Abstract
Objective
The purpose of this study was to test the efficacy of two brief interventions for alcohol misuse in a sample of combat veterans of the wars in Iraq and Afghanistan.
Method
Participants were 68 combat veterans (91.2% male; 64.7% White, 27.9% Black) with a mean age of 32.31 years (SD = 8.84) who screened positive for hazardous drinking in a Veterans Affairs Medical Center primary care clinic using the Alcohol Use Disorders Identification Test. More than half of the sample (57.4%) met criteria for PTSD (based on the Clinician-Administered PTSD Scale). Eligible veterans who elected to participate completed a baseline assessment and were randomized to receive one of two interventions (personalized feedback delivered with or without a motivational interviewing counseling session). Both interventions included information on hazardous drinking, PTSD symptoms, depression, and coping. Follow up assessments were conducted at 6 weeks and 6 months post-intervention.
Results
Both conditions resulted in statistically significant reductions in quantity and frequency of alcohol use, as well as frequency of binge drinking. Within group effect sizes (d) were in the small to medium range (.34 to .55) for quantity and frequency of alcohol use. There were no condition by time interactions, suggesting that both interventions were similarly effective. PTSD and Non-PTSD veterans responded equally well to both interventions, but veterans with PTSD assigned to Feedback+MI reported greater reductions in weekly drinking at the 6-week follow up.
Conclusions
These findings suggest that brief interventions for alcohol misuse may be effective for reducing drinking, even in an OEF/OIF Veteran population with a high degree of PTSD.
Keywords: Alcohol misuse, brief interventions, veterans, PTSD
Substance abuse among military combat veterans has become an issue of increasing interest to researchers and clinicians, and one of considerable public health importance, given that over 2 million American military personnel have served in recent combat theatres (Department of Defense, 2010). Research on veterans of the recent conflicts in Iraq and Afghanistan (abbreviated OEF/OIF/OND for Operations Enduring Freedom, Iraqi Freedom, and New Dawn) has demonstrated rates of alcohol misuse in the range of 25 to 40% (Calhoun et al., 2008; Jacobson et al., 2008). There is, unfortunately, a very low rate of help-seeking for substance abuse and mental health concerns in this population. One study found that only 2.5% of service members who screened positive for alcohol misuse had received any substance abuse treatment services (Burnett-Zeigler et al., 2011). Drinking in this population is further complicated by high rates of posttraumatic stress disorder (PTSD; McDevitt-Murphy et al., 2010), which may contribute to coping-motivated drinking, a particularly hazardous pattern (Kuntsche, Knibbe, Gmel, & Engels, 2005). Thus it seems that brief, opportunistic interventions, offered as part of regular medical care might be warranted for this population. To date, no brief intervention trials using samples of OEF/OIF/OND veterans have been published.
Brief alcohol interventions
Brief alcohol interventions (BAI) hold promise for reducing substance abuse across an array of populations. BAIs have emerged as the treatment of choice for heavy-drinking college students (Carey, Scott-Sheldon, Carey & DeMartini, 2007) and have become an important clinical tool with adults in medical settings (Ballesteros, Duffy, Querejeta, Arino, & Gonzalez-Pinto, 2004). BAIs used with college students typically include two primary components: detailed personalized feedback (usually several pages of written material that summarize the consequences and risks associated with each individual’s alcohol use), and motivational interviewing (MI), a counseling style characterized by a non-judgmental stance that aims to increase participants’ motivation to make positive changes (Miller & Rollnick, 2012). BAIs in medical settings are typically shorter, and provide less detailed feedback (Ballesteros et al., 2004).
Given the high level of alcohol misuse among OEF/OIF/OND veterans and the low rate of help-seeking in this population, BAIs may be a particularly relevant type of intervention to explore. The goal of the present study was to develop and compare two brief alcohol interventions for combat veterans, a group with a high level of PTSD symptoms. The impact of PTSD on BAI efficacy has been explored in one prior study (Monahan, McDevitt-Murphy, Dennhardt, Skidmore, Martens, & Murphy, 2013). That study used a sample of college students and found that students who endorsed symptoms of PTSD were responsive to both clinician-administered (MI) and computer administered brief alcohol interventions, but that they showed a better response to the MI intervention with respect to alcohol-related consequences. It is possible that counselor-delivered interventions might be preferable to no-contact interventions for individuals with PTSD due to the high level of negative affect associated with PTSD and the emphasis on empathy in MI. Therefore, a secondary goal of the present study was to examine the role of PTSD as a moderator of treatment effects. In this study, the interventions included both general and personalized information about PTSD and depression symptoms and the ways that these symptoms might influence drinking, whereas the interventions in the Monahan et al study did not explicitly address these symptoms.
Method
Participants
Participants were veterans seeking healthcare at an urban Veterans’ Affairs Medical Center (VAMC) recruited primarily from a specialized primary care clinic specifically for OEF/OIF veterans on their first visit to the VAMC. Other participants were recruited via advertisements posted around the VAMC. Of those that were eligible, a total of 68 participants completed the baseline assessment and intervention and are included in the present analyses. Participants were mostly male (91.2%; n = 62), with a mean age of 32.31 years (SD = 8.84). Participants described themselves as White (64.7%; n = 44), Black or African-American (27.9%; n = 19), Asian (1.5%; n = 1), or multiethnic (5.9%; n = 4). With respect to marital status, 29.4% reported being single (n = 20), 20.6% reported not being married but in a relationship (n = 14), and 41.2% reported being married (n = 28). A majority of participants reported that they had completed 1 (61.8%; n = 42) or 2 (29.4%; n = 20) OEF/OIF combat deployments. On average, veterans reported spending a total of 14.93 months (SD = 8.57) in an OEF/OIF combat zone.
Measures
Alcohol Use Disorders Identification Test (AUDIT)
The AUDIT (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001) is a 10-item self-report instrument that assesses quantity and frequency of alcohol use, symptoms of alcohol dependence, and alcohol related consequences. Items are rated 0 to 4, with total AUDIT scores ranging from 0 to 40 and scores of 8 or higher indicating hazardous drinking (Babor et al., 2001). For the sake of brevity, veterans responding to posted advertisements were screened via phone with the AUDIT-C (Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998), which consists of the first 3 items of the AUDIT. The internal consistency reliability of the AUDIT in our sample was adequate at .69.
Clinician Administered PTSD Scale (CAPS)
The CAPS (Blake et al., 1995) is a clinical interview assessing the frequency and intensity of the 17 symptoms of PTSD based on DSM-IV-TR criteria. Interviewers rate the frequency and intensity of each PTSD symptom on separate 5-point scales ranging from 0 to 4. Using the most common diagnostic scoring rule, a symptom is considered present if it is coded with a frequency score of at least 1 and an intensity score of at least 2 (F1/I2 rule). The CAPS has shown good internal consistency reliability in a sample of combat veterans (Blake et al., 1995). A random set of CAPS interviews (n = 13) were selected for interrater reliability analyses. An excellent intraclass correlation (.99) was found for CAPS total severity (one-way random effects model, single measure; Shrout & Fleiss, 1979).
Timeline Follow Back (TLFB)
The TLFB (Sobell & Sobell, 1996) is calendar-based assessment method used to obtain a participant’s self-report of the number of standard drinks consumed on each day for the past 30 days. A number of variables reflecting the frequency and quantity of past month alcohol use may be derived. The TLFB has shown good psychometric properties in many prior studies (e.g., Carey, Carey, Maisto, & Henson et al., 2004).
Drinker Inventory of Consequences (DrInC)
The DrInC (Tonigan & Miller, 2002) is a 50-item self-report measure assessing adverse consequences related to alcohol abuse in five domains: Interpersonal, Physical, Social, Impulsive, and Intrapersonal. Each item includes a lifetime score where the participant can endorse “Yes” or “No” this has happened to me. Each item also includes a score for the frequency with which this event has occurred in the past three months, rated (0) “Never” to (3) “Daily or almost every day.” We modified the DrInC to refer to the “past six weeks” in the version that was administered at the follow-ups. The internal consistency reliabilities of the DrInC subscales in our sample ranged from .66 to .83. The DrInC demonstrated good reliability in the current sample (α = .93).
Procedure
Participants who screened positive on the AUDIT/AUDIT-C were invited to enroll in the clinical trial. Upon completion of the baseline assessment, participants were randomized to receive one of two single-session interventions (see Figure 1 for details). Both conditions included detailed personalized drinking feedback (PDF) packets. A list of the PDF components is provided in Table 1. In the Motivational Interviewing (MI) condition, PDF was administered in the context of a one-hour session where the clinician proceeded through the pages of the PDF packet and used the material to engage the veteran in a MI-style discussion about the content. The session concluded with the clinician querying the impact of this information and engaging the veteran in collaborative goal-setting. In the Feedback Only (FO) condition, participants were provided with the PDF, without a counseling session. Participants were provided with the folder of written materials and asked to read through it thoroughly and then left alone for 30 minutes, after which the research assistant returned and gave the veteran a chance to ask questions. A randomly selected subset of 20% of the MI session recordings (N = 7) were reviewed and rated with respect to intervention adherence. The raters were doctoral students in clinical psychology who had been trained in Motivational Interviewing but who were not involved with this project. Using an adherence rating form developed specifically for this project, ratings were assigned for each of 24 session components using a scale with 4 anchors: 0 (“did not do this”), 1 (“did it poorly”), 2 (“met expectations”), and 3 (“above expectations”). Eighty-eight percent of components were rated with scores of 2 or 3, indicating that clinicians administered the intervention consistently. These sessions were also rated with respect to competence in MI-specific skills and clinicians were rated at least “met expectations” on 88% of these 12 items.
Figure 1.
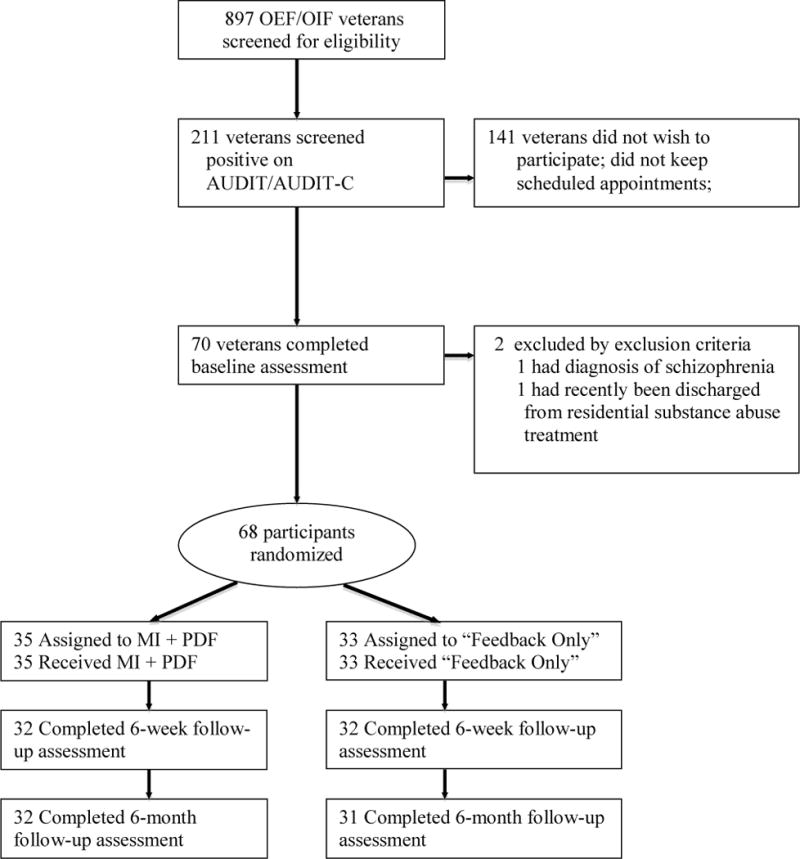
Flow chart illustrating recruitment, intervention assignment, and follow-up assessment.
Table 1.
Personalized Drinking Feedback components.
| Topic Area | Feedback component |
|---|---|
| Deployment-related Phenomena | Personalized feedback about combat experiences and post-deployment adjustment. |
| PTSD and Depression | General information about PTSD and depression Personalized feedback about veteran’s own symptoms |
| Coping | General information about coping styles Feedback about veteran’s own typical coping style |
| Substance Misuse | Normative feedback based on age- and gender-based norms Psychoeducation and personalized feedback about blood alcohol content (BAC) Binge drinking and risks associated with veteran’s own drinking Personal risk factors for alcohol dependence |
| PTSD-Alcohol Misuse | Information about the “vicious cycle” relationship between PTSD-related symptoms and alcohol misuse, included personalized information about the veteran’s motives for drinking. |
At the conclusion of both interventions, veterans completed a brief set of questionnaires and were asked to complete a comprehension check with 10 questions derived from the PDF. Participants scored an average of 92.6% on the comprehension check and there was no difference between the groups. Participants were compensated $50 for completing the baseline phase of the research project and were asked to return for follow-up assessments six weeks and six months later for which they were compensated $25 for each appointment. Follow-up rates were 94.1% (N = 64) at six weeks and 92.6% (N = 63) at six months and did not differ by condition.
Data Analysis Plan
Prior to conducting analyses, we corrected outliers and conducted transformations for variables with severely skewed or kurtotic distributions (Tabachnick & Fidell, 2007). A series of mixed-model repeated measures analyses were used to compare the two intervention conditions in terms of drinking-related outcomes, derived from the TLFB and the DrInC across three time points (baseline, 6-week follow-up, 6-month follow-up). An advantage of using a mixed-modeling approach is that these models can accommodate missing data resulting from missed appointments or treatment dropout by estimating parameters based on information available for any given individual with missing data.
Results
Baseline Comparison of Conditions
Eligible veterans who agreed to participate were compared to participants who did not participate on several variables (i.e., gender, age, race/ethnicity, relationship status, AUDIT score, and PTSD symptoms) and there were no differences on any of these variables. Veterans in the MI and FO conditions were compared on several baseline and demographic variables to assess whether the groups differed in any important ways prior to receiving the intervention. The groups did not differ on any of the TLFB, DrInC, or demographic variables. Group means and standard deviations are listed in Table 2. The groups also did not differ in terms of CAPS total severity (MI: M = 46.83, SD = 24.62; FO: M = 55.88, SD = 28.31; t(66) = −1.41, p = .16).
Table 2.
Mean scores across time on TLFB and DrInC variables.
| Variable | Baseline M (SD) | 6-Week Follow-Up M (SD) | 6-Month Follow-Up M (SD) | Within Groups Effect Size (d) 6-Week | Within Groups Effect Size (d) 6-Month |
|---|---|---|---|---|---|
| TLFB Variables | |||||
| Mean Drinks Per Week | |||||
| MI | 14.51 (17.13) | 9.53 (11.53) | 8.78 (11.63) | .34 | .39 |
| FO | 19.96 (25.33) | 11.26 (11.38) | 9.34 (10.34) | .44 | .55 |
| Mean Drinking Days Per Week | |||||
| MI | 2.40 (1.89) | 1.76 (1.80) | 1.97 (2.19) | .35 | .21 |
| FO | 2.84 (2.33) | 2.05 (1.70) | 2.15 (2.03) | .39 | .32 |
| Past month binge days | |||||
| MI | 4.54 (6.08) | 3.72 (5.46) | 2.97 (5.26) | .14 | .28 |
| FO | 6.85 (8.77) | 3.91 (4.66) | 2.77 (4.05) | .42 | .60 |
| Drinks Per Drinking Day | |||||
| MI | 5.74 (3.28) | 5.14 (3.73) | 4.16 (2.37) | .17 | .55 |
| FO | 6.44 (4.18) | 5.84 (3.74) | 5.13 (3.24) | .15 | .35 |
| DrInC Variables | |||||
| Recent Consequences | |||||
| MI | 6.89 (6.16) | 5.78 (7.61) | 4.83 (7.19) | .16 | .31 |
| FO | 8.33 (7.21) | 7.81 (7.63) | 5.26 (6.94) | .07 | .43 |
| Physical | |||||
| MI | 1.71 (1.56) | 1.53 (1.74) | 1.24 (1.72) | .11 | .29 |
| FO | 2.03 (1.69) | 1.65 (1.82) | 1.23 (1.45) | .22 | .51 |
| Interpersonal | |||||
| MI | 1.46 (1.40) | 1.06 (1.95) | 1.14 (1.85) | .24 | .20 |
| FO | 1.70 (1.81) | 1.87 (2.05) | 1.16 (2.07) | −.09 | .28 |
| Intrapersonal | |||||
| MI | 1.14 (1.65) | .94 (1.63) | .83 (1.61) | .12 | .19 |
| FO | 1.42 (1.98) | 1.48 (2.03) | .90 (1.92) | −.03 | .27 |
| Social Responsibility | |||||
| MI | .69 (.96) | .34 (.83) | .62 (1.37) | .39 | .06 |
| FO | .88 (1.34) | .68 (1.17) | .52 (1.36) | .16 | .27 |
| Impulse Control | |||||
| MI | 1.89 (1.88) | 1.81 (2.10) | 1.21 (2.11) | .04 | .34 |
| FO | 2.24 (1.90) | 2.10 (2.02) | 1.81 (2.43) | .07 | .20 |
Note: Means and standard deviations are based on values with outliers corrected. MI = Brief motivational interview. FO = Feedback only. Baseline sample sizes were MI (N = 35) and FO (N = 33). Drinks per drinking day variable was only computed for participants who reported any past month drinking, resulting in a smaller baseline sample size of MI (N = 33) and FO (N = 31). Sample sizes vary slightly at follow-up time points due to missing data.
Alcohol Use Outcomes
Separate 2 (condition) × 3 (time) mixed-model repeated measures analyses were conducted for quantity and frequency of alcohol consumption. Means and standard deviations for each treatment group on each alcohol use variable are presented in Table 2. A statistically significant main effect for time emerged for quantity (F(2, 119.69) = 8.95, p < .001) such that participants across both conditions reported a significant reduction in the number of drinks per week from baseline to 6 weeks, with the reduction maintained at 6-months. Likewise for frequency, there was a significant main effect for time with a reduction in the number of drinking days per week from baseline to 6 weeks, maintained at 6 months (F(2, 118.04) = 5.36, p = .006). Statistically significant reductions in the number of binge-drinking days per month, defined as 5 (men) or 4 (women) or more drinks per drinking occasion, also emerged across conditions from baseline to 6-week follow-up (F(2, 121.51) = 8.08, p = .001) and these reductions were maintained at 6 months. Furthermore veterans reported drinking fewer drinks per drinking day from baseline to 6 months (F(2, 109.23) = 3.25, p = .04). There were no statistically significant condition × time interactions.
A series of 2 (condition) × 3 (time) mixed-model repeated measures analyses were also conducted using each of the DrInC scales as dependent variables. Means and standard deviations for each DrInC scale are presented in Table 2. Statistically significant main effects for time resulted for several scales, including recent consequences (F(2, 119.88) = 6.24, p = .003), physical consequences (F(2, 124.34) = 3.84, p = .02), interpersonal consequences (F(2, 120.87) = 3.45, p = .04), impulse control consequences (F(2, 118.64) = 4.07, p = .02) and social responsibility consequences (F(2, 119.46) = 3.00, p = .05). There were no statistically significant condition × time interactions.
On the AUDIT administered at 6-months post-intervention, 40.7% of the participants for whom complete data were available (n = 59) no longer scored in the positive range. When examined separately by condition, fourteen of the 29 (48.3%) MI participants and 10 of the 30 (33.3%) FO participants screened negative. A chi-square test comparing these rates was not significant (χ2(1) = 1.36, p = .24).
Moderation Analyses: PTSD
We explored whether baseline PTSD status moderated treatment effects. In all 57.4% of the sample met criteria for PTSD at baseline and the rate did not differ by condition. This included 18 (51.4%) MI participants and 21 (63.6%) FO participants (χ2(1) = 1.04, p = .31). Table 3 shows means and standard deviations for each group by PTSD status and condition. Contrasts comparing MI participants with PTSD, MI participants without PTSD, FO participants with PTSD, and FO participants without PTSD on baseline TLFB variables did not reveal any statistically significant differences between these groups. Effect sizes for these comparisons were generally small to medium (absolute Cohen’s d’s range from .03 to .67)1.
Table 3.
Mean group scores on TLFB variables by baseline PTSD diagnostic status.
| MI | FO | |||
|---|---|---|---|---|
| PTSD+ (N = 18) M (SD) |
PTSD− (N = 17) M (SD) |
PTSD+ (N = 21) M (SD) |
PTSD− (N = 12) M (SD) |
|
| Mean Drinks Per Week | ||||
| Baseline | 11.52 (14.51) | 17.68 (19.47) | 23.93 (29.62) | 13.02 (13.72) |
| 6-Week Follow-Upa | 6.63 (11.26) | 12.42 (11.39) | 13.48 (13.37) | 7.56 (5.68) |
| 6-Month Follow-Upb | 10.86 (14.43) | 6.42 (7.09) | 9.28 (11.87) | 9.44 (7.26) |
| Mean Drinking Days Per Week | ||||
| Baseline | 1.98 (1.80) | 2.83 (1.94) | 3.06 (2.44) | 2.45 (2.16) |
| 6-Week Follow-Upa | 1.41 (1.88) | 2.11 (1.71) | 2.20 (1.84) | 1.81 (1.47) |
| 6-Month Follow-Upb | 2.45 (2.66) | 1.41 (1.37) | 2.02 (2.19) | 2.39 (1.78) |
| Total Binge Days | ||||
| Baseline | 3.27 (3.83) | 5.88 (7.70) | 8.33 (9.98) | 4.25 (5.58) |
| 6-Week Follow-Upa | 2.44 (4.34) | 5.00 (6.26) | 4.60 (5.49) | 2.75 (2.60) |
| 6-Month Follow-Upb | 3.88 (6.90) | 1.93 (2.19) | 2.75 (4.46) | 2.82 (3.37) |
| Drinks Per Drinking Day | ||||
| Baselinec | 5.21 (3.34) | 6.23 (3.25) | 7.05 (4.49) | 5.32 (3.45) |
| 6-Week Follow-Upd | 3.56 (2.18) | 6.63 (4.30) | 6.31 (3.95) | 4.95 (3.32) |
| 6-Month Follow-Upe | 3.38 (2.65) | 4.56 (2.00) | 5.16 (3.29) | 5.08 (3.32) |
Note: Means and standard deviations are based on values with outliers corrected. MI = Brief motivational interview. FO = Feedback only.
Due to missing data, group sample sizes are MI/PTSD+ (N = 16), MI/PTSD− (N = 16), and FO/PTSD+ (N = 20).
Due to missing data, group sample sizes are MI/PTSD+ (N = 17), MI/PTSD− (N = 15), FO/PTSD+ (N = 20) and FO/PTSD− (N = 11).
Because some Veterans reported no past month drinking at the baseline assessment, group sample sizes are MI/PTSD+ (N = 16), MI/PTSD− (N = 17), FO/PTSD+ (N = 20) and FO/PTSD− (N = 11).
Because some Veterans reported no past month drinking and due to missing data, group sample sizes are MI/PTSD+ (N = 15), MI/PTSD− (N = 16), FO/PTSD+ (N = 19) and FO/PTSD− (N = 10).
Because some Veterans reported no past month drinking, group sample sizes are MI/PTSD+ (N = 14), MI/PTSD− (N = 11), FO/PTSD+ (N = 16), and FO/PTSD− (N = 10).
A series of separate 2 (condition) × 2 (PTSD diagnostic status) × 3 (time) mixed-model repeated measures analyses were conducted using each of the TLFB variables to explore whether PTSD diagnosis moderated the effect of the intervention. There was a statistically significant condition × PTSD × time interaction for alcohol quantity (F(2, 115.63) = 5.89, p = .004). In follow-up analyses, pairwise comparisons revealed that at 6 weeks, PTSD veterans who received MI made larger reductions in the number of drinks per week than did PTSD veterans who received FO (F(1, 110.67) = 5.11, p = .03). Additional pairwise comparisons did not reveal any significant group differences as a function of PTSD at any other time point. A statistically significant condition × PTSD × time interaction (F(1, 114.45) = 4.81, p = .01) also emerged for drinking frequency, but follow-up analyses did not show any significant differences between the MI and FO conditions as a function of PTSD diagnostic status at any time point. No statistically significant condition × PTSD × time interactions were found for binge-drinking days or drinks per drinking day, nor for any analysis using the DrInC.
Discussion
We studied two brief interventions in a sample of OEF/OIF combat veterans and found that both were associated with significant improvements on several aspects of alcohol use and misuse. Both groups reduced their weekly drinking to a mean level that is consistent with federal recommendations for moderate drinking (http://health.gov/dietaryguidelines/) and participants maintained those improvements through six months post-intervention. One important outcome variable was screening status on the AUDIT, a well-validated screening measure for hazardous drinking on which participants screened positive to qualify for the study. The proportion of veterans screening positive on the AUDIT administered at the 6-month follow up point was 60%, reflecting a 40% reduction. This is noteworthy from a public health perspective.
These findings support the use of feedback-based brief interventions for this population and suggest that a brief intervention administered with minimal clinician involvement may be sufficient to evoke clinically meaningful reductions in alcohol use that persist over a six-month follow up period. The PDF packets provided to participants in this study were lengthy and addressed several aspects of alcohol use/misuse as well as other facets of the post-deployment readjustment experience and symptoms of PTSD and depression. The fact that the feedback-only intervention performed similarly to the MI condition was unexpected in this clinically complicated sample (i.e., social and physical health stressors, high base rate of PTSD), although studies with heavy drinking college students have often shown equivalent effects between MI and feedback-only (Murphy et al., 2004; White, 2006). In contrast, one study has examined the incremental efficacy of web-delivered personalized drinking feedback for veterans (Cucciare, Weingardt, Ghaus, Boden, & Frayne, 2013) and did not find that it significantly enhanced the efficacy of treatment as usual (brief physician advice). The personalized feedback documents used in the present study, however, were substantially more detailed than those used in the Cucciare et al. study. Personalized feedback holds promise as a potentially easily-disseminated intervention within the VAMC system. One possible application of this technology would be to encourage veterans to self-administer an assessment at a portal in a VAMC clinic, and then to receive PDF electronically, immediately prior to a primary care appointment where a clinician could provide follow up during routine clinical care.
Although we did not find a statistically significant overall advantage for the counselor-delivered brief motivational intervention, it is noteworthy that a) participants in the feedback-only intervention continued to drink at the binge level (mean of approximately 5 drinks per drinking day) while those in the MI condition were drinking more moderately (mean of approximately 4 drinks per drinking day), and b) there was a difference of 15 percentage points in the rate of positive AUDIT screens between the groups, with nearly half of participants in the MI condition, and one third of participants in the FO condition, screening negative at follow-up. This difference was not significant, but power to detect significant effects was hindered by our small sample and this should be investigated in future research. Additionally, the MI intervention was associated with greater drinking reductions for participants with PTSD at the initial (6 week) follow-up point. It is unclear why PTSD veterans might have responded more favorably to the MI based intervention, but one hypothesis for future investigation is that the empathic listening displayed by the MI counselors had the effect of defusing the PTSD veterans’ negative affect in session, allowing them to be more open to the content of the intervention. It is also possible that the counselor-administered MI enhanced retention and cognitive processing of feedback material, which may have enhanced its potency (Jouriles, et al., 2010), and perhaps this was especially beneficial for veterans with PTSD who may experience symptoms that interfere with concentration or memory.
Implications for PTSD veterans
These findings suggest that although veterans with PTSD might drink for coping reasons, which are typically associated with more severe drinking (Kuntsche et al., 2005), they are no less responsive to a brief intervention, particularly one that specifically addresses drinking to cope, and provides information about other coping strategies. For the duration of the follow up interval, PTSD veterans maintained their reductions in drinking as effectively as those without PTSD. An important question for future research is whether PTSD veterans show the same durability of effects over a longer-term follow up interval. It is important to highlight that both interventions in the present study included material relevant to PTSD symptoms and coping. It is not clear how veterans with PTSD would respond to a traditional BAI that did not include material about PTSD. Substance misuse is often a barrier to engagement in PTSD treatment and the present findings suggest that a brief intervention could potentially be a prelude to PTSD-specific treatment.
Strengths and limitations
One strength of this study was the use of combat veterans, a population for whom the development of effective BAIs is of critical importance. Another strength of this study was that we thoroughly assessed PTSD, a prevalent comorbid condition in this population, and we addressed PTSD explicitly in the intervention due to the fact that PTSD symptoms likely contribute to drinking. A limitation of our design was that we did not include a no-treatment or assessment-only control condition, which limits our ability to draw conclusions about the efficacy of both interventions. Additionally, our small sample impeded our ability to detect small effects.
In conclusion, these findings suggest that brief interventions may be effective for reducing hazardous drinking among combat veterans, even those with comorbid PTSD. This is encouraging news, given that combat veterans presenting to VAMC clinics tend to have multiple comorbid physical and psychological health conditions. The VA system has been promoting the use of universal screening and brief advice for hazardous drinking. These findings suggest that including personalized feedback might improve the efficacy of those efforts.
Acknowledgments
This work was conducted with support from the National Institute of Alcohol Abuse and Alcoholism (Grant # K23AA016120 to Meghan McDevitt-Murphy), and with support from the Office of Research and Development, Memphis Veterans’ Affairs Medical Center and the Tennessee Board of Regents, through the Center for Applied Psychological Research.
Footnotes
Additional detail about these contrast results is available from the first author.
Contributor Information
Meghan E. McDevitt-Murphy, The University of Memphis, Memphis Veterans’ Affairs Medical Center
James G. Murphy, The University of Memphis, Memphis Veterans’ Affairs Medical Center
Joah L. Williams, The University of Memphis, Memphis Veterans’ Affairs Medical Center
Christopher J. Monahan, The University of Memphis, Memphis Veterans’ Affairs Medical Center
Katherine L. Bracken-Minor, The University of Memphis, Memphis Veterans’ Affairs Medical Center
Jordan A. Fields, The University of Memphis, Memphis Veterans’ Affairs Medical Center
References
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for use in primary care. 2. World Health Organisation; Geneva: 2001. [Google Scholar]
- Ballesteros J, Duffy JC, Querejeta I, Arino J, Gonzalez-Pinto A. Efficacy of brief interventions for hazardous drinkers in primary care: Systematic review and meta-analyses. Alcoholism: Clinical and Experimental Research. 2004;28:608–618. doi: 10.1097/01.ALC.0000122106.84718.67. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Burnett-Zeigler I, Ilgen M, Valenstein M, Zivin K, Gorman L, Blow A, Duffy S, Chermack S. Prevalence and correlates of alcohol misuse among returning Afghanistan and Iraq veterans. Addictive Behaviors. 2011;36:801–806. doi: 10.1016/j.addbeh.2010.12.032. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonnell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief intervention screening test for problem drinking. Archives of Internal Medicine. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Calhoun PS, Elter JR, Jones ER, Kudler H, Straits-Troster K. Hazardous alcohol use and receipt of risk-reduction counseling among veterans of the wars in Iraq and Afghanistan. Journal of Clinical Psychiatry. 2008;69:1686–1693. doi: 10.4088/JCP.v69n1103. [DOI] [PubMed] [Google Scholar]
- Carey KB, Carey MP, Maisto SA, Henson JM. Temporal stability of the timeline followback interview for alcohol and drug use with psychiatric outpatients. Journal of Studies on Alcohol and Drugs. 2004;65:774–781. doi: 10.15288/jsa.2004.65.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: a meta-analytic review. Addictive Behaviors. 2007;32:2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucciare MA, Weingardt KR, Ghaus S, Boden MT, Frayne SM. A randomized controlled trial of a web-delivered brief alcohol intervention in veterans affairs primary care. Journal of Studies on Alcohol and Drugs. 2013;74:428–436. doi: 10.15288/jsad.2013.74.428. [DOI] [PubMed] [Google Scholar]
- Department of Defense. The impacts of deployment of deployed members of the armed forces on their dependent children. 2010 Retrieved from http://www.militaryhomefront.dod.mil/12038/ProjectDocuments/MilitaryHOMEFRONT/Reports/Report_to_Congress_on_Impact_of_Deployment_on_Military_Children.pdf.
- Dietary Guidelines for Americans. 2010 Retrieved October 4, 2012, from http://health.gov/dietaryguidelines/
- Jacobsen IG, Ryan MA, Hooper TI, Smith TC, Amoroso PJ, Boyko EJ, Bell NS. Alcohol use and alcohol related-problems before and after military combat deployment. Journal of the American Medical Association. 2008;300:663–675. doi: 10.1001/jama.300.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jouriles EN, Brown AS, Rosenfield D, McDonald R, Croft K, Leahy MM, Walters ST. Improving effectiveness of computer-delivered personalized drinking feedback interventions for college students. Psychology of Addictive Behaviors. 2010;24:592–599. doi: 10.1037/a0020830. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clinical Psychology Review. 2005;25:841–861. doi: 10.1016/j.cpr.2005.06.002. doi:1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Williams JL, Bracken KL, Fields JA, Monahan CJ, Murphy JG. PTSD symptoms, hazardous drinking, and health functioning among U.S.OEF/OIF veterans presenting to primary care. Journal of Traumatic Stress. 2010;23:108–111. doi: 10.1002/jts.20482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 3. New York, NY US: Guilford Press; 2012. [Google Scholar]
- Monahan CJ, McDevitt-Murphy ME, Dennhardt AA, Skidmore JR, Martens MP, Murphy JG. The impact of PTSD symptoms on the efficacy of alcohol interventions for heavy drinking college students. Addictive Behaviors. 2013;38:1719–1725. doi: 10.1016/j.addbeh.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Benson T, Vuchinich RE, Deskins M, Eakin D, Flood AM, McDevitt-Murphy M, Torrealday O. A comparison of personalized feedback for college student drinkers delivered with and without a counseling session. Journal of Studies on Alcohol. 2004;65:200–204. doi: 10.15288/jsa.2004.65.200. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback user’s guide: A calendar method for assessing alcohol and drug use. Toronto, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5. Boston, MA: Allyn and Bacon; 2006. [Google Scholar]
- White HR. Reduction of alcohol-related harm on U.S. college campuses: The use of personal feedback interventions. International Journal of Drug Policy. 2006;17:310–319. doi: 10.1016/j.drugpo.2006.02.006. [DOI] [Google Scholar]


