Abstract
Purpose
To compare the efficacy, predictability, safety, and induced higher-order aberrations (HOAs) between wavefront-guided and non-wavefront-guided photorefractive keratectomy (PRK).
Methods
The Cochrane Central Register of Controlled Trials, PubMED, and EMBASE were searched for randomized controlled trials. Trials meeting the selection criteria were quality appraised, and data was extracted by 2 independent authors. Measures of association were pooled quantitatively using meta-analytical methods. Comparisons between wavefront-guided and non-wavefront-guided ablations were made as pooled odds ratios (ORs) or weighted mean differences. The pooled ORs and 95% confidence intervals (CIs) were computed for efficacy, safety, and predictability. The weighted mean differences and 95% CIs were used to compare induced HOAs.
Results
The study covered five trials involving 298 eyes. After wavefront-guided PRK, the pooled OR of achieving an uncorrected distance visual acuity of 20/20 (efficacy) was 1.18 (95% CI, 0.53–2.60; p = 0.69), the pooled OR of achieving a result within ±0.50 diopter of the intended target (predictability) was 0.86 (95% CI, 0.40–1.84; p = 0.70). No study reported a loss of 2 or more lines of Snellen acuity (safety) with either modality. In eyes with wavefront-guided PRK, the postoperative trefoil aberrations (mean difference −0.02; 95% CI, −0.03 to −0.00; p = 0.03) were significantly lower. There were no significant differences between the two groups in the postoperative total HOAs (mean difference −0.04; 95% CI, −0.23 to 0.14; p = 0.63), spherical (mean difference 0.00; 95% CI, −0.08 to 0.09; p = 0.93), and coma (mean difference −0.06; 95% CI, −0.14 to 0.03; p = 0.20) aberrations.
Conclusions
According to the meta-analysis, wavefront-guided PRK offered no advantage in efficacy, predictability, or safety measures over non-wavefront-guided PRK, although it may have induced fewer trefoil aberrations.
Introduction
Today, excimer refractive surgery is the treatment of choice for the correction of low to moderate myopia. [1]–[4] However, irregularities in the optical system after refractive surgery can cause subjective complaints, such as halos and glare, that are attributed to an increase in higher-order aberrations (HOAs). [5], [6] This explains why nearly 30% of patients report night-vision problems after successful laser refractive surgery. [7], [8].
Wavefront-guided ablation was introduced to better control aberrations caused by refractive surgery. [9], [10] However, the effectiveness of wavefront-guided ablation has been questioned. Studies comparing wavefront-guided ablation and conventional treatment report inconsistent results, ranging from a significant reduction in preexisting aberrations to no difference to deterioration in preexisting HOAs in wavefront-guided-treated eyes. [11]–[14] According to the meta-analysis, wavefront-guided laser in situ keratomileusis (LASIK) did not offer any advantage in efficacy, predictability, or safety measures over non-wavefront-guided LASIK, although it induced fewer total HOAs. [15] However, as far as we can ascertain, there have so far been no clinical studies that have compared these visual, refractive, aberrometric outcomes between wavefront-guided and non-wavefront-guided photorefractive keratectomy (PRK) using meta-analysis. To determine whether wavefront-guided ablation shows any advantages over non-wavefront-guided alternatives in PRK, we performed a meta-analysis of all published randomized controlled trials (RCTs) of wavefront-guided laser treatments. We also compared the efficacy, predictability, safety, and change in optical aberrations between wavefront-guided and non-wavefront-guided PRK treatments.
Materials and Methods
In the following databases, data source articles limited to RCTs and published between January 2000 and the end of December 2013 were examined: PubMed (Medline), EMBASE, and Cochrane Central Register of Controlled Trials. Photorefractive keratectomy is the term for sensitive searches. Also, the reference lists of every primary article and all previous systematic reviews were scrutinized for information about additional trials. The searches were not restricted to a specific language.
Trial Selection
First, 2 reviewers (H.K., K.H.) independently assessed studies for possible eligibility at the title and/or abstract level. The inclusion criteria were met in patients randomly assigned prospectively to refractive error correction with a wavefront-guided laser treatment or a non-wavefront-guided laser treatment. A minimum follow-up of 3 months was required.
Data Extraction
Two independent reviewers (H.K., K.K.) extracted data from the included trials using a standardized form. The data of interest for each clinical outcome were extracted as follows:
Efficacy: the number of eyes postoperatively achieving an uncorrected distance visual acuity (UDVA) of 20/20 or better.
Predictability: the number of eyes achieving a postoperative spherical equivalent (SE) within ±0.50 diopter (D) of the intended target.
Safety: the number of eyes that lost 2 or more lines of postoperative corrected distance visual acuity (CDVA) relative to the preoperative CDVA [16]–[18].
Higher-order aberrations: the root mean square (RMS) values of the total HOAs, spherical, coma, and trefoil aberration.
The data extracted from each study were the numbers of eyes in the wavefront-guided and non-wavefront-guided groups according to the criteria stated above for the final follow-up visit. The sample size and the follow-up period were also recorded. The corresponding authors of the individual trials were also contacted for unpublished information.
The quality of each trial was assessed using the Jadad et al. [19] score with a scale of 0 to 5. Each trial was assessed by 3 main aspects of study design: randomization, masking, and participant withdrawals/dropouts. Trials with a score higher than 3 were considered to be of high quality.
Statistical Analysis
For efficacy, predictability, and safety, the data in each study were tabulated into 2 × 2 tables and the odds ratio (OR) and 95% confidence intervals (CIs) of the results between wavefront-guided treatments and non-wavefront-guided treatments were compared. The pooled OR and 95% CI were also determined according to a previously described methodology. [20] For HOAs, the statistical option used for meta-analysis was the weighted mean difference for comparing the mean postoperative RMS ± standard deviation (SD) values between the 2 groups. Eyes were divided into 2 subgroups on the basis of the preoperative total HOA values. Heterogeneity was also assessed, and an I2 value greater than 50% was considered significant. In this instance, a random-effects model was used because it gives a more conservative estimate and is less influenced by the weighting of each study. [21] When the level of heterogeneity was less than 50%, a fixed-effect model was used. Publication bias was assessed visually with a funnel plot. [22] Meta-analysis was performed with Revman software (version 5.2, Information Management Systems Group, Cochrane Collaboration).
Results
Results of Search
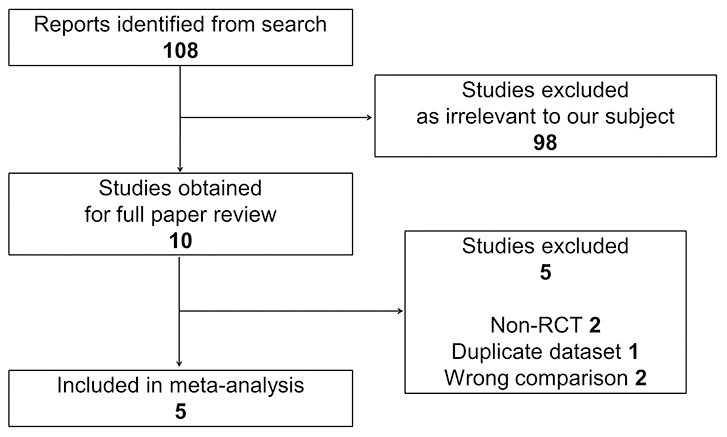
There were 108 articles relevant to the search terms. Ninety-eight studies were excluded after abstract evaluation. Of 10 publications, [23]–[32] which were initially considered potentially relevant, five were excluded because they did not meet the predefined inclusion criteria (Figure 1). [24], [26], [27], [29], [31] The other five prospective RCTs were included in this meta-analysis. [23], [25], [28], [30], [32].
Figure 1. Flow of trial selection. RCTs = randomized controlled trials.
Characteristics and Quality of Trials
Table 1 shows the main characteristics and quality score of the included trials. Three [28], [30], [32] of the 5 trials were unilateral-eye studies; eyes were matched for SE, and age matching and sex matching was not required. The other 2 studies [23], [25] used 2 different populations in 2 of the trials that matched groups for age and SE. Four studies compared wavefront-guided PRK and conventional PRK [23], [25], [28], [32], and the other study compared wavefront-guided PRK and wavefront-optimized PRK [30]. No study compared wavefront-guided PRK and topography-guided PRK. All the 5 trials were deemed to be of high quality (Jadad score ≥3).
Table 1. Characteristics and quality of included trials evaluating wavefront-guided versus non-wavefront-guided photorefractive keratectomy.
| Study* (Year) | Country | Score** | Mean Preop SE (D) | Platform | ||
| WG-PRK | NWG-PRK | WG-PRK | NWG-PRK | |||
| Mifflin [32] (2012) | USA | 4 | −3.22±1.86 | −3.2±1.72 | Visix Cutsom Vue | Visix S4, conv. |
| Moshirfar [30] (2011) | USA | 3 | −3.34±1.75 | −3.26±1.82 | Visix Cutsom Vue | Wavelight Allegretto |
| Karimian [28] (2010) | Iran | 5 | −4.92±1.60 | −4.92±1.60 | Technolas 217z Zyoptic | Technolas 217z, conv. |
| Mastropasqua [25] (2006) | Italy | 3 | −2.25±0.76 | −2.35±1.10 | Technolas 217z Zyoptic | Technolas 217z, conv. |
| Mastropasqua [23] (2004) | Italy | 3 | −4.39±1.31 | −4.08±0.97 | Meditec MEL 70, WASCA | Meditec MEL 70, conv. |
SE = spherical equivalent; WG = wavefront-guided; NWG = non-wavefront-guided; PRK = photorefractive keratectomy.
*First author; **Jadad scores.
Efficacy
Meta-analysis in relation to efficacy was performed for 3 of the 5 studies because 2 studies [23], [25] reported no proportion of eyes with a UDVA of 20/20 or better. The efficacy Forest plot showed an equivalent treatment efficacy between wavefront-guided PRK and non-wavefront-guided PRK (OR, 1.18; 95% CI, 0.53–2.60; p = 0.69) (Figure 2).
Figure 2. Forest plot comparing efficacy of WFG-PRK and Non-WFG-PRK.
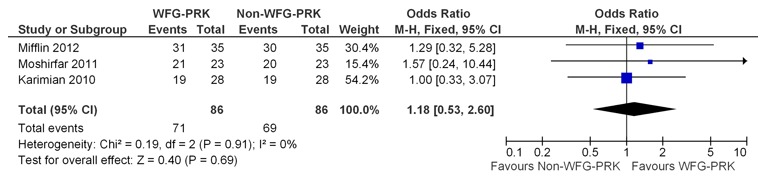
Each study is represented by a square at the point of treatment effect, and the area of the square is proportional to the weighting of that study in the analysis. A horizontal line on either side of each square represents the CI. The diamond at the bottom of the plot represents the overall treatment effect determined by the position at the center of the diamond and the CI of the combined data conveyed by the width of the diamond. WFG-PRK = wavefront guided photorefractive keratectomy, Non-WFG-PRK = non-wavefront guided photorefractive keratectomy, M-H = Mantel-Haenszel, CI = confidence interval, Chi2 = chi-square statistic, df = degrees of freedom, I2 = I-square heterogeneity statistic, Z = Z-statistic.
Predictability
Meta-analysis in relation to predictability was performed for 4 of the 5 studies because one study [23] did not include data on predictability. The predictability Forest plot showed equivalent predictability between wavefront-guided PRK and non-wavefront-guided PRK (OR, 0.86; 95% CI, 0.40–1.84; p = 0.70) (Figure 3).
Figure 3. Forest plot comparing predictability of WFG-PRK and Non-WFG-PRK.
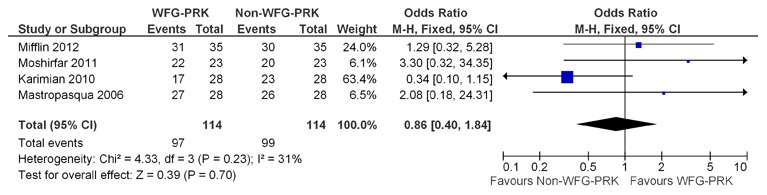
WFG-PRK = wavefront guided photorefractive keratectomy, Non-WFG-PRK = non-wavefront guided photorefractive keratectomy, M-H = Mantel-Haenszel, CI = confidence interval, Chi2 = chi-square statistic, df = degrees of freedom, I2 = I-square heterogeneity statistic, Z = Z-statistic.
Safety
Data for this outcome were collected from 2 trials. [30], [32] No patient lost 2 or more lines of CDVA; hence meta-analysis was not applicable. Table 2 shows the clinical data in the 5 studies with regard to safety.
Table 2. Eyes losing or gaining lines in Snellen CDVA.
| Number (%) | ||||||||
| Lost≥2 Lines | Lost 1 Line | No Change | Gained≥1 Lines | |||||
| Study* | WG-PRK | NWG-PRK | WG-PRK | NWG-PRK | WG-PRK | NWG-PRK | WG-PRK | NWG-PRK |
| Mifflin [32] | 0 | 0 | 4 (11.4) | 2 (5.7) | 18 (51.4) | 13 (37.1) | 13 (37.1) | 20 (57.1) |
| Moshirfar [30] | 0 | 0 | 1 (4.3) | 1 (4.3) | 16 (69.6) | 16 (69.6) | 6 (26.1) | 6 (26.1) |
| Karimian [28] | NA | NA | NA | NA | NA | NA | NA | NA |
| Mastropasqua [25] | NA | NA | NA | NA | NA | NA | NA | NA |
| Mastropasqua [23] | NA | NA | NA | NA | NA | NA | NA | NA |
CDVA = corrected distance visual acuity; NA = data not available; WG = wavefront-guided; NWG = non-wavefront-guided; PRK = photorefractive keratectomy.
*First author.
Higher-Order Aberrations
Meta-analysis in relation to total HOAs, and to spherical, coma, and trefoil aberrations was conducted in 3 of the 5 studies. Of the 2 omitted studies, one [25] reported results on preoperative total HOAs, but the postoperative values for each group were not reported. One study [30] reported the HOA data in the figures, but the aberratios values for each group were not shown in the text. The total HOAs, spherical, and coma aberration Forest plots showed no significant differences in these values after treatment between wavefront-guided PRK and non-wavefront-guided PRK (Figure 4 A, B, and C). The trefoil aberration Forest plots showed that the increase in trefoil aberration in patients who had wavefront-guided PRK was less than that in those who had non-wavefront-guided PRK (weighted mean difference = −0.02; 95% CI, −0.03 to −0.00; p = 0.03) (Figure 4 D). Table 3 shows the clinical data in the 5 HOA studies.
Figure 4. Forest plot comparing HOAs outcomes after treatment with WFG-PRK and Non-WFG-PRK.
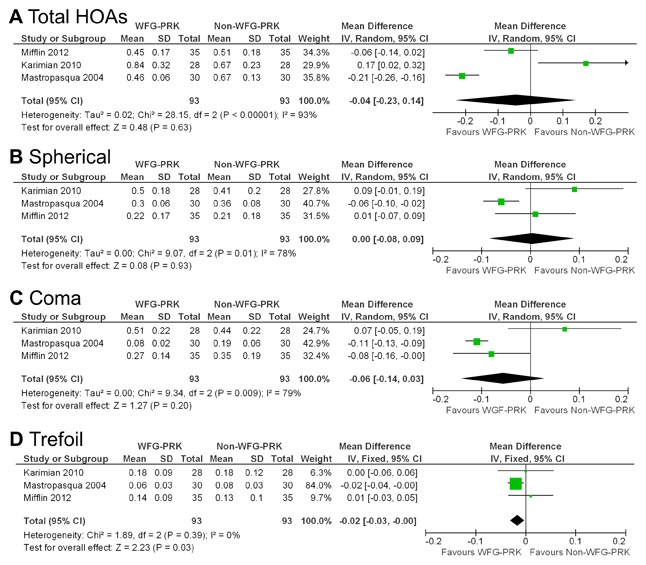
A, Total HOAs. B, Spherical aberration. C, Coma aberration. D, Trefoil aberration. HOAs = higher-order aberrations, WFG-PRK = wavefront guided photorefractive keratectomy, Non-WFG-PRK = non-wavefront guided photorefractive keratectomy, IV = inverse variance, CI = confidence interval, Tau2 = tau-square statistic, Chi2 = chi-square statistic, df = degrees of freedom, I2 = I-square heterogeneity statistic, Z = Z-statistic.
Table 3. Preoperative and postoperative total HOAs values by group.
| Preop total HOAs | Postop total HOAs | ||||
| Study* | Pupil size (mm) | WG-PRK | NWG-PRK | WG-PRK | NWG-PRK |
| Mifflin [32] | 6.0 | 0.38±0.13 | 0.33±0.13 | 0.45±0.17 | 0.51±0.18 |
| Moshirfar [30] | 6.0 | NA | NA | NA | NA |
| Karimian [28] | 6.0 | 0.33±0.09 | 0.34±0.08 | 0.84±0.32 | 0.67±0.23 |
| Mastropasqua [25] | 6.0 | 0.35±0.10 | 0.32±0.14 | NA | NA |
| Mastropasqua [23] | 5.0 | 0.27±0.10 | 0.28±0.09 | 0.46±0.06 | 0.67±0.13 |
HOAs = higher-order aberrations; WG = wavefront-guided; NWG = non-wavefront-guided; PRK = photorefractive keratectomy; NA = data not available.
*First author.
Two studies [23], [25] reported data with preoperative total HOA errors ≤0.3 µm. Analysis of these data revealed that the difference between the two groups was not statistically significant (weighted mean difference = −0.05; 95% CI, −0.12 to 0.03; p = 0.24) (Figure 5 A). Four studies [23], [25], [28], [32] reported data with preoperative total HOA errors of more than 0.3 µm. Analysis of these data revealed that the difference between the two groups was not statistically significant (weighted mean difference = −0.17; 95% CI, −0.39 to 0.06; p = 0.15) (Figure 5 B).
Figure 5. Forest plot comparing total HOAs outcomes after treatment with WFG-PRK and Non-WFG-PRK in patients divided into 2 groups based on preoperative total HOAs.
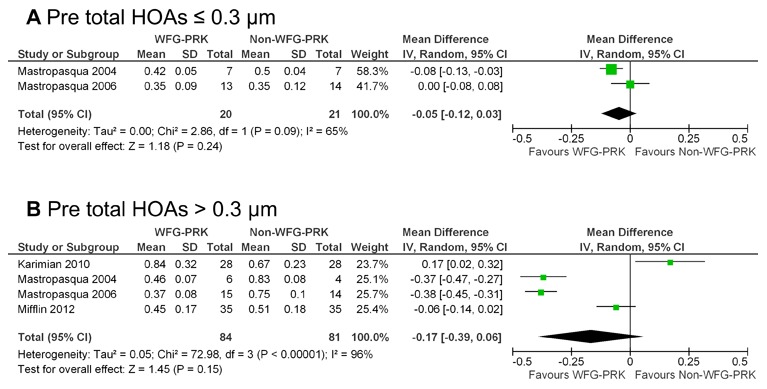
A, Preoperative total HOAs ≤0.3 µm. B, Preoperative total HOAs >0.3 µm. HOAs = higher-order aberrations, WFG-PRK = wavefront guided photorefractive keratectomy, Non-WFG-PRK = non-wavefront guided photorefractive keratectomy, IV = inverse variance, CI = confidence interval, Tau2 = tau-square statistic, Chi2 = chi-square statistic, df = degrees of freedom, I2 = I-square heterogeneity statistic, Z = Z-statistic.
Complications
None of patients in either group showed evidence of corneal haze in both groups at the last follow-up visit [23], [25], [28], [32].
Publication Bias
The publication bias was independently assessed graphically for each clinical outcome using funnel plots (Figure 6). For efficacy and predictability, each study was plotted with the OR against the standard error as a measure of weighting. For aberrations, each study was plotted with the weighted mean difference against the standard error as a measure of weighting. There was an almost equal distribution between studies with a low and high OR/weighted mean difference and a low and high standard error for efficacy, predictability, and trefoil aberration.
Figure 6. Funnel plots showing the distribution between studies comparing each outcome.
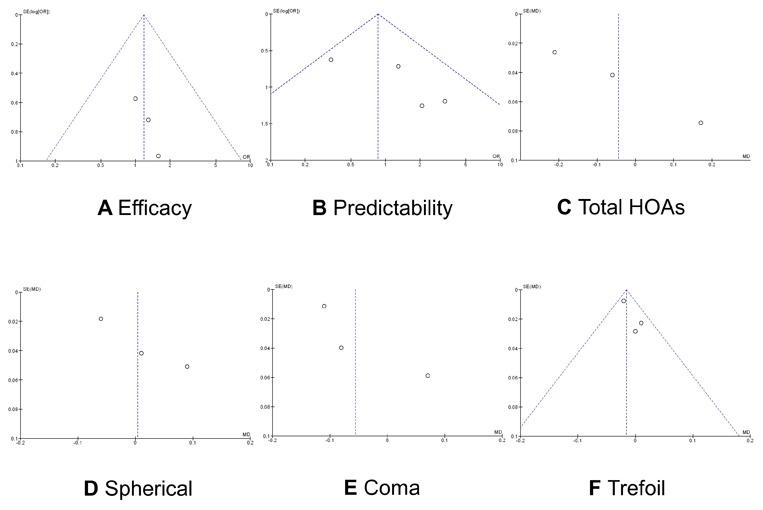
A, Efficacy, B, Predictability, C, Total HOAs. D, Spherical aberration. E, Coma aberration. F, Trefoil aberration.
Discussion
This meta-analysis provides evidence that wavefront-guided and non-wavefront-guided PRK approaches can provide similar results in terms of visual outcomes (efficacy, predictability, and safety). Our results agree with those of Fares et al. [15], who also noted these outcomes after wavefront-guided LASIK using meta-analysis. To our knowledge, this is the first published study to compare the visual outcomes between wavefront-guided and non-wavefront-guided PRK techniques using meta-analysis. Netto et al. [33] reviewed the benefits and limitations of wavefront-guided PRK. They concluded that, while wavefront-guided refractive surgery provides excellent results, evidence is limited that it outperforms the conventional technique, which incorporates broad ablation zones, smoothing to the periphery, eye-trackers, and other technological refinements.
Although PRK is currently not a gold standard of corneal refractive surgery, it offers some advantages over LASIK, in terms of less induction of higher-order aberrations [34], less induction of refractive regression [35], better biomechanical stability [36], and no risk of flap-related complications [37]. Therefore, PRK is still one of the viable surgical options for the correction of refractive errors.
The key indicator of efficacy of any given refractive surgical procedure is visual acuity. It is important that visual acuity should be specifically recorded for each time point, and that results should refer to the exact line seen by the patient on the Snellen acuity chart. Such detailed information is critical when outcomes in different studies are compaied. [38]–[40] Throughout our review, we noticed that authors had presented their outcome data in diverse ways. However, 3 of 5 studies reported the UDVA to be 20/20 or better. Thus, the efficacy in our study was evaluated only at 20/20 or better. The percentage of eyes with a UDVA of 20/20 or better at the last follow-up visit was 82.6% in the wavefront-guided group and 80.2% in the non-wavefront-guided group. However, this difference was not statistically significant.
Predictability data was reported by 4 of the 5 studies that qualified for inclusion in our study. The percentage of eyes with an SE of ±0.50 D at the last follow-up visit was 85.1% in the wavefront-guided group and 86.8% in the non-wavefront-guided group. However, this difference was not statistically significant.
Safety is also an important parameter when refractive surgery outcomes are reported, and it should be expressed in terms of the change in the Snellen lines of CDVA. Although the safety of both wavefront-guided PRK and non-wavefront-guided PRK has been reported, only 2 of the 5 RCTs included in our meta-analysis reported their safety criteria. It is important that more attention be paid to reporting safety criteria in studies of refractive surgery outcomes.
HOA data was reported by 3 of the 5 studies that qualified for inclusion in our study. We found no significant difference in the postoperative total HOAs, spherical, or coma aberration between wavefront-guided and non-wavefront-guided groups. However, there was a significant difference in postoperative trefoil aberration between the two groups. As far as we can ascertain, this is also the first study to assess the HOAs including spherical, coma, and trefoil aberrations after wavefront-guided and non-wavefront-guided PRK techniques using meta-analysis. Overall wavefront-guided PRK had fewer induced HOAs than non-wavefront-guided PRK, although our meta-analysis showed no significant difference. For eyes with preoperative total HOA values of ≤0.3 µm, the mean postoperative total HOA did not differ significantly between the two groups. On the one hand, in cases with preoperative total HOA values of >0.3 µm, wavefront-guided PRK resulted in a slightly better postoperative aberration profile, suggesting that in eyes with high preexisting HOAs, wavefront-guided treatment may have advantages over non-wavefront-guided treatment. With regard to wavefront-guided LASIK, meta-analysis showed that wavefront-guided technology induced a smaller increase of postoperative wavefront-error compared to non-wavefront-guided technology, particularly in patients with higher preoperative HOAs. [15] The induction of HOAs may lead to a deterioration in visual performance and subsequent patient dissatisfaction. As conventional PRK technique requires more laser ablation in high myopic eyes, the cornea becomes more oblate, resulting in more surgically induced HOAs, especially spherical aberrations. Wavefront-guided treatment has been reported to be more effective in reducing the induction of HOAs than conventional treatment.
This meta-analysis has several limitations that should be taken into account when its results are considered. First, the follow-up duration reported in these trials was limited. All the five studies reported data for less than 1 year, limiting the value of conclusions concerning the stability and long-term regression. Additionally, the recovery of corneal innervation and the restoration of a normal tear film and the ocular surface may take longer than 12 months. [41], [42] There is evidence that increases in higher order aberrations resulted from increased tear film and ocular surface irregularity. [43] Second, the small number of cases per trial and in total give these analyses low power. Subgroup analysis related to the degree of myopia was not possible because there was insufficient data. Nevertheless, this meta-analysis provides more powerful evidence than the individual reports alone, and we are unaware of any other similar meta-analyses. Third, we could include only data from published articles, and it is possible that bias is introduced if studies with small or reverse effects exist but have not been published. However, our asymmetrical funnel plots for efficacy, predictability, and trefoil aberration indicate that publication bias may be ruled out.
In summary, it can be assumed from this meta-analysis that wavefront-guided and non-wavefront-guided procedures have comparable efficacy, predictability, and safety for PRK. In addition, wavefront-guided PRK may induce fewer trefoil aberrations than non-wavefront-guided PRK, which might make it a better choice for wavefront custom ablation, although both approaches result in similar wavefront outcomes for total HOAs, spherical, and coma aberrations. Long-term follow-up trials with large patient populations are needed to determine the relative merits wavefront-guided and non-wavefront-guided PRK using current-day equipment and techniques.
Supporting Information
PRISMA checklist.
(DOC)
Acknowledgments
The authors are grateful to Mr. C. W. P. Reynolds for his careful linguistic assistance with this manuscript.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
These authors have no support or funding to report.
References
- 1. Sugar A, Rapuano CJ, Culbertson WW, Huang D, Varley GA, et al. (2002) Laser in situ keratomileusis for myopia and astigmatism: safety and efficacy: a report by the American Academy of Ophthalmology. Ophthalmology 109: 175–187. [DOI] [PubMed] [Google Scholar]
- 2. Solomon KD, Holzer MP, Sandoval HP, Vargas LG, Werner L, et al. (2002) Refractive Surgery Survey 2001. J Cataract Refract Surg 28: 346–355. [DOI] [PubMed] [Google Scholar]
- 3. Lindstrom RL, Maller BS (1999) Market trends in refractive surgery. J Cataract Refract Surg 25: 1408–1411. [DOI] [PubMed] [Google Scholar]
- 4. Duffey RJ, Leaming D (2002) U.S. trends in refractive surgery: 2001 International Society of Refractive Surgery Survey. J Refract Surg 18: 185–188. [DOI] [PubMed] [Google Scholar]
- 5. Bailey MD, Mitchell GL, Dhaliwal DK, Boxer Wachler BS, Zadnik K (2003) Patient satisfaction and visual symptoms after laser in situ keratomileusis. Ophthalmology 110: 1371–1378. [DOI] [PubMed] [Google Scholar]
- 6. Marcos S (2001) Aberrations and visual performance following standard laser vision correction. J Refract Surg 17: S596–601. [DOI] [PubMed] [Google Scholar]
- 7. Mrochen M, Kaemmerer M, Mierdel P, Seiler T (2001) Increased higher-order optical aberrations after laser refractive surgery: a problem of subclinical decentration. J Cataract Refract Surg 27: 362–369. [DOI] [PubMed] [Google Scholar]
- 8. Moreno-Barriuso E, Lloves JM, Marcos S, Navarro R, Llorente L, et al. (2001) Ocular aberrations before and after myopic corneal refractive surgery: LASIK-induced changes measured with laser ray tracing. Invest Ophthalmol Vis Sci 42: 1396–1403. [PubMed] [Google Scholar]
- 9. Williams D, Yoon GY, Porter J, Guirao A, Hofer H, et al. (2000) Visual benefit of correcting higher order aberrations of the eye. J Refract Surg 16: S554–559. [DOI] [PubMed] [Google Scholar]
- 10. Liang J, Williams DR, Miller DT (1997) Supernormal vision and high-resolution retinal imaging through adaptive optics. J Opt Soc Am A Opt Image Sci Vis 14: 2884–2892. [DOI] [PubMed] [Google Scholar]
- 11. Mrochen M, Kaemmerer M, Seiler T (2001) Clinical results of wavefront-guided laser in situ keratomileusis 3 months after surgery. J Cataract Refract Surg 27: 201–207. [DOI] [PubMed] [Google Scholar]
- 12. Du CX, Yang YB, Shen Y, Wang Y, Dougherty PJ (2006) Bilateral comparison of conventional versus topographic-guided customized ablation for myopic LASIK with the NIDEK EC-5000. J Refract Surg 22: 642–646. [DOI] [PubMed] [Google Scholar]
- 13. Vongthongsri A, Phusitphoykai N, Naripthapan P (2002) Comparison of wavefront-guided customized ablation vs. conventional ablation in laser in situ keratomileusis. J Refract Surg 18: S332–335. [DOI] [PubMed] [Google Scholar]
- 14. Phusitphoykai N, Tungsiripat T, Siriboonkoom J, Vongthongsri A (2003) Comparison of conventional versus wavefront-guided laser in situ keratomileusis in the same patient. J Refract Surg 19: S217–220. [DOI] [PubMed] [Google Scholar]
- 15. Fares U, Suleman H, Al-Aqaba MA, Otri AM, Said DG, et al. (2011) Efficacy, predictability, and safety of wavefront-guided refractive laser treatment: metaanalysis. J Cataract Refract Surg 37: 1465–1475. [DOI] [PubMed] [Google Scholar]
- 16. Zhang ZH, Jin HY, Suo Y, Patel SV, Montés-Micó R, et al. (2011) Femtosecond laser versus mechanical microkeratome laser in situ keratomileusis for myopia: Metaanalysis of randomized controlled trials. J Cataract Refract Surg 37: 2151–2159. [DOI] [PubMed] [Google Scholar]
- 17. Feng Y, Yu J, Wang Q (2011) Meta-analysis of wavefront-guided vs. wavefront-optimized LASIK for myopia. Optom Vis Sci 88: 1463–1469. [DOI] [PubMed] [Google Scholar]
- 18. Chen S, Feng Y, Stojanovic A, Jankov MR 2nd, Wang Q (2012) IntraLase femtosecond laser vs mechanical microkeratomes in LASIK for myopia: a systematic review and meta-analysis. J Refract Surg 28: 15–24. [DOI] [PubMed] [Google Scholar]
- 19. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, et al. (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17: 1–12. [DOI] [PubMed] [Google Scholar]
- 20. DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177–188. [DOI] [PubMed] [Google Scholar]
- 21. Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sterne JA, Egger M (2001) Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 54: 1046–1055. [DOI] [PubMed] [Google Scholar]
- 23. Mastropasqua L, Nubile M, Ciancaglini M, Toto L, Ballone E (2004) Prospective randomized comparison of wavefront-guided and conventional photorefractive keratectomy for myopia with the meditec MEL 70 laser. J Refract Surg 20: 422–431. [DOI] [PubMed] [Google Scholar]
- 24. Mastropasqua L, Toto L, Zuppardi E, Nubile M, Carpineto P, et al. (2006) Photorefractive keratectomy with aspheric profile of ablation versus conventional photorefractive keratectomy for myopia correction: six-month controlled clinical trial. J Cataract Refract Surg 32: 109–116. [DOI] [PubMed] [Google Scholar]
- 25. Mastropasqua L, Toto L, Zuppardi E, Nubile M, Carpineto P, et al. (2006) Zyoptix wavefront-guided versus standard photorefractive keratectomy (PRK) in low and moderate myopia: randomized controlled 6-month study. Eur J Ophthalmol 16: 219–228. [DOI] [PubMed] [Google Scholar]
- 26. Ghoreishi SM, Naderibeni A, Peyman A, Rismanchian A, Eslami F (2009) Aspheric profile versus wavefront-guided ablation photorefractive keratectomy for the correction of myopia using the Allegretto Eye Q. Eur J Ophthalmol. 19: 544–553. [DOI] [PubMed] [Google Scholar]
- 27. Falavarjani KG, Hashemi M, Modarres M, Sanjari MS, Darvish N, et al. (2011) Topography-Guided vs Wavefront-Optimized Surface Ablation for Myopia Using the WaveLight Platform: A Contralateral Eye Study. J Refract Surg 27: 13–17. [DOI] [PubMed] [Google Scholar]
- 28. Karimian F, Feizi S, Jafarinasab MR (2010) Conventional versus custom ablation in photorefractive keratectomy: randomized clinical trial. J Cataract Refract Surg 36: 637–643. [DOI] [PubMed] [Google Scholar]
- 29. Hashemi H, Nazari R, Amoozadeh J, Beheshtnejad AH, Jabbarvand M, et al. (2010) Comparison of postoperative higher-order aberrations and contrast sensitivity: tissue-saving versus conventional photorefractive keratectomy for low to moderate myopia. J Cataract Refract Surg 36: 1732–1740. [DOI] [PubMed] [Google Scholar]
- 30. Moshirfar M, Churgin DS, Betts BS, Hsu M, Sikder S, et al. (2011) Prospective, randomized, fellow eye comparison of WaveLight Allegretto Wave Eye-Q versus VISX CustomVueTM STAR S4 IRTM in photorefractive keratectomy: analysis of visual outcomes and higher-order aberrations. Clin Ophthalmol 5: 1185–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nassiri N, Safi S, Aghazade Amiri M, Sheibani K, Safi H, et al. (2011) Visual outcome and contrast sensitivity after photorefractive keratectomy in low to moderate myopia: wavefront-optimized versus conventional methods. J Cataract Refract Surg 37: 1858–1864. [DOI] [PubMed] [Google Scholar]
- 32. Mifflin MD, Hatch BB, Sikder S, Bell J, Kurz CJ, et al. (2012) Custom vs conventional PRK: a prospective, randomized, contralateral eye comparison of postoperative visual function. J Refract Surg 28: 127–132. [DOI] [PubMed] [Google Scholar]
- 33. Netto MV, Dupps W Jr, Wilson SE (2006) Wavefront-guided ablation: evidence for efficacy compared to traditional ablation. Am J Ophthalmol 141: 360–368. [DOI] [PubMed] [Google Scholar]
- 34. Oshika T, Klyce SD, Applegate RA, Howland HC, El Danasoury MA (1999) Comparison of corneal wavefront aberrations after photorefractive keratectomy and laser in situ keratomileusis. Am J Ophthalmol 127: 1–7. [DOI] [PubMed] [Google Scholar]
- 35. Miyai T, Miyata K, Nejima R, Honbo M, Minami K, et al. (2008) Comparison of laser in situ keratomileusis and photorefractive keratectomy results: long-term follow-up. J Cataract Refract Surg 34: 1527–1531. [DOI] [PubMed] [Google Scholar]
- 36. Kamiya K, Shimizu K, Ohmoto F (2009) Comparison of the changes in corneal biomechanical properties after photorefractive keratectomy and laser in situ keratomileusis. Cornea 28: 765–769. [DOI] [PubMed] [Google Scholar]
- 37. Yeh DL, Bushley DM, Kim T (2006) Treatment of traumatic LASIK flap dislocation and epithelial ingrowth with fibrin glue. Am J Ophthalmol 141: 960–962. [DOI] [PubMed] [Google Scholar]
- 38. Waring GO 3rd (2000) Standard graphs for reporting refractive surgery. J Refract Surg 16: 459–466. [PubMed] [Google Scholar]
- 39. Reinstein DZ, Waring GO 3rd (2009) Graphic reporting of outcomes of refractive surgery. J Refract Surg 25: 975–978. [DOI] [PubMed] [Google Scholar]
- 40. Dupps WJ Jr, Kohnen T, Mamalis N, Rosen ES, Koch DD, et al. (2011) Standardized graphs and terms for refractive surgery results. J Cataract Refract Surg 37: 1–3. [DOI] [PubMed] [Google Scholar]
- 41. Calvillo MP, McLaren JW, Hodge DO, Bourne WM (2004) Corneal reinnervation after LASIK: prospective 3-year longitudinal study. Invest Ophthalmol Vis Sci 45: 3991–3996. [DOI] [PubMed] [Google Scholar]
- 42. Rajan MS, Jaycock P, O’Brart D, Nystrom HH, Marshall J (2004) A long-term study of photorefractive keratectomy; 12-year follow-up. Ophthalmology 111: 1813–1824. [DOI] [PubMed] [Google Scholar]
- 43. Montés-Micó R, Cáliz A, Alió JL (2004) Wavefront analysis of higher order aberrations in dry eye patients. J Refract Surg 20: 243–247. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
(DOC)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.


