Abstract
Ecological momentary assessment was used to examine associations between negative affect, positive smoking outcome expectancies, and smoking urge during the first 7 days of a smoking quit attempt. Participants were 302 female smokers who enrolled in an individually tailored smoking cessation treatment study. Multilevel mediation analysis was used to examine the temporal relationship among: 1) the effects of negative affect and positive smoking outcome expectancies at one assessment point (e.g., time j) on smoking urge at the subsequent time point (e.g., time j + 1) in Model 1; and, 2) the effects of negative affect and smoking urge at time j on positive smoking outcome expectancies at time j + 1 in Model 2. The results from Model 1 showed a statistically significant effect of negative affect at time j on smoking urge at time j + 1, and this effect was mediated by positive smoking outcome expectancies at time j, both within- and between-participant. In Model 2, the within-participant indirect effect of negative affect at time j on positive smoking outcome expectancies at time j + 1 through smoking urge at time j was nonsignificant. However, a statistically significant indirect between-participant effect was found in Model 2. The findings support the hypothesis that urge and positive smoking outcome expectancies increase as a function of negative affect, and suggest a stronger effect of expectancies on urge as opposed to the effect of urge on expectancies.
Keywords: smoking, urge, negative affect, positive outcome expectancies, ecological momentary assessment
The majority of smokers attempting to quit relapse within the first week of a quit attempt (Hughes, Keeley, & Naud, 2004). The risk of smoking relapse may be highest in the early phase of a quit attempt because the theoretical determinants of smoking motivation such as urge and mood changes are most pronounced and dynamic during this time, with changes occurring from one day to the next, or within hours in a single day (Piasecki et al., 2002; Shiffman, 2009a). Furthermore, changes in one determinant may trigger changes in another determinant (Shiyko, Lanza, Tan, Li & Shiffman, 2012).
Urge/craving plays a prominent role in many theories of drug use and relapse (Baker, Morse, & Sherman, 1987; Drummond, 2001; Niaura et al., 1988; Niaura, 2000; Marlatt, 1985; Tiffany, 1990; Witkiewitz & Marlatt, 2004; Wise, 1988). Urge is frequently described as a subjective desire to use a drug (Brandon, Wetter, & Baker, 1996; Piasecki, 2006) and has been characterized as an indicator of motivation to smoke (Brandon et al., 1996; Piasecki, 2006). However, the notion that urge is a reliable predictor of smoking cessation outcomes has come into question (Witkiewitz & Marlatt, 2004; Wray, Gass, & Tiffany, 2013). For example, a systematic review on the association between urge and smoking cessation outcomes indicted that the time point at which urge is measured played a key role in this relationship. Smoking urge measured before a quit attempt did not have a strong association with smoking cessation outcomes, while smoking urge measured after a quit attempt was a fairly consistent of predictor of poorer cessation outcomes (Wray, Gass, & Tiffany, 2013). That is, several studies have shown that post cessation urge to smoke, measured in a variety of ways with a variety of methodologies, does indeed predict failure to quit and relapse (Blalock, Robinson, Wetter, Schreindorfer, & Cinciripini, 2008; Cofta-Woerpel et al., 2011; Javitz, Lerman, & Swan, 2012; Orleans, Rimer, Cristinzio, Keintz, & Fleisher, 1991). As such, research that contributes to a better understanding of urge during the early phase of a smoking quit attempt could potentially be used to inform treatments.
Cognitive social learning theories (CSLTs) of drug use and relapse (Marlatt, 1985; Niaura et al., 1988; Witkiewitz & Marlatt, 2004) posit that intrapersonal high-risk situations (e.g., negative affect) interact with cognitive determinants such as outcome expectancies (i.e., individuals’ beliefs about the consequences of smoking; Copeland, Brandon, & Quinn, 1995) to influence urge. According to Niaura and colleagues (1988), both urge and positive outcome expectancies (e.g., expectancy that smoking will alleviate symptoms of negative affect) increase as a function of negative affect (Brandon, Wetter, & Baker, 1996). Similarly, Marlatt (1985) proposed that greater negative affect is associated with greater urge; however, his model makes the distinction that outcome expectancies of drug use mediate that association. In each of these models, greater urge severity is hypothesized to increase the probability of drug use and relapse.
Associations among Affect, Outcome Expectancies, and Urge
Research has supported the hypothesis that negative affect triggers increased urge among smokers during a quit attempt (Baker, Morse, & Sherman, 1987; Killen, Fortmann, Newman, & Varady, 1991; Niaura et al., 1988; Shiyko et al., 2012). The most recent of these studies (Shiyko et al., 2012) showed that greater negative affect was associated with greater smoking urge among both relapsers and abstainers. However, this association weakened more gradually among relapsers than among abstainers over the course of two weeks post cessation.
Positive outcome expectancies also play a prominent role in theories of drug motivation (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004; Marlatt, 1985; Niaura et al., 1988; Witkiewitz & Marlatt, 2004). Among smokers, the most frequently endorsed smoking outcome expectancy is that smoking will alleviate negative affect (Brandon & Baker, 1991), and some evidence suggests that positive smoking outcomes expectancies may be triggered and increase as a function of internal states such as negative affect (Baker et al., 2004; Gwaltney, Shiffman, Paty, & Balabanis, 2005; Kirchner & Sayetter, 2007).
Moreover, positive outcome expectancies are generally hypothesized to increase urge (Marlatt, 1985), an association that has been demonstrated among smokers (Brandon, Wetter, & Baker, 1996). However, other researchers have proposed a different direction of effect, where positive smoking outcome expectancies may be influenced by smoking urge. For example, Kirchner and Sayette (2007) found that smoking urge measured while holding a lit cigarette, compared to holding a roll of tape, predicted higher positive smoking outcome expectancies.
A fundamental proposition of CSLTs is that associations among determinants of drug motivation (including affective state, outcome expectancies, and urge) are dynamic and reciprocal (Niaura et al., 1988; Witkiewitz & Marlatt, 2004). As such, methodologies such as ecological momentary assessments (EMA), which entail repeated administration of assessments in real time in participants’ natural environments serve to facilitate the collection of intensive longitudinal data that can capture the dynamic associations among determinants of smoking motivation (Shiffman, 2009a; Shiffman, 2009b). The ability to conduct frequent assessments with shorter spacing between observations, helps produce a clearer and more detailed examination of the process of smoking cessation than when measurement points are spaced further apart, which may produce misleading inferences (Collins & Graham 2002). Equally important, the use of EMA reduces retrospective recall bias and error (Shiffman, 2009a).
Present Study
In sum, although there is substantial theoretical and empirical work that suggests an association between greater negative affect and higher urge to smoke, there are few data addressing hypothesized mechanisms, such as outcome expectancies, that may mediate this relationship. Furthermore, there is a need to elucidate the dynamic associations among these constructs in individuals’ natural environments. Accordingly, the current study utilized EMA to examine moment-to-moment relationships among negative affect, positive smoking outcomes expectancies, and smoking urge. Four hypothesized associations were based on CSLTs of drug motivation: 1) negative affect will increase smoking urge, 2) negative affect will increase positive smoking outcomes expectancies, 3) positive smoking outcome expectancies will increase smoking urge, and 4) the effect of negative affect on urge to smoke will be mediated by positive smoking outcome expectancies. To better account for the dynamic conceptualization of these determinants involved in drug motivation (Niaura et al., 1988; Witkiewitz & Marlatt, 2004), a second model based on the work of Kirchner and Sayette (2007), was tested in which the association between negative affect and positive outcome expectancies was mediated by smoking urge.
It should be noted that negative affect may have a stronger effect on urge and smoking behavior among women than among men. For instance, women report greater smoking urge than men in response to a negative mood induction (Perkins, Karelitz, Giedgowd, & Conklin, 2013). Further, women are more likely to experience an increase in negative affect after initiating abstinence from smoking, and to relapse as a consequence of negative affect (Leventhal et al., 2007; Xu et al., 2007). Compared to men, women smokers also initiate smoking more quickly and have greater smoking intake in response to negative affect (Perkins, Giedgowd, Karelitz, Conklin, & Lerman, 2012; Weinberger & McKee, 2011). Given the particularly strong role of negative affect in smoking urge and behavior among women, the present study focused on female smokers during a quit attempt.
Method
Participants
A total of 302 female smokers from the Seattle metropolitan area participated in a randomized clinical trial examining an individually tailored smoking cessation treatment. Details pertaining to recruitment, research design, and treatment results can be found in Wetter et al. (2011). All participants in the parent study were women between the ages of 18 to 70 who reported smoking a minimum of 10 cigarettes per day. The study excluded women who reported pregnancy or lactation, use of bupropion, nicotine patch contraindication, use of tobacco products other than cigarettes, or a current psychiatric diagnosis of substance use, anxiety, and/or depressive disorders.
Procedure
Participants responding to recruitment advertisements were screened via phone, and those eligible to participate were scheduled for an in-person orientation where they received a detailed description of study procedures, were consented, completed baseline questionnaires, and set a smoking quit date. The day prior to the scheduled quit date (approximately 7 days after the orientation visit) participants were provided with a palm-top personal computer (PPC), received training in completing EMAs, and practiced completing EMAs using the PPC. Participants were then asked to carry the PCC with them at all times for 7 consecutive days starting on the participant’s quit day. They were also notified that project staff were available throughout the duration of the study should they need technical assistance. PPCs were programmed to deliver four random assessments between the participant’s stated wake-up time and bedtime. Participant’s waking hours were divided into four equal segments with one random assessment scheduled within each segment. If an assessment could not be completed immediately, it could be delayed for 5 minutes up to 4 times. Assessments with no response were recorded as missing. Participants could also self-initiate “temptation assessments” each time they experienced an urge to smoke a cigarette. If a participant initiated an assessment 15 minutes before a scheduled random assessment, the assessment was rescheduled for another random time within the same time segment. In the event that no time was left within the time segment, only three random assessments were delivered that day. Each EMA took approximately 2–4 minutes to complete. To encourage compliance, participants were compensated with $10, $25, or $50 gift certificates if they completed 50%–69%, 70%–89%, or ≥90% of the random assessments, respectively. Participants were not compensated for temptation assessments to avoid false reports of temptations. Additional details describing the EMA procedures can be found in Cofta-Woerpel et al. (2011).
All participants received a standard smoking cessation treatment that followed the recommendations of the Smoking Cessation Clinical Practice Guideline (Fiore, Bailey, & Cohen, 1996). Treatment consisted of five group counseling sessions and six weeks of the 21mg nicotine patch. Participants attended their first group counseling session three days prior to their scheduled quit date. The final session was one week after the quit date. After completing the group counseling and EMA on day 7, participants were randomized to one of two groups: computer-delivered treatment (n=151) or standard treatment (n=151). Participants assigned to the computer-delivered treatment group continued to use the PPC and received an individualized relapse prevention intervention for one additional month starting on day 7.
Baseline Questionnaire Measures
Demographic information
Demographic characteristics including age, marital status, education, income, and race/ethnicity were obtained prior to quitting.
Smoking characteristics
At the orientation session (prior to the quit attempt), participants reported smoking-related characteristics such as current smoking rate, years smoking, and previous quit attempts. They also completed the Fagerström Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerström, 1991).
Ecological Momentary Assessment Measures
All EMAs (random and temptation) were date and time stamped; and participants responded to the following questions.
Negative affect
Negative affect was assessed by asking participants to respond to the following statement: “My mood is negative.” Participants responded on a 4-point Likert scale with the following choices, 1 (definitely NO), 2 (mostly no), 3 (mostly yes), and 4 (definitely YES).
Positive smoking outcome expectancies
Positive smoking outcome expectancies were assessed with the item, “Would smoking right now improve your mood, be pleasurable, or help you cope with this situation?” Responses were on a 4-point Likert scale that included, 1 (definitely NO), 2 (mostly no), 3 (mostly yes), and 4 (definitely YES).
Urge to smoke
Urge was assessed with the item, “How strong is your urge to smoke?” on a 5-point scale that ranged from 1 (no urge) to 5 (severe urge).
Smoking abstinence
The first random EMA of each day included a question about any smoking during the previous day. Smoking abstinence was also assessed at each post-cessation clinic visit (i.e., days 3, 5, and 7). A participant was considered to have lapsed if she reported any smoking (i.e., even a puff on the EMA or at the clinic visits) or had a carbon monoxide level ≥10 parts per million (ppm) at any of the clinic visits.
Statistical Analysis
The current project generated longitudinal EMA data that were nested (i.e., assessment ratings nested within participants). To account for the dependent nature of nested EMA data (Raudenbush & Bryk, 2002), multilevel mediation analysis (MMA) using a sequence of hierarchical linear models (Zhang, Zyphur & Preacher, 2009) were performed by using the XTMIXED procedure in Stata/SE 12.1. Predictors in the MMA were group-mean centered to untangle the within-participant effects (i.e., variation within individuals over time) and between-participant effects (i.e., average differences between individuals; Raudenbush & Bryk, 2002).
A lagged analysis was used because testing associations with data collected simultaneously in the same assessment may confound cause and effect, making it difficult to discern the direction of an association (Chandra, Scharf, & Shiffman, 2011). To demonstrate the lagged analysis we provide an example with Model 1. For instance, if a participant completed four assessments in a day, responses for negative affect and positive smoking outcome expectancies recorded at the first assessment (e.g., at time j) were used to predict smoking urge reported at the second assessment (e.g., at time j +1). In turn, responses for negative affect and positive smoking outcome expectancies recorded at the second assessment (e.g., time j) were used to predict smoking urge reported at the third assessment (e.g., time j +1) and so forth.
The recommendations for MMA set forth by Krull and MacKinnon (1999; 2001) were used to examine the relationships among the predictor (X) measured at time j, mediator (M) at time j, and the outcome (Y) at time j + 1. This method allows estimation of the total effect of X on Y (specified by Path c), the effect of X on M (Path a), the effect of M on Y (Path b), and the direct effect of X on Y after M is added to the model (Path c′). To further examine the mediational relationship for both within-participant and between-participant effects, the product of the Path a and Path b coefficients and the Sobel standard error of the mediated effect were used to estimate the mediated effect of predictor (X) on outcome (Y).
MMA controlled for a log-transformed time of the assessment and lapse status during the 7-day assessment period. These covariates were included in the analysis because time of assessment and smoking could potentially influence the degree of smoking urge (e.g., participants reported progressively higher smoking urge across time within a day). The outcome variable in each model measured at time j was added as a covariate to reduce the probability that the observed relationships were not attributed to 1) a potentially strong association between the outcome variable measured at time j and mediator measured at time j or 2) a strong association between the outcome variable measured at time j and at time j + 1. MMA also controlled for the length of duration between assessment j and j + 1.
Results
Participant Characteristics
Demographic characteristics are shown in Table 1. The average age of the participants was approximately 43 years, the majority were non-Hispanic White, had at least some college education, and were married or living with a partner. The average self-reported smoking rate was 20.6 cigarettes per day, and the mean FTND score was 5.2. Among all participants, 75 (25%) lapsed during the 7-day assessment period.
Table 1.
Demographic characteristics of participants (n = 302)
| Characteristic | |
|---|---|
| Age in years, mean (standard deviation) | 42.89 (10.83) |
| Ethnicity/race, n (%)* | |
| Non-Hispanic White | 247 (81.80%) |
| Other | 53 (17.20%) |
| Education, n (%) | |
| ≤High school | 72 (23.80%) |
| At least some college | 230 (76.20%) |
| Marital status, n (%)** | |
| Married/living with partner | 118 (39.10%) |
| Other | 179 (59.3%) |
| Smoking variables | |
| Typical smoking rate, mean (SD) | 20.56 (7.77) |
| FTND score, mean (SD) | 5.16 (1.93) |
2 participants did not report this information
5 participants did not report this information
Assessment Completion
Participants completed a total of 12,533 assessments (including both random and temptation assessments) during the 7-day EMA monitoring period. A majority of participants (88.4%) completed at least one assessment on each day of the 7 day EMA monitoring period, and an additional 8.3% of participants completed at least one assessment on 6 out of 7 days. An average of 19.15 (SD = 5.06) random assessments and 22.62 (SD = 11.78) temptation assessments were completed per person during the 7-day assessment period, yielding an average of 2.77 (SD = .70) random assessments per day, and 3.28 (SD = 1.69) temptation assessments per day. The mean time between any two consecutive assessments was 125.90 minutes (SD = 178.75). The overall compliance rate for random assessments was 77.85%. No statistically significant association was found between the number of completed random assessments and the number of completed temptation assessments, suggesting that less compliant smokers did not differ from more compliant smokers in initiating and completing temptation assessments. Of the 12,533 completed assessments, 1,871 were the last assessment of the day, had no lagged outcome, and were excluded from analyses.
Multilevel Mediation Analyses
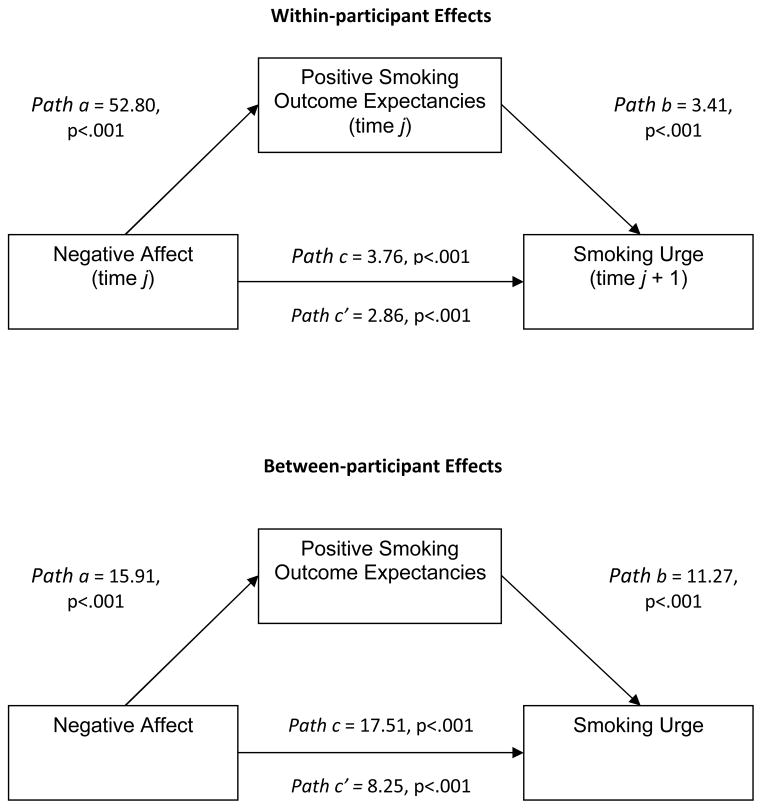
Model 1. Do positive outcome expectancies mediate the association between negative affect and urge?
MMA was used to test a model in which positive outcome expectancies at time j mediate the association between negative affect at time j and smoking urge at time j + 1. This model controlled for a log-transformed time of the assessment, lapse status during the 7-day assessment period, smoking urge at time j, and the length of duration between assessment j and j + 1. In Model 1, the within-person effect tested the moment-to-moment association between negative affect and smoking urge, and if that association was mediated by moment-to-moment changes in positive smoking outcome expectancies. The between-person effect tested the association between the 7-day overall mean of negative affect and smoking urge, and if that association was mediated by a 7-day overall mean of positive smoking outcome expectancies.
In the first step, the total effect of negative affect at time j on smoking urge at time j + 1 (Path c) was estimated. Both the within-participant (z = 3.76, p < .001) and between-participant (z = 17.51, p < .001) effects were statistically significant. In the following step the effects of negative affect at time j on positive outcome expectancies at time j was estimated (Path a). Again, these results indicated that both the within-participant (z = 52.8, p < .001) and between-participant (z = 15.91, p < .001) effects were statistically significant. Similarly, the effect of positive outcome expectancies at time j on smoking urge at time j + 1 (Path b) was statistically significant both within-participant (z = 3.41, p < .001) and between-participant (z = 11.27, p < .001). In addition, the direct association of negative affect at time j on urge at time j + 1 after positive smoking outcome expectancies at time j was added to the model (Path c′) was statistically significant for both within-participant (z = 2.86, p < .001) and between-participant (z = 8.25, p < .001) effects.
To test the significance of the mediation effect in the within-participant model, the product of the Path a and Path b coefficients and the Sobel standard error were used. Results from this analysis indicated that the mediated effect was statistically significant (z = 3.40, p < .001) and the proportion mediated effect (PME) was 0.473. That is, approximately 47% of the within-participant total effect of negative affect on smoking urge was mediated by positive smoking outcome expectancies. Using the same method, the product of Path a and Path b coefficients and the Sobel standard error indicated that the mediated between-participant effect was statistically significant (z = 9.20, p < .001) and the PME was 0.496. That is, nearly 50% of the between-participant total effect was mediated by positive smoking outcome expectancies.
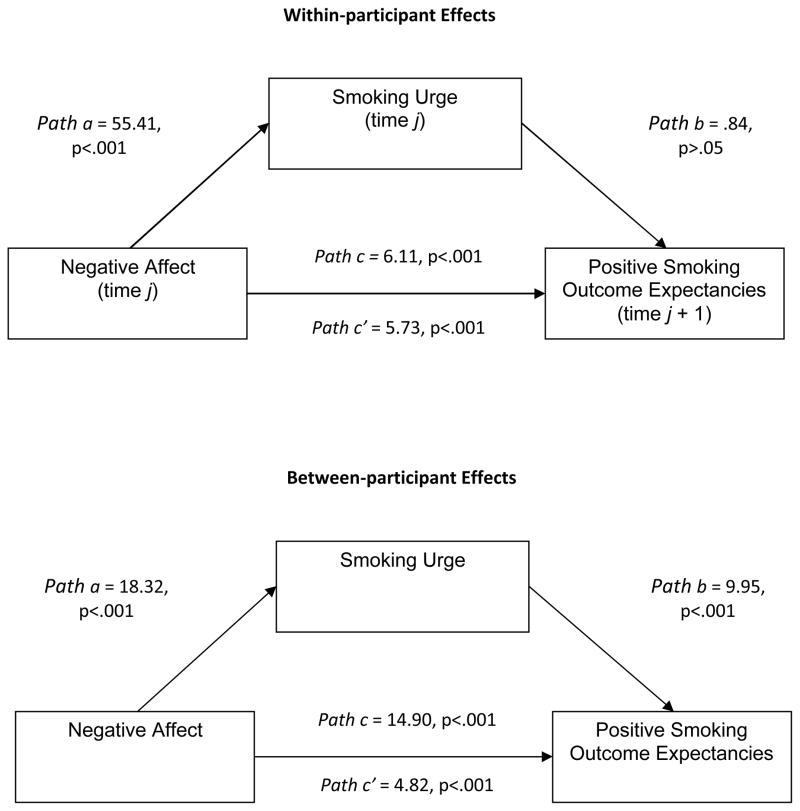
Model 2. Does urge mediate the association between negative affect and positive outcome expectancies?
MMA was also used to test a model in which smoking urge at time j mediates the relationship between negative affect at time j and positive outcome expectancies at j + 1. This model controlled for a log-transformed time of the assessment, lapse status during the 7-day assessment period, positive outcome expectancies at time j, and the length of duration between assessment j and j + 1. In Model 2, the within-person effect tested the moment-to-moment association between negative affect and positive smoking outcome expectancies, and if that association was mediated by moment-to-moment changes in smoking urge. The between-person effect tested the association between the 7-day overall mean of negative affect and positive smoking outcome expectancies, and if that association was mediated by a 7-day overall mean of smoking urge.
In the first step, the total effect of negative affect at time j on positive outcome expectancies at time j + 1 (Path c) was estimated. Both within-participant (z = 6.11, p < .001) and between-participant (z = 14.90, p < .001) effects were statistically significant. In the following step, the estimated effects of negative affect at time j on smoking urge at time j (Path a) were statistically significant in both within-participant (z = 55.41, p < .001) and between-participant (z = 18.32, p < .001) models. The analysis of smoking urge at time j on positive outcome expectancies at time j + 1 (Path b) indicated that the within-participant effect was not statistically significant (z = .84, p = .40) while the between-participant effect was statistically significant (z = 9.95, p < .001). Both the within-participant (z = 5.73, p < .001) and between- participant (z = 4.82, p < .001) effects of negative affect at time j on positive outcome expectancies at time j + 1 were statistically significant after smoking urge at time j was added to the model (Path c′).
The within-participant mediation effect was not statistically significant (z = .84, p = .40). The between-participant mediated effect was statistically significant (z = 8.74, p < .001), with a PME of 0.606, indicating that approximately 61% of the total between-participant effect was mediated by smoking urge.
Discussion
The current study tested the associations among negative affect, positive smoking outcome expectancies, and smoking urge among female smokers during the first 7 days of a smoking quit attempt. Consistent with our hypotheses, positive outcome expectancies mediated the association between negative affect and smoking urge in both within-participant and between-participant analyses. More specifically, within-participant results demonstrated that reporting a higher degree of negative affect at one time point was associated with an increased expectation that smoking would improve mood at the same time point, and in turn, this expectation was associated with increased smoking urge at the subsequent time point. Similarly, the between-participant results indicated that smokers who reported higher negative affect were more likely to report an increased expectation that smoking would improve mood, and in turn, reported greater urge to smoke.
Findings from an alternative model, in which smoking urge was hypothesized to mediate the effect of negative affect on positive outcome expectancies, showed inconsistent mediation effects within- and between participants. The within-participant model showed that reporting a higher degree of negative affect at one time point was associated with increased smoking urge at the same time point and positive smoking outcomes expectancies at the subsequent time point. However, smoking urge at one time point did not have a statistically significant association with positive smoking outcomes expectancies at the subsequent time point, and the mediational effect was not statistically significant. Conversely, findings from the between-participant model showed that smokers who reported higher negative affect reported greater severity of urge, and in turn, increased expectancies that smoking would improve mood.
One possible explanation for the difference in within- versus between-participant effects in Model 2 is a distinction in the conceptualization of smoking outcome expectancies, with within-participant effects being characterized as more situational (i.e., state), and between-participant effects being thought of as more generalized (i.e., trait) effects (Brandon, Juliano, & Copeland, 1999). Findings from the current study suggest that while positive smoking outcome expectancies are associated with urge more generally, urge may either not prospectively influence expectancies, or such influence may be fleeting and not captured given the delays between EMAs present in the current study.
Findings from this study support proposed associations found in prominent CSLTs that suggest 1) urge and outcome expectancies increase with higher negative affect, and 2) positive outcome expectancies mediate the association between negative affect and urge (Niaura et al., 1988; Marlatt, 1985). Furthermore, both models tested in this study support the conceptualization that determinants of smoking motivation have dynamic reciprocal relationships. However, examining moment-to-moment associations among these determinants suggested that positive outcome expectancies appear to be a better predictor of smoking urge than vice versa. This finding is noteworthy because it provides a more refined understanding of the mechanisms that may influence postquit smoking urge. This is particularly relevant to smoking cessation research given the association between postquit smoking urge and smoking cessation outcomes (Wray, Gass, & Tiffany, 2013).
Based on the findings that negative affect, positive smoking outcome expectancies, and smoking urge appear to have dynamic reciprocal relationships, smoking cessation interventions might address these determinants in multiple ways. One key strategy to reduce urge and relapse risk would be to reduce negative affect and downstream effects on expectancies and urge. For example, pharmacotherapies such as bupropion and varenicline have been demonstrated to decrease levels of negative affect during a quit attempt (Cinciripini et al., 2013; West, Baker, Cappelleri & Bushmakin, 2008). Furthermore, some research suggests that varenicline and nicotine vaccines may reduce the rewarding effects of smoking during a quit attempt; thus, potentially reducing positive smoking outcome expectancies (Hartmann-Boyce, Stead, Cahill, & Lancaster, in press; West et al., 2008).
Psychosocial interventions may also be used to reduce the levels of these determinants and weaken the links among them. For instance, interventions may decrease negative affect by improving smokers’ coping responses (e.g., soliciting social support); thus, reducing the reliance on smoking to improve mood (Baker et al., 2004; Brandon, 1994). Also, mindfulness-based interventions appear to promote more effective coping and affective regulation (Brown & Ryan, 2003; Grossman, Niemann, Schmidt, Walach, 2004; McKee, Zvolensky, Solomon, Bernstein, & Leen-Feldner, 2007); and show promise for both reducing negative affect and weakening the association between negative affect and smoking urge (Adams et al., 2012; Bowen & Marlatt, 2009). Lastly, positive smoking outcome expectancies may be reduced by targeting myths of drug effects and employing expectancy challenge strategies or cognitive restructuring (Larimer, Palmer, Marlatt, & 1999).
Limitations
Notably, the present study included only women who were predominantly non-Hispanic White. Thus, findings may not generalize to men, or to women of other racial/ethnic groups. Eligibility criteria also excluded women with a current psychiatric disorder. Therefore, these findings may not be representative of smokers with psychiatric comorbidities. Furthermore, all participants received nicotine replacement therapy and an intensive counseling intervention, which may have reduced negative affect and urge during the 7-day EMA monitoring period. It is possible that participants were less likely to respond to, or initiate, EMA when experiencing higher levels of craving and negative affect, and as such, episodes of higher craving and negative affect may be more likely to be “missing” (Shiffman, Engberg, Paty, Perz, Gnys, Kassel, Hickcox, 1997; Stone & Shiffman, 2002). We speculate that if the “missing” episodes were included in our analyses the strength of the tested associations between negative affect and craving may have been stronger because it has been suggested that smoking urge becomes more salient during states of negative affect (Shiffman, 2013). It is important to note that smoking urges may result from multiple causes (e.g., cue-induced vs. abstinence-based); however, differentiating among causes was outside the scope of the current study. Lastly, negative affect, smoking urge, and positive outcome expectancies were all measured using single EMA items and those items were very broad in scope. For example, the positive smoking outcome expectancies item included enhancement of positive affect, relief of negative affect, and usefulness as a coping strategy. Although, we are not aware of studies examining the reliability and validity of single item EMA measures, our findings are consistent with prior EMA research studies that are at least suggestive of construct and predictive validity. However, future EMA research would benefit from a more in-depth psychometric analysis.
Conclusion
Collectively, the findings from this study support the hypothesis that urge and positive smoking outcome expectancies increase as a function of negative affect (Brandon, Wetter, & Baker, 1996; Niaura et al., 1988). Secondly, the results lend support to Marlatt’s (1985) model positing that positive outcome expectancies for drug use mediate the association between high risk situations (e.g., negative affect) and drug urge. Third, given that the effect of positive smoking outcome expectancies on smoking urge was consistent among individual smokers over time and between smokers, this association may be stronger than the effect of urge on positive smoking outcome expectancies. The finding adds to the growing body of work utilizing state-of-the-science technologies to advance our understanding of the determinants commonly associated with smoking motivation and relapse. Future research might also consider testing the associations found in this study among unaided quitters and examining other potential mechanisms of smoking urge (e.g., self-efficacy).
Figure 1.
Model one with z-scores depicting positive smoking outcome expectancies mediating the effect of negative affect on smoking urge.
Figure 2.
Model two with z-scores depicting smoking urge mediating the effect of negative affect on smoking positive smoking outcome expectancies.
References
- Adams CE, Benitez L, Kinsaul J, Apperson McVay M, Barbry A, Copeland AL. Effects of brief mindfulness instructions on reactions to body image stimuli among female smokers: An experimental study. Nicotine & Tobacco Research. 2012 doi: 10.1093/ntr/nts133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Morse E, Sherman JE. The motivation to use drugs: A psychobiological analysis of urges. In: Rivers C, editor. The Nebraska Symposium on Motivation: Vol. 34. Alcohol use and abuse. Lincoln: University of Nebraska Press; 1987. pp. 257–323. [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. 0.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Blalock JA, Robinson JD, Wetter DW, Schreindorfer LS, Cinciripini PM. Nicotine withdrawal in smokers with current depressive disorders undergoing intensive smoking cessation treatment. Psychology of Addictive Behaviors. 2008;22:122–128. doi: 10.1037/0893-164X.22.1.122. [DOI] [PubMed] [Google Scholar]
- Bowen S, Marlatt A. Surfing the urge: Brief mindfulness-based intervention for college students. Psychology of Addictive Behaviors. 2009;23:666–671. doi: 10.1037/a0017127. [DOI] [PubMed] [Google Scholar]
- Brandon TH. Negative Affect as Motivation to Smoke. Current Directions in Psychological Science. 1994;3:33–37. doi: 10.1111/1467-8721.ep10769919. [DOI] [Google Scholar]
- Brandon TH, Baker TB. The smoking consequences questionnaire: The subjective expected utility of smoking in college students. Psychological Assessment. 1991;3:484–491. [Google Scholar]
- Brandon TH, Juliano LM, Copeland AL. Expectancies for tobacco smoking. In: Kirsch I, editor. How expectancies shape experience. Washington, DC: American Psychological Association; 1999. pp. 263–299. [Google Scholar]
- Brandon TH, Wetter DW, Baker TB. Affect, expectancies, urges, and smoking: Do they conform to models of drug motivation and relapse? Experimental and Clinical Psychopharmacology. 1996;4:29–36. doi: 10.1037/1064-1297.4.1.29. [DOI] [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Brown KW, Weinstein N, Creswell JD. Trait mindfulness modulates neuroendocrine and affective responses to social evaluative threat. Psychoneuroendocrinology. 2012 doi: 10.1016/j.psyneuen.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra S, Scharf D, Shiffman S. Within-day temporal patterns of smoking, withdrawal symptoms, and craving. Drug and Alcohol Dependence. 2011;117:118–125. doi: 10.1016/j.drugalcdep.2010.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cinciripini PM, Robinson JD, Karam-Hage M, Minnix JA, Lam C, Versace F, Wetter DW. Effects of varenicline and bupropion sustained-release use plus intensive smoking cessation counseling on prolonged abstinence from smoking and on depression, negative affect, and other symptoms of nicotine withdrawal. JAMA Psychiatry. 2013;70:522–533. doi: 10.1001/jamapsychiatry.2013.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cofta-Woerpel L, McClure JB, Urbauer D, Cinciripini PM, Wetter DW. Early cessation success or failure among women attempting to quit smoking: Trajectories and volatility of urge and negative mood during the first post-cessation week. Journal of Abnormal Psychology. 2011;120:596–606. doi: 10.1037/a0023755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, Graham JW. The effect of the timing and spacing of observations in longitudinal studies of tobacco and other drug use: Temporal design considerations. Drug Alcohol Dependence. 2002;68:85–96. doi: 10.1016/s0376-8716(02)00217-x. [DOI] [PubMed] [Google Scholar]
- Copeland AL, Brandon TH, Quinn EP. The Smoking Consequences Questionnaire – Adult: Measurement of smoking outcome expectancies of experienced smokers. Psychological Assessment. 1995;7:484–494. doi: 10.1037/1040-3590.7.4.484. [DOI] [Google Scholar]
- Drummond DC. Theories of drug craving, ancient and modern. Addiction. 2001;96:33–46. doi: 10.1080/09652140020016941. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Bailey WC, Cohen SJ. Smoking Cessation Guideline Panel. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Centers for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1996. pp. 1–125. [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Gwaltney CJ, Shiffman S, Paty JA, Balabanis MH. Situational correlates of positive smoking outcome expectancies. Poster session presented at the eleventh annual meeting of the Society for Research on Nicotine and Tobacco; Prague, Czech Republic. 2005. Mar, [Google Scholar]
- Hartmann-Boyce J, Stead LF, Cahill K, Lancaster T. Efficacy of interventions to combat tobacco addiction: Cochrane update of 2012 reviews. Addiction. doi: 10.1111/add.12291. in press. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2003;99:29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- Javitz HS, Lerman C, Swan GE. Comparative dynamics of four smoking withdrawal symptom scales. Addiction. 2012;107:1501–1511. doi: 10.1111/j.13600443.2012.03838.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killen JD, Fortmann SP, Newman B, Varady A. Prospective study of factors influencing the development of craving associated with smoking cessation. Psychopharmacology. 1991;105:191–196. doi: 10.1007/BF02244308. [DOI] [PubMed] [Google Scholar]
- Kirchner TR, Sayette MA. Effects of smoking abstinence and alcohol consumption on smoking-related outcome expectancies in heavy smokers and tobacco chippers. Nicotine & Tobacco Research. 2007;9:365–376. doi: 10.1080/14622200701188893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krull JL, MacKinnon DP. Multilevel mediation modeling in group-based intervention studies. Evaluation Review. 1999;23:418–444. doi: 10.1177/0193841X9902300404. [DOI] [PubMed] [Google Scholar]
- Krull JL, MacKinnon DP. Multilevel modeling of individual and group level mediated effects. Multivariate Behavioral Research. 2001;36:249–277. doi: 10.1207/S15327906MBR3602_06. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Palmer RS, Marlatt GA. Relapse prevention: Overview of Marlatt’s cognitive-behavioral model. Alcohol Research and Health. 1999;23:151–160. [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Waters AJ, Boyd S, Moolchan ET, Lerman C, Pickworth WB. Gender differences in acute tobacco withdrawal: Effects on subjective, cognitive, and physiological measures. Experimental and Clinical Psychopharmacology. 2007;15:21–36. doi: 10.1037/1064-1297.15.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt G. Relapse prevention: Theoretical rationale and overview of the model. In: Marlatt G, Gordon JR, editors. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York: Guilford Press; 1985. pp. 3–70. [Google Scholar]
- McKee L, Zvolensky MJ, Solomon SE, Bernstein A, Leen-Feldner E. Emotional vulnerability and mindfulness: A preliminary test of associations among negative affectivity, anxiety sensitivity, and mindfulness skills. Cognitive Behaviour Therapy. 2007;36:91–101. doi: 10.1080/16506070601119314. [DOI] [PubMed] [Google Scholar]
- Niaura R. Cognitive social learning and related perspectives on drug craving. Addiction. 2000;95:155–163. doi: 10.1046/j.1360-0443.95.8s2.4.x. [DOI] [PubMed] [Google Scholar]
- Niaura RS, Rohsenow DJ, Binkoff JA, Monti PM, Pedraza M, Abrams DB. Relevance of cue reactivity to understanding alcohol and smoking relapse. Journal of Abnormal Psychology. 1988;97:133–152. doi: 10.1037/0021-843X.97.2.133. [DOI] [PubMed] [Google Scholar]
- Orleans CT, Rimer BK, Cristinzio S, Keintz MK, Fleisher L. A national survey of older smokers: Treatment needs for a growing population. Health Psychology. 1991;10:343–351. doi: 10.1037/0278-6133.10.5.343. [DOI] [PubMed] [Google Scholar]
- Perkins KA, Giedgowd GE, Karelitz JL, Conklin CA, Lerman C. Smoking in response to negative mood in men versus women as a function of distress tolerance. Nicotine & Tobacco Research. 2012;14:1418–1425. doi: 10.1093/ntr/nts075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins KA, Karelitz JL, Giedgowd GE, Conklin CA. Negative mood effects on craving to smoke in women versus men. Addictive Behaviors. 2013;38:1527–1531. doi: 10.1016/j.addbeh.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piasecki TM. Relapse to smoking. Clinical Psychology Review. 2006;26:196–215. doi: 10.1016/j.cpr.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Piasecki TM, Fiore MC, McCarthy DE, Baker TB. Have we lost our way? The need for dynamic formulations of smoking relapse proneness. Addiction. 2002;97:1093–1108. doi: 10.1046/j.1360-0443.2002.00216.x. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Application and data analysis methods. 2. Thousand Oaks, CA: Sage Publication, Inc; 2002. [Google Scholar]
- Shiffman S. Commentary on Herd & Borland (2009) and Herd et al. (2009): Illuminating the course and dynamics of smoking cessation. Addiction. 2009a;104:2100–2101. doi: 10.1111/j.1360-0443.2009.02799.x/pdf. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Ecological Momentary Assessment (EMA) in Studies of Substance Use. Psychological Assessment. 2009b;21:486–497. doi: 10.1037/a0017074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Engberg JB, Paty JA, Perz WG, Gnys M, Kassel JD, Hickcox M. A day at a time: predicting smoking lapse from daily urge. Journal of Abnormal Psychology. 1997;106:104. doi: 10.1037//0021-843x.106.1.104. apa.org/journals/abn/106/1/104.html. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Commentary on Heckman et al. (2013): Negative affect increases craving—Questions about the relationship of affect, craving and smoking. Addiction. 2013;108:2079–2080. doi: 10.1111/add.12363. [DOI] [PubMed] [Google Scholar]
- Shiyko MP, Lanza ST, Tan X, Li R, Shiffman S. Using the time-varying effect model (TVEM) to examine dynamic associations between negative affect and self-confidence on smoking urges: Differences between successful quitters and relapsers. Prevention Science. 2012;13:288–299. doi: 10.1007/s11121-011-0264-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone AA, Shiffman S. Capturing momentary, self-report data: A proposal for reporting guidelines. Annals of Behavioral Medicine. 2002;24:236–243. doi: 10.1207/S15324796ABM2403_09. [DOI] [PubMed] [Google Scholar]
- Tiffany ST. A cognitive model of drug urges and drug-use behavior: Role of automatic and nonautomatic processes. Psychological Review. 1990;97:147–168. doi: 10.1037/0033-295X.97.2.147. [DOI] [PubMed] [Google Scholar]
- Weinberger AH, McKee SA. Gender differences in smoking following an implicit mood induction. Nicotine & Tobacco Research. 2011;14:621–625. doi: 10.1093/ntr/ntr198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West R, Baker CL, Cappelleri JC, Bushmakin AG. Effect of varenicline and bupropion SR on craving, nicotine withdrawal symptoms, and rewarding effects of smoking during a quit attempt. Psychopharmacology. 2008;197:371–377. doi: 10.1007/s00213-007-1041-3. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Fiore MC, Young TB, McClure JB, deMoor CA, Baker TB. Gender differences in response to nicotine replacement therapy: Objective and subjective indexes of tobacco withdrawal. Experimental and Clinical Psychopharmacology. 1999;7:135–144. doi: 10.1037/1064-1297.7.2.135. [DOI] [PubMed] [Google Scholar]
- Wetter DW, McClure JB, Cofta-Woerpel L, Costello TJ, Reitzel LR, Businelle MS, Cinciripini PM. A randomized clinical trial of a palmtop computer-delivered treatment for smoking relapse prevention among women. Psychology of Addictive Behaviors. 2011;25:365–371. doi: 10.1037/a0022797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wise RA. The neurobiology of craving: Implications for understanding and treatment of addiction. Journal of Abnormal Psychology. 1988;97:118–132. doi: 10.1037//0021-843x.97.2.118. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. American Psychologist. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Wray JM, Gass JC, Tiffany ST. A systematic review of the relationships between craving and smoking cessation. Nicotine & Tobacco Research. 2013;15:1167–1182. doi: 10.1093/ntr/nts268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J, Azizian A, Monterosso J, Domier CP, Brody AL, Fong TW, et al. Gender effects on mood and cigarette craving during early abstinence and resumption of smoking. Nicotine and Tobacco Research. 2009;10:1656–1661. doi: 10.1080/14622200802412929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Zyphur MJ, Preacher KJ. Testing multilevel mediation using hierarchical linear models: Problems and solutions. Organizational Research Methods. 2009;12:695–719. doi: 10.1177/1094428108327450. [DOI] [Google Scholar]