Abstract
Objectives
To explore associations of body mass index (BMI) and waist circumference (WC) with disability among the Chinese oldest old.
Design and Methods
5495 oldest old in the sixth wave of Chinese Longitudinal Healthy Longevity Study conducted in 2011 were included in this study. Disability was assessed by Activities of Daily Living (ADL); height and weight for BMI and WC were measured; information including socio-demographics, lifestyles and health status was collected.
Results
Generalized additive models analysis showed that the association of BMI/WC with ADL disability was non-linear. Among the males, logistic regression results supported a ‘J‘ shape association between ADL disability with BMI/WC--the highest tertile group in BMI or WC was significantly associated with an increased risk of ADL disability: odds ratio 1.78 (95% confidence interval (CI): 1.26-2.52) for BMI and 2.01 (95% CI: 1.44-2.82) for WC. Among females, an inverse ‘J’ shape association was found, only the lowest tertile group before the cutoff point had an increased risk of ADL disability: odds ratio 1.42 (95%CI: 1.02-1.97) for BMI and 1.47 (95% CI:1.06-2.04) for WC.
Conclusions
Associations of BMI and WC with ADL disability are significant even in the oldest old, but differ between the genders.
Keywords: Gender, Association, Body mass index, Waist circumference, Disability, Oldest old
Introduction
Disability has become an important health problem for many developed countries due to decreasing mortality, improvement in medical care and ageing, and the World Health Organization estimated that 650 million people live with a disability or functional impairment (1). Activity of daily living (ADL) disability represents one of the most severe stages of disability. Therefore, identifying the determinants of ADL disability is crucial for prevention and control of disability.
Body mass index (BMI) and waist circumference (WC) are often used as indicators of weight status or nutritional health status; BMI is usually used as a measure of general fatness, and WC is a reflection of abdominal fat. In recent years, obesity, assessed by BMI or WC, has been highlighted by researchers because of its possible relationship with disability as well as its high prevalence among the population. As a whole, many prospective or cross-sectional studies have demonstrated the associations between obesity and ADL disability; however, it is not yet clear that which measure, BMI, WC, or both, are significantly associated with ADL limitations. Among recent studies, especially when gender was considered, the association of BMI/WC with ADL disability was very inconsistent and controversial. Some researchers have found BMI associated with ADL impairment in older adults (2-5). Among studies that focused on both BMI and WC simultaneously, some found that WC was better predictive marker of self-reported ADL disability in both gender or only in women (6,7), some researchers supported the combination use of WC and BMI in assessing the risk of disability in older adults8; some others found that both BMI and WC were related with ADL(8,9) or just in the females.7 Some concluded that both BMI and WC were unrelated to ADL(10) or only related with specific ADL items of disability (11). Second, the association of underweight with disability was not clear and not fully studied (4,12), and even fewer studies focused on the association of underweight with ADL disability. Third, little is known regarding whether the association found in younger elderly is suitable for the oldest old. Except for one study (N=380) conducted in Sweden (13), the large majority of previous studies have only evaluated younger elderly or mixed-age groups. Fourth, few studies have been carried out in developing countries.
For the reasons stated above, the objective of this study was to address these knowledge gaps through analysis of the association of BMI and WC with ADL disability among a group of Chinese oldest old with a relatively large sample size.
Methods
Study subjects
Participants in this study were from the sixth wave of the Chinese Longitudinal Healthy Longevity Survey (CLHLS) conducted in 2011. The CLHLS was firstly conducted since 1998, and then followed in 2000, 2002, 2005, 2008 and 2011 in randomly selected half of the counties and cities in 22 provinces of China, was the first national longitudinal survey on determinants of health aging and has the largest sample of the oldest-old individuals in China. Details of the sample design have been described elsewhere and data quality was reported to be generally good (14, 15). Briefly, all centenarians were invited to be interviewed, one nearby octogenarian and one nonagenarian of pre-designated age and sex were randomly chosen to be interviewed, which ensured comparable numbers of randomly selected male and female oldest old aged 80 years and over. We used the wave of 2011 because it was the first year that included measurement of WC. The study was approved by the ethics committee of Peking University, and written informed consent was obtained from all participants (or their proxies).
Disability measurement
Disability was assessed using the Katz Activities of Daily living Scale (16). Interviewers asked participants if they experienced difficulty or needed assistance in performing the following activities: bathing, dressing, toileting, transfers, continence and eating. ADL disability was dichotomized as having difficulty or no difficulty in performing any one or more of the ADL tasks above.
Anthropometric measures
Weight and height were measured using standard methods rounded to the nearest integer. BMI was computed as weight in kilograms divided by height in meters squared. WC was measured using a non-stretchable tape in centimeters at a level between the lowest rib and Iliac crest (Ilium) with the subjects lightly clothed.
Description of covariates
Covariates included socio-demographic information (age, ethnicity, educational levels, marital status), behaviors and lifestyles (living arrangement, smoking, drinking, physical activities, leisure activities), resilience, and health status, which included self-rated health status, cognitive function, systolic blood pressure (SBP), diastolic blood pressure (DBP), the prevalence of heart diseases, stroke, respiratory disease, cancer and bone joint disease. If the participant was unable to answer, questions (except those used to measure cognitive function) could be answered by one adult family member who was most familiar with the living status of the participant. Education was defined as ‘no’ if the subject had no education whatsoever, and as ‘yes’ if the subject received any formal education at any time. Marital status was categorized as ‘yes’ if the subject was currently married, and ‘no’ if they were divorced, widowed or never married. Living arrangement was categorized as living alone or living with others. Physical activity was defined as ‘yes’ or ‘no’ by the question ‘Do you often do physical activities, including walking, playing ball, running and Qigong, etc.’. Leisure activities were assessed by the question, ”How often do you do the following leisure activities: outdoor activities, growing flowers, reading, raising pets, playing cards, watching TV, listening to the radio, and taking part in social activities.” Each kind of leisure activity was measured on a scale from 1 to 5, representing always, often, sometimes, rarely, or never. We dichotomized responses for each kind of leisure activity into two categories: ‘yes’ if the answer was “always” or “often”, and ‘no’ if the answer was sometimes, rarely or never. A positive response to any of the above leisure activities was coded as a positive value for the leisure activity variable (17). Resilience was assessed by a simplified resilience score (SRS) emphasizing coping and adjusting among the elderly, described in detail in our previous study (18), The SRS is based on seven questions related to resilience in our survey, which reflect personal tenacity, optimism, coping with negative mood, secure relationship and self-control, and the total SRS ranges from 0 to 22, with the higher scores reflecting greater resilience, and higher resilience was defined as a score >=16 (18). Cognitive function was measured by the widely used Mini-Mental State Examination (19). MMSE scores ranged from 0-30, with higher scores indicating better cognition. In this study, cognitive impairment was defined as a cut-off score of <18, as defined in a prior study that focused on the Chinese oldest old (17), most of whom were illiterate or not well educated. Physical examinations were also conducted by medical personnel. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured twice, and the mean values were used for our analyses.
Statistical analysis
All statistical analyses were conducted separately on male and female sub-samples. Subject characteristics were compared by analysis of variance for continuous variables and by chi-square tests for dichotomous variables between the subjects with and without ADL disability. Generalized additive models (GAMs) were employed to explore the shapes of the association of BMI and WC with ADL disability. The GAM is an extension of the generalized linear model in that one or more predictors may be specified using spline smooth function f(x) .The significant advantage of GAM over generalized linear model is the flexibility derived from the data-driven shape of the f(x) function, which avoid assumptions about the shape of the independent effect on the dependent variable. We estimated the shapes of their association, adjusting for BMI and WC with each other in addition to age.
Based on the results from the sex-specific GAM analysis, we could identify the cut-points of ADL disability risk for BMI and WC. Subjects were divided according to tertiles of their BMI and WC, respectively, before and after the cut-point. The three low groups were designated the low, lower and lowest for those subjects whose BMI or WC values were before the cut-off points; the three high groups were designated high, higher and highest for those subjects whose BMI or WC were over the cut-off points. Logistic regressions were used to analyze the associations of these groups with dependent variable ADL dichotomized as any disability or no disability; Odds ratio (OR) and 95% confidence interval (95%CI) were also calculated.
Models were all first run without adjustment, and then three adjusted logistic regression models were fit; adjusted for socio-demographic variables,(model 1); then adjusted additionally for ‘behaviors and lifestyles’ variables and resilience (model 2); and finally models were further adjusted for health status variables (model3).
All statistical analyses were performed with SAS, version 9.2 (SAS Institute Inc., Cary, NC, US). P<0.05 was considered statistically significant, and all P values were two-sided.
Results
Among the 9765 participants in the 2011 wave of CLHLS, 6530 were aged 80 years and over. We excluded subjects with missing data on key variables, such as ADL, weight, height and WC, so the final sample size was 5495 participants that included 2303 males and 3192 females. As shown in Table 1, the subjects with ADL disability were more likely to be older, illiterate, Han nationality and less likely to be married, they usually reported less physical activities and leisure activities, in addition to poor self-rated health, resilience and cognitive function. They had a higher prevalence of chronic diseases. Those with ADL disability usually had higher waist circumference among the males, but relative lower waist circumference among the females.
Table1.
Characteristic of Subjects by Absence or Presence of ADL Disability, Chinese Longitudinal Healthy Longevity Survey, China, 2011 a, b
| Male |
Female |
|||
|---|---|---|---|---|
| No Disability | ADL Disability | No Disability | ADL Disability | |
| N | 1674 | 629 | 1965 | 1227 |
| Age (years) | 89.3 (6.4) | 93.4(6.9) * | 91.6 (7.6) | 97.0 (7.4)* |
| Age groups* (years) | ||||
| 80-89 | 977 (58.4) | 208 (33.1) | 917 (46.7) | 236 (19.23) |
| 90-99 | 576 (34.4) | 296 (47.1) | 676 (34.4) | 459 (37.41) |
| 100+ | 121 (7.2) | 125 (19.9) | 372 (18.9) | 532 (43.36) |
| Illiterate | 593 (35.4) | 254 (40.4)* | 1489 (75.8) | 1045 (85.17)* |
| Han nationality | 1448 (86.5) | 583 (92.7)* | 1641 (83.5) | 1105 (90.06)* |
| Married | 735 (43.9) | 219 (34.8)* | 278 (14.2) | 83 (6.76)* |
| Living alone | 326 (19.5) | 56 (8.9)* | 479 (24.4) | 117 (9.54)* |
| Smoking | 515 (30.8) | 133 (21.1)** | 105 (5.3) | 66 (5.4) |
| Drinking | 452 (27.0) | 113 (18.0)** | 182 (9.3) | 93 (7.6) |
| Physical activity | 693 (41.4) | 136 (21.6)* | 615 (31.3) | 152 (12.4)* |
| Leisure Activities | 1537 (91.8) | 390 (62.0)* | 1661 (84.5) | 552 (44.9)* |
| Good Self-rated Health | 808 (48.3) | 210 (33.4)** | 868 (44.2) | 405 (33.0)** |
| Higher Resilience | 938(56.0) | 239 (38.0)** | 853(43.4) | 323 (26.3)** |
| Cognitive impairment | 1518 (90.9) | 599 (95.4)** | 1864 (94.9) | 1203 (98.1)** |
| Heart disease | 271 (16.2) | 151 (24.0)** | 299 (15.2) | 223 (18.2)* |
| Stroke | 196 (11.7) | 138 (21.9)** | 184 (9.4) | 195 (15.9)** |
| Respiratory Disease | 288 (17.2) | 153 (24.3) ** | 235 (11.9) | 184 (15.0) * |
| Joint Disease | 217 (12.9) | 108 (17.2)** | 318 (16.2) | 203 (16.5) |
| Cancer | 96 (5.7) | 50 (8.0) | 84 (4.3) | 79 (6.4) ** |
| SBP (mmHg) | 136.9 (20.5) | 131.5 (18.9)* | 140.2 (22.3) | 135.2 (22.7)* |
| DBP (mmHg) | 79.9 (12.2 | 79.1 (11.9) | 80.5 (12.9) | 79.9 (13.2) |
| WC (centimeter) | 81.4 (10.2) | 82.46 (12.0)* | 79.3 (11.4) | 76.7 (11.9)* |
| BMI (Kg/m2) | 20.6 (3.4) | 20.8 (3. 9) | 20.2 (3.9) | 19.4 (3.9)* |
Abbreviations: ADL, activities of daily living; BMI, body mass index; DBP, diastolic blood pressure; SBP, systolic blood pressure; SD, standard deviation; WC, waist circumference.
P<0.05;
P<0.05;
P<0.01
Data listed as n (%) for dichotomous variables, including age groups, illiterate, Han nationality, married status, living alone, smoking, drinking, physical activities, leisure activities, good self-rated health, higher resilience, cognitive impairment, heart disease, stroke, respiratory disease, joint disease, cancer, were tested using chi-square test. Data listed as mean (SD) for continuous variables, including age, SBP, DBP, WC and BMI, were tested for differences between the two groups using t-test.
There were two aspects of the GAM analyses, a linear regression model analysis and a smoothing model analysis. By linear regression analyses of the male data, there was no statistically significant linear association of BMI with ADL disability (P >0.05), but significant association of WC with ADL disability (P<0.05). Deviance in the smoothing model analysis showed that the spline of BMI and WC were all significantly related to ADL disability (P<0.05); this indicated that a non-linear association existed between them. From Figure 1 (males), the cut-points of BMI and WC for risk of ADL disability were 18.5 kg/m2 and 75 centimeters respectively. For women, there were non-linear associations for BMI and WC with ADL disability (P<0.05), as Figure 2 (females) shown, the cut-points of BMI and WC for the risk of ADL disability were 20 kg/m2 and 80 centimeters respectively.
Figure1.
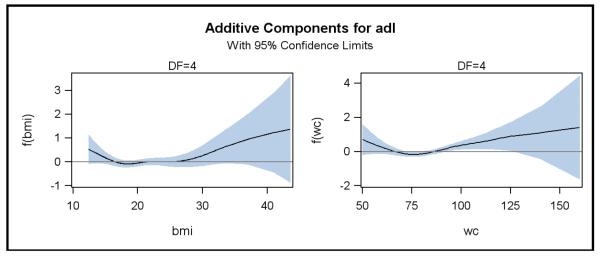
Associations of BMI and WC with ADL disability for the males oldest old, Chinese Longitudinal Healthy Longevity Survey, China, 2011
Abbreviations: ADL, activities of daily living; BMI, body mass index; WC, waist circumference. The lines depict the estimated function of BMI (left) and WC (right), respectively, for risk of ADL disability among the males oldest old, in the Chinese Longitudinal Healthy Longevity Survey, China, 2011, and the shaded area indicates the 95% confidence intervals.
Figure2.
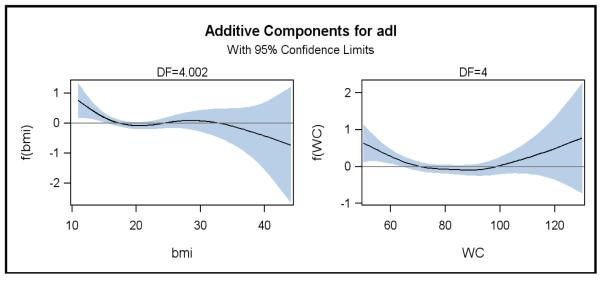
Associations of BMI and WC with ADL disability for the females oldest old, Chinese Longitudinal Healthy Longevity Survey, China, 2011.
Abbreviations: ADL, activities of daily living; BMI, body mass index; WC, waist circumference. The lines depict the estimated function of BMI (left) and WC (right), respectively, for risk of ADL disability among the females, in the Chinese Longitudinal Healthy Longevity Survey, China, 2011, and the shaded area indicates the 95% confidence intervals.
To further analyze the associations of BMI and ADL disability above and below the BMI cut-off value of 18.5 kg/m2 for males, we conducted logistic regression (three models). As shown in Table 2, among the subjects whose BMI values were less than 18.5 Kg/m2, BMI was not significantly associated with ADL disability whether the model was adjusted or not (P>0.05). For subjects whose BMI values were above 18.5 Kg/m2, the highest tertile group had an increased risk of ADL disability (P<0.05); the OR increased from 1.37 (95%CI: 1.05-1.79; P= 0.02) in the unadjusted model to 1.78 (95%CI: 1.26-2.52; P= 0.001) in the final fully adjusted model. For subjects whose WC values were below 75 centimeters, compared to the low group, WC in the lowest group had an increased risk of ADL disability when the model was unadjusted or adjusted only with demographic variables (model 1), while the association was not significant when further adjusted (P>0.05). For those with WC of 75 centimeters and above, the highest tertile group of WC was significantly associated with ADL disability; the OR increased from 1.42 (95%CI: 1.10-1.83; P=0.007) in the unadjusted model to 2.01 (95%CI: 1.44-2.82; P<0.001) in the final fully adjusted model.
Table 2.
Logistic Odds Ratio of ADL Disability by BMI and WC, respectively, among the Males oldest old, Chinese Longitudinal Healthy Longevity Survey, China, 2011 (n=2303) a, b, c,d
| Variables | Un-adjusted | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|
| BMI (<18.5 kg/m2, n=649) | ||||
| Lowest | 1.31 (0.88-1.96) | 1.23 (0.80-1.89) | 1.02 (0.61-1.70) | 0.93 (0.56-1.54) |
| lower | 0.79 (0.51-1.23) | 0.63 (0.40-1.01) | 0.70 (0.40-1.22) | 0.64 (0.37-1.09) |
| low | 1.00 reference | 1.00 reference | 1.00 reference | 1.00 reference |
| BMI (>=18.5 kg/m2, n=1654) | ||||
| high | 1.00 reference | 1.00 reference | 1.00 reference | 1.00 reference |
| higher | 1.17 (0.89-1.54) | 1.23 (0.93-1.64) | 1.34 (0.95-1.88) | 1.39 (0.98-1.97) |
| Highest | 1.37 (1.05-1.79) | 1.52 (1.15-2.01) | 1.78 (1.27-2.48) | 1.78 (1.26-2.52) |
| WC (<75 cm, n=579) | ||||
| Lowest | 1.57 (1.01-2.46) | 1.61 (1.01-2.56) | 1.28 (0.73-2.25) | 1.16 (0.64-2.09) |
| lower | 1.10 (0.71-1.72) | 1.05 (0.67-1.66) | 0.89 (0.51-1.54) | 0.91 (0.50-1.65) |
| low | 1.00 reference | 1.00 reference | 1.00 reference | 1.00 reference |
| WC(>=75cm, n=1724) | ||||
| high | 1.00 reference | 1.00 reference | 1.00 reference | 1.00 reference |
| higher | 1.06 (0.80-1.39) | 1.04 (0.78-1.38) | 1.14 (0.80-1.60) | 1.22 (0.85-1.75) |
| Highest | 1.42 (1.10-1.83) | 1.50 (1.15-1.96) | 1.94 (1.40-2.67) | 2.01 (1.44-2.82) |
Abbreviations: ADL, activities of daily living; BMI, body mass index; CI, confidence interval; OR, odds ratio; WC, waist circumference.
Data was shown as OR (95% CI), and the group ‘low ’ and ‘high’ were used as reference group.
Ranges for body mass index (BMI): Lowest 13.12 to <16.36; lower 16.36 to <17.58; low 17.58 to <18.5; high 18.5 to <20.55; higher 20.55 to <22.86; highest 22.86 to <=43.56.
Range for waist circumference (WC): lowest 51 to <68; lower 68 to <72; low 72 to <75; high 75 to <81, higher 81 to <88, highest 88 to <=160;
Model 1: adjustment for age, education, nationality, marital status; Model 2: additionally adjusted for living arrangement, smoking, drinking, physical activities, leisure activities and resilience; Model 3: additionally adjusted for self-rated health status, cognitive impairment, SBP, DBP, the prevalence of heart diseases, stroke, respiratory disease, cancer and bone joint disease.
Similar results were obtained when BMI and WC were both included in models.
Table 3 showed results of logistic regressions for females. Results for females appeared to be the inverse of the findings for males. Among subjects whose BMI values were less than 20 kg/m2, compared with those in the low tertile group, those in the lowest group had increased risk of ADL disability; the OR was 1.42 (95% CI: 1.02-1.97; P=0.03) in the fully adjusted model 3. For those whose BMI values were 20.0 kg/m2 and above, no significant association was found between BMI and ADL disability (P>0.05). Among the subjects whose WC values were less than 80 centimeters, the lowest tertile group in WC was also significantly associated with ADL disability whether the model was fully adjusted (P=0.02)or not adjusted (P<0.001). For those with WC of 80 centimeters and above, WC, like BMI, was not significantly associated with ADL disability (p>0.05).
Table 3.
Logistic Odds Ratio of ADL disability by BMI and WC, respectively, among the females oldest old, Chinese Longitudinal Healthy Longevity Survey, China, 2011 (n=3192).
| Variables | Un-adjusted | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|
| BMI (<20 kg/m2, n=1817 ) | ||||
| Lowest | 1.61 (1.28-2.03) | 1.51 (1.18-1.93) | 1.34 (0.97-1.84) | 1.42 (1.02-1.97) |
| lower | 1.34 (1.07-1.69) | 1.32 (1.04-1.69) | 1.25 (0.91-1.70) | 1.26 (0.92-1.73) |
| low | 1.00 reference | 1.00 reference | 1.00 reference | 1.00 reference |
| BMI (>=20 kg/m2, n=1375) | ||||
| high | 1.00 reference | 1.00 reference | 1.00 reference | 1.00 reference |
| higher | 0.72 (0.55-0.95) | 0.83 (0.62-1.11) | 0.82 (0.58-1.16) | 0.88 (0.61-1.26) |
| Highest | 0.84 (0.64-1.10) | 1.06 (0.79-1.41) | 1.04 (0.73-1.47) | 1.07 (0.74-1.54) |
| WC (<80 centimeter, n=1774) | ||||
| Lowest | 1.68 (1.33-2.12) | 1.49 (1.16-1.90) | 1.47 (1.07-2.03) | 1.47 (1.06-2.04) |
| lower | 1.25 (0.99-1.57) | 1.22 (0.95-1.56) | 1.22 (0.89-1.68) | 1.19 (0.86-1.65) |
| low | 1.00 reference | 1.00 reference | 1.00 reference | 1.00 reference |
| WC (>=80 centimeter, n=1418) | ||||
| high | 1.00 reference | 1.00 reference | 1.00 reference | 1.00 reference |
| higher | 0.85 (0.64-1.12) | 0.90 (0.67-1.22) | 0.94 (0.66-1.35) | 0.92 (0.64-1.33) |
| Highest | 0.76 (0.59-0.99) | 0.98 (0.74-1.31) | 1.02 (0.72-1.43) | 0.98 (0.69-1.41) |
Abbreviations: ADL, activities of daily living; BMI, body mass index; CI, confidence interval; OR, odds ratio; WC, waist circumference.
Data was shown as OR (95% CI), and the group ‘low ’ and ‘high’ were used as reference group.
Range for body mass index (BMI): lowest 12.01 to <16.65; lower 16.65 to <18.26; low 18.26 to <20,0; high 20.0 to <21.43; higher 21.43 to <23.67; highest 23.67 to <=44.06.
Range for waist circumference (WC): lowest 51 to <68; lower 68 to <74; low 74 to <80; high 80 to <84; higher 84 to <90, highest 90 to<=130;
Model 1: adjustment for age, education, nationality, marital status; Model 2: additionally adjusted for living arrangement, smoking, drinking, physical activities, leisure activities and resilience; Model 3: additionally adjusted for self-rated health status, cognitive impairment, SBP, DBP, the prevalence of heart diseases, stroke, respiratory disease, cancer and bone joint disease.
Similar results were obtained when BMI and WC were both included in models.
Discussion
In this sample, we found the prevalence of ADL disability was 27.31% and 38.44% among male and female respondents, respectively. By GAM, we found non-linear associations among BMI/WC and ADL disability in both male and female respondents, it was therefore deemed more appropriate to study the associations above and below the cut-points of BMI (18.5 and 20.0 kg/m2 for the males and females, respectively) and WC (75 and 80 centimeters for the males and females, respectively). These results were basically consistent with recommendations on malnutrition of various other agencies or organizations, such as World Health Organization and Food and Agriculture Organization, which consistently have recommended a lower BMI cutoff point for underweight or malnutrition as between 18.5 and 20.0 kg/m2 when physiological function was taken into account (20). Logistic regressions were further used to further explore the odds ratios for ADL disability among the four sub-populations defined by sex and cut-points. We categorized subjects according to tertiles of BMI or WC before and after the cut-points rather than simply using the current diagnostic criteria for general adults as the criteria are likely to be inappropriate for the oldest old because of composition changes. Our results supported a ‘J‘ shaped association between ADL disability with BMI and WC for the male oldest old--above the cutoff points, the highest tertile group in BMI or WC was significantly associated with increased risk of ADL disability, on the contrary, BMI or WC lower than the cutoff points were not. While an inverse ‘J’ shape association between ADL disability with BMI and WC was found in the female oldest old, which meant underweight was more likely associated with ADL disability among females.
In males, our results were consistent with other studies (2-4, 7, 21-23), which found associations of obesity, higher BMI or higher WC with increased risk of ADL limitation. There are several possible explanations for this association. First, increased BMI or WC could lead to major chronic diseases that could result in disability. Second, studies show that obesity is associated with poorer mobility and declining physical performance (24); abdominal obesity may adversely impact joint mechanics of the individual, increase postural instability (25), making it difficult or impossible to carry out activities of daily living. Third, obesity is associated with low-grade systemic inflammation and excessive oxidative stress (26), which could reduce muscle mass (27) and decrease the grip strength (28), thus lead to frailty (29) and low physical function (30).
In females, our results were consistent with other cross-sectional and longitudinal studies, which found that underweight might lead to mobility disability (4) and ADL disability (21). There are three possible explanations for the link between underweight and disability in women. First, being underweight would increase the risk of fracture and falls (31), and this risk would be even higher than that from overweight and obesity (32). Second, a low BMI in old age groups may reflect chronic malnutrition, illness or disease rather than a healthy body composition (23). Last, as BMI declines, motor function, such as strength, would be impaired significantly, therefore underweight may be a predictor of declining function (33).
There are also some studies which got inconsistent results with ours. Some studies found higher BMI/WC associated with ADL disability among men and women (2, 7, 8), or in elderly women only (4, 6, 9), or no significant association was found (10); some found WC appeared better than BMI as one predictor of ADL disability, as well as the gender difference as stated above. There are three possible explanations for these inconsistent findings. First, the population we studied was the oldest old that may be different from the younger elderly, while the subjects in almost all other studies were younger elderly, or a mix of younger and older elderly. Second, it is the fat distribution that is closely associated with increased morbidity and mortality risk, a preferential increase in abdominal fat, combined with a decrease in lower body subcutaneous fat usually occur in the ageing process. The simple anthropometric measures, such as BMI and WC, could reflect apparent obesity status, but have limitations to reflect the fat distribution, for instance, BMI fails to differentiate between mass contributed by muscle and that by adipose tissue, and WC cannot distinguish visceral fat and abdominal subcutaneous fat, although they are used as indicators of obesity in public health, and sometimes stable or reduced BMI or WC in the elderly may mask an increase in adiposity. That’s maybe one of reasons why inconsistent conclusions were obtained. Third, when BMI or WC was used as a measure of weight status in other studies, in most cases, subjects were categorized into four or three groups according to the clinical or diagnostic criteria recommended, which was developed for the general adult population, but not for the elderly, especially the oldest-old.
Several possible explanations may account for the gender differences discovered in this study. First, women have poorer physical performance and more limitations in functional abilities compared with the same-aged men (34), so women in the lowest BMI/WC, usually under malnutrition or illness (23), may report more ADL disability than men, which may be a real reflection of higher prevalence of disability among them (35). Another contributing factor may be gender difference in fat redistribution among those oldest old with a high level of BMI/WC. as studies have shown, the aging process is associated with a decrease in lower body subcutaneous fat and increase in abdominal fat. Abdominal fat consists of visceral fat and abdominal subcutaneous fat. Men are more likely to deposit visceral fat than women, and women have a greater proportion of their abdominal fat in subcutaneous depots compared with men (36, 37), while visceral fat is believed to pose greater adverse health consequences; it is more cellular, vascular and contains a larger number of inflammatory cells (38), which may lead to ADL disability, so the men ‘obese’ oldest old whose BMI/WC was at high level would be more likely to report disability, one life-threatening condition, than the women ‘obese’ oldest old, which may contribute to the men’ higher mortality rate.
There were several limitations of this study. First, our analysis was essentially cross-sectional, which meant we could not tell the causal relationship between them. There is also a potential bidirectional relationship between obesity/underweight and disability. Obesity or underweight could be the underlying cause of disability, but just as several other studies have shown, subjects who have already had disabilities might have increased risk of obesity (39, 40). Further analyses, as a part of a longitudinal study, can be conducted in the next wave of our survey with this cohort to address these important considerations. Second, most of the medical conditions included as statistical controls were based on self-report rather than objective measurement; however, we asked subjects whether the diseases they have were diagnosed by doctors.
Strengths of this study included the fact that unlike other studies, this study was, to our knowledge, one of the very few that have investigated the associations of BMI and WC with ADL disability among the oldest old. Furthermore, we studied a large sample of oldest old from a developing country. We used GAM models to explore the relationship of BMI/WC with ADL disability, thereby avoiding the assumption of a linear association among them in the absence of evidence. In addition, we conducted the analyses separately by sex, helping to shed light on gender differences in the obesity-disability relationship.
In summary, this study showed that high levels of BMI and WC were associated with ADL disability in the male oldest old, while very low level of BMI and WC were associated with ADL disability among females. More longitudinal studies should be conducted to elucidate the possible mechanism underlying these associations. These results also suggested that gender differences should be considered in programs to prevent ADL disability among the oldest old.
What is already known about the subject?
Obesity is associated with increased risk of Activities of Daily living (ADL) disability in the general elderly.
What this study adds?
1. Higher BMI/WC (obesity) is associated with Activities of Daily living (ADL) disability only in the male oldest old, while lower BMI/WC (underweight) is associated with ADL disability only in the female oldest old.
2. BMI and WC are still useful indicators for ADL disability risk even in the oldest old.
Acknowledgements
Zhaoxue Yin conducted the field survey and data analysis, and drafted and revised the manuscript. Yi Zeng and Xiaoming Shi designed the survey, reviewed and revised this manuscript. Virginia B. Kraus and Melanie Sereny Brasher help conduct data analysis and critically revised this manuscript. Huashuai Chen, Yuzhi Liu and Yuebin Lv help implementation the survey, and review the manuscript.
This work was supported by National institute of Ageing/ National institute of Health [R01 AG023627 to Z.Y.]; and the National Natural Science Foundation of China [71110107025 to Y.Z.] and National institute of Health / National institute of Ageing [Claude D. Pepper Older Americans Independence Centers 5P30 AG028716 to V.B.K.].
Footnotes
Competing interests: the authors have no competing interests.
Reference
- 1.World Health Organization . Disability and rehabilitation. World Health Organization; Geneva, Switzerland: [Accessed July 16, 2009]. 2009. http://www.who.int/disabilities/en/ [Google Scholar]
- 2.Backholer K, Pasupathi K, Wong E, Hodge A, Stevenson C, Peeters A. The relationship between body mass index prior to old age and disability in old age. Int J Obes (Lond) 2012;36:1180–1186. doi: 10.1038/ijo.2012.99. [DOI] [PubMed] [Google Scholar]
- 3.Al Snih S, Graham JE, Kuo YF, Goodwin JS, Markides KS, Ottenbacher KJ. Obesity and Disability: Relation Among Older Adults Living in Latin America and the Caribbean. Am J Epidemio. 2010;171:1282–1288. doi: 10.1093/aje/kwq087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Larrieu S, Pérès K, Letenneur L, Berr C, Dartigues JF, Ritchie K, et al. Relationship between body mass index and different domains of disability in older persons: the 3C study. Int J Obes Relat Metab Disord. 2004;28:1555–1560. doi: 10.1038/sj.ijo.0802755. [DOI] [PubMed] [Google Scholar]
- 5.Jenkins KR. Obesity’s Effects on the Onset of Functional Impairment Among Older Adults. Gerontologist. 2004;44:206–216. doi: 10.1093/geront/44.2.206. [DOI] [PubMed] [Google Scholar]
- 6.Angleman SB, Harris TB, Melzer D. The role of waist circumference in predicting disability in periretirement age adults. Int J Obes (Lond) 2006;30:364–373. doi: 10.1038/sj.ijo.0803130. [DOI] [PubMed] [Google Scholar]
- 7.Chen H, Guo X. Obesity and functional disability in elderly Americans. J Am Geriatr Soc. 2008;56:689–694. doi: 10.1111/j.1532-5415.2007.01624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nam S, Kuo YF, Markides KS, Al Snih S. Waist circumference (WC), body mass index (BMI), and disability among older adults in Latin American and the Caribbean (LAC) Arch Gerontol Geriatr. 2012;55:e40–47. doi: 10.1016/j.archger.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Houston DK, Stevens J, Cai J. Abdominal fat distribution and functional limitations and disability in a biracial cohort: the Atherosclerosis Risk in the communities study. Int J Obes (Lond) 2005;29:1457–1463. doi: 10.1038/sj.ijo.0803043. [DOI] [PubMed] [Google Scholar]
- 10.Na YM, Park HA, Kang JH, et al. Obesity, Obesity Related Disease, and Disability. Korean J Fam Med. 2011;32:412–422. doi: 10.4082/kjfm.2011.32.7.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guallar-Castillón P, Sagardui-Villamor J, Banegas JR, Graciani A, Fornés NS, López García E, et al. Waist Circumference as a Predictor of Disability among Older Adults. Obesity (Silver Spring) 2007;15:233–244. doi: 10.1038/oby.2007.532. [DOI] [PubMed] [Google Scholar]
- 12.Tahany MG. Relative body weight and disability in older adults: Results from a national survey. J Aging Health. 2010;22:403–418. doi: 10.1177/0898264310361367. [DOI] [PubMed] [Google Scholar]
- 13.Dong HJ, Unosson M, Wressle E, Marcusson J. Health Consequences Associated with Being Overweight or Obese: A Swedish population-Based Study of 85-Year-Olds. J Am Geriatr Soc. 2012;60:243–250. doi: 10.1111/j.1532-5415.2011.03827.x. [DOI] [PubMed] [Google Scholar]
- 14.Chen H. Assessment of the quality of the cross-sectional data collected in the 2008–2009 wave of Chinese longitudinal healthy longevity survey. In: Zeng Yi., editor. Research on elderly population, family, health and care needs/costs. Science Press; Beijing, China: 2010. pp. 350–352. [Google Scholar]
- 15.Zeng Yi. Towards Deeper Research and Better Policy for Healthy Aging--Using the Unique Data of Chinese Longitudinal Healthy Longevity Survey. China Economic Journal. 2012;5:2–3. 131–149. doi: 10.1080/17538963.2013.764677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katz S, Ford AB, Moscowitz RW, JACKSON BA, JAFFE MW. The index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 17.Yin ZX, Shi XM, Kraus VB, Fitzgerald SM, Qian HZ, Xu JW, et al. High normal plasma triglycerides are associated with preserved cognitive function in Chinese oldest old. Age Ageing. 2012;41:600–606. doi: 10.1093/ageing/afs033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zeng Y, Shen K. Resilience significantly contributes to Exceptional longevity. Curr Gerontol Geriatr Res. 2010;2010:525693. doi: 10.1155/2010/525693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 20.Stratton RJ, Green CJ, Elia M. Evidence base for oral nutritional support. In: Stratton RJ, Green CJ, editors. Disease-Related Malnutrition: An Evidence-Based Approach to Treatment. CABI Publishing; Oxfordshire, UK: 2003. pp. 168–236. [Google Scholar]
- 21.Reynolds SL, McIlvane JM. The impact of obesity and arthritis on active life expectancy in older Americans. Obesity (Silver Spring) 2009;17:363–369. doi: 10.1038/oby.2008.534. [DOI] [PubMed] [Google Scholar]
- 22.Backholer K, Wong E, Freak-Poli R, Walls HL, Peeters A. Increasing body weight and risk of limitations in activities of daily living: a systematic review and meta-analysis. Obes Rev. 2012;13:456–468. doi: 10.1111/j.1467-789X.2011.00970.x. [DOI] [PubMed] [Google Scholar]
- 23.Armour BS, Courtney-Long EA, Campbell VA, Wethington HR. Disability prevalence among healthy weight, overweight, and obese adults. Obesity (Silver Spring) 2013;21:852–855. doi: 10.1002/oby.20312. [DOI] [PubMed] [Google Scholar]
- 24.Vincent HK, Vincent KR, Lamb KM. Obesity and mobility disability in the older adult. Obes Rev. 2010;11:568–579. doi: 10.1111/j.1467-789X.2009.00703.x. [DOI] [PubMed] [Google Scholar]
- 25.Corbeil P, Simoneau M, Rancourt D, Tremblay A, Teasdale N. Increased risk for falling associated with obesity: mathematical modeling of postural control. IEEE Trans Neural Syst Rehabil Eng. 2001;9:126–136. doi: 10.1109/7333.928572. [DOI] [PubMed] [Google Scholar]
- 26.Mathieu P, Lemieux I, Després JP. Obesity, Inflammation, and Cardiovascular Risk. Clin Pharmacol Ther. 2010;87:407–416. doi: 10.1038/clpt.2009.311. [DOI] [PubMed] [Google Scholar]
- 27.Ferrucci L, Penninx BW, Volpato S, Harris TB, Bandeen-Roche K, Balfour J, et al. Change in muscle strength explains accelerated decline of physical function in older women with high interleukin-6 serum levels. J Am Geriatr Soc. 2002;50:1947–1954. doi: 10.1046/j.1532-5415.2002.50605.x. [DOI] [PubMed] [Google Scholar]
- 28.Howard C, Ferrucci L, Sun K, Fried LP, Walston J, Varadhan R, et al. Oxidative protein damage is associated with poor grip strength among older women living in the community. J Appl Physiol. 2007;103:17–20. doi: 10.1152/japplphysiol.00133.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hubbard RE, Woodhouse KW. Frailty, inflammation and the elderly. Biogerontology. 2010;11:635–641. doi: 10.1007/s10522-010-9292-5. [DOI] [PubMed] [Google Scholar]
- 30.Brinkley TE, Leng X, Miller ME, Kitzman DW, Pahor M, Berry MJ, et al. Chronic Inflammation Is Associated With Low Physical Function in Older Adults Across Multiple Comorbidities. J Gerontol A Biol Sci Med Sci. 2009;64:455–461. doi: 10.1093/gerona/gln038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Manandhar MC. Functional ability and nutritional status of free living elderly people. Proc Nutr Soc. 1995;54:677–691. doi: 10.1079/pns19950067. [DOI] [PubMed] [Google Scholar]
- 32.Tanaka S, Kuroda T, Saito M, Shiraki M. Overweight/obesity and underweight are both risk factors for osteoporotic fractures at different sites in Japanese postmenopausal women. Osteoporos Int. 2013;24:69–76. doi: 10.1007/s00198-012-2209-1. [DOI] [PubMed] [Google Scholar]
- 33.Honda A, Tanabe N, Seki N, Ogawa Y, Suzuki H. Underweight/overweight and the risk of long-term care: Follow-up study using data of the Japanese long-term care insurance system. Geriatr Gerontol Int. 2013 doi: 10.1111/ggi.12102. e-pub ahead print 10 June 2013; doi: 10.1111/ggi.12102. [DOI] [PubMed] [Google Scholar]
- 34.Crimmins EM, Kim JK, Solé-Auró A. Gender differences in health: results from SHARE, ELSA and HRS. Eur J Public Health. 2011;21:81–91. doi: 10.1093/eurpub/ckq022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Merrill SS, Seeman TE, Kasl SV, Berkman LF. Gender Differences in the Comparison of Self-Reported Disability and Performance Measures. J Gerontol A Biol Sci Med Sci. 1997;52:M19–M26. doi: 10.1093/gerona/52a.1.m19. [DOI] [PubMed] [Google Scholar]
- 36.Power ML, Schulkin J. Sex differences in fat storage, fat metabolism, and the health risks from obesity: possible evolutionary origins. Br J Nutr. 2008;99:931–940. doi: 10.1017/S0007114507853347. [DOI] [PubMed] [Google Scholar]
- 37.Lemieux S, Prud’homme D, Bouchard C, Tremblay A, Després JP. Sex differences in the relation of visceral adipose tissue accumulation to total body fatness. Am J Clin Nutr. 1993;58:463–467. doi: 10.1093/ajcn/58.4.463. [DOI] [PubMed] [Google Scholar]
- 38.Ibrahim MM. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev. 2010;11:11–18. doi: 10.1111/j.1467-789X.2009.00623.x. [DOI] [PubMed] [Google Scholar]
- 39.Dixon-Ibarra A, Horner-Johnson W. Disability Status as an Antecedent to Chronic Conditions: National Health Interview Survey, 2006–2012. Prev Chronic Dis. 2014;11:130251. doi: 10.5888/pcd11.130251. DOI: http://dx.doi.org/10.5888/pcd11.130251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yamaki K. Body weight status among adults with intellectual disability in the community. Ment Retard. 2005;43(1):1–10. doi: 10.1352/0047-6765(2005)43<1:BWSAAW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]


