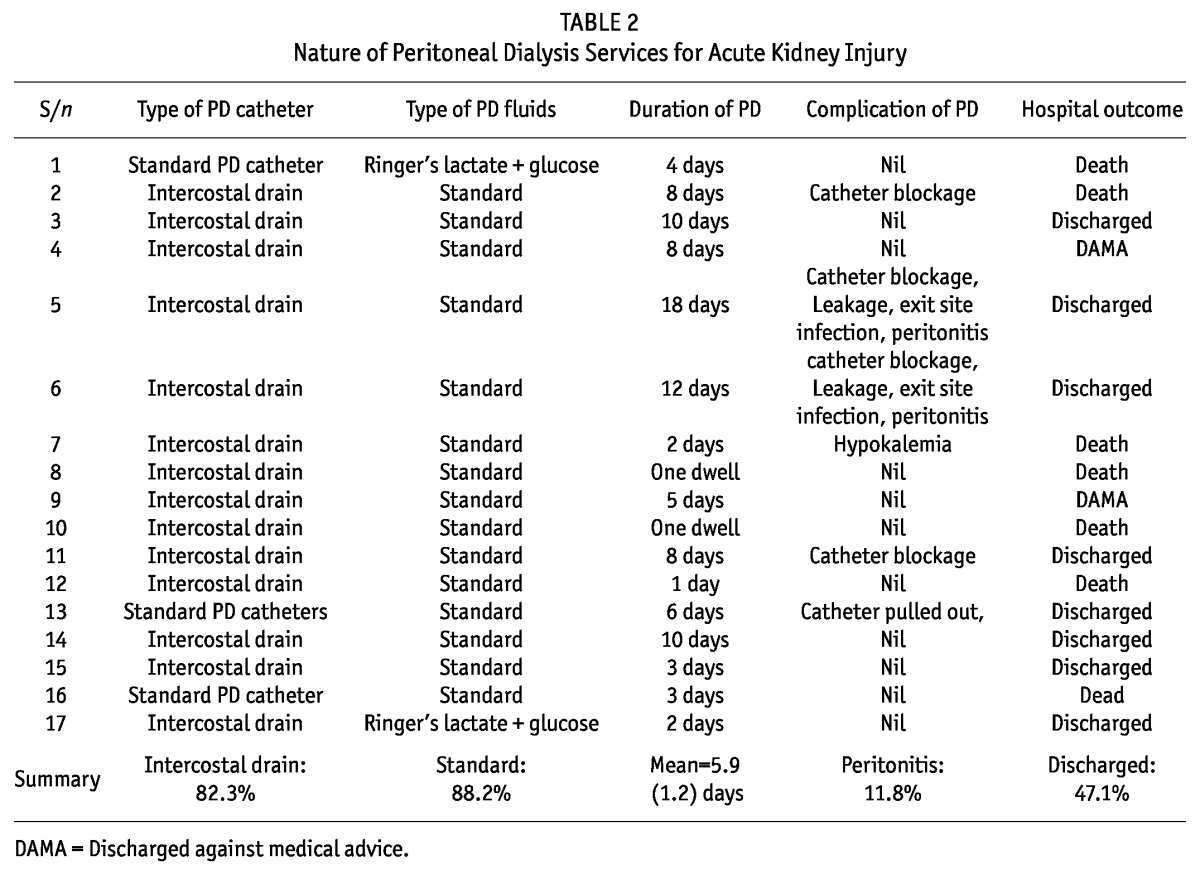
Eight (47.1%) children had resolution of AKI and were discharged from hospital. Two (11.8%) children were discharged from the hospital against medical advice by their parents while 7 (41.2%) children died in the hospital. In 4 (57.1%) of the 7 children who died, PD was provided for between one cycle to 2 days, while only 1 (12.5%) of the 8 children who survived received PD for less than 2 days.
Discussion
The present report describes the experience of a public hospital in southwest Nigeria with manual peritoneal dialysis for children with acute kidney injury. Following training support to two of the authors from the IPNA and the ISPD, provision of PD has become a regular service in Lagos University Teaching Hospital. Prior to the establishment of this service, provision of PD was virtually non-existent. Provision of acute PD services in Lagos University Teaching Hospital reflects the steady growth in the number of centers providing dialysis services for children in developing countries of the world (11-13).
Our report reveals that provision of PD for AKI is possible with fairly good outcome even in regions where the required equipment and consumables are not available. In our center almost every aspect of the PD set-up was improvised. For instance, we frequently used intercostal chest drains and occasionally had to prepare PD fluids in order to provide PD services. In three patients conventional PD catheters were used, the catheters were brought home when the managing paediatricians visited other centers outside the country. Standard PD catheters are frequently unavailable in Nigeria, and when available, the exorbitant cost represents a significant barrier to their use in most of our patients (13). The common need for most of the cuffed catheters to be inserted by the surgeons further discourages their use in our practice environment where most patients present late. On the other hand, the intercostal drains cost less than half the cost of the standard catheters and could be easily inserted at the bedside, cutting down the time to start of PD. In the literature, the use of nasogastric tubes, central venous catheters and urethral catheters has been described (7,13). While standard PD fluid was frequently available, its use was constrained by high cost, which went as high as 40 US dollars for a 2-litre bag during the study period. It is hoped that as more centers provide PD, in-country manufacture of PD fluid will be encouraged with the advantages of making stock-out less frequent and the overall cost of providing PD less exorbitant.
PD insertion at the bedside by the paediatricians in our center cuts down the time required to start dialysis. With a substantial number of the children treated for AKI in our center presenting late to hospital with complications of AKI, the ability to start PD promptly is desirable. Late presentation to the hospital is common in developing regions of the world and thus the use of PD for AKI over other forms of renal replacement therapy is recommended, despite the fact that all three modalities are reported to be equally effective for most cases of AKI (5,14).
Despite the challenges of providing PD in our center, about half of the children with AKI managed with PD survived and were discharged from hospital. We envisage that the proportion of children who would have survived would have been higher if the children with AKI presented to the hospital earlier. This view is supported by the observation that over half of the children who died received PD for two or fewer days, with two children dying after only one dwell of PD fluid. Nonetheless, the mortality rate in the present study is mid-way in the range of mortality rates described in various studies of AKI from other developing regions of the world (7,12,15). In a recent study from Ibadan, southwest Nigeria which documented a 70% survival rate in children who received PD for AKI, nine children who died from AKI following diethylene glycol poisoning and another five children whose hospital records were not available were excluded from analysis (7). The high mortality in these studies and ours underscores the fact that most children with AKI are severely ill and, in addition to renal replacement therapy, require intensive unit care (16,17). Unfortunately, access to an intensive care unit is generally unavailable in these regions of the world, where acute dialysis is also unavailable.
The low frequency of peritonitis in the present study, despite 40% of the children receiving dialysis for more than one week, is reassuring. In the two children who developed peritonitis, PD was performed for longer periods (12 and 18 days, respectively) and both had leakages from the PD site and exit site infection. Similarly low peritonitis rates have been reported in developing countries supporting the safety of PD for AKI in resource-poor settings (11,12). A common complication, however, was catheter blockage leading to a ball-valve effect in which filling was easily achieved but drainage of peritoneal cavity was ineffective. The use of intercostal drains with larger fenestrations rather than the finer fenestrations in standard PD catheters may have been responsible for this complication. In general, these complications associated with PD are infrequently encountered when Tenckhoff catheters, surgically inserted, and a PD cycler are used (18).
There is a need to curb the high cost of procuring standard PD fluid in resource-poor countries, as cost remains a significant hurdle to the provision of PD (2,9,13). In the short and long term, advocacy by organizations such as ISPD, IPNA and ISN to manufacturers of PD fluid could provide meaningful improvement in children’s access to dialysis. There is also the need to train more people, including nurses, in developing regions of the world were PD may be the only form of RRT available to children with AKI. Programs aimed at facilitating prompt presentation of sick children to the hospital may also improve the outcome of AKI in our region. However, sustainability should be the common feature of these efforts to improve access to and outcome of PD in resource-constrained regions.
A major limitation of the present study is the small number of children included and the inability to obtain AKI data before the initiation of the PD program. Nonetheless, the provision of PD in this center, as described in this report, represents a significant milestone in the care of children with kidney disease in this region of the world and also highlights the impact of fellowship programs by international organizations.
Conclusion
Peritoneal dialysis for acute kidney injury in children is feasible in developing regions of the world with reasonably good outcome. Catheter blockage was the most common complication encountered with the use of PD in this study.
Disclosure
The authors declare that no financial conflict of interest exists.
Acknowledgments
We express our gratitude to the resident doctors in the Department of Paediatrics of the Lagos University Teaching Hospital who participated in providing peritoneal dialysis during the study period.
References
- 1. Anochie IC, Eke FU. Paediatric acute peritoneal dialysis in southern Nigeria. Postgraduate medical journal 2006; 82:228–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Olowu WA. Renal failure in Nigerian children: factors limiting access to dialysis. Pediatric nephrology 2003; 18:1249–54 [DOI] [PubMed] [Google Scholar]
- 3. Esezobor CI, Ladapo TA, Osinaike B, Lesi FE. Paediatric acute kidney injury in a tertiary hospital in Nigeria: prevalence, causes and mortality rate. PloS one 2012; 7:e51229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gabriel DP, Caramori JT, Martim LC, Barretti P, Balbi AL. High volume peritoneal dialysis vs daily hemodialysis: a randomized, controlled trial in patients with acute kidney injury. Kidney international Supplement 2008; S87–93 [DOI] [PubMed] [Google Scholar]
- 5. George J, Varma S, Kumar S, Thomas J, Gopi S, Pisharody R. Comparing continuous venovenous hemodiafiltration and peritoneal dialysis in critically ill patients with acute kidney injury: a pilot study. Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis 2011; 31:422–9 [DOI] [PubMed] [Google Scholar]
- 6. Callegari JG, Kilonzo KG, Yeates KE, et al. Peritoneal dialysis for acute kidney injury in sub-Saharan Africa: challenges faced and lessons learned at Kilimanjaro Christian Medical Centre. Kidney international 2012; 81:331–3 [DOI] [PubMed] [Google Scholar]
- 7. Ademola AD, Asinobi AO, Ogunkunle OO, Yusuf BN, Ojo OE. Peritoneal dialysis in childhood acute kidney injury: experience in southwest Nigeria. Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis 2012; 32:267–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Phadke KD, Dinakar C. The challenges of treating children with renal failure in a developing country. Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis 2001; 21 Suppl 3:S326–9 [PubMed] [Google Scholar]
- 9. Abu-Aisha H, Elamin S. Peritoneal dialysis in Africa. Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis 2010; 30:23–8 [DOI] [PubMed] [Google Scholar]
- 10. Chadha V, Schaefer FS, Warady BA. Dialysis-associated peritonitis in children. Pediatric nephrology 2010; 25:425–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kilonzo KG, Ghosh S, Temu SA, et al. Outcome of acute peritoneal dialysis in northern Tanzania. Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis 2012; 32:261–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mishra OP, Gupta AK, Pooniya V, Prasad R, Tiwary NK, Schaefer F. Peritoneal dialysis in children with acute kidney injury: a developing country experience. Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis 2012; 32:431–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Esezobor CI, Oniyangi O, Eke F. Paediatric dialysis services in Nigeria: availability, distribution and challenges. West African journal of medicine 2012; 31:181–5 [PubMed] [Google Scholar]
- 14. Gabriel DP, Caramori JT, Martin LC, Barretti P, Balbi AL. Continuous peritoneal dialysis compared with daily hemodialysis in patients with acute kidney injury. Peritoneal dialysis international: journal of the International Society for Peritoneal Dialysis 2009; 29 Suppl 2:S62–71 [PubMed] [Google Scholar]
- 15. Acharya UT, Singla PN, Singh RG, Usha, Mishra OP. Outcome of dialysed patients with acute renal failure. Indian pediatrics 1996; 33:387–90 [PubMed] [Google Scholar]
- 16. Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney international 2007; 71:1028–35 [DOI] [PubMed] [Google Scholar]
- 17. Chang JW, Tsai HL, Wang HH, Yang LY. Outcome and risk factors for mortality in children with acute renal failure. Clinical nephrology 2008; 70:485–9 [DOI] [PubMed] [Google Scholar]
- 18. Wong SN, Geary DF. Comparison of temporary and permanent catheters for acute peritoneal dialysis. Archives of disease in childhood 1988; 63:827–31 [DOI] [PMC free article] [PubMed] [Google Scholar]


