Abstract
Background
Current guidelines recommend ≤90 minutes from first medical contact (FMC) to percutaneous coronary intervention (FMC2B) for ST segment elevation myocardial infarction (STEMI) patients. We evaluated the relationship between patient home distance from a percutaneous coronary intervention (PCI) center, prehospital electrocardiogram (ECG) use, and FMC2B time among patients with STEMI.
Methods
We performed a retrospective cohort study including all STEMI patients in the ACTION®-GWTG™ registry from 7/1/2008 to 9/30/2012 who were transported by ambulance to a PCI center. Patient home distance was defined as the driving distance from the patient's home zip code to the PCI center address. Distance was classified into tertiles, and linear regression was used to characterize the interaction between prehospital ECG use and patient home distance with respect to FMC2B time.
Results
Of the 29,506 STEMI patients, 19,690 (67%) received a prehospital ECG. The median patient home distance to the PCI center was 11.0 miles among patients with and 9.9 miles among those without a prehospital ECG. Prehospital ECGs were associated with a 10-minute reduction in the FMC2B time (p<0.0001), which was consistent across distance tertiles (11 vs 11 vs 10 minutes). The association between prehospital ECGs and shorter FMC2B was attenuated by 0.8 minutes for every 10 mile increase in distance (interaction p=0.0002).
Conclusions
Prehospital ECGs are associated with a 10-minute reduction in the FMC2B time. However, patient home distance from a PCI center does not substantially change this association.
Introduction
Approximately 250,000 patients suffer from an ST segment elevation myocardial infarction (STEMI) each year in the United States.1 Longer time to reperfusion in STEMI patients is associated with increased morbidity and mortality.2,3 The American Heart Association's goal is that STEMI patients who are transported to a hospital capable of performing primary percutaneous coronary intervention (PCI) should receive reperfusion within 90 minutes of first medical contact;4 however this goal is achieved in only a minority of patients.5
To improve timely access to PCI for patients, regionalized systems of care are being developed, and EMS bypass of non-PCI capable hospitals in favor of PCI centers for patients with STEMI on a prehospital electrocardiogram (ECG) is increasing.6-8 Prehospital ECGs reduce the time from first medical contact to device activation, or “balloon” time (FMC2B), which is the first attempt to mechanically open the culprit lesion and restore blood flow.9-13 However, the relative influence of the patient's distance from the PCI center on FMC2B time is unclear. The use of prehospital ECGs may mitigate the effect of long EMS transport times, reducing overall FMC2B time; however, this has not been well studied.
Therefore, we evaluated the relationship between prehospital ECGs and patient home distance from the PCI center on FMC2B time among patients with STEMI. Additionally, we evaluated the effect of presentation during work versus off-hours on FMC2B time. We hypothesized that the use of pre-hospital ECGs would be associated with shorter FMC2B time, an effect that would increase with longer patient home distance from the PCI center.
Methods
Study Design
We conducted a retrospective cohort study using data from the National Cardiovascular Data Registry's (NCDR®) ACTION Registry®-Get With The Guidelines (GWTG)™.14 The Registry is a voluntary quality improvement registry sponsored by the American College of Cardiology and the American Heart Association that focuses on patients with myocardial infarction. Definitions for the data elements of the registry are available at https://www.ncdr.com/webncdr/action/home/datacollection. The NCDR data quality program includes data abstraction training, data quality thresholds for inclusion, site data quality feedback reports, independent auditing, and data validation. Auditing of data has demonstrated chart review agreement of >93%.15 At participating sites this registry was either approved by an institutional review board, or considered quality assurance data and not subject to institutional review board approval based on individual site determinations. The Duke Clinical Research Institute serves as the data coordinating center to analyze de-identified data for research purposes.
Study Setting and Population
We included STEMI patients in the registry from July 1, 2008 through September 30, 2012, who were transported by ground EMS directly from the scene to a PCI hospital and underwent primary PCI. Patients were excluded for the following reasons:
STEMI first noted on subsequent rather than the initial ECG (n=5,107)
Non-system reasons for delay in PCI (n=5,860)
Missing or invalid zip codes (n=3,863)
Missing location of first ECG (n=26)
Missing time of first medical contact (n=330)
Missing time of first device activation (n=15)
Non-system reasons for PCI delay included difficult vascular access, cardiac arrest and/or need for intubation before PCI, patient delays in providing consent for the procedure, difficulty crossing the culprit lesion during the PCI procedure, and other documented reasons. The most common non-system delay was cardiac arrest and/or need for intubation before PCI, accounting for half (2,915) of the cases.
Measurements or key outcome measures
The primary outcome is time from first medical contact to device activation, defined as the time from first medical contact to first device activation in the cardiac catheterization lab. First medical contact is “the time when the patient was first evaluated by [EMS].” Device activation is “the time of the first mechanical treatment of the culprit lesion.” This definition encompasses all devices used to treat STEMI. If the culprit lesion intervention was unsuccessful, the time of guidewire introduction was considered the device activation time. This definition is standardized across the NCDR's registries. Patient home distance from the PCI hospital was defined as the driving distance in miles from patient's residential zip code to facility's zip code as calculated using Google Maps (Google Incorporated, Mountain View, CA). Work hours included 8am to 5pm from Monday through Friday; holidays, weekends; and all other times were considered off hours. Patients were classified as presenting during work versus off hours based on their time of arrival at the PCI hospital.
Data Analysis
Demographics and baseline characteristics were presented by prehospital ECG use. Patient home distance to the PCI hospital was classified into tertiles and the primary outcome was compared between the prehospital ECG yes versus no groups within each tertile. Categorical variables were compared using chi-square tests and continuous variables were compared using Kruskal-Wallis tests between the prehospital ECG yes versus no groups. To determine whether the use of prehospital ECG and patient home distance interact, time from first medical contact to reperfusion was fitted using two linear regression models, with and without adjustment. The unadjusted model included prehospital ECG, patient home distance, and the interaction as the independent variables. The adjusted model additionally adjusted for age, sex, race, weight, hypertension, diabetes mellitus, PAD, current/recent smoker, dyslipidemia, prior MI, prior PCI, prior CABG, prior HF, prior stroke, heart rate, systolic blood pressure, heart failure at presentation, shock at presentation, teaching hospital, hospital CABG capability, hospital region, and number of beds. In two different subgroup analyses, same approach was used, stratified by work hours and by gender. All analyses were performed using SAS software (version 9.3; SAS Institute, Cary, NC).
This research was supported by the American College of Cardiology Foundation's NCDR. The views expressed in this abstract represent those of the author(s), and do not necessarily represent the official views of the NCDR or its associated professional societies identified at www.ncdr.com.
Sources of Funding
ACTION Registry®–Get With The Guidelines™ is an initiative of the American College of Cardiology Foundation and the American Heart Association, with partnering support from the Society of Cardiovascular Patient Care, the American College of Emergency Physicians, and the Society of Hospital Medicine. The research described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health and by the National Heart, Lung, and Blood (NHLBI) Research Career Development Programs in Emergency Medicine. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
Results
We included 29,506 patients with STEMI in the registry during the 4-year study period who met inclusion criteria. Two-thirds of patients had a prehospital ECG. Overall, baseline characteristics of patients who did and did not receive a prehospital ECG were similar; however, patients who did not receive a prehospital ECG had more comorbidities and more critical presentations (Table I). The median FMC2B time was 82 minutes for those with and 92 minutes for those without a prehospital ECG (p<0.0001). Of those with a prehospital ECG, 64% met the 90-minute FMC2B goal, compared to 47% of those without a prehospital ECG (p<0.0001) (Table II.)
Table I.
Baseline characteristics.
| Prehospital ECG (N=19,690) | No Prehospital ECG (N=9,816) | |
|---|---|---|
| Demographics | ||
| Age (years)* | 60 (52-69) | 60 (52-71) |
| Male gender | 14,151 (71.9%) | 6,732 (68.6%) |
| Race/Ethnicity | ||
| White | 16,541 (84.0%) | 7,995 (81.5%) |
| Black | 1,759 (8.9%) | 1068 (10.9%) |
| Hispanic | 897 (4.6%) | 467 (4.8%) |
| Asian | 335 (1.7%) | 185 (1.9%) |
| Other/Missing | 158 (0.8%) | 101 (1.0%) |
| Insurance | ||
| Private/HMO | 11,339 (57.6%) | 5,426 (55.3%) |
| Medicare | 3,765 (19.1%) | 2,176 (22.2%) |
| Medicaid | 803 (4.1%) | 426 (4.3%) |
| Self-pay/None | 3,223 (16.4%) | 1,561 (15.9%) |
| Other | 560 (2.8%) | 227 (2.3%) |
| Medical History | ||
| Hypertension | 12,084 (61.4%) | 6,334 (64.5%) |
| Dyslipidemia | 10,531 (53.5%) | 5,311 (54.1%) |
| Diabetes mellitus | 4,068 (20.7%) | 2,252 (22.9%) |
| Prior MI | 3,769 (19.1%) | 2,039 (20.8%) |
| Home aspirin use | 6,092 (30.9%) | 3,190 (32.5%) |
| Presentation | ||
| Cardiac arrest† | 341 (3.9%) | 260 (7.2%) |
| Cardiogenic shock | 1,244 (6.3%) | 753 (7.7%) |
| During work hours | 7,728 (39.3%) | 3,503 (35.7%) |
| Geographic region | ||
| West | 3,110 (15.8%) | 920 (9.4%) |
| Northeast | 1,200 (6.1%) | 772 (7.9%) |
| Midwest | 4,537 (23.0%) | 3,107 (31.7%) |
| South | 10,843 (55.1%) | 5,017 (51.1%) |
Data presented as median (interquartile range)
Cardiac arrest was collected beginning in April 2011
MI=Myocardial infarction
Table II.
Patient outcomes by prehospital ECG.
| Prehospital ECG (N=19,960) | No Prehospital ECG (N=9,816) | P-value | |
|---|---|---|---|
| Time Intervals | |||
| FMC to device activation | 82 (68-98) | 92 (76-109) | <0.0001 |
| FMC to device activation ≤90 min | 12,586 (63.9%) | 4,623 (47.1%) | <0.0001 |
| FMC to hospital arrival | 31 (24-40) | 30 (22-38) | <0.0001 |
| Hospital arrival to CCL | 25 (14-38) | 37 (25-50) | <0.0001 |
| CCL arrival to device activation | 22 (17-29) | 22 (17-29) | 0.4314 |
| Door to Device activation | 50 (37-64) | 61 (48-75) | <0.0001 |
| In-hospital Events | |||
| Death | 540 (2 .8%) | 446 (4 .6%) | <0.0 001 |
| Death within 24 hours | 185 (1.0%) | 134 (1.4%) | 0.0008 |
| Post-admission MI | 177 (0.9%) | 107 (1.1%) | 0.1117 |
| Cardiogenic shock | 972 (5.0%) | 572 (5.9%) | 0.0011 |
All times are presented in minu tes as median (in terquartile range).
ECG=Electrocardiogram; FMC=First medial contact; CCL=cardiac catheterization laboratory; MI=Myocardial infarction
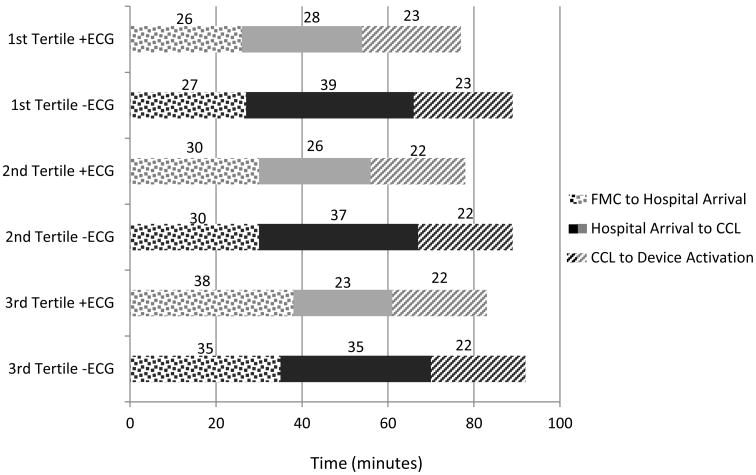
The median patient home distance to PCI center was 11.0 miles (IQR 5.8-21.5 miles) among patients with and 9.9 miles (IQR 5.0-19.8 miles) among those without a prehospital ECG. The association between prehospital ECG use and shorter FMC2B time was consistent across tertiles of distance (1st, median 11 minutes; 2nd, median 11 minutes; 3rd, median 10 minutes) (Table III). Within each tertile, the largest time differences between those with and without a prehospital ECG were seen in hospital arrival to cardiac catheterization lab arrival times (Figure I). In unadjusted linear model, the association between prehospital ECG use and shorter FMC2B time was attenuated by 0.8 minutes for every 10 mile increase in distance (interaction p=0.0002). After adjustment, the association was similar (attenuated by 0.7 minutes for every 10 mile increase in distance, interaction p=0.0010).
Table III.
Patient outcomes by distance tertiles.
| 1st Tertile <7.1 miles (N=9,876) | 2nd Tertile 7.1-16.2 miles (N=9,763) | 3rd Tertile >16.3 miles (N=9,867) | p-value | |
|---|---|---|---|---|
| Time Intervals | ||||
| FMC to device activation | ||||
| Overall | 84 (69 -100) | 84 (69 -101) | 89 (73 -107) | <0.0 001 |
| +ECG | 80 (66-95) | 80 (67-96) | 86 (71-103) | <0.0001 |
| −ECG | 91 (76-107) | 91 (76-108) | 96 (78-114) | <0.0001 |
| FMC to device activation ≤90 min | 6,066 (61.4%) | 5,996 (61.4%) | 5,147 (52.2%) | <0.0001 |
| FMC to hospital arrival | ||||
| Overall | 26 (21-33) | 30 (24-37) | 37 (27-49) | <0.0001 |
| +ECG | 26 (21-32) | 30 (24-37) | 38 (29-50) | |
| −ECG | 27 (20-34) | 30 (23-37) | 35 (25-46) | |
| Hospital arrival to CCL | ||||
| Overall | 32 (20-45) | 29 (18-42) | 27 (15-40) | <0.0001 |
| +ECG | 28 (17-40) | 26 (15-38) | 23 (11-35) | |
| −ECG | 39 (27-52) | 37 (26-50) | 35 (23-48) | |
| CCL arrival to device activation | ||||
| Overall | 23 (17-29) | 22 (17-29) | 22 (17-29) | 0.087 |
| +ECG | 23 (17-29) | 22 (17-29) | 22 (17-29) | |
| −ECG | 23 (17-30) | 22 (17-29) | 22 (17-30) | |
| In-hospital Events | ||||
| Death | 365 (3 .8%) | 336 (3 .5%) | 285 (2 .9%) | 0.8 5 |
| Death within 24 hours | 111 (1.2%) | 104 (1.1%) | 104 (1.1%) | 0.72 |
| Post-admission MI | 100 (1.0%) | 90 (0.9%) | 94 (1.0%) | 0.79 |
| Cardiogenic shock | 519 (5.4%) | 529 (5.5%) | 496 (5.1%) | 0.41 |
All times are presented in m inutes as median (interquartile range).
FMC=First medial contact; ECG=Electrocardiogram; CCL=cardiac catheterization laboratory; MI=Myocardial infarction
Figure I.
Time intervals by patient home distance and prehospital ECG.
ECG = Electrocardiogram; FMC = First medical contact; CCL = Cardiac catheterization laboratory
Subgroups
During off hours, the median FMC2B time was 91 minutes, compared to 74 minutes during work hours. In linear regressions, prehospital ECGs were associated with shorter FMC2B times, with an average decrease of 11.0 minutes during work hours and 9.8 minutes during off hours. These decreases were similar after the adjustment (10.7 minutes during work hours versus 8.9 minutes during off hours). During work hours, the association between prehospital ECGs and shorter FMC2B was attenuated by 1.4 minutes for every 10 mile increase in patient home distance (interaction p<0.0001). However, the association between prehospital ECGs and FMC2B was not changed across increasing patient home distance during off hours (interaction p=0.19). The adjusted analysis yielded similar results (data not shown).
The median FMC2B time in women was 89 minutes, compared to 84 minutes in men. Prehospital ECGs were performed in 64% of women and 68% of men. Among men, prehospital ECG use was associated with a 10.0 minute shorter FMC2B time, an association that was attenuated by 0.7 minutes for every 10 mile increase in distance (interaction p=0.01). Among women, prehospital ECG use was associated with a 12.2 minute shorter FMC2B time, an association attenuated by 1.1 minutes for every 10 mile increase in distance (interaction p=0.01). Results were similar after adjustment (data not shown).
Discussion
Using data from the NCDR over a 4-year period, we found that prehospital ECGs were associated with an approximately 10-minute reduction in FMC2B times. This association was relatively constant across increasing patient home distances from the PCI center and was not changed for patients presenting during off hours.
The reduction in FMC2B time in our data is clinically significant but more modest than that reported by others. Cone, et al., showed that prehospital ECGs combined with prehospital cardiac catheterization lab activation reduced door to balloon time by 50 minutes, from 87 to 37 minutes,16 and Camp-Rogers, et al., demonstrated a 22-minute reduction in FMC2B time with prehospital cardiac catheterization lab activation.10 In contrast, the 64% rate of patients with a prehospital ECG who met the 90-minute FMC2B goal in our study was similar to the 68% rate reported from five organized regional STEMI networks.13,17 In our data, prehospital ECGs were associated with a 12-minute reduction in door-to-balloon time (61 vs 50 minutes), with the difference between groups being a shorter time from hospital arrival to cardiac catheterization lab arrival and shorter door to balloon time for those with prehospital ECGs. Previous data from the NCDR showed a similar 14-minute reduction in door-to-balloon times with prehospital ECGs.12 The smaller differences in FMC2B time we observed may be due to improved processes of care – such as an ECG within 10 minutes of hospital arrival - for patients without a prehospital ECG, that have occurred due to initiative such as the American College of Cardiology's “D2B Alliance” and the American Heart Association's Mission:Lifeline programs, which have led to a substantial reduction in D2B times.
The association between prehospital ECGs and FMC2B in our data is likely modest due to heterogeneity in EMS and hospital practices in this large, nationwide sample. Previous studies suggest that maximum benefit is achieved when a STEMI system utilizes both prehospital ECGs and prehospital cardiac catheterization lab activation.8,13,21-23 Our data likely reflect system heterogeneity, with some systems consistently utilizing prehospital cardiac catheterization lab activation and emergency department bypass,16,24 while other systems may rely on emergency physician activation of the cardiac catheterization lab after patient arrival, potentially delaying reperfusion time. This may explain why we found that the reduction in FMC2B was similar for patients presenting on and off hours. In many STEMI systems, enthusiasm for prehospital ECGs and prehospital cardiac catheterization lab activation is tempered by concerns regarding false-positive pre-hospital ECG interpretation, especially in the absence of routine prehospital ECG transmission by EMS providers at the scene.17,25,26
Although the reduction in FMC2B stayed relatively constant with increasing transport times, we found that door to balloon times decreased with increasing patient home distance from the PCI center. This trend was driven by shorter times from hospital arrival to cardiac catheterization lab arrival, as the time from cardiac catheterization lab arrival to PCI was constant across distance tertiles. This likely reflects the use of prehospital ECGs and prehospital notification of the receiving hospital. Longer patient transport times provide more time for the cardiac catheterization lab to assemble prior to the patient's arrival at the PCI center. Thus, the cardiac catheterization lab is ready to take the patient sooner after hospital arrival, resulting in similar FMC2B times despite longer transport times
First medical contact to hospital arrival time was approximately 1 minute longer when a prehospital ECG is performed. While our data do not allow us to determine whether this minor delay is due to performing the prehospital ECG or due to bypassing a non-PCI capable hospital after the ECG shows STEMI, previous research shows that prehospital ECGs do not significantly prolong EMS on-scene time.23,27 This small delay in time to hospital arrival is more than offset by the time savings in door to balloon times and overall FMC2B times.
Women with STEMI have been shown to receive fewer prehospital ECGs, have longer EMS on scene to hospital intervals, and have longer door to balloon times when compared to men with STEMI.27-29 Our data demonstrate similar delays in processes of care among women. However, we found that the reduction in FMC2B time associated with prehospital ECGs was greater in women, suggesting that performance of a prehospital ECG and early recognition of STEMI are important steps in improving processes of care for women with STEMI.
Limitations
Because this registry does not collect EMS call location, we used patient home zip code as a surrogate for EMS call location, similar to prior studies.30 The majority of EMS scene responses are to residential locations, suggesting that home zip code is a reasonable surrogate for EMS call location.31 Also, we could not determine whether prehospital ECGs caused the reduction in time to PCI. We did not have information on the timing of cardiac catheterization lab activation, so we were unable to identify prehospital cardiac catheterization lab activations. Situations in which the cardiac catheterization lab was not activated based on the prehospital ECG would have biased results toward the null. Lastly, our study population reflects the heterogeneity in prehospital and hospital practices over a 4-year period; thus, our findings may not apply to all contemporary STEMI systems of care.
Conclusions
Prehospital ECGs are commonly used among STEMI patients and reduce FMC2B time by approximately 10 minutes. Patient home distance from a PCI hospital was not associated with this time interval, but presentation during off hours was associated with longer times.
Acknowledgments
Sources of Support: The first author is supported by the National Heart, Lung, and Blood (NHLBI) Research Career Development Programs in Emergency Medicine through grant #5K12HL108964-03. The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant #UL1 TR000002.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–5. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 3.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 4.O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:485–510. doi: 10.1016/j.jacc.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 5.Bagai A, Jollis JG, Dauerman HL, et al. Emergency Department Bypass for ST-Segment-Elevation Myocardial Infarction Patients Identified With a Prehospital Electrocardiogram: A Report From the American Heart Association Mission: Lifeline Program. Circulation. 2013;128:352–9. doi: 10.1161/CIRCULATIONAHA.113.002339. [DOI] [PubMed] [Google Scholar]
- 6.Le May MR, Wells GA, So DY, et al. Reduction in mortality as a result of direct transport from the field to a receiving center for primary percutaneous coronary intervention. J Am Coll Cardiol. 2012;60:1223–30. doi: 10.1016/j.jacc.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 7.Jollis JG, Mehta RH, Roettig ML, Berger PB, Babb JD, Granger CB. Reperfusion of acute myocardial infarction in North Carolina emergency departments (RACE): study design. Am Heart J. 2006;152:851 e1–11. doi: 10.1016/j.ahj.2006.06.036. [DOI] [PubMed] [Google Scholar]
- 8.Fosbol EL, Granger CB, Jollis JG, et al. The impact of a statewide pre-hospital STEMI strategy to bypass hospitals without percutaneous coronary intervention capability on treatment times. Circulation. 2013;127:604–12. doi: 10.1161/CIRCULATIONAHA.112.118463. [DOI] [PubMed] [Google Scholar]
- 9.Terkelsen CJ, Lassen JF, Norgaard BL, et al. Reduction of treatment delay in patients with ST-elevation myocardial infarction: impact of pre-hospital diagnosis and direct referral to primary percutanous coronary intervention. European heart journal. 2005;26:770–7. doi: 10.1093/eurheartj/ehi100. [DOI] [PubMed] [Google Scholar]
- 10.Camp-Rogers T, Dante S, Kontos MC, Roberts CS, Kreisa L, Kurz MC. The impact of prehospital activation of the cardiac catheterization team on time to treatment for patients presenting with ST-segment-elevation myocardial infarction. The American journal of emergency medicine. 2011;29:1117–24. doi: 10.1016/j.ajem.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 11.Curtis JP, Portnay EL, Wang Y, et al. The pre-hospital electrocardiogram and time to reperfusion in patients with acute myocardial infarction, 2000-2002: findings from the National Registry of Myocardial Infarction-4. J Am Coll Cardiol. 2006;47:1544–52. doi: 10.1016/j.jacc.2005.10.077. [DOI] [PubMed] [Google Scholar]
- 12.Diercks DB, Kontos MC, Chen AY, et al. Utilization and impact of pre-hospital electrocardiograms for patients with acute ST-segment elevation myocardial infarction: data from the NCDR (National Cardiovascular Data Registry) ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry. J Am Coll Cardiol. 2009;53:161–6. doi: 10.1016/j.jacc.2008.09.030. [DOI] [PubMed] [Google Scholar]
- 13.Rokos IC, French WJ, Koenig WJ, et al. Integration of pre-hospital electrocardiograms and ST-elevation myocardial infarction receiving center (SRC) networks: impact on Door-to-Balloon times across 10 independent regions. JACC Cardiovascular interventions. 2009;2:339–46. doi: 10.1016/j.jcin.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 14.Peterson ED, Roe MT, Rumsfeld JS, et al. A call to ACTION (acute coronary treatment and intervention outcomes network): a national effort to promote timely clinical feedback and support continuous quality improvement for acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:491–9. doi: 10.1161/CIRCOUTCOMES.108.847145. [DOI] [PubMed] [Google Scholar]
- 15.Messenger JC, Ho KK, Young CH, et al. The National Cardiovascular Data Registry (NCDR) Data Quality Brief: the NCDR Data Quality Program in 2012. J Am Coll Cardiol. 2012;60:1484–8. doi: 10.1016/j.jacc.2012.07.020. [DOI] [PubMed] [Google Scholar]
- 16.Cone DC, Lee CH, Van Gelder C. EMS Activation of the Cardiac Catheterization Laboratory Is Associated with Process Improvements in the Care of Myocardial Infarction Patients. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2013;17:293–8. doi: 10.3109/10903127.2013.773112. [DOI] [PubMed] [Google Scholar]
- 17.Rokos IC, French WJ, Mattu A, et al. Appropriate cardiac cath lab activation: optimizing electrocardiogram interpretation and clinical decision-making for acute ST-elevation myocardial infarction. Am Heart J. 2010;160:995–1003. e1–8. doi: 10.1016/j.ahj.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 18.Magid DJ, Wang Y, Herrin J, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA. 2005;294:803–12. doi: 10.1001/jama.294.7.803. [DOI] [PubMed] [Google Scholar]
- 19.Allaqaband S, Jan MF, Banday WY, et al. Impact of 24-hr in-hospital interventional cardiology team on timeliness of reperfusion for ST-segment elevation myocardial infarction. Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2010;75:1015–23. doi: 10.1002/ccd.22419. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez MA, Ben-Dor I, Wakabayashi K, et al. Does on- versus off-hours presentation impact in-hospital outcomes of ST-segment elevation myocardial infarction patients transferred to a tertiary care center? Catheterization and cardiovascular interventions : official journal of the Society for Cardiac Angiography & Interventions. 2010;76:484–90. doi: 10.1002/ccd.22515. [DOI] [PubMed] [Google Scholar]
- 21.Rezaee ME, Conley SM, Anderson TA, Brown JR, Yanofsky NN, Niles NW. Primary percutaneous coronary intervention for patients presenting with ST-elevation myocardial infarction: process improvements in rural prehospital care delivered by emergency medical services. Progress in cardiovascular diseases. 2010;53:210–8. doi: 10.1016/j.pcad.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Clark CL, Berman AD, McHugh A, Roe EJ, Boura J, Swor RA. Hospital process intervals, not EMS time intervals, are the most important predictors of rapid reperfusion in EMS Patients with ST-segment elevation myocardial infarction. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2012;16:115–20. doi: 10.3109/10903127.2011.615012. [DOI] [PubMed] [Google Scholar]
- 23.Swor R, Hegerberg S, McHugh-McNally A, Goldstein M, McEachin CC. Prehospital 12-lead ECG: efficacy or effectiveness? Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2006;10:374–7. doi: 10.1080/10903120600725876. [DOI] [PubMed] [Google Scholar]
- 24.Potter BJ, Matteau A, Mansour S, et al. Performance of a New “Physician-Less” Automated System of Prehospital ST-Segment Elevation Myocardial Infarction Diagnosis and Catheterization Laboratory Activation. Am J Cardiol. 2013;112:156–61. doi: 10.1016/j.amjcard.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Larson DM, Menssen KM, Sharkey SW, et al. “False-positive” cardiac catheterization laboratory activation among patients with suspected ST-segment elevation myocardial infarction. JAMA. 2007;298:2754–60. doi: 10.1001/jama.298.23.2754. [DOI] [PubMed] [Google Scholar]
- 26.Garvey JL, Monk L, Granger CB, et al. Rates of cardiac catheterization cancelation for ST-segment elevation myocardial infarction after activation by emergency medical services or emergency physicians: results from the North Carolina Catheterization Laboratory Activation Registry. Circulation. 2012;125:308–13. doi: 10.1161/CIRCULATIONAHA.110.007039. [DOI] [PubMed] [Google Scholar]
- 27.Aguilar SA, Patel M, Castillo E, et al. Gender differences in scene time, transport time, and total scene to hospital arrival time determined by the use of a prehospital electrocardiogram in patients with complaint of chest pain. The Journal of emergency medicine. 2012;43:291–7. doi: 10.1016/j.jemermed.2011.06.130. [DOI] [PubMed] [Google Scholar]
- 28.Coventry LL, Bremner AP, Jacobs IG, Finn J. Myocardial infarction: sex differences in symptoms reported to emergency dispatch. Prehospital emergency care : official journal of the National Association of EMS Physicians and the National Association of State EMS Directors. 2013;17:193–202. doi: 10.3109/10903127.2012.722175. [DOI] [PubMed] [Google Scholar]
- 29.Dreyer RP, Beltrame JF, Tavella R, et al. Evaluation of Gender Differences in Door-to-Balloon Time in ST-Elevation Myocardial Infarction. Heart, lung & circulation. 2013 doi: 10.1016/j.hlc.2013.03.078. [DOI] [PubMed] [Google Scholar]
- 30.Mathews R, Peterson ED, Li S, et al. Use of emergency medical service transport among patients with ST-segment-elevation myocardial infarction: findings from the National Cardiovascular Data Registry Acute Coronary Treatment Intervention Outcomes Network Registry-Get With The Guidelines. Circulation. 2011;124:154–63. doi: 10.1161/CIRCULATIONAHA.110.002345. [DOI] [PubMed] [Google Scholar]
- 31.Mississippi Department of Health. Emergency Medical Services; Jackson, MS: 1997. [Google Scholar]