Abstract
Objective
Both higher levels of educational attainment and a strong sense of control over one’s life independently predict better health and longevity. Evidence also suggests that these 2 factors may combine in multiplicative ways to influence subjective reports of health.
Method
In the Midlife in the United States (MIDUS) national sample (N = 6,135; age = 25 to 75 years), we tested whether stronger beliefs of control over one’s life would moderate the effect of education on 14-year mortality risk.
Results
Proportional hazards modeling indicated that both current levels of education and control beliefs were associated with lower risk of dying, over and above childhood socioeconomic level. In addition, there was a significant interaction between education and control beliefs. Among those low in education, higher control beliefs were associated with a decreased mortality risk. However, at greater levels of education, control beliefs were not associated with mortality risk. This effect remained after adjusting for potential confounding variables, including health behaviors, depressed affect, and general health (chronic illnesses, functional limitations, and self-rated health).
Conclusions
These findings demonstrate the importance of individual perceptions of control in buffering the mortality risk associated with educational disadvantage.
Keywords: education, control beliefs, mortality, social disadvantage, health inequalities
Individuals with fewer years of formal education are more likely to experience disease, disability, and premature mortality (Berkman & Kawachi, 2000). However, the elevated mortality risks associated with lower educational attainment are not always uniform: Not all individuals with low levels of education are at a higher risk of dying than those with higher levels of education, raising important questions about factors that may buffer the deleterious effects of the socioeconomic limitations associated with low education (Adler et al., 1994; Taylor & Seeman, 1999). Although effort has focused on psychosocial pathways mediating the influence of social disadvantage on health and longevity (Matthews, Gallo, & Taylor, 2010), rather less is known about moderating factors.
Two competing theoretical perspectives exist on the buffering role of individual-level dispositional constructs in the social gradient of health, including an education–longevity link. One view holds that the social–environmental pressures of low education are similar to the social psychological concept of a constant “strong situation” (Turner, 1988)— external pressures related to economic disadvantage that trump the health impact of individual differences in attitudes, behavioral propensities, and perceptions. In other words, because education is an early determinant of career options and earning power, subsequent wealth accumulation, and social circles populated by other persons possessing similar resources and societal influence, it creates a life niche characterized by daily opportunities or challenges related to socioeconomic status (SES; Galobardes, Shaw, Lawlor, Lynch, & Davey Smith, 2006a, 2006b). This theory was largely formalized in the landmark U.K. Black Report on social inequalities in health (Macintyre, 1997), and later in social epidemiology’s fundamental cause theory (Link & Phelan, 1996). An implication of this view is that personality or other individual difference constructs are less likely to impact health outcomes at low education because the situation and environment constrain any effects they might have. For instance, conscientious motivation to eat healthy will be difficult to enact and maintain if one’s economic options and social norms favor unhealthy food. By contrast, at higher levels of education, material resources permit the exercise of individual proclivities that may influence health (Minkler, 1999; Syme, 1990). This is a structuralist hypothesis, in that it emphasizes the power of societal structure rather than individual difference factors at lower levels of education (Macintyre, 1997).
Another possibility is moderation in the opposite direction. That is, the situational and environmental benefits engendered by higher education—access to health care, economic resources for health promotion and prevention, and social norms favoring healthy behavior—are so pervasive that they overpower the influence of personality dispositions. Under this conceptualization, individual differences may play less of a role at higher education. It is when the health-protective scaffolding of higher education lifestyles and environments are removed that trait-like tendencies may exert a larger influence on health, for better or for ill. A number of such tendencies, generally termed resilience factors, have been observed to play a large role at lower SES (Donnellan, Conger, McAdams, & Neppl, 2009). Ultimately, this is a self-deterministic hypothesis, in that it implies that persons have the power to mitigate or eliminate the consequences of social disadvantage for mortality risk.
Individual differences in sense of control are at least one factor that could mitigate the negative health effects associated with the structural and material limitations that often accompany low education and other indicators of SES (Lachman & Weaver, 1998). Control beliefs, also known as perceived control or sense of control, refer to subjective expectations regarding one’s ability to exert influence over life circumstances and outcomes in the surrounding environment (Lachman, Neupert, & Agrigoroaei, 2011). Similar to education, higher levels of control are associated with better health in the form of better physical functioning (Caplan & Schooler, 2003; Infurna, Gerstorf, & Zarit, 2011; Lachman & Agrigoroaei, 2010), decreased risk for cardiovascular disease incidence (Surtees et al., 2010), and lower mortality hazards (In-furna, Ram, & Gerstorf, in press; Penninx et al., 1997). Control beliefs are hypothesized to influence health through many of the same mechanisms as education, such as health behaviors (Lachman & Firth, 2004; White, Wójcicki, & McAuley, 2012) and cardiometabolic risk (Infurna & Gerstorf, in press). Lachman and Weaver (1998) found that among individuals from low-income groups, those with higher control beliefs had better self-rated health, fewer acute health symptoms, and better physical functioning than those endorsing lower control beliefs. These results support the self-deterministic hypothesis, in that the benefits for control were seen largely for those who were most vulnerable in terms of social disadvantage.
We sought to extend our understanding of the moderating role of control beliefs in the current study in several key ways. Because prior findings were based on self-report measures of health (Lachman & Weaver, 1998), we wanted to examine whether, and in what direction, control beliefs would moderate the negative health effects of low education for a more objective health outcome: 14-year mortality risk. We utilized two measures of education—parental and individual. Adjusting for parental education is an important extension of prior findings because it helps to determine whether control beliefs would moderate not only health disparities associated with a person’s own education but also the net of the persistent effects from parent’s education (Miller et al., 2011). Finally, we tested whether the effects of education and control persisted after adjusting for potential health-related confounders/mediators such as subjective and functional health ratings, number of chronic health conditions, common health behaviors, and depressed affect.
Method
Sample
The national survey of Midlife in the United States (MIDUS) is an interdisciplinary longitudinal study examining midlife development (for review, see Brim, Ryff, & Kessler, 2004). From 1994 to 1996, 7,108 participants were recruited from a nationally representative random-digit-dialing sample of noninstitutionalized adults between the ages of 25 and 75 years. Once potential participants consented to the study, they completed an approximately 30-min telephone survey and were mailed additional questionnaires. These questionnaires took approximately 2 hr to complete before being sent back to the study team. If surveys were not returned, participants were contacted and sent new questionnaires. The current sample drew from the 6,135 participants that completed both the phone and self-administered questionnaires at MIDUS 1 in 1995 to 1996. To be included in the current analysis, participants needed to have completed the following measures: demographics such as age, sex, and education; control beliefs; questions regarding alcohol and smoking; and questions assessing general health. Comparing those with full (n = 6,135) versus incomplete (n = 973) MIDUS 1 data, participants with full data were significantly older (t = 10.19; p < .001), had lower average levels of alcohol use (t = 6.13; p < .001), were slightly more likely to be female (χ2 = 17.03; p < .001), and had slightly more years of education (t = 6.48; p < .001), but did not differ in subjective rating of their health or the number of years they smoked cigarettes.
Study Variables
Demographic variables
All models were adjusted for age, sex, and race, as these variables have known associations with mortality risk. The age range of the sample spanned from 25 to 74 years (M = 46.38, SD = 13). The sex distribution was generally balanced, with 52% female (coded 0) and 48% male (coded 1). A dichotomous variable was created to contrast Caucasian (coded 0) from minority (coded 1) individuals. Approximately 91% of the sample was Caucasian.
Parental education
Participants reported on both of their parents’ highest level of education. A 12-point scale was constructed, ranging from 1 (no schooling or some grade school) to 12 (professional degrees such as PhD or MD) for the parent with the highest achieved level of education. Approximately 34% of the sample had at least one parent with some college training.
Participant education
Participants reported the highest level of education they obtained as of 1995 to 1996. The same 12-point scale used for parental education was used for participant education. Approximately 9.6% had less than a high school education, 29.03% had either a GED or high school degree, 23.05% had some college training, 25.06% had a college degree, and 13.26% had beyond a college degree.
Control beliefs
Control beliefs were operationalized by two dimensions: personal mastery and perceived constraints (Lachman & Weaver, 1998). Personal mastery refers to one’s sense of efficacy or effectiveness in carrying out goals, and perceived constraints indicates the extent one believes there are obstacles beyond one’s control that interfere with their ability to reach desired goals. Four items assessed personal mastery (e.g., “I can do just about anything I really set my mind to”; “When I really want to do something, I usually find a way to succeed at it”). Perceived constraint was assessed by 8 items (e.g., “What happens in my life is often beyond my control,” “I sometimes feel I am being pushed around in my life”). Respondents answered each question using a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree), and after reverse coding appropriate items, a total mean score of control was computed. Higher scores indicate higher control beliefs (α = .85).
General health measures
To capture a general subjective evaluation of health that is strongly predictive of mortality risk (Benyamini & Idler, 1999; Idler & Benyamini, 1997), we utilized participants’ 5-point rating of their present physical health (1 = poor, 5 = excellent). To index physical functioning (Ware & Sherbourne, 1992), participants rated whether their health limited them in doing nine different activities (e.g., limited bathing or dressing, limited climbing stairs) using a 4-point scale (1 = not at all, 4 = a lot). A mean score was computed by averaging scores for each of the nine activities so that higher scores indicated higher levels of functional limitation. To capture total health burden, participants indicated whether they had experienced or been treated for any of the 29 listed conditions over the past 12 months (e.g., ulcers, diabetes, stroke). A count variable was constructed, with higher numbers reflecting greater number of health conditions—a common approach in multi-morbidity quantification (Fortin, Bravo, Hudon, Vanasse, & Lapointe, 2005).
Health-related behaviors
To capture alcohol use, participants responded to the following question: “During the year you drank most, about how many drinks would you usually have on the days that you drank?” A continuous variable was constructed to represent the total number of years an individual reported smoking cigarettes. Participants who never smoked were assigned a score of zero.
Depressed affect
Participants answered “yes” or “no” to seven questions about depressed affect during 2 weeks in the past 12 months (e.g., “Did you lose interest in most things?”; “Did you have more trouble falling asleep than usual?”; “Did you think a lot about death?”). A count variable from 0 to 7 was constructed, with higher scores indicating higher depressed affect.
Mortality
Mortality data on participants was obtained through several National Death Index updates as of December 2009. The total number of MIDUS participants with full data that died from January 1995 through the censored end date of December 2009 numbered 570. Survival time for decedents was the interval from the date of MIDUS 1 completion (1995 to 1996) to the date of their death. Due to reasons of confidentiality, only the month and year of death were included in the MIDUS data set. Thus, every deceased participant was given the 15th day of the month as their day of death. Participants who were still alive (censored observations) had survival times that equaled the length of the follow-up (censored on January 15, 2010). The mean age of death was 68 years (SD =11; range =31 to 89), and the mean survival time for decedents was 8.01 years (SD = 3.90; range = .20 to 14 years).
Data Analysis
We tested a series of Cox proportional hazards models (Cox, 1972) using Mplus 6.0 software (Muthén & Muthén, 1998–2010) to estimate the hazard ratio (HR), or the increase in chances of dying over the follow-up period, associated with a one-standard-deviation unit of each predictor. The first model adjusted for basic demographic variables: age, sex, and race. The second model included both parental and participant education. The third model included control beliefs, and the fourth model included the education by control beliefs interaction term. The final fully adjusted model included potential health factors that could confound the relationship between the interaction term and mortality risk. Adjusting for general measures of physical health (i.e., self-rated health, functional limitations, and chronic health conditions), common health behaviors (i.e., alcohol, and tobacco use), and depressed affect is necessary because all of these variables have known associations with education and control beliefs, as well as longevity. Because these health variables were measured at the same time as the key predictors, it is not possible to determine whether they are causes or consequences of perceived control, although education is attained relatively early in life and thus widely regarded in the health inequalities literature as preceding health declines (Galobardes et al., 2006a, 2006b). Thus, these variables could be either mediators or confounders, but either way, they provide evidence of whether the observed effects of education and control exist even after statistical adjustment for relevant health factors.
Results
Tables 1 and 2 display descriptive data for study variables. Table 1 includes means, standard deviations, and correlations. Table 2 includes data for each educational category for both parent and participant. Overall, the sample was comprised of a greater number of individuals with high levels of education, but a greater number of those who died over the follow-up were in the low education groups. In addition, as either parent or participant education level increased, the mean level of control also increased.
Table 1.
Descriptive Statistics and Correlations for Study Variables
| Variable | M (SD) or % | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 46.38 (13.00) | — | ||||||||||||
| 2. Sex (male) | 48% | −.02 | — | |||||||||||
| 3. Race (minority) | 9% | −.10*** | −.03* | — | ||||||||||
| 4. Parent education | 5.53 (2.85) | −.29*** | .04** | −.06*** | — | |||||||||
| 5. Participant education | 6.77 (2.49) | −.10*** | .10*** | −.04*** | .41*** | — | ||||||||
| 6. Control beliefs | 5.50 (1.03) | −.10*** | .08*** | −.01 | .11*** | .18*** | — | |||||||
| 7. Self-rated health | 3.53 (0.99) | −.16*** | .03* | −.07*** | .18*** | .25*** | .28*** | — | ||||||
| 8. Function limitations | 1.48 (0.69) | .28** | −.12*** | .05*** | −.16*** | −.22*** | −.28*** | −.50*** | — | |||||
| 9. Chronic conditions | 2.41 (2.51) | .18*** | −.12*** | .02 | −.10*** | −.13*** | −.30*** | −.41*** | .44*** | — | ||||
| 10. Alcohol use | 3.26 (3.72) | −.15*** | .27*** | −.04** | −.01 | −.13*** | −.02 | −.08*** | .03** | .07*** | — | |||
| 11. Years smoked | 10.87 (14.05) | .35*** | .10*** | −.06*** | −.18*** | −.24*** | −.06*** | −.20*** | .20*** | .15*** | .20*** | — | ||
| 12. Depressed affect | 0.67 (1.84) | −.10*** | −.10*** | .01 | .01 | −.06*** | −.20 | −.14*** | .12*** | .09*** | .04*** | −.23*** | — | |
| 13. Net worth | 120,720.48 (209,396) | .31*** | .10*** | −.12*** | .06*** | .21*** | .12*** | .15*** | −.07*** | −.04*** | −.09*** | .03* | .15*** | — |
p < .05.
p < .01.
p < .001.
Table 2.
Descriptive Information by Education Category
| % of Sample | % Deceased | Control M (SD) | |
|---|---|---|---|
| Participant education | |||
| Some grade school | 0.54 | 13.16 | 5.22 (1.22) |
| Graduated grade school | 1.80 | 22.83 | 4.85 (1.20) |
| Some high school | 7.27 | 16.47 | 5.07 (1.16) |
| GED | 1.54 | 16.51 | 5.27 (1.04) |
| Graduated high school | 27.50 | 9.53 | 5.39 (1.04) |
| 1–2 years college | 18.35 | 9.37 | 5.48 (1.02) |
| 3+ years college | 4.69 | 6.61 | 5.63 (0.95) |
| 2-year college/vocation school | 7.58 | 8.18 | 5.53 (1.01) |
| Bachelor’s degree | 17.48 | 5.65 | 5.73 (0.92) |
| Some graduate school | 2.78 | 8.12 | 5.65 (0.95) |
| Master’s degree | 6.86 | 5.95 | 5.75 (0.94) |
| Professional degree | 3.62 | 7.39 | 5.72 (0.88) |
| Parent education | |||
| Some grade school | 6.05 | 16.75 | 5.26 (1.13) |
| Graduated grade school | 10.93 | 14.11 | 5.37 (1.11) |
| Some high school | 10.15 | 10.42 | 5.41 (1.01) |
| GED | 0.79 | 3.70 | 5.42 (0.95) |
| Graduated high School | 36.21 | 7.9 | 5.49 (1.01) |
| 1–2 years college | 8.14 | 8.30 | 5.64 (0.98) |
| 3+ years college | 1.34 | 3.30 | 5.65 (1.04) |
| 2-year college/vocation school | 5.29 | 4.72 | 5.60 (0.94) |
| Bachelor’s degree | 12.53 | 6.57 | 5.63 (0.96) |
| Some graduate school | 0.71 | 4.17 | 5.52 (1.14) |
| Master’s degree | 4.52 | 2.60 | 5.82 (0.91) |
| Professional degree | 3.35 | 6.14 | 5.60 (1.00) |
Note. % Deceased captures the percentage of individuals that died in that specific educational category. GED = general educational development.
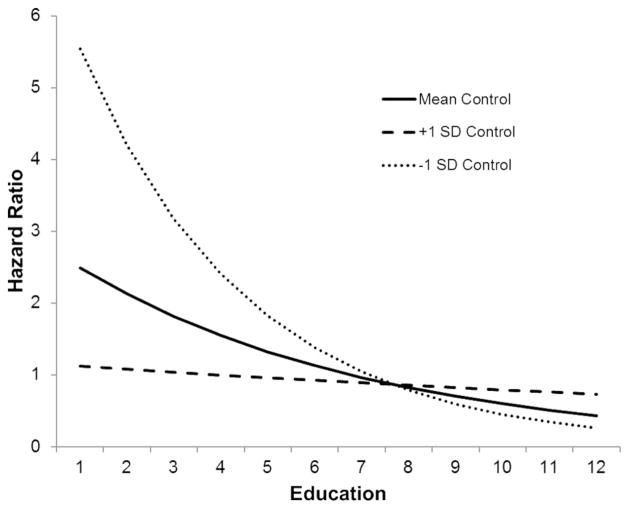
Table 3 displays the series of proportional hazards models. Model 1 indicates that older age, being male, and being a minority race were associated with an increased hazard of dying over the 14-year follow-up. In Model 2, parental education was not a significant predictor of mortality risk, but participants’ own education was. Specifically, there was a 17% reduction in the hazard of dying for every standard-deviation increase in education. Moving from a z score of 0 to 1 on education was roughly equivalent to moving from high school to an associate’s degree. After adding control beliefs to Model 3, the protective effect of education was unchanged, whereas stronger control beliefs predicted a 13% reduced hazard of dying. According to Model 4, there was a significant education by control belief interaction in predicting mortality, and this interaction is graphically illustrated in Figure 1.1 Using methods outlined by Aiken and West (1991) to plot the interaction effect, we used the parameter estimates from Model 4 to calculate the predicted HRs for the full response range for education at mean levels of control, and a standard deviation above or below the mean of control. The effects of control on mortality risk were stronger among those with lower levels of education. According to the Johnson–Neyman technique to assess the regions of significance (Hayes & Matthes, 2009; Johnson & Neyman, 1936) for the interaction effect, the Education × Control interaction was not significant at levels of education greater than 8.5 (approximately those with a college degree). Based on interpretation of Figure 1 and the regions of significance, there appears to be a threshold effect in which, at high levels of education (specifically those with a college degree or higher), high control beliefs were not associated with mortality risk, whereas at lower levels of education, control beliefs are protective against mortality.
Table 3.
Cox Regression Models With Mortality as Outcome
| Predictors | Model 1 Hazard ratio (95% CI) |
Model 2 Hazard ratio (95% CI) |
Model 3 Hazard ratio (95% CI) |
Model 4 Hazard ratio (95% CI) |
Model 5 Hazard ratio (95% CI) |
|---|---|---|---|---|---|
| Age | 3.32 [3.01, 3.67]*** | 3.23 [2.91, 3.60]*** | 3.22 [2.90, 3.58]*** | 3.22 [2.90, 3.58]*** | 2.75 [2.45, 3.09]*** |
| Sex (male) | 1.37 [1.17, 1.62]*** | 1.42 [1.19, 1.68]*** | 1.47 [1.24, 1.75]*** | 1.47 [1.24, 1.75]*** | 1.28 [1.06, 1.55]** |
| Race (minority) | 1.36 [1.01, 1.82]* | 1.24 [0.89, 1.71] | 1.22 [0.88, 1.69] | 1.19 [0.86, 1.65] | 1.02 [0.72, 1.44] |
| Parental education | 1.00 [0.96, 1.03] | 1.00 [0.97, 1.03] | 1.00 [0.97, 1.03] | 1.01 [0.97, 1.04] | |
| Participant education | 0.83 [0.76, 0.91]*** | 0.84 [0.77, 0.92]*** | 0.85 [0.78, 0.94]*** | 1.03 [0.93, 1.14] | |
| Control beliefs | 0.87 [0.80, 0.94]*** | 0.90 [0.83, 0.98]* | 1.07 [0.95, 1.21] | ||
| Education × Control | 1.12 [1.04, 1.22]** | 1.08 [1.01, 1.27]* | |||
| Self-rated health | 0.74 [0.67, 0.84]*** | ||||
| Chronic condition | 1.03 [0.95, 1.13] | ||||
| Functional limitations | 1.30 [1.19, 1.42]*** | ||||
| Alcohol use | 1.04 [0.97, 1.11] | ||||
| Years smoked | 1.31 [1.23, 1.39]*** | ||||
| Depressed affect | 1.01 [0.95, 1.06] | ||||
| −2 loga | 9272.06 | 8504.32 | 8450.65 | 8442.79 | 7942.73 |
| AIC | 9278.06 | 8514.32 | 8462.65 | 8456.79 | 7968.73 |
Note. AIC = Aikaike’s information criterion.
Likelihood ratio statistic.
p < .05.
p < .01.
p < .001.
Figure 1.
Cox regression survival curves based on level of education and sense of control. 1 = some grade school; 2 = graduated grade school; 3 = some high school; 4 = general educational development (GED); 5 = gradated high school; 6 = 1 to 2 years college; 7 = 3+ years college; 8 = graduated 2-year college/vocational school; 9 = bachelor’s degree; 10 = some graduate school; 11 = master’s degree; 12 = professional degree.
Lastly, we tested whether the interaction effect remained after adjusting for common health-related variables. First, we added each variable one by one. Alcohol use, chronic condition count, and depressed affect did not appreciably reduce the magnitude of the interaction effect on mortality risk, but subjective health ratings, functional limitations, and smoking did. Every one-point increase in subjective health rating (more positive health) resulted in a 41% reduced hazard of dying and reduced the HR for the interaction term from 1.12 to 1.09. For functional limitations, every one-standard-deviation increase resulted in a 55% increased hazard of dying and reduced the HR for the interaction term from 1.12 to 1.10. For smoking behavior, every 12-year increase in years smoked was associated with a 39% increased hazard of dying and reduced the HR for the interaction term from 1.12 to 1.11. Model 5 included all potential mediators/confounds in a conjoint model to determine their total explanatory effect. The same pattern of findings emerged: lower self-ratings of health, greater functional limitations, and greater number of years smoking were associated with a significantly increased hazard of dying over the 14-year follow-up. A product-by-coefficients method to testing mediation (or possible confounding; MacKinnon, Fairchild, & Fritz, 2007) indicated the indirect effect via this set of variables was significant (b = 0.04; 95% CI [0.01, 0.06]; p = .002). According to the mediated or possibly confounded portion (Kaufman, MacLehose, Kaufman, & Greenland, 2005; MacKinnon & Fairchild, 2009), because the HR of the Education × Control interaction effect was reduced from 1.12 in the unadjusted model to 1.08 in the fully adjusted model; self-rated health, functional limitations, and smoking behavior explained roughly 31% ([1.12–1.08]/[1–1.12]) of the difference across high and low education in the mortality risk of the perceived control interaction.
To ensure the robustness of the Education × Control interaction, we conducted a series of sensitivity analyses in regard to our main findings presented in Model 4. First, sex was tested as a moderator to determine whether this pattern of findings was true for both males and females. This interaction term did not approach statistical significance. Second, because the MIDUS study includes a subsample of twins (30%) and siblings (15%), one twin/sibling from each pair was randomly dropped, and all analyses were repeated with this reduced sample. The Education × Control interaction effect remained statistically significant, with essentially no drop in the hazard rate and only a slight widening of the confidence interval (HR = 1.07; 95% CI [1.01, 1.29]; p < .05) when compared with the effect with the full sample from Model 4 (HR = 1.08; 95% CI [1.01, 1.27]; p < .05).
To further examine any mediation or confounding of control beliefs as a moderator of education, we created interactions terms with education for each of the mediator/confounds we included in the fully adjusted model. Analyses revealed that none of the interactions with education approached statistical significance. Second, because education is only one aspect of socioeconomic position, we first tested whether the observed interaction effect would remain if we adjusted the models for an individual’s net worth (i.e., total amount of assets minus all debts). Although the sample size was substantially reduced (N = 5,379) due to missing net-worth data, the Education × Control interaction effect did not change. Second, when we tested whether control beliefs moderated the effects of net worth, instead of education, the same pattern of findings emerged (HR = 1.13; 95% CI [1.02, 1.25]; p = .02) when compared with findings from Model 4, albeit the findings were stronger. Again, control beliefs were not associated with mortality risk among those with greater net worth. However, among those with lower net worth, stronger control beliefs mitigated the increased hazard of dying. Third, we normalized both the education and net worth variables, and created an average score as a marker of SES. If a participant was missing data on net worth, education was used as the average score. We then created an interaction term with the averaged socioeconomic variable and tested whether this composite predicted mortality risk. The socioeconomic composite effect was significant and stronger (HR = 1.20; 95% CI [1.09, 1.32]; p = .001), demonstrating a similar pattern of findings as those testing the Education × Control interaction presented in Model 4 and the Net Worth × Control interaction findings.
Discussion
The current findings, parallel to prior work on control as a moderator of social class differences in health (Lachman & Weaver, 1998), support the hypothesis that sense of control is protective against declines in health at lower, but not higher, levels of education. The observed effects did not appear attributable to continuing effects of an individual’s childhood SES, as marked by parental education, and were net of subjective ratings of health and common health behaviors. These findings are contrary to classic structuralist explanations of social inequalities in health (Syme, 1990), which suggest that the situational and environmental challenges associated with lower SES overpower individual difference factors like control at low levels of education— or that stronger control beliefs are only beneficial at higher levels of SES. Instead, they are more consistent with a self-deterministic hypothesis—that high levels of perceived control is one type of resilience process (Donnellan et al., 2009) enabling persons with lower levels of education to achieve longer lifespans than others with similar socioeconomic challenges but less perceived control. A related literature concerns the orchid– dandelion hypothesis, which suggests that certain individuals are relatively strongly affected by their environment and require salutary surroundings to flower, whereas other persons are much less affected by the environment. Sense of control may be a phenotypic indicator of the orchid–dandelion continuum (Belsky & Pluess, 2009).
It is likely that perceived control involves a variety of factors, ranging from motivation to beliefs or cognitions, social and behavioral histories of successes and failures, different types of relationships with others, and affective tone. Some elements of perceived control may vary with changes in external situations, but many may be more dispositional. Thus, at a clinical level, it is not clear what constitutes the best lever to change perceptions of control. Nevertheless, there may be value in control-based behavioral intervention: Recent evidence documents naturalistic changes in control, and these changes predict mortality risk beyond initial levels of control (Infurna et al., in press). This finding is especially important from a public health perspective, because it suggests that control beliefs, despite trait-like aspects, are not utterly immutable but do show plasticity, and thus may be amenable to intervention. Some studies have demonstrated effective interventions to specifically increase levels of perceived control (Lachman et al., 2011), and it may be possible to enhance these interventions or tailor them for different populations, such as those with less formal education, in an attempt to level the playing field between haves and have-nots. Key questions for future research involve antecedents of changes in control beliefs over time, to what extent and how perceptions of control might be modified, and whether induced changes eventuate in decreased mortality risk or other beneficial health outcomes.
Our findings also provide some preliminary evidence of factors that may explain why those with low education, yet stronger control beliefs, lived longer. Those with stronger control beliefs reported better self-rated health, lower functional limitations, and smoked for fewer years compared with those with weaker control beliefs (see correlations in Table 1). These findings are not surprising, because subjective health ratings (Benyamini & Idler, 1999; Idler & Benyamini, 1997), functional limitations (for review see Pinquart, 2001), and smoking (Doll, Peto, Boreham, & Sutherland, 2004) are powerful predictors of mortality risk. We note that conclusions about mediation, however, must be tentative because the predictors and mediators were measured at the same point in time. The correlations in Table 1 are necessary but are not sufficient grounds for mediation. However, with future work, including repeated measurements of both control and health, one can begin to disentangle the directionality among these factors and control beliefs (see Cole & Maxwell, 2003; Lange & Hansen, 2011; MacKinnon & Luecken, 2008).
There are qualifications of the current study that must be discussed. First, education levels were, overall, slightly higher than population norms (61% with one or more years of college in contrast to the 1995 Current Population Survey figures of 51% [United States Department of Commerce, 1995]), although there was a sufficiently wide range in educational attainment. Second, although the sample is a large national sample of U.S. adults, the majority of the sample (approximately 91%) is Caucasian. Because there is considerable overlap between SES and race, we attempted to examine whether the effects of the current study would extend to more racially diverse samples. First, we would suggest these findings would apply to minority groups because the race covariate was not significant after including the education variables in Model 2. However, we also tested whether the pattern of effects found would be similar if we ran the analyses separately for Caucasians and non-Caucasian groups. For Caucasians (HR = 1.15; 95% CI [1.06, 1.25]; p = .01), the effects were parallel to those reported in the study. When including just non-Caucasian participants, the Education × Control interaction was not significant (HR = 0.83; 95% CI [0.62, 1.11]; p = .21). Because only 40 non-Caucasian individuals died from this group, we cannot be sure whether this small sample size led to lower power to detect the interaction effect. Although Caucasians (M = 5.51, SD = 1.02) and minority groups (M = 5.46, SD = 1.06) did not significantly differ in mean levels of control (t = 1.01; p = .31), it is plausible that a stronger perception of control somehow leads to beneficial effects in terms of longevity among Caucasian individuals. Future investigations might examine these processes and moderators of sociostructural health determinants in more diverse samples and/or in those having lower mean education (for discussion, see Roepke & Grant, 2011).
We also did not directly examine mechanisms. The conceptual model proposed by Lachman and colleagues (2011) suggests there are behavioral, motivational, affective, and physiological mediators linking control beliefs and health outcomes. For example, those with low education and low control beliefs may be less likely to utilize preventative health care assistance (e.g., yearly primary care physician visits) compared with those that endorse stronger control beliefs. Stress reactivity is another potential mechanism that could operate, especially for vulnerable populations (Diehl & Hay, 2010). Future studies investigating whether those who have higher levels of control would be more likely to perceive life stressors as controllable, minimizing the deleterious effects of stress, would provide such evidence. On balance, these limitations are accompanied by study strengths in the form of the size and country-wide nature of the sample, the novel nature of the competing hypotheses tested, the longitudinal follow-up period, the use of documented mortality as an outcome, and the enduring significance of questions about individual resilience factors vis-à-vis social–structural determinants of health.
Overall, our findings extend prior work by documenting that those with lower levels of attained education who endorse high control beliefs are more likely to live longer in contrast to those who endorse a low sense of control. Findings indicate that just because an individual does not have an extensive education does not necessarily mean they will experience elevated mortality risk. It will be worthwhile for future studies to determine exactly how those with lower educational attainment are able to develop stronger beliefs of control over their lives, and exactly why perceiving greater control leads to better health and reduced risk of dying.
Acknowledgments
This research was supported by Grant T32-MH018911-23 from the National Institute of Mental Health and PO1 AG20166, R01 AG17920, and K08 AG031328 from the National Institute on Aging.
Footnotes
Neither the parental education variable (HR = 0.93; vis-à-vis 95% CI [0.85, 1.02]; p = .11) nor the Parental Education × Control interaction emerged significant in a model either without (HR = 1.03; 95% CI [0.94, 1.12]; p = .54) or including (HR = 0.99; 95% CI [0.91, 1.07]; p = .76) the participant education variable. Alternatively, the Participant Education × Control interaction emerged significant regardless of whether parental education was (HR = 1.10; 95% CI [1.02, 1.19]; p = .01) or was not (HR = 1.11; 95% CI [1.03, 1.20]; p = .01) included.
Contributor Information
Nicholas A. Turiano, University of Rochester Medical Center
Benjamin P. Chapman, University of Rochester Medical Center
Stefan Agrigoroaei, Brandeis University.
Frank J. Infurna, German Institute for Economic Research (DIW Berlin), Berlin, Germany, and Humboldt University
Margie Lachman, Brandeis University.
References
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, Syme SL. Socioeconomic status and health: The challenge of the gradient. American Psychologist. 1994;49:15–24. doi: 10.1037/0003-066X.49.1.15. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Belsky J, Pluess M. Beyond diathesis stress: Differential susceptibility to environmental influence. Psychological Bulletin. 2009;135:885–908. doi: 10.1037/a0017376. [DOI] [PubMed] [Google Scholar]
- Benyamini Y, Idler EL. Community studies reporting association between self-rated health and mortality: Additional studies, 1995 to 1998. Research on Aging. 1999;21:392–401. doi: 10.1177/0164027599213002. [DOI] [Google Scholar]
- Berkman LF, Kawachi I. Social epidemiology. New York, NY: Oxford University Press; 2000. [Google Scholar]
- Brim OG, Ryff CD, Kessler RC, editors. How healthy are we? A national study of well-being at midlife. Chicago, IL: University of Chicago Press; 2004. [Google Scholar]
- Caplan LJ, Schooler C. The roles of fatalism, self-confidence, and intellectual resources in the disablement process in older adults. Psychology and Aging. 2003;18:551–561. doi: 10.1037/0882-7974.18.3.551. [DOI] [PubMed] [Google Scholar]
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Cox DR. Regression models and life tables. Journal of the Royal Statistical Society. 1972;34:187–220. [Google Scholar]
- Diehl M, Hay EL. Risk and resilience factors in coping with daily stress in adulthood: The role of age, self-concept incoherence, and personal control. Developmental Psychology. 2010;46:1132–1146. doi: 10.1037/a0019937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ: British Medical Journal. 2004;328:1519–1533. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnellan MB, Conger KJ, McAdams KK, Neppl TK. Personal characteristics and resilience to economic hardship and its consequences: Conceptual issues and empirical illustrations. Journal of Personality. 2009;77:1645–1676. doi: 10.1111/j.1467-6494.2009.00596.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L. Prevalence of multimorbidity among adults seen in family practice. Annals of Family Medicine. 2005;3:223–228. doi: 10.1370/afm.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (Pt. 1) Journal of Epidemiology and Community Health. 2006a;60:7–12. doi: 10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galobardes B, Shaw M, Lawlor DA, Lynch JW, Davey Smith G. Indicators of socioeconomic position (Pt. 2) Journal of Epidemiology and Community Health. 2006b;60:95–101. doi: 10.1136/jech.2004.028092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF, Matthes J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behavior Research Methods. 2009;41:924–936. doi: 10.3758/BRM.41.3.924. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- Infurna FJ, Gerstorf D. Perceived control relates to better functional health and lower cardio-metabolic risk: The mediating role of physical activity. Health Psychology. doi: 10.1037/a0030208. (in press) [DOI] [PubMed] [Google Scholar]
- Infurna FJ, Gerstorf D, Zarit SH. Examining dynamic links between perceived control and health: Longitudinal evidence for differential effects in midlife and old age. Developmental Psychology. 2011;47:9–18. doi: 10.1037/a0021022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infurna FJ, Ram N, Gerstorf D. Level and change in perceived control predict 19-year mortality: Findings from the Americans’ Changing Lives Study. Developmental Psychology. doi: 10.1037/a0031041. (in press) [DOI] [PubMed] [Google Scholar]
- Johnson P, Neyman J. Tests of certain linear hypotheses and their applications to some educational problems. Statistical Research Memoirs. 1936;1:57–93. [Google Scholar]
- Kaufman JS, MacLehose RF, Kaufman S, Greenland S. The mediation proportion. Epidemiology. 2005;16:710. doi: 10.1097/01.ede.0000171282.54664.71. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Agrigoroaei S. Promoting functional health in midlife and old age: Long-term protective effects of control beliefs, social support, and physical exercise. PLoS ONE. 2010;5:e13297. doi: 10.1371/journal.pone.0013297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman ME, Firth KM. The adaptive value of feeling in control during midlife. In: Brim OG Jr, Ryff CD, Kessler RC, editors. How healthy are we?: A national study of well-being at midlife. Chicago, IL: University of Chicago Press; 2004. pp. 320–349. [Google Scholar]
- Lachman ME, Neupert SD, Agrigoroaei S. The relevance of control beliefs for health and aging. In: Schaie KW, Willis SL, editors. Handbook of the psychology of aging. 7. New York, NY: Elsevier; 2011. pp. 175–190. [Google Scholar]
- Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. Journal of Personality and Social Psychology. 1998;74:763–773. doi: 10.1037/0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- Lange T, Hansen JV. Direct and indirect effects in a survival context. Epidemiology. 2011;22:575–581. doi: 10.1097/EDE.0b013e31821c680c. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Understanding sociodemographic differences in health—The role of fundamental social causes. American Journal of Public Health. 1996;86:471–473. doi: 10.2105/AJPH.86.4.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macintyre S. The Black Report and beyond: What are the issues? Social Science Medicine. 1997;44:723–745. doi: 10.1016/S0277-9536(96)00183-9. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ. Current directions in mediation analysis. Current Directions in Psychological Science. 2009;18:16–20. doi: 10.1111/j.1467-8721.2009.01598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Luecken LJ. How and for whom? Mediation and moderation in health psychology. Health Psychology. 2008;27:S99–S100. doi: 10.1037/0278-6133.27.2(Suppl.).S99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Gallo LC, Taylor SE. Are psychosocial factors mediators of socioeconomic status and health connections? A progress report and blueprint for the future. Annals New York Academy of Sciences. 2010;1186:146–173. doi: 10.1111/j.1749-6632.2009.05332.x. [DOI] [PubMed] [Google Scholar]
- Miller GE, Lachman ME, Chen E, Gruenewald TL, Karlamangla AR, Seeman TE. Pathways to resilience: Maternal nurturance as a buffer against childhood poverty’s effects on metabolic syndrome at midlife. Psychological Science. 2011;22:1591–1599. doi: 10.1177/0956797611419170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M. Personal responsibility for health? A review of the arguments and the evidence at century’s end. Health Education & Behavior. 1999;26:121–141. doi: 10.1177/109019819902600110. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6. Los Angeles, CA: Author; 1998–2010. [Google Scholar]
- Penninx BWJH, van Tilburg T, Kriegsman DMW, Deeg DJH, Boeke AJP, van Eijk JT. Effects of social support and personal coping resources on mortality in older age: The Longitudinal Aging Study Amsterdam. American Journal of Epidemiology. 1997;146:510–519. doi: 10.1093/oxfordjournals.aje.a009305. [DOI] [PubMed] [Google Scholar]
- Pinquart M. Correlates of subjective health in older adults: A meta-analysis. Psychology and Aging. 2001;16:414–426. doi: 10.1037/0882-7974.16.3.414. [DOI] [PubMed] [Google Scholar]
- Roepke SK, Grant I. Toward a more complete understanding of the effects of personal mastery on cardio-metabolic health. Health Psychology. 2011;30:615–632. doi: 10.1037/a0023480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surtees PG, Wainwright WJ, Luben R, Wareham NJ, Bingham S, Khaw KT. Mastery is associated with cardiovascular disease mortality in men and women at apparently low risk. Health Psychology. 2010;29:412–420. doi: 10.1037/a0019432. [DOI] [PubMed] [Google Scholar]
- Syme S. Control and health: An epidemiologic perspective. In: Rodin CSJ, Schaie KW, editors. Self-directedness: Cause and effects through the life course. Hillsdale, NJ: Erlbaum; 1990. pp. 213–229. [Google Scholar]
- Taylor SE, Seeman TE. Psychosocial resources and the SES– health relationship. Annals of the New York Academy of Sciences. 1999;896:210–225. doi: 10.1111/j.1749-6632.1999.tb08117.x. [DOI] [PubMed] [Google Scholar]
- Turner RH. Personality in society: Social psychology’s contribution to sociology. Social Psychology Quarterly. 1988;51:1–10. doi: 10.2307/2786979. [DOI] [Google Scholar]
- United States Department of Commerce, Bureau of the Census. Current Population Survey. 1995 http://www.census.gov/prod/techdoc/cps/cpsmar95.pdf.
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): Conceptual framework and item selection. Medical Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- White SM, Wójcicki TR, McAuley E. Social cognitive influences on physical activity behavior in middle-aged and older adults. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2012;67:18–26. doi: 10.1093/geronb/gbr064. [DOI] [PMC free article] [PubMed] [Google Scholar]