Abstract
Platelet satellitism is a unique, uncommon, in vitro phenomenon seen in peripheral blood smears prepared from EDTA-mixed blood. This is seen in the form of platelets adhering to polymorphonuclear leucocytes imparting a rosette-like appearance. There is no definite causal association with any disease. The cause may be immunological or non-immunological. Severe rosetting may lead to a misdiagnosis of thrombocytopenia unless peripheral smears are examined. Here, we describe a case of incidentally detected platelet satellitism in a healthy 48-year old male subject during a routine check-up.
Keywords: Platelet satellitism, EDTA, Thrombocytopenia
Sir,
Platelets adhering to neutrophilic leucocytes is an interesting but relatively rare phenomenon for haematopathologists. This clustering of platelets around polymorphonuclear leucocytes imparting a rosette-like appearance has been termed as “ Platelet satellitism”.
A 48-year old male was advised to undergo complete blood count (CBC) as a part of routine check-up by his family physician. The results showed hemoglobin level of 13.6 gm/dl with normocytic normochromic RBCs. The total and differential leucocyte counts were within normal limits. The platelet count was 1.90 lakh/cmm. Examination of Leishman-stained peripheral blood film showed evidence of platelet satellitism in majority of the neutrophils (Fig. 1). All other parameters were within normal range. Blood was again collected from the subject using tri-sodium-citrate as anticoagulant. Two direct smears (without anticoagulant) were also made. The platelet satellitism was absent in the slides prepared from citrated blood and in the direct smears. The platelet count increased to 3.10 lakh/cu.mm, when calculated from citrated blood after correction for dilution.
Fig. 1.
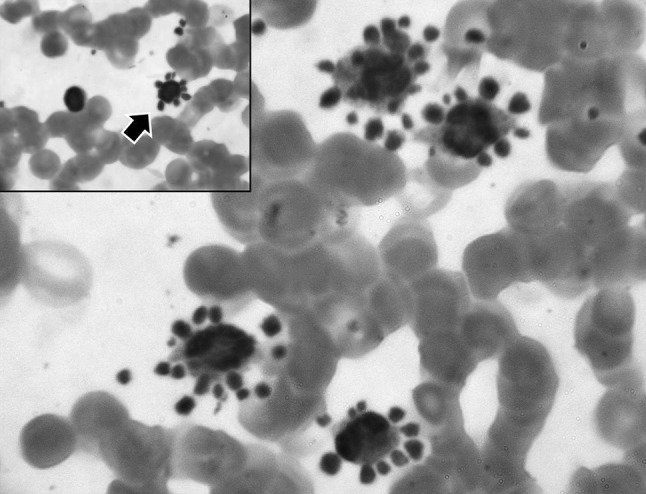
Microphotograph showing platelets adhering to the neutrophils forming rosettes. Only occasional lymphocyte seen to demonstrate this rosetting (Inset). Monocytes, eosinophils and most of the lymphocytes did not show this phenomenon. (Leishman stain; ×1,000 magnification)
Platelet satellitism was first described by Field and Macleod in the year 1963 as an in vitro phenomenon in peripheral blood film collected in Ethylene Diamine Tetra acetic Acid (EDTA) mixed blood and since then around 100 cases have been reported in literature [1]. This has been described in blood samples collected in EDTA only and not in anticoagulants like heparin, citrate, acid-citrate dextrose [1] and ammonium oxalate. Addition of kanamycin to EDTA anticoagulated blood (20mg/ml) has shown dispersion of platelets from the neutrophils [2]. When direct smears are made from these subjects this phenomenon disappear as happened in our case. Another interesting aspect is the lack of adhesion of platelets to leucocytes other than neutrophils however cases have been described when this adherence of platelets have been seen with lymphocytes or even basophils. The mechanism behind this observation is not well-understood but there is evidence that immunoglobin autoantibodies directed against the glycoprotein IIb/IIIa complex of the platelet membrane and the neutrophil Fc gamma (FcgRIII) receptor play a role [3]. EDTA may cause some alterations in the proteins in platelet and neutrophil membrane resulting in bridge formation between the two. Alternatively, the autoantibodies recognize the same epitopes in the membrane of platelets and neutrophils [4]. It may be possible that some cryptic epitopes in these cells may get exposed by EDTA and not by other anticoagulants [1]. A non-immunologic mechanism has also been proposed by Christopoulos et al. [4] which state that thrombospondin (or other α-granule proteins such as P-selectin) in presence of an activation stimulus is rapidly expressed on platelet surface favoring adhesion to neutrophils. More commonly seen in normal subjects, this phenomenon has also been observed in patients with vasculitis, lupus, mantle cell lymphoma, marginal zone B-cell lymphoma [5] and chronic liver disease [6], although a causal relationship is yet to be well-established.
The clinical importance of this phenomenon is that in some cases it may result in spurious thrombocytopenia or pseudothrombocytopenia leading to further unnecessary investigations. Thus, recognition of this in vitro phenomenon only re-emphasizes the necessity of age old practice of peripheral blood film examination.
Conflict of interest
The author declares that there is no conflict of interests.
Financial interest
The author has no financial interest or relationship with the organization where the work has been carried out.
References
- 1.Hernandez-Chjavarroa F, Vega B. Is Platelet satellitism an infrequent phenomenon? Rev Biomed. 2004;15:137–138. [Google Scholar]
- 2.Sakurai S, Tanigawa T, Nakahara K, Takenaka K, Ohkubo A. Effects of kanamycin on platelet satellitism and leukocyte adhesion phenomena. Rinsho Byori. 1995;43(2):142–148. [PubMed] [Google Scholar]
- 3.Bizzaro N, Goldschmeding R, von dem Rorne AE. Platelet satellitism is Fc gamma RIII (CD16) receptor-mediated. Am J Clin Pathol. 1995;103:740–744. doi: 10.1093/ajcp/103.6.740. [DOI] [PubMed] [Google Scholar]
- 4.Christopoulos C, Mattock C. Platelet satellitism and a-granule proteins. J Clin Pathol. 1991;44:788–789. doi: 10.1136/jcp.44.9.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bobba RK, Doll DC. Platelet satellitism as a cause of spurious thrombocytopenia. Blood. 2012;119((18):4100. doi: 10.1182/blood-2011-08-369173. [DOI] [PubMed] [Google Scholar]
- 6.Yoshikawa T, Nakanishi K, Maruta T, Takenaka D, Hirota S, Matsumoto S, et al. Anticoagulant-induced pseudothrombocytopenia occurring after transcatheter arterial embolization for hepatocellular carcinoma. Jpn J Clin Oncol. 2006;36(8):527–531. doi: 10.1093/jjco/hyl054. [DOI] [PubMed] [Google Scholar]


