Abstract
Objective
Cocaine users often present to treatment with a multitude of problems typically considered ‘addiction-related’, however there is little evidence that reductions in cocaine use are followed by reductions in these problems. This study evaluated the relationship between rates of cocaine use during treatment and the level of non-cocaine life problems experienced during a 12-month period following treatment in a pooled sample of 434 cocaine dependent individuals participating in one of five randomized controlled trials.
Method
Structural equation modeling (SEM), and latent growth curve modeling (LGCM) were used to evaluate the relationship between frequency of cocaine use within treatment (8- or 12-weeks) and a latent construct of ‘global problems’ indicated by the days of problems reported on the Addiction Severity Index (ASI) across follow-up time points (1-, 3-, 6-, and 12-months after treatment).
Results
Both a continuous latent cocaine use outcome measure (percent days abstinent, percent positive urines, and maximum days of consecutive abstinence) and a dichotomous measure of cocaine use (≥21 consecutive days of abstinence) during the treatment period were associated with frequency of cocaine use and global problems during follow-up. Overall, results indicated greater cocaine abstinence during the treatment period was associated with higher rates of abstinence and fewer global problems experienced following treatment.
Conclusion
This is one of the first studies to support a model that suggests ‘addiction-related’ problems decrease in accordance with achieving abstinence from cocaine, thereby providing evidence that within-treatment cocaine abstinence has benefits that extend beyond the frequency of drug use.
Keywords: cocaine use, addiction-related problems, treatment outcomes, follow-up, structural equation modeling
Substance users present for treatment with a multitude of problems in various life areas, including employment, physical health, legal, family, social, and psychological function. Problems in these areas are often the reasons for initial referral or re-entry to addiction treatment (Grella, Hser, & Hsieh, 2003), important for determining the setting and content of care (American Society of Addiction Medicine, 2007), and typically the major reasons for relapse to substance use following initial care (Hall et al., 1998; Marlatt & Gordon, 1980; McLellan et al., 1994; McLellan, Luborsky, Woody, O’Brien, & Druley 1983; McMahon, 2001). Such problems are generally considered “addiction-related,” and thus evaluated as part of most clinical and research assessment protocols, yet they are rarely deemed primary measures of treatment success. While the aim of treatment is often expressed as an effort to modify patients’ drug use behavior, improvement in psychosocial functioning is also the desired effect, as minimal change in drug use behavior without an impact on the psychosocial consequences “would be pointless” (Winchell, Rappaport, Roca, & Rosebraugh, 2012). Although there has been an implicit assumption that resolution of the primary substance use problem would produce improved functioning in other areas, this long held assumption has not been empirically confirmed.
Early evidence refuting the assumption that abstinence from alcohol or drug use would result in general improvement in other life areas appeared in a landmark paper by McLellan and colleagues (1981). They found that although significant reductions in problem severity were evident in the areas of employment, family, legal, psychological function, and drug and alcohol use following treatment, there was virtually no relationship between improvement in substance use and these other areas, with the exception of psychological functioning (McLellan et al., 1981). Specifically, the correlations between change in drug use and change in problem severity for other areas, such as medical, employment, and family domains were strikingly low (e.g., r = −.03, .01, .09, respectively) (McLellan et al., 1981). This early work supported the use of a multidimensional assessment of substance use treatment outcome (McLellan, Luborsky, Woody, & O’Brien, 1980). Subsequent studies have provided further support that these problem areas were relatively independent and weakly related to reductions in substance use (Borders et al., 2009; Kosten et al., 1992; Kosten, Rounsaville, & Kleber, 1987; Rounsaville, Tierney, Crits-Christoph, Weissman, & Kleber, 1982). On the other hand, some studies have reported improvements in psychosocial functioning were associated with drug abstinence: Rounsaville, Kosten, and Kleber (1987) found that among opioid dependent patients re-interviewed 2 ½ years after treatment, achieving abstinence from illicit opioids was associated with improvement in medical status and social functioning, as well as reduced criminal activity and abuse of other substances. A subsequent evaluation of these data found that those opioid dependent patients who increased their frequency of cocaine use had more severe problems on a wide range of dimensions than those who decreased use, with attainment of cocaine abstinence associated with improved psychosocial functioning (Kosten, Rounsaville, & Kleber, 1988). However, there is relatively little evidence that meaningful improvements in functioning are associated with reductions in cocaine use among cocaine-dependent individuals, nor strong evidence that better cocaine use outcomes are associated with better functioning after treatment ends.
Although several studies point to significant effects of behavioral therapies on increasing abstinence (see Dutra et al., 2008), in many studies these effects did not appear to extend to other problem areas, such as medical, legal, employment, family/social, or psychological. Whereas the field of alcohol treatment research has reported that within-treatment outcome measures such as greater abstinence rates and/or decreased percentage of heavy-drinking-days are associated with fewer drinking-related consequences at follow-up (Falk et al., 2010), there is little evidence of such associations among treated cocaine users. Improved psychosocial outcomes have been reported following cocaine treatment in general (Carroll et al., 1994; Crits-Christoph et al., 2001; Higgins, Wong, Badger, Haug-Ogden, & Dantona, 2000; Simpson, Joe, Fletcher, Hubbard, & Anglin, 1999), yet there are very few reports on associations between periods of cocaine abstinence during treatment and decreased problems at follow-up. Empirical evidence supporting such an association would be important to validate the patterns of within-treatment drug use behavior as a surrogate for clinical benefit, as the reduction in ‘addiction-related’ problems are often not evident during a short-term treatment period (McLellan, McKay, Forman, Cacciola, & Kemp, 2005). Furthermore, in the absence of complete drug abstinence, identification of patterns of drug abuse within treatment that are consistent with ‘good functioning’ in the long term would be useful for establishing markers of treatment effectiveness (Winchell et al., 2012).
A recent study by Ghitza and colleagues (2007) retrospectively analyzed data from two 25-week randomized controlled trials of abstinence reinforcement (i.e., contingency management) in 368 cocaine/heroin users maintained on methadone and found greater cocaine use during treatment (measured by urine toxicology) was associated with worse social adjustment, current cocaine dependence, and depression at study exit. Although this study did not examine medical or legal problems, it was one of the few direct tests supporting the association between the frequency of cocaine use and other psychosocial outcome variables, such as social functioning and depression, within treatment. Studies evaluating these relationships among cocaine users who are not maintained on methadone (and hence likely to be primary opioid users) are sparse, and fewer still have evaluated whether this association holds up during the months following treatment (i.e., does reduced cocaine use during treatment have long-term effects on other areas of functioning?).
To address these issues, the current study sought to evaluate the relationship between in-treatment cocaine use and problems in major life areas other than drug use (e.g., medical, legal, employment, family/social, psychological) within and following treatment. To enhance generalizability and power, this study used data collected from five independent, completed randomized controlled trials evaluating treatments for cocaine dependence. We hypothesized that, regardless of treatment received, greater periods of abstinence from cocaine (e.g., longer durations of consecutive abstinence, higher percentage of days abstinent) during the treatment period would be associated with better outcomes during the period following treatment (i.e., fewer problems in major life areas).
Methods
Overview
Data for this study were gathered from five independent randomized controlled trials evaluating behavioral (e.g., cognitive behavioral therapy [CBT], twelve-step facilitation [TSF], interpersonal therapy [IPT], contingency management [CM]) and pharmacologic (e.g., disulfiram) treatments for cocaine dependence in different populations (e.g., outpatient, methadone maintenance). The five studies were:
Study # 1
12-week trial evaluating five treatment arms (CBT plus disulfiram; TSF plus disulfiram; CBT alone; TSF alone; disulfiram plus clinical management) for ambulatory cocaine-dependent individuals with comorbid alcohol abuse or dependence (Carroll, Nich, Ball, McCance-Katz, & Rounsaville, 1998; Carroll et al., 2000);
Study # 2
12-week trial evaluating four treatment arms (CBT plus disulfiram; CBT plus placebo; IPT plus disulfiram; IPT plus placebo) in a general outpatient sample of cocaine-dependent individuals (Carroll et al., 2004);
Study # 3
12-week trial evaluating four treatment arms (TSF plus disulfiram; TSF plus placebo; disulfiram plus standard counseling; placebo plus standard counseling) in sample of cocaine-dependent individuals also receiving methadone maintenance therapy for opiate dependence (Carroll, Nich, Shi, Eagan, & Ball, 2012);
Study # 4
12-week trial evaluating four treatment arms (Disulfiram plus CM; Disulfiram alone; placebo plus CM; placebo alone) in a general outpatient sample of cocaine dependent individuals. Participants in each of the four treatment arms also received weekly individual cognitive behavioral therapy (Carroll, Petry, Eagan, Shi, & Ball, 2013).
Study # 5
8-week trial evaluating the effectiveness of a computer-delivered version of cognitive behavioral therapy (CBT4CBT) as an adjunct to treatment as usual in a general outpatient sample of substance users (Carroll et al., 2008; Carroll et al., 2009);
Participants
The sample size of participants randomized to a treatment condition in each trial were as follows: Study #1 (N = 117), Study #2 (N = 121), Study #3 (N = 112), Study #4 (N = 99), and Study #5 (N = 73). It should be noted that one trial (Study #5) included a general outpatient sample of substance users, and only the subgroup who reported cocaine as their primary substance of abuse (n = 43) were included here. Participants in all trials: (1) were 18 years of age or older, (2) met criteria for current cocaine dependence according to Diagnostic and Statistical Manual – fourth edition (DSM-IV; American Psychiatric Association, 1994) [DSM-III-R for Study #1; current substance dependence for Study #5], (3) did not meet DSM criteria for a lifetime psychotic or bipolar disorder, and (4) were not physically dependent on alcohol, such that detoxification was necessary.
Assessments
Each of the five trials included an identical assessment schedule, with assessments administered prior to treatment initiation, weekly and monthly during the treatment period, at the end-of-treatment, and at several follow-up time points. The follow-up assessments occurred at 1, 3, 6, and 12-months post-treatment, with the exception of Study #5 (‘CBT4CBT study’), which included only a 1-, 3- and 6-month follow-up assessment. All trials used a brief version of the Addiction Severity Index (ASI; McLellan et al., 1992), which was utilized for analysis in the current study. The ASI is one of the most commonly used interview-based assessments in the field of substance use disorders for measuring the severity of problems in several non-drug using domains, such as medical, employment, legal, family and social relationships, and psychiatric. In terms of substance use, each trial utilized a Substance Use Calendar (Carroll et al., 2004), similar to the reliable and valid Timeline Follow Back (Fals-Stewart, O’Farrell, Freitas, McFarlin, & Rutigliano, 2000; Hjorthøj, Hjorthøj, & Nordentoft, 2012; Sobell & Sobell, 1992) for self-reported cocaine use, as well as urine toxicology screens at each research visit. The frequency of urine toxicology screens varied across study depending on the setting, with once per week toxicology screens in Study #2 (general outpatient setting), up to three times per week in Study #3 (outpatient methadone maintenance setting). The substance use calendar allowed the collection of information on cocaine use on a day-by-day basis, as well as to ‘back fill’ missing data in case participants missed an assessment appointment, and thus provided a highly detailed and sensitive index of change in cocaine use and periods of abstinence (Donovan et al., 2012).
Data Analysis
Statistical models, described below, were estimated using Mplus version 7 (Muthen & Muthen, 2012). Given that participants were drawn from five different studies, we first assessed the effect of “study” on all outcomes. Intraclass correlations (ICC) for all outcome measures were calculated to determine the degree of dependence between participants within studies. Results indicated that ICCs were near zero for all outcomes (range = 0.000 – 0.001), suggesting that most of the variance was not explained by clustering within studies. Nonetheless we took into account the clustering of participants within studies by estimating all parameters using a weighted maximum likelihood function with the standard errors computed using a sandwich estimator (e.g., standard errors were adjusted for clustering in the data). Maximum likelihood estimation provides the estimated variance-covariance matrix for the available data and therefore all available data were included in the models.
The first step in the current analyses was to define the constructs in the model. Because there is little consistency within the cocaine treatment literature regarding a well-established common outcome measure (Donovan et al., 2012), we evaluated several indicators of cocaine use during the treatment period in order to define the ‘within-treatment cocaine use’ construct. Thus, this construct initially consisted of 11 different indicators that included both dichotomous and continuous indicators commonly reported in the cocaine treatment literature (Carroll et al., in press; Donovan et al., 2012; Dutra et al., 2008; McKay et al., 2001). Separate models were constructed for each of the within-treatment cocaine use indicators in order to determine which indicators had the strongest and most consistent relationship with cocaine use during the follow-up period across studies. The ‘follow-up cocaine use’ construct in these models was indicated by the mean days of cocaine use during the prior 28 at each of the expected follow-up assessment points. We then evaluated the strongest continuous outcome measures as a latent construct of ‘within-treatment cocaine use’ in a confirmatory factor model.
To evaluate the effect of within-treatment cocaine use on the change in global problems over time, we used latent growth curve (LGC) modeling. First, in order to examine global problems at each time point, we used longitudinal confirmatory factor analysis to create a latent measure of ‘global problems’ at each follow-up time point and to evaluate the equivalence of the ASI problem subscales over time. Due to some limitations regarding the ASI composite scores, particularly with respect to the subjective nature of respondents’ rating of severity or need for treatment (Alterman, Brown, Zaballero, & McKay, 1994; Brown, Seraganian, & Shields, 1999; Melberg, 2004; Wertz, Cleaveland, & Stephens, 1995), we chose to use the respondents’ report of the number of days in the past 28 that s/he experienced problems in that given area as the indicators of global problems. Second, we examined whether the factor structure was metric invariant over time by comparing a model with all item loadings and intercepts constrained to be equal at each time point to an unconstrained model with item loadings and intercepts freely estimated at each time point. Next, unconditional latent growth curve modeling was used to examine the changes in global problems over time. Finally, conditional latent growth curve modeling was used to examine the association between within-treatment cocaine use and follow-up levels of global problems over time controlling for baseline problems.
Results
Participants
Table 1 provides an overview of sample composition across studies. All trials included follow-up data on at least 80% of the randomized sample, with Study #1 as the exception (78%), with samples sizes of 91, 108, 112, 85, and 38 for the five trials, respectively. Overall, the pooled sample (N=434) was composed primarily of individuals who were male (67%), Caucasian (52%), not married/cohabitating (71%), unemployed (53%), with at least a high school degree/GED (78%). The average age was 36.5 years old, and few were on probation or parole at the time of treatment entry (15%). Mean days of cocaine use during the 28 days prior to treatment entry was 13.4 (SD=8.5).
Table 1.
Overview of trials included in analysis
| Participant Characteristics | Study #1 | Study #2 | Study #3 | Study #4 | Study #5 |
|---|---|---|---|---|---|
| Type of Treatment | CBT/Disulfiram TSF/Disulfiram CBT Only TSF Only DIS/Clin Mgmt |
CBT/DIS CBT/Placebo IPT/Disulfiram IPT/Placebo |
TSF/Disulfiram TSF/Placebo Disulfiram/TAU Placebo/TAU |
Disulfiram/CM Disulfiram Placebo/CM Placebo |
CBT4CBT/TAU TAU |
| Length of Study (Weeks) | 12 | 12 | 12 | 12 | 8 |
| Follow-up sample (N) | 91 | 108 | 112 | 85 | 38 |
| Percentage of Randomized Participants | |||||
| Reached for Follow-up (%) | 78 | 89 | 100 | 86 | 88 |
| Female (%) | 29 | 26 | 41 | 31 | 47 |
| Minority (%) | 57 | 35 | 36 | 60 | 76 |
| White (%) | 43 | 65 | 64 | 40 | 24 |
| African American (%) | 52 | 29 | 22 | 49 | 60 |
| Hispanic (%) | 3 | 6 | 14 | 6 | 13 |
| Other (%) | 2 | 0 | 0 | 5 | 3 |
| Unemployed (%) | 55 | 57 | 46 | 69 | 21 |
| Criminal justice referred (%) | 24 | 22 | 2 | 5 | 42 |
| Baseline days of cocaine use during past 28 - Mean (sd) | 13.6 (8.1) | 12.7 (8.5) | 15.5 (8.8) | 13.7 (7.8) | 7.8 (8.0) |
| FU1 Days of cocaine use during past 28 - Mean (sd) | 7.6 (8.5) | 5.5 (7.5) | 5.3 (7.4) | 4.2 (6.8) | 3.0 (5.6) |
| FU2 Days of cocaine use during past 28 – Mean (sd) | 7.6 (8.5) | 4.8 (6.9) | 6.0 (9.0) | 2.8 (6.2) | 2.5 (5.3) |
| FU3 Days of cocaine use during past 28 – Mean (sd) | 6.3 (8.0) | 5.8 (8.0) | 5.2 (7.7) | 3.6 (7.5) | 3.9 (6.5) |
NOTE: CBT = Cognitive Behavioral Therapy; TSF = Twelve-Step Facilitation; DIS = Disulfiram; Clin Mgmt = Clinical Management; IPT = Interpersonal Therapy; TAU = Treatment As Usual; CM = Contingency Management; CBT4CBT = Computer Based Training for Cognitive Behavioral Therapy; FU1 = Follow-up 1 (1-month post-treatment); FU2 = Follow-up 2 (3-months post-treatment); FU3 = Follow-up 3 (6-months post-treatment);
Continuous and Dichotomous Indicators
Results of the SEMs to evaluate the relationship between indicators of within-treatment cocaine use and follow-up cocaine use are displayed in Table 2. As expected, the continuous outcome variables were more strongly related to follow-up cocaine use than the dichotomous outcome variables. The continuous indicators with the consistently strongest standardized correlation across the five studies were ‘percent days abstinent’ (β ranged from −.25 to −.83), ‘maximum days of consecutive abstinence’ (β ranged from −.38 to −.52), and ‘percent cocaine positive urines’ (β ranged from .33 to .53). The confirmatory factor model with these three indicators was just identified (χ2 (0) = 0.00, p = 1.00; RMSEA = 0.00; CFI = 1.00) with factor loadings that exceeded .70 for all three indicators, and hence was deemed appropriate for use as a latent construct of ‘within-treatment cocaine use’ in the subsequent longitudinal models. Also, these three indicators of ‘within-treatment cocaine use’ had good internal consistency (Cronbach’s alpha = .83).
Table 2.
Standardized correlations of within-treatment cocaine use indicators and post-treatment days of cocaine use from SEM
| Within-treatment indicators | Mean Days of Cocaine Use During 12-month Follow-Up
|
||||
|---|---|---|---|---|---|
| Study #1 | Study #2 | Study #3 | Study #4 | Study #5 | |
| Dichotomous indicators | |||||
| ≥ 7 consecutive days of abstinence | −.07 | −.40 | −.38 | −.45 | −.50 |
| ≥ 14 consecutive days of abstinence | −.24 | −.37 | −.30 | −.63 | −.54 |
| ≥ 21 consecutive days of abstinence | −.30 | −.41 | −.34 | −.58 | −.56 |
| Abstinence during entire treatment period | −.01 | −.18 | −.19 | −.69 | −.24 |
| Abstinent during last 2 weeks of treatment | −.32 | −.34 | −.35 | −.34 | −.42 |
| ≥ 50% reduction in cocaine use | .13 | −.15 | .06 | .01 | −.15 |
| ≥ 75% reduction in cocaine use | .12 | −.20 | −.02 | .18 | −.16 |
| Continuous indicators | |||||
| Percent days abstinent | −.25 | −.67 | −.60 | −.83 | −.68 |
| Maximum days of consecutive abstinence | −.38 | −.44 | −.40 | −.52 | −.41 |
| Percentage of positive urine samples | .33 | .35 | .43 | .53 | .48 |
| Percent reduction in cocaine use | −.21 | −.54 | −.33 | wnc | −.26 |
Wnc = would not converge
The dichotomous indicator with the strongest standardized correlation with the follow-up days of cocaine use across studies was ‘≥21 consecutive days of abstinence’ (β ranged from −.30 to −.58). This dichotomous indicator was chosen for use in a separate longitudinal model to provide a clinically useful predictor of post-treatment functioning, as it outperformed the shorter durations of abstinence in terms of association with follow-up cocaine use here and its specificity/sensitivity to treatment effects in a separate evaluation of these data (Nich et al., 2013).
Within-Treatment Cocaine Use and Change in Global Problems
Results of longitudinal confirmatory factor analysis (LCFA) used to create a latent measure of global problems at each follow-up time point and to evaluate the equivalence of the ASI problems subscales over time revealed that at all time points the global problems latent factor provided an adequate fit to the data (1-month follow-up: χ2 (9) = 15.09, p = 0.09; RMSEA = 0.04; 3-month follow-up: χ2 (9) = 22.39, p = 0.01; RMSEA = 0.06; 6-month follow-up: χ2 (9) = 13.10, p = 0.16; RMSEA = 0.03; and 12-month follow-up: χ2 (9) = 14.91, p = 0.09; RMSEA = 0.04). Also, the model with loadings and intercepts constrained to equality did not fit significantly worse than the unconstrained model based on a χ2 difference test (Δχ2 (Δdf = 33) = 44.1, p = 0.09), indicating the factor structure was metrically invariant over time. Results of unconditional latent growth curve modeling used to examine the changes in global problems over time, revealed the global problems model, which included the global problems latent factor models at each follow-up time point, with a linear slope, provided an adequate fit to the observed data based on the CFI = 0.94 and RMSEA = 0.04 (90% CI of RMSEA: 0.03–0.04). The slope of problems was non-significant (linear slope B (SE) = −0.09 (0.09), p = 0.29), suggesting minimal changes in levels of global problems across the follow-up period.
Finally, conditional latent growth curve modeling was used to examine the association between within-treatment cocaine use and follow-up global problems over time using a continuous latent measure of cocaine use during treatment (described above) and a dichotomous measure of ≥21 days of abstinence from cocaine during treatment. In both models we controlled for baseline global problems and follow-up cocaine use (mean self-reported days of cocaine use during the prior 28 days at each of the expected follow-up assessment points).
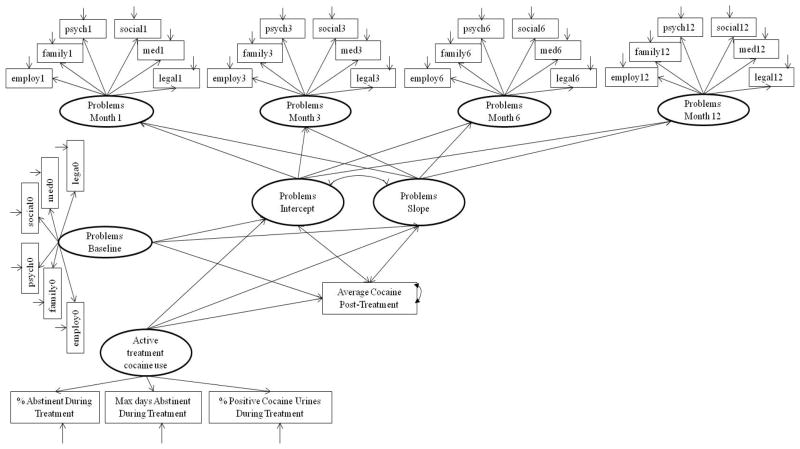
The model of latent within-treatment cocaine use (including percent days abstinent, percent positive cocaine urines, and maximum consecutive days of abstinence), revealed the latent growth model with covariates (see Figure 1) provided an adequate fit to the data based on the CFI = 0.92 and RMSEA = 0.03 (90% CI of RMSEA: 0.02–0.04). Results indicated that the latent measure of cocaine use during treatment was significantly associated with levels of cocaine use during follow-up (β = −0.43; B(SE) = −0.12 (0.007), p < 0.001) and the intercept of global problems at follow-up (β = −0.17; B (SE) = −0.01 (0.003), p = 0.002), such that less within-treatment cocaine use (i.e., greater percent days abstinent, fewer positive urines, more days of consecutive abstinence) was associated with significantly less cocaine use and lower levels of global problems at the initial follow-up time point. Likewise, the intercept of global problems at follow-up was significantly associated with cocaine use (β = 0.32; B (SE) = 0.32 (0.07), p < 0.001), such that more problems were associated with more days of cocaine use (on average) at follow-up. The slope of global problems was significantly associated with baseline problems (β = −0.50; B (SE) = −0.23 (0.11), p = 0.03), but was not associated with the latent measure of within-treatment cocaine use (β = 0.26; B (SE) = 0.01 (0.003), p = 0.06) or follow-up cocaine use (β = −0.18; B (SE) = −0.36 (0.73), p = 0.63). The combination of baseline problems and within-treatment cocaine use explained 52.7% of the variance in the global problems intercept (i.e., initial level of problems at the first follow-up time point) and 32.4% of the variance in the slope (i.e., change in levels of problems during the entire 12-month follow-up period).
Figure 1.
Latent Growth Curve (LGC) evaluating within-treatment cocaine use and change in general functioning problems during the follow-up period
Using ≥21 consecutive days of abstinence from cocaine during treatment as a dichotomous predictor of global problems during follow-up also provided an adequate fit to the data based on the CFI = 0.93 and RMSEA = 0.027 (90% CI of RMSEA: 0.02–0.03). Results indicated that 21 or more days of consecutive abstinence during treatment significantly predicted the average level of follow-up cocaine use (β = −0.36, B (SE) = −4.19 (0.36), p < 0.001) and the intercept of global problems at follow-up (β = −0.20; B (SE) = −0.46 (0.12), p < 0.001). Results were such that continuous abstinence for 21 days or more during treatment was associated with significantly less cocaine use and lower levels of global problems at follow-up. Again, the intercept of global problems at follow-up was significantly associated with average cocaine use during follow-up (β = 0.31; B (SE) = 0.31 (0.10), p = 0.002). The slope of global problems was not significantly associated with baseline problems, within-treatment cocaine use, as measured by 21 days or more of consecutive abstinence, or average cocaine use at follow-up. The combination of baseline problems and within-treatment cocaine use explained 53.6% of the variance in the global problems intercept and 25.5% of the variance in the slope.
Additional analyses were conducted with (1) global problems at end-of-treatment as an additional indicator in the growth model; (2) within-treatment cocaine use examined as a latent growth curve model with global problems at follow-up regressed on the level of cocaine use and change in cocaine use during treatment; and (3) with a negative binomial distribution with log link function used to estimate the global problems latent factors at each time-point. Results were consistent across these additional analyses: within-treatment cocaine use was associated with global problems at the end-of-treatment and during follow-up, regardless of whether using the latent measure of within-treatment cocaine use, the dichotomous indicator of ≥21 days of consecutive abstinence, or a growth model of cocaine use during treatment.
Discussion
This study evaluated the strength of the relationship between within-treatment cocaine use outcomes and both cocaine use and global problems during a 6- to 12-month follow-up period among a pooled sample of 434 cocaine-dependent individuals participating in one of five clinical trials. This pooled sample of individuals had similar demographic and cocaine use characteristics as the population of individuals entering treatment for cocaine use in the United States in 2011 (SAMHSA, 2013). These analyses indicated: (1) both continuous and a dichotomous measure of cocaine use during treatment were strongly associated with cocaine use over a 12-month follow-up period, such that greater rates of abstinence during treatment were associated with less cocaine use during the follow-up; (2) higher rates of cocaine use reported during a 12-month follow-up period were associated with more problems in major life areas (e.g., medical, legal, employment, psychological, family and social conflict) during the same time period; and (3) higher levels of cocaine abstinence (as measured by a continuous latent construct or dichotomous indicator) during treatment were associated with fewer reported problems in major life areas at the end of treatment and during the initial period following treatment, controlling for baseline levels of problems. This latter finding is notable, as there has been little direct evidence that abstinence achieved during treatment is strongly associated with other life problems (i.e., ‘addiction-related problems’), particularly after treatment ends. Despite the lack of change in problem areas over time during the follow-up period (i.e., after treatment termination) and some limitations in the available data from the five trials examined in this study, it appears that greater abstinence achieved during treatment is associated with fewer addiction-related problems after treatment.
Although the rates of co-occurring problems among cocaine users presenting for treatment are relatively high, the effectiveness of a given treatment has typically been measured by its ability to reduce cocaine use. However, merely reducing cocaine use during treatment (which has proven difficult, in its own right), has not been considered sufficient for most patients, treatment providers, payers, and policy-makers, who place a greater emphasis on ‘recovery’ (i.e., positive function in most outcome domains) from drug use disorders (McLellan, Chalk, & Bartlett, 2007). Recently, an editorial comment provided by Winchell and colleagues (2012) from the US Food and Drug Administration (FDA) in response to a ‘responder analysis’ study by McCann and Li (2012), highlighted the need for drug abuse treatment trials, particularly pharmacotherapy trials, to demonstrate some clinical benefits of the abstinence-based measure used to define responders versus non-responders. Specifically, Winchell and colleagues noted a need for data supporting either the health benefits of a given abstinence-based outcome or data supporting that outcome as a predictor of ongoing abstinence, in order to use the responder definition as an endpoint (i.e., establishing a cutoff level of abstinence as a marker of treatment success). The findings presented here provide evidence to support both of these criteria. Both the latent construct (percent days abstinent, percent cocaine positive urines, maximum consecutive days of abstinence) and dichotomous measure (≥ 21 consecutive days of abstinence) of cocaine use during the treatment period were strongly associated with cocaine use following treatment (i.e., ‘ongoing abstinence’). Importantly, both measures of cocaine use were associated with global problems following treatment, with less cocaine use associated with fewer problems (i.e., ‘clinical benefits’). Thus, data from this set of randomized controlled trials provide evidence that levels of within-treatment cocaine abstinence can be used as a valid indicator for defining success from treatment, with benefits that extend beyond merely the frequency of drug use.
These results are valuable for both researchers and clinicians in the field of treatment for cocaine use disorders. For researchers, evidence that standard cocaine use outcome measures, such as the percentage of days abstinent, the maximum number of consecutive days of abstinence, and the percentage of cocaine positive urine toxicology screens, are associated with less cocaine use and fewer global problems following treatment offers some greater validation of these measures as valid outcome indicators for establishing treatment effectiveness in future clinical trials. Furthermore, the dichotomous measure of “≥21 consecutive days of abstinence” may be useful as a benchmark (i.e., primary efficacy endpoint) for future pharmacotherapy clinical trials, as it can serve as a valid surrogate for long-term clinical benefits, which is essential for achieving FDA approval (as there is no currently approved medication for cocaine dependence). The establishment of “no heavy drinking days” as a valid primary efficacy endpoint for alcohol clinical trials was supported by evidence of its association with fewer alcohol-related consequences following treatment (Falk et al., 2010), and thus the similar results presented here offer support for “≥21 consecutive days of abstinence” as a potential benchmark for cocaine pharmacotherapy trials. Such results have implications for clinicians as well, as there is now some support for the implicit assumption that reducing cocaine use has clinical benefits in the long-term, which had not previously been empirically supported. Also, the cutoff of 21 days of consecutive abstinence could be useful as a treatment target with clients, as these results offer evidence of the benefits of such a cutoff. Lastly, because these results were generated from a large, pooled sample fairly representative of the population of individuals entering treatment for cocaine use, the findings are particularly generalizable to the community at large, rather than being limited by homogeneous, high-functioning samples of cocaine users that are common in well-controlled clinical trials.
One potential reason this study was able to find an association between cocaine abstinence and overall functioning in non-drug areas from the ASI, whereas others have not, was the use of a latent construct of ‘global problems’ rather than examining each problem area individually. Cocaine users may have certain areas that are more problematic than others, with many having no problems in some life areas, resulting in negatively skewed data on the non-drug use ASI problem areas. This in turn, affects the likelihood of significant results when examining correlations or mean differences on problem areas according to level of cocaine abstinence. This study also utilized the ‘days of problems’ item from the ASI, whereas most prior studies have examined the composite scores of non-drug use areas, which have shown little relation to the severity of drug dependence (Romelsjo, 2004). By including ‘days of problems’ from all non-drug use ASI areas as indicators of a global latent construct, we may have improved the sensitivity toward finding an effect by increasing the variability in the sample.
The findings of longitudinal growth curve models suggest there was relatively little change overall in the level of problems experienced during the 12-month period following treatment termination. This was not particularly surprising. Although some studies have reported significant reductions in problem severity on the ASI between pre- and post-treatment periods (Crits-Christoph et al., 2001; Vaughan & McMahon, 2006), the effect size of change is considerably larger for the drug- and alcohol-use areas compared to the non-drug areas, with some areas showing little meaningful change (e.g., medical, employment). Moreover, significant reductions are often found within the first few months following entry into treatment, yet tend to level off over the course of longer-term follow-up periods, which suggests maintenance of treatment gains following treatment termination (Guydish et al., 1999). Results from this set of randomized trials provide similar results, suggesting stability of treatment gains with little change in global problems during the 12 months following treatment, which likely limited the association between within-treatment cocaine use and the slope of global problems during the follow-up period. However, even when controlling for the baseline level of problems, the frequency of cocaine use was significantly associated with the global problems construct at the end of treatment and with the intercept of global problems during the follow-up period. Taken together, this indicates the frequency of cocaine use during treatment affects the level of global problems at the end of treatment and through an initial period following treatment (i.e., 1-month follow-up), with gains maintained over the course of a 12-month follow-up period.
The primary strength of this study is the use of a large, pooled sample of participants across five well-controlled randomized trials for cocaine dependence, which used a common assessment approach and included follow-up interviews up to a year after treatment. Structural equation modeling (SEM) allowed for the evaluation of several indicators of problems in major life areas as well as cocaine use, without having to statistically correct for the multiple analyses when using separate regression analyses. Furthermore, we were able to evaluate a latent construct of within-treatment cocaine use that included both self-report and urine toxicology. Also, the use of advanced SEM procedures, such as latent growth curve modeling, allowed for examination of change in global problems over time using all available data, with the ability to relate change in problems to levels of cocaine abstinence achieved during the treatment period.
Despite the strengths, there were some limitations with the available data used in this study. First, the main source of information regarding psychosocial functioning was the subscales of the Addiction Severity Index, which limited the ability to evaluate comprehensive physical health outcomes. That is, although the ASI is well-validated and widely used, the measure still relies on participant self-report, which has its limitations. Second, the trials did not include a ‘quality of life’ or other life satisfaction measure, which could have added an indicator of overall functioning potentially more useful as an outcome of addiction treatment (Miller & Miller, 2009; Tiffany, Friedman, Greenfield, Hasin, & Jackson, 2012). Lastly, our analyses did not include a ‘treatment’ construct in order to evaluate the effect of treatment on cocaine abstinence and global problems. Defining a ‘treatment’ variable in this study was particularly difficult given the range of treatments provided across the five trials, with some including various combinations of behavioral and pharmacotherapy without placebo controls. Although we considered including a ‘retention in treatment’ variable as an indicator of the level of treatment received, we ultimately decided against it because of the misleading assumption regarding the actual number and quality of treatment sessions received solely based on the number of days retained in the treatment study, and it’s poor performance as a clinically meaningful indicator of treatment outcome relative to other measures in these studies (Carroll et al., in press).
Nevertheless, this study provides evidence that the level of cocaine abstinence achieved while in treatment is related to the amount of problems experienced following treatment in a number of major life areas. Although there was relatively little change in overall problems during a 12-month period following treatment, less cocaine use during treatment as indicated by either a latent continuous construct or a dichotomous measure, was associated with fewer addiction-related problems following treatment, even when controlling for baseline levels of problems. This relationship appears to be in part accounted for by the frequency of cocaine use during the follow-up period. However, these findings suggest that within-treatment cocaine use outcome measures can be valid indicators of treatment success because they are directly related to cocaine use and the level of global problems following treatment.
Acknowledgments
This research was supported by a supplement to National Institute on Drug Abuse (NIDA) grant R01 DA015969-09S1 (PI: Carroll), as well as NIDA grants P50-DA09241 (PI: Carroll), and U10 DA015831 (Carroll, PI). We gratefully acknowledge Tami Frankforter and Karen Hunkele for their invaluable help with assembling the dataset, and to the participants, research staff and colleagues who participated in the original clinical trials.
Footnotes
Dr. Carroll works with Yale University to manage any potential conflicts of interest.
Contributor Information
Brian D. Kiluk, Yale School of Medicine
Charla Nich, Yale School of Medicine.
Katie Witkiewitz, University of New Mexico.
Theresa A. Babuscio, Yale School of Medicine
Kathleen M. Carroll, Yale School of Medicine
References
- Alterman AI, Brown LS, Zaballero A, McKay JR. Interviewer severity ratings and composite scores of the ASI: A further look. Drug and Alcohol Dependence. 1994;34:201–209. doi: 10.1016/0376-8716(94)90157-0. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington DC: APA Press; 1994. [Google Scholar]
- American Society of Addiction Medicine. ASAM Patient Placement Criteria for the Treatment of Substance-Related Disorders, Second Edition-Revised (ASAM PPC-2R) Chevy Chase, MD: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- Borders Tyrone F, Booth Brenda M, Falck Russel S, Leukefeld Carl, Wang Jichuan, Carlson Robert G. Longitudinal changes in drug use severity and physical health-related quality of life among untreated stimulant users. Addictive Behaviors. 2009;34(11):959–964. doi: 10.1016/j.addbeh.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown Thomas G, Seraganian Peter, Shields Norm. Subjective appraisal of problem severity and the ASI: Secondary data or second opinion? Journal of Psychoactive Drugs. 1999;31(4):445–449. doi: 10.1080/02791072.1999.10471775. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio T, Gordon MA, Rounsaville BJ. Computer-assisted cognitive-behavioral therapy for addiction. A randomized clinical trial of ‘CBT4CBT’. American Journal of Psychiatry. 2008;165(7):881–888. doi: 10.1176/appi.ajp.2008.07111835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Fenton LR, Ball SA, Nich C, Frankforter TL, Shi J, Rounsaville BJ. Efficacy of disulfiram and cognitive-behavioral therapy in cocaine-dependent outpatients: A randomized placebo controlled trial. Archives of General Psychiatry. 2004;64:264–272. doi: 10.1001/archpsyc.61.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Kiluk BD, Nich C, DeVito EE, Decker S, LaPaglia D, Ball SA. Towards empirical identification of a clinically meaningful indicator of treatment outcome for drug addiction: Features of candidate indicators and evaluation of sensitivity to treatment effects and relationship to one year cocaine use follow-up outcomes. Drug and Alcohol Dependence. doi: 10.1016/j.drugalcdep.2014.01.012. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Ball SA, McCance-Katz E, Rounsaville BJ. Treatment of cocaine and alcohol dependence with psychotherapy and disulfiram. Addiction. 1998;93:713–728. doi: 10.1046/j.1360-0443.1998.9357137.x. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Ball SA, McCance-Katz EF, Frankforter TF, Rounsaville BJ. One year follow-up of disulfiram and psychotherapy for cocaine-alcohol abusers: Sustained effects of treatment. Addiction. 2000;95:1335–1349. doi: 10.1046/j.1360-0443.2000.95913355.x. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Petry NM, Eagan DA, Shi JM, Ball SA. Disulfiram and contingency management to enhance CBT for cocaine dependence: Part 1, Effects on cocaine use. 2013 doi: 10.1016/j.drugalcdep.2015.12.036. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ, Gordon LT, Nich C, Jatlow PM, Bisighini RM, Gawin FH. Psychotherapy and pharmacotherapy for ambulatory cocaine abusers. Archives of General Psychiatry. 1994;51:177–197. doi: 10.1001/archpsyc.1994.03950030013002. [DOI] [PubMed] [Google Scholar]
- Carroll Kathleen M, Ball Samuel A, Martino Steve, Nich Charla, Babuscio Theresa A, Rounsaville Bruce J. Enduring effects of a computer-assisted training program for cognitive behavioral therapy: A 6-month follow-up of CBT4CBT. Drug and Alcohol Dependence. 2009;100(1):178–181. doi: 10.1016/j.drugalcdep.2008.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll Kathleen M, Nich Charla, Shi Julia M, Eagan Dorothy, Ball Samuel A. Efficacy of disulfiram and Twelve Step Facilitation in cocaine-dependent individuals maintained on methadone: A randomized placebo-controlled trial. Drug and Alcohol Dependence. 2012;126(1–2):224–231. doi: 10.1016/j.drugalcdep.2012.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crits-Christoph P, Siqueland L, McCalmont E, Weiss RD, Gastfriend DR, Frank A, Thase ME. Impact of psychosocial treatments on associated problems of cocaine-dependent patients. Journal of Consulting and Clinical Psychology. 2001;69:825–830. doi: 10.1037//0022-006x.69.5.825. [DOI] [PubMed] [Google Scholar]
- Donovan Dennis M, Bigelow George E, Brigham Gregory S, Carroll Kathleen M, Cohen Allan J, Gardin John G, Wells Elizabeth A. Primary outcome indices in illicit drug dependence treatment research: Systematic approach to selection and measurement of drug use endpoints in clinical trials. Addiction. 2012;107(4):694–708. doi: 10.1111/j.1360-0443.2011.03473.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. American Journal of Psychiatry. 2008;165(2):179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- Falk Daniel, Wang Xin Qun, Liu Lei, Fertig Joanne, Mattson Margaret, Ryan Megan, Litten Raye Z. Percentage of subjects with no heavy drinking days: Evaluation as an efficacy endpoint for alcoholclinical trials. Alcoholism: Clinical and Experimental Research. 2010;34(12):2022–2034. doi: 10.1111/j.1530-0277.2010.01290.x. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- Ghitza Udi E, Epstein David H, Preston Kenzie L. Psychosocial functioning and cocaine use during treatment: Strength of relationship depends on type of urine-testing method. Drug and Alcohol Dependence. 2007;91(2–3):169–177. doi: 10.1016/j.drugalcdep.2007.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella Christine E, Hser Yih-Ing, Hsieh Shih-Chao. Predictors of drug treatment re-entry following relapse to cocaine use in DATOS. Journal of Substance Abuse Treatment. 2003;25(3):145–154. doi: 10.1016/s0740-5472(03)00128-4. [DOI] [PubMed] [Google Scholar]
- Guydish Joseph, Sorensen James L, Chan Monica, Werdegar David, Bostrom Alan, Acampora Alfonso. A randomized trial comparing day and residential drug abuse treatment: 18-month outcomes. Journal of Consulting and Clinical Psychology. 1999;67(3):428–434. doi: 10.1037//0022-006x.67.3.428. [DOI] [PubMed] [Google Scholar]
- Hall Sharon M, Wasserman David A, Havassy Barbara E, Maude-Griffin Peg, Higgins Stephen T, Katz Jonathan L. Cocaine abuse: Behavior, pharmacology, and clinical applications. San Diego, CA US: Academic Press; 1998. Relapse to cocaine use; pp. 389–407. [Google Scholar]
- Higgins ST, Wong CJ, Badger GJ, Haug-Ogden DE, Dantona RL. Contingent reinforcement increases cocaine abstinence during outpatient treatment and one year follow-up. Journal of Consulting and Clinical Psychology. 2000;68:64–72. doi: 10.1037//0022-006x.68.1.64. [DOI] [PubMed] [Google Scholar]
- Hjorthøj CR, Hjorthøj AR, Nordentoft M. Validity of Timeline Follow-Back for self-reported use of cannabis and other illicit substances - Systematic review and meta-analysis. Addictive Behaviors. 2012;37(3):225–233. doi: 10.1016/j.addbeh.2011.11.025. [DOI] [PubMed] [Google Scholar]
- Kosten Thomas R, Gawin Frank H, Kosten Therese A, Morgan Cindy, Rounsaville Bruce J, Schottenfeld Richard, Kleber Herbert D. Six-Month Follow-Up of Short-Term Pharmacotherapy for Cocaine Dependence. The American Journal on Addictions. 1992;1(1):40–49. doi: 10.1111/j.1521-0391.1992.tb00005.x. [DOI] [Google Scholar]
- Kosten Thomas R, Rounsaville Bruce J, Kleber Herbert D. Multidimensionality and prediction and treatment outcome in opioid addicts: 2.5-year follow-up. Comprehensive Psychiatry. 1987;28(1):3–13. doi: 10.1016/0010-440x(87)90038-1. [DOI] [PubMed] [Google Scholar]
- Kosten Thomas R, Rounsaville Bruce J, Kleber Herbert D. Antecedents and consequences of cocaine abuse among opioid addicts: A 2.5-year follow-up. Journal of Nervous and Mental Disease. 1988;176(3):176–181. doi: 10.1097/00005053-198803000-00006. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Gordon GR. Determinants of relapse: Implications for the maintenance of behavior change. In: Davidson PO, Davidson SM, editors. Behavioral Medicine: Changing Health Lifestyles. New York: Brunner/Mazel; 1980. pp. 410–452. [Google Scholar]
- McCann David J, Li Shou-Hua. A novel, nonbinary evaluation of success and failure reveals bupropion efficacy versus methamphetamine dependence: Reanalysis of a multisite trial. CNS Neuroscience & Therapeutics. 2012;18(5):414–418. doi: 10.1111/j.1755-5949.2011.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Alterman AI, Koppenhaver JM, Mulvaney FD, Bovasso GB, Ward K. Continuous, catergorical and time to event cocaine use outcome variables: Degree of intercorrelation and sensitivity to treatment group differences. Drug and Alcohol Dependence. 2001;62:19–31. doi: 10.1016/s0376-8716(00)00156-3. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Chalk M, Bartlett J. Outcome performance, and quality--What’s the difference. Journal of Substance Abuse Treatment. 2007;32:331–340. doi: 10.1016/j.jsat.2006.09.004. [DOI] [PubMed] [Google Scholar]
- McLellan A Thomas, Alterman Arthur I, Metzger David S, Grissom Grant R, Woody George E, Luborsky Lester, O’Brien Charles P. Similarity of outcome predictors across opiate, cocaine, and alcohol treatments: Role of treatment services. Journal of Consulting and Clinical Psychology. 1994;62(6):1141–1158. doi: 10.1037//0022-006x.62.6.1141. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Argerious M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic evaluation instrument for substance abuse patients: The Addiction Severity Index. Journal of Nervous and Mental Disease. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP, Druley KA. Predicting response to alcohol and drug treatments: Role of psychiatric severity. Archives of General Psychiatry. 1983;40:620–625. doi: 10.1001/archpsyc.1983.04390010030004. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP, Kron R. Are the addiction-related problems of substance abusers really related? Journal of Nervous and Mental Disease. 1981;169:232–239. doi: 10.1097/00005053-198104000-00005. [DOI] [PubMed] [Google Scholar]
- McLellan AT, McKay JR, Forman R, Cacciola JS, Kemp J. Reconsidering the evaluation of addiction treatment: From retrospective follow-up to concurrent recovery monitoring. Addiction. 2005;100:447–458. doi: 10.1111/j.1360-0443.2005.01012.x. [DOI] [PubMed] [Google Scholar]
- McMahon Robert C. Personality, stress, and social support in cocaine relapse prediction. Journal of Substance Abuse Treatment. 2001;21(2):77–87. doi: 10.1016/s0740-5472(01)00187-8. [DOI] [PubMed] [Google Scholar]
- Melberg Hans Olav. Three problems with the ASI composite scores. Journal of Substance Use. 2004;9(3–4):120–126. [Google Scholar]
- Miller Peter G, Miller William R. What should we be aiming for in the treatment of addiction? Addiction. 2009;104(5):685–686. doi: 10.1111/j.1360-0443.2008.02514.x. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. MPlus User’s Guide. 7. Los Angeles, CA: Muthen & Muthen; 2012. [Google Scholar]
- Romelsjo Anders. The Addiction Severity Index (ASI) and the severity of dependence: How large are the associations? Journal of Substance Use. 2004;9(3–4):127–131. [Google Scholar]
- Rounsaville Bruce J, Kosten Thomas R, Kleber Herbert D. The antecedents and benefits of achieving abstinence in opioid addicts: A 2.5-year follow-up study. The American Journal of Drug and Alcohol Abuse. 1987;13(3):213–229. doi: 10.3109/00952998709001511. [DOI] [PubMed] [Google Scholar]
- Rounsaville Bruce J, Tierney Terrence, Crits-Christoph Katherine, Weissman Myrna M, Kleber Herbert D. Predictors of outcome in treatment of opiate addicts: Evidence for the multidimensional nature of addicts’ problems. Comprehensive Psychiatry. 1982;23(5):462–478. doi: 10.1016/0010-440x(82)90160-2. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Fletcher BW, Hubbard RL, Anglin MD. A national evaluation of treatment outcomes for cocaine dependence. Archives of General Psychiatry. 1999;56:507–514. doi: 10.1001/archpsyc.56.6.507. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline followback: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. New Jersey: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Substance Abuse and Mental Health Service Administration (SAMHSA) Treatment Episode Data Set (TEDS): 2001–2011. National Admissions to Substance Abuse Treatment Services. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. (HHS Publication No. (SMA) 13-4772) [Google Scholar]
- Tiffany Stephen T, Friedman Lawrence, Greenfield Shelly F, Hasin Deborah S, Jackson Ron. Beyond drug use: A systematic consideration of other outcomes in evaluations of treatments for substance use disorders. Addiction. 2012;107(4):709–718. doi: 10.1111/j.1360-0443.2011.03581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughan Ellen L, McMahon Robert C. Changes over time in Addiction Severity Index problem dimensions among cocaine abusers treated in community settings. Substance Use & Misuse. 2006;41(9):1287–1294. doi: 10.1080/10826080600754892. [DOI] [PubMed] [Google Scholar]
- Wertz Jennifer S, Cleaveland Bonnie L, Stephens Robert S. Problems in the application of the Addiction Severity Index (ASI) in rural substance abuse services. Journal of Substance Abuse. 1995;7(2):175–188. doi: 10.1016/0899-3289(95)90003-9. [DOI] [PubMed] [Google Scholar]
- Winchell Celia, Rappaport Bob A, Roca Rigoberto, Rosebraugh Curtis J. Reanalysis of methamphetamine dependence treatment trial. CNS Neuroscience & Therapeutics. 2012;18(5):367–368. doi: 10.1111/j.1755-5949.2011.00288.x. [DOI] [PMC free article] [PubMed] [Google Scholar]