Abstract
Purpose
Proximal humeral fractures are common and frequently associated with osteoporosis. Little is known about the association between the patho-anatomical fracture pattern of proximal humeral fractures and patient characteristics. The purpose of this six year longitudinal registry analysis of proximal humeral fractures was to study overall numbers, certain predefined pathoanatomical patterns and distribution compared with specific patient characteristics.
Methods
Data of patients treated between 2006 and 2011 in a country hospital that provides care >95 % of the city’s hospitalised patients with fractures was retrospectively reviewed. Data were analysed according to patient characteristics of age, gender, comorbidity, accompanying injuries and radiological analysis of pathoanatomical fracture patterns based on Neer and Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification.
Results
Eight hundred and fifteen proximal humeral fractures (67 % women/33 % men; mean age 66 years, range 19–99) were analysed. During the study period, an overall increase of 42.5 % was found: according to AO classification, 46 % were type A, 22 % type B and 32 % type C. Based on the Neer classification, 86 % were displaced, and 49 % were complex with more than three parts. Of complex fractures, 57 % were female patients >60 years. The number of complex fractures was five times higher in women >60 years than in men of the same age group.
Conclusions
An overall increase of inpatients with displaced proximal tibial fractures was documented. Interestingly, complex displaced proximal humeral fractures, especially in older women with comorbidities, accounted for the majority of cases. These results suggest that health-care planning and hospital-based therapeutic strategies should focus on this patient group.
Keywords: Epidemiology, Proximal humeral fractures, Proximal humerus fractures, Shoulder fractures, Classification, Neer, AO, OTA
Introduction
Proximal humeral fractures are common osteoporotic fractures [1]. The Neer and the Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification are frequently used for classification [2, 3]. Epidemiological studies have reported an overall increase in the incidence of proximal humeral fractures from 1970 to 2007 [4–6]. However, little is known about the association between specific patient characteristics and the pathoanatomical fracture pattern [7–10, 3]. We previously reported an increasing number of complex proximal humeral fractures, primarily three- and four-part fractures, according to the Neer classification in women >60 years [11].
The purpose of this retrospective longitudinal registry analysis was firstly to study specific patient characteristics (age, gender, comorbidities, trauma type, associated injuries) and secondly whether overall numbers and certain predefined prognostic classification categories (especially complex proximal humeral fractures based on Neer and AO classifications), changed between 2006 and 2011 compared with data from 1997 to 2005. Thirdly, we evaluated possible associations between patient characteristics and pathoanatomical fracture patterns.
Material and methods
The study is a retrospective longitudinal analysis based on data from a hospital registry, which was conducted in a country hospital for trauma surgery serving as a transregional level 1 trauma centre and university hospital. The institution treats >95 % of the city’s hospitalised patients with fractures. Between 2006 and 2011, the city’s population ranged from 83,740 to 83,248 inhabitants. We reviewed records of 815 proximal humeral fractures in adult inpatients and outpatients (>17 years of age), including 183 who were referred to the trauma centre, between 1 January 2006 and 31 December 2011; a further 18 paediatric fractures were excluded. With an initial phone survey, the privately practicing orthopaedic or trauma surgeons of the area, who do not provide surgical fracture treatment, were asked about the numbers of minimal displaced and displaced proximal humeral fractures in adult patients treated nonoperatively by them; these 192 fractures were also excluded.
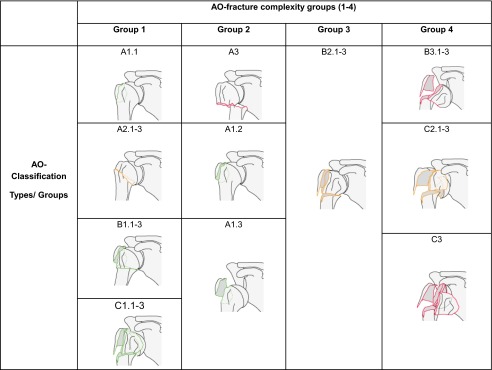
The internal hospital documentation system was used for chart and X-ray evaluation of all patients. Data recorded included age, gender, trauma type (high-energy trauma such as sports accidents, road traffic accidents, falls from heights > 2 m; low-energy, during walking, stumbling, syncope) and pre-existing comorbidities (cardiovascular; neurologic/psychiatric; alcohol and nicotine abuse; malignancies; underlying diseases, including bone diseases; confirmed diagnosis of osteoporosis; diabetes mellitus; obesity; rheumatoid arthritis and osteoarthritis; immunosuppressive therapy; thyroid disorders; pulmonary diseases; other metabolic disorders), fracture-associated local injuries (neurologic, vascular, open fracture) and fracture-associated general injuries (fractures of upper and/or lower extremities, polytrauma, others). We reviewed standard radiographs with anterior–posterior and axillary or scapula-Y views of all 815 patients and 147 computed tomography (CT) scans. Fractures were classified by an experienced trauma surgeon according to the three AO types (A–C) and nine AO groups (A1–C3) and parts (2–4), and Neer classification analysis (categories I–VII) [2, 3, 12]. AO classification was made according to the four predefined ordinal groups (1–4) of ascending complexity:
Group 1: A1.1 extra-articular, unifocal, nondisplaced greater tuberosity fracture; A2.1–3 extra-articular, unifocal, impacted metaphyseal fracture; B1.1–3 extra–articular, bifocal fracture with metaphyseal impaction; C1.1–3 articular fracture, slightly displaced
Group 2: A1.2 extra-articular, unifocal, displaced greater tuberosity fracture; A1.3 extra-articular, unifocal, greater tuberosity fracture associated with glenohumeral dislocation; A3 extra-articular, unifocal, nonimpacted metaphyseal fracture
Group 3: B 2.1–3 extra-articular. bifocal fracture without metaphyseal impaction
Group 4: B 3.1–3 extra-articular, bifocal fracture with glenohumeral dislocation; C2.1–3 articular fractures, impacted and significantly displaced; C3.1–3 articular fracture with glenohumeral dislocation (Table 1)
Table 1.
Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification arranged in four predefined groups of ascending complexity (groups 1–4) (Source: www.aosurgery.org)
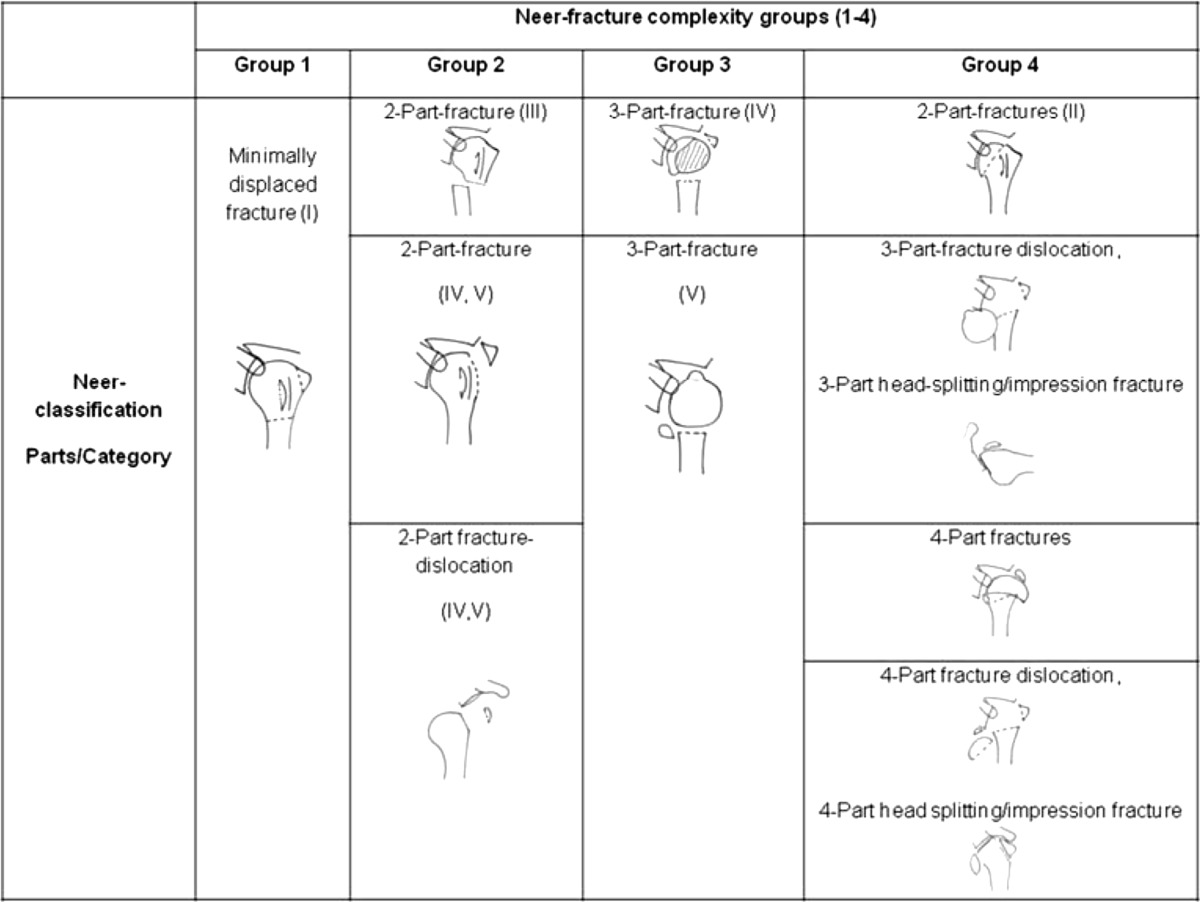
Neer classification is arranged in four predefined groups of ascending complexity:
Group1: minimally displaced fractures (category I)
- Groups 2–4: displaced proximal humeral fractures:
- Group 2: two-part fractures (category III surgical neck, IV, V), two-part-fracture dislocations (category IV and V)
- Group 3: three-part fractures
Table 2.
Neer classification arranged in four predefined groups of ascending complexity (groups 1–4). Groups 3 and 4 are defined as complex fractures
Statistical analyses were performed using JMP 8.0.2 (SAS Institute, Cary, NC, USA). Descriptive statistics were calculated, and categorical data were reported as percentages and numbers of the total. Chi-square test was performed to compare categorical data; level of statistical significance was p < 0.05.
Results
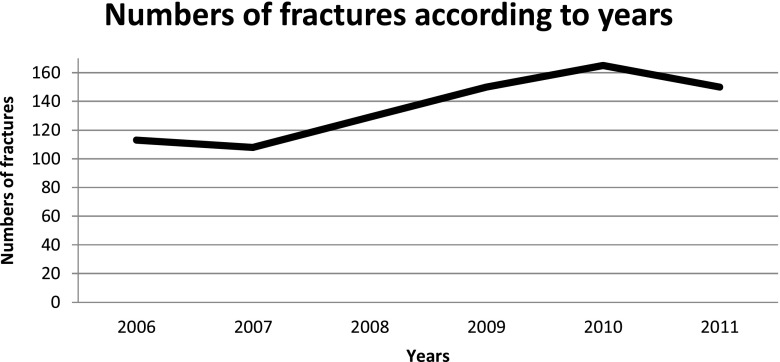
We reviewed 815 proximal humeral fractures. During the study period, the overall number of treated proximal humeral fractures increased from 113 and 108 in 2006 and 2007, respectively, to 165 and 150 in 2010 and 2011, respectively, which is an increase of 42.5 %. Of the 815 patients, 542 were women (66.5 %). Overall mean patient age was 66.3 years (median 69; range 19–99 years); 421 patients (51.7 %) were women >60 years, 162 (19.9 %) were men <60, 121 (14.8 %) were women <60 and 111 (13.6 %) were men >60. Of all patients,161 (19.8 %) had no comorbidity, 390 (47.9 %) had one or two, and 264 (32.4 %) had three or more; 611 patients (75.0 %) had a low-energy trauma. There was a significant association between low-energy trauma and female gender, age >60 years and presence of more than one accompanying comorbidity (p < 0.001). Proximal humeral fractures between 2006 and 2011 according to age group and gender are presented in Figs. 1 and 2
Fig. 1.
Proximal humeral fractures between 2006 and 2011
Fig. 2.
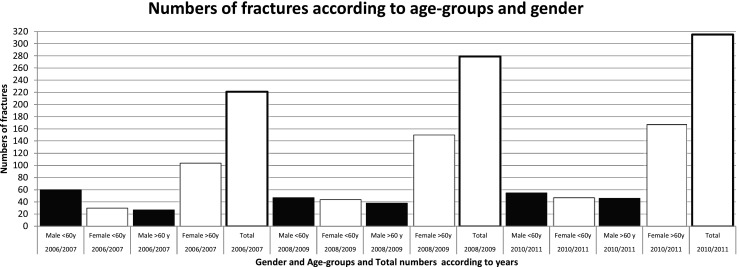
Proximal humeral fractures between 2006 and 2011 according to age and gender
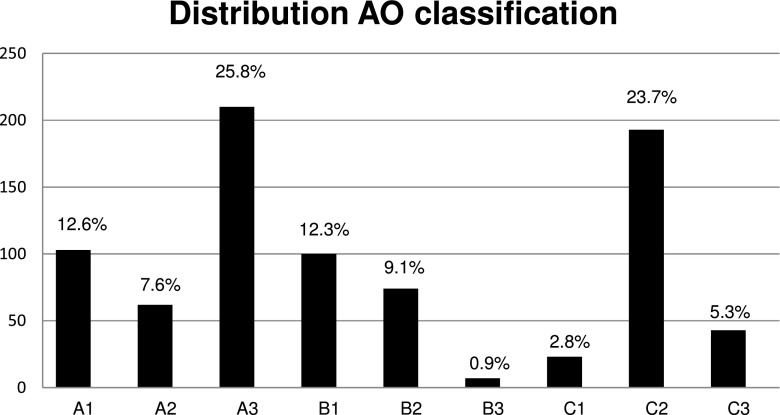
Six patients (0.7 %) had a fracture of the contralateral side at the same time and a further 12 (1.5 %) at some time during the study period. Twenty six patients (3.2 %) had associated local injuries (23 isolated neurological injury, one combined neurological injury and open fracture, one open fracture and one accompanying vascular damage). Six hundred and twenty-nine patients had no additional injuries; 186 (22.8 % ) also had one or more other injuries [15 polytrauma; Injury Severity Score (ISS) >16, (1.8 %], 60 fractures of the upper (7.3 %) and 31 of the lower (3.8 %) extremity, eight mild traumatic brain injury (1.0 %) and 99 other mainly soft tissue injuries (12.1 %). According to the AO classification, 375 (46.0 %) had type A, 181 (22.2 %) type B and 259 (31.8 %) type C. According to AO classification, the three most common groups were A3 [210 (25.8 %)], C2 [193 (23.7 %)] and A1 [103 (12.6 %)] (Fig. 3).
Fig. 3.
Distribution (numbers/percentages) of the 815 proximal humeral fractures according to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification
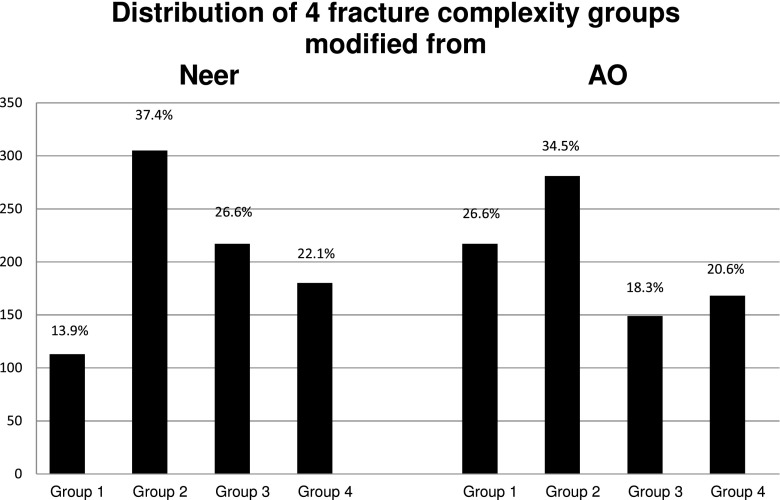
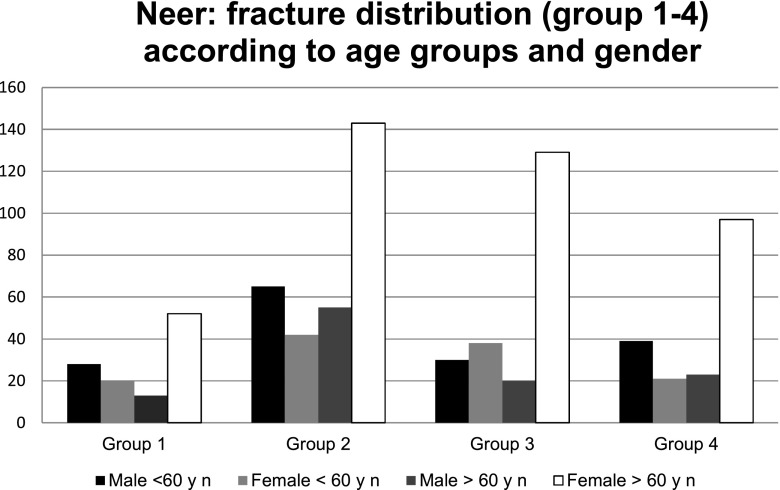
According to AO classification, 440 of 815 fractures (54.0 %) were B or C, 242 of which (55.0 %) were in women >60 years, 79 (18 %) in men <60, 68 (15.5 %) in women <60 and 51 (11.6 %) in men >60. Based on the Neer classification, 113 (13.9 %) were minimally displaced proximal humeral fractures (fracture-complexity group 1) and 702 (86.1 %) displaced proximal humeral fractures (fracture-complexity groups 2–4); 397 of 815 (48.7 %) were complex proximal humeral fractures, with three or more parts including fracture dislocations and head-splitting fractures (fracture-complexity groups 3 and 4). Of these 397 fractures, 226 (56.9 %) were women >60 years, and 69 (17.4 %) were men <60 years (Fig. 4).
Fig. 4.
Number and the percentage of the four complexity groups
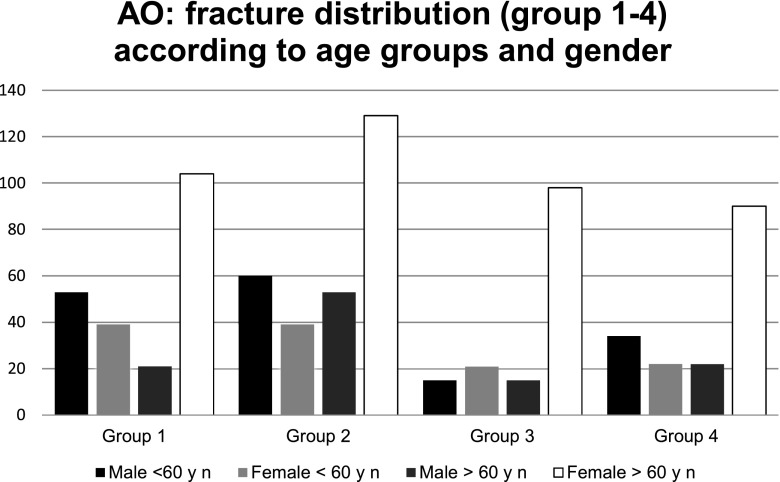
Fracture-complexity groups 3 and 4 based on Neer/AO classifications were 5.3 and 5.1 times higher, respectively, in women >60 years than in men of the same age group. Overall, there was a significant difference between fracture distribution according to fracture groups by age and gender (p = 0.001/0.0005). Figures 5 and 6 show the distribution of proximal humeral fractures (groups 1–4) according to age and gender with reference to AO/Neer classifications. Fracture severity according to the four groups showed no significant increase over the study period (p = 0.09).
Fig. 5.
Distribution of proximal humeral fractures (complexity groups 1–4) according to age and gender with reference to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification
Fig. 6.
Distribution of proximal humeral fractures (complexity groups 1–4) according to age and gender with reference to the Neer classification
One hundred and eighty-three of the 815 patients (average 31 patients per year; range 22–37) were diagnosed primarily elsewhere and then referred to our institution for treatment; 94 were women (51.4 %). Overall mean patient age was 57.0 years (median 57, range 19–85). Sixty-two (33.9 %) had no comorbidity, 79 (43.2 %) had one or two and 42 (22.9 %) had three or more. There were 98 patients (53.6 %) with a low-energy trauma; 19 of these 183 patients (10.4 %) had minimally displaced proximal humeral fractures (group 1), 71 (38.8 %) group 2, 39 (21.3 %) group 3 and 54 (29.5 %) group 4 fractures according to the Neer classification. According to AO classification, 41 (22.4 %) were group 1, 68 (37.2 %) group 2, 23 (12.6 %) group 3 and 51 (27.9 %) group 4. Further statistical analysis demonstrated no significant difference between gender (p = 0.34), age (p = 0.56), comorbidities (p = 0.09), trauma type (p = 0.62) and fracture complexity of referred patients over the six year study period (Neer, p = 0.58; AO, p = 0.35).
Discussion
The purpose of this long-term longitudinal registry analysis was to document specific patient characteristics and whether overall numbers of proximal humeral fractures and certain predefined prognostic classification categories have changed. In addition, possible associations between patient characteristics and fracture patterns were evaluated.
Within the recent years, epidemiological studies reporting mainly health insurance data have found an increase in the incidence of all proximal humeral fractures [13, 5, 14]. The most important information across all hospital registry studies is that the number of hospital-treated displaced proximal humeral fractures has also increased [7–9, 15, 16, 10, 3, 12]. In our institution, the numbers of proximal humeral fractures have more than doubled in 15 years, with an increase from 70 per year in 1997 to 150 in 2011. Factors influencing this change may include increasing life span, an accompanying increase in osteoporosis and a higher risk for falls primarily in the growing elderly population. In Germany, a female child born in 2009 has a ten year longer life expectancy than one born in 1960 (72.4 years vs. 82.7 years) [17]. Another strong risk factor for fracture is osteoporosis; 30 % of all postmenopausal women living in the USA and Europe have osteoporosis, with the subsequent general decrease in bone mass [18]. On the other hand, about 30–50 % of all people >75 years fall at least once a year [19, 20]. During their lifetime, half of all women >50 years sustain a fracture [21]. Another important aspect is that few studies have reported the pathoanatomical pattern from a large consecutive series of proximal humeral fractures. Studies from the 1970s report that 80 % of proximal humeral fractures were minimally displaced, categorised as group I Neer classification and have a shaft displacement of <1 cm and/or an angulation <45°. For such fractures, the treatment of choice remains conservative [12]. The overall numbers of minimally displaced proximal humeral fractures (group 1 according to Neer) in our study region was 35–40 %, including fractures treated by local physicians. Authors from Scotland, Japan and France report a comparable proportion of minimally displaced proximal humeral fractures of between 36 % and 51 % [15, 16, 10].
Compared to a former study the absolute numbers of proximal humeral fractures per year have more than doubled between 1997 and 2011. In this study, the majority of fractures (48.7 %) treated in our hospital were complex proximal humeral fractures, including fracture dislocations and head-splitting/impression fractures according to Neer. Using the AO classification, 39 % were nonimpacted and/or displaced type B and C fractures, including fracture dislocations; C2 fractures were found in 23.7 % of cases. These fractures are grouped under three- and four-part fractures according to the Neer classification. In the former study group, the percentage of complex fractures (groups 3 and 4) was 49.7 % [11]. Thus, with reference to this study, it should be noted that since 1997, the percentage of complex fractures remained relatively unchanged. We observed that complex fractures occurred predominantly in younger male patients after high-energy trauma. However, this group accounted only for 20 % of all fractures; the majority of complex fractures occurred in older women (more than half of all complex fractures after low-energy trauma). According to these patient characteristics, an association between proximal humeral fracture and osteoporosis is likely, even if osteoporosis is not documented explicitly. According to Court-Brown, 70–80 % of proximal humeral fractures are affected by an accompanying osteoporosis [22].
This study has some limitations. Regardless of the high number of patients (815) with proximal humeral fractures the study was limited to a special hospital situation. Our hospital is indeed the primary medical provider for fracture care, except for one fourth of minimally displaced proximal humeral fractures treated by privately practicing orthopaedic or trauma surgeons. However, when comparing the two time periods of 1995–2005 and 2006–2011, the percentage of minimally displaced proximal humeral fractures treated by the hospital remained unchanged at 14 % [11]. We also showed that the numbers of referred proximal humeral fractures from other hospitals was stable and did not change over the entire study period. Further evaluation of these referred fractures revealed especially that no significant shift to more older, sick patients with complex proximal humeral fractures had occurred. Therefore, we believe that taking all aspects mentioned into account, a representative sample for analysis was selected and a reliable statement for the chosen population can be made. However, comparisons with other published studies are problematic due to possible differences in patient selection criteria, follow-up time and classifications used. We diagnosed a substantially higher proportion (48.7 % of all fractures) of complex three- and four-part fractures, including fracture dislocations according to Neer classification compared with Court-Brown’s study with 13.3 %, Tamai’s study with 19.6 % and Roux’s study with 27 %, respectively [16, 10, 15]. However, the low observer reliability of the Neer classification reported elsewhere could to some extent explain the differences in reported incidences of minimally or displaced fractures and other fracture groups [23]. For this reason, only one colleague classified fractures to minimise intra- and interobserver variation [10].
The relatively high proportion of complex fractures could be one among many other reasons for the change in the therapeutic regime of proximal humeral fractures. Surgical intervention is becoming more popular, especially in central Europe. In contrast, the overall number of minimally displaced proximal humeral fractures presenting in hospitals, and presumably the use of conservative treatment, are declining. These data are supported by an international survey reporting that >60 % of hospitals in Germany, Austria and Switzerland treat >60 % of proximal humeral surgically [24]. This trend was also documented for northern Europe and the USA [5, 25].
Results of our study cannot be used to support any effect of surgical intervention for proximal humeral fractures. Results only suggest that health-care planning and hospital-based therapeutic strategies should focus on this patient population.
Conclusion
This long-term longitudinal registry analysis documents an overall increase of patients hospitalised with displaced proximal humeral fractures, which in older patients account for the majority of cases. Results suggest that health-care planning and hospital-based therapeutic strategies should focus on this patient population.
Acknowledgments
Conflict of interest
None.
Contributor Information
Christian Bahrs, Phone: 07071 6063823, Email: C.Bahrs@gmx.de.
Stojicevic Tanja, Email: tanja.stojicevic@hotmail.de.
Blumenstock Gunnar, Email: Gunnar.Blumenstock@med.uni-tuebingen.de.
Brorson Stig, Email: sbrorson@hotmail.com.
Andreas Badke, Email: abadke@bgu-tuebingen.de.
Stöckle Ulrich, Email: ustoeckle@bgu-tuebingen.de.
Rolauffs Bernd, Email: brolauffs@bgu-tuebingen.de.
Freude Thomas, Email: tfreude@bgu-tuebingen.de.
References
- 1.Hagino H, Yamamoto K, Ohshiro H, Nakamura T, Kishimoto H, Nose T. Changing incidence of hip, distal radius, and proximal humerus fractures in Tottori Prefecture. Japan Bone. 1999;24(3):265–270. doi: 10.1016/S8756-3282(98)00175-6. [DOI] [PubMed] [Google Scholar]
- 2.Jakob RP KT MK, Ganz R, Muller ME. . (1984) Classifications and aspects of treatment of fractures of the proximal humerus. In: JE Bateman and RP Welsh, Editors, Surgery of the shoulder, BC Decker, Philadelphia:330–343.
- 3.Neer CS., 2nd Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am. 1970;52(6):1077–1089. [PubMed] [Google Scholar]
- 4.Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87–92. doi: 10.1097/01.blo.0000194672.79634.78. [DOI] [PubMed] [Google Scholar]
- 5.Bell JE, Leung BC, Spratt KF, Koval KJ, Weinstein JD, Goodman DC, Tosteson AN. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am. 2011;93(2):121–131. doi: 10.2106/JBJS.I.01505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lippuner K, Popp AW, Schwab P, Gitlin M, Schaufler T, Senn C, Perrelet R. Fracture hospitalizations between years 2000 and 2007 in Switzerland: a trend analysis. Osteoporos Int. 2011;22(9):2487–2497. doi: 10.1007/s00198-010-1487-8. [DOI] [PubMed] [Google Scholar]
- 7.Kristiansen B, Barfod G, Bredesen J, Erin-Madsen J, Grum B, Horsnaes MW, Aalberg JR. Epidemiology of proximal humeral fractures. Acta Orthop Scand. 1987;58(1):75–77. doi: 10.3109/17453678709146347. [DOI] [PubMed] [Google Scholar]
- 8.Sonderegger J, Simmen HP. Epidemiology, treatment and results of proximal humeral fractures: experience of a district hospital in a sports- and tourism area. Zentralbl Chir. 2003;128(2):119–124. doi: 10.1055/s-2003-37765. [DOI] [PubMed] [Google Scholar]
- 9.Edelson G, Saffuri H, Obid E, Vigder F. The three-dimensional anatomy of proximal humeral fractures. J Shoulder Elbow Surg. 2009;18(4):535–544. doi: 10.1016/j.jse.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 10.Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72(4):365–371. doi: 10.1080/000164701753542023. [DOI] [PubMed] [Google Scholar]
- 11.Bahrs C, Bauer M, Blumenstock G, Eingartner C, Bahrs SD, Tepass A, Weise K, Rolauffs B. The complexity of proximal humeral fractures is age and gender specific. J Orthop Sci. 2013;18(3):465–470. doi: 10.1007/s00776-013-0361-x. [DOI] [PubMed] [Google Scholar]
- 12.Neer CS., 2nd Four-segment classification of proximal humeral fractures: purpose and reliable use. J Shoulder Elbow Surg. 2002;11(4):389–400. doi: 10.1067/mse.2002.124346. [DOI] [PubMed] [Google Scholar]
- 13.Dimai HP, Svedbom A, Fahrleitner-Pammer A, Pieber T, Resch H, Zwettler E, Thaler H, Szivak M, Amrein K, Borgstrom F. Epidemiology of proximal humeral fractures in Austria between 1989 and 2008. Osteoporos Int. 2013 doi: 10.1007/s00198-013-2339-0. [DOI] [PubMed] [Google Scholar]
- 14.Kannus P, Palvanen M, Niemi S, Sievanen H, Parkkari J. Rate of proximal humeral fractures in older Finnish women between 1970 and 2007. Bone. 2009;44(4):656–659. doi: 10.1016/j.bone.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 15.Roux A, Decroocq L, El Batti S, Bonnevialle N, Moineau G, Trojani C, Boileau P, de Peretti F. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res. 2012;98(6):715–719. doi: 10.1016/j.otsr.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 16.Tamai K, Ishige N, Kuroda S, Ohno W, Itoh H, Hashiguchi H, Iizawa N, Mikasa M. Four-segment classification of proximal humeral fractures revisited: a multicenter study on 509 cases. J Shoulder Elbow Surg. 2009;18(6):845–850. doi: 10.1016/j.jse.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 17.Pressekonferenz SB. Bevölkerung Deutschlands bis 2060. Berlin: Statistisches Bundesamt; 2009. [Google Scholar]
- 18.O’Brien MS, Donnell A, Miller J, Iven VG, Pascale M. An abnormal bone lesion of the scapula in a collegiate basketball player: a case report. J Athl Train. 2013;48(6):859–863. doi: 10.4085/1062-6050-48.3.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duckworth AD, Bugler KE, Clement ND, Court-Brown CM, McQueen MM. Nonoperative management of displaced olecranon fractures in low-demand elderly patients. J Bone Joint Surg Am. 2014;96(1):67–72. doi: 10.2106/JBJS.L.01137. [DOI] [PubMed] [Google Scholar]
- 20.Gimigliano F, Iolascon G, Riccio I, Frizzi L, Gimigliano R. Post-surgical rehabilitative approach to fragility fractures. Aging Clin Exp Res. 2013;25(Suppl 1):23–25. doi: 10.1007/s40520-013-0094-x. [DOI] [PubMed] [Google Scholar]
- 21.Lippuner K, Johansson H, Kanis JA, Rizzoli R. Remaining lifetime and absolute 10-year probabilities of osteoporotic fracture in Swiss men and women. Osteoporos Int. 2009;20(7):1131–1140. doi: 10.1007/s00198-008-0779-8. [DOI] [PubMed] [Google Scholar]
- 22.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37(8):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 23.Brorson S, Bagger J, Sylvest A, Hrobjartsson A. Diagnosing displaced four-part fractures of the proximal humerus: a review of observer studies. Int Orthop. 2009;33(2):323–327. doi: 10.1007/s00264-008-0591-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tepass A, Blumenstock G, Weise K, Rolauffs B, Bahrs C. Current strategies for the treatment of proximal humeral fractures: an analysis of a survey carried out at 348 hospitals in Germany, Austria, and Switzerland. J Shoulder Elbow Surg. 2013;22(1):e8–14. doi: 10.1016/j.jse.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 25.Huttunen TT, Launonen AP, Pihlajamaki H, Kannus P, Mattila VM. Trends in the surgical treatment of proximal humeral fractures - a nationwide 23-year study in Finland. BMC Musculoskelet Disord. 2012;13:261. doi: 10.1186/1471-2474-13-261. [DOI] [PMC free article] [PubMed] [Google Scholar]