Abstract
Objective
Weight dissatisfaction, defined as discordance between actual and goal weight, may be associated with increased risk for several obesity-related comorbidities. The purpose of the study was to examine the association between weight dissatisfaction and risk of developing type 2 diabetes.
Methods
This longitudinal study used data from 9,584 adults enrolled in the Aerobics Center Longitudinal Study with an average of 5.1±4.1 years of follow-up. Key variables included multiple measures of measured weight, self-reported goal weight, and incident diabetes. Weight dissatisfaction was defined as being above the median of measured weight minus goal weight. Cox proportional hazards regression estimated hazard ratios (HR) and 95% confidence intervals (95%CI) for diabetes incidence by weight dissatisfaction.
Results
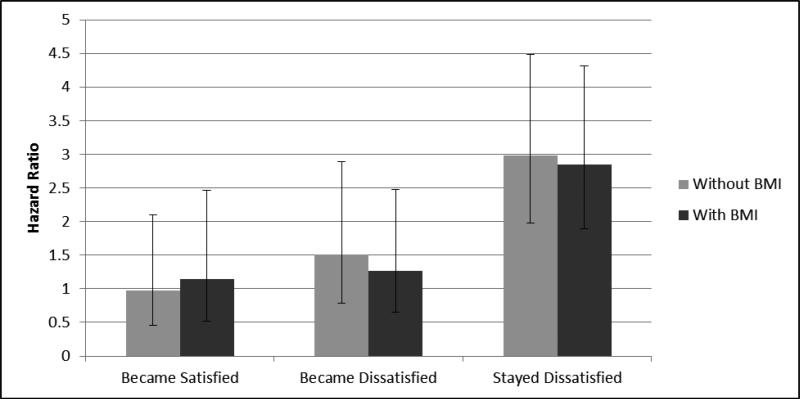
HRs for time-until-diabetes diagnosis revealed that family history of diabetes (HR=1.46, 95%CI=1.13-1.90), age (HR=1.03, 95%CI=1.02-1.04), and weight dissatisfaction (HR=1.83, 95%CI=1.50-2.25) at baseline were statistically significant predictors. Longitudinally, higher risk was observed in individuals who either stayed dissatisfied (HR=2.98, 95%CI=1.98-4.48) or became dissatisfied (HR=1.51, 95%CI=0.79-2.89), compared to those who either stayed satisfied (HR=1.00, referent) or became satisfied (HR=0.98, 95%CI=0.46-2.10). After additional adjustment for BMI, the elevated HR for those who remained dissatisfied compared to those who remained satisfied persisted (HR=2.85, 95%CI=1.89-4.31).
Conclusions
Chronic weight dissatisfaction increased type 2 diabetes risk. Weight dissatisfaction, regardless of BMI, represents a potentially important psychophysiological modifier of the relationships between BMI and risk of type 2 diabetes and warrants greater attention in future studies of chronic disease risk.
Keywords: Weight Dissatisfaction, Diabetes, Obesity, Physical Activity, Chronic Disease Risk Factors
Introduction
The epidemics of obesity and related chronic diseases, such as type 2 diabetes, are rapidly spreading throughout the world (Caballero, 2007; Pednekar, Gupta, Hebert, & Hakama, 2008; Wang & Beydoun, 2007; Wang & Lobstein, 2006). Currently, it is estimated that 11.3% of US adults have diabetes; nearly two million new type 2 diabetes diagnoses occurred in 2010 alone; and globally about 346 million people suffer from diabetes (NDIC, 2011; Sherwin & Jastreboff, 2012; WHO, 2011). Obesity has been shown to be strongly associated with the incidence of diabetes via numerous previously described mechanisms, such as increased insulin resistance and inflammation (A. J. Garber, 2012; Nolan, Damm, & Prentki, 2011). Several studies have indicated increased type 2 diabetes risk among those consuming primarily Western diets, which are higher in fats, simple carbohydrates and proteins and lower in fruits and vegetables compared with other diets (Fung, McCullough, van Dam, & Hu, 2007; Lazarou, Panagiotakos, & Matalas, 2012; van Dam, Rimm, Willett, Stampfer, & Hu, 2002); those with low levels of physical activity (Bird & Hawley, 2012; Sherwin & Jastreboff, 2012); those who consume excessive alcohol; and active smokers (Baliunas et al., 2009; Willi, Bodenmann, Ghali, Faris, & Cornuz, 2007). Proper weight management and engagement in positive health-promoting behaviors are crucial to preventing or delaying the onset of type 2 diabetes (Djousse, Driver, Gaziano, Buring, & Lee, 2013).
Helping populations achieve healthy weights has been cited as the most important goal for slowing the progression of this serious public health crisis (Bird & Hawley, 2012; Casazza et al., 2013; Sherwin & Jastreboff, 2012). A potentially important barrier to weight loss and control is a lack of motivation (Haslam & James, 2005). Several factors can potentially affect a person's motivation to achieve and maintain a healthy weight, one of which is degree of weight satisfaction or dissatisfaction.
Weight satisfaction, defined as a close correspondence between actual weight and self-reported goal weight, has been associated with better self-reported perceived health, as well as healthier lifestyle behaviors including more jogging, better cardiorespiratory fitness and greater consumption of fruits and vegetables (Kim, Lim, & Kwak, 2008; Kuk et al., 2009). Weight satisfaction also is associated with less intention to change physical activity, diet, or body weight (Kim, et al., 2008; Kuk, et al., 2009). Among individuals who are overweight or obese, positive perceptions of weight status or weight satisfaction and negative intentions toward behavior change may preclude motivation to make changes in weight-related health behaviors and increase risk of type 2 diabetes (Duncan et al., 2011).
In contrast, greater weight dissatisfaction, defined as a larger discrepancy between actual weight and goal weight, has been shown to be associated with higher body mass index (BMI) and many unhealthy weight-related behaviors including poor eating habits or eating disorders such as vomiting, binging, use of weight loss pills, bulimia, yo-yo dieting, skipping meals, and increased frequency of snacking and fast food meals (Blake et al., 2013; A. K. Garber, Boyer, Pollack, Chang, & Shafer, 2008; Keel, Baxter, Heatherton, & Joiner, 2007; Satia, Galanko, & Siega-Riz, 2004). Weight dissatisfaction also has been shown to be associated with higher rates of tobacco use, higher educational attainment and income, and diagnosed mental illness, as well as poorer self-perceived health (Blake, et al., 2013; Forrester-Knauss & Zemp Stutz, 2012; Matthiasdottir, Jonsson, & Kristjansson, 2012; Minsky, Vreeland, Miller, & Gara, 2013; Noor, Lua, & Nik, 2011; von Lengerke & Mielck, 2012). Weight dissatisfaction estimates range from about 25% to over 50% across different population groups (Arroyo et al., 2010; Forrester-Knauss & Zemp Stutz, 2012; Niskar, Baron-Epel, Garty-Sandalon, & Keinan-Boker, 2009; von Lengerke & Mielck, 2012). Women compared to men and European Americans compared to African Americans are consistently more likely to be dissatisfied with their weight, regardless of BMI status (Bennett & Wolin, 2006; Dorsey, Eberhardt, & Ogden, 2009; Forrester-Knauss & Zemp Stutz, 2012; Hendley et al., 2011). Dissatisfaction with one's weight may be more important to motivate individuals to lose weight than actual measured weight (Kuk, et al., 2009; Lemon, Rosal, Zapka, Borg, & Andersen, 2009; Yaemsiri, Slining, & Agarwal, 2011). It is possible that weight dissatisfaction may be an important motivator among overweight and obese adults to engage in more positive health behaviors leading to future reductions in risk of chronic diseases, such as type 2 diabetes. A better understanding of relationships between weight dissatisfaction, health behaviors, and risk of type 2 diabetes would provide important insights for prevention and treatment efforts.
There is little consensus in the literature on the direction of relationships between weight dissatisfaction, health behaviors, and chronic disease risk, including type 2 diabetes. Furthermore, the long-term impact of weight dissatisfaction on type 2 diabetes risk is unknown. The purpose of this study is to elucidate these relationships by examining the impact of weight satisfaction and dissatisfaction over time on risk of developing type 2 diabetes. This study examined the hypothesis that chronic weight dissatisfaction is associated with increased type 2 diabetes risk among a population of adults from the Aerobics Center Longitudinal Study (ACLS). In addition to cross-sectional relationships with weight dissatisfaction, we also hypothesize that those who move from being dissatisfied to satisfied will exhibit a reduction in risk of type 2 diabetes compared to those who remain dissatisfied and that this movement will be accompanied by positive changes in health behaviors.
Methods
Study Population
The study population was comprised of 9,584 adults from the ACLS, which accounts for 29% of the total population. The ACLS is an epidemiological investigation based on patients who came to the Cooper Clinic (Dallas, Texas) for preventive evaluations. The ACLS is reviewed and approved by the Cooper Institute Institutional Review Board on an annual basis. To be eligible for the current study, subjects of either gender needed to be greater than 20 years of age, have undergone at least two clinical examinations between 1977 and 2006, have height that ranges from 120 to 209 cm, and have complete data on objectively measured weight, self-reported goal weight, age, BMI, physical activity, smoking, alcohol consumption, and family history of diabetes (i.e., self-reported parental diabetes diagnoses). Subjects included in the analyses had no baseline diabetes, defined as a physician diagnosis, insulin use, or fasting glucose ≥126mg/dL, and no cardiovascular disease (CVD), cancer, ulcers, gallbladder disease, jaundice, hepatitis, cirrhosis, or colon polyps in any of the examinations. Additionally, all participants completed a treadmill exercise test to at least 85% of their age-predicted maximal heart rate [220- (age in years) beats per minute] (Peel et al., 2009). We further excluded those whose body mass index [BMI=weight(kg)/height(m)2] was <18.5 or ≥50 kg/m2, which may represent subclinical disease or measurement error (n=349).
Clinical Examination
All participants provided written informed consent to participate in the study and they arrived for the clinical examination after at least a 12-hour overnight fasting period. Examination methods and procedures followed a standard manual of operations, as described previously (Blair et al., 1989; Lee et al., 2012). Collected information included personal and family health histories, fasting blood chemistry analyses, anthropometry, resting blood pressure, electrocardiogram, and a maximal graded exercise test. BMI was computed from measured weight and height. Participants were asked “What do you consider a good weight for yourself?” which was used to assess goal weight at the clinical examination. Weight dissatisfaction was defined as measured weight minus the goal weight. For baseline-only analyses, categories of weight dissatisfaction were specifically determined by using a median split of the difference between measured weight and self-reported goal weight which was 7.75 pounds (3.52kg) among males and 8.00 pounds (3.64kg) among females. A secondary analysis focused on the difference in weight dissatisfaction using the baseline visit and the visit at which at least two years of follow-up was achieved (referred to as time point 2). This required participants to have at least three clinic visits with no diabetes diagnoses at the first two examinations. For these secondary analyses, weight dissatisfaction at baseline was subtracted from the weight dissatisfaction at time point 2. Due to varying lengths of time between these two time points across subjects, this difference was divided by the number of years between time points. A four-level weight dissatisfaction categorical variable also was created. If a subject had been satisfied or dissatisfied at both baseline and time point 2, they were classified as ‘stayed satisfied’ or ‘stayed dissatisfied’, respectively. If a subject changed from dissatisfied to satisfied or satisfied to dissatisfied, they were classified as ‘became satisfied’ or ‘became dissatisfied’, respectively.
A standardized medical history questionnaire was used to obtain information on smoking habits (current, former, or non-smoker), alcohol intake (drinks per week), personal history of myocardial infarction, stroke, cancer, hypertension, diabetes, hypercholesterolemia, ulcer, gallbladder disease, jaundice, hepatitis, cirrhosis, colon polyps, eating habits, and dieting frequency. Self-assessment of physical activity was ascertained and consisted of questions on current moderate and vigorous physical activity and intention regarding future activity (Blair, et al., 1989; Lee, et al., 2012). Resting blood pressure was recorded as the first and fifth Korotkof sounds by ausculatatory methods. Serum samples were analyzed for lipids and glucose using standardized automated bioassays by a laboratory that participates in the CDC Lipid Standardization Program and meets its quality control standards.
A maximal treadmill test was used to asses cardiorespiratory fitness (CRF) using a modified Balke protocol (Balke & Ware, 1959; Blair, et al., 1989; Lee, et al., 2012). The treadmill speed was 88m · min-1 for the first 25 min. During this time the grade was 0% for the first minute, 2% the second minute, and increased 1% for each minute thereafter. After 25 min, the grade remained constant while the speed increased 5.4 m · min-1 each minute until test termination. Patients were encouraged to give a maximal effort during the test. Strong positive correlations have been observed between the duration of the maximal exercise treadmill test on this protocol and directly measured maximal oxygen uptake in men and women (r = 0.92 and 0.94, respectively) (Pollock et al., 1976; Pollock et al., 1982), an accepted measure of CRF. Maximal metabolic equivalents (METs, 1 MET = 3.5 ml O2 uptake • kg-1 • min-1) were estimated from the final treadmill speed and grade (ACSM, 2005).
Statistical Analyses
All analyses were performed using SAS® (version 9.3, Cary, NC). Frequencies or means and standard deviations were calculated for demographic and health-related characteristics. To examine differences between weight dissatisfaction categories (i.e., satisfied vs. dissatisfied) when stratified by sex, chi-square tests were used for categorical variables and t-tests for continuous variables. Cox proportional hazards regression was used to estimate hazard ratios (HRs) and 95% confidence intervals (95%CI) for diabetes incidence according to weight dissatisfaction. Follow-up time was computed from baseline (i.e., first visit) until the last examination for those who did not develop diabetes or the earliest reported diabetes diagnosis for those who developed diabetes. Covariates include age, sex, physical inactivity (inactive vs. active as defined by no leisure-time activity during the 3 months prior to baseline), smoking status (current vs. non-smoker), alcohol intake (heavy vs. non-heavy drinker defined as >14 drinks for men or >7 drinks for women per week), and family history of diabetes at baseline. Weight dissatisfaction was analyzed both as a categorical and continuous measure. In separate models, we additionally adjusted for baseline BMI. To test effect modification according to sex, risk estimates were compared after stratifying the main analyses by sex. There were no differences in the interpretation of the results and thus only results of all subjects are presented in Table 2. The proportional hazards assumptions were met by comparing the log-log survival plots, as well as testing the significance of time-dependent covariates that were created by computing an interaction term between weight dissatisfaction and the log of follow-up time.
Table 2.
Hazard ratios (95% Confidence Interval) for diabetes incidence for all covariates
| Variable | Hazard Ratio | 95% CI |
|---|---|---|
| Weight Satisfaction: Dissatisfied vs. Satisfied | 1.83 | 1.50 – 2.25 |
| Physical Activity: Inactive vs. Active | 0.99 | 0.78 – 1.26 |
| Smoking Status: Current vs. Non-Smoker | 1.08 | 0.76 – 1.52 |
| Sex: Female vs. Male | 0.78 | 0.59 – 1.05 |
| Family History of Diabetes: Yes vs. No | 1.46 | 1.13 – 1.90 |
| Alcohol Use: Heavy Drinker vs. Non-Heavy | 1.02 | 0.75 – 1.40 |
| Agea | 1.03 | 1.02 – 1.04 |
Continuous variables – hazard ratios are based on a 1 unit increase.
For the secondary analyses, follow-up began at time point 2 until diabetes diagnosis or censorship, which had to be a minimum of two years for inclusion. Categorical variables were created to describe the change in smoking status, physical activity, and alcohol intake between time points (e.g., stayed nonsmokers, became nonsmokers, became smokers, stayed smokers). The change in BMI was defined as the difference between the two time points. Again, Cox proportional hazards was used to determine HRs and 95%CIs for the categorical and continuous forms of the difference in weight dissatisfaction after adjustment for baseline age, sex, and family history of diabetes, and the change in smoking status, physical inactivity, and alcohol intake.
Results
A total of 9,584 subjects (7,821 male and 1,763 female) had complete data for weight dissatisfaction, diabetes diagnosis, and all covariates. Total average follow-up time was 5.1±4.1 years. A total of 397 (4%) subjects developed type 2 diabetes. Overall, subjects included in this study compared to the full ACLS population were more likely to be female (18.4% vs. 16.5%), inactive (20.1% vs. 16.4%), smokers (10.2% vs. 8.1%), heavy drinkers (11.7% vs. 10.4%), and older (mean age: 46.4±9.4 vs. 46.0±9.9), as well has have a family history of diabetes (12.9% vs. 11.2%). Even though these differences were all statistically significant (p<0.01), they were small in magnitude. Table 1 displays double-stratified population characteristics by sex and weight dissatisfaction (i.e., satisfied vs. dissatisfied). Among men, those who were dissatisfied were younger, more likely to smoke, drink heavily, have a previous diagnosis of hypertension or hypercholesterolemia, and have a family history of diabetes. In addition dissatisfied men had poorer health indictors including higher percent body fat, BMI, waist circumference, systolic and diastolic blood pressure, glucose and cholesterol levels, and lower treadmill time and maximal METs. These differences were all statistically significant. The same relationships were observed among women, except for smoking status and age. In addition, drinking status showed an opposite association; dissatisfied women were less likely to drink heavily than satisfied women.
Table 1.
Population and Health Characteristics by Weight Dissatisfaction Category and Sex at Baseline
| Characteristic | Men (n=7821) | Women (n=1763) | ||||
|---|---|---|---|---|---|---|
| Satisfied (n=3937) | Dissatisfied (n=3884) | p-value | Satisfied (n=901) | Dissatisfied (n=862) | p-value | |
| Categorical Characteristics | ||||||
| Smoking Status | ||||||
| Non-Smoker | 3564 (91%) | 3374 (87%) | 860 (95%) | 813 (94%) | ||
| Current Smoker | 373 (9%) | 510 (13%) | <0.01 | 41 (5%) | 49 (6%) | 0.28 |
| Drinking Statusa | ||||||
| Non-Heavy Drinker | 3578 (91%) | 3437 (88%) | 720 (80%) | 724 (84%) | ||
| Heavy Drinker | 359 (9%) | 447 (12%) | <0.01 | 181 (20%) | 138 (16%) | 0.03 |
| Family Diabetes History | ||||||
| No | 3508 (89%) | 3328 (86%) | 790 (88%) | 721 (84%) | ||
| Yes | 429 (11%) | 556 (14%) | <0.01 | 111 (12%) | 141 (16%) | 0.02 |
| Physical Activity Levelb | ||||||
| Active | 3271 (83%) | 2896 (75%) | 769 (85%) | 666 (77%) | ||
| Inactive | 666 (17%) | 988 (25%) | <0.01 | 132 (15%) | 196 (23%) | <0.01 |
| Hypertensionc | ||||||
| No | 3059 (78%) | 2577 (66%) | 797 (88%) | 701 (81%) | ||
| Yes | 878 (22%) | 1307 (34%) | <0.01 | 104 (12%) | 161 (19%) | <0.01 |
| Hypercholesterolemiad | ||||||
| No | 3022 (77%) | 2535 (65%) | 735 (82%) | 642 (74%) | ||
| Yes | 915 (23%) | 1349 (35%) | <0.01 | 166 (18%) | 220 (26%) | <0.01 |
| Continuous Characteristics | ||||||
| Age | 46.9±10.1 | 46.0±8.4 | <0.01 | 46.4±9.9 | 46.1±9.2 | 0.51 |
| Percent Body Fat | 18.1±5.0 | 24.3±4.9 | <0.01 | 22.6±5.2 | 29.4±5.5 | <0.01 |
| Body Mass Index (kg/m2) | 24.2±2.0 | 28.3±3.1 | <0.01 | 21.0±1.5 | 25.2±3.3 | <0.01 |
| Waist Circumference (cm) | 87.3±6.5 | 98.4±8.8 | <0.01 | 68.5±6.0 | 78.0±9.5 | <0.01 |
| Treadmill Time (minutes) | 21.4±4.4 | 18.2±4.1 | <0.01 | 16.6±4.4 | 13.6±3.8 | <0.01 |
| Maximal METse | 13.3±2.4 | 11.7±2.0 | <0.01 | 11.0±2.1 | 9.6±1.8 | <0.01 |
| Systolic Blood Pressure (mmHg) | 120.3±12.8 | 122.4±12.3 | <0.01 | 112.0±13.4 | 114.6±14.5 | <0.01 |
| Diastolic Blood Pressure (mmHg) | 80.0±8.8 | 82.8±9.3 | <0.01 | 75.1±9.1 | 77.0±9.6 | <0.01 |
| Glucose (mg/dL) | 96.5±8.2 | 98.9±8.5 | <0.01 | 91.4±7.8 | 93.4±8.1 | <0.01 |
| Cholesterol (mg/dL) | 201.6±36.7 | 212.5±39.1 | <0.01 | 195.2±37.0 | 203.5±39.9 | <0.01 |
Column percents may not equal 100% due to rounding. P-values for categorical variables were based on chi-square tests and p-values for continuous measures were based on t-tests.
Defined as >14 drinks for men or >7 drinks for women per week.
Inactive was defined as no leisure-time activity during the 3 months prior to the first baseline visit.
Defined as a resting blood pressure of ≥ 140/90 mmHg or physician diagnosed.
Defined as total cholesterol ≥ 240mg/dl or physician diagnosed.
Achieved during treadmill test.
HRs for time until diabetes diagnosis for each variable in the fully adjusted model at baseline are presented in Table 2. Family history of diabetes (HR=1.46, 95%CI=1.13-1.90) and age (HR for one-unit change: 1.03, 95%CI=1.02-1.04) were statistically significant predictors of type 2 diabetes. Of primary interest, the HR for weight dissatisfaction was 83% greater compared to those who were satisfied (HR=1.83, 95%CI=1.50-2.25). When stratified by sex, there was no difference in the interpretation of the results (males: HR=1.82, 95%CI=1.47-2.27; females: HR= 1.88, 95%CI=1.08-3.27). The HR for a one-unit increase in weight dissatisfaction (described as continuous) was 1.024 (95%CI=1.017-1.030). However, after additional adjustment for BMI, the HR for being dissatisfied was no longer statistically significant (HR=1.23, 95%CI=0.95-1.58). Even though BMI was highly correlated with weight dissatisfaction (r=0.72, p<0.01), additional post-hoc analyses determined that BMI (i.e., normal vs. overweight/obese) was not an effect modifier; the HRs for weight dissatisfaction were 1.70 (95%CI=1.15-2.50) and 1.45 (95%CI=1.06-1.97) for those who were normal and for those who were overweight/obese, respectively.
The secondary analyses examining the difference in weight dissatisfaction between baseline and time point 2 included 2,742 subjects (≈29% of the total baseline population, exclusions: 4,485 did not have at least 3 clinic visits; 159 did not achieve at least a two-year difference between baseline and the second time point; and 2,198 did not achieve at least 2 years of follow-up after the second time point) with an average time between measurement points of 3.4±1.9 years. The average follow-up time from the second time point was 6.1±3.5 years. The number of subjects who stayed satisfied, became satisfied, became dissatisfied, and stayed dissatisfied was 1,268 (46%), 291 (11%), 322 (12%), and 861 (31%), respectively. An increasing trend in HRs for time until diabetes diagnosis was observed when comparing those who became satisfied (HR=0.98, 95%CI=0.46-2.10), those who became dissatisfied (HR=1.51, 95%CI=0.79-2.89), and those who stayed dissatisfied (HR=2.98, 95%CI=1.98-4.48) to those who stayed satisfied (Figure 1). After additional adjustment for BMI, the statistically significantly elevated diabetes HR for those who stayed dissatisfied compared with those who stayed satisfied persisted (HR=2.85, 95%CI=1.89-4.31) (Figure 1). Even compared to those who became satisfied, those who stayed dissatisfied still had a statistically significantly increased risk of type 2 diabetes (HR=3.04, 95%CI=1.44-6.39). Further analyses indicated a reduction in BMI of -0.99kg/m2 among those who became satisfied, whereas those who became dissatisfied or stayed dissatisfied increased BMI by +1.34 kg/m2 and +0.40 kg/m2, respectively (both p<0.01 compared to those who became satisfied). Additionally, those who stayed dissatisfied were more likely to become inactive compared to those who became satisfied (9.3% vs. 6.5%, p=0.02). Again, these HRs did not differ when stratified by sex or BMI. The HR for the continuous form of the difference in weight dissatisfaction between baseline and time point 2 was 1.04 (95%CI= 0.98-1.10).
Figure 1.
Hazard ratios for diabetes incidence and 95% confidence intervals for the change in weight satisfaction. ‘Became Satisfied’, ‘Became Dissatisfied’, and ‘Stayed Dissatisfied’ were compared to the ‘Stayed Satisfied’ category. All models adjusted for baseline age, sex, and family history of diabetes, and the change in smoking status, physical inactivity, and alcohol intake. Light grey bars represent adjusted models without BMI and the dark grey bars represent adjusted models with additional adjustment for BMI.
Discussion
In this study, main findings indicated that weight dissatisfaction was associated with increased risk of type 2 diabetes; this was especially true for those who remained chronically weight dissatisfied over a period of years. Furthermore, weight dissatisfaction was associated with fewer positive health behaviors and outcomes including less physical activity and treadmill time and higher glucose and cholesterol levels.
Being dissatisfied with one's weight may not result in motivation to engage in healthier weight-related behaviors among all individuals, despite literature suggesting that weight dissatisfaction is associated with greater effort at weight loss (Kuk, et al., 2009; Lemon, et al., 2009; Yaemsiri, et al., 2011). Chronic weight dissatisfaction may actually perpetuate poor dietary and lifestyle behaviors, therefore increasing, or at least sustaining, one's overweight/obesity status. If this hypothesis is correct, then poor dietary and lifestyle behaviors such as lack of physical activity, Western-style diets (i.e., high in fats, protein, and sweets), tobacco use, and heavy alcohol consumption may, at least partially, explain the increase in type 2 diabetes risk with chronic weight dissatisfaction observed in this study. This was partially evidenced by findings that men who were dissatisfied with their weight were more likely to be current smokers and moderate/heavy drinkers in the current study. One previous study also found that former smoking status among men and current or former smoking status among women were statistically significant predictors of weight dissatisfaction (Forrester-Knauss & Zemp Stutz, 2012). It is possible that these findings reflect a fatalistic approach to health or that health concerns do not influence their behavior. Qualitative studies on factors that influence food choice have demonstrated that health is often a less prominent influence on behavior than other values that dominate decision-making processes (e.g., convenience, self-image) (Blake, Bisogni, Sobal, Jastran, & Devine, 2008; Connors, Bisogni, Sobal, & Devine, 2001). It is possible that similar value negotiations influence response to one's weight and may help explain relationships between chronic weight dissatisfaction and increased risk of type 2 diabetes. To provide further evidence for this mechanism, numerous studies have shown increased type 2 diabetes risk with these poor dietary and other lifestyle choices (Bird & Hawley, 2012; Lazarou, et al., 2012; Psaltopoulou, Ilias, & Alevizaki, 2010), which may act, in part, through inflammatory-related mechanisms (Ahluwalia, Andreeva, Kesse-Guyot, & Hercberg, 2012; A. J. Garber, 2012; Lavie, Church, Milani, & Earnest, 2011; Prasad, Sung, & Aggarwal, 2012). However, this hypothesis could not be tested in the current study. Further study of chronic weight dissatisfaction and health behaviors would provide greater insight into these findings, especially in relation to chronic disease risk.
These findings call into question the relevance of concerns regarding weight satisfaction among those who are overweight or obese (Duncan, et al., 2011). Results indicating that adults who are satisfied with their weight tend be more physically active and have lower long-term risk of type 2 diabetes were found regardless of changes in health behaviors or BMI which is a strong predictor of type 2 diabetes (Huerta et al., 2013; Kodama et al., 2012). Furthermore, our findings suggest that those who move from being dissatisfied to satisfied with their weight became more physically active during the study period and exhibited trends toward lower risk of type 2 diabetes at follow-up. These results are in accordance with previous findings (Kim, et al., 2008; Kuk, et al., 2009). For example, a study by Kuk et al. found that weight satisfaction was associated with a greater distance walked or jogged per week compared to those who were dissatisfied with their weight (Kuk, et al., 2009). Individuals who are fit or become and stay fit may be evincing motivation that is different in important ways from the motivation of those who are dissatisfied with their weight and dieting primarily to lose weight (Dacey, Baltzell, & Zaichkowsky, 2008; Kreutz, 2008; Yap & Davis, 2008). Image also may matter with health behavior aimed primarily toward fitness (rather than weight control) (Halliwell, Dittmar, & Orsborn, 2007). Physical activity has been shown to increase self-esteem and body image regardless of BMI (Fuller-Tyszkiewicz, Skouteris, & McCabe, 2012; Korn, Gonen, Shaked, & Golan, 2013; Schmalz, Deane, Birch, & Davison, 2007). Perhaps overweight adults who become active for reasons other than merely weight control develop a more positive outlook on their weight (i.e., they become satisfied).
Strengths of the study are its large sample size and detailed information on weight, weight satisfaction, anthropometrics, fitness, and health outcomes. We used the discrepancy between self-reported ideal weight and actual measured weight to assess weight dissatisfaction. Our approach is consistent with recent studies that have examined relationships between weight self-perceptions and health behaviors and outcomes (Kuk, et al., 2009). Our approach has strengths over many self-reported weight satisfaction measures that ask individuals to indicate level of satisfaction because these may capture other aspects of body dissatisfaction or dieting behavior not specific to weight or that are more susceptible to social desirability bias (Al Sabbah, Vereecken, Abdeen, Coats, & Maes, 2009; Thompson, 2004). Also, the longitudinal nature of this study allowed us to examine the temporality of the relationships between weight dissatisfaction and risk of type 2 diabetes, which to our knowledge, has not previously been done. Limitations include the homogeneity of the mostly European-American, educated, and middle to upper-income study sample, which means results may not be generalizable to the US population. Other population groups such as African-American or Native-American populations have higher prevalence of obesity and type 2 diabetes and different cultural attitudes toward body size (NDIC, 2011; Ogden et al., 2006; Padgett & Biro, 2003). It is possible that weight dissatisfaction may lead to different behaviors and outcomes in these populations. The significant findings in this lower-risk population serve to highlight the importance of examining the relationship between weight dissatisfaction, health behaviors, and health outcomes in populations at higher risk of type 2 diabetes. Additionally, certain psychosocial measures (i.e., the Center for Epidemiologic Studies Depression scale) could not be analyzed due to the amount of missing data (i.e., 86%). However, additional adjustment for several occupational and home stress-related measures, which were missing between 10-14% of the population, did not change the interpretation of the results. Lastly, only about 29% of the population was included in the secondary analyses examining chronic weight dissatisfaction. However, statistically significantly increased diabetes HR among those who were chronically weight dissatisfied compared to those who stayed satisfied were still observed, even with the reduced sample size.
Findings from this study provide important insights for future behavior change interventions for chronic disease prevention. Despite prior studies suggesting that weight dissatisfaction might be a motivator for healthy behavior changes (Kuk, et al., 2009; Lemon, Rosal, Zapka, Borg, & Andersen, 2009; Yaemsiri, et al., 2011); weight dissatisfaction may actually preclude engagement in positive health behaviors. Weight dissatisfaction may be a marker of higher chronic disease risk, independent of other predictors and measurement of this construct could be used to refine targeting of intervention efforts. Furthermore, the emphasis on weight loss in many health promotion programs for chronic disease prevention may not include messages that are salient to those with weight dissatisfaction. Other motivators, that we were unable to assess, such as having more energy, better job performance, or increased happiness, may be more salient motivators for adoption and maintenance of healthy behaviors that have an impact on chronic disease risk in this population. Future studies should focus on understanding what motivates those who are dissatisfied with their weight to engage in positive health behaviors that lead to reductions in chronic disease risk.
This study demonstrated that greater dissatisfaction with one's weight may be indicative of less healthy diet and physical activity behaviors and reflective of higher type 2 diabetes risk compared to counterparts with similar BMI. Longitudinal studies that examine these relationships in other populations at higher risk of type 2 diabetes would greatly improve our ability to develop effective intervention strategies. Weight dissatisfaction provides important insights into relationships between perceptions, behavior, and health that can be used to frame future research and intervention efforts.
Acknowledgments
This study was supported by National Institutes of Health grants AG06945, HL62508, and DK088195. Dr. Wirth's participation was supported through an ASPIRE-II Grant from the University of South Carolina Office of Research and by the South Carolina Cancer Prevention and Control Research Network funded under Cooperative Agreement Number 3U48DP001936-01 from the Centers for Disease Control and Prevention and the National Cancer Institute. Dr. Hébert is supported by an Established Investigator Award in Cancer Prevention and Control from the Cancer Training Branch of the National Cancer Institute (K05 CA136975). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank the Cooper Clinic physicians and technicians for collecting the data and staff at the Cooper Institute for data entry and data management.
Bibliography
- ACSM . American College of Sports Medicine: ACSM's Guidelines for Exercise Testing and Prescription. 7th ed. Lippincott Williams and Wilkins; Philadelphia: 2005. [Google Scholar]
- Ahluwalia N, Andreeva VA, Kesse-Guyot E, Hercberg S. Dietary patterns, inflammation and the metabolic syndrome. Diabetes Metab. 2012 doi: 10.1016/j.diabet.2012.08.007. doi: 10.1016/j.diabet.2012.08.007. [DOI] [PubMed] [Google Scholar]
- Al Sabbah H, Vereecken C, Abdeen Z, Coats E, Maes L. Associations of overweight and of weight dissatisfaction among Palestinian adolescents: findings from the national study of Palestinian schoolchildren (HBSC-WBG2004). J Hum Nutr Diet. 2009;22(1):40–49. doi: 10.1111/j.1365-277X.2008.00901.x. doi: 10.1111/j.1365-277X.2008.00901.x. [DOI] [PubMed] [Google Scholar]
- Arroyo M, Basabe N, Serrano L, Sanchez C, Ansotegui L, Rocandio AM. Prevalence and magnitude of body weight and image dissatisfaction among women in dietetics majors. Arch Latinoam Nutr. 2010;60(2):126–132. [PubMed] [Google Scholar]
- Baliunas DO, Taylor BJ, Irving H, Roerecke M, Patra J, Mohapatra S, Rehm J. Alcohol as a risk factor for type 2 diabetes: A systematic review and meta-analysis. Diabetes Care. 2009;32(11):2123–2132. doi: 10.2337/dc09-0227. doi: 10.2337/dc09-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balke B, Ware RW. An experimental study of physical fitness of Air Force personnel. U S Armed Forces Med J. 1959;10(6):675–688. [PubMed] [Google Scholar]
- Bennett GG, Wolin KY. Satisfied or unaware? Racial differences in perceived weight status. Int J Behav Nutr Phys Act. 2006;3:40. doi: 10.1186/1479-5868-3-40. doi: 1479-5868-3-40 [pii]10.1186/1479-5868-3-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird SR, Hawley JA. Exercise and type 2 diabetes: new prescription for an old problem. Maturitas. 2012;72(4):311–316. doi: 10.1016/j.maturitas.2012.05.015. doi: S0378-5122(12)00199-5 [pii] 10.1016/j.maturitas.2012.05.015. [DOI] [PubMed] [Google Scholar]
- Blair SN, Kohl HW, 3rd, Paffenbarger RS, Jr., Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262(17):2395–2401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- Blake CE, Bisogni CA, Sobal J, Jastran M, Devine CM. How adults construct evening meals. Scripts for food choice. Appetite. 2008;51(3):654–662. doi: 10.1016/j.appet.2008.05.062. doi: 10.1016/j.appet.2008.05.062. [DOI] [PubMed] [Google Scholar]
- Blake CE, Hebert JR, Lee DC, Adams SA, Steck SE, Sui X, Blair SN. Adults with Greater Weight Satisfaction Report More Positive Health Behaviors and Have Better Health Status Regardless of BMI. J Obes. 2013;2013:291371. doi: 10.1155/2013/291371. doi: 10.1155/2013/291371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caballero B. The global epidemic of obesity: an overview. Epidemiol Rev. 2007;29:1–5. doi: 10.1093/epirev/mxm012. doi: 10.1093/epirev/mxm012. [DOI] [PubMed] [Google Scholar]
- Casazza K, Fontaine KR, Astrup A, Birch LL, Brown AW, Bohan Brown MM, Allison DB. Myths, presumptions, and facts about obesity. N Engl J Med. 2013;368(5):446–454. doi: 10.1056/NEJMsa1208051. doi: 10.1056/NEJMsa1208051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connors M, Bisogni CA, Sobal J, Devine CM. Managing values in personal food systems. Appetite. 2001;36(3):189–200. doi: 10.1006/appe.2001.0400. doi: 10.1006/appe.2001.0400. [DOI] [PubMed] [Google Scholar]
- Dacey M, Baltzell A, Zaichkowsky L. Older adults' intrinsic and extrinsic motivation toward physical activity. Am J Health Behav. 2008;32(6):570–582. doi: 10.5555/ajhb.2008.32.6.570. doi: 10.5555/ajhb.2008.32.6.570. [DOI] [PubMed] [Google Scholar]
- Djousse L, Driver JA, Gaziano JM, Buring JE, Lee IM. Association between modifiable lifestyle factors and residual lifetime risk of diabetes. Nutr Metab Cardiovasc Dis. 2013;23(1):17–22. doi: 10.1016/j.numecd.2011.08.002. doi: 10.1016/j.numecd.2011.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorsey RR, Eberhardt MS, Ogden CL. Racial/ethnic differences in weight perception. Obesity (Silver Spring) 2009;17(4):790–795. doi: 10.1038/oby.2008.603. doi: oby2008603 [pii]10.1038/oby.2008.603. [DOI] [PubMed] [Google Scholar]
- Duncan DT, Wolin KY, Scharoun-Lee M, Ding EL, Warner ET, Bennett GG. Does perception equal reality? Weight misperception in relation to weight-related attitudes and behaviors among overweight and obese US adults. Int J Behav Nutr Phys Act. 2011;8:20. doi: 10.1186/1479-5868-8-20. doi: 1479-5868-8-20 [pii] 10.1186/1479-5868-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrester-Knauss C, Zemp Stutz E. Gender differences in disordered eating and weight dissatisfaction in Swiss adults: Which factors matter? BMC Public Health. 2012;12:809. doi: 10.1186/1471-2458-12-809. doi: 1471-2458-12-809 [pii] 10.1186/1471-2458-12-809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Tyszkiewicz M, Skouteris H, McCabe M. A re-examination of the benefits of exercise for state body satisfaction: Consideration of individual difference factors. J Sports Sci. 2012 doi: 10.1080/02640414.2012.746723. doi: 10.1080/02640414.2012.746723. [DOI] [PubMed] [Google Scholar]
- Fung TT, McCullough M, van Dam RM, Hu FB. A prospective study of overall diet quality and risk of type 2 diabetes in women. Diabetes Care. 2007;30(7):1753–1757. doi: 10.2337/dc06-2581. doi: dc06-2581 [pii] 10.2337/dc06-2581. [DOI] [PubMed] [Google Scholar]
- Garber AJ. Obesity and type 2 diabetes: which patients are at risk? Diabetes Obes Metab. 2012;14(5):399–408. doi: 10.1111/j.1463-1326.2011.01536.x. doi: 10.1111/j.1463-1326.2011.01536.x. [DOI] [PubMed] [Google Scholar]
- Garber AK, Boyer CB, Pollack LM, Chang YJ, Shafer MA. Body mass index and disordered eating behaviors are associated with weight dissatisfaction in adolescent and young adult female military recruits. Mil Med. 2008;173(2):138–145. doi: 10.7205/milmed.173.2.138. [DOI] [PubMed] [Google Scholar]
- Halliwell E, Dittmar H, Orsborn A. The effects of exposure to muscular male models among men: exploring the moderating role of gym use and exercise motivation. Body Image. 2007;4(3):278–287. doi: 10.1016/j.bodyim.2007.04.006. doi: 10.1016/j.bodyim.2007.04.006. [DOI] [PubMed] [Google Scholar]
- Haslam DW, James WP. Obesity. Lancet. 2005;366(9492):1197–1209. doi: 10.1016/S0140-6736(05)67483-1. doi: S0140-6736(05)67483-1 [pii] 10.1016/S0140-6736(05)67483-1. [DOI] [PubMed] [Google Scholar]
- Hendley Y, Zhao L, Coverson DL, Din-Dzietham R, Morris A, Quyyumi AA, Vaccarino V. Differences in weight perception among blacks and whites. J Womens Health (Larchmt) 2011;20(12):1805–1811. doi: 10.1089/jwh.2010.2262. doi: 10.1089/jwh.2010.2262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huerta JM, Tormo MJ, Chirlaque MD, Gavrila D, Amiano P, Arriola L, Navarro C. Risk of type 2 diabetes according to traditional and emerging anthropometric indices in Spain, a Mediterranean country with high prevalence of obesity: results from a large-scale prospective cohort study. BMC Endocr Disord. 2013;13:7. doi: 10.1186/1472-6823-13-7. doi: 1472-6823-13-7 [pii] 10.1186/1472-6823-13-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keel PK, Baxter MG, Heatherton TF, Joiner TE., Jr. A 20-year longitudinal study of body weight, dieting, and eating disorder symptoms. J Abnorm Psychol. 2007;116(2):422–432. doi: 10.1037/0021-843X.116.2.422. doi: 2007-06673-017 [pii] 10.1037/0021-843X.116.2.422. [DOI] [PubMed] [Google Scholar]
- Kim MJ, Lim YR, Kwak HK. Dietary behaviors and body image recognition of college students according to the self-rated health condition. Nutr Res Pract. 2008;2(2):107–113. doi: 10.4162/nrp.2008.2.2.107. doi: 10.4162/nrp.2008.2.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodama S, Horikawa C, Fujihara K, Heianza Y, Hirasawa R, Yachi Y, Sone H. Comparisons of the strength of associations with future type 2 diabetes risk among anthropometric obesity indicators, including waist-to-height ratio: a meta-analysis. Am J Epidemiol. 2012;176(11):959–969. doi: 10.1093/aje/kws172. doi: kws172 [pii] 10.1093/aje/kws172. [DOI] [PubMed] [Google Scholar]
- Korn L, Gonen E, Shaked Y, Golan M. Health Perceptions, Self and Body Image, Physical Activity and Nutrition among Undergraduate Students in Israel. PLoS One. 2013;8(3):e58543. doi: 10.1371/journal.pone.0058543. doi: 10.1371/journal.pone.0058543 PONE-D-12-31123 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreutz G. Does partnered dance promote health? The case of tango Argentino. J R Soc Promot Health. 2008;128(2):79–84. doi: 10.1177/1466424007087805. [DOI] [PubMed] [Google Scholar]
- Kuk JL, Ardern CI, Church TS, Hebert JR, Sui X, Blair SN. Ideal weight and weight satisfaction: association with health practices. Am J Epidemiol. 2009;170(4):456–463. doi: 10.1093/aje/kwp135. doi: kwp135 [pii] 10.1093/aje/kwp135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavie CJ, Church TS, Milani RV, Earnest CP. Impact of physical activity, cardiorespiratory fitness, and exercise training on markers of inflammation. J Cardiopulm Rehabil Prev. 2011;31(3):137–145. doi: 10.1097/HCR.0b013e3182122827. doi: 10.1097/HCR.0b013e3182122827. [DOI] [PubMed] [Google Scholar]
- Lazarou C, Panagiotakos D, Matalas AL. The role of diet in prevention and management of type 2 diabetes: implications for public health. Crit Rev Food Sci Nutr. 2012;52(5):382–389. doi: 10.1080/10408398.2010.500258. doi: 10.1080/10408398.2010.500258. [DOI] [PubMed] [Google Scholar]
- Lee DC, Sui X, Church TS, Lavie CJ, Jackson AS, Blair SN. Changes in fitness and fatness on the development of cardiovascular disease risk factors hypertension, metabolic syndrome, and hypercholesterolemia. J Am Coll Cardiol. 2012;59(7):665–672. doi: 10.1016/j.jacc.2011.11.013. doi: 10.1016/j.jacc.2011.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemon SC, Rosal MC, Zapka J, Borg A, Andersen V. Contributions of weight perceptions to weight loss attempts: differences by body mass index and gender. Body Image. 2009;6(2):90–96. doi: 10.1016/j.bodyim.2008.11.004. doi: S1740-1445(08)00130-7 [pii] 10.1016/j.bodyim.2008.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthiasdottir E, Jonsson SH, Kristjansson AL. Body weight dissatisfaction in the Icelandic adult population: a normative discontent? Eur J Public Health. 2012;22(1):116–121. doi: 10.1093/eurpub/ckq178. doi: ckq178 [pii] 10.1093/eurpub/ckq178. [DOI] [PubMed] [Google Scholar]
- Minsky S, Vreeland B, Miller M, Gara M. Concordance between measured and self-perceived weight status of persons with serious mental illness. Psychiatr Serv. 2013;64(1):91–93. doi: 10.1176/appi.ps.201100515. doi: 1487315 [pii] 10.1176/appi.ps.201100515. [DOI] [PubMed] [Google Scholar]
- NDIC. Centers for Disease Control and Prevention . National Diabetes Fact Sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2011. [Google Scholar]
- Niskar A, Baron-Epel O, Garty-Sandalon N, Keinan-Boker L. Body weight dissatisfaction among Israeli Jewish and Arab women with normal or overweight-obese body mass index, Israeli INHIS-1, 2003-2004. Prev Chronic Dis. 2009;6(2):A51. doi: A51 [pii] [PMC free article] [PubMed] [Google Scholar]
- Nolan CJ, Damm P, Prentki M. Type 2 diabetes across generations: from pathophysiology to prevention and management. Lancet. 2011;378(9786):169–181. doi: 10.1016/S0140-6736(11)60614-4. doi: S0140-6736(11)60614-4 [pii] 10.1016/S0140-6736(11)60614-4. [DOI] [PubMed] [Google Scholar]
- Noor SZ, Lua PL, Nik MM. Body weight satisfaction: association with weight control practices among type 2 diabetic patients. Malays J Nutr. 2011;17(1):55–66. [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. doi: 295/13/1549 [pii] 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Padgett J, Biro FM. Different shapes in different cultures: body dissatisfaction, overweight, and obesity in African-American and caucasian females. J Pediatr Adolesc Gynecol. 2003;16(6):349–354. doi: 10.1016/j.jpag.2003.09.007. doi: S1083318803001918 [pii] [DOI] [PubMed] [Google Scholar]
- Pednekar MS, Gupta PC, Hebert JR, Hakama M. Joint effects of tobacco use and body mass on all-cause mortality in Mumbai, India: results from a population-based cohort study. Am J Epidemiol. 2008;167(3):330–340. doi: 10.1093/aje/kwm293. doi: 10.1093/aje/kwm293. [DOI] [PubMed] [Google Scholar]
- Peel JB, Sui X, Matthews CE, Adams SA, Hebert JR, Hardin JW, Blair SN. Cardiorespiratory fitness and digestive cancer mortality: findings from the aerobics center longitudinal study. Cancer Epidemiol Biomarkers Prev. 2009;18(4):1111–1117. doi: 10.1158/1055-9965.EPI-08-0846. doi: 1055-9965.EPI-08-0846 [pii] 10.1158/1055-9965.EPI-08-0846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollock ML, Bohannon RL, Cooper KH, Ayres JJ, Ward A, White SR, Linnerud AC. A comparative analysis of four protocols for maximal treadmill stress testing. Am Heart J. 1976;92(1):39–46. doi: 10.1016/s0002-8703(76)80401-2. [DOI] [PubMed] [Google Scholar]
- Pollock ML, Foster C, Schmidt D, Hellman C, Linnerud AC, Ward A. Comparative analysis of physiologic responses to three different maximal graded exercise test protocols in healthy women. Am Heart J. 1982;103(3):363–373. doi: 10.1016/0002-8703(82)90275-7. doi: 0002-8703(82)90275-7 [pii] [DOI] [PubMed] [Google Scholar]
- Prasad S, Sung B, Aggarwal BB. Age-associated chronic diseases require age-old medicine: role of chronic inflammation. Prev Med. 2012;54(Suppl):S29–37. doi: 10.1016/j.ypmed.2011.11.011. doi: 10.1016/j.ypmed.2011.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psaltopoulou T, Ilias I, Alevizaki M. The role of diet and lifestyle in primary, secondary, and tertiary diabetes prevention: a review of meta-analyses. Rev Diabet Stud. 2010;7(1):26–35. doi: 10.1900/RDS.2010.7.26. doi: 10.1900/RDS.2010.7.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satia JA, Galanko JA, Siega-Riz AM. Eating at fast-food restaurants is associated with dietary intake, demographic, psychosocial and behavioural factors among African Americans in North Carolina. Public Health Nutr. 2004;7(8):1089–1096. doi: 10.1079/PHN2004662. doi: 10.1079/PHN2004662 S1368980004001405 [pii] [DOI] [PubMed] [Google Scholar]
- Schmalz DL, Deane GD, Birch LL, Davison KK. A longitudinal assessment of the links between physical activity and self-esteem in early adolescent non-Hispanic females. J Adolesc Health. 2007;41(6):559–565. doi: 10.1016/j.jadohealth.2007.07.001. doi: 10.1016/j.jadohealth.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherwin R, Jastreboff AM. Year in diabetes 2012: The diabetes tsunami. J Clin Endocrinol Metab. 2012;97(12):4293–4301. doi: 10.1210/jc.2012-3487. doi: jc.2012-3487 [pii] 10.1210/jc.2012-3487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JK. The (mis)measurement of body image: ten strategies to improve assessment for applied and research purposes. Body Image. 2004;1(1):7–14. doi: 10.1016/S1740-1445(03)00004-4. doi: 10.1016/S1740-1445(03)00004-4. [DOI] [PubMed] [Google Scholar]
- van Dam RM, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Dietary patterns and risk for type 2 diabetes mellitus in U.S. men. Ann Intern Med. 2002;136(3):201–209. doi: 10.7326/0003-4819-136-3-200202050-00008. doi: 200202050-00008 [pii] [DOI] [PubMed] [Google Scholar]
- von Lengerke T, Mielck A. Body weight dissatisfaction by socioeconomic status among obese, preobese and normal weight women and men: results of the cross-sectional KORA Augsburg S4 population survey. BMC Public Health. 2012;12:342. doi: 10.1186/1471-2458-12-342. doi: 1471-2458-12-342 [pii] 10.1186/1471-2458-12-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1(1):11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- WHO. World Health Organization diabetes fact sheet. 2011 http://www.who.int/mediacentre/factsheets/fs312/en/index.html.
- Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2007;298(22):2654–2664. doi: 10.1001/jama.298.22.2654. doi: 10.1001/jama.298.22.2654. [DOI] [PubMed] [Google Scholar]
- Yaemsiri S, Slining MM, Agarwal SK. Perceived weight status, overweight diagnosis, and weight control among US adults: the NHANES 2003-2008 Study. Int J Obes (Lond) 2011;35(8):1063–1070. doi: 10.1038/ijo.2010.229. doi: ijo2010229 [pii] 10.1038/ijo.2010.229. [DOI] [PubMed] [Google Scholar]
- Yap TL, Davis LS. Physical activity: the science of health promotion through tailored messages. Rehabil Nurs. 2008;33(2):55–62. doi: 10.1002/j.2048-7940.2008.tb00204.x. [DOI] [PubMed] [Google Scholar]